Editor's note: This text-based course is a transcript of the webinar, Multisensory Stimulation Rooms for Persons with Dementia: Design on a Dime, presented by Kathleen Weissberg, OTD, OTR/L.
Learning Outcomes
- After this course, participants will be able to identify calming and stimulating sensory interventions for persons with dementia.
- After this course, participants will be able to list design principles to consider when designing a multisensory space.
- After this course, participants will be able to recognize everyday objects, activities, lo-tech, and sensory inputs to include in a multisensory environment to facilitate purposeful engagement.
Introduction
Hello everyone. Before I get started, I want to tell you where this content originated. I am the National Director of Education with Select Rehabilitation and cover many different states. I happened to be working in a facility with a Snoezelen room that no one was using. This facility handed over the entire design process to the vendors and spent upwards of about $20,000 on this space. I thought there had a be a better way.
You will hear me throughout this talk call a Snoezelen room a space. I do not know where everyone is working. I will assume that the majority are working in skilled nursing, assisted living, or home care. These principles will apply to many different settings, and not everyone has the space to dedicate an entire room to it. A Snoezelen room can be a space in the corner of your therapy gym or day room, or if you are working in home care, it may be portable to take to someone's room or home.
Dementia
- Progressive decline in cognition along with a short- and long-term memory loss due to brain damage/disease
ICD-9-CM, 2013
- Impairment in memory and at least one domain of cognitive functioning that represents a decrease from the previous functional level & results in an impairment in daily activities
(Buffington, Lipski, & Westfall, 2013)
I now want to give a quick background on dementia. We know that it is an impairment in memory, cognitive functioning, et cetera. Along with that, we see behavior and personality changes.
Background
- Estimated 5 million Americans suffer from dementia
- More than 15 million provide caregiving
- Costly to treat ($215 B in 2010)
- Caregiving is the most costly aspect of dementia care
(AHRQ, 2014)
Dementia is incredibly costly to treat. These are the most recent statistics that I pulled from the Agency of Healthcare Research and Quality from 2014. It shows that dementia costs about $215 billion to treat, including formal caregiving (nursing, therapy) and informal caregiving (spouses, children, volunteers). What was even more interesting is that when an individual who has dementia has behaviors as well, that cost goes up by about 30%.
- In the US, 1 in 9 persons over 65 have AD
- 16 million by 2050
- An estimated 75% of persons with AD are admitted to an SNF
- AD is the 6th leading cause of death in the US
- Only disease in the Top 10 that cannot be prevented or cured
(Alzheimer's Association, 2015)
What is staggering to me is that one in nine, over the age of 65, have Alzheimer's disease or related dementia. This number climbs to one in three for anybody living over the age of 85. It is also estimated that 75% of individuals with Alzheimer's or related dementia are admitted to skilled nursing, most likely due to behaviors caregivers cannot handle. They may become a safety concern if they stay in the home environment.
BPSD
- Behavioral and psychological symptoms of dementia
- Symptoms of disturbed perception, thought content, mood, or behavior frequently occur in patients with dementia.
- As many 76% of residents have BPSD.
- Labels used to describe BPSD include agitated, aggressive, and disruptive
(AHRQ, 2014)
You may have heard of the term BPSD or Behavioral and Psychological Symptoms of Dementia. When we look at the nursing home population, 67-78% of the individuals, depending on what literature you read, have Alzheimer's or related dementia. Of that subset of the people, about 76% of them have BPSD. These behaviors are hitting, biting, scratching, calling out, inappropriate sexual behaviors, disrobing, wearing too many clothes, wandering, et cetera.
Unfortunately, we use a lot of labels to describe these individuals like agitated, aggressive, disruptive, belligerent, non-compliant, difficult, etc. I often hear it in therapy, "So-and-so won't cooperate with me. She's being belligerent and won't follow through with activities." This person is not purposefully doing that; it is the behavior from dementia.
Behaviors and Dementia
- "Behavioral symptoms related to dementia are defined as verbal, vocal or motor activities that are considered to be aggressive, excessive or lack adherence to social standards."
- Behaviors result from interactions between the resident, the caregiver, and the setting.
(Boustani et al., 2005)
I love this second bullet point as it speaks to me. The question is, "Are we going to change the resident?" The answer to that is no. Can we change the caregiver? We absolutely can change our approach and setting.
Disruptive Behaviors
- Inappropriate, repetitive, or dangerous behaviors which are disruptive to the living and working environment in the NH
- Most common disruptive behaviors
- Wandering
- Aggression
- Agitation
Ahn & Horgas, 2013
The most common disruptive behaviors are wandering, aggression, and agitation. We see wandering in about 40-60% of individuals. Again depending upon the literature, aggression or agitation can be seen in anywhere between 50-80% of our residents.
Behaviors
- ALL behavior has meaning and indicates something
- Behavior is a form of communication
- Look at every behavior as an unmet need
- Behaviors are considered a problem when
- Safety or well-being of patient or others is compromised
- A trigger or cause cannot be identified
All behavior has a meaning, and the person is trying to communicate something. They are overstimulated, under-stimulated, or they have an unmet need. It only becomes genuinely problematic when the safety of the individual is compromised, or we cannot figure out the trigger. A skilled intervention is to figure out the cause of a behavior and then do something about it. Sensory stimulation comes into play when treating behavior.
Why Sensory Stimulation
- Everyday objects can trigger emotions and memories
- A way to explore a safe, stimulating environment with age-appropriate and enjoyable activities
- Can give a means for expression
- Can promote feelings of safety, relaxation
- Improves mood, self-esteem, well-being
Sensory stimulation is not new, it started in the 1960s in Europe. Sensory stimulation is a way for seniors with dementia to explore their environment in a safe, enjoyable, meaningful, purposeful, engaging, and age-appropriate way. Sensory stimulation is an occupational therapy treatment. We can use everyday objects to trigger memories and emotions in individuals who maybe have lost their ability to communicate with the world.
- Familiar objects
- Focusing on one sense at a time
- The therapist provides reassuring nonverbal and verbal cues to stimulate a response.
- Activities are often linked to interests the person had prior to dementia and can help build a connection to everyday life.
We use five basic senses. The sense that we frequently forget is kinesthesia, or a sense of movement. We use familiar objects and focus on one sense at a time, which seems like an oxymoron because we talk about multisensory stimulation.
Benefits of Sensory Stimulation
- Improves behavior and mood
- Promotes alertness
- Increases brain function
- Improves communication
- Boosts self-esteem and well-being
There are many good benefits as you can see. For example, you can massage a client's hand, which is tactile, but in the meantime, there can be music playing in the background to tap into their auditory sense. Or, they can be watching a movie to tap into their visual sense.
There may be multiple things going on; however, we do not want to inundate this person with too much sensory sensation as they may become overwhelmed. We want to try and hone in on one sense at a time. The beauty of this is that we can provide nonverbal verbal cues to stimulate a response, and we will watch that response.
If what we are giving the person is too complex or challenging, we can use our OT skills to make that a little bit easier or vice versa if too easy to make the activity a "just-right" challenge. We are using tasks and activities to bring in a sensory component. We will be bringing in things that a person enjoys and are linked to their interests.
Standardized assessments are outside of the scope of this talk, but you can use the Role Checklist, Interest Checklist, Pleasant Events Checklist, the Preferences for Everyday Living Inventory (PELI), and even the occupational profile.
I want to add a caveat that we do not always want to link our activities to their history. For example, my father-in-law was an artist by background. He had dementia and moved into a community near me. Due to his experience, the OTs and PTs used art during every treatment session. I went to visit him one day, and he was angry. He said, "You know, I've worked my whole life, and here I am still working. I do not want to do this." The therapists thought they were doing meaningful activities linked to his prior interests, but he felt it was like work and wanted to do something different. This is where the occupational profile is so excellent as it gets to the crux of not just what a person can do but what they like to do. In the earlier stages of dementia, you may be able to get that information. In later stages, I am not so sure.
The benefit of sensory stimulation is to reduce disruptive behaviors. We can use this sensory space when family members come to visit, or we use this sensory space to calm the resident before ADLs.
Examples
- Multisensory activities are activities that combine two or more senses
- Drawing and listening to classic music
- Hand-massage and conversation
- Relaxing on a beanbag while watching colorful landscapes on a TV screen
- Having nails groomed in a garden setting
Here are a few examples of multisensory activities like drawing, sculpture, or painting. A client could work on art while listening to classical music. There could also be an aroma in the air. Or, a client could have tactile sensation via a hand massage while music is playing. Another example is relaxing on a beanbag or a recliner while watching a movie.
Multisensory Interventions
There is evidence to support this. I want you to look at how old these bullet points are. Recently, these studies have been replicated as they are effective. We need to start using it more in some of our environments.
- Increased engagement in multisensory environments (Heyn, 2003; Maseda et al., 2014)
- Sound
- Natural environments decrease agitation (Whall et al., 1997)
- Sight
- Light intensity improves performance and sleep (Koss & Gilmore, 1998)
- Smell
- Lavender oil decreases agitation (Holmes et al., 2002; Thorgrimsen, Spector, Wiles, & Orrell, 2003)
- Sound
There is increased engagement in multisensory environments. This can be seen as increased conversation or improved consumption at mealtime. Natural environments and sounds like a babbling brook, the ocean, the rain, or similar stimuli tend to decrease agitation, mainly related to ADL. The light intensity can improve ADL performance and sleep. Lastly, lavender can be calming via a 2% lavender oil and aromatherapy stream or a 10% concentration in a lotion for a massage.
One other thing before I go on is that these interventions are not long-lasting. If I bring somebody into this space for calming, this may only last one or two hours, or maybe into the evening. We cannot expect that that will last until the next day or week. The other thing is that this treatment is not OT specific. It is everyone's space, including PT, speech, volunteers, activities, social work, nursing, CNAs, family members trying to get an excellent, engaging visit with their loved ones. I have a few positive quotes from nurses that have used these interventions at the end of the talk.
- Snoezelen Multisensory Stimulation Therapy (MMS)
- Combines the therapeutic use of light, tactile surfaces, music, and aroma
- Neuropsychiatric symptoms may result from periods of sensory deprivation
- Short-term benefits on behaviors were significant (Chung & Lai, 2009)
This brings up Snoezelen Multisensory Stimulation Therapy (MMS). You may be familiar with this already, mainly if you have ever worked in pediatrics. We are seeing a lot more of this in the long-term care sector. These spaces include therapeutic light, tactile surfaces, music, aromatherapy, fiber optic curtains, bubble tubes, etc. Many different things are going on because neuropsychiatric symptoms (BPSD) may result from periods of sensory deprivation. And, we often see sensory deprivation in our seniors. They are sitting at the nurse's station or passively sitting in activities for bingo or sing-alongs, or watching tv. I already mentioned that the short-term benefits are significant.
- We can get information into our brains through our senses
- Too much stimulation – overwhelmed
- Too little stimulation – lose interest and ability
- Sensory deprivation impacts well-being and health
Remember, the only way we get information to our brains is through our senses. If there is too much stimulation, clients can get overwhelmed, but with too little stimulation, clients miss out on activities and lose their interests and abilities. I read a study about staff interactions using this modality. It makes perfect sense to me that if they bring somebody into this space for a calming intervention and then do an ADL, there will be better interaction. The staff saw great results, loved their job even more, and they become the provider of choice in that community. Job satisfaction improved because they had tools at their disposal to make a difference.
Benefits of a Sensory Room
- The stimulation provided in a controlled way
- Can be stimulating or calming in their effects
- Positive changes in mood and behavior for late-stage dementia
- Improves staff interactions with residents
We have talked about some of this. We can control stimulation again as it can be calming or alerting. We see a lot of changes in mood and behavior, particularly for individuals who are in the later stages of dementia. We will talk more about that a little bit.
Deficiencies of Sensory Rooms
- Aesthetics and functionality are not satisfying and appropriate
- The equipment and set up is not age-appropriate; juvenile
- Difficult to connect with
- Cluttered and distracting
- Insufficient multisensory stimulation
These photos pull together some of these concepts and deficiencies. When we turn over the design to vendors without our input, we sometimes see this. People will say, "We've stopped using our sensory room because when we set it up, we did not think about who was going to be using that space."
Here is a picture from Mike Ayres' design (Figure 1).

Figure 1. A multisensory room with too much stimulation and patterns.
For example, look at the carpeting alone. There is also a disco ball and lots of neon. Figure 2 is from the Hidden Angel Foundation. You can see a lot is going on in there as well.

Figure 2. Another multisensory room with lots of stimulating light and bubble tubes.
There are projections all over the walls and bubble tubes. Bubble tubes can be great, but they put them in front of a mirror, so it looks like there are many bubble tubes. Figure 3 also shows lots of visual stimulation.

Figure 3. Last example of a stimulating multisensory room with neon lights.
Many times the seating surfaces are not appropriate for a senior living population. Again, there are fabulous elements, like the fiber optics and bubble tubes, but there is too much. The spaces need to be edited and toned down a bit.
Factors When Designing a Space
- Feeling comfortable and safe
- Meaningful and familiar
- Multisensory experience
- Stimulation and relaxation
- Control and interaction
- Age-appropriate and usable
These are the factors to keep in mind when designing a multisensory space. I will skip over this slide as we are going to talk about each of these in turn.
Feeling Comfortable and Safe
- The space should be intimate, contained, and quiet.
- Minimized or zero capacity for disturbance or distraction
- Low-level sensory stimulation to activate the parasympathetic nervous system
The first concept is feeling comfortable and safe. We want this space to be intimate, contained, and quiet. We do not want it to be in a place where people will be walking in and out, poking their heads in, or where there is a lot of noise and distractions. We want this to be a place of calm. Everything should be intentional and not dramatic in this space for a low-level type of input to activate the clients' parasympathetic nervous systems.
- Textiles, fabrics, and other soft materials
- Soft blankets
- Soft cushions and soft toys
- Plain textile curtains
One of the first ways to induce comfort and safety is through textiles and fabrics. These can be soft blankets to wrap clients in or put on their laps. Warm towels just out of the dryer are also great options. If you look in long-term care, much of the furniture is hard, covered in vinyl, or just not comfortable. We can put different coverings on the furniture like Sherpas.
We can use soft items under their feet or textile curtains. We can make the space smaller, like a section of a day room, or use plain textiles to cover things. There can be bookshelves filled with different manipulatives and sensory items. We can also put fabric up on the wall. We can project things onto the wall, maybe with a handheld flashlight or an LED type of projector, making the room look very different. If there is a distracting or too stimulating wallpaper, you can cover that with a textile.
- Appropriate Lighting
- Soft, indirect light for general lighting
- Dimmer switch
- Daylight
- Selective stimulating lights create visual focal points.
It is essential to have appropriate lighting. This is a little harder in some of our places due to the overhead fluorescent lighting. You have to work with what you have. You might be able to put a shade on that or, in some cases, use a dimmer switch. We want to avoid overhead lighting and use soft and indirect lighting if possible. This can be achieved with sconces or lamps. Many of these items can be found at garage sales. Touch style or lava lamps are great. You can even use rope lights that go around the room. We have to be very cautious about how often those lights change and the color palette. Blues, purples, and greens are going to be very calming. Reds and oranges are going to be more stimulating.
We want to have a slow transition in this space. What I mean by that is you will want to draw people into this space with brighter lighting and music playing at the entrance. Then, as you move into the space, the lighting should dim to facilitate a slow transition. This is why a dimmer switch is terrific.
If you can have a window in the space, that is wonderful. Daylight is excellent, but we need to ensure no glare, especially if the person is working on a task. Selective stimulating lights like handheld orbs and small handheld fiber-optics are inexpensive.
- Avoid
- Very dark spaces
- Glares and flickering lights
- Lights and reflections moving around the room
- Overstimulation
- Decorative lights
As I said, everything should be very intentional. You want to avoid dark spaces as they can be scary. We should also prevent glare and flickering lights. Go back to those photos that we showed. Somebody with dementia may see flickering as insects crawling in the room. Only recognizable flickers like a fire or a movie projector should be used.
I want to tell you another story about my father-in-law when he had a moderate level of dementia. He worked for Andy Warhol as an artist for years. I took him to the Andy Warhol Museum in Pittsburgh shortly before passing. There was a giant velvet curtain, and he loved it. You could see there was a movie playing behind it. He said, "What's going on? Is there a movie back there?" He was not remotely afraid of that. He recognized what was playing and said, "I was at that party. That's the factory." Before this, he was not engaged or conversational. After the curtain and movie, he could not stop talking. It was beautiful to hear him reminisce. So, a movie projector is an excellent tool for this space.
- Contact with Nature
- Bring the feeling of the outdoors inside
- Easy Access
- No stark contrast between multisensory room and rest of home
- Sensory cues direct the resident to the sensory space
- Visual contact with the rest of the facility
You can bring in natural items like pine cones, seashells, plants, water features, fish, potted herbs, et cetera. You have to make sure the plants are not poisonous.
We also want to have easy access to this space. We want it to be separate, but we do not want it to be a stark contrast. If you have a bubble tube going on in this space, there can also be a small bubble tube somewhere out in the rest of the community. If you are doing some tasks in this space, there can also be a rummage station with tactile items somewhere else in the community. We want sensory cues directing that person there. As mentioned, it could be music or a specific type of lighting. You also want visual contact using a glass door or a muslin curtain. You want it separate yet still visible.
- Over-Stimulation
- Provide a visually calm space with a visual focus
- Limit visually stimulating equipment
- Eliminate disturbing noise:
- Comfortable furniture
- Soft, tactile surfaces/material:
- Comfortable and relaxing positions
You want to declutter that space, especially when not using it, and limit the stimulating visuals and noise. LED projectors, color wheels, and similar equipment can have fan and motor sounds that can disturb a person who has dementia. When purchasing items, try to get quieter things.
It is also essential to have comfortable furniture with soft tactile surfaces and a comfortable, relaxed position. You can also incorporate footrests, ottomans, recliners, or day beds so the clients can lie down. It is also lovely to include rocking chairs or gliders. However, you will have to follow your facility policy and procedure for infection control. If you can bring things into this space that belong directly to that resident, those can be returned when done. Pillows and blankets that can be laundered may be considered if infection control is prioritized. Disinfectant wipes or sprays also may be an option. Family members, activities departments, or grants may be options to get specific items for this multisensory space.
I am going to digress for a minute. I have been running a focus group talking to long-term care providers asking, "What happened during COVID? What went well, what didn't go well, what would you keep, and what would you change?" One hundred percent of my providers said, "We dropped the ball. We could not figure out how to keep people in quarantine and isolation engaged." Going back to infection control, can we have a clear plastic bin or something that is only for a particular individual that stays in their rooms?
- Serving snacks and drinks
- To enhance the sense of comfort
- Pleasant climate
- Comfortable room temperature:
- Good air quality and sufficient oxygen
The last thing on feeling comfortable and safe is serving snacks and drinks. This is not about eating a meal; this is about opening up and getting that sense of comfort. Providing small snacks like coffee or a tray of cookies can convey a sense of comfort. This is where an activity can be enjoyable. "Your family is coming to visit. Let's set the table for your family and prepare a pot of tea and a snack tray." This is also very sensory.
You also want the room to be at a comfortable room temperature. You can use a fan or air conditioner to help with this.
Meaningful and Familiar
The concept is meaningful and familiar, which screams what we do as OTs. We want things relevant to the resident's life and their stage of dementia. You want to know where they are both cognitively and physically. If they cannot do fine motor things because they have progressed, we do not want to give them a fine motor task.
- Provide familiar, personal, appropriate experiences
- Relevant to the resident's life and stage of dementia
- Everyday objects to trigger memories/ conversation
- Exploring and engaging in appropriate activity; create a sense of purpose
We want to use everyday objects to trigger memories and conversations. For example, you may give them measuring cups or spices to smell because they love to bake. They may start to talk about what they used to bake. My husband's space would include hockey and fishing paraphernalia, while my father's space would include antiques and hunting items. You are going to customize these experiences to trigger these memories. This is where you look around and see what is available to you. We also want to provide appropriate activities that create a sense of purpose. Perhaps they are slicing a banana to make banana bread or having a banana as a snack. You may want the person to do something a certain way, but they changed it up in some way. That is okay. You are looking for meaningful engagement. If the engagement is strong, continue the activity even if it did not play out the way you planned.
- Appropriate use of technology
- Technology needs to be multisensory and age-appropriate
- A mix of natural things and technology
- A mix of the new and the familiar
- Everyday items, old items, familiar imagery
- Playing old songs and music
Along these lines, we can also use a mix of technology. We can use bubble tubes, aromatherapy, and such. Objects that we obtain from vendors can be suitable for individuals in the later stages of dementia because they need a more substantial sensory input. You want to use a mix of new and old items. Familiar imagery could be family videos or images, a glowing fire, or nature/landscape pictures. Other significant items or activities are everyday tools or music. A faster tempo will be more stimulating, while a slower tempo is going to be a little more relaxing.
- Offering appropriate tactile stimulation
- Prepare the room for individual sessions
- Cultural relevance
Tactile stimulation is one of those senses that we tend to forget. Using culture as your guide, bring things into the space from the residents' room or home to interact with what they know.
Multisensory Experience
Let's now start talking about the actual senses.
- All the senses need to be addressed!
- The visual sense is often overvalued.
- Tactile stimuli are limited.
- Stimulating the vestibular and kinesthetic sense
- Use equipment, items, material that are multisensory in design
All senses need to be stimulated, not just the visual sense.
- Sight
- Light and color
- Films and videos
- Projections on fabric
- Material of different optical qualities catching the light in different ways
- Food and natural things found outdoors
- Motion
Sight is easy as we can look at light and color. It could be fiber optics, a kaleidoscope, a suncatcher, or bright objects. It is vital to avoid those things that are flashing or projecting too quickly, like films and videos, as we already discussed. Old movies or a color wheel can be projected on fabric or the wall. I know I am aging myself by talking about color wheels like we used to put in front of our aluminum Christmas trees as kids. They still make things like this and are inexpensive. You can also see an LED or a handheld flashlight and project on different materials like velvet, silk, wood, leather, or whatever. This is going to alter the way that the light looks.
Food and natural items are also excellent. Let's take an orange, for example. It is visual and tactile. They can smell the orange, cut and squeeze it, and then drink the juice. We have now tapped into different senses. You can see how multisensory this experience can be. Bananas are another excellent food to use.
For motion, you can use bubble tubes, pinwheels that catch the wind, and wind chimes.
- Touch
- Active tactile stimulation
- Passive tactile stimulation
- Natural and everyday objects
- Sensory cushions, blankets, books
- Sensory armchairs and pockets
- Tactile activities
- Small vibrating items
- Experiencing different temperatures
We can work on tactile stimulation with different textures, shapes, and familiar objects. Touch can also be passive with a hand massage or a foot bath.
Sensory cushions or armchairs with big pockets can be great to hide items. They can explore to find things. You can also have them do different types of art or sculpture with things like finger painting or clay. You can use small vibrating items. I would recommend staying away from vibrating furniture as these are probably inappropriate for this age group.
We can also experiment with different temperatures like cold and hot drinks, ice cream, or warm snacks. We can also provide the client with a warm blanket, an ice pack, or different things like that.
- Sound
- Relaxation
- Stimulation
- Musical Instruments
- Sing-along and rhythm sessions
Sound is another fantastic tool. You want sounds that will relax the client like rainfall, wind blowing, and what have you. To stimulate the client, you may want to use music from a specific era or with a dance tempo. You can use real musical instruments like a piano or a water bottle, or a Quaker Oats container with beans. We can do a sing-along or a rhythm session. Music is so powerful because the brain area impacted by dementia does not affect music. They may not be able to communicate, but they may sing.
- Smell
- Scented rooms/space
- Hand massage
- Scented bags
- The smell of everyday things
- Continued throughout the facility and the day
You can have a ton of fun with the smell. It can be aromatherapy, scented objects, or even the scent of everyday things like pets or familiar foods. We can use lemon and mint as those are uplifting, or we can use lavender and eucalyptus that are soothing. Chocolate, coffee, peppermint, tea, and spices are also popular items. One of my favorite activities is to use spices from a dollar store. This stimulates questions like, "What can you bake with this?" I worked with an administrator who baked bread every morning with a breadmaker and cookies in an Otis Spunkmeyer oven in the afternoon. These familiar smells trigger memories.
- Taste
- Taste
- Ensure you have a range of salt, sweet, sour, bitter
- Texture
- Ensure you have a range of different textures such as crunchy, soft, melting
- Taste
- Movement
- Different seating positions
- Opportunities of movement
Inducing taste does not have to include a full meal. You can have different flavors and textures: bitter, sour, salty, sweet, crusty, chewy, soft, melty, et cetera. It is crucial to take into account any precautions for swallowing. You can use peppermint, crackers, yogurt, raw vegetables, and popcorn. When you taste, you smell at the same time. These senses trigger a lot of memories.
It is also essential to use different seating positions and allow linear movement like rocking. Rocking can be calming, and spinning is going to be stimulating. I am not advocating that you go out and spin your residents, but you can have them reach outside of the base of their support for crossing midline and bilateral types of integration. This movement will be stimulating.
Stimulation and Relaxation
- Stimulating
- Sight
- Lights of high intensity, the color red, reminiscent images and objects
- Smell
- Citrus smells, peppermint
- Sound
- Loud music, fast tempo, sing-along tunes, abstract sounds
- Touch
- Textured objects, spiky balls, random contact
- Taste
- Citrus fruits, peppermint, sour sweets, sherbet
- Movement
- Random movements, spinning
- Sight
- Relaxing
- Sight
- Low level, slow-changing lighting, fairy lights, Christmas tree lights
- Sound:
- Quiet music, slow tempo, natural sounds
- Touch
- Hand massage, stroking, soft fabrics such as fur, velvet, silk, or fleece
- Taste
- Milky foods such as chocolate, pudding, yogurt
- Smell
- Lavender, the smell of baking cakes or bread
- Movement
- Linear rocking such as a rocking chair
- Sight
These ideas are for your reference. Again, if you want to stimulate a client, you can use the color red, peppermint, spiky balls, and random contact and movements. If you want the client to relax, the opposite stimuli would be warranted like quiet music, slow tempo, milky foods, linear motion, etc.
Control and Interaction
- The right level for the individual
- Promotes brain activity
- Increases confidence/feelings of self-worth
- Opportunity and empowerment to choose
- Mastery over the environment
If the client chooses a relevant and appropriate activity, they will be successful. This will empower them, help with their self-worth, and give them some dignity.
Age Appropriate and Useable
- Not perceived as juvenile or childish
- Dignity is important
- Items are in easy reach
- Ergonomically designed for elders
Whatever we use, make sure the clients can interact with it. For example, if a client is in a wheelchair, you need to ensure the stimuli/activity is at their level. Suppose the person has arthritis and has trouble with fine motor tasks. You will want to provide more gross motor activities. Another example is giving contrast between items if the client has poor vision.
Helpful Design Tips
- Less is more
- Familiar items promote relaxation
- Avoid dramatic smells
- Do not use overhead lighting
- Space should hold only 4-6 people
These spaces do not have to be grandiose. They just have to meet the needs of the person using it. Per the literature, the room should hold four to six, but I would say probably one to two is more appropriate.
- Play music at a moderate level
- Start small. Find a balance between high-tech items and familiar household items.
- Think through each of the senses
- Keep rooms neutral and light
- Use contrast for better visibility
- Use less complex artwork
I love the idea of keeping the room neutral and light. Think through those senses and make sure that every sense is represented. Keep it moderate and in balance. I also love the idea of having the residents create the artwork, and then we can swap that out depending on the resident who is in there.
We already talked about contrast as well. Think about your color scheme. Stimulating colors are reds and oranges, and calming colors are blues and greens. Blues and violet will make the space look larger, and reds and oranges will make it look smaller and warmer. You need to design for the person who is in there.
Examples
- Office
- Virtual Forest
- Rummage dresser
- Outdoor garden shed
- Old car
Here are some examples. Can you set up office space? For a person who insists on working, you can have a desk, file cabinets, and pens and pencils. I worked with a nurse years ago that insisted on charting, so we had a whole rack of charts where she went and did her "charting" for the day.
A virtual forest could include natural items like feathers, rocks, seashells, plants, or whatever is appropriate for where you live and suitable for that person. For example, if they spent all their summers at the shore, seashells would be a suitable medium. Another example would be an avid hiker in this type of space.
I love the idea of a rummage dresser. This does not just have to be in this space. The dresser could have socks, washcloths, and other trinkets. The client can fold or sort the laundry or interact with the other items.
I also love the idea of gardening as this is very multisensory. A client can dig in compost for tactile sensation. They can smell it and then cut flowers later if appropriate. We can also add flowers in the dining room for continuity.
I do not know that you could have an old car, but I did work in a community that had an old car in the back. Individuals washed and waxed it. I even had somebody change the oil on it, which was awesome. We also had a gentleman and his wife sit in the car and watch a movie like a drive-in. For another individual who was struggling to eat, we had him sit in that car and brought him his food like a carhop.
I do not think you need to go to that level, but even wherever you are, look around you. What is available to you? It may be something like a coffee table book or something from a library. It has a feel. It has a smell. It meets the visual requirements. Here is a video to illustrate some of these points.
https://www.youtube.com/watch?v=9lUK1RYM3Zs
Touch, taste, sight, smell, and hearing. Our five senses are often taken for granted, but for an Alzheimer's or dementia patient, stimulating these senses can make a huge difference in mental health and provide a source of comfort and relief. That's why we provide a Multisensory Environment or MSE. The MSE is a therapeutic space that utilizes rotating light, vibrating bubble tubes, soothing light strands, aromatherapy, and cozy seating, to intentionally stimulate the five senses in order to help overcome the cognitive disability related to dementia and other cognitive disorders. These attractions can be seen, heard, smelled, and or touched by the resident. The MSE promotes changes in brain chemistry, which allows the person to respond in a more normal way. For example, it can help them communicate more effectively, decrease agitation, increase their attention spans, and improve their ability to move. This can make a huge difference in the quality of life of our residents.
As therapists, we can bring somebody into our clinic and do therapeutic exercises until we are blue in the face; however, we may not get the responses that we saw on the faces of those individuals in the video. Their faces lit up, and they were engaged. In the video, you saw the guy using both hands and the woman taking that fiber-optic thread and tying it into knots. They were both reaching up on the wall, outside of the base of support. We can use these spaces to decrease certain behaviors and calm clients or stimulate and engage them to meet therapeutic goals.
I will show you a couple of other photos to show you a few things I have seen or have used.

Figure 4. A shelf holding different treatment items.
This shelf cost me maybe $125 to put together. There is a bin of washcloths to fold, silk flowers that can be arranged, and other sensory items. Clients can grab a bin and interact with a sensory activity. It does not have to be a space. Figure 5 is another sensory space.

Figure 5. Multisensory space.
As you can see, there are great seating surfaces. Again, I am not a huge fan of the bubble tubes in front of the mirrors, but I love the idea that they put fiber optics in front of the chairs so that clients can interact with those. Figure 6 shows another space with different types of seating surfaces.

Figure 6. Multisensory space with different seating options.
They mix up the seating and textiles in this room. Another example is shown in Figure 7.

Figure 7. Another multisensory space.
Figure 8 is a great one from the Cleveland Clinic.

Figure 8. A multisensory space from the Cleveland Clinic.
It is very simple with pillows, a small bubble tube, and fiber optics. Figure 9 shows a lava tube (my favorite) and colored orbs.

Figure 9. Space with a lava lamp and lighted orbs.
In the last picture (Figure 10), these are everyday objects like an old wedding dress, an old lamp, doilies, and those sorts of things.

Figure 10. A room with old, familiar objects.
A space does not need to be high-tech; it can be very simple.
Multisensory Interventions
Massage and Touch
- To reduce depression and anxiety
- Hand massage with calming music
- Tactile input during meals
- Gentle massage 3X/day
- Intermittent touch with talking
- Massage and touch therapy may have beneficial effects
(Hansen et al., 2009; Gleeson & Timmins, 2004)
We already talked about massage and touch, but the reality is that it provides excellent dividends. For example, when you are having a meal with someone, touching the back of their hand or arm can improve engagement.
Music
- Reduces repetitive disruptive vocalizations and self-stim behavior (Casby & Holm, 1994)
- Promotes mobility skills and body awareness (Pomeroy, 1993)
- Improves posture, competence, and sensory awareness (Gotell, Brown, & Ekman, 2003).
- Reduces agitation and time spent with meals (Sherratt, Thornton, & Hatton, 2004)
- Ambient music played other than at mealtimes can reduce undesired behaviors (Padilla, 2011)
We have already talked about how music is powerful. It improves body awareness, posture, and competence. Any type of music pertinent and appropriate for the resident can provide benefits. Music can also be played throughout the facility as well.
Animal-Assisted Therapy
- Robotic cats, plush toys, fish tanks, resident cat/dog
- Decreases in agitated and disrupted behaviors
- Increases in social and verbal interactions
- Decreases in passivity
- Increases in nutritional intake
(Greer et al., 2001; Martindale, 2008; McCabe et al., 2002)
Animal-assisted therapy does not just have to be a facility dog or cat. I have seen a peacock, a pig, and a kangaroo. The person can pet or brush the animal. There can be a lot of sensory engagement. You can also use robotic or plush animals. There is a lot of extraordinary evidence, particularly related to COVID and isolation, of how robotic animals have increased engagement.
Specialized Environments
- Moderate level noise promotes improved engagement in activities (Mercado & Mercado, 2006; Cohen-Mansfield, 2010)
- Homelike, personalized rooms reduce behaviors.
- Small dining rooms, large clock, printed mealtimes help with confusion (Chaudhury et al., 2013)
Looking at specialized environments, you can see some of the same themes occur.
Montessori Approach
- Dr. Cameron Camp adapted the Montessori method to treat people with Alzheimer's
- Engages the senses and evokes positive emotions
- Stimulation of cognitive, social, functional skills
- Conducted one-on-one
Dr. Cameron Camp adapted the Montessori method for our Alzheimer's dementia population. It has some of the same principles.
- Use Everyday Materials
- Match Interests & Skills
- Use Past Experiences & Preferences
- Adapt According to Cognitive & Physical Status
- Simplify as Much as Necessary
It is important to use everyday materials, match interests, and use their preferences.
- Every participant should have an activity that they can successfully handle.
- If materials are used inappropriately, but engagement is strong, let the activity occur.
- Provide demonstration as needed
- Matching Shapes/Colors
- Color Sorting
- Picture Puzzle
- Pairing & Sorting
- Sensory Boxes
You want to provide activities that the client can successfully handle. If it is used appropriately, engagement will be strong. I see a lot of overlap between multisensory rooms and Montessori.
- Sensory boxes
- Offer an opportunity to stimulate as many senses as possible, for example:
- Balls box
- Cereal Box
- Kinetic Sand
- Seeds
- Food
- Offer an opportunity to stimulate as many senses as possible, for example:
Montessori has a lot of sensory types of things as well.
Activity Ideas
- Golf ball scoop
- Living/non-living or Happy/not-happy
- Memory BINGO
You can have a box with different balls like a golf ball, a tennis ball, a squish ball, or whatever. Clients can dig through rice, cereal, or seeds to find items. You want to make sure things are safe, and they are not putting things in their mouth. Food is excellent too as it is gustatory and visual. The following are some actual Montessori activities.
Figure 11 is a golf ball scoop.
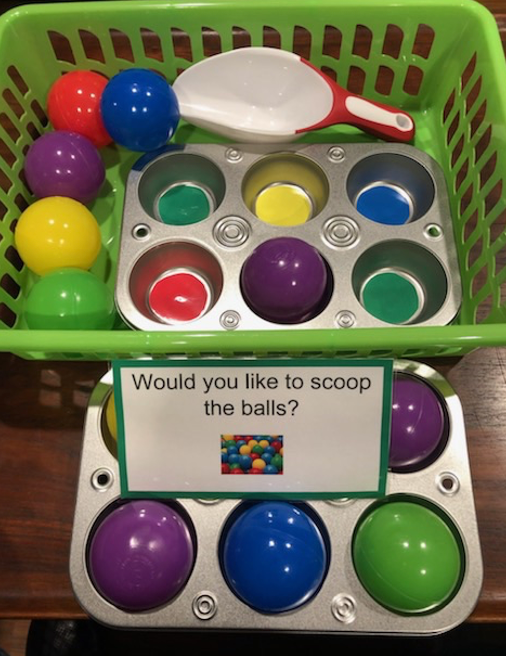
Figure 11. Golf ball scoop.
This may seem contrived, but as you can see, there are different colors and kinesthetic movement with scooping. Figure 12 is something I put together for one of my patients (Figure 12).
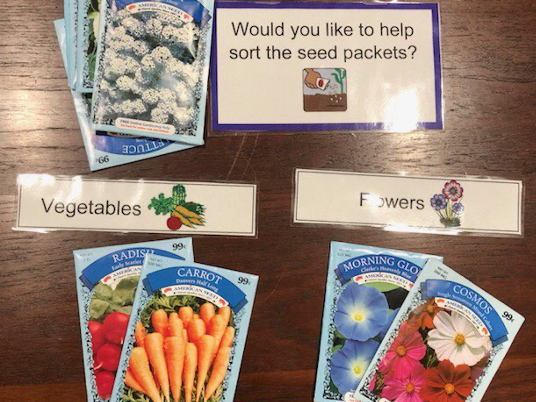
Figure 12. Seed matching activity.
I live in a very rural community where there are a lot of farmers. I put this sorting activity together for vegetables and flowers. We planted these seeds and then cut the flowers. It can be used as a progressive type of activity.
- Cognitive stimulation
- Sorting
- Matching
- Discussion
These are examples of cognitive activities. Figure 13 shows a simple puzzle for matching.
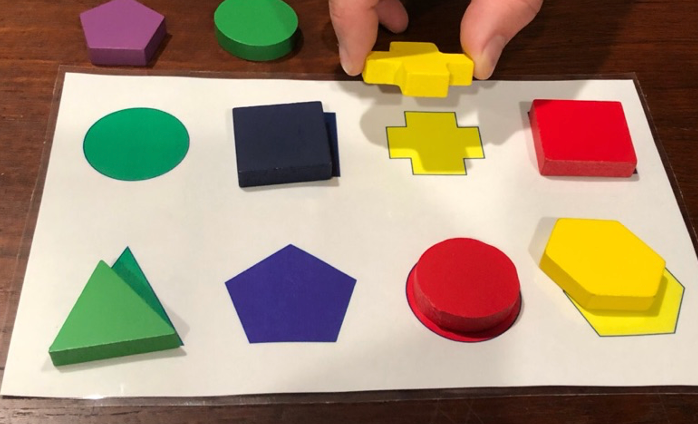
Figure 13. Shape matching puzzle.
I created this animal matching game for a farmer in my care (Figure 14).
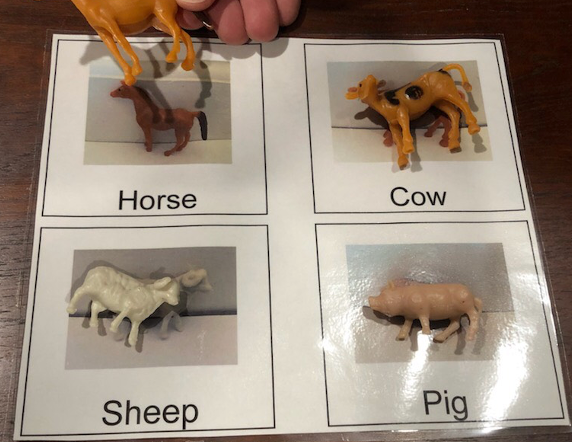
Figure 14. Animal matching game.
Then, I had him match these to the actual animals on the farm. This also spurred a lot of conversation about farming.
- Life Skills
- Meal-related
- Sorting
- Pouring
- Squeezing
Life skills are OT. Figure 15 shows many sensory activities like folding laundry, washing the dishes, polishing the silver, polishing shoes, and darning socks.

Figure 15. Examples of life skill activities.
There are different activities to work on like pouring, sorting, squeezing, and the list goes on. You can even work on crafts.
- Sensory stimulation
- Massage
- Olfactory
- Rice bin
Finally, Figure 16 shows some sensory activities.
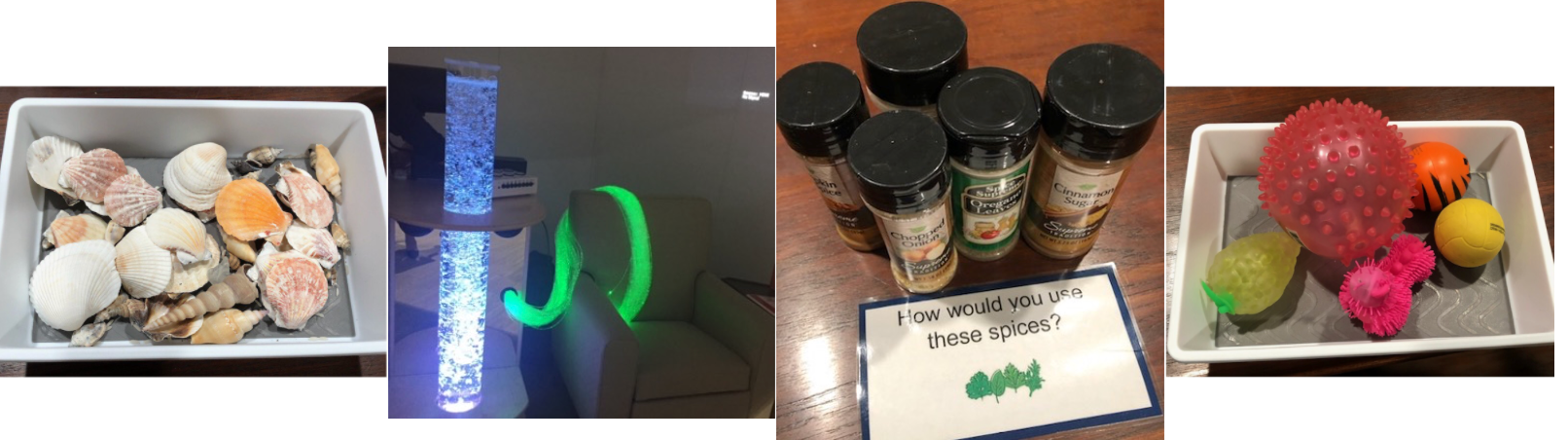
Figure 16. Examples of sensory activities.
Again, these are Montessori-type activities, but these areas can overlap. With the shells, you can match them for a cognitive task or talk about the shells. "Where would you find these?" Or, "What did you like to do at the beach?" You can use light options, spices, balls, et cetera. The sky is the limit. Look at what is available to you.
Activities By Stage
- Early-stage of dementia
- Activities that focus on the whole task
- Mid-stage of dementia
- Activities that focus on the individual steps of the activity
- Late stages of dementia
- Activities that focus on the sensory part of the activity
Keep in mind activities by stage. You would most likely not be bringing a client with early-stage dementia into these types of spaces. Those, in the earlier stages of dementia can do activities that focus on the whole task. For example, we may mix up bread dough, knead it, punch it down, and then bake the bread.
If I am working with mid-stage dementia, I may only focus on the individual steps. If I am baking a cake, I might just have them measure out the flour, crack the eggs, or spread the frosting. If potting a plant, they may put the root ball down into the compost or water. If it is a craft activity, they may scrunch up the tissue paper or apply the glue.
In the later stages of dementia, we may focus on tasting the frosting, smelling the compost, or smelling the flowers.
Staff Feedback
- "I can see they are much happier after the group. I thought they were slow and irresponsive, now I know I was wrong."
- "I would not have thought to give them that activity before."
- "Now I know that if we give them a chance, they can achieve something after all."
As promised, here is nursing feedback. We see clients happier after the multisensory experiences.
Questions and Answers
Can a multisensory room be suggested in a home care environment to limit wandering and safety in the home?
When we look at multisensory stimulation, it addresses behaviors, but we still have to get to the crux of why that behavior is occurring.
Can I use multisensory stimulation in the home environment?
It does not have to be your space or a room. It could be a shoebox with different sensory types of things. We can do the same thing in long-term care.
Do you generally have only one resident in the space at a time?
The literature would tell you there should be no more than four to six individuals in this space at any given time. Take it for what it is worth. I think that is too many and can be a little overwhelming. I have had excellent results with only having one person in this space, maybe two or three at most. I would keep it a little bit on the smaller side.
References
Booth, S., Zizzo, G., & … Robertson, J. (2018). Positive Interactive Engagement (PIE): A pilot qualitative case study evaluation of a person-centred dementia care programme based on Montessori principles. Dementia Online. https://doi.org/10.1177/1471301218792144
Camp, C. J. (2010). Origins of Montessori programming for dementia. Non-Pharmacological Therapies in Dementia, 1(2), 163–174.
Camp, C. J. (2013). The Montessori approach to dementia care. Australian Journal of Dementia Care, 2(5), 10–11.
Camp, C. J., & Lee, M. M. (2011). Montessori-based activities as a trans-generational interface for persons with dementia and preschool children. Journal of Intergenerational Relationships, 9, 366–373.
Cheng, C., Baker, G., & Dursun, S. (2019) Use of multisensory stimulation interventions in the treatment of major neurocognitive disorders. Psychiatry and Clinical Psychopharmacology, 29(4), 916-921. DOI: 10.1080/24750573.2019.1699738
Collier, L., & Jakob, A. (2017). The Multisensory Environment (MSE) in Dementia Care: Examining Its Role and Quality From a User Perspective. HERD: Health Environments Research & Design Journal, 10(5), 39–51. https://doi.org/10.1177/1937586716683508
De Witt-Hoblit, I., Miller M. N., & Camp C. J. (2016). Effects of sustained, coordinated activities programming in long-term care: The memory in rhythm program. Advances in Aging Research, 5, 1–8. doi.org/10.4236/aar.2016.51001
Elliot, G. (2012). Montessori methods for dementia: Focusing on the person and the prepared environment (US Edition). Solon, OH: Center for Applied Research in Dementia.
Erkes, J., Camp, C., & Raffard, S. (2019). Assessment of capabilities in persons with advanced stage of dementia: Validation of The Montessori Assessment System (MAS). Dementia, 18(5), 1840-1857. https://doi.org/10.1177/1471301217729533
Giroux, D., Robichaud, L., & Paradis, M. (2010). Using the Montessori approach for a clientele with cognitive impairments: A quasi-experimental study design. International Journal of Aging and Human Development, 71(1), 23–41.
Griffiths, S., Dening, T., Beer, C., & Tischler, V. (2019). Mementos from Boots multisensory boxes – Qualitative evaluation of an intervention for people with dementia: Innovative practice. Dementia, 18(2), 793–801. https://doi.org/10.1177/1471301216672495
Hitzig, S., & Sheppard, C. (2017). Implementing Montessori Methods for Dementia: A Scoping Review. The Gerontologist, 57(5), e94–e114, https://doi.org/10.1093/geront/gnw147
Jakob, A. & Collier, L. (2017). Sensory enrichment for people living with dementia: increasing the benefits of multisensory environments in dementia care through design. Design for Health, 1(1), 115-133. DOI: 10.1080/24735132.2017.1296274
Jakob, A. & Collier, L. (2017). Sensory Design for Dementia Care – The Benefits of Textiles. Journal of Textile Design Research and Practice, 5(2), 232-250. DOI: 10.1080/20511787.2018.1449078
Joltin, A., Camp, C. J., Noble, B. H., & Antenucci, V. M. (2012). A different visit: Activities for caregivers and their loved ones with memory impairment (2nd ed.). Solon, OH: Center for Applied Research in Dementia.
Lin, L. C., Huang, Y. J., Watson, R., Wu, S. C., & Lee, Y. C. (2011). Using a Montessori method to increase eating ability for institutionalized residents with dementia: A crossover design. Journal of Clinical Nursing, 20(21–22), 3092–3101.
Lin, L. C., Yang, M., Kao, C., Wu, S., Tang, S., and Lin, J. (2009). Using acupressure and Montessori-based activities to decrease agitation in residents with dementia: A crossover trial. Journal of the American Geriatrics Society, 57, 1022–1029.
Love, K. (2006). Montessori-based activities: A guide for using therapeutic engagement to enhance function for individuals with dementia. District of Columbia Office on Aging, Washington DC.
Mahendra, N., Hopper, T., Bayles, K. A., Azuma, T., Cleary, S., & Kim, E. (2006). Evidence-based practice recommendations for working with individuals with dementia: Montessori-based interventions. Journal of Medical Speech-Language Pathology, 14(1), XV–XXV.
Roberts, G., Morley, C., Walters, W., Malta, S., & Doyle, C. (2015). Caring for people with dementia in residential aged care: Successes with a composite person-centered care model featuring Montessori-based activities. Geriatric Nursing, 36(2), 106–110.
Sheppard, C., McArthur, C., & Hitzig, S. (2016). A Systematic Review of Montessori-Based Activities for Persons With Dementia. Journal of the American Medical Directors Association, 17(2), 117-22.
Smit, D., de Lange, J., Willemse, B., & Pot, A. (2017). Predictors of activity involvement in dementia care homes: a cross-sectional study. BMC Geriatrics, 17, Article number: 175.
Smith, B. & D'Amico, M. (2019) Sensory-based interventions for adults with dementia and Alzheimer's Disease: A scoping review. Occupational Therapy In Health Care. DOI: 10.1080/07380577.2019.1608488
Van der Ploeg, E. S., Eppingstall, B., Camp, C. J., Runci, S. J., Taffe, J., & O'Connor, D. W. (2013). A randomized crossover trial to study the effect of personalized, one-to-one interaction using Montessori-based activities on agitation, affect and engagement in nursing home residents with dementia. International Psychogeriatrics, 25, 565–575.
Verkaik, R. (2019). Effects of enriched thematic multisensory stimulation on BPSD in a Beach Room: A pilot study among nursing-home residents with dementia. NIVEL - The Netherlands Institute for Health Services Research. https://www.nivel.nl/nl/publicaties/7334
Wilks, S., Boyd, A., & … Bates, S. (2017). Montessori-Based Activities Among Persons with Late-Stage Dementia: Evaluation of Mental and Behavioral Health Outcomes. Dementia, 18(4), 1373-1392. https://doi.org/10.1177/1471301217703242
Citation
Weissberg, K. (2022). Multisensory stimulation rooms for persons with dementia: Design on a dime. OccupationalTherapy.com, Article 5481. Available at www.occupationaltherapy.com
