Introduction
Hello, everybody. I would love to chat a little bit more about where I started because I think it is pertinent to the presentation topic today. I have been doing OT for a long time in pediatrics. About four years ago, I encountered a situation where I was the OT and then there was an ABA therapist working with the child. The child was in the sensory gym, and he was upset and crying. I could hear him so I went in and tried to talk to the ABA therapist. I said, "He is probably dysregulated and I do not know if he is going to be able to calm down by himself. I know he likes swinging and that might help." The ABA therapist replied, "No, that's not how we do things," and basically asked me to leave because she felt like it was interfering with their treatment process. That was my first interaction with an ABA therapy, and it left a sour taste in my mouth. The relationship between her and I felt a bit tense, and naturally, this seeped into our treatment and progress with the child. I decided to talk to her about it. I said, "Okay, let's get to the bottom of this. I want to see your perspective, and I really would like to tell you mine." Once we were able to talk through our perspectives, I got a handle on where she was coming from. Of course, I cannot speak to whether she has figured out where I was coming from, but at least I got a better understanding of ABA therapy. I thought that if I was encountering this, there were lots of other OTs doing the same. I felt that there needed to be a bridge between the two.
During my doctorate, I decided to do a certification course in ABA. I took that with FIT, which is the Florida Institute of Technology. Ironically, when I was doing the online certification course, the professor would ask, "How many OTs are here? How many speech therapists?" And, during the entire course, he was very derogatory towards OTs, our field of practice, and our evidence or the lack of it in his opinion. And I thought, "Wow, here's another example where we need to build a bridge." We are not going to progress as a field and collaboratively provide the best health care if we are not on the same page. I waited until my certification was over, but I did email him. I said, "I loved your content, and I think was brilliant. However, I do want to say that it would go a long way for you to try to understand the perspective of what OT can bring rather than just knocking us."
Also, during this time, my son was struggling in school. Being an OT, I really thought I could handle it. He had ADHD and anxiety so I did all the traditional avenues and nothing was really working. He was spiraling into this negativity of, "I'm rubbish, and I'm never going to get school." And, "I'm not made out for this." I was just so defeated. It was during my doctorate that I found Fit Learning which is based on ABA principles. I decided to look into it. It has transformed my son. When I saw the transformational results, I decided to bring it to the Chicagoland area to further foster my love of bridging the gap between OT and ABA. So, that is just a little intro about me and how and where I got started. Figure 1 shows a picture of me doing some ABA fluency building with academics.

Figure 1. Me working in one of my labs.
I have two labs in Chicago. We only do academics, and it is all based on a form of ABA called precision teaching which the highest gold standard of ABA. My passion is still in OT and bridging that gap as I said.
Playing Nice in the Sandbox
Let's start by talking about what ABA therapists and OTs think (Figure 2).
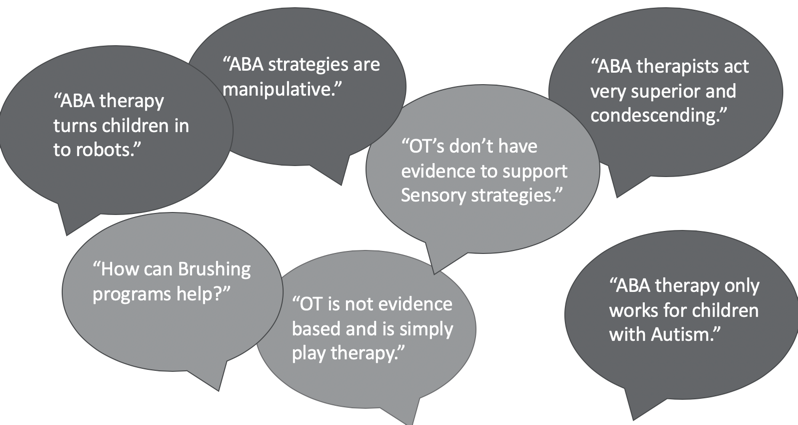
Figure 2. ABA vs. OT.
I have heard this a lot from ABA therapists, "Brushing is just playing. It does not really do anything." And, "It is not evidence-based." They think a lot of our therapeutic interventions are not evidence-based, and we are just playing with the child. Sensory is a huge area where ABAs think that we just do not have the data and research to support us. On the flip side, what do OTs think of ABA? "It can be awfully robotic." Many OTs think that it turns children into robotic responders. I do want to caution you with this thought. ABA therapists work with an autism population. And in autism, students or children tend to have a hard time generalizing with affect and in different situations. They have a propensity to be more robotic anyway. I am not sure how much of that is ABA and how much of that is part of the diagnosis. "ABA strategies are manipulative." I also hear this a lot from OTs who feel that ABA therapists are being sneaky and manipulative. My opinion is yes and no. As OTs and ABAs, and other therapists, we are all scientists. We look at a problem, and we try to change the variables to get a positive outcome. We manipulate our responses and the environment. I feel like manipulation is a negative connotation, but when you are a scientist, it is what you have to do to get the desired results for the child. "ABA therapists are superior and condescending." I have encountered this over and over again. However, I have also encountered this with other OTs and speech pathologists earlier on in my career. "ABAs only work with autistic children." While that is true for the most part, ABA is expanding. Insurance typically only covers autism. However, behavior applies to everybody. I do not care what diagnosis you have, behavior is prominent. It is a binding factor in human nature. ABA therapists can work with various diagnoses, but they are being a bit pigeonholed in the autism arena. We all have beliefs regarding each other's position in the field of healthcare. It comes down to playing nice in the sandbox because we all have a common goal.
Common Goal
Our common goal is to use evidence-based strategies to get the best outcomes for our clients or students.
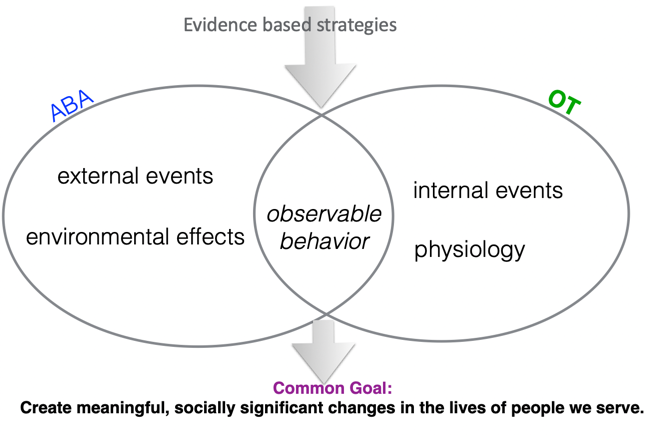
Figure 3. Our common goals.
If you look at our goals and our position statement in OT and ABA, we all want to create meaningful and socially significant changes for the people that we're serving. And so instead of being contentious, if we come together, we can really address this holistically. So what do ABAs look at? In ABA, they look at more of an external environmental situation. What's going on externally? What's the environment looking like? And they take observable behavior and try to figure out what's going on and manipulate the environment or external environments. What do we do as OTs? We have the breadth of knowledge of anatomy, physiology, neurology, all those internal cognitive abilities too. We have that extra knowledge, and we try to look at that and ascertain what can we do to help this child or client achieve a common goal? So the area we can overlap in is looking at behavior. I mean imagine if you have all this knowledge and you can add observable behavior and principles on how to manipulate that, how powerful your intervention can really be.
Internalistic Vs. Externalistic
- Internalistic-OT:
- Physical/psychological barrier
- Adaptations/ accommodations
- Consider feelings and emotions
- Consider culture, environment, values & beliefs.
- Externalistic-ABA:
- Not the child’s fault
- Try different ways of teaching
- Never blame the child if learning does not occur
- Change the environment and consequence to change behavior
Just breaking this down further, OTs take a more internalistic approach. OT looks at physiological and psychological barriers. We also look at cognitive processing, values, and beliefs. We try to figure out how can we help a child with adaptations or accommodations. We consider feelings, emotions, and culture, or family dynamics. We look at the client holistically. Whereas, ABA tends to be more externalistic. It is all based on what is going on in the environment. It is not internal at all. They do not blame the child. ABA therapists look at different ways of teaching and modifying the environmental factors to change the consequence, and therefore the behavior. It is the opposite. As you can see, ABA is very linear in their thinking where we are more holistic and look at all these facets of learning and behavior.
Interprofessional Collaboration in Education
When it comes to interprofessional collaboration in education, it is so important and that's why AOTA has taken this position.
(Earnest & Brandt, 2014)
AOTA has been working towards this goal of interprofessional collaboration. OTs already have profound knowledge that they have learned in school, but if they can add a layer of ABA and behavioral principles, this is going to give you a great impact. The research shows that when achieving goals collaboratively, there are improved health outcomes, client experiences, and reduced costs. If there is both an OT and an ABA therapist on the team, and the OT says one thing and the ABA says another, this can create a lot of anxiety for that client. The caregivers might be confused as to who to listen to. And if the OT and ABA cannot come together, that can also create a rift within the team. I often see OT clients when they are on a waitlist for ABA. I am able to help them with a lot of the ABA principles until they get an ABA provider. By no means am I replacing the ABA provider, but I am able to help. Inadvertently, I am also reducing healthcare costs.
What is ABA?
- ABA is the use of scientific principles of learning and using motivation to teach effectively for skill acquisition, fluency, and maintenance as a means of decreasing problematic behaviors.
(Cooper, Heron, & Heward, 2007)
I think everyone has a notion of what ABA is. It is based on the science of learning. The science of learning is what motivates each person to learn. How can we use that to teach effectively for skill acquisition, fluency, and maintenance, and to also decrease problematic behaviors that impede progress? For OTs, I think this is what we need. For example, if you have a student with a lot of behaviors, you cannot help them to get to that next level because you are trying to figure out how these behaviors are impacting progress. This is where I think ABA can be helpful to our practice.
Respondent Vs. Operant Behavior
There are two types of behaviors.
- Respondent:
- Controlled by antecedent in the environment
- Not learned
- Occurs naturally
- Un-conditioned
- Pavlov
- Reflexive
- Involuntary
- Operant
- Controlled by consequence
- Learning occurs based on consequence that follows
- BF Skinner
- Voluntary
Respondent is controlled by something in the environment. This would be more of your sensory response and automatic response. It is not learned, and it occurs naturally. It is not contrived in any way, and it is unconditioned. Nobody has taught you to do this. This is where Pavlov's dogs come into play. They salivate when they hear the bell at the thought of food. It is a reflexive, involuntary response. It is not turned on. Operant behavior is what is controlled by the environment. In ABA, they look at operant behavior for the most part. They know that learning occurs based on the consequence that follows, and this is based on B.F. Skinner's teachings. This is completely voluntary. I want to go through each one of these scenarios to go over these types of behaviors.
- Raising a hand in class to answer a question? Operant
- Shivering in the cold? Respondent
- Stopped by a police officer for speeding? Operant
- Tickle in your throat? Respondent
- Walking in the hallway? Operant
- Name calling? Operant
- Knee jerk when tapped with a hammer? Respondent
The first is raising your hand in class. This is a voluntary response, and it is not reflexive. Shivering in the cold is next. Can you control that? You could try, but it is really a reflexive, involuntary response. When you are followed by a police car with their lights on, slowing down might be reflexive, but the act of stopping the car is a voluntary response. Somebody is actually choosing to do that action. A tickle in your throat is reflexive or respondent. Let's look at walking in the hallway. Are you choosing to do that? Is it a voluntary response? That would be an operant response. Name calling is operant. It could be respondent if you are talking about something like Tourette's syndrome. In that scenario, it could be a reflexive, sensory response, automatic. But for the main part, it is a choice you are making when you are calling someone a name. Lastly, a knee-jerk is respondent. Your leg moves on its own when that hammer hits that knee. It is really important to understand respondent and operant behavior. Respondent behavior is going to more of a sensory realm, and this is something that is not always in their control. I wanted to give you the definition of operant behavior because this is what we are going to focus on.
Operant Behavior
“All we need to know in order to describe and explain behavior is this: Actions followed by good outcomes are likely to recur, and actions followed by bad outcomes are less likely to recur.”
(Skinner, 1953)
Operant behavior is the premise that actions that are followed by good outcomes are more likely to occur. They can occur again and again. Whereas, actions that are followed by bad outcomes are less likely to occur. I think we all know this, and this is where reinforcement and punishment come in.
Reinforcement
- “when a behavior is followed immediately by the presentation of a stimulus that increases the future frequency of the behavior” (Cooper, Heron, & Heward, 2007).
- Positive = add and Negative = take away.
- Negative: when a person's behavior causes something they don’t like from happening to be taken away.
- Positive: add or present something that you like into your environment.
I really want to break down reinforcement, because sometimes we use this phrase very loosely. Reinforcement is only called reinforcement in ABA if it increases the future frequency of that behavior. If it does not, then it is not a reinforcer. For example, I love M&Ms.
