Introduction and Overview
Good morning, I'm excited to be presenting to you today on the topic of yoga, and how it can be beneficial for individuals recovering from an addiction. First of all, we are going to define and break down the concept of addiction as a disease. According to Merriam-Webster.com, a disease is defined as "a condition of a living animal or plant body or one of its parts that impairs normal functioning and is typically manifested by distinguishing signs and symptoms: sickness, malady, infectious diseases." That's a pretty straight-forward and specific definition. When we look at the meaning of addiction, several organizations have offered their own definitions of what constitutes an addiction.
- The National Institute on Drug Abuse: Addiction is defined as a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences. It is considered a brain disease because drugs change the brain—they change its structure and how it works. These brain changes can be long-lasting, and can lead to the harmful behaviors seen in people who abuse drugs.
- American Society of Addiction Medicine: Addiction is a primary, chronic disease of brain reward, motivation, memory and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social and spiritual manifestations. This is reflected in an individual pathologically pursuing reward and/or relief by substance use and other behaviors.
- DSM-IV Substance Use Disorders: The DSM-5 no longer uses the terms substance abuse and substance dependence, rather it refers to substance use disorders, which are defined as mild, moderate, or severe to indicate the level of severity, which is determined by the number of diagnostic criteria met by an individual. Substance use disorders occur when the recurrent use of alcohol and/or drugs causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. According to the DSM-5, a diagnosis of substance use disorder is based on evidence of impaired control, social impairment, risky use, and pharmacological criteria.
Definitions related to addiction have evolved over the years. Back in the 1930s, the founders of Alcoholics Anonymous described alcoholism as an allergy, or an internal itch. If someone is allergic to strawberries, if they eat a strawberry, that allergen enters their bloodstream, resulting in a reaction that leads to a visible rash on their skin. With alcohol and addiction, the theory is that the itch is internal, and the only way to soothe that itch is to bring in more of the same substance. Since the 1930s, there has been extensive research and medical advances to better define and describe addiction. Recently, the DSM-5 has started to acknowledge technology addictions, such as video games, the internet and social media. As defined by Tommy Rosen, yoga teacher and addiction recovery expert, "Addiction is any behavior that you continue to do despite the fact that it brings negative consequences into your life." Throughout this presentation, it is important to recognize not only the more "standard" substance addictions, such as drugs and alcohol, but also behavioral addictions, such as gambling, sex and food.
How Do We View Addiction?
First, I want everyone to take a moment and ask yourself a few questions:
- How do you view addiction?
- What is your experience with addiction?
- Have you been impacted directly by addiction?
When I'm doing a talk out in public, many people respond to these questions by saying they're not affected by addiction at all. However, if you think about it, addiction costs taxpayers money. When we start looking at things like emergency medical responders, fire fighters, social workers, etc. -- in those ways, we are all affected by addiction.
Do you view addiction as a choice or a disease? Or, is it a nature versus nurture situation? One might as well argue which came first, the chicken or the egg? The way I look at it is using the following analogy: If the truck is in the ditch, it really doesn't matter how it got there. What we have to be focused on is how we're going to get that truck out of the ditch. How are we going to look at this situation and doing something about it?
Who Will Become Addicted?
Now I would like to give you a scenario. Three gentlemen from different walks of life each slip and fall on the ice, and tear their right ACL. All three of them had the same surgeon, and all three were prescribed Percocet with exactly the same instruction.
- Joe is a corporate executive with a great salary. He has a perfect life, with a wife and two children. He owns a house, a boat, and a cabin in the woods. He is happy and loves his life.
- Elvan on the other hand is making $40,000 a year working in a restaurant on the kitchen staff. He has five children and a wife. He owns a car that needs brakes. His family is living in an apartment, and they struggle every day to make ends meet.
- Jose is homeless. He is unemployable, living on the street.
Which one of these men is going to become the addict? The reality is that there is no way to determine which one is going to become an addict. For example, right now I'm working with a woman who is 70 years old. She is a good Christian woman, never had a drink in her life, always went to church. She had a hip replacement and was put on Percocet. At the end of the first prescription, her doctor refilled it. When that refill ran out, the doctor would not refill it again, and sent her home without detoxing her. Lying on her couch going through severe withdrawal, her nephew went to got her some heroin. We're now working with a 70-year-old woman who is a heroin addict. We're trying to educate people that you cannot rely on stereotypes, and that what you think is going on might not be the case. We have to stay open-minded.
Next, I would like to conduct an exercise to determine whether or not a person might have an addiction issue. Think about the first time you drank alcohol. When I give talks and I ask this question, if someone describes their first drink by saying, "Oh, I don't know, maybe it was in college. I really can't remember," I would determine that that person is probably not headed into addiction. However, when I ask that question and I get a response like, "Oh, it was a beautiful summer afternoon and I had a glass of wine on the patio, and the angels started to sing and I could dance and hold a conversation and I was no longer shy and ugly," that's probably a good indicator that there might be a potential for addiction. This is because in the body of the addicted person, the response can be significantly different. The addictive substance or behavior does for the addict what it doesn't do for the non-addicted person. It affects them on a neurological and hormonal level. There is a significant difference between the person who nonchalantly remembers their first experience, and the person who falls deeply into the experience and what it did for them.
Signs and Symptoms of Addiction
There are many signs and symptoms of addiction. Some of these we will discuss in further detail in part two of this series (Figure 1):
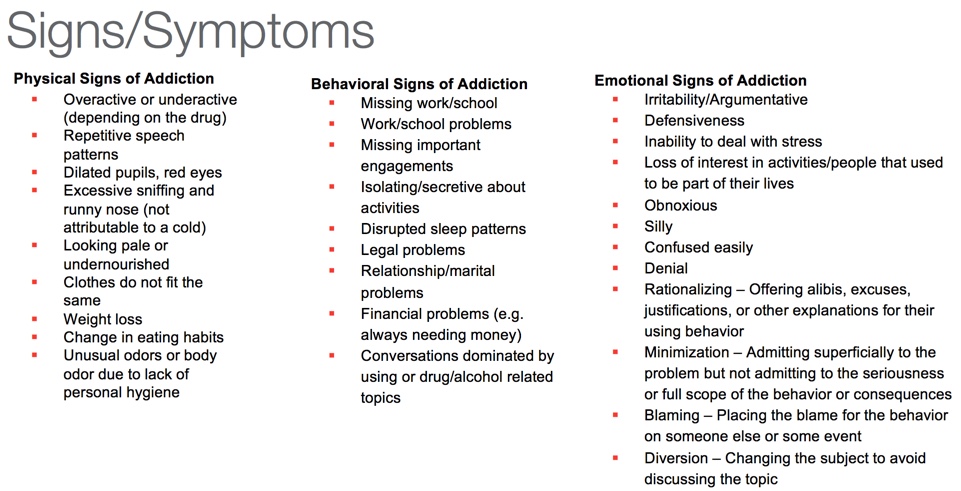
Figure 1. Signs and symptoms of addiction.
Trauma and Addiction
Recently, people have begun to focus more on the effects that trauma has on addiction and addictive use. The physical response to trauma is one of tensing and readiness, fight or flight. That grasp, that holding of the breath, tightening of the perineum, the protective response are all examples. When a trauma occurs, the brain automatically goes into a protective response. We know this from our studies, and we know this from our education as therapists. When the body returns to normal and the trauma passes, everything comes back into a regulated and calming state.
Trauma can be described as a protective reaction caused by a stressful occurrence which is outside the range of usual human experience. What is a "usual" human experience? What might be usual for me is certainly not usual for someone else. If I live in an abusive household, yelling and screaming is usual and normal. If I've grown up in a quiet household where shouting is not the norm, the first time it happens can be very traumatic.
If you're a child and living in the mountains, and a grizzly bear comes into the house, that is a traumatic event. What happens if the bear comes into the house every night? What happens to the child's physical body and their physical and emotional state if night after night, that trauma occurs and as it becomes normalized over time? More study needs to be done in this area, and we'll go into it a little bit more in part two, but I wanted to give you a foundation of how trauma potentially relates to addiction.
Another increasingly common occurrence is therapist post-traumatic stress disorder. As we work with clients who relay their traumatic experiences to us, we're empathizing with them. As a client tells their story, our heart rate may increase, and we may begin to sweat. In those instances, our body is taking on a little bit of that person's trauma. It is important for therapists to be aware of this.
Pendulum of Normal vs. Addictive Behavior
In Figure 2, the arrow down the center represents the pendulum of normalcy, so to speak. It hangs straight down. What happens when someone starts using drugs or alcohol? I like to use the analogy of autopilot on an airplane. When you set your airplane on autopilot, it is not flying the plane from point A to point B in a straight line. The function of autopilot is to bring the plane back on course if it goes off the mark. You're not flying from point A to point B, but rather you're in this erratic pull back and forth, always correcting stay on the right path.
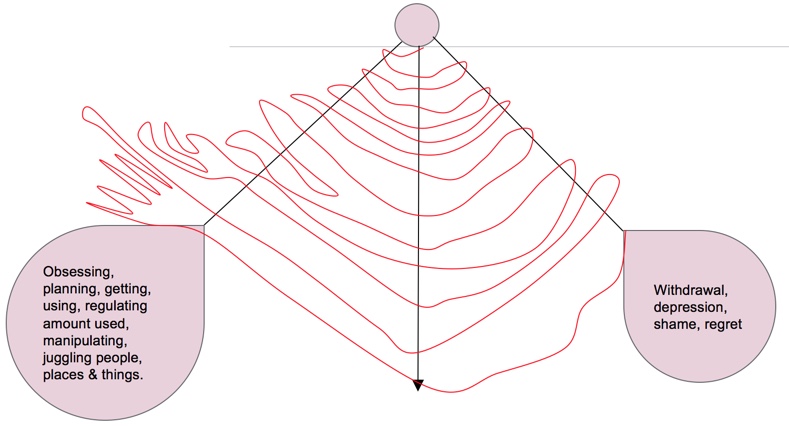
Figure 2. Pendulum of normal vs. addictive behavior.
If someone uses drugs or alcohol, they might drink a little too much at a wedding, for example. The next day, they're starting to look back at their behaviors. The pendulum of the addicted person will swing to the right, feeling withdrawn and depressed. They can't believe how they behaved the night before, and they are extremely hungover but they must to go to work. What do they do next? They start thinking about what's going to fix their situation to bring it back to normal. Is a good breakfast going to fix it, or possibly vomiting? Perhaps they will stop the shakes by taking a Xanax. Over time, the pendulum swings further, and the person becomes obsessive. They begin to justify their behavior, and manipulate situations to their advantage. They start a juggling act, of people, places, things. They set up their environment so that as use increases, the behaviors needed to bring that pendulum back into alignment start to grow, resulting in a wider range of those signs and symptoms that I pointed out earlier. As more time passes, this pendulum swing is no longer smooth. It becomes very erratic, and covers a wider area. Over time, it will continue to swing out into the obsessive behavior, the planning, the manipulating, conniving and lying, in order for the person to maintain their addiction in any way possible. As the weight of addiction gets heavier, happiness, health and everything that is typical in a "normal" person's life is thrown out of balance.
Three Cs of Addiction
The three Cs of addiction can be described as follows:
- Loss of control over the amount and frequency of use
- Cravings and compulsive using, accompanied by compulsive thinking
- Continued use in the face of adverse consequences
I'd like to assert that there's a fourth C of addiction: the loss of community supports. Over time, the addict burns up jobs, co-workers, friends and, at a certain point, their family. The Al-Anon program uses the phrase, "detach with love". You have to protect yourself. If you don't cut off an addict, and they don't hit rock bottom, and it's never going to stop. Disown them, cut them out of your life, send them on their way for your own self-protection. However, when that happens, it's like cutting the final thread. Unfortunately, many times that is not a wakeup call for the addict, but it becomes a death sentence, as there are no remaining threads normalcy holding that person together.
There's a book called Beyond Addiction: How Science and Kindness Help People Change (Foote, Wilkens and Kosanke, 2014). It outlines how family members can change their behaviors and support themselves, and at the same time, not enable the addict to continue in the behavior. It's more of a loving kindness approach to health for everyone. Until it's over for that individual, it's not going to be over. For some people, over could mean that they had one too many drinks at a wedding and they never have to drink again. For other people, it's homelessness, job loss, near death and multiple overdoses before it finally clicks for them. I encourage you to check out this book, which asserts that there is a softer, easier way to help people get to that bottom, without it being an absolute crash-and-burn situation.
Sobriety
What is the opposite of addiction? The typical response I hear to this question is sobriety. Sobriety is defined as the quality or state of being sober. Sobriety connotes dignity, level-headedness and common sense. How many times have we all heard, "If she would just stop using, it would be okay," or "If he could just control how much he drinks"? With an addict, they use because their substance is the mental, physical, emotional and spiritual solution. Simply being sober is not the answer, and in fact, it is a more dangerous place. If you take an addict or an alcoholic and lock them in a room, they will be sober. However, that is not where we need to be going. What we need to be looking at is recovering and what recovery means.
Recovery
Recovery is comprised of many different layers. First, recovery is abstinence from primary and secondary substances. In other words, you can't stop doing heroin and start drinking whiskey. You can't give up the whiskey and switch to marijuana. One must abstain from primary and secondary substances. In addition, recovery means a return to health: physically, mentally, emotionally and spiritually. Finally, recovery involves becoming an active member in the community.
In order for an addict to recover, yes, they must stop taking drugs or drinking alcohol. However, once the substances are out of the body and out of the bloodstream, there's a huge realm of change that needs to occur in order to bring this person into full recovery, and into full life once again. Recovery can be a balancing act, especially early recovery. Too much of anything risks injury, too little risks atrophy. The person in recovery needs to find a state of homeostasis, and equal balance.
