Introduction
I am super excited to be here today. My hope is that you will go from feeling unsure of where to start teaching gross motor skills to feeling better prepared and more confident. I hope to impart a simple, yet strategic therapy framework to support the developmental progression of the key mobility milestones for infants and toddlers.
Here is a little bit about me. I am a clinic owner in Seattle, Washington.

Figure 1. More about me.
One of my greatest projects so far has been launching my website playitforwardtherapy.net. My wish is to use this website to really convey the value of occupational therapy and to provide ideas and inspiration for other OTs as well as parents and teachers. Another thing that is near and dear to my heart is advocating for our profession as therapists. I have had the chance to testify at the Washington state legislature to help make sure that our clients are not facing obstacles to getting the special services that we provide. I love being an OT, have 20 years of pediatric experience, and I am looking forward to sharing with you what I know about early intervention.
This is an introductory course. At the end of the presentation, I will give you some more information on how we can continue to have clinical conversations and answer any questions that you might have. I also hope that you find the handout helpful as you go through this presentation. Like I mentioned earlier, this is an introduction to gross motor milestones which is a huge topic. I have created a step-by-step guide to infant mobility.
Figure 2. Motor milestones link. https://www.playitforwardtherapy.net/optin-milestones/
Role of Motor Skills in Overall Development
- Motor skills are essential for infants and toddler’s participation and occupations in activities of daily living, play skills, self-care and social interactions (Case-Smith et al., 2013)
- Motor skills are key for learning and enable children to explore and learn about the world around them.
It is from newborn to walking, and the above handout includes the major milestones and the key transitional movements to get to the next phase. It is also clearly outlined to systematically guide your therapy sessions. When I started 20 years ago, I really wish I had had something like this. So, hopefully, I am saving you 20 years in figuring out what step goes where and being really clear on mobility milestones. When I came into the profession in early intervention, I did not have a whole lot of training on mobility and how to help infants and toddlers with their gross motor milestones. So, I hope that you will find helpful. The presentation is going to be an overview, so I am hoping that this handout will really be a good supplement for your learning and for your knowledge.
The Pediatric Intervention Framework

Figure 3. Pediatric Intervention Framework.
The Pediatric Intervention Framework is a framework that I use to help guide my clinical reasoning and how I approach sessions. You are going to start with the targeted skill or activity. And, of course, you want to ask, "What is the purpose of this activity?" And for positioning, "What are some strategies for positioning?" Finally, you want to look at their practice. "What are some ways that you can integrate this session or the therapy milestones that you are working on in your session to everyday routines?"
The next part of the framework is playing. In pediatrics in general, play is such a huge component. It is definitely one of the primary roles and one of the domains that OTs need to address. It is one of the most challenging, exciting, and fun parts of being able to work with this age group. It is really embedding our therapy sessions with play to make things motivating especially for activities that are really hard for kids or that they do not want to do. That is the key element.
The other component of the Pediatric Intervention Framework is progress. You want to make sure that you are tracking progress and that you are writing goals that are SMART (specific, measurable, relevant, realistic, achievable, and timely). As we go through the slides and each of the motor milestones, you are going to see some of these concepts highlighted, and that will refer back to the Pediatric Intervention Framework.
Primary Areas of Intervention for an OT in EI
The primary areas of intervention for an OT in early intervention are in Figure 4.
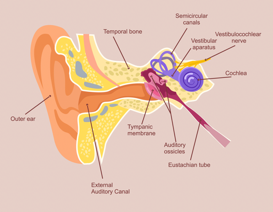
Figure 4. Primary areas of intervention.
One area is cross-training. OTs and PTs are often called motor therapists. We are responsible for working on gross motor skills and mobility as well as knowing how to help kids with their fine motor, sensory, and adaptive skills.
Motor Skills Follow a Specific Pattern of Development
- From head to toe (cephalocaudal)
- From the center of the body to the outside (proximal to distal)
The acquisition of motor skills follows a very specific pattern of development from head to toe, cephalocaudal, and also from the center of the body to the outside, or proximal to distal. An example of cephalocaudal development would be head control. It is a prerequisite for other motor skills. Lifting the head strengthens the neck and the back, and it allows the infant to prop and to move on its arms and legs. And, good head control is also prerequisite for rolling, sitting, and walking because all of these milestones are dependent upon voluntary changes in head position.
An example of proximal to distal is core strength and shoulder stability. It is really important for the child to have good core strength and shoulder stability because this supports the development of more fine motor and dexterity skills.
Risk Factors for Motor Delays
Let's talk about some of the risk factors for motor delays.
- Medical and birth history
- Neurological problems
- Retained primitive reflexes
- Visual impairment
- Hypotonia (low muscle tone)
- Decreased strength & endurance
- Increased joint flexibility
- Short limbs: arm and/or leg length discrepancy
The first one is medical and birth history. Medical problems might include prematurity, prior hospitalizations, chronic infections, ear problems that will impact balance. Neurological problems can be cerebral palsy and hemiplegia. Retained primitive reflexes, visual impairment, as well as hypotonia, or low muscle tone, are other issues. Some children might have lower muscle tone in different parts of their bodies like in their extremities which might make it difficult for them to prop on their arms or walk. This is commonly seen in children with Down syndrome for example. Decreased strength and endurance, as well as, increased joint flexibility or laxity are also common problems. The ligaments holding the bones together have a lot more slack, and in cases of decreased joint stability, you may see kids with flat feet or dislocations of their shoulders or hips. The other aspect is short limbs or having an arm or a leg length discrepancy.
In this first slide, we have Baby M who you will see throughout this presentation. She us our little case study. She was born prematurely. Her mom went into labor at 29 weeks, and when she was delivered, she had an APGAR score of one out of 10.
Figure 5. Baby M- APGAR 1/10.
As a refresher on APGAR, A is for appearance, P is for pulse or heart rate, G is for grimace, which is reflexes, A is for activity for muscle tone, and R is for respiration, or breathing rate and effort. Then on the next slide, we have another baby just demonstrating one of the reflexes, the asymmetrical tonic neck reflex.

Figure 6. Demo of the ATNR.
How to Adjust for Prematurity
- Two important dates
- Birthday
- Expected due date
- Take the age of the infant in weeks and subtract the number of weeks born early.
- Example: 16-week-old (born 4 weeks early)
- The adjusted age is 12 weeks or 3 months.
When working with infants who are premature, it is really important to make sure that you adjust for the baby's age for prematurity. There are two important dates to consider. The first is birthdate, and the second is their expected due date. You want to take the age of the infant in weeks and subtract the number of weeks born early. For example, if you have a 16-week old that was born four weeks early, the adjusted age is 12 weeks or three months. Even when they catch up in physical size that is typical for their age, they still might be experiencing some delays. It is important to go back to their birth and medical histories to shed some light on some things that might be impacting their development like prematurity. It is also important to read your assessment manuals to make sure at what age you should be adjusting for prematurity when scoring.
Sensory Processing Influences Motor Skill Acquisition and Temperament
Sensory processing influences motor skill acquisition and temperament. I want to go over a very quick review.
The vestibular system is your receptors in your inner ear. They sense balance, position in space, and movement (Figure 7).
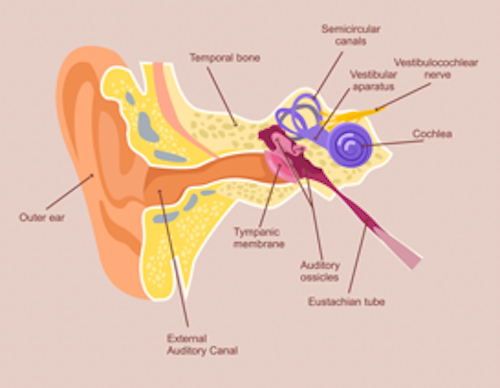
Figure 7. Vestibular system in your inner ear.
Your proprioceptive system is the receptors in the muscles and joints. They detect deep pressure input which is important for body awareness (Figure 8).
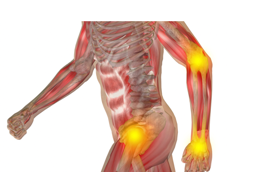
Figure 8. Proprioceptive system in the muscles and joints.
Sensory Profile
- Motor-Driven
- Seek vestibular input and/or proprioceptive input.
- May have difficulty grading the force of movement.
- Observer
- Tend to avoid vestibular input or have an impaired sense of balance; therefore tend to be more cautious.
A child's sensory profile can also impact temperament, either motor-driven or as an observer. It is important to think about how sensory processing impacts their approach to motor skill acquisition. The first one is motor driven. Does the baby seek vestibular input and/or proprioceptive input? They may have difficulty grading the force of movement. These are the kids that are often described as extremely active. Or, are they an observer? Do they tend to avoid vestibular input or have an impaired sense of balance? If this is the case, they might tend to be more cautious or a little bit more fearful when attempting movement or new milestones.
Video 1

This is Baby M, who you saw coming out as a premature infant. What do you think her sensory profile is? If you were thinking "motor-driven," then you are correct.
I want to share with you a little bit of how her medical history could impact this type of behavior. First of all, it is very cute. However, this is not typical to continually fall back and roll over and over. When she was in the womb, her mom was on bed rest for almost two months. Normally, when babies are in the womb, they are getting a lot of sensory input from the mother, both vestibular and proprioceptive information. If kids do not get that in the early phases of development, you will see that come out later. This is an example of that, and it makes sense for her sensory profile.
Developmental Progression of Gross Motor Milestones
- Phase 1: Tummy Time, Side lying and Back lying
- Phase 2: Rolling
- Phase 3: Sitting, Transitions
- Phase 4: Crawling
- Phase 5: Pulling to Stand, Standing, and Cruising
- Phase 6: Walking
- Phase 7: Post Walking Skills: Running, Jumping, Ride-on toys, Stair Climbing, Ball skills
I broke this up into different phases. Phase one is tummy time, side lying, and back lying. Phase two is rolling. Phase three is sitting and really important transitions. Phase four is crawling. Phase five is pulling to stand, standing, and cruising. Phase six is walking, and phase seven is post walking skills, like running, jumping, ride-on toys, stair climbing, and ball skills. This talk today is going to cover phases one through six. In a future course, I will cover Phase seven.
Phase 1: Tummy Time, Side Lying, and Back Lying
- Parents not putting infants on stomachs for supervised playtime has impacted the rate of acquisition of motor skills (AJOT; Salls, Silverman, Gatty 2002).
- One Level II study found significant improvements in Bayley-3 scores for infants with Down syndrome whose caregivers initiated tummy time early (Wentz, 2017).
Here is a little bit of history for tummy time. In 1994, the American Academy of Pediatrics introduced the Back to Sleep campaign. This was to help prevent SIDS, which is Sudden Infant Death Syndrome. The campaign was to educate parents about safe sleeping and to put infants on their backs when sleeping. The interesting thing is that it also affected tummy time as some parents may have been more hesitant to put their children on to their stomachs. Tummy time is definitely a good thing, especially during waking hours and during supervised playtime. There was a study from AJOT in 2002 that highlighted that when parents did not put infants on their stomachs for supervised playtime that it impacted the rate of acquisition of motor skills. Another study found that there were significant improvements in Bayley-3 scores for infants with Down syndrome whose caregivers initiated tummy time early.
Safe Sleeping & Supervised Tummy Time
- Sleeping: Back to Sleep
- Playing: Supervised tummy time. Practice a few minutes a few times a day.
When babies are sleeping, they need to be on their backs, but when they are awake, it is important to have supervised tummy time and to practice a few minutes and for a few times a day. In the next couple of slides, I am going to talk to you about some strategies and some ways to encourage tummy time.
Tummy Time: 0-3 months
- PURPOSE
- Develop head control
- Increase tolerance for prone position
- Head control is an important precursor for rolling, crawling and the timely acquisition of motor skills
The purpose of tummy time in the 0-3 month stage is for them to develop head control and increase their tolerance for a prone position. Head control is an important precursor for rolling, crawling, and the timely acquisition of motor skills. Here is an example of a little one who is on an incline in prone (Figure 9).

Figure 9. Positioning on a wedge.
In this picture, I want you to notice her leg position. We really do not want frog legs. We want her legs straight. She is almost two here, and she had a significant history of hospitalizations and major surgeries as an infant. During the time that she normally would have been in prone and on her tummy, she was in the hospital much of the time on her back.
