Editor’s note: This text-based course is a transcript of the webinar, Mindfulness Practices for Managing Pain and Promoting Occupational Performance, by Richard Sabel, MA, MPH, OTR, GCFP.
Learning Outcomes
- After this course, participants will be able to identify how Tai Chi, Yoga, and Feldenkrais can be used to manage pain.
- After this course, participants will be able to identify how Tai Chi, Yoga, and Feldenkrais can be used to promote occupational performance.
- After this course, participants will be able to identify the benefits of straw breathing or pursed-lip breathing as an effective pain/stress management intervention.
Introduction
Before I get into the formal lecture, I want to share that I have lived with chronic back pain for over 20 years. One day when I was in my 20's I hurt my back, and for the next 20-plus years, I really struggled. Sometimes, it took me a long time to just get out of a chair or to be more upright. There were days and weeks where I would feel pretty good, but for 20-plus years, I had issues. I became an OT, went to OT school when it was in my 40s, so when I entered OT school, I was still dealing with back pain. Through serendipity and people telling me about things, I discovered yoga, and I was introduced to restorative yoga. And then, I got introduced to the Feldenkrais Method, of which I got a certification and training. It was these mindfulness-based approaches that ultimately turned things around for me. Here I am at 65, and I still maintain a clinical practice. I move with much more comfort and ease, and my back, for many years now, has not been an issue. I have found that these traditions, both Eastern and Western traditions (Feldenkrais is from the West), complement occupational therapy. Weaving mindfulness-based traditions with what we know as occupational therapists provide a potent intervention to our clients. But I also want to say that everything I will talk about today is good for you too. We are doing little bits of snippets of experiential pieces with some of these traditions. We could think of it as like every now and then a tray will come by with some hors d'oeuvres. You will take one hors d'oeuvre, and we will taste that one for a little bit. Then, we will move on to another hors d'oeuvre.
Unrelieved Pain is a Global Health Issue
- An estimated 20.4% (50.0 million) of U.S. adults had chronic pain, and 8.0% of U.S. adults (19.6 million) had high-impact chronic pain.
Dahlhamer J, Lucas J, Zelaya, C, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults — United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:1001–1006. DOI: http://dx.doi.org/10.15585/mmwr.mm6736a2external icon.
Chronic pain is a global health issue. Unfortunately, millions of people live with chronic pain, which impedes their ability to engage in occupations fully.
Physical and Emotional Pain
Not only is physical pain debilitating, but I also want to acknowledge emotional pain. Emotional pain can be equally debilitating. And oftentimes, people with physical pain are also dealing with emotional pain.
Pain is in Your Head
- Neuro Matrix of Pain: Multiple parts of the brain acting together - sensory, emotional, cognitive, motor, and behavioral
The neural matrix theory of pain basically says that multiple brain regions are stimulated when we experience pain. When they do scans, they can see that. It is not just one spot in the brain that lights up, but multiple places light up. These are parts of the brain that deal with sensation, emotion, cognition, motor function, and behavior.
- Helps explain why people in pain report difficulty:
- concentrating and thinking
- heightened sensitivity to sounds or light
- moving with ease
- controlling emotions – more irritable and outburst
Barbara mentioned this in the first presentation. This is why people who have pain have difficulty concentrating and thinking. They are also more sensitive to sound and light, and movement is much more challenging. It can be difficult for some to control their emotions, and they are more labile.
Pain is Subjective
Pain is subjective, and Barbara also talked about that. How we think about pain influences the experience of pain. It is multi-dimensional.
- Attention
- Prior pain
- Culture
- Mood
When someone is feeling pain, how much attention do they give it? This is going to influence their experience. Prior experiences with pain are also going to influence this. What is my mood? We all know that some days we are in a really positive frame of mind. If a painful stimulus occurs, this might be less impactful based on your mood. On other days, this same stimulus could be really painful, even debilitating. Of course, the home you grew up in and how people reacted to pain, and the larger culture around you also is influenced your pain experience.
Mindfulness
- “the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience, moment by moment” (p. 145).
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delacourt, New York.
This leads to mindfulness. Let's just take John Kabat-Zinn's definition, mindfulness, "The awareness that emerges through paying attention on purpose in the present moment and nonjudgmental to the unfolding of experience, moment by moment." If I am relying on past experiences and how they affected me, I am not in the moment to truly judge what is happening right now. When we think of this ability to pay attention, we want to pay attention to the things going on around us external to our bodies. This includes paying attention to the people we talk to, listening well, truly hearing what they have to say, and not thinking about what we're going to have for dinner.
Body Awareness
- Interoception - sensing the physiological state of the body
- Proprioception and Kinesthesia - sensing the body’s position in space
- Neuromuscular Education 97112
- Performed to Improve:
- Balance
- Coordination
- Kinesthetic sense
- Posture
- Proprioception
- to improve function
There is also body awareness or that internal focus. Interoception is sensing our physiological state. Equally important to that is helping to learn to better sense movement and proprioception, sensing our body's position in space. It is important to help clients develop a better kinesthetic sense, or body awareness, to enable them to sense what is happening within themselves and then make appropriate adjustments when necessary. We will get into this more in a little bit.
What I am talking about is not esoteric. You can see on this slide I have the Medicare definition of neuromuscular education, which is one of the most-used billing categories. The Medicare definition says that if we are working on improving somebody's kinesthetic sense or proprioception to improve function, that is billable. Thus, every time we work with people to better pay attention, that is better for them, and it is 100% billable.
- Examining the interrelationships between:
- cognition
- stress
- emotions
- physical sensations (pain)
- behavior
- Non-judgmental:
- acceptance
- kindness
- openness
- curiosity
- patience
- equanimity
- non-striving
- Reflection:
- What if anything is different?
With mindfulness, we help people reflect and examine the interrelationships between cognition, stress, emotions, the actual sensation of pain, and the behaviors that ensue in reaction to the pain. When you feel pain, it is not so easy to be nonjudgmental, but can I accept the pain, can I be kind to myself, can I be open, can I be curious, and can I be patient with myself to work towards equanimity. This is seeing at the moment what is going on. This becomes important for pain because, as Jon Kabat-Zinn talked about, in the book "Full Catastrophe of Living," rolling out the red carpet for pain is a possible strategy. Rather than make it an enemy, pain can be viewed as information. What is that information telling us?
If I can focus on the pain in a non-judgmental way or in a mindful way, it opens the door to experiencing the fluctuations that can be there within the pain. Pain is not like turning a light switch, where you flip it on or off. It is not always the same, and people need to realize that there is a lot of variability in pain sensations and experiences. When people start to see the variability, this gives them a sense of understanding of how they could work with it more effectively.
The other piece here is reflection. After we treat somebody, we reflect on how the session went and what we could have done differently. We also have to help the people we work with to reflect afterward as well. We live in a busy world, and a client may run to PT, then OT, the dry cleaners, and so on. They often do not stop to reflect, to sense, or to notice. "I just did something in therapy. Do I notice any differences?" We have to set the conditions to help people slow down a little bit to notice anything. As therapists, it is not often that we take the mallet, swing it, hit the bell at the carnival. Sometimes, we do one thing, and it works well, but usually, it is the small changes that lead to bigger changes over time. We have to help the people we work with to notice those small changes.
The Mind-Body Circle of Influence
Figure 1 shows a model to think about how to address pain.
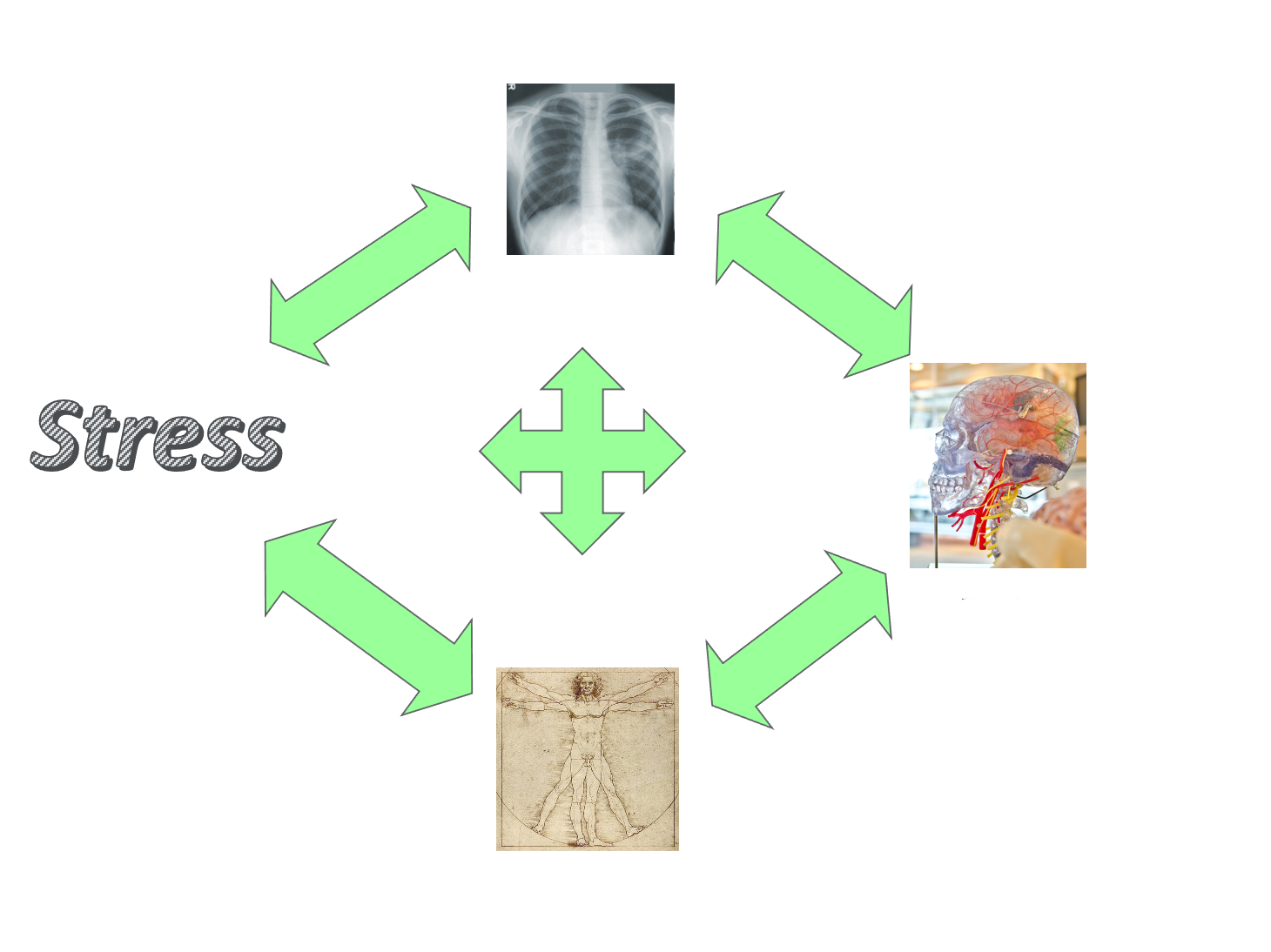
Figure 1. The Mind-Body Circle of Influence.
The picture at the bottom by Leonardo da Vinci represents the body, and the picture on the far right is a brain that represents the brain and thinking. With this pain, perhaps the client thinks, "Why did I get this pain? This is the pain I experienced a month ago that was really debilitating." How is this type of thinking going to affect their stress level? It will most likely increase their level of stress if they start thinking about all the potential problems and the issues related to past and current pain. This will release more cortisol into the body, which then makes their breathing get more rapid. This, in turn, feeds the stress response. When a person gets stressed, do the muscles get more relaxed or tighter? They get tighter. Ultimately, there are interrelationships between thinking, breathing, the physical body, and how that all contributes to stress.
This model also shows us a great way in which to work with people. We can use their breath to help. Remember, when we get stressed, our breath gets more rapid and shifts us, possibly from the parasympathetic branch to the autonomic nervous system's sympathetic branch. If I can slow my breathing down, this will quiet my mind, reduce the stress, and relax my body. I can also work with gentle, mindful movement, which will immediately impact my breath. Or, I can do things with the mind.
Creating a New Narrative
Let's also never forget that as occupational therapists, we get our clients engaged in an activity that captures their attention. Occupations are an integral piece to managing pain. I hope to show that by creating a new narrative and a new way of thinking, we can increase our own health and well-being and that of our clients. We will be using these traditions to address that.
- Feldenkrais
- Stress
- Feel
- Think
- Act
- Yoga
- Tai Chi Chuan
- Meditation
- Breath
These words here are from Moshe Feldenkrais, who started the Feldenkrais tradition. I think of these every time I work with a client, whether they have chronic pain or not. If I can help my clients sense things differently, that will influence how they feel. "When I reached for something on the floor, it didn't hurt. Maybe I can get down on the floor and play with my grandkids." This new thinking leads to action. As an OT, I like to change the word action to engagement. Changing a way of thinking can lead to more engagement.
Breath
- The bridge between the mind and the body.
Breath is the bridge between mind and body. You and I breathe in over 20,000 cycles of breath per day. When I graduated from my OT program, we did not really talk much about breathing. I spent many years realizing that most of the people I was working with were not breathing efficiently. Breath is vital. If I had only one thing to do, it would be working with breath because it impacts every aspect of our wellbeing. Figure 2 shows the lungs and all the different areas that are impacted by breathing.
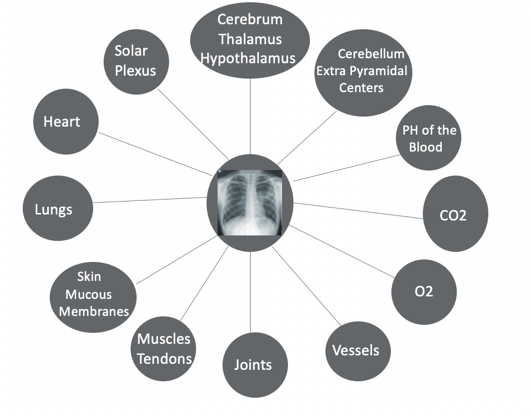
Figure 2. Example of things that breath impacts.
Additionally, if we breathe rapidly, that influences the pH level, impacting how every cell in the body metabolizes, like in muscles, tendons, joints, et cetera. Breath impacts us globally.
Common Breath Holding Patterns
- Chest Breathing
- Reverse
- Breathing/Paradoxical Breathing
- Collapsed Breathing
- Hyperventilation
- Dyspnea
These are the most common breathing patterns. When working with somebody who has pain, look at their respiratory rate and how quickly they are breathing. What does that pattern look like? Are they doing chest breathing? Chest breathing expands the chest, raises the shoulders slightly, and then lets them drop to exhale. That is a shallow breath. When we breathe in, we should expand a little bit, and when we breathe out, we contract. When people do the opposite, that is called reverse and paradoxical breathing. Collapsed breathing has more to do with posture. If a person is more collapsed, that will restrict their breath. Hyperventilation is when clients are breathing at a respiratory rate of 20 cycles of breath per minute. This is a mild version of hyperventilation which has a lot of consequences. All of these lead to shortness of breath. Figure 3 shows me completing a shallow breath.
Figure 3. Example of a shallow breath.
Impact of These Breathing Patterns
- Chronic tension in upper body, especially around the neck, shoulders, back, and jaw
- Anxiety, increased stress response (heart disease, hypertension, muscle tension)
- Lack of circulation in abdominal area leading to indigestion, heartburn, and bloating
- Greater difficulty learning movement because basic pattern of breathing (movement) can be upside down
- Confused and disoriented state of mind
More Efficient Breathing Will Contribute To:
- More energy to engage in occupations
- A calmer, clearer perspective
- Manage pain
- Greater ease of movement
These triangles on the body in Figure 4 show how there should be more movement lower down and less movement on top.

Figure 4. More breath movement should be lower down, as represented by the triangles.
Many people have the triangle turned the opposite way. What does that do when we are breathing shallowly? There can be chronic tension in the upper body, especially around the neck, shoulders, back, and jaw. All the secondary muscles of respiration, like the scalenes, are working overtime when they are only supposed to work part-time. The stress response also taps into the sympathetic branch, so we feel more anxiety. There is also a lack of circulation in the abdominal area because when we are in fight or flight mode, all the blood is pushed out of the belly and goes to our arms, legs, and brain for fighting so we can survive. It becomes difficult for our clients to learn new skills or movement patterns because if they are stressed. Learning becomes very challenging, and if somebody is in a mild hyperventilation state, they can be confused or a little bit disoriented. Helping the client breathe more efficiently gives them more energy to engage in occupations and a calmer and clearer perspective to manage pain. This is the focus of today's presentation. Lastly, it will give them greater ease of movement.
Straw Experiment
Let's just do one experiment. You will need a straw. You will breathe in through your nose, and then I want you to breathe out through the straw. If you do not have a straw, do pursed-lip breathing. Exhale through pursed lips as if you were going to blow up a bubble with one of those with the soapy water. This is what we teach people with COPD, as it is the gold standard. It creates back pressure when we slow down the exhale rate, which the straw will do, and opens the airways to allow more air to get out of the lungs. This ultimately then allows more air to get in. It also slows down the respiratory rate shifting us more to the parasympathetic branch than the sympathetic branch. For the next minute, either use pursed-lip breathing or straw breathing. Take a moment to sense how you feel right now. This is going to slow down your respiratory rate and allow you to take a deeper breath without having to think about, "How do I take a deeper breath?" It promotes diaphragmatic breathing and is a wonderful pain management tool. It takes the awareness of the pain often from the front burner of the person's awareness and shifts it to the back burner. After you have done this for one minute, sit there for a moment and notice if you feel differently. When we start to slow down our respiratory rate, the pH level begins to shift. We also begin to shift from the fight or flight mode to the rest and digest mode. Again, if I had only one intervention to work with people with chronic pain, it would be breathing because of its global impact.
I did a group for many years when I worked at Beth Israel Medical Center. It was a breath group where there was a different breath lesson every day. People would come in with a lot of pain because they were post-surgery. Afterward, they might report some pain, but it was definitely not at the level it was before. And for many people, it would go away.
Tai Chi Chuan
I am sure that you are all familiar with what Tai Chi looks like (Figure 5).
