Editor's note: This text-based course is a transcript of the webinar, Community-Based Occupational Therapy, presented by Krista Covell-Pierson, OTR/L, BCB-PMD
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
- After this course, participants will be able to describe the core principles and benefits of community-based occupational therapy as a service delivery model.
- After this course, participants will be able to identify potential community-based settings and populations that can benefit from occupational therapy services.
- After this course, participants will be able to list the steps and considerations for launching a community-based OT program, either independently or within an existing organization.
Introduction
I want to begin by thanking you all for taking the time to attend this course on Community-Based Occupational Therapy. This is one of my greatest passions, and I’m genuinely excited to share it with you. I hope today sparks some creative ideas and helps you think about occupational therapy in ways and settings you may not always associate with the field.
So let’s go ahead and dive in. I’ll start with my disclosures, followed by the limitations and risks of the course. Then I’ll outline our learning outcomes. We’ll discuss the core principles and benefits of community-based OT, explore some less obvious settings and populations that can benefit from our work, and then get into the practical side. I’ll share steps and considerations for launching a community-based OT program, whether you’re envisioning an independent practice, expanding your role within an existing organization, or pursuing something wholly new and creative. I always enjoy hearing innovative ideas and look forward to those conversations.
Whenever I take a course, I appreciate knowing who the presenter is, and I also like to understand who I’m speaking with to tailor my approach. Since I can’t meet each of you one-on-one, we’ll do a quick poll later to understand who’s here today.
I graduated from Colorado State University. I’m currently the CEO of Coval Care and Rehabilitation, which I founded 18 years ago. Over the years, I’ve pursued my board certification in biofeedback for pelvic muscle dysfunction. That came later in my career, after spending years in community-based practice and realizing just how often pelvic health—issues like incontinence—was a barrier to full participation. I had patients who wouldn’t leave their homes until late in the morning out of fear of an accident, which was devastating to their daily lives and engagement with their community. That realization drove me to dive deeply into pelvic health to serve my clients better.
On a more personal note, I have seven-year-old twin boys and a four-year-old son who keep me very busy, along with a goldfish, a tree frog, and a bulldog. Needless to say, our house is lively. I’m married, love to travel, actively engage in volunteer work, and have had the privilege of serving as president of OTAC. In fact, I’ll be speaking there again in the next couple of weeks on pelvic health and entrepreneurship.
One of the things I love most is mentoring other occupational therapy practitioners (OTPs). I see myself as an OT for others—someone who can provide guidance, encouragement, and support to clinicians and aspiring business owners. When I started practicing in the community nearly two decades ago, there were very few occupational therapists to connect with in that space, which often felt isolating. That’s why I now make it a priority to foster connection and collaboration. We’re stronger when we support each other, and I believe it’s essential for our profession to cultivate that culture of sharing.
If you have further questions or want to discuss community-based practice further, my contact information is included in the presentation, and I’m always happy to connect. For now, let’s move into a quick poll so I can get a sense of who’s here today, what your backgrounds are, and what perspectives you’re bringing into this conversation.
Poll (Live Event)
So, who is here today? Are you currently working in community-based care, hoping to start a community-based practice on your own or with someone else, or working in a setting where you’d like to grow community-based programming within your organization? Go ahead and make your choice, and then we’ll see the results together.
I always think it’s fun to reflect on your own community during exercises like this, because your community is going to have its own unique needs compared to mine. As we move through today’s discussion, I encourage you to view everything through the lens of your own surroundings and think about how you can adapt the ideas we talk about to fit your specific environment.
Alright, let’s take a look at what we’ve got. It’s a great mix across the board. Thirty-one percent of you are already working in community-based care, twenty-seven percent are hoping to start a practice, and forty-seven percent aim to build a program within your current workplace. I love seeing that, especially the large number working to create something within existing organizations. Hopefully, we’ll cover strategies and talking points today that will be useful for conversations with your administrators or management teams to help get those programs off the ground.
Bravo—you all bring such valuable perspectives. I’m excited to continue the conversation and appreciate your input on the poll.
Skilled OT Services Provided in Clients’ Natural Contexts
And when we talk about community-based occupational therapy, it’s essential to define what that means, how it works, and where it happens. When we say “community,” what are we really talking about?
Community-based OT refers to occupational therapy outside the traditional settings we usually picture, such as outpatient clinics, hospitals, or skilled nursing facilities. Those are common and vital areas for occupational therapy practitioners, but they’re not the only ones. Community-based practice extends into people’s homes, workplaces, schools, recreation centers, libraries, shelters, transportation systems, and other community environments.
It’s also worth pointing out the distinction between community-based OT and traditional home care, because they can look similar at first glance. For example, we often meet patients in their homes with Coval Care, which might lead people to assume we’re a home health service. But we’re not. We operate as a private practice, billing to Medicare Part B. In contrast, traditional home health agencies usually bill Medicare Part A, and their patients must meet strict criteria—such as being homebound and needing skilled medical services in the home.
This difference is at the heart of why community-based OT matters so much. Home health aims to stabilize clients so they remain at home and eventually safely transition to outpatient therapy. But life doesn’t only happen within the four walls of a home. If someone struggles to access the grocery store, manage public transportation, participate in church, or join recreational activities, traditional home health isn’t set up to help.
I experienced this firsthand in facility-based practice. I would discharge patients home, knowing they could return for outpatient services if needed, but I often felt limited. If we were working on bathing, cooking, or cognition, I knew the clinic setting wasn’t always relevant enough to prepare them for real life, truly. Context matters deeply in occupational therapy. Practicing a cooking task in a therapy kitchen isn’t the same as doing it at home with a person’s layout, tools, and routines.
The same is true for all of us—if something limited our ability to engage in the everyday places that make up our lives, we’d want support to get back to them. That’s where community-based OT shines: meeting people where they are, in the contexts that matter most, across different populations and settings.
This approach is effective for functional outcomes and is also more cost-effective. Even if a person doesn’t truly require home health services, they can still greatly benefit from OT without the additional expense to our healthcare system. That’s a win for clients, payers, and therapists who want to provide meaningful, real-world care.
Built On OT Foundational Principles
Community-based occupational therapy is built directly on our foundational principles as occupational therapy practitioners. Honestly, it’s always struck me as surprising that we don’t see it more widely implemented, because the need is so apparent—and as OTs, we feel that deeply. This work is in our blood.
At its core, community-based OT is about accessibility. It’s about helping people gain access to the places they need and want to go. And accessibility isn’t always as straightforward as it appears. A building may meet ADA requirements for a wheelchair, but is it also accessible to someone with dementia who might need extra support navigating the environment? That’s where OT comes in. We can even play a role in training businesses or organizations to create environments that are not just technically accessible but truly supportive. In my town, several businesses—restaurants, banks, shops—have gone through dementia-friendly training and proudly display stickers in their windows. Seeing this kind of initiative is so encouraging, because it tells those living with dementia and their families, “You are welcome here, we are prepared to support you.”
This aligns perfectly with the Person-Environment-Occupation (PEO) model, one of our core frameworks. In practice, that means we look closely at the individual—their strengths, challenges, and goals—alongside their environment. Then we figure out how to bring those two pieces together to allow meaningful engagement in occupation. Real life isn’t always visible from the clinic. In an outpatient session, a client may tell us that they can shower independently in their bathtub. But when you go to their home, you discover clutter stacked around, poor lighting, and hazards that make the task unsafe. Context changes everything, and community-based OT allows us to see and address those realities.
This also opens the door for prevention, another powerful benefit of community-based work. By intervening in real-world environments, we can reduce fall risk, prevent declines in daily living skills, and help clients ward off depression by ensuring they remain connected and engaged. Participation is central to this approach. We want people to participate in the activities that matter most to them, and our interventions to be truly client-centered. That means taking what is essential to them and making it equally important to us, so together we can support full participation in their life and community.
Quotes About Community-Based Care
AOTA Statement
A statement from the American Occupational Therapy Association reminds us that AOTA fully supports community-based practice. They highlight how it expands OT’s scope, supports holistic care, and promotes occupational participation in natural contexts. I agree; it’s a well-crafted statement, and I appreciate seeing that endorsement.
That said, I think it’s worth pausing on the word “expands.” Because to me, this isn’t actually an expansion of our scope—it’s always been part of our scope. What community-based practice really expands is how the broader world sees us and understands what we do.
Helping someone get back to work is in our scope. Supporting them so they can attend their grandkids’ soccer game is in our scope. Our scope is ensuring they can get to their doctor’s appointments safely. These are not additions; they’re core to who we are as occupational therapy practitioners. What’s often missing is awareness. The community doesn’t always realize how far-reaching our role can be, so part of our job is to make that visible—to show just how expansive and impactful OT has always been.
Munar et al. (2021) Quote
Here’s another quote I appreciate: community-based OT significantly improves functional outcomes, psychosocial well-being, and participation when interventions are rooted in real environments. This captures the essence of why this model is so powerful. When we work with people in the actual settings where they live, work, and play, the outcomes are naturally more relevant, meaningful, and sustainable.
If you’re looking to develop a program within your workplace, this is the research and evidence you want to keep at hand. It’s compelling, and it speaks directly to decision-makers' priorities. Upper management is always interested in strategies that demonstrate better outcomes while reducing costs. Community-based OT does precisely that—it helps keep people healthy, engaged, and thriving, reducing hospital admissions and readmissions.
The heart of it is simple for us as OTPs: We want people to remain as healthy as possible and fully participate in their lives. For administrators and leadership, the added benefit is that community-based practice aligns with organizational goals of lowering costs and improving measurable outcomes. That combination makes it a powerful case to present.
What Does Community-Based OT Look Like?
What does community-based OT actually look like? On the surface, it can feel similar to the kinds of therapy you may have done in more traditional settings, but the scope is much broader and more dynamic.
One of the most significant shifts is that we have to look at the whole patient profile in ways we might not in a hospital or clinic setting. Of course, we remain client-centered—that’s at the very core of occupational therapy, and I don’t need to convince you of that. However, the way we apply that principle looks different in the community.
Take environmental adaptation, for example. In someone’s home, we can often make modifications—grab bars, furniture rearrangement, lighting changes—if the client is willing. However, in public settings like the grocery store, we can’t redesign the environment to fit their needs. Instead, we adjust how we prepare clients, train them, and sometimes educate community partners. We’ll get into more of what that looks like.
Caregiver and family training also becomes essential in community-based OT. Families may be navigating situations they’ve never experienced before, and they play a critical role in reinforcing skills and strategies in natural contexts.
When it comes to treatment, sometimes our focus is on compensation, and other times it’s on restoration. For instance, I once worked with a client with a leg amputation. He desperately wanted to get back into the community but was terrified of losing his balance in crowded spaces. We started with small outings to places that weren’t very busy, gradually moving to larger, more crowded environments. It was about building his confidence, helping him compensate for what couldn’t be restored, and giving him the tools he needed to participate again fully.
In other cases, we might be aiming to help restore function. Say someone has had a hip replacement and wants to return to grocery shopping. Our role is to build strength, endurance, and safe movement strategies to restore their independence in real-world activities.
Another key feature of community-based OT is the depth and length of treatment plans. These sessions can naturally take more time. For example, supporting a client through a grocery store visit involves far more steps, problem-solving, and real-world challenges than facilitating a shower at home. That increased complexity creates opportunities for meaningful progress, but we also need robust treatment plans that account for longer and more varied interventions.
In short, community-based OT involves walking alongside people in the environments that matter most to them, adapting, compensating, restoring, and empowering—always anchored in participation. Figure 1 shows some examples.

Figure 1. Images of clients doing different tasks.
I always like to show real people doing real things, because it brings these concepts to life. These are actual clients and real situations from my company, and I think it’s fun to see what people are doing in the community.
At the top, you can see a gentleman in a turquoise T-shirt. In that picture, a PT and an OT lead a boxing class for people with Parkinson’s. Research shows that boxing is incredibly beneficial for individuals with Parkinson’s, so twice a week, this clinic in Fort Collins hosts a class dedicated just for them. If you notice, many of the clients are on the floor, and they all have Parkinson’s. The OT and PT are there to adapt and modify each participant's activities, ensuring everyone can fully engage. But the focus is broader than boxing itself—it’s also about working on things like voice projection, large amplitude movements, and, most importantly, participation. If someone misses class for a while, the therapists check in. They can bring therapy directly into the house if something needs attention at home. It demonstrates how community-based practitioners can be chameleons—floating between a group boxing class, a client’s home, or wherever support is needed.
Below that is my client, Crystal. She was born with a progressive neurological disease and has used a power wheelchair since she was four years old. She has never walked, so the chair is her lifelong partner. Recently, she was due for a new one, and this time we could provide her with a standing chair—something she’d never had before. One of her goals was to be a bridesmaid at her best friend’s wedding and to stand during the ceremony. With her new standing chair, we practiced, problem-solved, and built her confidence until she was ready. On the wedding day, she proudly came down the aisle standing, just like the other bridesmaids. That’s real client-centered practice, rooted in meaningful participation. We’re now working with her on another goal—being able to stand at a concert.
In the center is another client, pictured with her daughter. Her husband of nearly 60 years had recently passed away, and she was suddenly faced with doing things alone, like going to the bank, which had always been a shared responsibility. She also relied on a walker, so managing it while getting in and out of the car—things her husband used to do—was intimidating. We focused heavily on community outings to help her independently navigate daily activities. Over time, her confidence grew, and now she’s back to being active and independent all over town.
At the top right, you can see an example of community-based OT merging into advocacy and environmental modification. For that client, a stair lift was the safest and most practical option for accessing her home. It wasn’t about adding a ramp but installing something that fit her needs. Being out in the community often gives us opportunities to notice issues like unstable railings and advocate directly for safer spaces.
And finally, in the bottom right, you see home modification in action. In Colorado, Medicaid offers around $14,000 per lifetime for clients to make safety-related modifications to their homes. We’re actively helping patients access those funds and make tangible changes. In this case, we removed a bathtub and replaced it with a walk-in shower, dramatically improving safety and independence.
That’s the beauty of community-based OT. We’re everywhere that matters to our patients—at clinics, in homes, out in the community, and inside businesses—because all of it plays a role in enabling meaningful participation.
Real-Life Applications
Let’s talk about the different populations we serve, our settings, and what meaningful occupations look like across community-based practice. One of the things that excites me most about this area of OT is just how creative and diverse practitioners are in meeting the needs of their communities. I’ve had the privilege of meeting therapists all over the country, and I’m always so impressed with the unique ways people implement community-based programs.
For instance, I know of therapists who work specifically with individuals recovering from strokes by engaging them in hands-on mechanical activities like working on cars. This therapy is therapeutic in fine motor skills, cognition, and sequencing, but it also taps into meaningful occupations that bring back a sense of identity, purpose, and confidence. That, to me, is the heart of OT—connecting the work directly to what matters most to the person.
Another great example is the work some therapists do around driving evaluations. Becoming a certified driving rehabilitation specialist is a significant undertaking, but it’s deeply needed. Driving is a critical piece of independence, and we need more certified professionals to assess, train, and support individuals in this area. I was speaking with a colleague earlier this week who told me her caseload is increasingly made up of young adults—about 21 or 22 years old—who are neurodivergent and just beginning to learn to drive. That’s an essential part of their participation, and OT is uniquely suited to provide both driving rehabilitation and related life skills support at home.
And of course, we often think about working with older adults in community-based OT. This lovely woman in Figure 2 is an example of the population many of us start with or picture first, and while that’s true and vitally important, it’s far from the only group we can serve. From young adults learning independence to individuals managing chronic conditions, from stroke survivors to people navigating cognitive changes, community-based occupational therapy touches every stage of life.
The point is that meaningful occupations are unique to each population and each person. Whether driving, mechanical hobbies, social engagement, or managing daily life skills, our role is to support full participation in whatever brings value and purpose to the individual’s life.

Figure 2. A woman cooking while sitting.
Working with an OTP can benefit all kinds of populations, and it's our job to help people understand that. So, we'll discuss population settings and some meaningful occupations we can engage folks in.
Populations
When we think about populations in community-based OT, older adults aging in place are often the first group that comes to mind. It’s common, needed, and where many of us start—thinking about safety, fall prevention, driving, and helping people remain independent in their homes as long as possible. However, the scope of who we can serve and how we can serve them is much broader.
Take pre- and post-surgical candidates. I worked with a woman who was prescribed OT before her total knee replacement, which was such a win. We prepped her environment, installed a raised toilet seat, rehearsed how to get into her tub safely, and practiced with a sock aide. Because she had these strategies before surgery, she went into the procedure more confident and less overwhelmed. Her recovery process was more complicated than expected—low confidence, lingering anesthesia effects—but step by step, we built her back up. We progressed from basic ADLs to reducing her reliance on a walker and cane to kitchen safety tasks like carrying bowls of water and hot pans, and finally to community outings. Even with solid physical recovery, her confidence was the biggest hurdle—she once refused to get out of the car at Starbucks because she was afraid she might fall. With time and graded exposure, she returned to coffee dates, the gym, and her volunteer work. That’s the value of OT during transitional times like surgery.
For people with chronic conditions such as ALS, Huntington’s, or Parkinson’s, traditional home health often isn’t an option. These clients usually face profound fatigue just from daily living. Community-based OT allows us to meet them where they are, conserving their energy and helping them adapt routines without the burden of traveling to a clinic. Often, the consistency of those visits builds trust to the point where we take on the role of a skilled friend—someone who understands their journey and helps them navigate it.
Pediatric clients are another area where community-based practice makes a huge difference. Whether the child is navigating cancer, developmental disorders, or disabilities, OT can help them and their families engage more fully with peers, school, and play. We might introduce assistive technologies, provide coaching, or allow children to participate more fully in their communities. For young adults aging out of pediatric services around 21, OTs often become a bridge to adult life, guiding them in building independence, routines, and new life skills as other services drop off.
Mental health is also an exciting and vital area. My first OT job was in an inpatient psychiatric hospital, and I saw so many clients cycle back repeatedly after discharge because they had no community support systems. Community-based OT can break that cycle by helping with structure, routines, and occupation-focused strategies that support recovery and participation outside the hospital. This is equally true for populations in transitional housing, such as individuals in addiction recovery or people reentering society after incarceration.
Occupational therapy can be a lifesaver for perinatal and postpartum populations. When you combine the physical recovery from birth or surgery with the demands of a newborn and the exhaustion that comes with it, daily function can feel overwhelming. Community-based interventions allow us to meet moms right at home, help them restore functional routines, and support them physically and emotionally through that transition.
We also see OTs partnering with agencies that serve unhoused individuals and families. I recently saw a program where nurses provided medication management and then brought on an OT to address skills and environmental challenges. Validating our role in such spaces is powerful and needed.
People with brain injuries are another group that benefits deeply from OT. Because brain injuries can be largely invisible, clients often struggle with executive function, memory, and safety in ways that are not obvious to others. We can support their return to work, social life, and community participation, tailoring strategies to real-world challenges. Transitions to alternate transportation can be daunting for clients retiring from driving, but OTPs can guide them in exploring new systems and strategies that preserve independence.
Because these populations are so diverse, we need portable, flexible, and meaningful assessments in community contexts. The Canadian Occupational Performance Measure (COPM) is a go-to tool, helping clients identify and rate what matters most to them while giving us measurable outcomes. The Kitchen Task Assessment is excellent for observing cognitive and functional skills in real ADL contexts like cooking. I also like the Assessment of Life Habits, which looks at daily routines and social roles, highlighting adaptations or assistance needed. These tools are practical, portable, and fit right into real-life environments.
Community-based OT takes us far beyond the walls of a hospital or clinic. We work in homes, neighborhoods, businesses, and even travel settings. It allows us to focus on what matters most to each client—supporting participation, independence, and well-being in the contexts that define their lives. Figure 3 shows a client who has a temporary disability, but she is headed out to a wedding with her daughter.

Figure 3. Client traveling to a wedding.
We educated her and her daughter on how to manage a rented wheelchair, how to take care of the skin under that boot, and other things. She has a grippy thing on her shoe and a cane. She is ready to go and have some fun.
Settings
There are so many different settings and contexts where community-based OT can take place, and the variety is part of what makes this work so rewarding. Private homes are often the first space that comes to mind, but it goes well beyond that. Assisted living, independent living, and memory care facilities are all places where occupational therapy has a role, even if those facilities already contract with therapy providers. You can bring that expertise into those environments if you have a specialty, such as lymphedema management. It may mean checking in at the front desk, coordinating with staff, and respecting their systems, but your skills are still needed and welcomed in those settings.
Parks are another great setting, and one we use often in Colorado. They give clients safe spaces to practice balance and mobility on varied terrain and allow for spread-out practice without feeling crowded. Trails are beneficial for confidence-building and often match people’s real-world goals if they want to stay active outdoors. Pools can also be powerful therapeutic spaces. In Denver, one OT built a thriving aquatics program for kids using water-based therapy. Some therapists use pools with adults, too, whether for groups or individual sessions. Billing for aquatic activities can be complicated, especially with Medicare, so knowing the rules is essential, but the functional and engagement benefits can be enormous.
Rec centers are another rich space. We often work alongside clients as they learn gym equipment, pacing strategies, or the logistics of managing locker rooms and clothing changes. I once helped a client who wasn’t struggling with exercise but with the real task of managing her bathing suit and dressing independently before getting into the pool. Those community routines matter just as much as the exercises.
Workplaces and churches also provide opportunities. People often stop going to church because they feel limited by low vision, incontinence, or mobility challenges. OTs can help bridge those barriers so clients can return to what’s meaningful. Coffee shops and support groups are another example. Simply going to that first support group can be overwhelming. An OTP might help by providing strategies beforehand, coaching on how to participate (or say no if they’re not ready), and monitoring the client’s comfort and reactions during the group. While not every moment in that setting is billable, the skilled support makes a tremendous difference.
Grocery stores are a practical and often essential therapy site. Since the pandemic, many stores have removed benches and seating, making pacing more difficult. Managing the grocery trip can be exhausting for someone with a walker, an oxygen tank, or balance issues. Practicing strategies in real time at the store is invaluable.
Other creative settings really highlight the flexibility of community-based OT. Rock climbing gyms are now being used in programs for neurological rehabilitation, with strong evidence supporting benefits for conditions like MS. Golf courses are another setting where OTPs are active. I don’t golf myself, but many colleagues do, and they’ve taken patients—post-surgical, living with dementia, or managing other conditions—back onto the course to rebuild confidence and restore their occupations.
And it doesn’t stop there. Concerts, banks, and community events are all real places where OTPs have worked with clients. The common thread is simple: go where life happens and provide the support, skills, and adaptations that allow individuals to participate fully. That’s the essence of community-based OT.
Here's an example of Maddie in Figure 4, an occupational therapist, practicing car transfers with a family so that they can start going back out. They're learning how to get in and out of the car.

Figure 4. Client practicing a car transfer with an OT with family watching.
This is where it starts, because you have to figure out transportation to get out into the community. So you can always ask how to get out into the community.
Meaningful Occupations
We discussed meaningful activities like attending an exercise class at the pool or buying coffee independently. On the surface, those might sound simple, but they often require very intentional OT support in practice.
For example, I had a patient who was a veteran from Vietnam with a brain injury. He struggled with social cues despite being incredibly kind and well-meaning. When he went to the coffee shop, he would end up monopolizing the barista’s time and talking for hours, which wasn’t appropriate and left him feeling isolated when he realized people were pulling away. For him, just getting out of the house was important—he’d been staying home too much and was battling depression. We worked on internal cues and external strategies to make his coffee visits manageable and functional, allowing him to connect with others more sustainably.
Managing appointments is another important area. Sometimes, I meet patients at their physician appointments to support them and build relationships and communication with their care team. It’s a great chance to advocate, share insights, and collaborate more effectively.
Transportation is also a big one. With Uber and Lyft becoming more widely used, we can support patients in learning how to access and use these services safely and independently. I’ve graded sessions where we would ride Uber together, then progress to the patient arranging and taking a solo trip. I’ll never forget the pride on one client’s face when they arrived at the library independently after their first solo ride.
Medical equipment like oxygen tanks or other devices can significantly hinder community participation. Many patients resist going out simply because managing those tools feels overwhelming. A huge part of our work is problem-solving around those challenges to make participation possible and less stressful.
Work can be another area where OT advocacy differentiates between someone thriving and leaving the workforce. I supported a woman in a university job after a brain injury left her exhausted by fluorescent lights, meetings, and computer screens. Her team encouraged her to go on disability, but she desperately wanted to keep working. We modified her environment by adding a cot in her office for rest breaks, adjusting lighting, and setting up computer screens—and I also met her at work to troubleshoot. She was able to stay employed full-time on her own terms.
I’ve also supported clients in retail work. One gentleman with Parkinson’s worked as a greeter at Walmart. By the end of his shift, he was bent forward and fatigued, and the company wasn’t happy with his posture at the front door. Through advocacy and negotiation, we secured a podium he could rest on, which allowed him to continue working with dignity.
Community-based practice can extend to travel, too. Helping someone plan for a cruise or vacation and staying in public are just as crucial to quality of life as daily activities.
And of course, we can never forget about caregivers. They are often the backbone of daily support, and their well-being directly affects our clients’ outcomes. I see caregivers and clients as partners in need of equal attention. When we support both, we strengthen the entire system of care. Figure 5 shows a caregiver.

Figure 5. A caregiver.
Even if I’m not billing a caregiver’s insurance, I prioritize addressing their needs alongside the patients'. When the caregiver is healthier, more confident, and more supported, they can better care for their loved one. That might mean helping them figure out how to fit in a simple walk, set up safe transitions so they feel comfortable leaving the house, or carve out time to see friends or play Bunko without being weighed down by guilt or fear that their partner will be unsafe.
Supporting caregivers in staying engaged in their communities is just as important as supporting our patients. These conversations can be eye-opening because caregivers often express deep feelings of loss: “My life isn’t as important anymore,” or “I don’t have time for myself.” Those are powerful indicators of burnout, and we know how damaging it can be for them and the patient they’re caring for.
Part of our role is to normalize those feelings, help problem-solve barriers, and build routines that protect time and energy for the caregiver. By doing so, we’re not just treating one person; we’re supporting the entire care system.
Treatment Ideas
We talked about a lot of this type of stuff. Whether on a trail, as in Figure 6, or at a grocery store, you're still looking at things similarly if you were in a home care setting or a clinic.

Figure 6. Helping a client on a trail.
The environment in community-based practice is constantly changing, and that’s one of the things that keeps you sharp as a practitioner. In a hospital, the walls, equipment, and routines are consistent day after day. But in the community, your therapy context shifts with every client and session—it’s dynamic and unpredictable, making it so powerful and occupation-centered.
Take the woman I mentioned earlier, whose husband had passed away. She had never paid her rent before but wanted to take control of that task. The bank happened to be across the street from her apartment. That became our treatment environment. It wasn’t about role-play or simulation—it was about the real activity, in the real setting.
We started with her leaving her apartment alone, without her daughter, using her walker. That alone required attention to confidence and safety. Then we moved down the sidewalk, navigated a ramp, crossed a fairly busy street at her slower pace, and tackled the incline of a curb cut into the bank’s parking lot. She tended to look at her walker too much, so we worked on keeping her eyes up and monitoring her environment.
Getting to the bank door and opening it was harder than expected, which we wouldn’t have anticipated if we hadn’t been there together. She made it inside, paid her rent, and then we turned around to go back. By the time she returned home, she was out of breath and weak, which told us we had more work to do to build stamina.
That’s the essence of community-based practice. You’re not running through simulations—you’re embedded in real contexts, addressing barriers as they happen, and practicing the skills that matter most. It’s occupation-based at the core.
Caregiver Training
With caregivers, there’s so much we can do to build skills and confidence—whether that’s training around behaviors, adapting environments, addressing daily needs, or fostering self-advocacy. We can practice these things directly in the community, in real settings, while modeling strategies both for the patient and for their family. Caregivers can then practice those strategies with our feedback, which helps them feel more competent and prepared.
Sometimes it’s the simplest recommendations that make the most significant difference. For instance, going to a restaurant with a client who is hard of hearing and showing them that sitting with the wall behind them reduces background noise can completely change their ability to engage in conversation. These minor environmental adjustments lead to greater confidence, stronger participation, and better quality of life.
When we focus not only on the client but also on the caregiver, the impact of our work is multiplied. By addressing the holistic needs of both care recipients and caregivers, occupational therapy professionals strengthen innovative models of care while ensuring the home continues to feel like a restorative and meaningful space. This dual focus is essential. Caregivers and clients must be considered together, and if we exclude caregivers from our treatment model, we miss a vital part of the occupational profile and a huge determinant of success.
Goal-Writing
Let’s talk about goal writing. It’s fun to brainstorm creative treatments and interventions, but we also need to make sure what we’re doing is skilled, measurable, and defensible. The process of writing goals doesn’t change whether you’re in acute care, inpatient rehab, or community-based practice—the structure is the same. Goals need to be specific, measurable, time-based, and client-centered.
Here are a few examples that reflect community-based settings:
Patient will schedule a ride with the community transit system three out of three times over three weeks using her phone app to attend oncology appointments. This goal is clear, measurable, and focused on her real-world participation.
Patient will manage paying his monthly bills for 30 days using compensatory strategies such as calendar tracking, color coding, and sorting systems with modified independence to continue living alone. This connects functional independence directly to life participation.
The patient will attend two wellness classes per week for three weeks with supervision, using a single-point cane to improve community engagement and physical endurance. This will emphasize both the physical component and the social participation aspect.
One thing I learned as a younger therapist, and many of you may recognize this, was assuming that home health covered these types of goals and interventions. They often don’t, and even less so in recent years. That gap is where community-based OT steps in. The model allows us to see people longer, spend more time in sessions, and address truly individualized goals. Of course, that requires careful billing and documentation—if you’re spending more than an hour, you need to ensure your CPT codes match your work and that your notes clearly outline why the intervention was medically necessary.
When writing goals in community-based practice, a great place to start is by asking clients directly: “What do you want to be able to do?” The answers are often functional and meaningful: going to the gym, visiting a family member, or confidently walking into a coffee shop. From there, we break those occupations down, analyze the underlying impairments and activity demands, and build goals that lead back to that specific participation. Essentially, we start with where they want to go and then work backwards to get them there.
Launching a Program
If you’re thinking about launching a community-based OT program—whether you’re working independently or building with a team—there are some important steps to consider.
Start by clearly defining the problem your program will solve. For me, when I was working in a skilled nursing facility, I found myself drawn to patients with dementia. I loved working with them, but I kept seeing a gap: once these patients returned home, they weren’t getting OT services, or if they did, it was very short-lived. I wanted to fill that gap and support people living with cognitive impairment in their homes and communities so that they could not only function, but truly thrive. That passion became the foundation for my program.
From there, identify who your clients are going to be. Are you drawn to children? To caregivers? To older adults and aging populations? To individuals with chronic medical conditions? Almost every population can benefit from OT—but the key is matching your community’s needs with your passion and skills. And remember, every community looks different. A program that’s needed in my town may not be the same as what’s required in yours, so take time to really understand where the gaps are.
Part of that involves doing a needs analysis. Find out if there are existing community-based OT programs in your area. Even if there are, chances are they can’t meet every need—and there’s almost always room for more providers and collaboration. Don’t let an extensive existing practice intimidate you. Instead, think of your role as carving out your niche and educating the community about the breadth of OT.
You’ll also want to consider logistics. Is this a solo operation, or will you partner with an organization? Sometimes we go into adult day centers, for example, and do fall-risk screenings for their participants. From there, we might make equipment recommendations or follow up with them individually at the center or in their homes. You don’t have to do it all alone—you can partner, subcontract, or expand within an existing facility depending on what works best for you.
Understanding billing and documentation is another critical piece. We’ll look at specific billing codes and documentation strategies separately, but know that it’s essential to align your work with requirements for reimbursement and compliance.
Finally, start thinking early about how you’ll measure and share your outcomes. Personal stories are powerful—like the client who learned to pay her rent independently for the first time—but you’ll also want to quantify outcomes. Document improvements in functional participation, fall risk reduction, and mental health indicators like decreased depression or community engagement. These tangible outcomes make your work visible and credible to your clients and administrators, payers, and other stakeholders.
At the end of the day, the process combines passion, creativity, and strategy. Find the need that lights you up, meet it with skillful OT practice, and track and show the difference you’re making. That’s what builds programs that last and expand.
Barriers and Solutions
Sometimes there will be barriers, and that’s simply part of the process when you’re building or growing a community-based OT program. Funding is one of the first big ones. You’ll need to decide if you’ll take insurance, work cash-based, or even blend the two. Navigating insurance can feel overwhelming at first, but it’s something you can learn. There are courses, resources, and colleagues who can guide you, and over time, it becomes manageable as you understand the rules, codes, and systems you need to work within.
Another barrier is other professionals’ understanding—or misunderstanding—of what you do. Early on, a nurse asked me if what I was doing was legal. That was shocking to me, but she had only ever seen “mobile” therapy in the form of traditional home health. She didn't know it existed when she saw me in the community context. That moment taught me that part of our role is consistent education, because many professionals and community members don’t yet understand the reach of community-based OT.
Physician buy-in is another challenge. Years ago, therapists could bring lunch and educate a physician face-to-face, but those days are largely gone. Physicians are incredibly busy and often surrounded by gatekeepers, making it harder to reach them directly. So how do we connect? Marketing teams can play a role, especially if you’re tied to a larger organization. Faxing, mailing letters, and sharing success stories with outcome data go a long way. Most physicians will pay attention if you show them evidence of better functional outcomes, reduced falls, and fewer hospital readmissions.
Community education is just as important. Sometimes you give a presentation and only three or four people show up. That might feel discouraging, but those small engagements matter—they build word of mouth and credibility, and often lead to your strongest advocates.
As a community practitioner, you must also see your surroundings as part of your “clinic.” In skilled nursing, you know where the wheelchair closet is, where to grab a gait belt, and which kitchen you can use for a session. In community practice, your resources shift: the grocery store becomes your therapy gym, the park becomes your mobility center, and local organizations become your referral network. It’s about embedding yourself in your community and learning who the other specialists are. Who can you refer to? Who can refer to you?
And yes, explaining what occupational therapy is can be tiring. But the truth is that advocacy and education are inseparable from our profession. Whether you’re talking to physicians, caregivers, or community leaders, you’ll likely find yourself explaining OT repeatedly. That repetition isn’t a setback—it’s how we expand understanding and open doors for our role in the community.
Be Part of Your Community!
We want to be part of our communities—not just as clinicians, but as active participants. Education and training events are a simple and powerful way to do that. In this picture, for example, we were teaching a group how to assist people with transfers safely. It wasn’t just helpful for those attending, it strengthened connections and highlighted OT's role in supporting patients and caregivers.
Community events like the Alzheimer’s Walk are another great example. We participate in fundraising for causes that matter to us and often invite the families we work with to join in. It helps them feel connected, supported, and part of something bigger. And if we have a family facing a crisis, we’ll rally together and raise money for them, too. That’s valuable for clients and reminds everyone that we’re not separate from our communities—we’re embedded in them.
Being involved this way benefits the community and our patients and fuels us as therapists. It reinforces why we do this work and strengthens the relationships that make community-based practice so impactful.
Figure 7 shows examples of people working in the community.
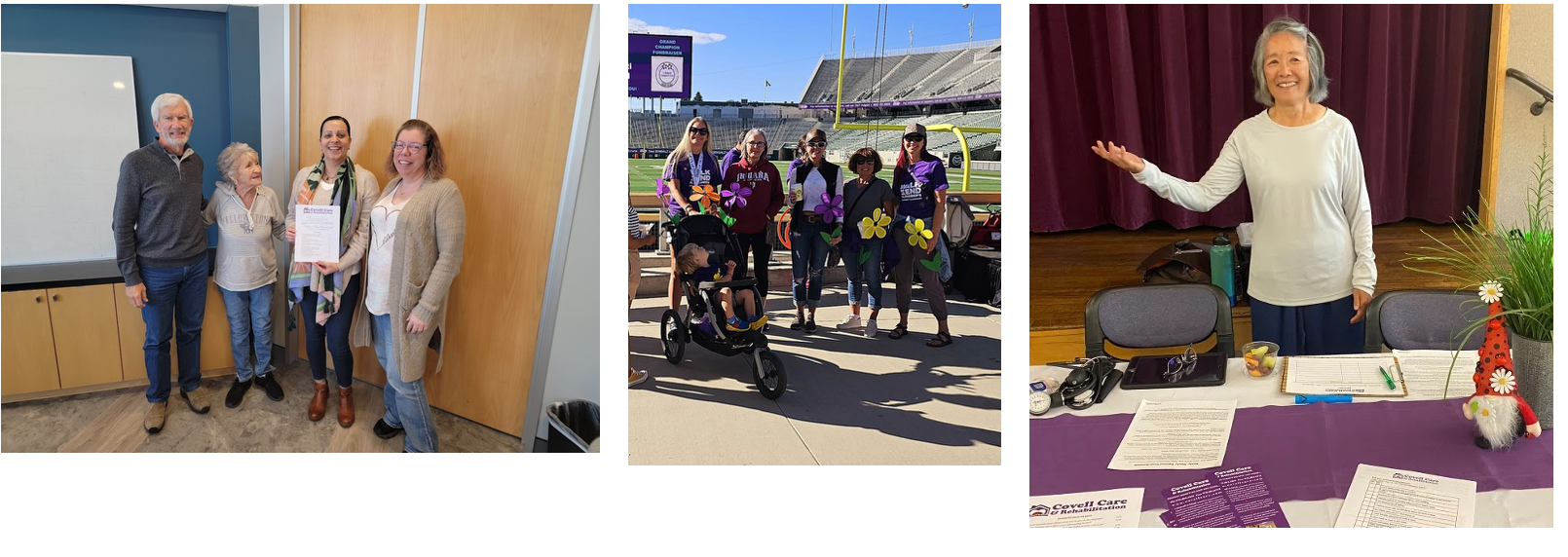
Figure 7. Examples of being out in the community.
This is Gail, a fitness instructor teaching Tai Chi at a senior center. She’s also sharing information with the group. What I love about this example is how it reflects the spirit of servant leadership. So much of community-based OT is about serving individuals in treatment and the community as a whole. We aim to help people stay connected, engaged, and plugged into community life.
One way we do that is by leveraging relationships with local organizations. If I can get a caregiver connected with the Alzheimer’s Association for a support group, that’s not just a resource—it’s a lifeline. It’s also far easier when you already have a relationship with those organizations. For instance, I might call and say, “I have a daughter caring for her mom who’s really struggling. Her name is Kathy, she permitted me to share, and she’d like to attend a group. What does your calendar look like?” That personal connection smooths the process and ensures she’s welcomed.
It’s also important because, as community practitioners, we will encounter challenges for which we don’t have immediate answers. None of us can know everything. But suppose you’ve built relationships with partners in the community. In that case, whether that’s the Alzheimer’s Association, senior centers, or other local resources—you can call them up to brainstorm solutions and get support. Those networks make us better problem-solvers and help us deliver more holistic, informed care to our clients and their families.
Reimbursement Options
Regarding reimbursement, Medicare Part B is the main pathway for billing mobile, outpatient, or community-based OT. The process uses the same CPT codes you would already be familiar with if you’ve billed for Medicare Part B in a skilled nursing facility or outpatient clinic. The main thing to remember is how codes are limited per calendar day across disciplines.
For example, if you bill CPT code 97530 (therapeutic activities), you can only bill up to a certain number of units in one calendar day. If both you and a physical therapist are seeing the same client that day and both of you bill the same code, one of you may end up with a denial if the combined codes exceed the daily limit. This doesn’t happen all the time, but tracking when you’re doing longer community sessions—like going to the pool, assisting with changing clothes, entering the water, and completing activities is essential. These sessions can efficiently run longer than traditional outpatient appointments, so careful use of codes is necessary to ensure reimbursement.
Medicare Advantage plans usually follow Medicare rules and regulations fairly closely, so in most cases, you can bill community-based OT through them. The nuances will vary between plans, so it’s worth checking each contract directly. Medicaid coverage is state-specific—here in Colorado, Medicaid does cover community-based OT, but if you’re in a different state, you’ll need to review that state’s billing manuals.
Private insurance generally does cover community OT if it aligns with what Medicare allows, but every insurer has its own quirks. Medicare sets the standard in almost all cases, and private insurers follow with slight differences.
The Veterans Administration (VA) is also a valuable payer to consider. They fund a wide range of programs for veterans, including home modifications, and they are currently the only payer that reimburses directly for driving assessments. Since driving and transportation are such meaningful areas of practice in community-based OT, partnering with VA programs can be a unique opportunity.
Beyond insurance, you can also look into grants and partnerships. For instance, an adult day center we collaborated with applied for a fall-prevention grant and had planned to use some of that funding to bring us in for staff training and family education. While their application wasn’t approved, it’s a good example of how grant funding can support OT services at the community level.
And of course, there’s private pay. This can be a straightforward model when insurance isn’t an option. Still, one important caveat: if a client has Medicare Part B and your service is generally billable under Part B, you cannot simply bypass the insurance and accept cash payment. Occupational therapists are not permitted to “opt out” of Medicare. So if a client is Part B eligible, you must bill that way.
The world of insurance and reimbursement can feel intimidating, but it’s all figure-outable. You can connect with a biller, talk to other therapists already billing community-based OT, or research payer guides specific to your state. With time, you’ll find a system that works and discover what funding streams are available for you and your community.
Crystal is shown in Figure 8.

Figure 8. The client is riding in her wheelchair with the author's son.
She's the patient I showed you who could stand now in her wheelchair. And medicine adds days to lives. Occupational therapy adds life to days. And that little boy is my little boy.
This is a barbecue that we went to at New Motion. If you are in the world of wheelchairs and assistive technology, you know that New Motion is one of the bigger organizations, and that's where her chair came from. So I was invited to a barbecue, and I invited Crystal to come. And it wasn't a billable treatment session or anything, but it's just being in the community together, and it's fun.
And then my little boy hopped on the back of that, and she was riding all over. And then I didn't think about it, but the guy at New Motion called out and said, Crystal, that might void your warranty. So we laughed quite a bit, and then told him to look away. But it's fun to have fun with your patients in the community. It helps them see you as a real person, not just a medical professional giving advice, and it'll keep you on your toes.
As occupational therapy practitioners, some of the things that you can specialize in or that I see a lot of are. A lot of need for low vision techniques in the communities, wheelchairs, and assistive technology out in the community. Pelvic health is a big one, along with transportation and driving. And we also have adaptive gyms around, and you can always plug into that. So you may not be doing as much treatment in the adaptive gym as possible, but as an occupational therapist, you can go in and do education and then see patients at home.
So, like, what we do right now, we have a clinic where we have physical therapists, but they work with massage therapists, acupuncturists, chiropractors for everybody that has a spinal cord injury, spina bifida, similar diagnoses to that. Then, the clients are there, and the occupational therapy practitioners see those patients at home. And we can work on all kinds of things in the community and the house. So there are a lot of areas that you can work. You can also work in larger organizations.
Caregivers call out sick to work more than any other reason for employers nationwide. So if you can work with some big organizations on caregiver stress and how to manage things, that can be helpful too. So, the sky's the limit to being in the community. Occupational therapy practitioners have a unique skill set that allows us to work in so many different areas with passion, education, and help people be as functional as possible.
Questions and Answers
How do we apply to work with adults in their homes?
If referring to insurance, you must apply through the CMS website. Each state has a fiscal intermediary (a Medicare contractor) that oversees the process, and that will be the application you complete. In addition, you must also apply through your state’s Medicaid website.
Can you share examples of interventions for someone with ALS?
Absolutely. One patient I worked with lived alone and had bowel incontinence. Through compensatory training, she managed her bowels independently until her caregivers arrived.
Another example is that she had a lifelong dream of traveling to Alaska. After inheriting a small amount of money, she could go—using her power chair and oxygen with the help of two caregivers. Despite breaking her ankle during the cruise, she refused to leave the ship, saying, “I don’t walk anyway, I want to stay here.”
Success came from training at home, preparing caregivers, selecting the right wheelchair batteries, and managing her oxygen, which enabled her to travel safely and fulfill that dream.
What types of interventions would you recommend for a position on the Community Disability and Sensory Team?
I am not 100% sure about this specific role. However, I’d be happy to provide more detailed guidance if you email me directly.
Can you give examples of working with children and teens with autism?
Yes. Much of the work involves a close partnership with caregivers and parents. We focus on:
- Safety training
- Behavior modification
- Sensory integration
- Practicing in real-world, community environments
This can be stressful for parents, so part of the intervention is understanding family dynamics, helping parents adapt, and supporting children in meaningful activities. Sometimes it’s also about guiding parents through gradually giving children more independence.
References
See additional handout.
Citation
Covell-Pierson, K. (2025). Community-based occupational therapy. OccupationalTherapy.com, Article 5829. Retrieved from https://OccupationalTherapy.com
