Agenda
- OT Evaluation
- Discharge Recommendations: Destinations and Insurance Considerations
- Interventions for the Hospitalized Geriatric Patient
- What is an ACE Unit?
- Future Directions
- Q & A
Acute care OT is an exciting and evolving field. We are going to be covering in this talk the OT evaluation, interventions for the hospitalized geriatric patient, discharge destinations like ACE units, and some future directions for OT in acute care.
Higher Hospital Spending On OT Is Associated With Lower Readmission Rates
- OT was the ONLY service category where there was a statistically significant relationship between increased spending and lower readmission rates.
Rogers, Bai, Lavin, & Anderson (2016)
In a study that used Medicare claims and cost report data, it was determined that OT was the only spending category that helped reduce 30-day readmission rates for clients with heart failure, pneumonia, and myocardial infarctions. Preventable hospital readmissions are recognized as an important indicator of hospital quality and increased hospital expenditures. Many older adults leave the hospital with new self-care impairments after adjusting for demographic, health, and functioning characteristics. In this study, unmet ADL needs were associated with a higher risk of hospital readmission. The implication here is to evaluate and plan before discharging home.
Occupational Therapy Role
- Assessing the functional level and providing discharge recommendations
- Skilled engagement in routine
- promote recovery
- prevent decline
- Patient and family education
- Collaboration with team
In the OT role, we focus quite a lot on assessing a patient's functional level and how this holistically impacts their discharge. We want to optimize engagement in a daily routine while the patient is hospitalized. We collaborate and consider the patient, the family, and the entire medical team. OTs can work on different units of the hospital anywhere from critical care to med surg., orthopedics, the emergency room, and more.
Evaluation
Beginning the Evaluation
- Chart review
- Ensure orders
- Medical history and admitting information
- Labs
- Any baseline or social information
- Nurse check-in
After receiving an order, we complete a chart review. We are interested in the client's medical history, admitting information and relevant labs, and baseline home information. Before going in to evaluate the patient, it is a great idea to check in with the nurse. This patient may have had a new event or change in status, and we want to make sure that if there are new issues not reflected in the chart that we are aware of them. We also want to find out what their existing equipment is at home.
Evaluation Components
- Prior Level of Function
- ADLs
- IADLs
- Functional Mobility
- Valued Occupations
- Environment
- Physical
- Social
- Cultural
- DME
We need to consider the client's prior level of function as well as the physical/social environment at home. We need to evaluate and develop client-centered goals to form a plan of care.
Building an Occupational Profile
Ultimately, we want to develop a person's occupational profile (see Figure 1).
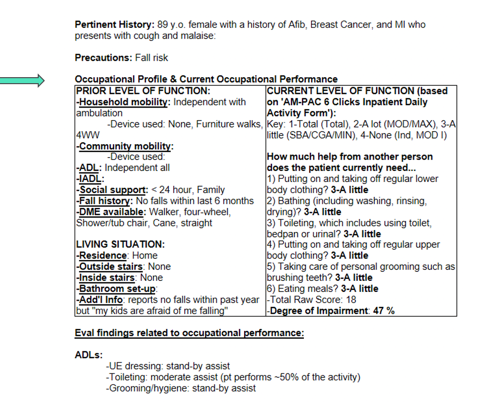
Figure 1. Example of an occupational profile.
The occupational profile includes the prior level of function, the living situation, the client's assets, and their strengths, barriers, and values. In this example, some of the pieces are not complete. This is because in acute care, we may or may not have family available or be able to gather all the pieces of information at our initial evaluation.
Functional Performance
The next step in the evaluation process is to engage the patient in self-care tasks to identify their strengths and impairments. We are simultaneously using clinical reasoning to assess activity demands and grade our tasks accordingly. Getting patients up early in their stay and helping them perform their daily routine is so important to prevent decline.
Self-care Related Mobility
The following are some basics with self-care related mobility.
- Set up the room prior to initiating –
- chair set up
- obstacles removed
- lines manageable
- have a backup plan if needed
- Pay attention to positioning and body mechanics
First, you want to make sure your environment is set up carefully prior to initiating movement. You want to move obstacles, ensure lines are manageable, and you want to think through a backup plan. You may also want to have a second set of hands with you. You want to use proper body mechanics during the positioning of both yourself and the patient.
- Encourage the patient to perform as much of mobility event as possible
- Step-wise progression of milestones
- Hospital policies for use of bed and chair alarms
One fundamental principle is that we want to encourage the patient to perform as much of the mobility task as possible. There is a step-wise progression of milestones. Initially, we are going to work on bed mobility and sitting at the edge of the bed for ADL tasks, such as grooming. If the patient can tolerate that, the next step would be to get them out of bed to the chair. From there, we could work on standing at the sink for grooming tasks and working on functional endurance. We need to meet the patient at their level and progress the milestones. You want to make sure to follow your hospital's policy regarding bed and chair alarms. For example, in my setting, all of our patients who are considered a high fall risk should be on a bed or a chair alarm. You also need to consider if the patient is safe to be left up in the chair especially if they have some kind of cognitive impairment. You always need to check with the nurse before you leave somebody up in the chair unattended.
Gait Belt Basics
- Gait belts should be used for transfers or ambulation with high fall risk patients, per the hospital’s policy
- Most patients can use a gait belt around the waist with a few exceptions:
- A large sternal or abdominal incision
- Multiple rib fractures
- Large burns or other wounds
- Trunk flap
- Colostomy
- Chest tube
Gait belts typically should be used whenever you are mobilizing a patient. You want to follow whatever your hospital's policy is. For example, we have single-use gait belts so that we do not spread infection from patient to patient, and it also allows us to have the patient take the gait belt home with the family as needed. We need to consider the patient's medical situation and use clinical reasoning when you are positioning the gait belt. You want to avoid affected areas like surgery sites, a colostomy, rib fractures, and so on. In these cases, you may want to position the gait belt in a different area instead of low and around the hips like we normally would. Sometimes, we need to train our nursing colleagues and model how to safely mobilize and handle patients.
Evaluation Considerations
- Strength
- Endurance
- Balance
- Performance skills
- Vision
- Falls history
- Safety awareness
- Functional Cognition
This is not an exhaustive list. Sometimes this is measured more formally with a standardized assessment. Other times, we are looking at clinical factors in the context of the self-care activity itself.
Cognition
- Cognitive Performance = Predictor for Failure at Home
- Cognition is one of the strongest predictors of medication non-adherence.
- Falls are also highly prevalent in individuals with cognitive decline.
Functional cognition considers the thinking and processing skills needed to complete everyday activities. This a unique cornerstone of OT. Many of our patients are on multiple medications, have new medications, or have a brand new medical condition to manage. Functional cognition considers not just the details of their cognitive status but how that translates into instrumental activities and daily living and higher-level tasks. Older adults may have the ability to carry out a conversation and retain some of their language skills, but they may have difficulty with novel problem solving or memory. The takeaway is to not be fooled by the patient who can carry on a great conversation. We need to dig further and make sure that they are understanding and carrying over instruction.
- Prevalence of Cognitive Dysfunction
- Parkinson’s Disease
- Various dementias
- Alzheimer’s, Vascular, FTD, Lewy Body
- Delirium
- Cerebral Vascular Accident (CVA)
- Hypotension
- Diabetes
- Brain damage
- Multiple sclerosis
The prevalence of cognitive impairment is associated with many conditions. We know that cognitive impairment is associated with Parkinson's, various dementias, delirium, which we will talk more about, stroke, hypotension, which relates to the body's ability to profuse the brain, diabetes, brain damage, and multiple sclerosis.
- Poorer Outcomes And Greater Healthcare Costs For Hospitalized Older People With Dementia and Delirium: A Retrospective Cohort Study
- Patients with cognitive impairment experience a greater length of stay
- When discharged to their usual residence are more likely to be readmitted to a hospital within 28 days as compared with those without cognitive impairment.
Tropea, LoGuidice, Liew, Gorelik, & Brand (2017)
Patients who have cognitive impairment are more likely to experience a greater length of stay. When they are discharged to their usual residence, they are also more likely to be readmitted within 28 days, as compared to those who do not have a cognitive impairment. Additionally, the costs are higher. There is also a higher chance of delirium developing the longer that patient's hospital course. OT can play an instrumental role in helping to increase outcomes.
Dementia, Delirium, or Both?
Delirium is extremely common in older adults. Delirium is due to pathophysiologic consequences of medical illness, certain medications, and combinations of medications. Having baseline dementia increases the patient's chance of becoming more delirious. It is certainly possible that a patient can have both, and this can create a confusing clinical picture. When you are not familiar with the patient, it is always helpful if a caregiver or family member can provide a little bit of context for you. However, in an acute setting, that is not always the case.
- Delirium: Confusion Assessment Method (CAM)
One of the ways we assess for delirium is by using the Confusion Assessment Method (CAM). According to the CAM, the presence of delirium requires both features one and two.
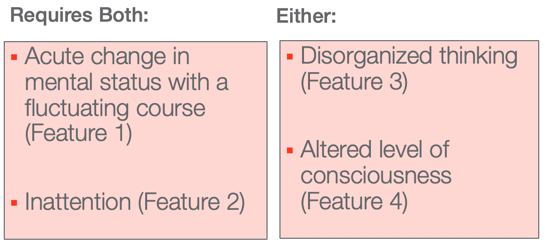
Figure 2. Way to determine if delirium is present.
Specifically, we're looking to see, has there been an acute change in mental status? As well as a fluctuating course, and some inattention? It requires the presence of either disorganized thinking or an altered level of consciousness.
Types of Delirium
There are different types of delirium (see Figure 3).
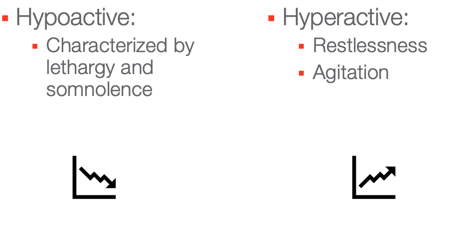
Figure 3. Types of delirium.
Hypoactive delirium is more common though it can be overlooked. An example is a patient who is sleeping, may have some motor slowing, and somnambulance. Hyperactive delirium may look like restlessness, agitation, or aggression. Both hypo and hyperactive folks, who have delirium, are at a higher risk for falls. The following are some of the things that we can do for patients who either have delirium or we believe are at risk for delirium. We can provide the patient with frequent reorientation. We do not want to quiz the patient, but rather, we can provide the information. You want to introduce yourself and your role with each new interaction. Utilize tools in the room like a calendar or a clock to help them reorient. You want to normalize any sensory deficits. If they wear glasses or hearing aids, make sure they have them. We want to implement as much of a routine as possible. This might mean making sure the lights are on. We want to have the windows open during the day. Try to get them on a normal sleep schedule which can be difficult if they are not feeling well. They need to spend more time out of bed than in bed. We want to normalize their ADL routine and communicate in calm and concise ways. Try to engage the patient in conversation about well-known and meaningful topics. We also want to encourage family and friends to visit the patient. Sometimes you can ask them to bring in familiar objects and pictures from home. These strategies can help a person to keep their bearing over their hospital course.
Vision
- Many seniors have eye conditions: cataracts, glaucoma, macular degeneration, etc.
- Reinforce the need for sensory devices, such as glasses. Ask the family to bring them.
- Reinforce eye care with the medical provider
We also want to consider is a patient's vision and possible impairments. A lot of seniors have eye conditions such as cataracts, glaucoma, macular degeneration, et cetera. Like we just said, we want to make sure that the person has access to their sensory devices like glasses, and we want to reinforce routine eye care with a medical provider. Sometimes, the patient has not seen a vision specialist for a while and they may not have updated information in their chart. We want to reinforce good habits and routines.
Standardized Assessments
- AM-PAC “6-Clicks” – Inpatient Daily Activity
- Mini-Cog
- Montreal Cognitive Assessments (MoCA)
- Menu Task
Another part of the evaluation is considering standardized assessments and using your clinical judgment to decide which standardized assessments you may want to incorporate. The AM-PAC "6-Clicks" Inpatient Daily Activity discusses self-care performance. The Mini-Cog looks at recall and a patient's ability to correctly draw a clock. What does this reveal to us? We want to see if they can create the shape, accurately place the numbers, and add in the clock hands for the appropriate time. This is just a brief screen of cognitive performance that is feasible in an acute care setting that might reveal some underlying deficits. The Montreal Cognitive Assessment is a widely-known 30-item screen. It looks at various cognitive constructs. There is value in it for that reason. Many on the medical team may be familiar with the MoCA, and we can be speaking the same language that they are. It might show issues with recall or executive performance as a screening tool, but we need to then extrapolate that information to make clinical predictions about what that means in their daily life. The Menu Task is a performance-based assessment that is designed to screen for deficits in functional cognition using a familiar activity of a simulated hospital menu.
- Executive Function Performance Test (EFPT)
- Allen Cognitive Level Screen (ACLS)
- Cognistat Neurobehavioral Exam
- Routine Task Inventory (RTI)
- Barthel Index/Modified Barthel
Another example of a standardized assessment is the Executive Function Performance Test. This looks at a variety of performance skills including the ability to manage medication. One of the things that I think is nice about this one is that it does have strong face validity and can be very helpful. Our teammates and families can understand why we are using a tool like this when we see a relevant activity like medication management being assessed. The Allen Cognitive Level Screen looks at novel problem solving within the cognitive disabilities model. I really appreciate this tool because it helps us screen levels of assistance needed at discharge. This is a very OT specific tool that helps distinguish our value. Another tool you might incorporate is the Cognistat Neurobehavioral Exam. This is a neuropsychological measure that provides a cognitive performance profile. It is a widely used tool, and OTs are specially mentioned in the manual as being one of the providers that are qualified to use and interpret the Cognistat. Another thing I think that is nice about the Cognistat is that one of the cognitive profiles looks at dementia syndrome. Specifically, some of the areas that may be identified as deficits are not being oriented, difficulty with constructing a design, and memory. Again, someone's language skills may still be intact, but they may be starting to struggle with things like abstract reasoning. As OTs, we are not diagnosing dementia, but this still could be helpful collateral information for the team. Dementia is not always listed in someone's medical history, but it is possible that they are having some struggles in that area. The Routine Task Inventory takes into account self-care performance from both the patient and the caregiver perspective. Barthel also looks at the patient's ability to perform ADLs.
Living Situation
- Private residence
- Stairs
- Bathroom set-up
- Support
- Habits/routines
- Independent living/senior housing
What is the patient's living situation? Where is this person going to go next when they discharge from the hospital? Did they come in from home? And, if so, what does that look like? Do they have stairs? Do they have a handrail? What is their bathroom setup? What level of support do they have? For example, if they live with a family member, does that family member work during the day, and are they available to provide assistance if that is a needed thing upon discharge? What are their habits and routines? Were they highly active before they came in? Were they sedentary? Understanding what their prior level of function and what their living situation is very relevant to our treatment planning. Sometimes, we have to tease this information out a little bit. In the chart, the patient may have been admitted, for example, from the emergency room. The chart may incorrectly identify where the person actually lives. While the medical chart is an important starting place, it is also great to try to get this information through our evaluation as well. People may also come in from assisted living.
- Assisted living
- Traditional
- Memory Care
Assisted livings are interesting in that they vary in terms of the level of services provided. We cannot assume that because they came in from assisted living that they have as much help as they need. They may provide only meals and housekeeping. Sometimes a resident can pay for assistance with things like bathing, medications, and dressing. There are also some distinctions for assisted living locations that focus on memory care. These are a little more inclusive, and they are more expensive. Usually, assisted living is private pay though sometimes individuals can qualify if they are low income or if they have long-term care insurance. It is great if they planned ahead and they bought long-term care insurance. However, more often than not, in my experience, folks do not have that. Assisted living may take some time to set up, and it may not be a direct transition from the hospital, even if that is what we want to recommend for discharge. I think it is important to have an awareness of that as you help to create the discharge plan. For example, a person may either need to go home with some support in the interim or go to a post-acute rehab setting before they can transition back to assisted living.
- Long-term care
Sometimes folks come in from long-term care. This can also be referred to as a nursing home, although that term is falling out of favor. Depending on how your hospital manages caseloads and triages, it may be pertinent to have the patient followed by an OT at the long-term care setting who knows their prior level of function instead of in an acute care setting. With that said, this does not mean we always would just sign off of this patient. If the patient was previously able to perform transfers to the toilet or the commode, and we want to promote that level of independence or engagement, we would continue to work on that skill in the acute care setting. Oftentimes, there are staffing limitations. Thus, we may spend more time on those people who need a discharge plan.
Interventions
Let's talk about some of the OT interventions that we might see in the acute care setting.
Activities of Daily Living
Activities of daily living are an OT hallmark. We want to make sure that we are engaging the patient in their daily routine and providing skilled assistance to improve their function and prevent decline due to the risk of immobility. A really basic one is oral care. This can be very neglected, and you may have some interesting surprises. Of course, this is part of nursing care as well, but it is an important thing to check up on while the patient is in the hospital especially if they have been confused. Reducing bacteria can decrease their chance of developing infections like pneumonia or sepsis.
Discharge Planning
- DC planning begins during the initial evaluation
- Continue to be assessed over the hospital course
Discharge planning begins over their entire hospital course. We need to think about it from initial evaluation all the way up to discharge. Lengths of stay can be quite short and there are many different discharge destinations: home, home therapy, sub-acute rehab, outpatient therapy, acute rehab, long-term acute care hospital.
Let's talk through some of these discharge scenarios. Perhaps, we recommend that somebody goes home but they need increased support. If they do not have family or somebody to help, could they use hired help? It is helpful for the team if we can distinguish the level of support that we mean. Are we talking about 24-hour support? Are we talking about daily checks? Are we talking about weekly checks? Are we only talking about transportation? The Cognitive Disabilities Model speaks to this directly in terms of what can be reasonably expected and the levels of assistance required. I particularly like the Allen Cognitive Level Screen for this reason. It can help determine what level of support is necessary. Oftentimes, home therapy can also be useful during the transition and carryover the instruction that we provided in the hospital. Also, they have the benefit of seeing the patient in their actual environment. We can make this recommendation that somebody goes home with home therapy. We can also make a referral to outpatient therapy or to an adjunct specialty service like pulmonary rehab or cardiac rehab.
Other services include an assessment for low vision OT or a driving evaluation. Often times, patients become deconditioned or debilitated and need a course of post-acute rehab. We are helpful in determining what makes the most sense. Should the placement be subacute rehab or is the acute rehab setting more appropriate? Acute rehab is going to require that the patient be able to participate for up to three hours a day, and there are also specific diagnostic criteria. Additionally, they may look at qualifying diagnoses like a neurological event, a stroke, brain injury, or an orthopedic injury. We often work with the physician and rehab team to determine if the patient qualifies or not. They may need more repetitive training over a more extended period of time, and we want to think through if that makes the most sense. If someone has a complicated medical, pulmonary, or skin integrity issue, a long-term acute care hospital might be more appropriate. This is referred to often as an LTAC. We need to use our clinical judgment in these cases.
Other Considerations
- Insurance
- Inpatient status vs. observation status-> may impact dc options
The payor source is important. We want to think this through as we develop our discharge plan. Medicare inpatients can go to a nursing facility for post-acute rehab if they are appropriate and have remaining days. Managed Medicare plans often have different stipulations. For example, they can go to post-acute rehab even if they are only an observation patient. For example, let's say a patient was admitted as an observation patient only. They would not have a qualifying stay under regular Medicare. This is important to consider. However, sometimes folks may not initially have a qualifying event, like a UTI, but it worsens over time, the patient might transition to inpatient status. Once they have reached those three midnights, they can go to post-acute rehab so long as they have some remaining days. It is important to collaborate with the case manager or social worker on the floor.
Patient and Caregiver Education
OTs provide all sorts of levels of patient education. Examples include reducing the risk of falling, encouraging engagement in self-care to minimize the risk of immobility, and providing diagnosis-specific care. We can also offer home safety and energy conservation tips. For example, a patient may have a new oxygen requirement. We can educate them on breathing techniques that will facilitate more functional endurance and safe mobilization during transfers.
Fall Risk Factors
- Physiologic/Individual
- Hazards in the environment
Falls are highly prevalent amongst older adults. They can be debilitating and deadly. Fall risks are multifactorial. It can be the combination of medication side effects, impaired vision, decreased safety awareness, poor footwear, as well as some environmental hazards. We can collaborate with our physical therapy colleagues to prescribe an appropriate assistive device for mobility like a walker. As an occupational therapist, we might be able to assess if the patient is cognitively able to utilize the walker effectively. They may need repetitive training and cues and how to sequence the different steps. There is a cycle that can occur when patients have a fall or even if they have not had a fall but are afraid. This can be seen in Figure 4.
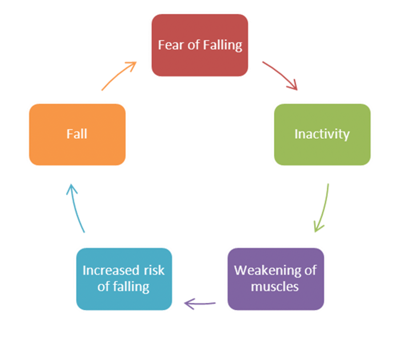
Figure 4. Fear of falling cycle.
There are adaptive and maladaptive strategies. One of our roles can be to help the patient understand the cycle that can occur. We want to take precautions to keep them safe, but also keep them engaged. The restricting of their activity can lead to the progression of decline. Inactivity might also lead to a weakening of the muscles and decreased strength. This increases their risk of falling. If they have another fall, they then become more fearful. As you can imagine, having a fall is a strong predictor of future falls.
Home Safety Recommendations
In addition to fall reduction strategies, we can teach medication adherence strategies. Our nursing colleagues might explain the specifics on the actual medications, but we can reinforce good habits and routines like using a medication organizer box. We can also encourage them to seek care for chronic medical conditions. We can also provide recommendations to the patient and family for IADL support like preparing meals and transportation. If they are not safe upon discharge, are there community services to assist? We also need to look at home safety and equipment needs.
- Bathroom
- Use of seat in the shower
- Tub/shower can be modified with a tub transfer bench
One of the key areas to hone in on is the bathroom. We know a lot of falls happen either on the stairs or in the bathroom. We should ask about their setup and then provide that education. If I have any concerns about their fall risk, I recommend they do a seated shower. Some patients are not as amenable to this as we would like, but we at least need to stress, "Hey, this is an area where you may be at risk of falls, and we want you to conserve your energy and decrease the chance of getting injured." If somebody has a tub shower, they can modify it with a tub transfer bench. Keep in mind that DME is not necessarily covered. So, if we are making these recommendations, we want to provide some different suggestions where the patient or family can either purchase or secure a loaner.
- Clutter
- Remove or tape down area rugs
- Pets
- Adequate lighting
Some other general principals around home safety are to reduce the amount of clutter and remove or tape down area rugs. If they have pets, they may need to seek out assistance for their care like walking in the short term or potentially long term if they have a new assistive device. They also need adequate lighting in their home.
- Individuals with severely impaired vision may benefit from:
- Low vision OT evaluation
- Support groups
Many older adults have different eye conditions so they may benefit from further outpatient screening. We have a low vision OT clinic where I work. It is nice to have this referral source. specific devices and collaboration with the ophthalmologist. They, as well, might benefit from home therapy where they could have somebody come in and make modifications and recommendations in their own setting, and, then, sometimes it's just helpful to have a support group. So, you might be recommending these things if someone has severe visual impairments.
Community Resources
- Caregiver education
- Support groups
- Diagnosis-specific services
We can provide community resource information. For example, if they complete certain high fall risk activities like yard work, snow shoveling, and deep cleaning, we can pass along community resources regarding these services. There are also diagnosis-specific resources and support groups that might be helpful. Here are some examples of resources available near me, but every community is different. I would encourage you to familiarize yourself with what is available near you.
- Local agencies
- Senior transportation options
- A Little Help
- https://www.alittlehelp.org/
- Rebuilding Together
- https://rebuildingtogether.org/?gclid=EAIaIQobChMI84KIhKmn5wIVhcDACh3DfAHTEAAYASAAEgLUffD_BwE
- Parkinson’s Association
- https://parkinsonrockies.org/
- Alzheimer’s Association
- https://www.alz.org/
Local government agencies often have some resources. For example, there can be different options for transportation. The organization, A Little Help, partners seniors with neighbors to help with high fall risk activities like the deep cleaning and yard work. Rebuilding Together is a national organization that has local branches that might help the patient with installing grab bars, building a ramp, or taking care of some things that are beyond reach for some seniors who are still living in the community. There are the Parkinson's Association and Alzheimer's Association in my area. The Parkinson's Association provides a lot of resources for exercise, support groups, and education groups. The Alzheimer's Association has a 24-hour hotline, and I think that is a really reassuring tool for patient's families who need dementia care strategies or a connection to resources.
What is an Acute Care for the Elderly Unit (ACE)?
Definition
This is a concept that has developed in some hospitals. The idea is to take care of the hospitalized older adult. Sometimes it is a physical unit, while other times it is a team within the hospital that serves geriatric patients. If the patient is being admitted for something more specialized like oncology, neurology, or a surgical procedure, they may be more likely to go to those services.
Specialized Team
One of the unique characteristics of an ACE service is that there is a specialized team. For example, there are specially trained nurses who are more familiar with geriatrics. You may have a geriatrician or a hospitalist who specializes in older adults. The team often also includes a social worker, case manager, CNAs, OT, PT, pharmacist, nutrition, and speech pathologist as needed. At my hospital, we also have a mobility tech who helps focus on getting patients up, making sure that they are participating as much as they can, in addition to what we have provided within the therapy context. Another helpful resource that we have on our interdisciplinary team is a resource discharge nurse. Her role is to summarize our discharge recommendations which can be really confusing when somebody is going home. They may need repetition of information, and this resource nurse has the ability to review our recommendations more thoroughly with the patient and family upon discharge. Sometimes these units are designed physically with seniors in mind, and that can be particularly nice. One of the important things that this service offers is interdisciplinary rounds. This is often a fruitful discussion of what are the barriers and what is the progression of the patient's medical course. We can then synthesize that from all the interdisciplinary perspectives in order to formulate a plan.
Common Diagnoses
- Frequent dx: PNA, UTI, s/p fall, AMS, orthopedic issues (often 2/2 fall), “FTT”
- Comorbidities
Common diagnoses that I have seen on the ACE unit are pneumonia, urinary tract infection, falls, altered mental status, sometimes orthopedic issues that are less complicated. This might include a patient who fell and had a humeral fracture, but they are not going to have surgery as an example. They might be more likely to end up on our ACE unit, as opposed to our orthopedic unit. Many times, there is a catch-all "failure to thrive" before the person has had a more specific medical condition diagnosed. Additionally, many older adults have a lot of comorbidities. We want to take that into consideration as well.
Future Directions for OTs in Acute Care
Policy and Payment Changes
- Cost-effective services
- Decreasing lengths of stay
- Avoiding costly post-acute rehab
- Quality outcomes
- Hospital-acquired conditions (falls, skin, infection)
Healthcare is dramatically transforming, and I think OTs can really impact patients at both the clinical and the system level in acute care. We can participate in different committees like ones on fall reduction or how to help with hospital throughput. OT has a relevant voice, and I encourage you to volunteer for those opportunities when able. As policy and payment changes continue to evolve, there is an emphasis on cost-effective services, decreasing the length of stay, avoiding costly post-acute measures, and quality outcomes. These measures can be tied to how the hospital is reimbursed. So, there is a lot of motivation to make sure that there is good patient experience and preventing hospital-acquired conditions.
Upstream Opportunities for OT
OT in acute care is an exciting and evolving field, and there is a great opportunity. Thanks for your time. I will now take some questions.
Questions and Answers
What is the typical length of stay on an ACE?
It is really variable, but I would say anywhere from three to five days. We have also had patients with limited resources and these folks have ended up in the hospital setting for crazy lengths of stay. The goal is always to minimize their chance of developing an iatrogenic condition and developing more sickness in the hospital. While we may want to move them along to the next setting, there may be variables out of our control. Are they getting worse? Have we had an opportunity to do caregiver training? Does the patient have a payor source for post-acute rehab? So, the length of stay can be variable.
How are visits are becoming more and more limited, and what can we do in terms of providing education or teaching patients, and caregivers?
The earlier we are able to become involved the better so that we can have repetitive training overtime. Sometimes, the "one and done" approach with this population is not enough. If we can start early with our intervention, this can help with the transition.
What do you recommend is most important to address aside from fall risks?
Let's say they have CHF or newly diagnosed diabetes. I think helping partner with our nursing colleagues to make sure that they know the management principles of taking care of those issues when they get home is a valuable role for the OT. Are they carrying the new information over into the next session? If we do not think it is within their ability, we want to work with their family and make sure that they are going home with support. When you are in a hospital, it can be overwhelming. There are so many different factors happening. We need to make sure that our client or their family is understanding what is needed for their care. A good example is how to safely mobilize a patient. A family member could benefit from both watching the therapist perform the activity and then demonstrating it. I like to have them practice taking a gait belt on and off and practice how would they safely cue a patient.
Can you talk more about a low vision OT clinic?
This is an excellent tool that many communities have available. Patients need to be relatively cognitively intact to be referred to the low vision clinic because they are being taught using different strategies and need to be able to carry it over.
Do you spend a fair amount of time educating the physicians to get quick and appropriate early referrals?
I would say this is a continuous challenge. I work in a teaching hospital so that means that each month, we have to reestablish who is appropriate for therapy and try to get into that kind of routine. Certain diagnoses already have PT/OT as part of the order. There are also those times when we do not need to see the patient as they are at their prior level of function, even if that prior level of function meant they have a spinal cord injury.
Are we as OTs providing the best care possible in this setting?
I think this is a great question. I feel like there are a lot of things that I would like to focus upon more with my patients, but then I have to balance that with the limitations of staffing. The hospital is a business, and they allocate resources accordingly. There are not always enough OTs around. We need to be focused on where to expend our energy. Can we see the right patient at the right time?
Will the role of the occupational therapy assistant change in the acute care setting?
We have had different COTAs on staff in the past, and we look to potentially have them in the future. There is some challenge in that they are not able to perform evaluations, but they certainly are our care partners. I am not aware of a trend in one direction or another with regard to COTAs in the acute care setting.
Is there any advice or techniques that you use to ensure special instructions with nursing staff are followed?
I think there are multiple ways that we can address this. We can provide direct instruction with nursing. With that said, it may not carry over to the next one so we would want to be sure it is documented in the plan of care. We have an electronic medical record system. At the very top of each of our notes, whether it is an evaluation or a progress note, there is a box that has highlighted information that says "recommendations to nursing." It identifies what level of assistance they need for basic self-care and transfers as examples. We can also provide group instruction in transfer training and safe handling strategies. Our nurses received orientation, but it can be helpful to provide an in-service on these sorts of things so that there is improved carry over and gives them an opportunity to practice with an occupational or physical therapist directly. Another tool to help with carryover is a whiteboard that is in front of each of the patient's beds. On the whiteboard, there is some information to help the patients stay oriented and decrease their chance of developing delirium. There is also some information about what level of assistance is needed for performing functional mobility and self-care tasks. We want to be sure and keep that information updated.
Can you share some fall risk protocols?
In our setting, we want to have the patient on a bed or a chair alarm if they are at a high fall risk. We also use yellow socks if the patient is a high fall risk as a quick visual cue. Nursing staff reassesses it every shift (every 12 hours). The patient is reassessed to determine if they are a high fall risk and are reoriented to using the call light and not getting up on their own. We want to help keep them safe and balancing that with not trying to restrict their activity level. We want them to engage in their daily routine, but we want to reassure them that we like to have a staff person with them. I think sometimes it is helpful to ask the patient, "Can you show me what you would do if you needed some help?"
References
Depalma, G., Xu, H., Covinsky, K. E., Craig, B. A., Stallard, E., Thomas, J., & Sands, L. P. (2012). Hospital readmission among older adults who return home with unmet need for ADL disability. The Gerontologist, 53(3), 454–461. doi: 10.1093/geront/gns103
Inouye, S. K. (1990). Clarifying confusion: The Confusion Assessment Method. Annals of Internal Medicine, 113(12), 941. doi: 10.7326/0003-4819-113-12-941
Pritchard, K. T., Fisher, G., Rudnitsky, K. M., & Ramirez, R. D. (2019). Policy and payment changes create new opportunities for occupational therapy in acute care. American Journal of Occupational Therapy, 73(2). doi: 10.5014/ajot.2018.732002
Rogers, A. T., Bai, G., Lavin, R. A., & Anderson, G. F. (2016). Higher hospital spending on occupational therapy is associated with lower readmission rates. Medical Care Research and Review, 74(6), 668–686. doi: 10.1177/1077558716666981
Tropea, J., Logiudice, D., Liew, D., Gorelik, A., & Brand, C. (2016). Poorer outcomes and greater healthcare costs for hospitalised older people with dementia and delirium: a retrospective cohort study. International Journal of Geriatric Psychiatry, 32(5), 539–547. doi: 10.1002/gps.4491
Citation
Andrews, M. (2020). Acute care back to the basics: Gerontology. OccupationalTherapy.com, Article 5176. Retrieved from http://OccupationalTherapy.com
