Introduction
There are continued concerns about disparities in health care. There is a need for health care systems and therapists to accommodate an increasingly diverse patient population. Cultural and linguistic competency has become a matter of national concern, if you will.
Definitions and Terminology
Cultural and linguistic competency is defined as the capacity for individuals and organizations to work and communicate effectively in cross-cultural situations. Cultural and linguistic differences between you and your patients can result in a lot of problems (HHS OMH, 2013).
- Miscommunication
- Lack of understanding regarding diagnosis or treatment
- Other consequences that may negatively influence health outcomes
Developing cultural and linguistic competency can help you as a therapist minimize communication errors, increase understanding, and overcome barriers that may affect the care that you are providing to your patients. Cultural linguistic competency includes increasing our awareness of our communities, as well as us becoming culturally aware ourselves. When we get into the presentation, we are going to go through, or at least I can highlight for you, a specific tool for how you can do a self-assessment of your own cultural competency.
Awareness of your community's perspectives, as well as your own personal attitudes, beliefs, biasses, behaviors, and recognizing that all of these can impact your patient care, can help you as a therapist to improve your patient's quality of care, access to care, and their health outcomes.
Culture is the integrated pattern of thoughts, communications, actions, customs, beliefs, values, and institutions associated wholly or partially with racial, ethnic, or linguistic groups, as well as religious, spiritual, biological, geographical, or sociological characteristics. Culture is dynamic in nature and individuals may identify with multiple cultures over the course of their lifetimes depending on their background. The culturally and linguistically appropriate services, or the CLAS, are standards. These are services that are respectful of and responsive to an individual's cultural health beliefs and practices, preferred languages, health literacy levels, and communication needs employed by all members of an organization regardless of size at every point of contact.
One of the handouts that you can download are the National Standards for Culturally and Linguistically Appropriate Services in Health and health care. This handout outlines all the different standards that you can help your facility put into place. It talks about communication and language assistance, accountability, continuous improvement, and the like. I strongly urge you to download this and take a look at these standards.
Persons with limited English proficiency, or LEP, are unable to communicate effectively in English and may have difficulty speaking or reading English (HHS OCR, 2003). Limited English proficiency refers to a level of English proficiency that is insufficient to ensure equal access to services without language assistance. Health, and we will talk about this more, encompasses a lot of different aspects, physical, mental, social, etc. (HHS OMH, 2013). Health disparities adversely affect groups of people who have systemically experienced greater obstacles to health based on some factor (HHS OMH, 2011). It could be either a racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognition, sensory or physical disability, sexual orientation or gender identity, geographic location, or other characteristics that are historically linked to discrimination or exclusion. Health care disparities are the differences in the receipt of, experiences with, and quality of health care that are not due to access-related factors or clinical needs, preference, or appropriateness of intervention (IOM, 2003).
Other definitions of culture include:
“A culture, in the anthropological sense, is the set of beliefs, rules of behavior, and customary behaviors maintained, practiced, and transmitted in a given society. Different cultures may be found in a society as a whole or in its segments, for example, in its ethnics groups or social classes.” (Hahn, 1995)
“The cluster of learned and shared beliefs, values (enrichment, individualism, collectivism, etc.), practices (rituals and ceremonies), behaviors (roles, customs, traditions, etc.), symbols (institutions, language, ideas, objects, and artifacts), and attitudes (moral, political, religious) that are characteristic of a particular group of people and that are communicated from one generation to another.” (Gardiner & Kosmitzki, 2005)
If you look at some of these definitions, I think it ties really nicely with the occupational profile that hopefully we are all using in clinical practice, and we can certainly tap into some of these elements related to culture.
What is Culture?
Culture is learned. It is transmitted from one generation to the next. You learn culture through interaction with others and listening to, observing, and assessing those interactions (Carpenter-Song, et al, 2007).
Culture is localized. It is from such interactions that you identify and learn what elements, objects in the world, aspects of human relationships, proper behavior, and more, define the cultural universe that you share with other members of a society. Those meaningful elements are shared with some, but not all of the individuals within that society.
Culture is patterned. Repetition that creates expectation is essential for successful social behavior and the creation and maintenance of societies. It is essential for individuals within a group to develop patterns for behavior that minimize ambiguity and avoid having to renegotiate every interaction that they have (Yerxa, 2002).
Culture confers and expresses values. Values define the concepts and the behaviors that are important to a cultural system, and those values are embedded in the culture and in individual behavioral decisions and choices (Fowers & Davidov, 2006).
Finally, culture is persistent, but adaptive. In general, culture is pretty stable, but it can also adaptive. Cultural knowledge continues to change over the course of your life as you encounter new objects or new situations or ideas in your own environment (Whaley & Davis, 2007). Those experiences serve to shape you as a unique person.
Why is Cultural Competence Important?
Why is cultural competence important? Delivering care in a culturally and linguistically appropriate manner is a key way that you as a therapist can help improve the quality of care for diverse patients that you serve, improve the quality of services, increase patient safety, and increase patient satisfaction (Beach et al., 2004; Goode, Dunne, & Bronheim, 2006; Betancourt, 2006; Brach & Fraser, 2000; Thom, Hall, & Pawlson, 2004.
Demographic Changes
The U.S. Census Bureau projects that by 2060, the United States will become an even more multicultural society (U.S. Census Bureau, 2012). Unfortunately, the changes that we have seen in the demographics within the health care workforce have not kept pace with society as a whole (Genao, Bussey-Jones, Branch, & Corbie-Smoth, 2003; IOM, 2004b; Sullivan & Mittman, 2010). About 70% of the allied health care workforce is non-Hispanic or White. Because of that, cultural competency takes on a whole new meaning. Workforce diversity can certainly lessen the cultural difference or gaps that may exist between us as providers and our patients, who come from different backgrounds, and the provision of culturally-appropriate services also can help to close that gap.
Figure 1 comes directly from the U.S. Census Bureau from 2012, and I am going to quote the acting director of the U.S. Census Bureau. He says, "The next half-century marks key points in continuing trends. The United States will become a plurality nation, where the non-Hispanic White population remains the single largest group, but no group is in the majority. And as the United States increasingly becomes a more multi-ethnic, pluralistic, and linguistically diverse society, the possibilities for misunderstandings, mixed messages, and errors in communication are inevitable."
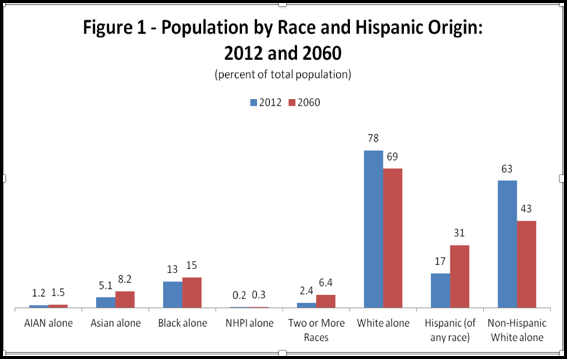
Figure 1. Population by race and Hispanic origin.
This drives home the purpose and the importance to this.
Contributing Factors to Health and Health Care Disparities
Research indicates that there is a persistence of health disparities; it is abundant in our culture. The National health care Disparities Report and the Health Disparities and Inequalities Report that come directly from the Agency for health care Research and Quality show that there are a lot of different factors that contribute to disparities in health care.
- Social determinants of health
- Lifestyle choices
- Patients’ care-seeking behavior
- Linguistic barriers
- Variations in the predisposition to seeking timely care
- Degree of trust
- Ability to pay for care
- Location, management, and delivery of health care services
- Clinical uncertainty
- Beliefs of health care practitioners
There are social determinants of health like education, income, and access to healthy food. Lifestyle choices are another. Care-seeking behavior means that we may seek care differently based on our cultural beliefs. There is the ability to pay for care directly or through insurance coverage, because some folks do not have the ability to pay. The location, the management of health care services, beliefs of health care practitioners, and certainly a degree of trust between the patient and the health care practitioner are other factors.
Health and health care disparities are well-documented across many different cultural linguistic groups. Individuals of different races, members of the lesbian, gay, bisexual, and transgender communities, individuals with physical disabilities, and individuals living in rural areas all may experience health and health care disparities over their lifetime. In fact, racial and ethnic minorities experience higher rates of chronic disease and disability, higher mortality rates, & lower quality care, compared to non-Hispanic Whites (HRET, 2011; IOM, 2003). Suicide is the third-leading cause of death among youth age 15 to 24, and LGBT youth are more likely to attempt suicide compared with their heterosexual peers (Hatzenbuehler, 2011). Individuals with lower incomes are more likely to experience preventable hospitalization compared to individuals with higher incomes (HHS CDC, 2011). Delivering care and services in a culturally-appropriate manner is a way for everyone to help address health and health care disparities in our system.
Why Cultural Competency Matters
Importance of Culture
Culture shapes our language, our behaviors, our values, and our institutions. In health care settings, culture and language differences can result in misunderstandings, lack of compliance, particularly with a home exercise program or some instruction that we are giving to the patient, or other factors that can negatively impact the clinical situation.
Culturally Appropriate Care
Providing culturally appropriate care is especially urgent, because again, research is showing that many cultural and linguistic groups received lower quality health care even when socio, economic, and access-related factors were controlled or the same (IOM, 2003; HHS OMH, 2001; HHS OMH, 2013). Cultural groups encompass not only racial, ethnic, or linguistic groups, but also religious, spiritual, biological, geographical, or sociological characteristics. Linguistic minorities include people with limited English proficiency, as we already said, people with limited literacy skills, and those who are deaf or hard of hearing. Bias, stereotyping, prejudice, and other clinical uncertainties contribute to these disparities in health care (IOM, 2003). We need to keep that in check as we deliver care.
Terminology
There are some additional terms with which you should be familiar. Bias is a preference or an inclination, especially one that inhibits impartial judgment or an unfair act or policy stemming from prejudice (IOM, 2003). An assumption is an underling assumption that is an unconscious, taken-for-granted belief and value that helps determine behaviors and perceptions (Schein, 2010). Prejudice is a negative attitude toward a specific people, like a race or religion (Pincus, 2006). A stereotype is an oversimplified conception, opinion, or belief about some aspect of an individual group of people (Purnell, 2005). Discrimination are actions that deny equal treatment to persons perceived to be members of some specific group (Pincus, 2006). Everyone has biases and make assumptions about other people. These biases and assumptions become problematic when they result in prejudiced treatment, discrimination, or some other sort of unfair treatment.
Why Does Competency Matter?
The Institute of Medicine (2001) recommends that we, as health care providers, adopt as our explicit purpose to continually reduce the burden of illness, injury, and disability, and to improve the functioning of individuals. We need to provide health care that is:
- Safe
- Effective
- Patient-centered
- Timely
- Efficient
- Equitable
To reach this goal, we need to aim to provide health care that is safe, so we are avoiding injuries to our patients from care that is actually intended to help them. Care needs to be effective, so we are providing services based on the best available evidence. Care that is patient-centered means we are providing care that is respectful of and responsive to individual preferences, needs, and values. It is timely, so we are reducing waits and sometimes harmful delays. It is efficient, avoiding waste in particular of equipment or supplies. Finally, the health care needs to be equitable; providing care that does not vary in quality just because of personal characteristics like gender, ethnicity, geographic location, or socioeconomic status. Again, as health care professionals, we want to learn as much as we can about diverse population groups and continuously examine and enhance our awareness, knowledge, and skills related to those differences.
Factors Affecting Competency
Let's take a look now at the different factors that affect competency.
Self-Awareness
I strongly urge you to download the handout called the Checklist PHC. It promotes cultural and linguistic competency and is a self-assessment checklist for health care services. It goes through everything: the environment, materials, resources, your values and attitudes, your communication style, and starts to pinpoint where you might have bias or an assumption about a particular group of people. When you are aware of it, you can then try to change that bias. Awareness of our own values and those of the health care system is the foundation of competent care (Leonard & Plotnikoff, 2000; Barnes, 2004).
Terms like ethnocentrism, essentialism, and power differences may impact your ability to provide culturally-sensitive and appropriate care. You may be very unconscious of the fact that you have some of those beliefs, and we want to make sure that we are aware of our own beliefs.
Ethnocentrism
Ethnocentrism is a belief that your way of life and your view of the world is inherently superior to others, and therefore more desirable. In health care, this can prevent you from working effectively with a patient whose beliefs or cultures do not match your own ethnocentric worldview. If we do not address it, it can certainly compromise your relationship with your patient and lead to either mistreatment or insufficient treatment.
Essentialism
Essentialism defines groups as essentially different with characteristics natural to a group. Essentialism does not take into account any variation within a culture, and obviously, there is a lot of variation within our cultures. Essentialism can lead you as therapists to stereotype your patient, and as such, your clinical practice then starts to focus on beliefs about the groups instead of being individualized to that specific patient.
Power Differences
Power differences reflect the imbalance in the patient-provider relationship. Those with power are often not fully aware of the effect that they have on their patients. Some cultural groups may feel powerless when they are faced with institutionalized racism and other forms of privilege that might be enjoyed by the dominant group or the group in power. And again, without knowing about power differences and their effects, you as a therapist can perpetuate health care disparities. Specifically learning about a patient's truth, if you will, formed by their culture, their language, their experience, their history, their sources of care and their power differentials is an integral component in delivering competent care. The patient comes to you with their truth, and we need to figure out what that is, how care can be delivered around that, and incorporate that into our care.
