Editor's note: This text-based course is a transcript of the webinar, Digital Health: Apps and Biometrics For You And Your Caseload, presented by Teresa Fair-Field, OTD, OTR/L.
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
- After this course, participants will be able to identify key digital health tools and apps relevant to occupational therapy practice and their potential applications in client care.
- After this course, participants will be able to list the benefits and challenges of incorporating biometric devices into occupational therapy interventions.
- After this course, participants will be able to recognize the role of digital health technologies in supporting evidence-based practice and improving client outcomes in occupational therapy.
Introduction
Hello, and welcome! Today, we’ll explore how digital health tools and biometric devices are becoming integral in occupational therapy and healthcare. I aim to illustrate how we can leverage consumer-driven health technology to support our occupational therapy objectives and clients' overall well-being. By the end, I look forward to hearing your questions. Whether you’re familiar with some of these tools or they’re completely new to you, I believe there’s much to gain from considering their applications in OT.
Before we dive in, I want to share a brief disclosure: I will discuss specific products and apps available on the market. However, I have no financial or personal ties to these organizations. I intend to provide a snapshot of current digital health solutions.
Incorporating these digital tools can enhance traditional OT interventions in truly practical ways. For example, one of my clients, an individual with chronic pain, found motivation and insight through a wearable that tracked her daily activity, allowing her to self-manage flare-ups better by pacing her activities. On another occasion, a young client with attention challenges found increased focus using a biofeedback app that allowed him to track his breathing and heart rate during therapy. These tools can add tangible, real-time feedback that motivates and empowers clients, often essential for creating sustainable health habits.
Throughout this session, I’ll share similar examples and invite you to consider how these tools can support various therapy goals and client needs. So, let’s get started on how digital health tools can enrich and evolve our work as occupational therapy practitioners (OTPs).
eHealth, mHealth, Digital Health
First, I want to introduce what we commonly call the "ecosystem of digital health." Although this may seem straightforward, it’s a complex and multilayered concept once we delve into its various components. Part of this complexity stems from how these tools initially appeared on the market and evolved into staples in healthcare today (Figure 1).
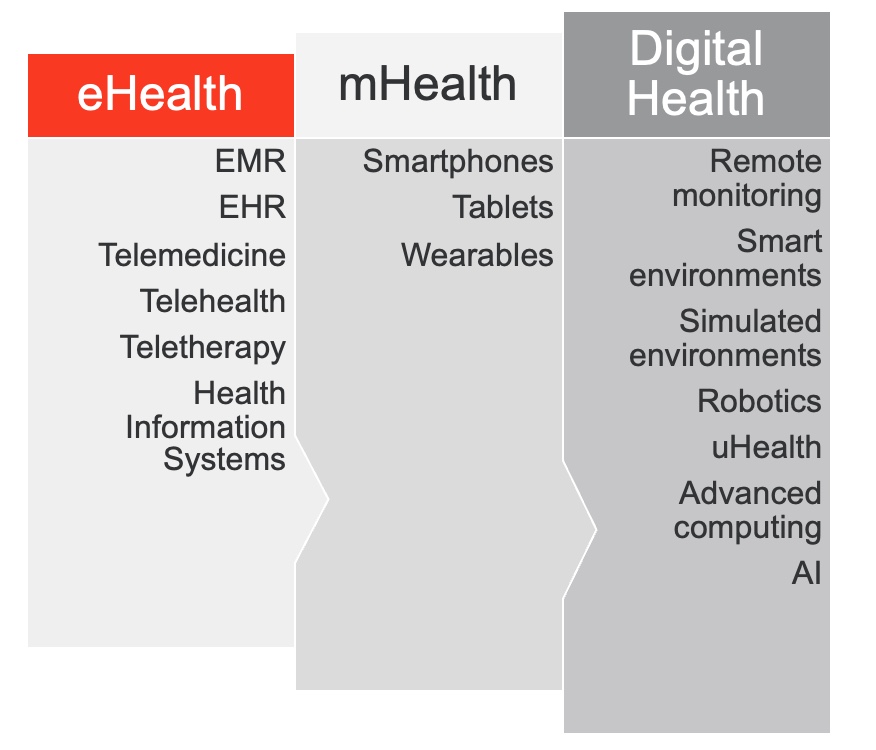
Figure 1. Overview of digital health.
Historically, you may have encountered the term "eHealth," though it may not have fully registered as we were often more focused on specific components that comprise it. At its core, eHealth includes products like the Electronic Medical Record (EMR), Electronic Health Record (EHR), telemedicine, telehealth, and other digital health information systems—particularly the ones larger institutions rely on for comprehensive, integrated care. We quickly became accustomed to these digital systems and their efficiencies, while the term "eHealth" itself received less emphasis.
Then, in the early 2000s, a new branch emerged known as "mHealth" or "mobile health," driven primarily by the widespread adoption of mobile phones. Unlike eHealth, which focuses more broadly on digital health information systems, mHealth targeted consumers directly through their devices, highlighting mobility as its defining feature. Around 2005, the World Health Organization (WHO) recognized mHealth's potential as an accessible, cost-effective way to deliver healthcare, particularly to underserved global populations without robust healthcare infrastructure. For instance, low-cost mobile solutions like text message reminders for medication adherence or mobile-accessible health information services opened up possibilities for addressing specific global health needs, bringing basic healthcare to previously inaccessible areas.
Today, the all-encompassing term "digital health" includes eHealth, mHealth, and other electronic tools that enhance healthcare delivery. Digital health now covers remote monitoring devices—like continuous glucose monitors that automatically relay data to providers—and smart environments, including sensors that detect falls or trigger alerts. It also includes more advanced systems like virtual reality and robotics, which offer simulated therapy or surgical training environments. A relatively new concept in the field is "uHealth" (ubiquitous health), where advanced computing and AI technology make health services available anywhere, seamlessly integrated into daily life.
This evolving ecosystem, with its many digital layers, is expanding our reach and our impact, offering healthcare innovations that are increasingly adaptable and patient-centered. The opportunities in this digital health landscape are extensive, allowing us to rethink how we engage clients in managing their health through cutting-edge technology, whether they’re in rural communities or receiving care right at home.
uHealth
Ubiquitous health, or uHealth, represents a shift toward “healthcare everywhere,” where individuals have continuous access to precise, personalized data to make informed healthcare decisions—often alongside their providers but increasingly independently. The core idea behind uHealth is that health insights and metrics are available anytime, anywhere, supporting individuals in real-time decision-making about their health.
This rise in accessible data has transformed behaviors around health, with many consumers—spanning all age groups—turning to these metrics to make daily lifestyle decisions. For example, people use data to decide what to eat, how and when to exercise, gauge exertion levels, and plan their recovery. Some even track recovery effectiveness, monitoring how their bodies respond after rest or physical exertion and using these insights to tailor future activities.
Of course, not everyone embraces this constant flow of data. Many prefer a more intuitive approach, reminding us that health awareness and feedback can often be observed without any device—just by tuning into our natural signals for free. However, if you’re here, you may lean toward that first group, looking for innovative and actionable ways to leverage and interpret health data. This interest aligns well with what many clients are also doing, often using their devices to monitor aspects of their health that they find meaningful and informative.
As we continue, I’ll share approaches to effectively gathering, interpreting, and incorporating this data within occupational therapy practice, enhancing both the client’s and therapist’s ability to foster wellness. Whether it's tapping into data to enhance physical activities, understand stress management, or track recovery, the possibilities are increasingly diverse and, more importantly, actionable.
Definition of Terms
I’d like to touch on a few terms you may not recognize by their formal names, such as PGHD—Patient-Generated Health Data. PGHD refers to health data recorded directly by patients, often through wearable devices or health apps. This data can be shared with healthcare providers or used independently to help inform clinical care and personal health decisions. PGHD covers a broad range, from activity tracking to vital sign monitoring, with applications growing as wearable tech becomes more sophisticated.
Another emerging concept is mobile rehabilitation, or “mRehab.” With more patients generating their health data, there’s an increasing interest in how we, as therapists, can integrate this data into mobile rehabilitation services. Unlike traditional telehealth or teletherapy, mRehab enables patients to participate actively in therapy remotely through guided exercises, real-time compliance monitoring, and progress tracking—all facilitated by their devices. For example, clients could perform their prescribed exercises with built-in feedback mechanisms, allowing us to monitor adherence and adjust as needed.
Then there’s RPM, or remote patient monitoring, which uses digital tools to gather and send health data to healthcare providers from different locations. Continuous glucose monitoring is one common example, allowing clients and providers to monitor blood glucose levels consistently without needing multiple in-office visits. We’ll explore some additional examples of RPM shortly.
The prevalence of wearable devices raises the question: How often are we—or our clients—using the data these devices generate? And, importantly, how can we guide our clients to use this information meaningfully to improve their health, independence, and even the quality of our documentation? Incorporating wearable data into our notes could lend precision and real-time insights to our session records, supporting evidence-based documentation.
To illustrate, let’s look at findings from the Shandy et al. study from Duke University Health System, which surveyed over 1,300 patients. Impressively, 98% of them owned a smartphone, highlighting how widespread access to health technology has become. The challenge—and opportunity—for us as therapists lies in helping clients harness this data to foster engagement, enhance their care, and achieve long-term health goals.
Wearable Users
Nearly all participants in this study owned at least a smartphone, a figure that’s a bit higher than the North American average, which tends to fall in the high 80s to low 90s, depending on the source. Perhaps even more telling, 60% of these smartphone users also owned a wearable device, with a nearly equal split between popular brands like Fitbit and Apple. The remaining 14% encompassed various brands, indicating a diverse wearable tech landscape.
A few interesting patterns emerged in the demographics of wearable use. For instance, a slightly higher percentage of women than men reported using wearables. Yet, while women tended to wear these devices more episodically, often around fitness activities, men used them more consistently over time. This difference in usage patterns could reflect varying motivations, such as fitness tracking versus long-term health monitoring, which could be relevant in tailoring our interventions or recommendations for wearable use in therapy.
Educational background also appeared to influence wearable adoption, with 41% of high school diploma holders using wearables—a promising statistic suggesting wearable technology’s appeal isn’t confined to those with advanced education. Interestingly, more than half of retired individuals and those with disabilities also reported using wearables, suggesting that these devices offer valuable support for those managing long-term health needs. This cross-sectional engagement highlights wearables as practical tools for diverse groups, each with unique ways of integrating this technology into their daily lives.
These insights can help us, as therapists, think creatively about incorporating wearable data into therapy. For instance, clients who use wearables episodically may benefit from guidance on tracking recovery or activity more consistently, while those using devices long-term might appreciate strategies for interpreting this data to support chronic condition management or everyday wellness.
Reasons for Wearables
The primary reason most participants cited for using wearables was to access fitness-related data. Whether it was tracking steps, heart rate, or calories burned, fitness monitoring emerged as the leading motivation. A close second, however, was the convenience of on-the-go communication features such as phone, email, or text—something that varies by device type since not all wearables are communication-integrated. This difference is largely influenced by device choice; for example, smartwatches like the Apple Watch and certain Fitbit models offer seamless communication integration, while others focus solely on health metrics.
Interestingly, the most common secondary reason for wearing a device was access to broader health information beyond fitness. This includes heart rate variability (HRV), oxygen saturation, body temperature, and ovulation tracking. Sleep data also drew significant interest, with 33% of users citing it as a reason to wear their devices. Sleep tracking has become a major consumer interest, with people eager to understand and optimize their sleep patterns and overall restfulness.
On the other end of the spectrum, fashion was the least cited reason, with only 4.5% of respondents reporting that they wore a device primarily for its style. Notably, of those who valued fashion, 69% were Apple Watch owners, suggesting that Apple’s branding and aesthetics may carry social value for users who appreciate the look as much as the function of their wearable.
Regarding usage patterns, depending on the study, between 42% and 56% of people reported wearing their devices almost around the clock, day and night, with very few days off. This trend reflects the wearables’ growing role in health and lifestyle management and presents exciting potential for continuous health data integration in therapy.
Health Monitoring-Occupation
We’re witnessing the emergence of health monitoring as a meaningful occupation, especially as interest in healthy aging and longevity science becomes mainstream. Many of our clients, their families, and even we, as healthcare providers, are engaging in health monitoring not just as a side activity but as a regular, deliberate practice. This shift is driven by the growing popularity of preventive health and proactive aging strategies, and wearables play a pivotal role by providing accessible, daily insights that empower individuals to make healthier choices.
These wearable devices and apps support people in adopting more active lifestyles, fostering a sense of personal responsibility toward their health. They transform everyday activities—monitoring steps, heart rate, sleep patterns, or hydration—into small, measurable goals contributing to long-term wellness. For many, this kind of monitoring can be a motivator to stay on track, creating a cumulative impact on health behaviors.
From a public health perspective, some researchers suggest that wearables have the potential to address a range of prevalent health issues by making personal health data available on a larger scale. With widespread adoption, the data from these devices could help identify health trends, support early interventions, and encourage health-conscious behaviors across populations. As occupational therapy practitioners, we can play a key role in guiding clients to use these tools in ways that support their daily lives and align with larger wellness goals, making health monitoring an integral, beneficial part of their routines.
The Technology Can Be Used To…
In one study, Ferrera et al. highlight the potential of wearable technology in monitoring the health of older adults, with particular emphasis on supporting aging-at-home initiatives. By allowing for continuous health monitoring, wearables could help reduce hospitalization rates and, ultimately, mortality by identifying changes in health early on. The technology provides real-time alerts for caregivers, notifying them of potential disease conditions or exacerbations that may go unnoticed until they reach a critical stage.
Beyond physical health, wearables enhance mental well-being, encourage healthier lifestyle choices, and support emergency management. For example, wearables can promote daily movement, positively affect mood and cognition, and serve as a lifeline in emergencies by triggering alerts if a fall or irregularity in vital signs occurs. With these capabilities, wearable technology can empower older adults to maintain their independence while enhancing home safety and quality of life. These tools represent a significant opportunity for OTPs to support clients’ autonomy and address physical and mental health needs, fostering a more holistic approach to aging.
Perceived Behavior Change Amongst Older Adults
A recent study by Kaplan et al. (2023) explored perceived behavior change among older adults using wearables, offering intriguing insights into the impact of these devices on health behaviors. In this study, 20 community-dwelling older adults without dementia used a wearable for four weeks, with results showing a generally positive experience. About half of the participants reported eating healthier, nearly half incorporated more physical activity into their day, and a few noted improved sleep patterns.
However, this study measures perceived behavior change rather than actual, measurable behavior change, introducing some limitations. Participants’ responses could be influenced by social desirability bias or the tendency to respond favorably to please the researchers. Additionally, the Hawthorne effect may be at play, where participants alter their behavior simply because they know they’re being observed or studied. These factors can color results, making the data somewhat subjective.
Despite these limitations, the study’s positive findings are still significant. It suggests that older adults perceive wearables as beneficial, with many noting improvements in their daily routines. This positive outlook points to an openness among older adults toward adopting these tools, even if long-term impacts on measurable behavior remain to be determined. For therapists and healthcare providers, these insights hint at the potential of wearables to encourage healthier choices among older adults while also underscoring the importance of further studies to assess sustained, quantifiable behavioral change.
Device Abandonment
An important limitation in studies like Kaplan et al.’s is the “honeymoon period” effect, which captures how many of us respond enthusiastically to shiny new gadgets in the initial weeks. Data collected within these four weeks may reflect the early excitement rather than indicate long-term adoption. Research shows that nearly a third of consumers stop using wearables within six months or significantly reduce their engagement with the data they provide. This tendency has several contributing factors.
The first step in wearable abandonment often begins with a disruption in routine. Once donning the device becomes habitual, even a small disruption can unravel that routine. Many of us may have noticed this with our gadgets—the shift can be surprisingly easy, as these devices are often passive in prompting engagement.
The top reasons for device abandonment include, first and foremost, issues with the device itself. A broken, misplaced, or dead battery can be a significant barrier to continued use. Many wearable devices have a limited lifespan—most users expect a smartwatch to last about two to five years before encountering issues like battery degradation or seeking an upgrade to a newer, more advanced model. Planned obsolescence and evolving tech features contribute to the replacement cycle, often prompting users to shelve the older device.
A second reason for falling out of the wearable habit is a break for a holiday. Many users may not feel inclined to track health metrics while on vacation, although some do the opposite, using their devices to track how much more active they are than usual. Nonetheless, this break can lead to inconsistent use or even permanent abandonment once they return to daily life.
The third most common reason is a simple lapse in habit: the device is taken off for a reason, perhaps to charge it, and is forgotten afterward. Without the nudge to resume the habit, users often let it go, especially if they weren’t deeply engaged with the data. In these cases, it’s not that they actively choose to stop using the device; rather, they don’t miss it when it’s off, leading to a gradual disengagement.
Another intriguing reason for device abandonment is “social comparison fatigue,” especially among users who use social features in companion apps, like leaderboards or shared activity logs. Initially motivating, these metrics can become a source of stress, particularly if users feel they’re constantly falling behind others. Over time, the fun and motivation may wane, leading to a loss of intrinsic motivation and eventually abandoning the device altogether.
These insights reveal that maintaining wearable use requires more than just novelty; it requires a meaningful connection to the data and a routine that consistently adds value to the user’s daily life. For occupational therapy practitioners, this underscores the importance of helping clients find sustained, intrinsic motivation to engage with their devices, which can help them overcome common barriers to long-term use.
Longitudinal Results
Zhang et al. from Boston University looked at a large sample of middle-aged to older adults exceeding the initial "honeymoon" phase to gain more substantial insights into the longer-term impacts of wearables. This longitudinal study analyzed cardio data, step counts, and heart rate data for over 30 days, providing a more realistic view of sustained engagement with wearables.
The study found that, on average, participants wore their devices for about 14 hours daily, typically removing them at night. A key finding was that individuals with a lower resting heart rate and a higher daily step count showed better cardiorespiratory fitness, reinforcing the link between these metrics and cardiovascular health. According to the study, monitoring heart rate and step count with wearable devices could empower users to track their physiological health actively, potentially motivating them to improve cardiorespiratory fitness and cardiovascular well-being.
This study also highlights the close correlation between wearable data and clinically measured metrics. It’s reassuring that many wearables offer data quality that closely approximates traditional clinical assessments, making them a valuable, accessible tool for ongoing health monitoring. We’ll delve further into this by looking at the range of available wearable data and how each type aligns with clinical metrics, bridging personal health tracking and professional healthcare insights.
Wearable Devices and Providers
In a recent study, over 90% of wearable users expressed interest in sharing their data with their healthcare provider—a significant increase from 56% in 2021. This sharp rise reflects a growing patient engagement and desire for collaboration in health management. Interestingly, nearly 87% of these users indicated they prefer providers who actively incorporate wearable data into their care. As occupational therapy practitioners, this trend allows us to engage with our clients’ wearable data, affirming its value in their therapy.
To begin incorporating wearable data meaningfully, we might start by discussing the specific metrics that align with our client’s therapy goals, such as step count, activity levels, or sleep patterns. By identifying metrics that directly impact their daily routines and health objectives, we can guide clients to use their wearables in ways that reinforce their progress. For example, for a client-focused on mobility, we could use daily step data to celebrate progress or identify patterns that might need attention.
Additionally, we can convey that their data matters by making it a routine part of our check-ins and noting any significant trends they’ve observed. A simple acknowledgment, like, "I noticed your steps have increased—have you felt any difference in your stamina?" shows clients that their efforts are being tracked and valued.
For those comfortable with wearable tech, we could even integrate their data into our documentation and goal-setting, using it as objective evidence for progress or areas needing adjustment. As more clients seek out providers who integrate wearable data, these small steps can build confidence and foster a collaborative, data-informed approach to therapy. This approach respects clients’ engagement with their health and demonstrates the role of wearable data as a meaningful and actionable tool in therapy.
In our client activities, a helpful approach is “see something, say something.” When you notice a client wearing a device, start a conversation. You might incorporate it naturally into their occupational profile, initial evaluation, or during the session. For instance, you could say, “I see you’re wearing [mention brand or model if you recognize it]—that’s great! I haven’t seen that one before; which one is it?”
Engaging this way opens up a dialogue about how they’re using their wearable and what data might be helpful for their therapy. You could add, “Let’s take a look at your steps before and after therapy today,” making the wearable part of their immediate, tangible progress. This approach acknowledges their interest and helps incorporate real-time data into your activities, making the device a valuable tool within their therapy experience.
Begin the Conversation With Data
We can start by weaving their data into our sessions to engage clients already using wearables, reinforcing this health-monitoring habit as a meaningful occupation. Simple positive reinforcement can go a long way—something as straightforward as, “Let’s use your wearable to check out your heart rate during this next activity.” By focusing on their device’s data, we can emphasize the personal health value in metrics like heart rate and oxygen saturation, which often go unnoticed in daily life but offer rich insights.
Opening the conversation around wearable data can help clients become more familiar with these metrics and understand their relevance to overall health. For instance, we might say, “Let’s check your app to see how your sleep has been going lately.” This can naturally transition into discussing sleep hygiene—an essential ADL—and broader topics such as energy management and mood. Similarly, oxygen saturation readings can help us discuss respiratory health, opening doors to conversations around sleep apnea, COPD management, or exercise strategies, which could include guided breathing exercises as part of their therapy.
Regarding cardiac metrics, examining resting versus active heart rates can highlight the body’s response to physical activity, linking directly to fitness goals, stress management, and overall wellness. Wearables with cognitive features, like memory or focus games, are also a unique way to incorporate cognitive health into our sessions. If a client is engaging in cognitive exercises on their device, we can ask about their experiences and explore how these activities might support memory, focus, or problem-solving, all of which contribute to their daily life.
By making these wearable metrics a focal point, we empower clients to view their data as more than numbers, supporting their understanding of its significance to health and reinforcing wearables as tools that contribute meaningfully to their well-being and therapy progress.
Wearables As a Caregiving Tool
Wearables hold promising potential as tools for caregiving, though research in this area remains limited. While a few studies have explored wearables from the perspective of caregivers’ usage, little has been done on how wearables can actively support caregiving tasks. However, these devices offer unique ways to monitor and assist with daily care. For instance, a caregiver could adjust the orientation of the wearable’s face, making data easily visible for regular checks. Daily vital readings could help caregivers monitor signs of agitation through fluctuations in heart rate or respiration.
Features like heart rate variability (HRV) might assist with fall detection, while oxygen levels could serve as early indicators of illness. Some wearables, already in studies, suggest that certain physiological changes could signal oncoming illnesses, and features like location tracking and sleep monitoring further support safety and well-being.
As we move into an overview of available wearables and their capabilities, it’s important to note that I have no associations with these companies. The devices are listed alphabetically, all either FDA-approved or in the pipeline, and each provides patient-generated data. Many of them are connected to populations we encounter clinically or perhaps in our personal lives. This field is continually evolving, with new updates in device offerings, evidence, and integration capabilities within healthcare, so today’s insights are truly a snapshot.
With that in mind, let’s explore key discoveries in digital health technology shaping approaches to our most challenging health conditions.
Vitals/Cardiac
- AirStrip® https://www.airstrip.com/ (clinical integration)
- Kardia by AliveCor https://alivecor.com/
- MyTherapy (+med mgmt) https://www.mytherapyapp.com/
- Spire Health Tag https://www.spirehealth.com/patients
- Zio Patch by iRhythm https://www.irhythmtech.com/
AirStrip® is an innovative clinical integration platform that channels patient-generated data directly from mobile devices into clinical systems. It allows physicians to monitor heart rhythms in real time across their caseloads. Another branch, Airstrip OB, focuses on obstetrical data. These tools are designed for direct provider access rather than consumer use, requiring adoption by hospitals or clinical settings. This kind of integration addresses a significant barrier in digital health: harmonizing data systems that often differ across medical environments. For those tracking digital health developments, tools like AirStrip® offer insight into the ongoing effort to incorporate patient-generated data into the broader clinical data stream.
Another familiar tool is Kardia, which is known for its electrocardiogram (ECG) monitoring devices. Kardia offers a couple of devices, including the compact KardiaMobile, a six-lead ECG device slightly thicker than a stick of gum, and the KardiaMobile Card, designed to fit into a wallet with the same shape and thickness as a credit card. These devices go beyond the single-lead ECG found in some smartwatches, detecting a wider range of arrhythmias, such as atrial fibrillation (AFib), bradycardia, and tachycardia, with more precision. While recent FDA-approved tools like Apple and Fitbit’s products can detect AFib with clinical accuracy, they may not detect more complex arrhythmias as Kardia’s devices. This distinction makes Kardia especially useful for those with active cardiac conditions who require detailed monitoring beyond what consumer-targeted wearables provide.
The MyTherapy app stands out in the medication compliance field, particularly because it is free for all users. Unlike many apps that rely on paid tiers, MyTherapy is funded by corporate partners who have made it accessible to the general public. The app’s minimalist interface is a strong feature, especially for older adults, as it avoids overwhelming visual elements, making medication reminders easy to manage with low cognitive demand. Additionally, it syncs with wearables, allowing users to track basic health data like heart rate and activity levels, which they can then share with their providers. The app supports sharing information through printouts or a provider-friendly dashboard if the healthcare professional has a compatible account.
The Zio Patch is also notable, particularly in outpatient or ambulatory settings. This small, wearable biosensor collects continuous cardiac data for clinical diagnostics. Compared to the traditional Holter monitor, which many are familiar with, the Zio Patch is marketed as lighter and more comfortable, with greater compliance reported for long-term use. While Holter monitors are typically preferred for short durations (24 to 48 hours), the Zio Patch’s design enables extended wear—up to a week or more—resulting in higher patient compliance for long-term cardiac monitoring needs.
Each tool demonstrates the expanding scope of wearable technology and its applications, from real-time clinical monitoring to supporting medication adherence and long-term health data tracking. This landscape of wearables provides valuable options for managing some of the more complex and persistent health conditions, with the potential to transform routine health management and provider engagement.
Pulmonary/Respiratory
- ADAMM-RSM https://www.healthcareoriginals.com/professional/
- AsthmaMD https://www.asthmamd.org/
- MyCOPD https://mymhealth.com/mycopd
- NuvoAir Smart Spirometer https://nuvoair.com/
- Propeller Health https://propellerhealth.com/
- Spire Health Tag https://www.spirehealth.com/patients
In the realm of pulmonary and respiratory support, there are a growing number of apps and devices focused on medical-grade respiratory monitoring, distinct from wellness-focused apps like Calm or Breathe, which primarily address mindfulness and stress management. Here are a few notable devices and platforms advancing respiratory health technology:
The ADAMM-RSM family offers respiratory monitoring devices that capture data like respiratory rate, heart rate, temperature, coughing, wheezing, and activity level. Although it’s not yet available for direct consumer purchase, it’s poised to provide detailed pulmonary data, particularly for those with asthma or those interested in respiratory health. This device exemplifies the shift toward comprehensive respiratory-focused wearables instead of general activity monitors.
AsthmaMD and MyCOPD are apps that blend education with limited data integration. For instance, MyCOPD offers Bluetooth integration for wearable devices, a simple interface, and low cognitive demand visuals tailored for older adults. The app provides education on lung anatomy, COPD, medication, and preparatory insights for medical visits. Additionally, users can access data-informed visuals on lung function, suggested exercises, and a digital support community. In MyCOPD, providers can assign tailored educational content to patients, facilitating an individualized patient-provider connection.
NuvoAir offers a digital smart spirometer, marketed as a “virtual first” model that enables at-home care to prevent flares and reduce clinic visits through proactive monitoring. Evidence in Pulmonary Physiology Journal shows bioequivalence between NuvoAir’s home spirometry and clinic-based spirometry, providing confidence in at-home assessments. The platform also includes a virtual visit feature for patients needing clinical follow-up, creating an integrated telehealth solution.
Propeller Health, a branch of ResMed, brings “remote therapeutic monitoring” to inhaler use. A sensor attaches directly to the inhaler, allowing providers to track usage frequency and timing. This goes beyond traditional compliance monitoring, offering insights into the patient’s activity levels and potentially revealing symptom patterns and triggers. This data can support a more detailed provider-patient conversation, enhancing personalized asthma and COPD management.
The Spire Health Tag system offers a unique approach with disposable adhesive sensors that attach to clothing and monitor heart rate, respiration, sleep, and activity. The Spire Tags track metrics without requiring user interaction, making them particularly useful for individuals with cognitive impairments or those who may not tolerate traditional wearables. Each tag has a year-long battery life and is washable and transferable between clothing items. The Spire membership provides ongoing replacements, making it ideal for continuous monitoring, especially in older adults who may wear the same garment consistently.
These wearable monitors embedded in or attached to clothing are advancing rapidly in healthcare and athletic performance. They offer real-time, unobtrusive data collection that is seamlessly integrated into daily life. For providers and caregivers, these options expand opportunities for supporting respiratory health and improving care through unobtrusive, continuous monitoring.
Metabolic Management/ Diabetes
- Blueloop (juvenile) https://blueloop.mycareconnect.com/
- FreeStyle Libre https://www.freestyle.abbott/us-en/home.html
- Sensoria Smart Socks https://www.sensoriafitness.com/
- Tidepool https://www.tidepool.org/
- Zoe https://zoe.com/
The field of metabolic management, particularly for diabetes, is rapidly advancing with various digital health tools and wearables designed to improve monitoring and control. Some tools, like Blueloop, focus on pediatric diabetes, providing young users and their caregivers with a user-friendly interface for logging blood glucose, insulin, and carbohydrate intake. This app supports engagement and self-advocacy in younger children, helping them and their families manage blood sugar levels effectively.
Another well-known device is the FreeStyle Libre continuous glucose monitor (CGM), which offers real-time glucose data via a small sensor worn on the back of the arm. The Freestyle system streams detailed glucose data to healthcare providers, capturing historical information and allowing for customizable alerts, enabling more proactive diabetes management. For those without diabetes, CGMs are increasingly used episodically for metabolic insights, often covered by insurance, to help individuals better understand their glucose response.
The Sensoria Smart Socks represent an innovative tool in the diabetes and athletic industries, providing gait analysis and foot health monitoring. These socks are especially beneficial for people with diabetic or peripheral neuropathy who may need to monitor foot health closely. Sensoria also offers a wheelchair cushion designed for the neuro clinic environment, which collects pressure relief and sitting symmetry data, allowing consumers or providers to view insights via the Sensoria app.
Tidepool is another recently FDA-approved platform that integrates data from various devices to enable automated insulin dosing for type 1 diabetics ages six and up. It collects continuous glucose data from CGMs and uses it to adjust insulin delivery in real-time through infusion pumps, which automatically increase, decrease, or suspend insulin based on predicted glucose values.
Zoe is unique among these tools, blending wellness with metabolic monitoring. It leverages a continuous glucose monitor to assess your blood glucose response to food, a gut microbiome analysis, and other biomarkers to offer tailored dietary recommendations. Zoe focuses on enhancing metabolic health by providing individualized responses to foods, positioning itself as one of the most personalized nutrition apps available.
These wearables and platforms showcase exciting developments in metabolic health management, offering clients and providers versatile and tailored solutions for proactively managing diabetes and metabolic health.
Seizure Detection
- Embrace2 https://www.empatica.com/embrace2/
- Smart Monitor Inspyre https://smart-monitor.com/
In seizure detection, a few notable devices are making strides in providing monitoring and emergency alert capabilities. Embrace, a smart wrist-worn device, requires a medical prescription as it is classified as a medical device by the FDA. It detects seizures by monitoring electrodermal activity, heart rate, and movement and functions as an emergency alert system. When a potential seizure is detected, the device notifies a pre-set list of emergency contacts, ensuring that help can reach the user quickly. Currently, in its second generation, the Embrace2 device requires participants to register, reflecting its clinical-grade focus.
Another option, Smart Monitor’s Inspyre, offers similar seizure detection with the added benefit of geolocation tracking. This feature could be especially helpful for individuals with cognitive impairments, as it alerts emergency contacts if the user leaves a designated safe area. However, users must consider the balance between the advantages of location tracking for safety and the potential privacy concerns related to sharing personal location data.
Both of these devices highlight practical applications in seizure management, with the emergency alert capabilities providing a valuable safety net for users. Additionally, they present use cases for other populations, such as those with cognitive impairments, where monitoring location and movement may support safety and independence within defined boundaries.
Medication Management
- MyTherapy (+med mgmt) https://www.mytherapyapp.com/
- PillPack https://www.pillpack.com/
A few tools stand out in medication management for their ease of use and support for individuals managing complex regimens. PillPack, an Amazon service, is ideal for community-dwelling individuals who need a simplified, dependable way to manage medications. The service pre-packages medications into tear-off packets labeled by dose and time, making it easier to follow medication schedules accurately.
MyTherapy is a medication management app that goes a step further by incorporating features like health journaling and mood tracking, which can be particularly valuable for those taking psychosocial medications. It also provides reminders for medications and doctor’s appointments, helping users manage chronic conditions or mental health needs. MyTherapy serves as a valuable repository of health information, allowing users to track progress and share updates easily with their healthcare providers. This app supports proactive medication management, fostering communication and consistency in treatment plans for those with ongoing health needs.
mRehab, Fitness & Progress
- FitMi https://www.flintrehab.com/
- Pacer https://www.mypacer.com/
- PTPal https://www.ptpal.com/
- Stridekick https://www.stridekick.com/
- Stroke Riskometer https://www.strokeriskometer.com/
Several mRehab programs and tools are designed to support recovery and rehabilitation in engaging, accessible ways. FitMi by Flint Rehab, for example, is a home-based device tailored for individuals recovering from stroke or neurological conditions. It offers gamified, interactive exercises focused primarily on upper extremity improvement and can be used in clinic and home settings. FitMi adapts to the user’s skill level, allowing therapists to track progress remotely and discuss advancements during in-person sessions.
Pacer is another tool that allows integration with various wearables to track metrics like steps, distance, and calories burned. Its interface provides a more streamlined alternative to some native phone interfaces, which can benefit clients who need a simpler setup.
PTPal is an app that connects therapists and patients, facilitating custom exercise prescriptions and reminders. While it’s marketed primarily for physical therapy, it includes resources useful for occupational therapy practitioners. It offers options for task-based rehabilitation with valuable follow-up features.
Stridekick brings a social element to health tracking by allowing families to integrate data and support one another’s wellness goals, creating friendly competition through gamification. This tool could be especially motivating for clients and family members who wish to engage in a supportive health journey together.
The Stroke Riskometer, offered by the Health Stroke Association, is a tool for assessing individual stroke risk. It provides users with insights into their health and potential preventive measures, allowing them to make informed decisions about lifestyle adjustments. Together, these tools provide various options to support rehabilitation, whether through gamified exercises, family engagement, or preventive health tracking.
Sleep Analysis, Monitoring & Tx
- Dreem https://beacon.bio/
- Oura Ring https://ouraring.com/
Several advanced wearable options for sleep analysis provide detailed insights with user comfort in mind. The Oura Ring, now in its fourth generation, is a well-known device that captures high-quality sleep metrics comparable to clinical polysomnography but in the compact form of a ring. It provides data on sleep stages, heart rate variability, and more, all while being discreet and easy to wear.
Another option is the Dreem headband, a high-tech device that collects sleep data and offers audio programs designed to improve sleep quality. These programs include relaxation exercises tailored to help users fall asleep more easily. The Dreem headband provides a different approach by integrating active sleep support alongside data collection, making it suitable for those who prefer a more interactive sleep aid.
Both options offer valuable insights. The choice between them largely depends on individual comfort and whether a user prefers a minimalistic ring or an immersive headband with relaxation features.
Ovulation/Menstruation/Pregnancy
- Ava https://www.avawomen.com/
- Clue https://helloclue.com/
- Flo https://flo.health/
- Ovia https://www.oviahealth.com/apps/
- Natural Cycles (pairs with Oura ring) https://www.naturalcycles.com/oura
Several digital health tools are available for tracking ovulation, menstruation, and pregnancy, each offering unique features and integrations that might appeal based on personal preferences and existing wearables. Many of these apps integrate data from wearable devices, using metrics such as skin temperature and heart rate to provide insights.
For example, Natural Cycles has an integration agreement with the Oura Ring, allowing users to sync temperature and other data seamlessly. This integration provides detailed fertility tracking, with options to log sleep, energy levels, mood, and other personal metrics. Each app has a slightly different interface and may offer specific integrations, so users can select the one that best aligns with their preferences and current wearable devices.
These tools support a personalized approach to reproductive health, making it easier for users to track cycles, understand body patterns, and monitor relevant health data, all while fitting seamlessly into daily routines.
Mental Health & Wellness
- Apollo Neuro https://apolloneuro.com/
- Feel Therapeutics https://www.feeltherapeutics.com
- Headspace https://www.headspace.com/
- MoodPath https://www.psychiatry.org/psychiatrists/practice/mental-health-apps/evaluations/moodpath
- Muse https://choosemuse.com/
- Pocket Rehab (addiction) https://getpocketrehab.com/
The mental health and wellness app space is expanding rapidly, with various options beyond mainstream meditation apps like Calm or traditional telehealth platforms. The following devices and apps offer unique approaches to mental health support, utilizing wearable technology and physiological feedback.
Apollo Neuro is a wearable device stimulating the vagus nerve through gentle vibrations. This may influence relaxation and stress levels. Research on vagus nerve stimulation shows mixed results, but Apollo offers an unobtrusive option for those interested in exploring its potential benefits.
Feel is another wearable focused on tracking physiological signals, such as heart rate variability (HRV) and skin conductance, to measure emotional changes. By monitoring these indicators, Feel aims to help users gain insights into their stress and emotional states.
Headspace, well-known in the meditation app space, is now moving into clinical integrations, bridging the gap between mindfulness practice and clinical mental health.
MoodPath is a mood-tracking app that offers a 14-day assessment to detect symptoms and provides insights based on cognitive behavioral therapy (CBT). It helps users better understand their mood patterns and provides resources for managing emotional well-being.
Muse, a headband for meditation guidance, uses EEG feedback to help users improve their mindfulness practice through real-time brainwave monitoring. It provides an interactive way to enhance meditation and self-awareness.
Pocket Rehab is a digital recovery tool focused on addiction rehabilitation. It connects users with a supportive community and offers various tools to aid in substance abuse recovery, making it a valuable resource for individuals seeking connection and guidance through their recovery journey.
Each app and device offers unique features, allowing users to explore and manage their mental health beyond standard meditation or talk therapy. These apps utilize technology that uses physiological data for a more personalized experience.
Aging/Longevity Science
- Eterly http://eterly.com/
- Inside Tracker https://www.insidetracker.com/
- Welltory https://welltory.com/
These are focused on aging and longevity science, either focusing on using data from your existing wearables to provide and push out information or those that collected blood tests, DNA, etc. There's a lot of movement towards that level of biomarker as well.
Why Not?
Understanding why some smartphone users avoid wearables can help us better support clients interested in using them. Cost is the most common barrier, with 31% of people citing expense as a major factor. Some users find wearables difficult to read, although this can be addressed by viewing data on a larger screen, such as a tablet or a connected app. Other reasons include distrust of the technology, lack of knowledge about wearables, privacy concerns, and, for some, no particular reason.
For clients interested in incorporating wearables, we can offer guidance to help make the data meaningful in their recovery process. By showing them how to interpret metrics or adjust settings to fit their comfort and privacy needs, we can help them maximize the wearable’s benefits and integrate this data meaningfully into their health goals.
Select Your Device Carefully
When choosing a wearable device, starting with a clear purpose is essential. Think about your primary goal and the specific problem you aim to solve—will this device provide what you need to support your health journey? Being intentional about these questions can help avoid the frustration of purchasing a device that doesn’t ultimately fit your needs.
Next, consider whether the device is clinically validated or FDA-approved. You can easily verify FDA approval by looking up the device on the FDA’s website, which can give you extra peace of mind about its safety and accuracy. Equally important is understanding what type of data the device produces. Will this information be genuinely useful for my health or my client?
Another key factor is whether the device fits seamlessly into your daily routine. If it requires too much effort or feels disruptive, it will likely end up unused in a drawer soon. Think about integration options, too—does it work well with other devices or apps you already use? Integration can amplify its utility and make the experience more cohesive.
Privacy and data protection are also significant considerations. Given common concerns around data security, it’s essential to understand how your information is being safeguarded. Additionally, weigh the cost of the device against its benefits. Is it worth the investment for the features it provides?
Finally, the quality of customer support must be assessed. Devices with reliable, responsive support can make a huge difference in your experience, particularly if technical issues arise.
Whether you choose a device for yourself or guide a client in their selection, these considerations will help ensure that wearable technology becomes a meaningful and enduring part of your health routine rather than a quickly abandoned gadget.
Summary/Engage with Digital Health
If digital health interests you, dive deeper into learning opportunities: read current research articles, participate in webinars, or take CEUs focused on digital health advancements. Certifications in specific digital health areas can also add to your expertise, allowing you to adopt and integrate these tools more confidently into your personal life and professional practice.
Privacy and security are critical considerations, so a deeper understanding of these issues is essential. Partnering with digital health startups or innovators can open up new possibilities and keep you at the forefront of advancements in this rapidly evolving field. You can find like-minded professionals by attending conferences focused on digital health, where you’ll also gain insight into emerging technologies and trends. By promoting digital health literacy within your teams, you’ll help create an environment ready to embrace the future of healthcare, fostering a more informed, tech-forward practice for clients and colleagues.
Questions and Answers
Can you provide an example of a short-term goal using wearable data in interventions?
Certainly, the specifics would depend on the population and activity, but wearable data, such as heart rate or steps walked, can be integrated in various ways. For example, I used Apple Watch data with a patient who had a significant brain injury and used a walker. The watch tracked their walking distance in a home health caregiving setting, helping us measure progress tangibly. It’s a flexible tool – your creativity, the client’s needs, and current goals can guide how you use wearable data, whether as a caregiving tool or for client self-tracking.
References
See separate handout.
Citation
Fair-Field, T. (2024). Digital health: Apps and biometrics for you and your caseload. OccupationalTherapy.com, Article 5755. Available at www.occupationaltherapy.com
