Introduction & Grounding
I want to begin this course with a grounding exercise since we are going to address stress and trauma for the next hour. Take a moment; hopefully, you are in a setting where you can be seated. Sit up nice and tall with both feet flat on the floor and your back into the chair. Take a moment to come into this space, recognizing and applauding yourself for being here because you understand the importance and need for self-care. Take three deep breaths. Nice deep inhales through the nose and exhales through the mouth. Inhale through the nose, and exhale through the mouth. On this last inhale, taking it in through the nose, see if we can drop our shoulders away from the ears on the exhale. Good, I hope that felt as good for you as it did for me. Those of us who have entered into a helping or healing profession such as healthcare, often come for two reasons. Perhaps we did not have a great childhood and want to ensure others do not experience what we did. Or the opposite, we had an enjoyable childhood experience, and want to ensure everyone experiences the health and well-being we did. That is where self-care and mindfulness come in. We need to practice self-care so that none of our personal issues spread into the workspace with our patients.
Stress & Trauma
Stress is a state of mental or emotional strain and tension resulting from adverse or very demanding circumstances. Being stressed is not a normal state, even though it may feel like it in today's world. Stress is caused by adverse experiences and is a reaction to a stimulus that disturbs our physical or mental equilibrium. This experience generally refers to a psychological perception of pressure because each of us has a different viewpoint. We have different outlooks in certain situations and environments. The body's response to stress involves multiple systems: metabolism, muscle, and memory. Every time we experience a highly toxic level of stress, that causes long-term impacts on our health and well-being. I want to discuss the levels of stress because the term often carries a negative connotation. Stress is not always bad; some stress is positive.
Positive Stress
This type of stress creates a brief increase in the stress response, which could be a quickened heart rate or shallow breathing. Positive stress is a limited or perceived threat, but once the threat has passed and the problem is solved, we return to our normal state. Generally, we can handle positive stress. Those stress hormones dissolve in our body, and the heart rate returns to normal.
Tolerable Stress
This type of stress is a temporary increase in the stress response. Typically, tolerable stress is caused by a serious but, temporary threat to safety. Tolerable stress is buffered when we have supportive relationships and resources to deal with the threat posed. This can be preventable if we are aware of the situation arising, and can avoid it. If left unaddressed, tolerable stress can become chronic stress. An example of tolerable stress might be a flat tire on the freeway, and it's only tolerable if you have the resources and relationships to buffer that experience. For example, if I get a flat tire on the freeway, I'm going to panic, but I've got AAA and know those things will be taken care of. Eventually, my tire will get fixed, and I'll be back on the road.
Toxic Stress
Toxic stress is an overwhelming stress response, which gives stress its negative connotation. This occurs when your body is so overwhelmed. Typically, the heart rate increases, pupils dilate, and you are focused on what's happening that you can't pay attention to anything else. Generally, there is a serious or prolonged threat. Toxic stress removes our ability to cope with what is occurring at the moment. Again, we are overwhelmed, and it pulls us out of our normal ways of thinking and being, which can lead to physical illness or disease. Toxic stress is a prolonged activation of the stress response, which means there is adrenaline and cortisol running through our body without resolution.
Trauma
Judith Herman's book, Trauma & Recovery defines trauma as "a deeply distressing or disturbing experience" (Herman, 1997). She says traumatic events overwhelmed the ordinary systems of care that give people a sense of control, connection and meaning. Trauma can be a one-time event, or it can be multiple events. A key aspect is being able to recognize that trauma overwhelms our ability to care for ourselves and we feel a loss of control. Trauma pulls us away from being in community with others. Some individuals lose their sense of meaning, purpose, or place in this world when enduring trauma.
Three-Part Brain
When we discuss stress and trauma, certainly we need to consider how it impacts the body and brain. The perception of threat, as I mentioned, is occurring through our senses. Am I smelling, seeing, hearing, tasting or touching something that is a threat? Then our brains figure out if we are safe or how to keep us safe by sending signals to the body. We can either eliminate the threat, or we can move through it and heal on the back end. The brain and body relationship are essential, and it is important to remember that two-way street. Our bodies are communicating to our brains, and our brains are communicating to our bodies.
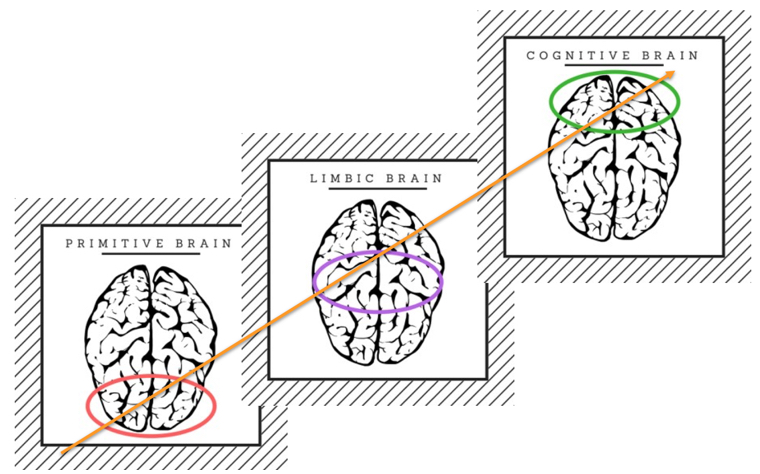
Figure 1. Three-Part Brain
Reptilian Brain
The primitive or reptilian brain includes our prefrontal cortex and is the portion of the brain we use to think. As the three-part brain develops, our primitive brain develops first, then our limbic brain, and lastly, our cognitive brain. The way we engage our brain to be regulated is essential since we can not automatically jump into the cognitive brain without ensuring both our limbic and primitive brains are regulated. Since the reptilian brain is primitive and developed first, babies can only eat, sleep, and have bodily functions. They have a minimal range of motion until they develop and gain further skills. This includes the brainstem and the cerebellum. The brainstem and cerebellum regulate our body's vital functions (i.e., breathe, blink, and swallow). They are continuously working to preserve our safety and maintain our equilibrium. Any injury to this part of the brain indicates a ceasing of those unconscious functions.
Mammalian Brain
The mid-brain or emotional brain is where our perception of emotions occurs. In the mammalian brain, the limbic system sits taking in all the information from your senses and then trying to encode it. The Amygdala, Hippocampus, Hypothalamus, and Thalamus are the main parts of the limbic system. The brainstem is regulating us, and the mid-brain is where we have our relations to relate and connect with others. Also, recorded memories and learning occur here in the mammalian brain. The Hippocampus is our memory center, which influences our behavior. The ability to control our anger and emotions are occurring in the limbic system. This is also where healing happens when there is stress or trauma. We tend to isolate and want to be on our own after experiencing trauma. In your work, simply saying hello to your patients as they come in to see you, making eye contact, that can pull in their limbic system and allow patients to connect.
Limbic System: Learning Center. The Amygdala and Hippocampus have an interesting and inverse relationship. The bundles of neurons on the end of the Hippocampus is where our perception of emotions comes from. That is also where the fear response originates, our flight, fight, or freeze response. Impulse control, memory creation, and aggression control occur in the Hippocampus as well. When we receive information through our senses, our Amygdala and Hippocampus communicate to say, wait, have we experienced this before? The Hippocampus then enables the flight, fight, or freeze response. For some of us, when we are triggered and stressed, that toxic level of stress can cause the Hippocampus to go offline. You may have heard that during a crisis or trauma, people have trouble remembering exactly what happened. When you are in that state of fear, or threat, memory storage goes offline.
Stress Impacts the Learning Brain. When there is a stress response in the limbic system, the Amygdala is being triggered by a threat, real or perceived. If stress is significant enough, memory recall goes offline. That's one of the first depth of knowledge levels in Webb's DOK. Recalling what you were taught becomes unavailable to you. This is also important for the work that you do as healthcare professionals. You may be assuming that someone who is sitting in front of you should be able to tell you something. If they are having trouble recalling or responding to you, it may be because there is a level of stress going on in their brain, or that they're just unregulated in their brainstem. It might be this person hasn't eaten anything all day, and now they're sitting in front of you. Or they haven't slept all night. That's going to impact their interaction with you and their ability to learn and recall. Sometimes it can be very frustrating to work with patients who are not able to recall information.
Rational Brain
The cognitive brain receives, analyzes, and converts information from the rest of the brain to help us form an accurate and usable representation of the world for action. It's the part of the brain that gives us an accurate representation of the world, and of ourselves. This is the part of the brain that gives us that meaning, control, and connection. The brainstem is responsible for regulation, the midbrain is relation, and our neocortex is responsible for rationalization. The rational brain is where we perform higher-level thinking skills (i.e., imagination, judgment, logic), abstract and rational thought, foresight, hindsight, and insight. Our development and understanding of human language occur here also.
Grounding
We have talked a little bit about stress and trauma. I wanted to take a moment and provide you with another grounding activity. If you have the ability where you are, sit up nice and tall in your chair with both feet flat on the floor. Go ahead and close your eyes, and if you are not in a place where you want to do that, soften your gaze, and look toward the floor. The reason we are doing this is to remove the vision from our senses so that we can focus on our hearing. I want you to focus on the sounds around you in the space where you are. Keeping the breath moving, just listening to the sounds around you. Then slowly open your eyes, coming back into your space, and noticing what you were able to hear. It's always nice to take a moment to pull away from everything busy so that we can calm ourselves in our surroundings. If you can be outside, that is even better. Taking that moment and time for yourself during the workday is important. I think that was a two-minute exercise, and we all have two minutes to give, especially for our self-care.
I appreciate this Gandhi quote, "Happiness is when what you think, what you say, and what you do are in harmony." I think for those of us in the helping and healing professions, this is how we do our work. We feel very passionate about the work that we do, and we want to do that work every day. We want to be with people, make connections, heal, and help others. Burnout is the opposite of this. If happiness is when what you think, say, and do are in harmony, burnout is disharmony of those aspects.
Burn Out
The buildup of toxic stress that can lead to cynicism, depression, and exhaustion. Burn out is a physical or mental collapse caused by overwork or stress. Cynicism is very dangerous, especially in the healthcare profession, because we have to show up completely whole with respect for those we serve. When you have a high level of toxic stress and burnout in your life, you can become cynical about the people that you are serving. The buildup of toxic stress can lead to cynicism, depression, and exhaustion. This happens when you are not in control of your work, or how you carry out your job. When we are working toward a goal that does not resonate and causes a sense of detachment from the work we perform. If you lack social support, this can add to the stress. Remember in all those levels of stress, from positive to toxic; resources and relationships can buffer stress.
Compassion
Compassion is sympathetic pity or concern for the sufferings or misgivings of others. For most of us in the healthcare profession, compassion is why we perform the work we do. We did not just fall into this line of work. We all purposely came to our profession because we are compassionate. The root of the word compassion is to suffer "with."
Compassion fatigue. Burnout in the helping and healing profession is often accompanied by compassion fatigue. Typically this type of burnout can be experienced as a result of the frequency or number of misgivings. Especially if you are in a small niche of the healthcare or the helping or healing fields. For those of us who work with the homeless population, it's very easy to find ourselves in the sense of compassion fatigue, because our compassion does not meet the levels of support and resources that are available for them. This can cause stress, pain, and sadness because we can't do everything we want to do for those we serve.
Dr. Charles Figley Tulane states, "Compassion fatigue is a state experienced by those helping people in distress. It is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it can create secondary traumatic stress for the helper." Our professions can become a preoccupation with the suffering of those that we serve, while also showing indifference to those who suffer. Often clinicians take their work home with them, but this can create secondary traumatic stress also.
Signs of Compassion Fatigue:
- Strong identification with helpless, suffering, or traumatized people
- Blaming others for their suffering
- Lack of strong supports for self-care/poor self-care
- Feelings of hopelessness or powerlessness
- Difficulty concentrating
Vicarious Trauma
Vicarious trauma is a response to the accumulation of exposure to the pain of others. I like the term accumulation of exposure because vicarious trauma does not happen in a short period. Depending on the risk level of those that you are serving, vicarious trauma can occur over several years. If you have been a provider or clinician long enough, you recognize that vicarious trauma sneaks up on us. Even though it's vicarious trauma, it still has the same impact on our brain and our body, as someone who's experiencing that trauma firsthand. We can experience the same trauma symptoms in our brain and body as those we serve who are experiencing the trauma firsthand. That's very important to remember.
Self-Care
To prevent burnout and compassion fatigue, and to buffer vicarious trauma, we must commit to self-care. I do not know if burnout is preventable, because we work in a world where, unless you are working independently and in control of your parameters, burnout can become an inevitable part of being an adult. There are ways we can buffer ourselves so that when we begin to feel ourselves burning out, we can have an intervention and stop it.
Self-care is what people do for themselves to establish and maintain health to prevent and deal with illness. I know self-care has a lot of connotations for people. Some individuals attach selfishness, greediness, or being self-centered to the term. However, self-care is something you do for yourself, but it benefits everybody else around you. It benefits your family, it benefits your colleagues, and it benefits those we serve.
6 Domains of Self-Care:
- Physical
- Professional
- Inter-relational
- Emotional
- Psychological
- Spiritual
You want to think about each of these domains individually, and ways that you can work within each domain to make you feel happy, healthy, and whole. I have a simple three-step process to begin noticing these areas and begin self-care.
Notice It
To treat toxic stress and trauma, we must first notice and acknowledge it is occurring. Many of us can go through our work, get it done, and do it well. Then at the end of the day, we fall down from exhaustion, and we are completely tired. Did we notice things along the way that we could have taken care of? Checking in with yourself throughout your day is an important part of self-care. How is it in my mind? What are my thoughts like? Am I cynical? Do I need to do something physically? How is it in my heart? What is my connection to other people and what kind of love and compassion am I holding for myself or others? Throughout the day it is important to check in with yourself. This self-check is an internal weather report because like the weather, the forecast is always changing.
Name It
Dr. Dan Seigel has a theory, "Name it to tame it." This theory is based on how our emotions activate the Amygdala, that fight, flight, or freeze response. By naming our emotions or saying it out loud, this can deactivate the Amygdala. Stating how you feel out loud does not take all emotions away. Think about the last time you were upset. If you were able to say, "I'm angry, I'm really upset right now" this deactivates the stress level. Because you can name it, you felt that release. Naming our emotions diffuses the energy and charge that emotion carries, and it also lessens the burden the emotion caries.
Move It
Taking action is the last step to improving self-care. Once we can notice and name our emotions, then we have to take action. At times, this can be stretching or exercising. When we move our bodies, and we move our breath, which increases blood flow and oxygen to the brain. It gives us a little more space to think. It may increase the size of our Hippocampus, which makes learning and memory a little easier. Norepinephrine is released that increases our heart rate, attention, and motivation. Serotonin comes in when we are exercising and moving, and that enhances our mood. Dopamine is also running through our body, which provides motivation, focus, and learning. When we are moving our body, we are creating the opposite effect of what stress causes to our body and brain.
Mindfulness
Jon Kabat Zinn is the creator of the Mindfulness-Based Stress Reduction Program. I highly recommend looking into the research for Mindfulness-Based Stress Reduction. He gives a simple definition of mindfulness, "paying attention, in a particular way: on purpose, in the present moment, and without judgment." As humans, we tend to ruminate on the past, or project into the future. Being in the present is very difficult for us. A reptile or a mammal has to be in the present to survive; they have to be constantly assessing the threat. For humans, we no longer have to do that, we do not have to be in the present moment. We can ruminate on the past, and we can project into the future, and still survive. Mindfulness is the practice of being fully present at the moment; noticing your thoughts and letting them go without any judgment. Mindfulness is a practice that is similar to meditation. This is very important in the healthcare professions as patients come to us in distress or with a problem. They come to us seeking help or healing.
Mindful Movement
Moving the body and breath at the same time helps ground our brainstem (e.g., primitive brain), and allows us to pull into our cortex (e.g., thinking brain). This stimulates our body into a rhythm that allows us to calm down and to be in the present moment. To finish the course, I have a few breathing exercises here which you can use on your own, as self-care. Please share these with those that you serve and work with.
Take 5 Breaths. This breathing exercise is very simple. Take your hand, with your other index finger start tracing at the base of the thumb. Inhale up the thumb and exhale down. Inhale up the index finger and exhale down. Inhale up the middle finger and exhale down. Inhale up the ring finger and exhale down. Then inhale up the pinky finger and exhale down. You can put your hand on your chest, lap or in your pocket, and just feel your fingers.
Elevator Breath. This is the same breathing exercise we did together at the beginning of the course. Inhale, bringing our shoulders all the way up to our ears, and on the exhale let it drop. Let's do that one more time. Inhale up, and exhale drop.
Lions Breath. A fun breathing exercise that everyone enjoys because you might look silly doing this one. With both feet flat on the floor and hands on top of the thighs. We are going to take a nice deep inhale through the nose, and on the exhale, we are going to stick our tongue out as far as we can and roar like a lion. One more time. Inhale and exhale. Sticking the tongue out of the mouth allows the jaw to relax just a little bit.
Birthday cake breath. Imagine your birthday cake, try to picture what kind of cake it is (i.e., vanilla, chocolate, etc.). Then take a nice deep inhale and on the exhale blow out the candles nice and slow. Let's do one more. Inhale, and on the exhale.
References
Figley CR. Compassion fatigue as a secondary traumatic stress disorder. Brunner-Routledge; New York: 1995. pp. 1–20.
Herman, J. L. (1997). Trauma and Recovery: The aftermath of violence from domestic abuse to Political Terror. New York: Basic Books.
Citation
Steward, N. (2018). Stress, trauma, and mindfulness: Self-care for healthcare professionals. Occupationaltherapy.com, Article 5202. Retrieved from www.occupationaltherapy.com
