Editor's note: This text-based course is a transcript of the webinar, Assessment And Treatment Strategies To Boost Brain Skills In Partnership With The Pocket Occupational Therapist, presented by Cara Koscinski, OTD, MOT, OTR/L, CAS.
Learning Outcomes
- After this course, participants will be able to:
- Identify the importance of movement to overall brain function and occupational performance.
- Recognize physical manifestations of immature brain function.
- List movement strategies that can be used to improve brain skills and build movement opportunities.
About Me
- Mother to two children with autism
- Advisor for OT and contributing author for Autism Asperger, Sensory Digest Magazine
- Speaker across the US for Universities, Future Horizons, state and local organizations
- Founder of The Pocket Occupational Therapist
- Former lead at the University of St. Augustine’s OTD & MOT
I am excited to be here. As a mom and therapist, I want to help to make all of our lives better. I just love our profession and that we can work together and learn from each other. This is a topic that I am passionate about because of the two little boys that you see in Figure 1.
Figure 1. The author's two sons on the cover of a magazine.
These are my boys, and they are not little anymore. My older son will be 22 next month, and my younger son is 19. In the early 2000s, the internet was not as big as now. I did a lot of reading about autism and wanted to share it with other parents. I did not start my career as a pediatric OT. I graduated from Duquesne in 1997 with a master's in occupational therapy but worked with grownups until my kids were diagnosed, and then I switched gears. I started writing books at this time, as shown in Figures 2 and 3.
Figure 2. Author's books.
Figure 3. More of the author's books.
As they got older, you could see the progression of all of my work throughout my kids' lives. My younger son has a complicated medical history, and he and I wrote a social story called My Mighty Mito and published it. I wrote the Sensorimotor Interventions book because I felt I was not meeting student outcomes. I did a lot of research and found that many kids were stiff and robotic in their movements. I wanted to figure out why and did a lot of research.
Why Movement?
- Children often struggle with fidgeting, decreased attention, and immature motor patterns, which manifest themselves through frustration and behavior issues.
- When our body’s systems are not integrated to form a strong foundation, difficulties in many areas occur.
- The optimal function of our bodies occurs when our sensory and motor systems are strong and able to adapt to the demands of the environment.
Movement is critical. When there was no technology and people worked on the land, people usually got up very early. They were out in the sun or rain, and their melatonin was released when it got dark. People were not as sedentary, and chemicals developed in our brains through movement. When there are immature body systems due to disease, disability, birth injury, et cetera, there can be many issues in the body's systems.
I wrote the book Sensorimotor Interventions before COVID, and I am finding that it is even needed more now. For example, we now have something called "tech neck." This is overuse of the spine due to looking down at devices. The ramifications of the overuse of devices are decreased melatonin production, increased pain in the neck, and increased stress. Right now, I want you to take a deep breath and relax your shoulders. We need to understand that demands in our environment affect our performance, and it is essential to take time to take a mindful moment. Examples of container syndrome and poor posture are shown in Figure 4.
Figure 4. Examples of kids in poor postures.
My niece is the child on the left, and my son is on the right. I do not feel qualified to make comments about anyone else's child, but I can tell you that my son and niece both have sensory issues that may or may not have resulted from positioning. My niece is three weeks old in this picture, and you can see she is in a position of flexion. Her hands are flexed, and her toes and feet are coiling up into flexion. Flexion is a natural position of babies, and we will talk more about that in a moment. Her spine is slumped with no neck control. Infants do not have neck musculature because they have never sat up. And when you put a baby in a sitting position before they are mature and for a prolonged period, you might get some issues because their head is heavy.
The second image shows him W-sitting. I will not say if this is good or bad because I do not like labels like that. However, I can tell you that my son and many kids in my many years of practice have core muscle weakness and poor distal coordination. When he is trying to focus on something at midline using bilateral integration, he needs a stable position. When a child is W-sitting, you need to look at the cause and the ramifications. Do they assume a W sit when working with their hands, eating, or when trying to organize themselves?
Research Review
- Postural stability and adjustments were associated with age and were influenced by sensory manipulation.
- The ability to perform anterior-posterior adjustments was more evident, and sensory maturation occurred in the visual system first, followed by proprioceptive, and finally, the vestibular system, reaching functional maturity at nine years of age.
(Sá, C., Boffino, C. C., Ramos, R. T., & Tanaka, C., 2018)
Postural stability is influenced by age and sensory manipulation. We need a sensory-rich environment to have learning and movement experiences. I think OTs know that, but I want to highlight how important this is. When you have a child with a sensory processing deficit, this will limit their experiences. It is up to us as OTs to broaden their exploration through play.
In 2018, the researchers looked at anterior-posterior movement. They found maturation in the visual system first, followed by proprioception, and then the vestibular system. All of these systems reach full maturity by nine years of age. Early intervention is vital, and this is supported in many studies.
- Physical activity increases the secretion of neurotransmitters and hormones that facilitate intellectual development.
- They enhance the generation of new neurons and multiply and strengthen the existing neural connections among the brain areas related to memory and learning.
- Emotional control, memory, and the capacity to adapt to different tasks and environments are essential for optimal psychological and physical development.
- Postural control is a system that uses and coordinates different strategies: biomechanical (especially in the lower limbs), movement (through unconscious postural adjustments), sensory (using somatosensory, visual, and vestibular information), and cognitive (through attention and learning from experiences).
- Girls perform better in tasks that challenge postural control and overcome them by executing smoother (i.e., less accelerated) and slower movements than boys.
- They have better postural control than boys.
- Similarly, active children have better postural control than sedentary children, although sedentary girls have better balance than active boys.
- Movement must promote the incorporation of activities that stimulate the activity of the somatosensory system through exercises conducted under monopodal stance conditions with deprivation of visual information and/or on unstable surfaces.
(García-Soidán, J. L., García-Liñeira, J., Leirós Rodríguez, R., & Soto-Rodríguez, A., 2020)
Physical activity increases the secretion of neurotransmitters and hormones that facilitate intellectual development, make us feel good, enhance the generation of new neurons, and multiply and strengthen those that are there. The more we move, the more we make connections.
Emotional control, memory, and the capacity to adapt to tasks are essential as that is how we learn. We also have to be somewhat flexible to have optimal development. Postural control uses and coordinates many strategies to help with postural adjustments, and we are not even aware of this. Postural adjustments utilize visuals, so the eyes are a huge part of it. Postural adjustments also use the vestibular system, and I will explain how in a moment. Even attention and cognition affect development. Thus, the research supports what we want to do.
The García-Soidán et al. study in 2020 looked at the difference between boys and girls and between kids with special needs and those typically developing. They found that girls perform better in tasks that challenge postural control and can overcome them easier even with less practice. So even if the girls were sedentary for a bit, they had better balance than active boys.
A movement must promote the incorporation of activities that stimulate the somatosensory system in exercises in a monopodal stance or standing on one leg and by the deprivation of visual information. Knowing this, what about kids that are blind?
- While sensory organs develop in utero (e.g., the mature neonate is born with a fully functional vestibular organ), higher-order sensory processing has yet to mature in the full-term neonate.
- Input from visual and somatosensory modalities contribute to the development of egocentric and allocentric reference frames, respectively.
- This allows distinguishing movement in the environment from self-movement.
- Compromised multisensory integration (MSI) is seen in
- delayed motor development
- moderately severe to severe cerebral palsy
- intellectual disability
- autism spectrum disorders
- ADHD
- sensory organ dysfunction/sensory processing disorders
- language development
- learning disabilities (e.g., dyslexia)
(Tele-Heri, B., Dobos, K., Harsanyi, S., Palinkas, J., Fenyosi, F., Gesztelyi, R., More, C.E., & Zsuga, J., 2021
Kids use systems other than vision when you blindfold them and put them on something unstable. It is a beautiful, smooth, natural compensation that we can facilitate through our interventions. While sensory organs develop in utero, the neonate is born with a fully functional vestibular organ. This is so cool to me as they float in liquid in utero. The actual effects of gravity do not come about until they are born. And this input is significant as it distinguishes movement in the environment from self-movement. When infants are born, they are egocentric as they have limited vision and color input from their surroundings. Through rehearsal, the infant realizes that they are separate from their environment.
Compromised integration can cause all these things noted in the list above. We treat many of these things in the clinic, and research supports what we are seeing. For example, children with learning disabilities and ADHD often have compromised multisensory integration. Thus, when you get a referral for handwriting, a learning disability, or dysgraphia, you need to also look at the child's posture, core muscles, and the integration of the sensory system as part of a thorough evaluation. Handwriting is not our true priority, but it is a gateway and opens the window to development. We can then get our hands on the child and see what affects their handwriting.
- 95% of OTs across settings use SI approaches (Schaff et al., 2018)
- Andelin, L., Reynolds, S., & Schoen, S. (2021) study supported ASI 3x per week to improve motor skills and achieve goals.
- ASI can be effective in SBMDs.
- *ASI = Ayres approach focuses on tactile, vestibular, and prop systems.
OTs use sensory integration approaches, specifically the Ayres approach. I am not going into this today, but Lucy Jane Miller and other approaches are sensory processing techniques different from the original Ayres sensory integration model. We need to be aware of our approaches and look at the data and research as we know that sensory processing disorder is not an official diagnosis yet. It did not make it into the Diagnostic and Statistical Manual (DSM) 5 right now, but they continue to push for it.
Vestibular System
- UNIQUE as it is the only sensory system to utilize multiple receptors in many systems.
- Inner ear
- Visual input
- Proprioceptive receptors
Let's look at the vestibular system in particular as it is unique and the only one that uses receptors from different systems. Taste originates in the mouth, hearing is mainly in the ear and the brain, and tactile receptors are under the skin and muscles. The vestibular system involves the inner ear, vision, and includes proprioception, thus differentiating it from solely proprioception.
Ear Anatomy
The ear anatomy is in Figure 5.
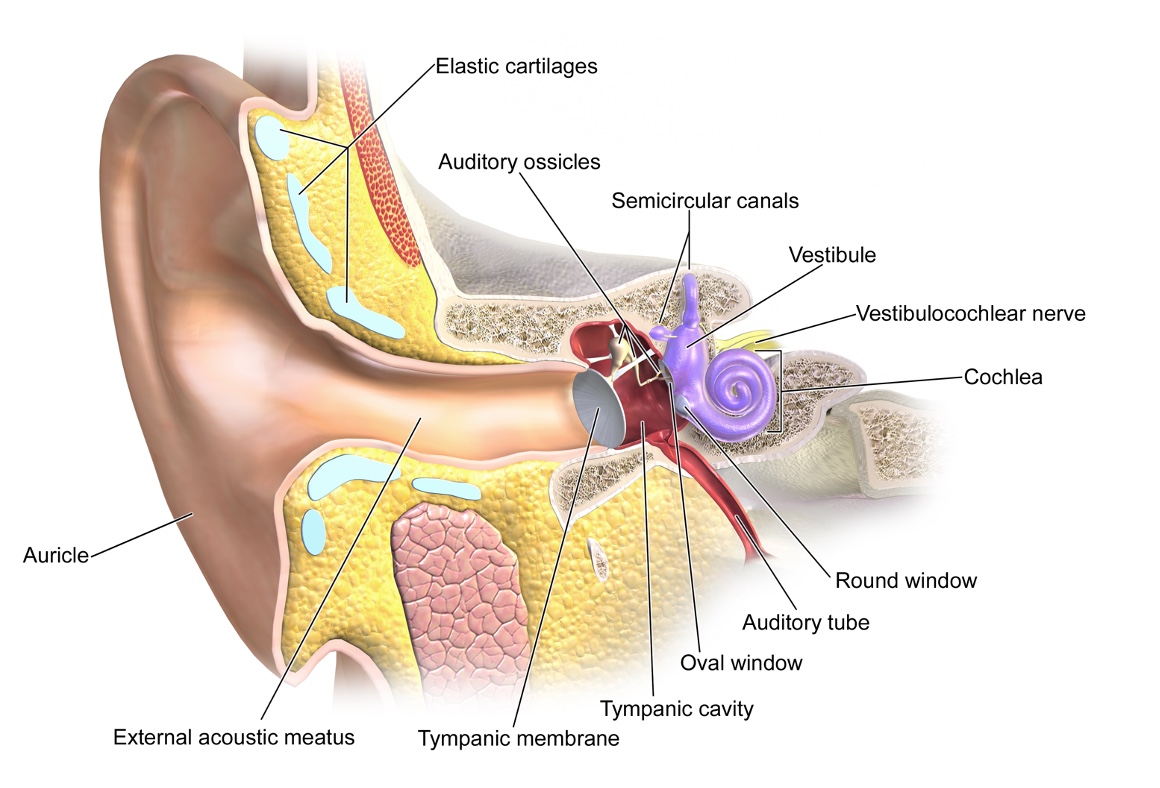
Figure 5. Inner ear anatomy.
I do not want to get too much into the ear anatomy today. The auricle of the ear is on the outside and is a receptacle. As I was preparing these slides, my son pointed that out to me: "It looks like my funnel." I thought that was a terrific way to describe it. The inner ear is shown in purple.
Five Receptors in Each Ear
- Three semicircular canals (horizontal, anterior, and posterior) that transduce rotational angular acceleration
- Two otolith receptors (utricle and saccule) that transduce linear accelerations
The three semicircular canals are in different directions, which is critical to know.
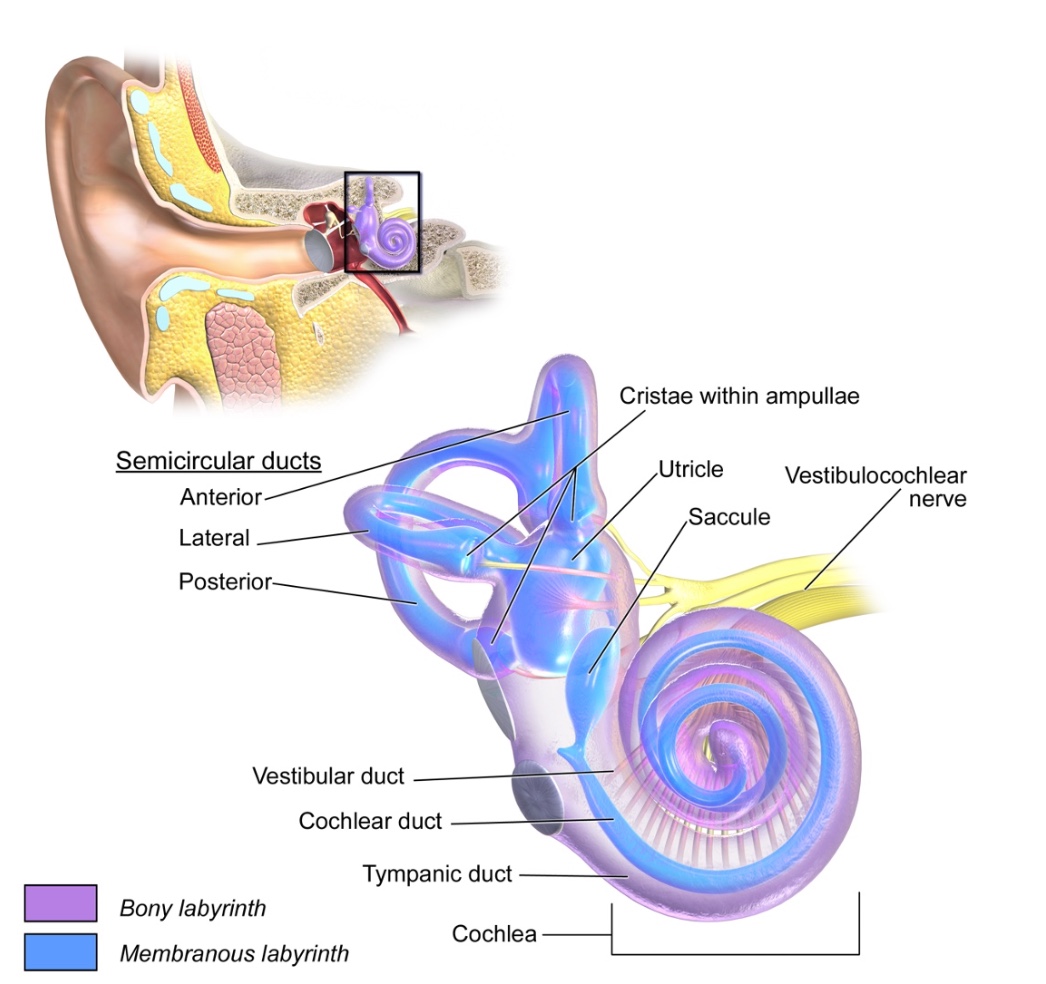
Figure 6. Receptors in the inner ear.
The semicircular canals are positioned vertically (anterior and posterior) and horizontally (lateral). There are cilia or hairs in these fluid-filled canals, and depending on the way you move, this gives the body information on your position. Close your eyes and move your head from side to side. The fluid moves in the canals, stimulates the cilia, and sends signals to the brain. Forward and backward positional movement and speed come from otolith receptors called the utricle and saccule. They are swellings in the inner ear that transduce linear acceleration. Oto means rock in Latin, and these receptors if we are going forward or backward.
When you have an ear infection, it affects the entire body. We have to be mindful of this when we are working with kids. I have had allergies and sinus issues my whole life. In fact, before this course, I got very dizzy and had to hold on when I moved diagonally. This dizziness also affected my stomach because I got nauseous and disoriented. Many of our kids may be living like this a lot of the time. Often, behavior is communication, and they may be trying to tell us something.
Vestibular Reach
Let's look at the visual in Figure 7.
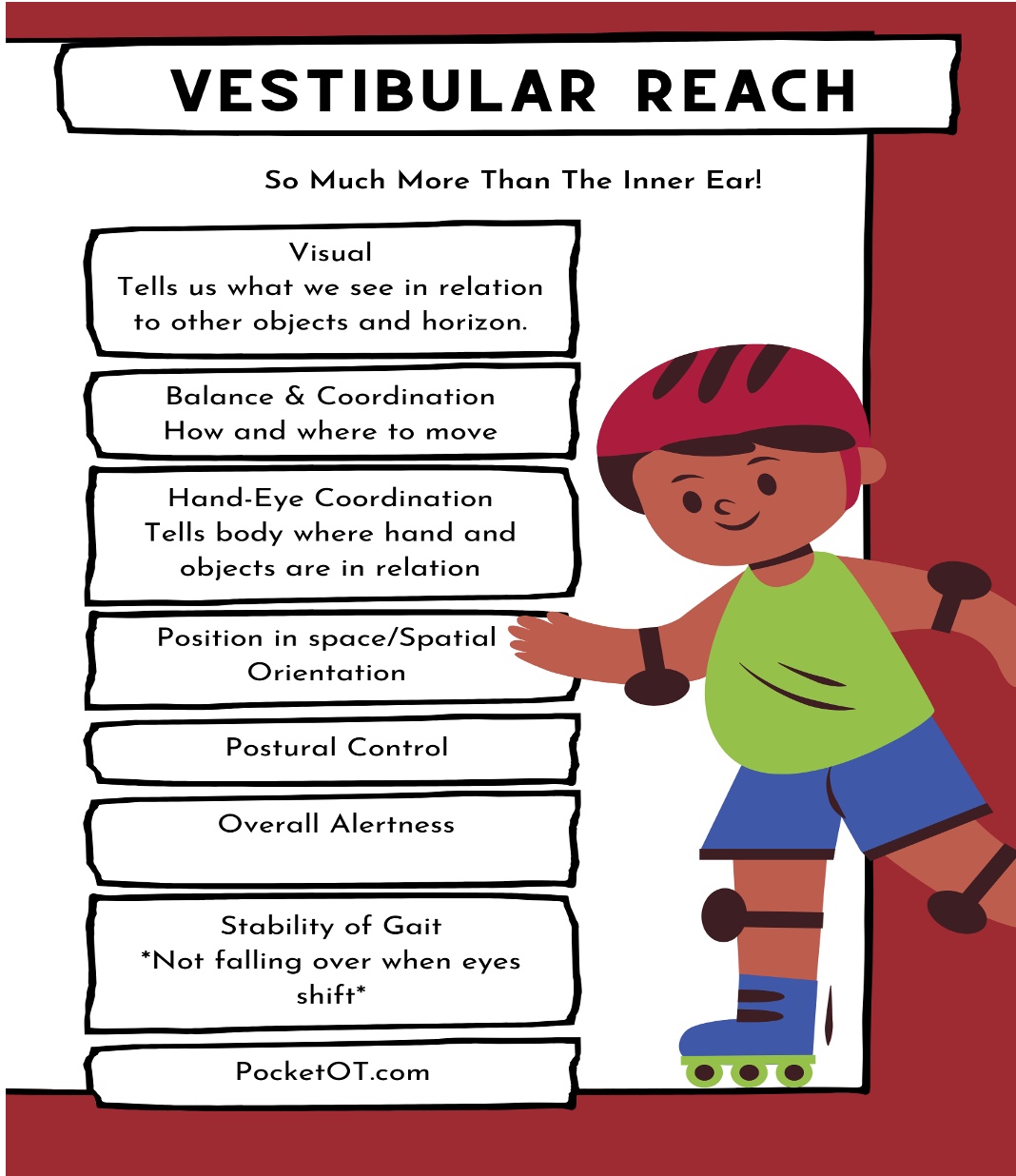
Figure 7. Areas affected by the vestibular system.
The vestibular system lets us know where the horizon is as we move. It allows us to understand where and how to move from one location to another for balance and coordination. The vestibular system impacts hand-eye coordination and movement with the body and other objects. An example of this is a tennis ball or a baseball coming at you and moving quickly to avoid it. The vestibular system controls the position in space, spatial orientation, postural control, and overall alertness of the body. It also stabilizes gait and prevents us from falling over when our eyes shift.
Vestibular Movement in All Planes
- RED: Sagittal Plane
- BLUE: Frontal Plane
- GREEN: Transverse Plane
Remember our ear anatomy and the different movement as seen in Figure 8.
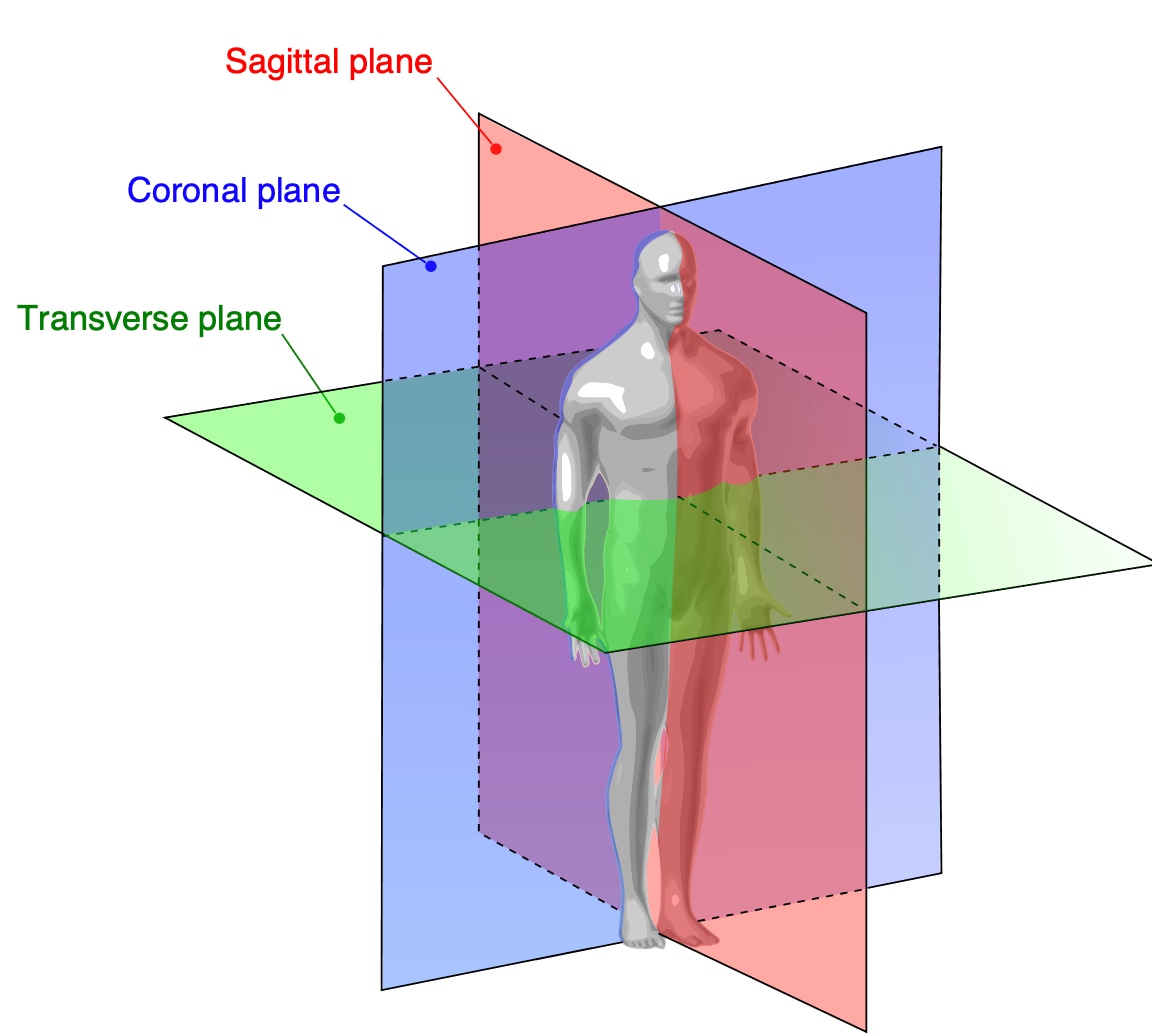
Figure 8. Different planes of movement.
The first plane is the sagittal plane, and this is anterior-posterior movement. Rock back and forth in your seat, the sagittal plane. The coronal plane is side to side movement. Keep your head looking straight ahead and move side to side. Linear motion is generally calming, either forward and backward or side to side. An example of a transverse plane movement is a rotation of the head and neck, a very mature movement. Due to ball and socket joints and spinal flexibility, rotation is available at the neck, shoulders, trunk, and hips. Many kids walk like a stick as they lack rotation in a transverse plane. What does that have to do with the brain? Let's look at the pyramid of learning from Williams and Shellenberger.
Pyramid of Learning
- Higher Abstract Concrete Thought Affiliation
- Attachment
- Sexual Behavior Emotional Reactivity Motor Regulation Arousal
- Appetite/Satiety Sleep
- Blood Pressure
- Heart Rate
We can think of our body as a pyramid, as noted in Figure 9.
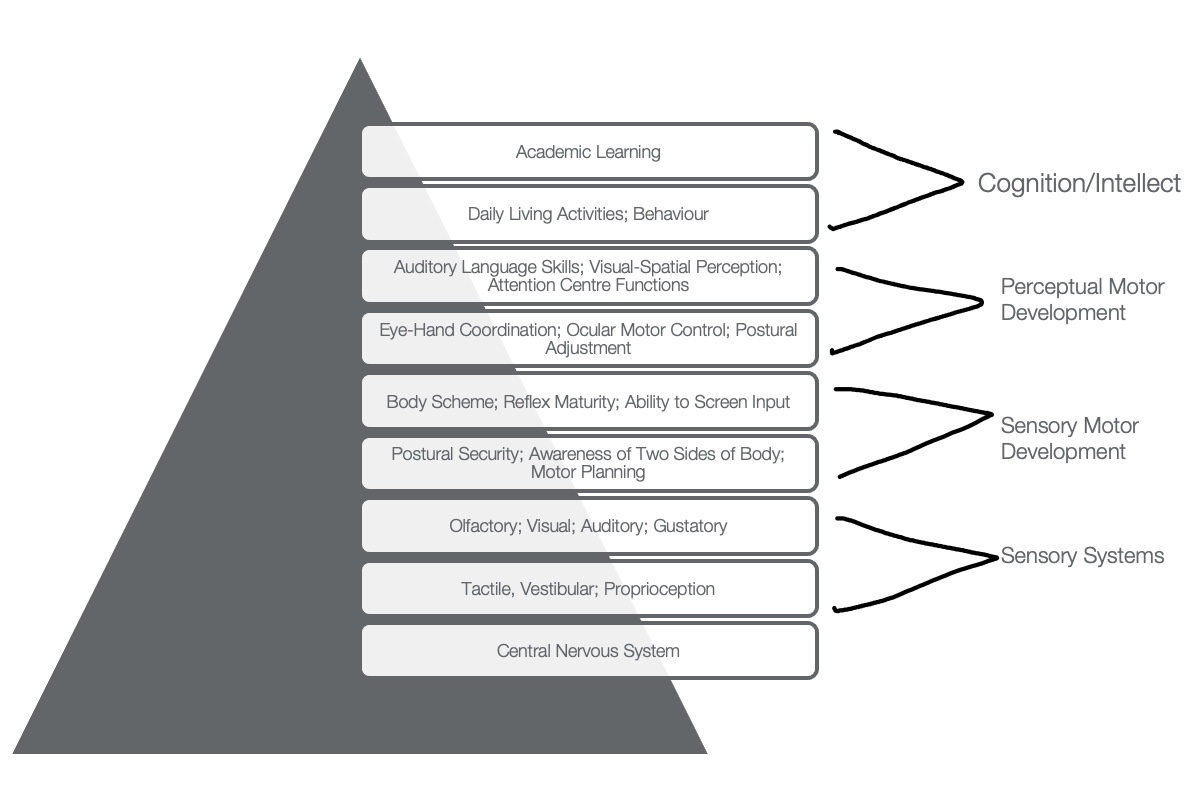
Figure 9. Pyramid of Learning (Modified from Williams & Shellenberger, 1996). Click here to enlarge the image.
The central nervous system is at the pyramid's base, including heart rate, blood pressure, sleep, appetite, and arousal. We do not think about or have much influence over these systems. Interoception and the homeostasis of our body are part of the foundation. Next, a sensory layer includes tactile, vestibular, and proprioceptive senses. The sensory and motor components make up the middle of the pyramid, and sensory integration is significant for our body scheme. At the top of the pyramid is academic learning. All of these areas build upon each other to access higher-level cognition. Dr. Daniel Siegel calls this the upstairs brain or the higher brain. If there is a gap somewhere in the pyramid, you can scaffold it, but you need to know the different layers and how they build upon each other.
How Do We Achieve Modulation?
- Modulation and regulation are in the brain stem and mid-brain.
- Begin with existence, then move from chemical reactions to behavioral states.
- When a task demand is too much, and the body cannot handle it, the child melts down, and they ‘fall apart’ because they are simply existing/surviving!
Modulation and regulation happen in the brain stem and mid-brain. The brain stem is only eight centimeters long, yet our survival depends on it. When we are infants, we do not have higher-level cognitive memories, which is good because we have a lot to undergo a lot of trauma going through the birth canal or a C section. We are also egocentric and focused on getting basic needs met, and then we move from that to behavioral states, which I will go over in a little bit.
When stress is too much for an infant or us, we naturally melt down. When you see a child falling apart, it may be due to a lack of skills. The brain stem functions to protect us, and when we have a total shutdown, a meltdown is all we can handle. It can be a "straw that broke the camel's back" moment that you may see coming or not. When you are stressed out, you cannot access higher-level thinking.
Gaze Stability- Vestibule-Ocular Reflex
- Coordinates eye and head movements
- Experiment: Look at a point across the room and move your head from side to side.
- No matter how the head moves, the eyes naturally focus on the point to ensure balance/stability!
The vestibular ocular reflex coordinates eye and head movements. I want you to look at a point across the room and move your head from side to side while keeping your focus on that point. No matter how your head moves, your eyes do not follow due to a reflex for focused stability designed to keep us steady on the horizon. If you are walking toward your friends and are focused on them, you do not get dizzy as you are moving.
Gait Stability
- Maintaining an upright stance on one or two feet requires constant communication between the sensory signals from the feet, legs, and spine to the brain.
Gait stability maintains an upright stance on one or two feet requiring communication between the feet, legs, and spine to the brain. A child with one-sided weakness from a stroke needs to work on weight-bearing. Points of control in NDT are in transverse movement in the head, neck, shoulders, hips, and pelvis. Weightbearing is critical because it gives us information about where our body is in space and helps coordinate that information.
Sensory Processing Disorder (SPD) Chart
Our sensory chart is shown in Figure 10.
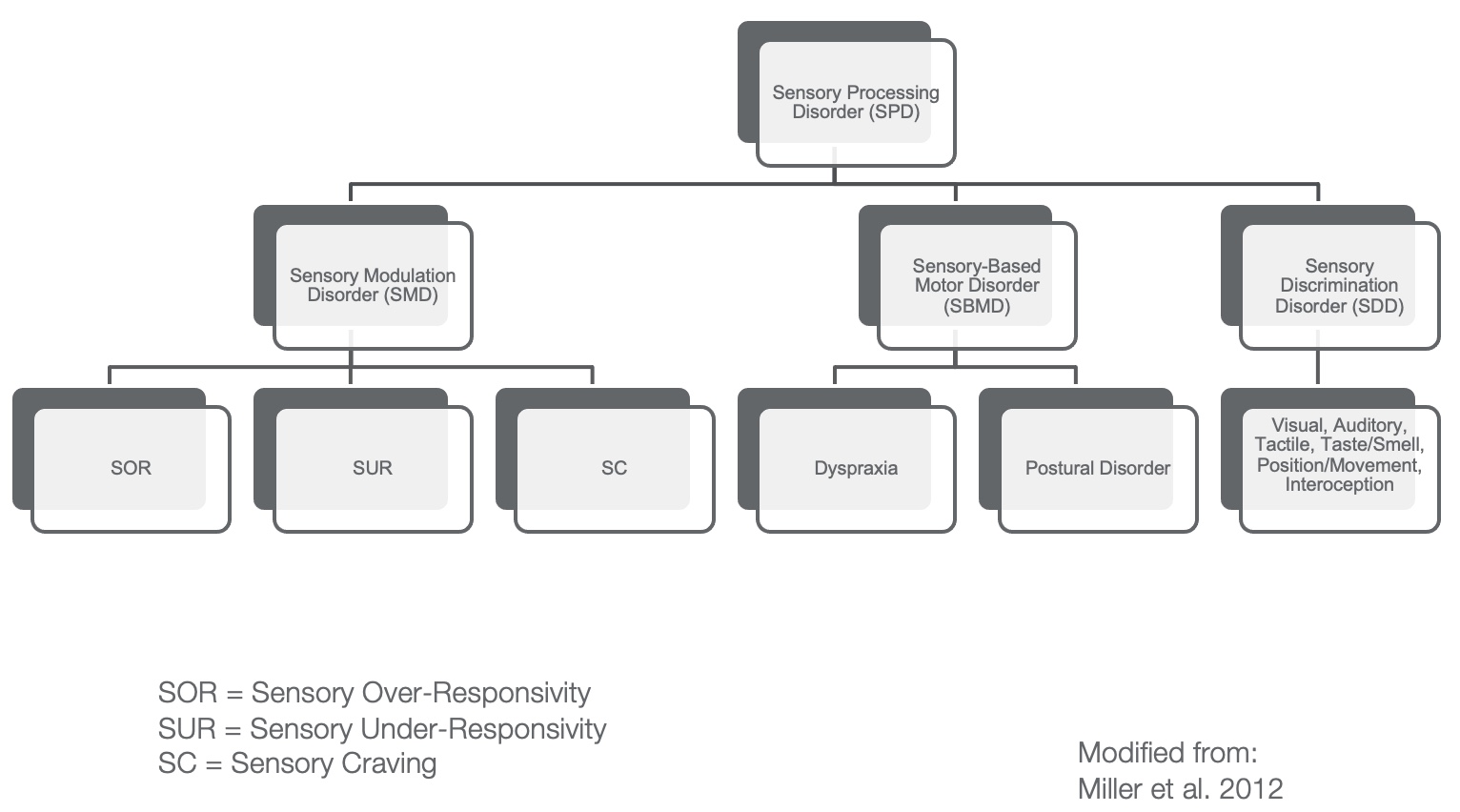
Figure 10. Sensory chart from Lucy Jane Miller and team. Click here to enlarge the image.
This is a nosology chart modified from Lucy Jane Miller and her team's work in 2012.
Sensory Modulation Disorder
- Sensory MODULATION disorder
- Problem regulating the response to input
- Results in withdrawal of/negative responses
- Signs:
- Upset by noises and sounds
- Easily distracted by visual stimuli
- Difficulty falling/staying asleep
- Hypersensitivity to clothing
Sensory modulation disorder comprises sensory over responders (SOR), sensory under responders (SUR), and sensory cravers. Sensory over-responsitivity examples are individuals who do not tolerate noises, tags in clothing, or other stimuli. Sensory under-responsivity is the opposite. An example of this is when I was giving a talk, and this lady told me her son was bitten by about 50 fire ants in Texas, was bleeding, and his throat was closing, and he continued to play as if nothing had happened. I live in Florida and have been bitten by fire ants, and it hurts. You may also see kids with bruises (besides trauma and abuse) and have no idea how they got them. Then we have our cravers. These individuals like to seek input and often crash into things. These are the modulation disorders that are not regulating responses to input. The result is a withdrawal of or a negative response to something in their environment.
Dyspraxia
- Problem in planning, sequencing, executing unfamiliar actions
- Signs:
- Awkward/poorly coordinated motor skills
- Difficulty w/ADLs
- Prefers routine
- Awkward pencil grasp and patterns
- Does not prefer sports
Next are sensory-based motor disorders. Dyspraxia is a problem in planning, sequencing, and executing unfamiliar actions. Many kids have awkward body movements and can also have dyspraxia in speech. As they are so uncoordinated, they prefer routine. You may see this in a child with an awkward pencil grasp. They grip the pencil so hard as they have trouble forming a new motor plan. This may manifest itself in ADLs, and many do not like sports as a result.
Postural-Ocular Disorder
- Problem w/control of posture or control of movements seen in muscle tone or joint instability and/or poor functional vision
- Seen in vestibular and prop. problems
- Signs:
- Flat feet
- Slumps while sitting
- Weaker than other children
- Fatigues easily
- Problems with eye-tracking
The postural-ocular disorder is a problem with posture or control of movements, muscle tone, joint instability, and or poor functional vision. We are also looking at functional vision. Often, these kids have flat feet, might slump while sitting, are weaker than other children, fatigue quickly, and have problems with tracking. You can say, "Follow my finger and track it."
Sensory Discrimination Disorder
- A problem in recognizing/interpreting differences or similarities in qualities of stimuli
- Signs:
- Uses too much force
- Crashes/bumps into objects
- Drops or knocks things over
- Afraid of heights
- Poor balance
In a sensory discrimination disorder, children cannot interpret the differences in stimuli.
Sensory State and Available Emotions
Emotional regulation is the ability to have an emotional state that matches the task or setting. Our moods are affected by what our body state is. I have made a chart (Figure 11) that pulls this all together.
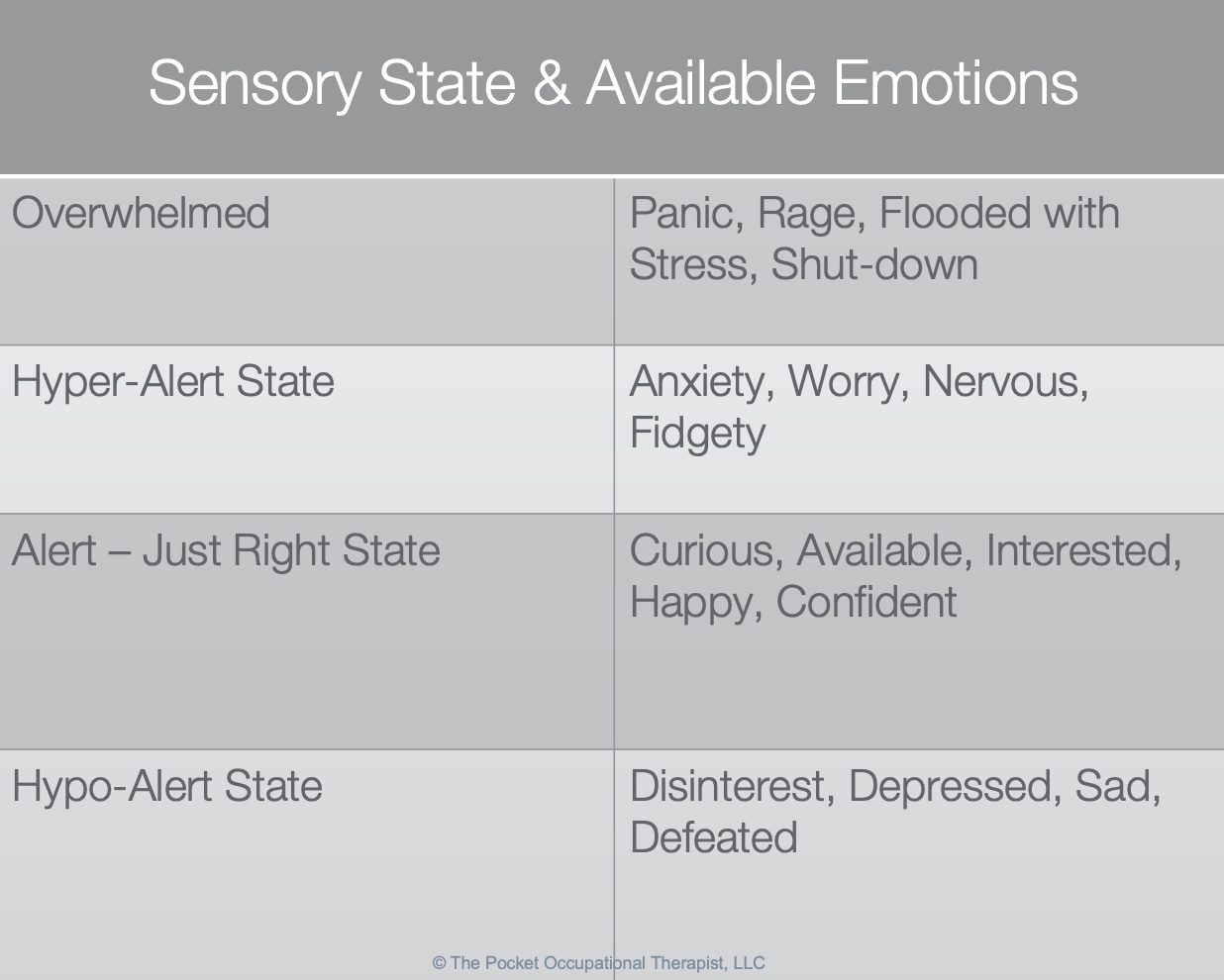
Figure 11. Sensory state and available emotions.
Being overwhelmed can result in panic, rage, being flooded with stress, and shutting down. A hyper-alert state can result in anxiety, worry, nervousness, and being fidgety. They are always looking for the next threat in their environment. I have a hyper-alert son and another with a postural ocular disorder. Alert is being in the just-right state. They are curious, available, interested, happy, and confident. This is the top of the pyramid for learning. Lastly, a hypo-alert state or low arousal may cause the child to be disinterested, depressed, sad, and defeated.
How Do We Regulate?
- Sympathetic NS
- Sympathetic nervous system is the ‘accelerator’ to the body
- **Fight, Flee, or Flight**
- Cortisol-driven
- Located in the thoracic cord
- Sexual climax
- Parasympathetic NS
- The parasympathetic nervous system is the ‘decelerator’ to the body
- **Rest, Recover, and Digest**
- Located in the sacral cord
- Controls bladder and colon
- Sexual arousal
The sympathetic nervous system is our accelerator and is cortisol-driven. Cortisol is located in the thoracic cord, and which is interesting to know that the spinal cord has some influence here. When we accelerate fight, flight, or flee, there is something called feigned death where it gets so bad that you shut down. People in a traumatic situation may say, "I looked down at myself and do not remember moving."
The parasympathetic is "rest and digest." For this course, I want you to think of it as the decelerator. It lets us rest and recover. This system is located in the sacral cord as it also controls our bladder and colon. By the way, sexual climax is part of the sympathetic nervous system and in the thoracic cord, and sexual arousal is a parasympathetic response.
Three Levels of Brain Function
- 1)Arousal for basic survival and action. Posture in flexion and extension. A sense of self-focus is on needs and self.
- 2)Alertness motivation, emotion for movement, and action on the object.
- a)Postural is lateral flexion and weight shift. Task-based play, imagination, motivation/emotion, attend to the environment – naturally occurs around pre-school.
- 3)Awareness for challenges, skills, and actions to and in response to objects in surroundings.
- a)Postural skills are trunk rotation, rhythm, and timing. A mature perspective can complete entire routines with:
- b)HOW, WHY, WHEN – naturally occurs at school-aged +
The three levels of brain function are arousal, alertness, and awareness. Arousal is the level where we are born. Posture is in flexion-extension physiologically, and we can only really focus on our needs and ourselves.
We are ready to go at the alertness level and can access postural and lateral flexion and shift our weight from side to side. This happens at the preschool level with increased attention to the environment and task-based and imaginative play. As the posture develops, brain connections do as well.
Awareness of challenges is the last level. The highest level is when we are aware, ready for a challenge, and learning something new. We see trunk rotation, rhythm, and timing.
Let's go back for a moment and think about a child with stiff body movement. Can they go into a lateral weight shift stance? Perhaps they can assume a lateral stance and move side to side, but is there an actual rotation at the trunk? We need to assess these different levels.
Early Brain Function
- Born with a CHAOTIC brain
- Through a process known as synaptic pruning, neurons that are not useful to the brain die off.
- Connections are building into an organized state by 2-3 years of age.
- The concept of neuroplasticity explores how the brain changes in the course of a lifetime and how different areas of the brain can evolve and adapt over time.
We are born with a chaotic brain. For example, an eight-month-old may have 1000 trillion synapses, but they are disorganized and do not connect to anything, visually like a bowl of spaghetti. By two years old, the brain creates 2 million synapses per second, and the brain is becoming organized.
"The brain that fires together, wires together" is a quote I believe by Dan Siegel. We also know that neuroplasticity occurs over a lifetime.
Physiological Flexion
- Tonic Labyrinthine Reflex
- Present at birth (comes at 12 weeks in utero) and is progressively integrated between the 3rd and 4th year.
- Head flexes, (below level of spine) whole body flexes
- Head extends (below level of spine) whole body incl. arms, legs, and torso extend
Babies are in physiological flexion, where the head flexes and curls up like a spring, as noted in Figure 12.
Figure 12. Baby in physiological flexion.
If you move the baby into extension, they pop back into flexion. You saw my niece sitting in a flexed posture which is not fully integrated until the third or fourth year of life.
Maladaptive Postures
- Decreased or reversed spinal curvature
- Extension
- Developmental Interference:
- Attachment, flexion, sitting, crawling, leg ext., rotation, dissociated movement, flexor, and ext. imbalance
- Physiologic Interference:
- Breathing, eating, position of diaphragm, tight upper trunk musculature,
- Oral motor structure in poor alignment
Flexion is the springboard for movement in an infant unless there are maladaptive postures. For example, premature infants not in that physiological flexed position may have impacted breathing, eating, and movement into the midline. Go into body extension and think about trying to feed from a bottle or swallow from this position. It is tough. While extension is critical to later movement, it does not serve a baby well. We have to get the babies back to flexion and work from there.
Figure 13 shows the fencing reflex, or asymmetric tonic neck reflex (ATNR), typically integrated by 6-7 months of age.

Figure 13. Example of an ATNR.
Change Over Time
- As we age, we change and become more SYMPATHETIC (not in personality but in our NS)
- Consider:
- Increased heart rate
- Increased blood pressure
- When children grow, they are parasympathetic as kids and need more rest in order to recover and develop.
Over time, our body becomes more sympathetic in the nervous system with increased heart rate and blood pressure. Infants are more parasympathetic because they make brain connections and recover and rest.
Brain Chemicals
- Oxytocin
- Serotonin
- Cortisol (stress hormone)
- Acetylcholine
Essential brain chemicals are oxytocin, serotonin, cortisol, and acetylcholine. Oxytocin and serotonin are the "feel good" chemicals, and cortisol and acetylcholine or ACH are stress hormones. In the parasympathetic system, more calming hormones are released, but when a person gets dysregulated, you start to see the release of stress hormones.
Levels of Brain Function
- The brain will do what it takes to SURVIVE, so it uses compensatory strategies.
- When a child has a stressed system, he is ‘dysregulated.’
- The dysregulated child cannot focus on higher-level brain functions because they are CONSTANTLY looking for potential threats in the environment.
The brain does what it takes to survive. When kids are stressed, they become dysregulated and cannot focus as they are looking for threats. This would be similar to being in an earthquake-prone zone and always on alert. This constant level of alertness would wear you out. This is why our kids have meltdowns at the end of the school day as they are trying to survive. They are not regulated or balanced, and their nervous system's sympathetic and parasympathetic parts are not working in harmony. They are consistently high, always low, or go up and down too much. The interplay of the hormones is what keeps us regulated, alive, and stable. We cannot always look for threats and cannot always sleep.
What is Self-Regulation?
- Constant balancing of the sympathetic and parasympathetic nervous systems keeps us in a state of ability to interact with our environment- this is REGULATION.
- Interplay between the two so our conscious matches what we are doing.
- How does STRESS affect us?
Signs of STRESS in Children - Amygdala = FEAR
- Acting out/behavior
- Stomach and headaches
- Sleeping issues
- Anger or aggression toward others
- Dilated pupils
- Sweating
- Flushing of cheeks
- Wide “deer in headlights” eyes
When kids are in a fear state, they may act out or have stomachaches or headaches. They may also have sleeping issues, anger, dilated pupils, sweating, flushed cheeks, and a "deer in headlights" look.
Signs of a Dysregulated Child During Occupation
- Easily frustrated
- Worry and stresses easily
- Impulsive, irrational, aggressive
- Hyperaware of environment
- Poor fine motor skills
- Poor handwriting
- Insists on routine
- Difficulty with organization
- Panic attacks
- Difficulty sleeping
- Difficulty toileting
- Poor attention and focus
- Distracted by or bothered by smell, sound, sights, and sensory information
- Unexpected touch causes anxiety
As an OT, you may wonder how to know when a kid is struggling. Look at them, take data, and complete an occupational therapy profile questionnaire. You can also look at their occupational performance as this might tell you something about where they are in their sensory and regulation state.
The Structures Involved in the Relay of Information
- Perception Is Communication & Interpretation
- Pons relays messages from the cortex and the cerebellum.
- Without the pons, the brain would not be able to function because messages would not be able to be transmitted or passed along.
- Need an interpreter for the sensory information going to the cortex.
Perception is about communication and interpretation. Remember, I said earlier that it is perceived stress based on your life experiences, genetics, and how and where you were raised. The pons relays the message between the cortex and the cerebellum. Without the pons, the brain could not function cause it could not transmit messages.
- Thalamus is responsible for relaying information from the sensory receptors to proper areas of the brain where it can be processed. If this part of the brain is damaged, sensory information would not be communicated.
The thalamus is the interpreter and is responsible for getting this to processing.
Brain damage can cause some dis-communication.
- Perception is ALL About Interpretation!
- Stimulus can be
- Perceived (phantom limb)
- Or considered a Sensation
- Some sensations cause perceptions, and others are NOT perceived but evoke responses in the body such as blood pressure, blood gas...
- Stimulus can be
Perception is all about interpretation. If someone has phantom limb pain, we cannot understand that because we have not had a limb removed. Phantom limb pain is a perceived sensation stimulus, but it is a miscommunication somewhere. Perhaps, the brain is so used to that leg being attached that it is still trying to send information there as the brain is being protective.
- Challenge: is HOW WE INTERPRET the information
- Why we have visual tricks/puzzles
- Why shots are more traumatic to some people
- Why do we THINK we move at a red light when someone next to us moves
- Weber’s Law demonstration ****What’s important to one may not be registered by another.****
Our body has to interpret information like blood gas, blood pressure, and all the interceptive pieces related to our sensory systems. Have you ever been at a red light and it appears that the car is moving next to you? Your body is not moving, but your eyes see movement. This is an incongruency in our visual system.
Weber's Law is what is important to one may not be registered by another. For example, a person may feel the weight difference of 2 ounces when someone else may not.
Presentation Questions
- How does the maturation of our sensory and motor systems improve school performance?
- How can you provide movement experiences to improve attention?
- What factors in society are detrimental to building a strong foundation in both movement and sensory experiences?
Here are some questions to review. I challenge you to answer these questions throughout your review or this presentation. For example, we examined how technology is a significant influencer on our systems and can be detrimental to building movement opportunities. Do the research, and you will see.
Proprioception and Tactile
- Tactile information
- Received through the skin. There are at least six types of receptors. Notice disruption in their cell membranes or chemical changes.
- Proprioception
- Monitors position of joints, tendons of joints and ligaments, and the state of muscular contraction.
- Tendon organs which measure the strain on a tendon, and muscle spindles which monitor the length of the skeletal muscle (Innvista.com).
- Therapeutic input lasts 2-4 hours.
Tactile information is received through the skin, and there are at least six types of receptors that notice a disruption in their cell membrane or through a chemical change. Our body talks via chemical changes in the skin.
Proprioception is the position of joints, tendons, and ligaments and tells us information about the state of muscle contraction. Tendon organs, which measure the strain on a tendon and the muscle spindle, give us proprioceptive input. The website innvista.com has some excellent illustrations on there. Therapeutic input to the proprioceptive system lasts two to four hours. Let's say you are doing some weight-bearing or similar activities. This input will last two to four hours at a time.
Signs of Immature/Retained Postural Reflexes
- Poor body alignment
- Difficulties with reading & writing
- Gravitational insecurity
- Anxiety disorders
- Weak head control
- Bilateral coordination deficits
- Vision & gaze disorders
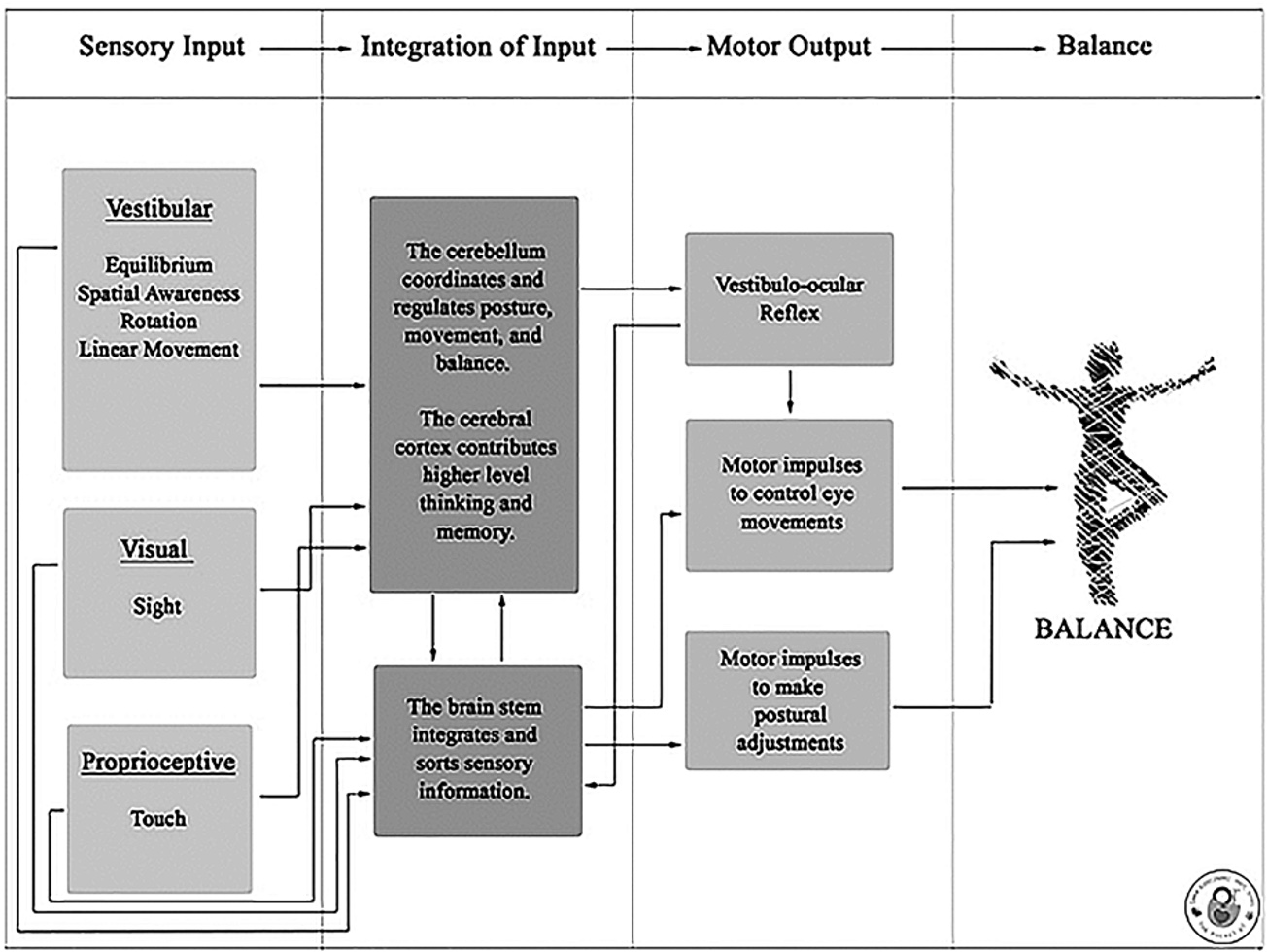
These are signs of immature retain reflexes. The illustration in Figure 14 is from my Sensory Interventions book showing sensory input, integration, and then motor output.
Figure 14. Sensory inputs, integration, and sensory output chart. Click here to enlarge the image.
The cerebellum coordinates and regulates posture, the cerebral cortex contributes to high-level thinking and memory, and the brain stem integrates and sorts all of the sensory information.
Get to the Core/Core Stability
- Core muscles: help in developing mid-line
- Respiratory activation helps with the Valsalva maneuver.
- Gravity and movement cause a baby to gain activation of the core muscles and refine them as they grow and develop.
The core is essential, and it is the first thing that we want to work on with babies. We help them to work on sitting and moving to the midline. We can also work with kids on deep breathing exercises to activate the respiratory system to help calm them and create stronger contractions for bowel movements via the Valsalva maneuver. Movement against gravity also allows the core to develop.
- Practice and development of many body systems (including sensory, reflex integration, motor, and cognitive)
- Alignment changes w/gravity and movement to support activation of the inner core team in the first 2-3 years of life and refined into adolescence.
- Vision is important for hand-eye coordination, tracking/scanning for danger, etc.
Practice and development help refine the core for the first two to three years, and it continues to be refined into adolescence. So if you see issues with an older child in prone, supine, or standing on one foot, you can still work on those muscles. You can use obstacle courses and weight-bearing and heavy work activities. Another fun activity is having them sit on the ball for some postural movements while throwing a ball at specific targets or letters. This incorporates hand-eye coordination also to impact the core.
Levels of Brain Function
- When primitive reflexes are retained, there’s a ‘tug of war’ between the brainstem and the higher levels of the brain.
- The cortex then must use too much energy for basic function and cannot do its own job: learning, thinking, and attention to task.
A "tug of war" occurs in the brain when there is a retained reflex. Ensure that you are working through that and looking at the child's energy level in your assessment. How tired is the child? How does the child look at the end of the day? Occupation performance reflects some of these physical manifestations.
Vision is Important
- Our brain allocates a great deal of ‘real estate’ toward vision.
- Critical in ongoing postural reflexes that maintain upright position.
- Hand-eye coordination
- Dr. Roberto Kaplan
Vision is so critical that our brain allocates a ton of real estate toward our visual systems. Vision is vital for postural reflexes and maintaining an upright position. When you are sitting on a ball, and someone pushes you, you can pop up into an upright position. Vision helps keep postural reflexes so they can be smoothly processed. You can test this on your clients, but I would not start on a ball as this is high level. You can push them in different directions with their eyes open and closed. You want to see how effective they are at regaining their upright posture. If they are proficient at that, you can start working on twisting and bilateral integration. Dr. Roberto Kaplan, a vision therapist, has some excellent exercises.
Why Vision?
- “The brain is like a system of roads. Information travels from one location to another.
- If the roads are direct and smooth, the travel is easy. If construction creates a barrier, the highway is blocked, and traffic is redirected into clogged side streets.
- Children with severe visual dysfunction spend too much time on these side streets, and the simple act of perceiving the world becomes a nightmare.”
- Children with behavioral problems typically have multiple sensory issues, and visual dysfunction is one of them. 80% of the information we receive from our environment is visual!”
We know that our brain is a system of connections. The brain homunculus, or a map along the cerebral cortex where each part of the body is processed, shows how much of your brain is allocated to the sensory and perceptual areas. The visual area and the face have a lot of sensory distribution, so they are important for brain processing.
Dr. Marie Fox, a vision therapist, says that children with behavioral issues typically have multiple sensory issues, including visual dysfunction. She found that up to 80% of information from our environment is visual in her research. You could see then why a child that is not processing visual information appropriately could have severe issues.
Spatial Orientation
- The vestibular system helps you perceive which direction your body is moving, if you are tilting side to side, or moving at all!
- These perceptions contribute to your sense of equilibrium (state of physical balance).
- Keeps you safe from falling
The vestibular system helps you perceive which direction your body is moving, called spatial orientation. In our documentation, we may say, "Decreased spatial orientation as evidenced by the fact that the child is not aware that he or she was moving." A child's emotional state is also affected by spatial orientation. Remember, the brain craves safety and strives for equilibrium, and the amount of emotions that we have is directly congruent with our sensory and physiological state. You may have a child that comes into your clinic that is falling a lot and has gravitational insecurity. We need to look at their planes of movement and see how that impacts their emotional state.
When documenting, I also encourage you to print the Occupational Therapy Practice Framework from the AOTA, as it gives you terminology to guide your documentation. Standardized assessments are critical to show progress, but your clinical observations are also essential.
Postural Control
- Affected by self-regulation
- Multiple system involvement:
- Primitive Reflexes
- Muscles
- Sensory system information and integration
- Previous experiences
- Nervous system
Ready Bodies, Learning minds is a book and program that I love for postural control. I also love Move Play Thrive from Sonya Storey, which looks at reflex integration and rhythmic movement. Our previous experiences are also vital. Suppose a child has a disability or a movement problem like being restricted to a wheelchair. In that case, we need to get the child into other situations without gravity to help them move their body to help integrate their sensory system. Aquatherapy is a great activity to get a child moving against gravity and to bring in connections.
- Subconscious maintenance of posture
- Requirement throughout life to live against gravitational pull
- RIGHTING:
- Birth throughout life
- Help when there’s a loss of balance
- Head control through standing
- EQUILIBRIUM:
- Six mo. throughout life
- Event-specific and unique to each situation!
- Cortex with cerebellum to fine tune
- Base of support
Postural reflexes and righting reactions that begin at birth help keep us upright and prevent a loss of balance. Equilibrium starts at six months and continues throughout life. Six months is when kids begin to bear weight and work on their core.
Core Stability
- Compensation Strategies
- Motor Patterns
- MOVE IN A TRANSVERSE PLANE
- Breathing
- Rib cage, spine, pelvis alignment
- More compensation as time goes on...not good for balance, gross motor, fine motor, and oral-motor skills.
Transverse plane movement is the big takeaway. Remember what I said about brain states. Children will not be able to access higher-level learning if there is an incongruency between their state of movement and their brain. Deep breathing helps with alignment and increases movement in the ribcage and pelvis.
Core and Emotion
- Breath
- Posture
- Emotion
- Use of extremities
- Emotional arousal
We also need to remember that the core of our body helps with breathing, and deep breathing expands the ribcage. Posture and working in midline help build core strength and balance. We can then add in the extremities. By doing this, emotions can start to be more regulated.
Oculomotor
- Marsden ball
- Hit a tennis ball with a stick/dowel rod
- Balance board
- Arrows and jumping
- Toss bean bag in a rainbow arc from one hand to the other and follow with eyes.
- Crawl with something on your back and rotate your head from side to side (ATNR integration)
How do you boost oculomotor control? A Marsden ball can be hung from your clinic ceiling. They can hit it with a whiffle ball or a tennis ball with a stick. I also like using arrows and jumping. You can have them jump on the forward and backward arrows. Moving a ball from side to side while following with their eyes is helpful. They can crawl and rotate their heads side to side to help with weight-bearing, core muscle development, and sensory input. This can be incorporated into an obstacle course.
Motor Muscles PULL but don’t PUSH
- Jump on a trampoline while catching a ball
- Pigeon and duck walks
- Jumping over line w/ both feet
- Foot maze
- Make a box with each arm then each leg
- Balance beam
- Any activity requiring movement of the body in a coordinated way
We know that jumping on the trampoline while catching is very effective and high level. Pigeon and duck walks are also great activities, especially for those with very stiff bodies. Anything requiring the brain and body to move together with the hands will help. The big takeaway is that motor muscles pull but do not push. For example, elbow flexor muscles (biceps) pull into flexion, and then extensor muscles (triceps) pull into extension.
Formal Programs
- S’ Cool Moves
- YOGA Tools for Schools
- Brain Gym
- YOGA4 Classrooms
- Ready Bodies Learning Minds
- VAMPS Assessment – Koscinski, 2018 Pocket OT
There are some tremendous formal programs out there. S' Cool Moves is fun. Yoga for classrooms is one of my favorites. Other programs are Brain Gym and Ready Bodies Learning Minds.
Motor
- Rock while in prone flexion (lineally and then laterally)
- SLOW the swing down
- Frog swing
- Straddle bolster and do activities that force midline crossing
- Bosu ball while tossing and catching
- Reaching for items presented backward and behind
- Sitting back-to-back with OT to play ‘around the world’
Rocking in prone with linear and lateral movement is a great activity. Slower movements require a lot more coordination than faster movements do. Straddling bolsters and tossing and catching items can promote motor coordination, especially with limited space and equipment.
Crossing Midline
- Elbow to Knee (Cross Crawls)
- Figure Eights
- Balance Walking
- Use taped line, curb, or 2 x 4 piece of wood
- Bend and pick things up while on the beam
- Toss and catch while on the beam
- Balloon toss
Elbow to knee cross crawls and figure-eight tasks are great crossing midline and bilateral integration activities. I also love putting tape on the floor as a "balance beam." It helps to engage eyes and hand-eye coordination during balance activities.
Brain Breaks
I have brain breaks on my website that can be used for all children.
Figure 15. Brain Break cards.
YOGA + Public School PE Standards
- Balance while bending and stretching
- Recognize that skill development requires practice
- Identify various body parts and location
- Move each joint in a full range of motion
- Learn teamwork through partners and groups
- Uses the entire body
- Move body safely
I love yoga because it safely uses the body. Make sure you do both sides as it is about balance. I have given you some activities in the handouts.
Mind Over Matter
- Use affirmations
- Theme songs
- Send love and kindness to our bodies while in poses
- Can use with multi-sensory experiences such as a food or flower
These children have a lot of emotions and are easily frustrated. Try to use something positive at the end of your session, like a theme song. Many of my teenage clients pick Phil Collins' "In the Air Tonight" as their song. Give them some song choices that empower them.
Calming Techniques
- Return to flexion
- Lower lighting
- Decrease environmental stimulus
- Proprioceptive Input: PUSH, PULL, LIFT, CARRY
Many kids with movement disorders, including my own, are often bullied. Here are some calming techniques to use. Flexion is our comfort position. It is essential to allow the child to assume flexion in an area with decreased stimuli and lower lighting for calming. This calm state can last up to six to eight hours. It is essential to know what you are doing with these techniques. I have had many situations with other therapists working with my kids who did not do some good things. All of your movement should be child-directed, and you should never force kids to spin for long times.
Summary
We need to recognize the physical manifestations of immature brain function. I gave you some common diagnoses that kids can have and the immature movement patterns associated with those. We also need to be aware of their emotional state. We need to build movement opportunities with them, and hopefully, I gave you some ideas on how to do that. It takes practice, but as OTs, we can do many things to change these kids' lives.
References
Please refer to the additional reference handout.
Citation
Koscinski, C. (2022). Assessment and treatment strategies to boost brain skills in partnership with the pocket occupational therapist. OccupationalTherapy.com, Article 5502. Available at www.occupationaltherapy.com