Learning Outcomes
- After this course, participants will be able to differentiate the three types of bariatric body types.
- After this course, participants will be able to analyze three safe techniques of manual handling of bariatric patients.
- After this course, participants will be able to identify three environmental risk factors.
Introduction
Today, I want to give an overview of the bariatric body. I will also go over patient care, but first, we need to understand how to handle clients with specific bariatric body types.
What is Bariatric?
- The term ‘bariatric’ is used to describe the field of medicine that focuses on the causes, prevention, treatment, and management of obesity and its associated diseases (Mosby’s Medical Dictionary, 2006).
- The National Institute of Clinical Excellence (NICE) recommends the use of Body Mass Index (BMI) in conjunction with waist circumference as the means for measuring overweight and obesity and determining health risks.
The term bariatric is used to describe the field of medicine that focuses on the causes, prevention, treatment, and management of obesity. NICE, the National Institute of Clinical Excellence, recommends that we use the body mass index in conjunction with weight circumference to classify a person as an obese patient and the different types of obesity.
- Body Mass Index (BMI) greater than 35 kg/m2 plus comorbidities or over 40kg/m2 (NICE 2006) National Obesity Observatory 2010)
- Waist circumference greater than 88cm for women and 102cm for men (NICE, 2014) (Ref: NICE (2014))
We are also going to talk about body mass index. This presentation has a lot of material, so when we come across a critical slide, I will ask that you note it, such as this one. If your body mass index is greater than 35 kilograms per meter squared with comorbidities or over 40 kilograms per meter squared, you are classified as a bariatric patient. The waist circumference criteria are anything greater than 88 centimeters for women and 102 centimeters for men.
- The most commonly accepted and consistent language for identifying and defining bariatric patients has been through the use of the Body Mass Index or BMI.
- The World Health Organization describes people who have a BMI greater than 30 as obese and those having a BMI greater than 40 as severely obese (WHO, 2000).
The most commonly accepted and consistent language for identifying and defining bariatric patients has been through the BMI. The World Health Organization, WHO, describes people who have BMI greater than 30 as obese, and those with a greater than 40 as severely obese.
- Other definitions of bariatric include overweight by more than 100-200 pounds or body weight greater than 300 pounds (Hahler, 2002).
Another definition of bariatric includes being overweight by more than 100 to 200 pounds or body weight greater than 300 pounds.
Relationship Between “A Body Shape Index (ABSI)” and Body Composition in Obese Patients with Type 2 Diabetes
Gomez-Peralta F, Abreu C, Cruz-Bravo M, et al. Relationship between "a body shape index (ABSI)" and body composition in obese patients with type 2 diabetes. Diabetol Metab Syndr. 2018;10:21. Published 2018 Mar 20. doi:10.1186/s13098-018-0323-8
Many of our patients who are obese have diabetes.
- BMI > 35-40
- Waist > 88 cm Females
- Waist > 102 cm Males
- Body Fat:
- Men > 25%
- Women > 3
Those obese with diabetes have a high risk of comorbidities, including decreased sensation and skin integrity.
Important Definitions
- Dynamic Risk Assessment: An undocumented continuous process of identifying hazards and the associated risk and taking steps to eliminate or reduce them in the rapidly changing circumstances.
- Risk Assessment: The overall process of risk identification, risk analysis, and risk evaluation (Ref: HSE Integrated Risk Management Policy, 2017).
Let's go through some crucial definitions because we will discuss all these terms as we move ahead. Dynamic risk assessment is a continuous undocumented process of identifying the hazards and the associated risks and taking steps to eliminate or reduce them in a rapidly changing circumstance. Think about doing a patient transfer. We are constantly evaluating during the process. What is going on with the bedsheets, the bed, IV lines, and the walker? It is not a documented thing but a scene assessment.
The risk assessment is the overall process of identifying, analyzing, and evaluating, which you do before approaching the patient. You will assess what the space looks like, what the environment looks like, and how many people you will need. How many times in our practice do the best-laid plans go sideways? A dynamic risk assessment occurs when you are in the process of doing the transfer, whereas a risk assessment is before the task.
Service User: In the context of this guideline, the term service user is applied to anyone who accesses the services provided by the HSE ( i.e., Hospital patient or client/resident in a community setting. (Adapted from HSE Incident Management Framework, 2018) (^)
TILE means Task, Individual capability, Load, and Environment that we will review.
The term service user in this talk is applied to anyone who accesses the service provided by the HSE (hospital, client, ambulance workers, families, et cetera). Whoever will be around this patient or touch this patient is a service user.
Body Type-Apple
Description
- Apple ascites: weight carried high; abdomen may be rigid
- Apple pannus: weight carried high; abdomen mobile (apron) and hanging down
- Apple android: fat stored around the waist
For apple ascites, the weight is carried high with a rigid abdomen. The weight is carried high in the apple pannus type, but the abdomen is mobile and hangs. Apple android is where the fat is stored around the waist. I want you to visualize a patient. I am picturing men with beer bellies. Even when they lay down, you can see their belly—nothing on their frame moves or changes. Apple pannus is an apron belly, and apple android is fat stored around the waist.
Figure 1 shows the apple body type.

Figure 1. Apple body type. Image: Continued (licensed from Getty Images)
Identifying these different body types is crucial as your handling and transfer techniques will change with each.
Apple Ascites
- High waist to hip ratio
- Unable to tolerate supine and prone position
- Rigid abdomen, restricted chest wall movement, poor ventilation (O2 sats < 90%), poor endurance.
- Associated postural adaptation: hypertrophy of accessory muscles, jugular vein distention, elevated clavicles
Those with an apple ascites shape have a high waist to hip ratio. These patients have trouble tolerating any supine or prone position. Why do you think that is? The rigid abdomen causes restricted chest wall movement, poor ventilation, decreased diaphragmatic activity, and hypertrophy of accessory muscles. They will be very uncomfortable if you want them to lay down in treatment.
- The size of the legs may be relatively normal; intact hip and knee flexion and limited trunk flexion; limited ambulation, difficulty propelling w/c.
- Mobility: Sit up on their elbows and do a flat spin, moves hips closer to the edge of the bed, pushes up the upper body by lowering legs over the edge of the bed.
- May tolerate rolling but may not be able to lay supine for a log roll.
The size of their legs may be relatively normal with intact hip and knee flexion. However, they may display limited trunk flexion, ambulation, and wheelchair propulsion. If their hips and knees are intact, they should be able to walk around. Ask them what they can do and make them use their legs when doing a transfer. Chances are, they have found a way to work around their large abdomen. Again, they may not be able to bend too far forward, have limited ambulation, and have difficulty propelling a wheelchair due to the large abdominal mass.
As far as mobility is concerned, they may be able to prop on their elbows and do a flat spin to bring their hips closer to the edge of the bed. Then, they may be able to push up their upper body and bring their legs over the edge of the bed for you. If you see this body type and they can move their legs up and down while supine in bed, you can instruct them to push up on their arms and spin around. They may tolerate rolling, but they may not be able to lay supine for a log roll.
Apple Pannus
- Soft abdomen
- Belly button is mobile, and abdomen hangs. When abdomen is stabilized, patient tolerates supine position.
Apple pannus, as we said, they've got a softer abdomen.

Figure 2. Example of apple pannus. Image: by FatM1ke, Public domain, via Wikimedia Commons
Here the belly button is mobile, and the abdomen does hang a little bit. When the abdomen is stabilized, the patient can tolerate the supine position. Figure 3 shows a large pannus.

Figure 3. Example of a large pannus. Image: Muybridge, Eadweard, 1830-1904, Public domain, via Wikimedia Commons
In the case of an apple pannus shape, the hips and knees remain intact, and the leg size may be normal. There is also a pannus classification.
- Hip and knee flexion remains intact, and leg size may be relatively normal(1).
- Grade 1 pannus covers the pubic hairline but not the entire mons pubis.
- Grade 2 pannus covers the entire mons pubis.
- Grade 3 pannus covers the upper thigh.
- Grade 4 pannus extends to midthigh.
- Grade 5 pannus extends to the knee and beyond. (2)
The first level of pannus covers the pubic hairline but not the entire mons pubis. The second grade is when covers the mons pubis. Grade 3 covers the upper thigh, the mid-thigh (4), and the knee and beyond (5). Figure 3 shows a grade-four pannus. These clients can, given the parameters, help you or help themselves.
- Position and Transfer
- Able to turn on the side for ventilation and improve diaphragmatic excursion, thus improved ventilation.
- May place the pannus on some pillows for support while in flat side-lying
- Able to ambulate distance.
As far as positioning and transfers are concerned, these clients can turn on their side for ventilation and improved diaphragmatic excursion. You can place the pannus on some soft pillows while lying on their side. Typically, they can ambulate distances.
- Transfer: supine to sit: Some patients of apple pannus distribution use a supine flat spin to perpendicular and sit up to the edge of the bed.
- On/off the bed: Prone entry techniques may include a prone flat spin on the bed or a four-point entry.
Some patients with the apple pannus distribution use a supine flat spin, and they pop themselves perpendicularly to sit up at the edge of the bed. They are the guys who scootch sideways and then prop themselves on their arms to sit up. The easier way for these guys to get on and off the bed is using a prone quadruped technique.
Body Type-Pear
Description
- Pear abducted: weight carried below the waist; tissue bulk between knees
- Pear adducted: weight carried below the waist; tissue bulk on outside of thighs
- Pear gynoid: fat stored around hips
Next, we have pear-shaped bodies, as shown in Figure 4.

Figure 4. Example of a pear body type. ParentingPatch, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
The first kind is the pear abducted. The weight is carried below the waist, and tissue bulk is between the knees. The weight is carried below the waist in the pear-adducted body, and tissue bulk is outside on the thighs. The pear gynoid is where the fat is around the hips.
Questions to ask yourself before we go to the next slide are: Do you think these clients will be to 1)transfer, 2)complete bed mobility, and 3) go from sit to stand? Things to ponder are where they are carrying their weight and what is biomechanically at their hips and lower extremities. Do they have bulk in between the knees or bulk on their hips? We need to do some critical thinking on a patient-by-patient basis. We need to look at what the lower extremity is doing rather than focusing on individual regions.
Pear Abducted
- Very low waist to hip ratio.
- Femurs are in an abducted posture because the majority of tissue bulk is medially located about the thighs and prevents the knees from making contact or midline posture.
- Limitations in hip and knee flexion may be present. In sitting, the individual will present with the legs abducted or spread.
- Able to tolerate supine position.
- Able to breathe since the weight distribution is lower down
Pear abducted have a very low waist to hip ratio, and the femurs are in an abducted position because the majority of the tissue bulk is medially located. There are limitations in hip and knee flexion because of the bulk that they are carrying. The individual will present with legs abducted in a spread-out position in sitting. These folks are okay with a supine position because there are few restrictions in their torso.
- Demonstrate difficulty with rolling secondary to extreme abducted lower extremity posture.
- Rolling is generally an inefficient movement pattern since lifting a heavy leg requires strength possibly not available relative to body mass.
As far as transferring these folks, they demonstrate difficulty with rolling secondary to an extremely abducted lower extremity position. Even with many personnel, rolling will not be an option since lifting their heavy leg is impossible due to their body mass.
- Transfer move supine to long sitting or semi-long sitting (sitting with legs in front) and finally to short sitting over the edge of the bed.
- Equipment implications may require a narrow lower bed and a wider wheelchair.
The way to transfer these folks is supine to long sitting. Guide them into sitting over the edge of the bed. Equipment may include a lower, narrow bed and a wider wheelchair.
Other Body Types
- Other body types can be classified as:
- Proportional: A weight distribution comparable to the person's height
- Anasarca: Severe generalized edema
- Bulbous Gluteal: Excessive buttock tissue with a posterior protruding shelf
There are other body types. Proportional is where a person's weight distribution is comparable to their height. An example would be a tall guy who carries his weight well. Anasarca is where there is severe generalized edema causing an increase in weight because of fluid retention. Bulbous gluteal is where there is a protruding posterior shelf due to the excess buttock tissue. There can be patients who can exhibit more than two body types at once.
Anasarca
- Characterized by severe generalized edema due to build-up of body fluid in the extracellular space and is not removed via the lymphatic system.
- Decreased range of motion of the joints and a shift in the person’s center of gravity towards the knees when seated
- Increased perspiration (i.e., profuse sweating) due to decreased heat dissipation
- Leads to skin tears, shears
The generalized edema is body fluid buildup due to impaired lymphatics. Due to this, the clients have decreased joint range of motion and a shift in the center of gravity towards the knees when seated. They also have increased perspiration due to reduced heat dissipation, leading to skin tears and shearing. We want to be careful with those who are retaining water, especially if there is excessive sweating and folds, as we do not want to hurt them.
Bulbous Gluteal
- Posterior protruding shelf
- Extends beyond the trunk in sitting
Figure 5 shows a bulbous gluteal protruding shelf.

Figure 5. Bulbous gluteal protruding shelf. Image: Continued (licensed from Getty Images)
Looking at this body type biomechanically, you can imagine that this may put increased stress on the lower back. A log roll may not be the best option for this body type. And now, there are many people getting buttock and breast implants. This new change in body biomechanics can cause pain in the upper and lower back. A log roll may not be the best option for this body type.
Risk Factors
When looking at a patient's body type, we also have to consider our body frame and health. Are we overweight or small and underweight? What is the ideal body weight for therapists, nurses, or service staff?
Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training
Garzillo EM, Monaco MGL, Corvino AR, et al. Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training. Int J Environ Res Public Health. 2020;17(14):4971. Published 2020 Jul 10. doi:10.3390/ijerph17144971
This study looked at healthcare workers and manual patient handling.
- Aim: to propose an MPH training model involving interdisciplinary aspects. A scheduled training program was performed with 60 healthcare workers (HCWs) from a hospital in Naples, Italy, providing training divided into three sections (occupational health—section one; physical therapy—section two; psychosocial section—section three) and lasting six hours.
- N= 52 health care workers
The study was on a multi-professional handling training model performed with 60 healthcare workers. The training was divided into three sections: occupational health, physical therapy, and psychosocial. They did this training with a limited staff of different backgrounds for about six hours, and about 52 of them were healthcare workers.
- Method: In section one, a questionnaire about risk perception related to specific working tasks was administered. Section two provided specific exercises for the postural discharge of the anatomical areas most involved in MPH. The last section provided teamwork consolidation through a role-playing exercise.
The first section of the paper focused on risk perception. What do you think is going to go wrong? Section two provided specific exercises for postural discharge of the anatomical areas most involved in manual patient handling, and the last section was about teamwork consolidation.
Let's do some role play. Earlier, we discussed the example of eight different disciplines coming together to transfer this patient. Many health professionals can communicate via eye contact, but imagine an untrained nurse or an intern jumping in to help.
- Outcome: The training program could also be useful for risk assessment itself, as they can examine the perceptions of the specific risk of the various workers and incorrect attitudes and therefore correct any incorrect procedures, reducing exposure to specific risks in the field.
- Result: Training programs could also be useful for risk assessment itself, as they could examine the perceptions of the specific risk of the various workers and incorrect attitudes and therefore correct any uncorrected procedures, reducing the exposure to specific risks in the field.
The outcome was that the training program could also be used for risk assessment. The clinician should examine the perceptions and attitudes of the specific risk of various workers and enhance the incorrect procedures. Who is trained and how much? And not all therapists are adequately trained in bariatric transfers. It was a good pilot study that looked at different disciplines' perceptions.
BE-SAFER
- B: Bariatric Assessment
- E: Equipment assist
- S: Space assessment
- A: Assistive Personnel
- F: Formulation of plan
- E: Evacuation/Execution of plan
- R: Respect for bariatric patient
The acronym BE SAFER is outlined above. B stands for bariatric assessment, where we look at their body type. As a therapist, you are usually the first person on the scene and taking the lead. Next, we will look at what equipment is at our disposal. You could also be working in the community. They might be a new discharge and have a Hoyer lift available. Or, they may show up at an outpatient clinic without any resources.
The "S" is looking at the space. This is vital as we are looking at the size of the patient and the number of people (therapists, family members) involved. How many family members, how many therapists. The equipment is going to be big and bulky as well. There are also hospital trays and tables that are often in the way. It is essential to empty the room as much as possible.
For assistive personnel, you will determine how many are needed and who has done this before? Depending upon experience, you will direct the individual to prevent injury. How many people are experienced and know what they are doing? Formulate a plan and give people roles. Most importantly, we need to look at the evacuation or execution of the plan. How many times does a transfer go as planned? We need to execute the plan and know when to evacuate or abort. Things can go sideways, and we may need to back off and reposition the client.
Most importantly, we have to respect the bariatric patient and make sure that we take care of the client's dignity and listen to their input. Are they in pain, or are you hurting them? Are they comfortable and can help? At the time, we are thinking about load and logistics, but we cannot let their dignity and life take a back seat.
Bariatric Assessment
- Patient’s ability to assist due to medical reasons, fatigue, medications, etc.
- Discuss the task with the patient
- Ensure that the patient is medically stable for the activity
- If the patient has weight-bearing capability, determine the stronger side to transfer
Let's now look at bariatric assessment. You want to document the patient's ability to assist you due to medical reasons, fatigue, or medications. You also want to consider if your patient is drowsy due to a lack of sleep or is not alert. Discuss the task with the patient inside and with the team outside of the room.
You also want to ensure that the patient is medically stable for the activity. You are in charge of the patient in that environment. Trust me, damage control in this situation is way harder than actually executing the transfer. If you are not comfortable with it, and you are the ship's captain, do not do it. The patient may not be following commands or is too tired to move. Think about carrying a five or a six-year-old when they are sleeping. How heavy do they feel? If your patient cannot help, they will be "dead weight." If they are about to bear weight and follow commands, talk to them to figure out a plan.
Determine the strongest side to transfer. The patient can usually tell you the information you need.
- Level of comprehension/cooperation of the task
- Level of assistance: Independent/ Partial assist/ Dependent
- Weight-bearing capacity
- Upper extremity strength
- Height/weight
- Any conditions that may affect the task, i.e., joint replacement, respiratory/cardiac compromise, history of falls, etc.
Do they understand you? Are they cooperative? If a client is saying they do not want to do it or do not feel like it, even a 120-pound client can be a challenge at that point.
What is the level of assistance that they need? Are they independent, partial assist, or entirely dependent on you? What are their weight-bearing capacity and upper extremity strength? Can they push themselves up, or do they have upper extremity injuries? Do they have any conditions that may affect the task, like joint replacements or respiratory or cardiac complications? You have to think about their height, BMI, or waist-hip circumference. I am 5'5" and a half inches tall. When I am with a 6'4" patient, I need to think that if this guy goes down, can I help him? It might be a load beyond your capacity or anybody else who touches the patient.
Risk Factors for Service Workers
- Research conducted by the Health and Safety Executive in the UK on the bariatric patient pathway identified the following risk factors.
- Patient Factors
- Building, vehicle, space, and design
- Equipment and furniture (manual handling)
- Communication
- Organizational & Staff issues
Research conducted by the Health and Safety Executive or the HSE in the UK looked at risk factors for service workers. One is the bariatric patient himself. As we all discussed earlier, things can go sideways. They also looked at the building, vehicle, space, and design. Have you walked into a room and thought, "How am I going to get around this?" Or, "Did anybody think of renting a Hoyer for that client's weight or a specialized wheelchair?" Sometimes, I wonder how the bed even fits through the doorway. Many buildings lack the right equipment.
Then, we have communication factors. For example, has the nursing staff been told by the administration staff that they are expecting a bariatric patient or when they are being discharged? Has the right equipment been ordered? An air mattress is a terrible surface from which to transfer somebody. Many locations also have staffing issues. We all have to deal with real-life situations on the ground and are part of your dynamic risk assessment. When you are in mid-transfer and see that the wheelchair will not work with this patient or the bed does not go low enough for the patient's feet to touch the ground, these are scary situations. Admission information also may be lacking.
Patient Factors
- Challenges to healthcare providers - to provide dignified care that is effective and safe for both the service user and staff.
- Many of these service users, due to their size and difficulty with mobility, require assistance with numerous activities of daily living.
Patient factors, like their size and difficult mobility, can prevent dignified care by healthcare workers. Often they require help for all activities of daily living. Moving from lying to sitting is the first step, and sitting to standing is the next one.
- The more mobility dependent the person is, the greater the risk of injury to those providing their care.
- The person’s ability may be impaired by pain, medication, level of consciousness, and their mobility limitations. Motivation, privacy, dignity, and comfort also contribute to manual handling risks.
The more mobility dependent a person is, the greater the risk of injury to themselves and other people. The person's ability may also be impaired by pain, medication, level of consciousness, motivation, privacy, dignity, and comfort. Your patient may be capable, but he is not feeling comfortable. This is why I said that you should talk to your team outside the door. Your communication and conversation with your patient is a one-on-one private, dignified communication. You tell them that there are five people on the other side of the door and the plan to get them up. You want to know if they are hurting or if they are injured. You want to know how they usually transfer, move their legs, and if they can move their arms. You can say, "Tell me what you need from me so I can make this comfortable and right for you. We do not want to tug pull on you. We want you to work with us, so can you let us know how we can work with you?" They have lived with their body so let them tell you what works for them. I have had many patients that have had a bizarre way of getting from point A to point B, but it works for them.
- Morbid obesity → high risk of falls
- Report joint pain
- Instability
- Decreased mobility
- Functional limitations
- Peripheral neuropathy
Morbid obesity leads to a high risk of falls, joint instability, decreased mobility, limitations in function, and peripheral neuropathy. We talked at the beginning about people with diabetes. Imagine your patient with neuropathy in his feet trying to stand. Does he need grippy socks or other footwear?
- Other conditions that interfere with transfer activities.
- Operative risks
- Abdominal incisions
- Sedation
- Cancer
- Elevated cholesterol
- Type II Diabetes; Gall Bladder ds; Sleep Apnea; OA
Other conditions that interfere with transfers are operational risks, abdominal incisions, sedation, cancer, elevated cholesterol, Type II diabetes, gall bladder disease, sleep apnea, OA, etc. Often, they have numerous comorbidities. You should review their chart, but in case you miss something, you can ask them. They may also have a preference for their mobility. A client may typically roll out of bed on their right side, but in rehab, they cannot as there is a wall. We may need to move the bed to maximize this person's mobility.
- National Institute for Safety and Health (NIOSH): the maximum weight that should be lifted manually by a healthcare worker under ideal conditions is 35 pounds, and the weight limit should decrease as the lift becomes less than ideal (i.e., causing caregivers to reach, twist, or stand in awkward positions when performing a task). (*)
https://bariatrictimes.com/patient-transferring-challenges/
According to the National Institute for Safety and Health, the maximum weight that should be lifted manually by a healthcare worker under ideal conditions is 35 pounds.
Equipment
- The risks associated with manual handling equipment and clinical equipment may include availability, suitability, maximum weight capacity, size, etc.
- The generic manual handling risks associated with equipment include the patient/equipment interface (fit, maximum weight capacity (MWC), size and application) and the equipment/equipment interface (compatibility).
- The air-assisted devices show the lowest biomechanical stresses. (9)
The risks associated with manual handling equipment and clinical equipment may include availability, suitability, and maximum weight capacity and size. And the generic manual handling risks associated with equipment include the patient, the equipment, and the interface. A Hoyer lift may not be enough. Do they have gait belts or straps? Is this equipment suitable for the patient's body type? This is why we spent time learning about different body types. Air-assisted devices show the lowest biomechanical stress in ideal situations.
- Measure the weight capacity of the needed equipment
- Understand the appropriate operation of the needed equipment
- Determine the level of assistance required to safely use the equipment
- To avoid interrupting care, have the correct size equipment easily accessible
Measure the weight capacity of the needed equipment, understand the proper operation, and determine the level of assistance that you require to use the equipment. Is it two-person equipment, or can only one handle it? To avoid interrupting care, you need to have the correct size equipment.
- As found by Hales, de Vries, and Coombs (2017), the size and height of chairs or shower stools had a significant impact on the ability of larger patients to access facilities in a comfortable and independent manner, and there was poor availability of specialized bariatric equipment such as large-sized hospital gowns and anti-embolism stocking. (10)
Hales, de Vries, and Coombs found that the size and height of the chairs or shower stools had a significant impact on larger patients' ability to access equipment comfortably and independently. There was poor availability of specialized bariatric equipment, such as large-size hospital gowns and anti-embolism stockings. I believe every institution should have the appropriate equipment, from socks and stockings to gait belts.
- Appropriate weight-rated and sized equipment.
- A bariatric bed, preferably with an expandable deck, having a power-assisted drive for moving and a built-in weigh scale. An expandable deck allows for the deck of the bed to be pushed inwards to allow the bed to pass through doorways and then increased in width once in a room to provide adequate support for the patient.
Having appropriate weight-rated and sized equipment is imperative. A bariatric bed, preferably with an expandable deck, a power-assisted drive for moving, and a built-in weight scale, are ideal. An expandable deck allows the bed to be pushed inwards to enable the bed to pass through the doorways. And then, once they are in, you can slide it out to allow the patient to have enough room on the bed.
Morbidly obese patients’ experiences of mobility during hospitalization and rehabilitation: A qualitative descriptive study
Hales, C., Curran, N., & de Vries, K. (2018). Morbidly obese patients’ experiences of mobility during hospitalization and rehabilitation: A qualitative descriptive study. Nursing Praxis in New Zealand, 34(1), 20-31.
- Aim: To explore the mobility experiences and needs of morbidly obese patients before and during hospital admission.
- Method: A qualitative descriptive methodology was used where semi-structured interviews with morbidly obese patients were undertaken and content analysis conducted.
The aim was to explore the mobility experiences and needs of a morbidly obese patient via a qualitative descriptive method. They interviewed morbidly obese patients to see their take on their experiences.
- Findings
- 'compromised pre-existing mobility,' with a subcategory of ‘accessing services prior to admission’;
- 'mobilization difficulties during hospitalization,' with a subcategory of 'dissonance between dependency and need for assistance.'
They found compromised preexisting mobility with a subcategory of accessing services before admission. There were also mobilization difficulties during the hospitalization. With a subcategory of dissonance between dependency and need for assistance. They then asked, "If you had issues with mobility before admission, how did that change when you were here?" They asked the same thing with the mobilization piece. "How dependent did you get, and how much more assistance do you need?"
- Conclusion: Bariatric care pathways for the morbidly obese patient need to be developed to take into consideration mobility status and include a comprehensive mobility assessment prior to or on hospital admission for both elective and acute admissions. This would inform the use of appropriate equipment and support patient independence and rehabilitation. Professional development focusing on patient-centered rehabilitation for morbidly obese patients is needed to improve quality of care and patient satisfaction.
They found that bariatric care pathways for morbidly obese patients need to be developed to find satisfactory answers to "how can we help you?" There is a bariatric patient with normal function but now has a fractured femur. Until his traumatic fall 48 hours ago, he was independently living his life. How does that change with the injury and hospitalization? Does he need more assistance, or is he dependent?
They concluded that bariatric care pathways for morbidly obese patients need to be developed to consider the client's mobility status and conduct a mobility assessment prior to or after hospital administration for elective and acute admissions. Ask them, how did you move before this? If they use a cane or walker, ask them if they can bring it from home. Use their equipment if possible and safe. What is the harm? This would support patients as they are used to their equipment. They trust their walker or cane. Professional development focuses on patient-centered rehab for morbidly obese patients to improve the quality of care and patient satisfaction. Ask the patient what they did before hospitalization? How we can bring some of those experiences over to the hospital.
Communication
- Very important!!
- The sharing of timely and appropriate information between disciplines
- The management of service users with bariatric needs over their life expectancy has been described as a journey (Hignett et al., 2007)
We need to listen to what our patients say, and communication is critical. We need to share timely and appropriate information with other disciplines. The administrative staff does not always communicate well. I have worked in skilled nursing facilities, and we did not always know what admissions we would get. Because we did not have a heads-up, the rooms were not prepared. And the management of service users with bariatric needs over the life expectancy has been described as a journey. Often caregivers get burnt out taking care of bariatric patients.
- Effective communication between disciplines, ensuring resources and safe systems are in place are key in managing this journey and reducing the associated risks with managing this client profile.
- Ensure appropriate staffing levels, specialist equipment, and environmental modifications; and hence the more time wards/departments/community services have, the more likely they will be able to plan and manage the service user effectively.
Effective communication between the disciplines ensures resources and safety systems to reduce the risk of managing this patient. We also want to provide enough staffing levels, equipment, environmental modifications, and time with community services. To do this takes a mammoth effort.
Organizational and Staffing Issues and Factors
- Training manual for operational guidance and procedures to lead the process planning assessment (to include resources and training)
- Management of manual handling risks for the care and treatment of these service users.
- Risk assessment procedures for all assisting staff
- Training
- Staffing levels.
- Any equipment provided for the service user must be reviewed regularly to make sure it remains suitable, and that weight limits are not exceeded. A people handling risk assessment must be available to all staff and carers involved in the care of the service user.
A training manual for operational guidance and procedures leads the planning assessment. For example, you get a fancy Hoyer, but nobody knows how to use it. Perhaps, there is an in-service to demo the equipment. However, the Hoyer sits there because the trained staff is not on duty or not available when they need it. We need to manage the manual handling risk for the care team, even those who see them infrequently, like in x-rays. After moving clients onto a table all day long, they have pain. I often ask, "Did you ask the patient if they could help or how they do a transfer normally?" The patient does not always know what you are up to, so you have to talk to them. There is also training, staffing, and equipment on the organizational side. Under every category, we are touching on the same things.
We have covered communication between us and the patient, the team, floor staff, and administration. Imagine going to a patient's room, and they have had diarrhea and are dehydrated and weak. You may be ready with equipment in place; however, no one has told you that today is not a good day to get the client out of bed. What else is within your scope of practice? Many of you said bed mobility and exercises in bed, but remember, he is wiped out. We can look at his skin and go over bedsore prevention, especially after having diarrhea. We can help with pressure relief and roll him to the side if possible. Nursing should be turning him every two hours, but what if he is getting sweaty between that period? We know that nurses are understaffed and overworked, and they may not get to him for three or four hours. Even if a client cannot complete a transfer, that does not mean our role stops there. As therapists, we have multiple roles and responsibilities.
Risk Activities
Then, we have the risk activities.
- Transferring patients to and from different rooms
- Supporting the patient to stand upright
- Picking up the patient, especially if there is only one clinical aide present
- Lifting patients who are confused
- Weighing a patient
Some risk activities include transferring patients to and from different rooms, supporting clients during standing activities, and picking up the patient, especially if only one clinical aide is present. Lifting patients who are confused can be hazardous. Remember, cooperation and cognition are extremely important. OTs get messed up taking them to the bathroom and shower. Even helping the nurses put the patient on the scale can be risky. A wheelchair scale is excellent. If this is not available, the client will need help to step up onto the scale, typically without a device.
- Repositioning a patient in a bed or a chair
- Changing an incontinence product
- Dressing/undressing a patient
- Giving a bed bath
- Applying anti-embolism stockings
(https://www.performancehealthacademy.com/here-s-what-you-need-to-safely-work-with-bariatric-patients.html)
Repositioning a patient or changing an incontinence product can be problematic for the caregiver. Other risky activities are dressing, undressing, giving a bath, and applying stockings. I have difficulty putting stockings on typical clients without edema and heavy legs.
Considerations for Assisting Staff and Caregivers
- Lifting/supporting of legs
- Washing and bandaging of legs
- Positioning the service user on the bed to inspect pressure areas
- Provision of personal care
- Cleaning /inspecting skin within skin folds or under the abdominal apron
- Dressing and grooming
- Assisting with walking; Assisting with transfers
There are many considerations for staff and caregivers, including lifting and supporting legs and washing and bandaging legs. Additionally, many obese patients have lymphatic and skin integrity issues. It is essential to clean and inspect the skin within the folds or under the abdominal apron. Other personal areas include dressing, grooming, walking aids, and assisting with transfers.
- What works for some bariatric patients may not work for another.
- Some patients may require more help (and more force) to perform the task
- Unexpected movements that involve more counteractive force
- Performing the same motions repeatedly without a substantial break can also cause clinical staff to fatigue, RSI
What works for some bariatric patients may not work for others. I like to ask what equipment they use at home. Depending on their ability level, some patients may require more help and more force to perform the task. There are also unexpected moments that involve more counteractive force. It is always imperative to communicate whether the client is obese or not. Performing the same motions repeatedly without a substantial break can also cause staff to fatigue.
- Assuming positions that place stress on the body like reaching above shoulder height, kneeling, squatting, leaning over a bed, bending or twisting the torso while lifting is one of the greatest risk factors for injury.
- *“One leg is approximately 16% of a person’s total body weight. It is recommended that the spinal loading be limited to forces below 3400N, which is about 35 pounds. The weight of a leg of a 350-pound patient would be 62 pounds.”
Individuals with dementia, geriatric, cardiac, or bariatric have unique issues. Patients may not be cognitively there or emotionally or physically able to help us. This can be exhausting for service providers.
We can assume positions that stress the body, like reaching above shoulder height, kneeling, squatting, and leaning on the bed. For example, one leg is approximately 16% of a person's total body weight. Let this sink in when you are lifting a leg. The recommendation for spinal loading should be limited to forces below 3,400 Newtons, which is 35 pounds, and the weight of a leg of a 350-pound patient could be about 62 pounds. How much spinal loading are we going to be doing? There may not be equal assistance when four people do a transfer. Someone may lose their grip or balance. Keep this in mind, and try to recruit as much help as needed.
Environmental Considerations
- Limited in space,
- Uneven floors or surfaces.
- Tripping hazards.
- Environmental Factors
- External door widths and access to/from the property
- Internal door widths
- Weight limits of floors and ceilings where equipment is going to be installed
- Weight limits of domestic furniture, e.g., beds and armchairs
We talked about space, floors, tripping hazards, and door widths. We also need to think about the weight limits of floors and ceilings and where the equipment will be installed.
- Environment Space or vertical/height restrictions, narrow corridors
- Floor uneven, slippery or has varying surface
- Workplace prevents lifting/handling at safe height
- Floor/footrest unstable
- Temperature, humidity, lighting, ventilation unsuitable
- Stairs
- Trailing leads, untidy storage, or other trip hazards
- Weight limits of domestic toilets
- Equipment needs and storage
- Space requirements to allow for service user mobility and for caregivers to work without constraints on posture
Other things we need to consider in the environment are the vertical height restrictions, hallways, floor textures, temperature, lighting, ventilation, et cetera. Sometimes the workplace prevents lifting or handling at a safe height. Additionally, are there stairs or proper storage to allow clear spaces? There can be weight limits on equipment and domestic toilets. Can we use a Hoyer lift or use a walker in the room? Is there space to treat your client, or do you need to maneuver into small nooks and crannies?
Building, Vehicle, Space, and Design
- For effective treatment and care of service users with bariatric needs, adequate space is required to accommodate the person, caregivers, equipment, and furniture.
- For those working in the community and the National Ambulance Service, the size of rooms, door widths, corridors, and stairs in the service user's home may prove challenging if the person needs to be moved or transported to another facility.
Adequate spaces are required to accommodate the person, the caregivers, equipment, and furniture. When we look at the environment, we need to consider all the people involved in that room. We also need to consider things in the community. For example, can your ambulance take the weight of a patient?
Space Assessment
- Evaluate the environment for potential barriers/hazards and remove them, if possible
- Map out a route
- Consider the size of doorways and equipment if the patient handling activity involves traveling.
- Determine the amount of space needed to accomplish the patient handling task, including the maneuverability of equipment and assistive personnel
Get rid of everything you can and have a route or pathway. Also, consider the size of the doorways and the equipment. You do not want to put in all that effort to transfer a patient into the wheelchair, and then the wheelchair does not go through the door, or the wheelchair is not the correct size. You need to plan out the transfer ahead of time and make sure you address all of the details.
Other Considerations
- Ambulance
- Emergency evacuation
- Equipment needs:
- Lifts, hoyers - weight considerations
- All equipment purchased/rented must be accompanied with a certification to state that it has been designed and tested to accommodate the specified safe working load / safe patient weight.
- Lifts, hoyers - weight considerations
We should always talk about emergency evacuation procedures. Does your organization have that provision for a bariatric patient? Are they put in rooms next to the emergency staircases, or are they in a room in the L-shaped hallway around the corner?
Do we need to purchase equipment or rent it? Have they been serviced on time? Have the staff been trained for the equipment? Can they take the weight?
- Number and frequency of bariatric admissions• Equipment purchase cost • Equipment rental cost • blood pressure cuffs, gowns • Equipment storage • Length of stay • Equipment cleaning and maintenance
- Space considerations – door widths, room dimensions, hall widths, toilet with heavy-duty grab rails, large seats, handheld showers.
- Isolation measures
- In the event of an evacuation, locating the bariatric service user ideally at ground floor level or alternatively at a floor level that contains an accessible link corridor to an adjoining building.
As far as the organization is concerned, what is the number of bariatric admissions, and what is the cost? Appropriate blood pressure cuffs, gowns, and equipment weights should be considered. We also need to consider the length of the patient's stay, equipment cleaning and maintenance, and the overall space. Is there a bariatric isolation room? All these considerations need to be addressed by the administration before bringing a patient into the facility.
As the treating therapist, you always listen to your instinct. Damage control is the hardest thing to do. You can get a client into a wheelchair, but how will you get him back into bed after the patient fatigues? What is the plan? Do not hesitate to make that plan because you could be saving another person from getting injured.
Moving and handling care of bariatric patients: a survey of clinical nurse managers
Sara Dockrell, Graham Hurley
- Aim: This study explored the frequency, logistics, and barriers to the provision of bariatric patient-handling care, including equipment availability in acute hospitals.
- Methods: A cross-sectional study, anonymous 24-item questionnaire was used to survey 322 clinical nurse managers.
This research was done with clinical nurse managers and explored the frequency, logistics, and barriers to bariatric patient handling. It was a cross-sectional study that used a 24-item questionnaire. The survey was sent to over 300 nurse managers.
- Results
- Lack of equipment (75%), staff (65.2%), and training (57.6%).
- 11.4% owned all the required equipment.
- Owning equipment provided significantly greater access to a hoist (P = 0.001) and chair (P = 0.032) than renting.
- Only 9.5% reported that rented equipment always arrives on time.
- 74.4% did not have guidelines for caring for bariatric patients, and 46.2% considered this to be a barrier.
Seventy-five percent of the participants talked about the lack of equipment, 65% said their staff and training were inadequate, and 11.4% said the equipment was old and tired in this study. They also found that owning equipment provided significantly greater access to hoists and chairs than renting. Only 9.5% reported that the rented equipment always arrived on time, and 74% of people said they did not have guidelines on caring for a bariatric patient. Those are some massive numbers.
- Conclusions
- The need for education and training and the dissemination of policies and guidelines were identified.
Body Mechanics
- While body mechanic training can help staff prepare for assisting bariatric patients
- Use of specialized bariatric equipment designed for higher weights
- Staff training on mobility and handling procedures and use of specialized equipment
- Patient/resident assessments during the admission process and by nursing staff while in the patient care area
Body mechanic training can help the team prepare for assisting bariatric patients, and anybody on that floor who puts their hands on the patient should be trained. We also need to have specialist bariatric equipment designed for higher weights.
- Development and use of patient/resident bariatric algorithms (flow charts that guide the worker on what to do during care when handling bariatric patients)
- Mobility and handling policies specific for bariatric care
We need algorithms for mobility and safe handling for bariatric care. Let's now look at the TILE abbreviation.
TILE-Task (T)
- Over frequent
- Over prolonged
- Involves the spine
- Insufficient rest/recovery
- Excessive lifting or lowering
- Excessive carrying distances
T stands for the task. What is the task? Working with bariatric clients involves excessive lifting and stress to the spine, long carrying distances, and insufficient rest or recovery. How frequently are you dealing with the load? For example, if you are doing lymphatic drainage, how long are you holding the leg up? If you are helping a patient turn in bed, how long have you been doing this, and is it affecting your back? Are you lifting or lowering? Lowering is tricky as you will not plunk someone's leg or arm down. Then, what are you doing with distances at load?
- Fixed work rate imposed by process
- Too strenuous
- Only achieved by twisting movement of trunk
- Likely to result in sudden movement of load
- Made with body in unstable posture
What is the fixed work rate imposed by the process? Is it too strenuous or only achieved by twisted movement of the trunk or other awkward positions? Is your patient predictable, or are they going to make a sudden move? Is he on a slippery surface or bed? Does the bed fluctuate because of its air, putting the body in an unstable posture? Are they going to pass out on you if you get them at the edge of the bed? You can have them move their arms and pump their ankles to get their blood pumping before sitting up at the bed's edge.
TILE- Individual (I)
- Individual (I) Physically unsuited to task in question
- Unsuitable clothing/footwear/other personal effects
- Inadequate training or knowledge
- Young, old or inexperienced employee
- Pregnant or breastfeeding employee
- Employee physically unfit
The second portion, I, of the TILE acronym is individual. Is the individual physically unsuited to the task? One of the clinicians can also be a mismatch. Other personal characteristics may be unsuitable, like clothing or footwear. Is your patient going to fight you? Does he have sticky socks or an adequate hospital gown?
Is the staff adequately trained or know how to assist? Are they too young, too old, or are they inexperienced? Is the employee pregnant or breastfeeding? It is good to check in with the team before the intervention. "Is everybody okay to do this, or does anybody have any injuries and need to sit this one out?" You should also check in with yourself to ensure you are having a good day. If you can not participate, you may be able to observe and lead the team.
TILE- Inanimate Load (L)
- Too heavy or too large
- Unwieldy/difficult to grasp
- Unstable or contents likely to shift/move unexpectedly
- Manipulated or held at distance from the trunk
- Shape requires bending/twisting of the trunk
- Temperature, contours, consistency, texture unsuitable
"L" stands for the load. Is it too heavy or too oversized? Is the client challenging to grasp? Do you have gait belts or other things to grasp? Your patients should also have something to hold on to because the last thing you want is them holding on to you. When they panic, they will grab the first thing next to them. What is your physical distance from your patient or the space barriers, especially during COVID times? Are you able to reach your patient, or do you have to lean over them?
We also talked about individual and environmental factors like temperature, contours, consistencies, and textures. Are they sweaty? You do not want your hands to slip if your patient is sweaty. They may have body odor and may not be pleasant to transfer after laying in bed all night.
TILE- Personal Load (L)
- Person Load (Patient) (L) History of falls
- Pain
- Drips/drains/catheter
- Infection
- Communication/Sensory
- Skin condition/tissue viability
- Recent surgery
- Amputation
- Muscle spasm
- Weight-bearing
- Joint replacement
- Walking aids
- Physical disabilities
- Psychological/mental health
- Culture/religious considerations
- Day/night variation; Other considerations
This is the load of the patient himself, their history of the falls, and any other issues like pain, drips, drains, catheters, infections, and their communication style. What is the sensation? Do they have neuropathy? Have they had any recent surgeries, or are any planned? Does the patient have a history of muscle spasms? Are they able to bear weight? Have they had a recent joint replacement? What walking aids are available, or what do you need? Did the patient bring their device? Ask the family to get something from home if not. Do they have other disabilities? Are they hearing, cognitively impaired, or have other physical or psychological issues? Are they able to follow instructions? Do they have cultural or religious considerations? For example, they may only want males or females.
Patient Assessment Tools
- Assess and document during the admitting assessment and on a regular basis.
- Change of ability depending on pain, medication, level of consciousness, or mobility limitations secondary to their other medical condition(s).
Assess and document during the admission and on a regular basis. Any change in the mental state, physical state, or health state should be reported. Change of ability depending on pain, medications, consciousness, mobility, limitations, secondary to any other medical conditions should also be documented.
- Assessment Includes:
- Level of assistance for patient;
- Weight-bearing capability;
- Height and weight;
- Other conditions: hip/knee replacements, paralysis, amputations, contractures, osteoporosis, skin/wound conditions, and spine stability.
How much assistance is this patient going to need? How much weight bearing can they do? What is the individual's height and weight? What are the other medical conditions? This should go into your SOAP notes or some information that you can pass on to your colleagues from other disciplines. This information will make everyone's life easier, especially the night shift. Other things to think about are medication schedules or sundowning, affecting performance.
Other Assessment Considerations
- The People Handling risk assessment should consider all the handling tasks that may need to be performed by community staff, including:
- Lifting/supporting of legs
- Washing and bandaging of legs
- Positioning the service user on the bed to inspect pressure areas
- Provision of personal care
- Cleaning /inspecting skin within skin folds or under the abdominal apron
- Dressing and grooming
- Assisting with walking
- Assisting with transfers
People handling risk assessment should consider all the handling tasks that may be needed. We see a lot of complications like sores, blisters, and even gangrene. We need to inspect pressure areas which are not always easy. Lastly, we look at personal care like dressing, grooming, transfers, and ambulation.
Discharge Checklist
- Equipment checklist
- Bedframe and support surface
- Bedside chairs
- Commodes
- Shower chairs
- Portable floor-based lifts
- Gantry lifts
- Wheelchairs
- Walkers
- Bariatric scales
- Stretchers or stretcher chairs
Here is a checklist that you can use if you are doing a discharge from a hospital, skilled nursing facility, or home health.
Workspace Guidelines
Figure 6 shows the recommended guidelines for workspaces.
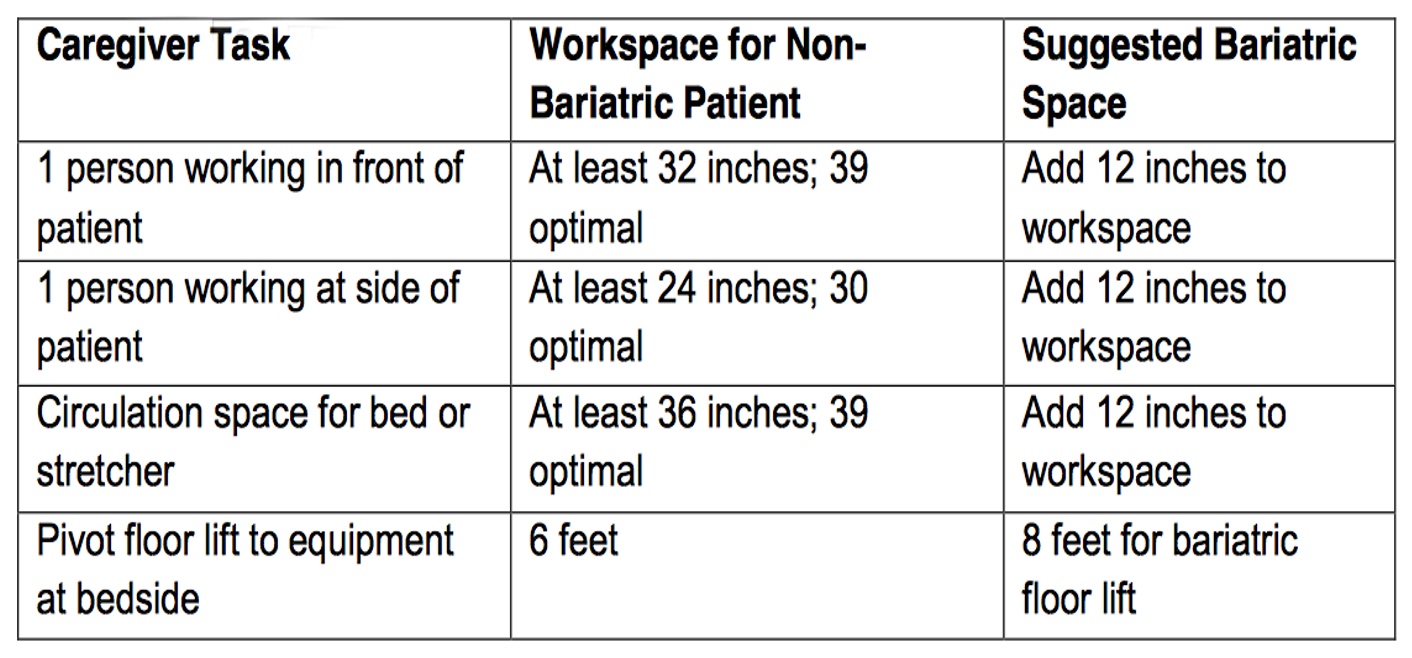
Figure 6. Workspace guidelines.
It is not just the patient but it is also the people involved. How much space do you ideally need around a patient? According to the chart, you want to at least add a foot more to most everything.
Assistive Personnel
- Determine the number of staff needed to perform the task safely
- Routinely obtain the appropriate support staff and equipment/patient handling aids to assist with turning, repositioning, lifting, or transferring the patient
- Encourage patients to assist in their own transfers whenever possible to help reduce risk
You need to figure out how many people, equipment, and patient handling aids you need to assist with turning, repositioning, lifting, or transferring. Ask for help, and do not be shy. You also need to encourage patients to assist if they are able.
Formulation of a Plan
- Establish a plan for the patient handling activity based on the assessment of the patient equipment and space
- Seek input from the patient and family on successful strategies they may have employed to manage safe maneuvers in other settings
- Minimize, if possible, how many actions/transfers are required to accomplish the task
- Consider privacy and comfort issues
- Identify a task leader
- Review the sequence of the task with all assistive personnel
Establish a plan for the patient handling activity. Again, we need to figure out what equipment and space are available. Ask the patient and the family about any strategies they may have employed in the past. You can have them bring in their equipment.
Minimize the steps if possible. How many steps are required to accomplish the task? We need to consider privacy and comfort issues. I keep on reinforcing this but identify a leader. Remember I said it is like a team in the ER. The leader will say, "On my count, you do this." For example, if someone has a bad back, they may be delegated to help with an arm. Review the task sequence with all the assistive personnel before you begin.
Sample Pathway for Service Users with Bariatric Needs
This is a sample pathway for public knowledge released by the HSE and a great resource. I am going to review this flowchart. Before the admission, we will need the information from the pre-assessment clinic, the general practitioner, the ambulance, the height, weight, BMI, body shape, and so on. Even if it is an emergency admission, we will need the same amount of information. What techniques are they going to be using? Do we have the right number of staff? Do we have the correct equipment and PPE? Does the staff need more training? Do we have enough space? As somebody said, their bariatric rooms are at the end of the hallway. That is poor planning. We need to consider bone density, tissue viability, and compatibility when selecting equipment. For all this, they need somebody who knows the job. Others involved can be a manual handling instructor, nurse specialist, dietician, endocrinologist, psychologist, x-ray tech, therapists, etc. Get everybody on board, do your risk assessment, complete all the clinical assessments, and refer to the appropriate doctors as you keep going.
Before the patient even arrives, the team should start thinking about discharge. For example, some equipment for the patient might be on backorder. As the patient is coming in, the discharge committee should start thinking about where they are going. Discharge may be to a community hospital, intermediate care, nursing home, or home, and you would use the same checklist. In addition to the other questions, you would ask about family support and the physical environment. Does somebody live close to the patient should they need help? Does the person have somebody in the house who is capable of helping them? If they need help, how quickly can they get help? This flow chart keeps all of this information in one place.
There is also an area for the National Ambulance Service included in this pathway. On what floor does the patient live? They also need to know the service user's weight, width, and weight distribution. What is their body shape and level of mobility? This information goes on the assessment sheet and OASIS.
Anybody who touches the patient needs to have a risk assessment done. And as I was speaking earlier, we also need to include family members. Do they have people in the home, or are there nearby relatives who can call emergency services if required? Do they have a call light or a button? Even if you are discharging a patient and they can walk out with a walker, that does not mean that he is risk-free. He could be at home, sustain a fall, and not be able to get up. Many patients cannot get off the toilet seat due to Valsalva, loss of BP, low toilets, numbness, missing grab bars, toilet seat height, fatigue, et cetera. They may also have poor leverage mechanics as the seats are not right. The toilet seats can be too narrow, or their feet may be positioned poorly. What about the equipment around them? Their walker may not fit. They also may have rhabdomyolysis, a condition where prolonged muscle compression can leak protein out of the muscles. Imagine how much weight is going through their legs while sitting in that sustained position. There can be a muscle breakdown, and they lose energy due to decreased muscle contraction. Many incidents occur in the bathroom, and the doors are incredibly narrow. Emergency services often struggle to get into the bathroom to evacuate the patient. So writing all this on your assessment goes a long way.
Other Factors
- Other factors Is movement or posture hindered by clothing or PPE?
- Is suitable PPE available and being worn?
- Quantity, availability, and suitability of equipment?
- Staffing levels
- Supervision of manual handling activities
Other factors include clothing and PPE. Is there suitable PPE available and being worn? Again, we are in COVID times and have to be careful. We also need to look at the quantity, availability, and suitability of the equipment, the staffing levels, and the supervision of manual handling activities.
TILE- Execution/Evaluation of the Plan (E)
- Have the leader direct the patient handling activity
- Use proper body mechanics, recognizing that using proper mechanics is not always possible and does not guarantee protection against injuries
- When finished, the team should debrief and identify any modifications needed to improve the procedure
E is for evacuation and evaluation of the plan. There needs to be a leader that supervises proper body mechanics. Proper body mechanics are not always possible and do not guarantee protection against injuries. I have so many examples of personnel (doctors, nurses, morticians, et cetera) injuring themselves because I do consultation work for hospital staff from a physical therapy perspective. All my patients are hospital staff, from ambulance workers to lab technicians. I treat the people who treat the people.
Despite using the correct technique, why do they hurt themselves? What do you think is happening here? Are they going out of their base of support? You are therapists, and you can hurt yourself. What do you think will be that risk factor where you can hurt yourself? One is that the client suddenly changes status or moves on you. There can be a lack of appropriate equipment. Other team members may not be trained, or unexpected events can occur. This brings me back to my first question. How many times do things go as planned? It could be a patient or environmental factor. You can be prepared all you want, but something can still happen. When finished, the team should debrief and identify any modifications you used or could have used.
- Document/revise the patient’s plan of care to describe the components of the patient handling activity
- Obtain feedback from patients regarding their comfort and experiences during the task
Document and revise the patient's plan of care to describe the components of the handling activity and obtain feedback from the patients. How did you think that went? They are your best teachers. They may tell you, "I didn't like when you guys lifted me because you were compressing my chest." Or, "You guys were holding me by my ankle, but there is a blister under my sock." So ask the patient how it went so you can improve your technique.
Respect for the Bariatric Patient
- Use special care in situations that require exposing the patient; close the door or use privacy curtains, and keep the patient covered
- Demonstrate respect and sensitivity to the patient
- Recognize that bariatric patients can experience psychological impact or emotional responses associated with discrimination and prejudice
- Effectively interact with your patients to promote comfort, safety, respect, and compassion
I keep saying this over and over, but it is so important. Be careful exposing the patient, close the door, cover their bed with the curtains, keep the patient covered, and demonstrate respect and sensitivity when you speak with them and when speaking around them. Recognize that bariatric patients can experience psychological impact or emotional responses associated with discrimination and prejudice. Effectively interact with your patients to promote comfort, safety, respect, and compassion. I am also going to add trust. They may be thinking, "I'm 600 pounds. What are these people going to do with me?" You have to establish trust.
Risks to Healthcare Organizations and Staff Who Manage Obese (Bariatric) Patients and Use of Obesity Data to Mitigate Risks: A Literature Review
Highlights
- Patient bodies are not uniform, body shape and weight are unevenly distributed, and there are no convenient handholds to grasp.
- Further challenged by pain levels, immobility, levels of sedation, and lack of cooperation.
- Bariatric patients require more frequent repositioning than normal weighted patients to prevent pressure ulcers, avoid respiratory issues and assist in wound healing.
Highlights of this article are that the patient's bodies are not uniform, and everything is unevenly distributed. You may not have a proper grasp and may be dealing with mobile structures. It can be further challenged by pain, immobility, sedation, and a lack of cooperation. Bariatric patients require more frequent repositioning than normal weighted patients to prevent ulcers, respiratory issues and wound healing. Our challenges on healthcare staff are doubled with these patients.
- An additional 1.5 hours of care per day can be required when managing unconscious obese patients or patients requiring full care compared to normal weighted patients,
- An unconscious patient with obesity may involve up to 5 staff to safely lift or reposition
An additional one and a half hours of care per day can be required when managing unconscious obese patients or those patients requiring full care. An unconscious patient with obesity may involve up to five staff for safety, and I have heard eight people move a patient that was nearly 1000 pounds. It is mind-boggling.
- Bariatric nursing tasks that exceed safe working load limits, such as changing patient dressings involving elevating and supporting limbs weighing approximately 16% of an obese patient’s total body weight. (For a patient with obesity weighing 250 kilograms, changing a dressing may result in supporting 40 kilograms.)
Bariatric nursing tasks can exceed safe working load limits. Remember, 35 pounds is the magic number for safe patient handling. Many bariatric nursing tasks exceed safe working load limits, such as changing a patient's dressing or elevating and supporting limbs. They either need assistance or perhaps the client can assist. Are they able to bend their hip and knee? Or, "I going to turn you. What's the way you do it?"
- A 2007 American study determined that during a 1-year period, obese patients represented less than 10% of all patients; however, 30% of all carer injuries were due to bariatric patient handling.
A 2007 American study determined that obese patients represented less than 10% of the patients during one year. However, 30% of the carer injuries were due to bariatric patient handling. You guys have come to the right place today.
Other Challenges
- conducting physical assessments,
- positioning patients,
- drug dosing and
- accessing appropriate and safe equipment for diagnosis and treatment.
Completing a physical evaluation can be a challenge, including patient positioning, drug dosing, and assessing proper equipment.
- A clinician’s ability to physically assess and diagnose patients with obesity may be ineffective or inadequate due to increased skin folds obscuring affected areas, large abdomens, inability to locate anatomical landmarks, and difficulties in moving larger, heavier body parts.
- BP cuffs, x-ray, MRI machines
A clinician's ability to physically assess and diagnose patients with obesity may be ineffective or inadequate due to the presence of skin folds, large abdomens, and finding anatomical landmarks. Specialized BP cuffs, x-rays, MRI machines, and so on may be required.
Common Bariatric Medical Complications
- Reduced life span by as much as 10 -15 years compared to the non-bariatric population.
- More prone to chronic illness including:
- cardiac disease;
- hypertension;
- respiratory disease;
- diabetes;
- skin conditions, such as dermatitis and ulcers;
- osteoarthritis
What are the common complications that we come across for medical complications for the bariatric patient? Their lifespan is reduced as much as by 10 to 15 years compared to the non-bariatric population.
- More prone to chronic illness including (cont.):
- Stress incontinence;
- Hyperlipidemia;
- Depression; decreased self-esteem;
- Certain types of cancers; and gallbladder disease (Muir & Haney, 2004).
- Obstructive sleep apnea and require assisted breathing devices during sleep so as to address the build-up of excess carbon dioxide in their blood that can further contribute to cardiac issues, such as congestive heart failure.
- Skin; Reduced mobility
Bariatric clients are more prone to chronic illnesses. These secondary illnesses are going to hinder our work with clients. This is why everyone should complete a chart review on each patient. Even if someone says, "Hey, can you give me a hand with this transfer?"
Let me give you an example that happened to me. A nurse needed an extra pair of hands and recruited me for a transfer. This was a larger woman who had fractured her leg. Four or five people were around the bed, trying to transfer her to a gurney using a board. The woman was panicked, and the tenser she was, the more complex the transfer. The team was attempting to slide here with a sheet. I stopped everyone and talked to the patient to get more information. I asked when she broke her leg and how she was walking before that. She had slipped on the stairs and broke her leg the night before. So I determined that she could move everything else other than her leg. I encouraged her to move, and she could scoot herself from one point to the other.
It is your job as a PT to review systems with your patient. Although we may only focus on one aspect of our patient right now, like a cardiac or orthopedic issue, the bariatric condition is in the background unless you deal with patients after a post-bariatric surgery.
Let's Talk a Bit More About the Skin
- Hygiene and toileting: skin folds, large abdomens, and larger, heavier body parts; difficulty in reaching and moving adequately.
- Excoriation, rashes, or ulcers in the deep tissue folds of the perineum, breast, legs, and/or abdominal areas (Gallagher, 1996).
- Fluid retention and poor circulation secondary to heart and kidney failure. Diaphoresis, aka leaky skin → infections and tearing.
Hygiene and toileting are essential when it comes to the skin. We are looking at more chances of rashes, ulcers, sweat, infections, and bacterial growth because they cannot manage their hygiene on some levels. They are dependent on others, and we do not know how good their caregivers are. Are they turning in bed regularly? Are we adequately staffed to do frequent turning? There can be many challenges, and skin cannot be ignored. They may also have fluid and lymphatic issues. There's going to be extravasation of fluid through the skin. Let's not forget that they might have other cardiac and kidney problems, sweat, ulcers, blisters, and diabetic complications. And often, you are the eyes because your patient can't see all of their skin. It's up to you to say, "Do you know you have a rash on your back?" Take care of the skin while manual handling.
- Anti-fungal/ yeast treating medication,
- Assess for assistive devices, OA, general endurance.
During transfers and manual handling, we have to take care of the skin at that point. This is a pretty good resource I have listed.
Handling the Bariatric Patient
Considerations During Transfers
- Cardiac and/or respiratory status: Take into consideration the weight of the chest and its implication on stress on breathing muscles.
- Elevation of head of the bed: Keep it elevated to avoid respiratory distress. If the head of the bed must be lowered, it should be lowered for only a very limited time, monitor the vitals
- Side-lying position: Wedge foam cushions are more supportive and effective than regular pillows, which easily crush under a heavy load.
How do you encourage a tired patient? As far as physical therapy is concerned, it could be any little thing that you can do with them, even if it is turning in bed. Perhaps they can move their knees or assist another way. You can time your visits after sleep or naps. Give them a personal goal to work toward. Start slow, and build up the exercises. Positive encouragement goes a long way. They may not be motivated, and it is hard when your patients give up. We are cheerleaders and have to keep encouraging them. If I have an 80-year-old who does not want to get out of bed after a hip replacement or an obese patient who does not want to get out of bed, my job is the same. I need to get them better, but we cannot force anybody to work with us. You may need to chat with them and find out what their goals are. Have a conversation with them and their family and build a rapport. Sometimes, family members can help you to encourage them.
You can also brighten up the setting. Add some colors, open up the windows, play music, make the activity fun, et cetera. How did they get to this point in their life? Do they need mental health support and a change in their outlook? Play them their favorite music, et cetera.
Always look at their cardiac and respiratory status. Is it stressful for them to breathe? You can elevate the head of the bed to avoid respiratory distress. If the head of the bed must be lowered, it should be only lowered for a very short time.
You can also try a side-lying position with wedge cushions.
VA Algorithm
- The U.S. Department of Veteran Affairs pioneered creating the algorithm specifically designed for bariatric patient handling (Muir & Archer-Heese, 2009). They are comprised of 8 different routines described as follows (Baptiste, 2007):
- Bariatric Algorithm 1: Transfer To and From: Bed/Chair, Chair/Toilet, or Chair/Chair
- Bariatric Algorithm 2: Lateral Transfer To and From: Bed/Stretcher/Trolley
- Bariatric Algorithm 3: Bariatric Reposition in Bed: Side to Side, Up in Bed (see Figure)
- Bariatric Algorithm 4: Bariatric Reposition In Chair: Wheelchair, Chair, or Dependency Chair
- Bariatric Algorithm 5: Patient Handling Tasks Requiring Access to Body Parts (Limb, Abdominal Mass, Gluteal Areas)
- Bariatric Algorithm 6: Bariatric Transporting
- Bariatric Algorithm 7: Bariatric Toileting Tasks
This is a VA algorithm from 2007 outlining these different activities. It looks at the factors of cooperation, comprehension, height, weight, BMI, and comorbidities. Then there are individual algorithms looking at the actual transfers and tasks, the number of staff needed, and the type of equipment.
First, we have transfer to the bed, chair, and toilet for Algorithm 1. Can the patient bear weight, and are they cooperative? If yes, you are in luck and might only need a single caregiver. If not, you will need to gather the team. Do they have upper extremity strength? If yes, then we can use a seated transfer. If they do not, then we need to get the troops ready. If they can partially weight-bear, try a stand pivot transfer using a gait belt. For seated transfer aid, you should use a chair with removable arms. If there is partial weight-bearing, the transfer should be towards the stronger side. Toilet slings and bathing slings are available. You have to make sure there is equipment in place. This is a consideration from chair to chair.
Algorithm 2 is a lateral transfer from bed to stretcher or trolley, so bed to bed. Again, can your patient assist? If they are less than 200 pounds, then use a friction-reducing device. If they cannot help you and are more than 200 pounds, we need to get more caregivers involved. Even if they can assist, be on the safe side, and keep people around you. After a few transfers, you may be able to decrease the amount of personnel. We do not want to catch their skin or any folds in between surfaces for all lateral patient moves. For patients with stage three or four pressure ulcers, care should be taken to avoid shearing force.
Repositioning in bed is the third algorithm. Let the patient do as much as possible and communicate this with the nurses. We want them to use their core and/or extremity muscles, and all staff should be educated on this. When pulling a patient up in bed, the bed should be flat or in the Trendelenberg position so that gravity can assist. Please be very careful of the skin with stage three or four pressure ulcers. Can the patient flex their knees?
Then we have the wheelchair to chair as Algorithm 4. You are asking the same questions. Are they able to assist? How many people do we need around them? Do they have their heavy-duty walker? You need to use your discretion. If the patient falls and is on the floor, we must check for injuries and follow the facility fall protocol. What staff and equipment are available?
You can use these algorithms to help with your decision-making and post them in the room. You can also add client-specific needs like a friction-reducing device, a sling, or four people to assist him using his walker. He may shift from the right side of his body or roll in that direction. Perhaps he like bed rails to assist. Clients know their compensatory strategies. Most of them place their wheelchairs perpendicular to them and use the armrests to pull themselves upright. As the patient improves, these specific guidelines with be an excellent marker to know how they have improved.
Objectives
- The objectives were to increase the knowledge and practice of SPHM principles by healthcare workers in the rehabilitation department and decrease work-related musculoskeletal disorders (WRMDs) the total claims, restricted work hours, and lost workdays.
- Method: training the staff
- Time: 12 week
- Collins, Felicia. Implementing a Safe Patient Handling and Mobility Program to Prevent Staff Injury [DNP Scholarly Project]. Greenville, NC: East Carolina University; July 2020.
The objectives were to increase the knowledge and practice of the patient handling principles by healthcare workers in the rehab department. Now this study was done with the rehab people. They wanted to see how many injuries they had and the claims and lost workdays. First of all, they decided to train the staff for about 12 weeks. This is better than what they had done for four hours or six hours with the nurses. So they did a 12-week safe patient handling and mobility program.
Results
- 90% reduction in restricted work hours
- 91% improvement in lost days over the prior year (PY). T
- Total worker’s compensation claims resulted in a 33% reduction over the PY. Worker’s compensation expense for FY 2020 was annualized to improve by a 95% reduction with the implementation of an SPHM program.
They found a 90% reduction in restricted work hours and a 91% improvement in lost days compared to the previous year. The worker's compensation claims were reduced by 33% from a year earlier. And worker's compensation expense for the first year, 2020, was analyzed to improve by 95%, so train your staff. Train the trainers, movers, and handlers.
Body Mechanics
- Establish a Firm Base of Support:
- To ensure you have adequate balance and power, give yourself a comfortable and athletic stance.
- Keep Your Body in Proper Alignment:
- Align your body so there are no twists or contortions needed from your neck, trunk, or extremities to complete the task. This will ensure that you can efficiently use your strength with as little musculoskeletal strain as possible.
- Remember Lifting Fundamentals:
- Instead of bending at your lumbar spine and generating power from your back, bend your knees into a squat and lift with your legs, glutes, and core.
- Maintain your posture!
- For less strain on your arms during a lift, keep the patient as close to your body and base of support as possible.
As far as body mechanics are concerned, we are all very aware that we need a good base of support, our body in alignment, and not twist or turn neck, back, or extremities. I consult for a mental health hospital. They practice restraints in the UK and often deal with physical assaults. That is a huge dynamic load on the body. No matter how good your body mechanics are, you can never predict what the client will do. As in a car, we get our oil and brakes checked and have seatbelts in place, then we hope for the best.
Specialty Equipment
- Full body slings and specialty slings, such as limb slings and pannus slings
- Wheelchairs in varying widths and depths
- Walkers
- Stretchers with a 1,000 pound capacity and extra width, and also Stretchairs, which are stretchers that have the capability of being adjusted into a chair with armrests and preferably a knee gatch or seat tilt feature
- Stepstool and aerobic bench
- Commode up to 42 inches wide
- Bariatric bedpans
- Bariatric washbasins
- Shower chair or shower stretcher
- Sit-Stand device
- Pressure reducing mattresses
- Trapeze Bar System for over the bed
- A powered tugger to move loaded beds and stretchers
- A low-air-loss mattress for comfort, easy of bed mobility, and prevention of pressure sores
- Visitor Chairs that allow for bariatric patients or bariatric visitors to sit comfortably and safely
I apologize if my equipment slides are primitive because I have not done bariatric care in a while. I am sure there are more products out there. It helps to have a checklist for your home discharge patients. Bariatric clients may also have family members that are overweight. In one incident, a family member sat in a chair with open sides and then got stuck as she was carrying her weight on the outside of the hips. Be mindful of these risks as well. Sometimes it is easier to use chairs without arms, but be careful.
Other Needs
- Other equipment considerations include patient-care supplies. A readily available bariatric cart supplied with the following items allows for a smoother admission and provides better and more dignified care. We encourage such a cart to include the following:
- Larger hospital gowns, pants, housecoats, slippers
- Blood pressure cuffs that will fit around a bariatric arm; Longer needles and catheters
As we are dealing with more body mass, you may need larger gowns, clothes, blood pressure, cuffs, longer needles, and catheters.
SPHM: Safe Patient Handling and Mobility
- Aim: the aims of our study were to explore the frequency of inpatient admissions of patients who are morbid (body mass index [BMI] ≥ 40 kg/m) and super obese (BMI ≥ 50 kg/m), their specific characteristics, and to identify their utilization of hospital services and resources, 30-day readmission rates, safe patient handling equipment, and patient clinical outcomes
- Method: retrospective chart review of adult patients hospitalized at our institution (n = 1670) who are morbidly obese or super obese. We collected and compared data regarding the characteristics of patients, the services and resources used, the use of any special handling equipment, and patient clinical outcomes
- Results: wound care and occupational therapy services were more likely to be required for the patients who are super obese (odds ratio [OR] = 1.49, P = 0.04) than for those who are morbidly obese (odds ratio [OR] = 1.36, P = 0.02). Use of safe patient handling devices was twice as likely for the super-obese group (OR = 2.09, P < 0.01).
Another study explored the frequency of inpatient admissions of patients who are morbidly obese and their specific characteristics. They looked at the utilization of hospital services and assessed if they got readmitted via a chart review of 1600 patients. They found that wound care and OT services were likely to be required. Occupational therapists were instrumental in helping the clients to navigate for ADLs. Wound care, as one would expect, was also a complication. Wherever your patient is, you meet them there. If he is lying down and unable to get up, work with him in this position.
Therapeutic Interventions
- Strengthening: Generalized weakness due to a recent diagnosis
- Requires additional assistance with functional mobility
- Cardiovascular compromised status due to existing or new diagnosis (In addition to generalized weakness)
- Gait rehab (Parallel bars weight restrictions)
There is nothing new that I will say that you guys do not already know. Before we get to their range of motion, we want to work on endurance, diaphragmatic breathing, strength, and mobility.
- Aerobic training: Sitting equipment, stationary bike
- Balance training/Transfer training
- Post-surgical rehab
- Wound care
- Patient education
- Hydrotherapy
Aerobic training is one of the most beneficial parts of the movement because it leads to cardiovascular endurance and creates weight loss. Diaphragmatic breathing mobilizes the gut for less constipation. Bariatric therapy can occur in any setting like post-surgically, for wound care, or a neurological or orthopedic issue. Each client is going to be different. Do they have a stronger side? Their range of motion will be restricted due to body mass and other complications. We have to be cognizant of that because we can only expect a near-normal range. Sometimes we get carried away with wanting 90-degree knee flexion to do a sit to stand, but sometimes that is not possible for your patient to do that due to body mass issues. Providing a higher chair may be a better option.
Clinical Documentation
- Vital signs: in position and activity
- Strength: Pay attention to stronger areas to use them for transfers
- ROM: may vary secondary to soft tissue restrictions and comorbidities
- Posture
- Body type
- Aerobic capacity
- Respiratory status
- Balance
- Skin integrity
Above is everything that we need to document. Do not forget to document things like the door, corners, floor, their technique, et cetera.
Bed Mobility and Transfers
- Trapeze
- Bed rails
- Airflow mattress
- Bariatric beds
- Bariatric wheelchairs/sliding board
- Friction reducing sheets
- Communication between staff/ staff and patient/ staff
- Mechanical lifts: proper body mechanics will only help to a certain extent
- Patient positioned at 90/90 to prevent slipping off.
- Ceiling lifts
- Slings; walkers
These are different tips again for bed mobility and transfers.
Hoists
Ceiling Hoists
- CONs:
- Less flexible, doorways altered, ceiling joists may need to be reinforced
- PROs:
- Occupies less floor space
- Easy operation
- Suitable for long-distance transfer
- Unit may be transferable and detachable.
- Electricity powered and with battery backup
If they are installing ceiling lifts at the hospital or their home, we need to look at the integrity of the device with the environment. Some people will look at that, but it is up to you to see how the device works in the space. It is good to have a checklist. Sometimes you can ask the family to bring in pictures or dimensions, so we know what is going on. Figure 7 shows examples of ceiling hoists.

Figure 7. Examples of ceiling hoists.
Portable Overhead Hoists (Gantry Hoists)
- Portable
- Used for short amount of time
- Folds and fits into the trunk of the car
- https://www.independentliving.co.uk/cp-editorials/bariatric-transfers/
An overhead hoist that is portable is shown in Figure 8.

Figure 8. Example of a portable lift.
Portable overhead lifts can be used for a short amount of time and fit into the trunk of a car.
Mobile Hoists
- Pro: do not require track installation
- Cons:
- Requires more effort from the carer/ clinician
- Not for long-distance transfer: use for w/c or shower chair
- Needs room for maneuver.
- Smooth floor surface: not for carpets/ threshold strip
- Sufficient operating range to lift the person clear of any surface, and perhaps also to pick them up from floor level in an emergency.
- Storage area
Mobile hoists need room because they have gawky legs that need to get under the surfaces and require a storage place.
Repositioning in Bed
- Avoids pressure damage, required for hygiene, ADLs, etc.
- Shown here is a unique powered turning system, which can be used with patients weighing up to 400 kg (63 stone). It consists of two powered rollers and sidebars, which fit to each side of a profiling bed, with a cotton sheet attached between them, resting on a slide sheet beneath. As one roller turns, it winds in the cotton sheet, gently initiating a turning movement. The carer can use their free hand to guide the patient into the desired position.
- Repositioning immobile bariatric patients in bed: a heavyweight repositioning sheet, which remains on the bed, can be used. If combined with an overhead hoist, the repositioning sheet can enable one carer to move and turn a patient safely.
Figure 9 is a repositioning bed.

Figure 9. Repositioning bed.
Make a note of this link because it is an incredible piece of equipment.
Transfer Boards
- Facilitates moves from wheelchair to easy chair, bed to wheelchair, etc.
- The unique shape of these boards enables them to be used for an angled transfer as well as straight side to side.
- Handles may be used by the patients with upper body strength
- Patient must have dynamic sitting balance
- Used with patients on lower end of the obesity scale
I do not have to tell you guys about transfer boards. These can be seen in Figure 10.

Figure 10. Examples of transfer boards.
Standing Transfer Aid
- For patients that can bear weight for short period of time
- Adjustable supportive knee pads.
- Can be used to move a patient from a sitting to standing position or to transfer them in a standing position with the use of the retractable safety belt.
- The foot tray can be removed, allowing the stand aid to be used for walking rehabilitation purposes.
A transfer aid example is in Figure 11.

Figure 11. Example of a transfer aid.
Bariatric Evacuation
Here is an excellent video for bariatric evacuation. This video is for the evacuation of a bariatric client down the hospital stairs and through an emergency exit.
Egress Test (Assess ability to assist in transfer)
- Sit to stand to sit x 3: Test weight bearing
- Marching in place: To test endurance
- Advance step and return each foot
How do you assess if a patient can help you? The Egress Test has them go from sit to stand three times to test their weight-bearing. It also looks to see if they can march in place and tests their endurance. Finally, it looks at their ability to step front and back. This three-step test shows you whether the patient can participate in a transfer.
Transfers
- Evaluate the endurance and strength of your patient. In some cases, the bariatric patient will be able to transfer with minimal assistance, though they may have low endurance.
- Structure the rehab day with scheduled rest breaks so that the patient will have adequate energy to complete the transfers on their own.
- Multiple gait belts attached together to be able reach all the way around them.
Here is a quick cheat sheet. You want to evaluate their endurance and strength and determine your risks. Just make sure that you are transferring them at minimal risk. Structure the day to schedule the rest breaks. You may also need to combine gait belts.
- Bed transfer: The bed surface should be raised, and additional staff may be needed to ensure safety. Use a mechanical lift should be used as needed.
- Patient Education: proper positioning during a transfer-- “nose over toes” (to keep their nose above their toes to help with their balance).
- Push up with their hands from the surface after the surface is raised up.
Does the bed surface need to be raised, or is a lift required? Again patient education and communication are crucial. Encourage them to use their hands if possible, and do not let them just go for a ride.
Moving Bariatric Patient Into Bed
- Before moving the patient into bed, make sure the bed frame can handle bariatric patients.
- Nursing Spectrum suggests that once the patient has a bariatric bed, place the wheelchair against the side of the bed.
- Staff or those helping the bariatric patient should be placed on one of the patient's sides, with one person holding the wheelchair securely down.
- As the bariatric patient is lifted, the feet and thighs should be parallel to the floor.
- The legs should be closed and the elbows at the bariatric patient's side.
- Make sure the sheets are drawn so that those assisting do not have to move the sheets out from under the bariatric patient.
Before moving the patient into the bed, make sure the bed frame is a bariatric model and can handle the weight. You also need to have a bariatric wheelchair right next to it. You can set up the chair at 90 degrees for them to do a stand pivot turn. Somebody should be manning the wheelchair as well. You are on the transferring side of the patient with somebody manning the wheelchair. The last thing you want is for the patient to plunk down in the wheelchair sending it backward. Things can go sideways in so many different ways. As a bariatric patient is lifted, their feet and thighs should be parallel to the floor, and their legs and elbows should be crossed. Make sure the sheets are drawn. The team should shorten their lever arms and bend their hips and knees.
Shower Transfers
- Shower transfer: wet body, slippery surfaces, pose challenges:
- Non-slip surface of the bathroom;
- Transfer the patient to the shower chair with their shoes and some clothing still on.
- After shower: completely dry the surface, and patient: put on clothing/non-slip socks, don the gait belt/s, then transfer
You need all of your precautions in place and make sure everything is completely dry. Use a gait belt and then transfer.
Extra Reading
- https://osha.oregon.gov/edu/grants/train/Documents/va-patient-care-ergonomics-resource-guide-part-1-rev-8-2005.pdf
- https://www.dir.ca.gov/dosh/dosh_publications/backinj.pdf
- https://www.ems1.com/ems-products/bariatric-patient-transport/articles/10-tips-for-transporting-obese-patients-I2RX6fFVpMYnb4Ie/
Here are some additional reading resources.
Summary
The thing about bariatric patients is that we can encounter them in any setting behind a primary diagnosis. What I want you to take home from this lecture is that we are only skimming the surface because we may also be dealing with a primary diagnosis. Know your body types and how your transfers can be made easy.
A risk assessment, TILE guidelines, a space environment evaluation, patient cooperation, and cognition assessment go a long way. Be prepared for unstable loads, and ensure that your team is well trained. Again, talk to your team outside the room, as respect and dignity go a long way. Everything will depend on what equipment and staffing your facility has. The most important thing that you can take home from today is how to communicate and document with the other people on the staff so that they do not hurt themselves.
Questions and Answers
What is the percentage of the bariatric population in the US, UK, et cetera?
This is an interesting question. If you go to Europe or the UK, you will notice that everything is small. Even the king-size bed is not king-size like in the US. The cars are also pretty micro. Whereas in the US, we routinely drive trucks and SUVs. This makes sense because the roads are tiny. I also think that is why they have the double-decker buses here. Another big adjustment is the size of the parking spots. An overweight person trying to integrate into a European lifestyle would be challenging. I have not seen as many overweight people here either. I do not know if it is because of the European diet or the "walk" or "bike" culture. People also prefer to take public transportation because they do not want to pay for parking. Like at my university, my parking spot is £3 a day. Europeans are pushed towards fitness as a necessity. Here is an example. When we go to Sam's Club, we can get those large jars of ibuprofen or Tylenol with 500 pills in a bottle. Here, Tylenol is called Panadol, and the maximum you can get is 16 in a pack. My relatives always ask me to bring the big bottles. I think there is a lot of stress on healthy eating and living. My daughter and I were just talking about that as the portions are smaller and are digested quickly. They also do not have refills on soft drinks; you have to pay for those. Culturally, I think the US and Europe are very different. And people say that Europeans live a little bit healthier than the Brits do.
Is there extra urgency for early mobilization and standing in very heavy patients as mobility can be easily lost?
Yes, especially if they were only household ambulatory to start. We need to work on their endurance as quickly as possible, especially for diagram function. If a person is doing shallow breathing for many hours due to pain or surgery/injury, the diaphragm starts losing tone. The diaphragm begins to go into atrophy mode, whereas skeletal muscles take about 48 hours to lose proteins, and proteolysis starts kicking in. We need to get them up as soon as possible. You can start some weight-bearing if you have a tilt table or a cardiac chair. Use what is available.
References
Muir, M., Archer-Heese, G., (January 31, 2009) "Essentials of a Bariatric Patient Handling Program" OJIN: The Online Journal of Issues in Nursing Vol. 14, No. 1, Manuscript 5.
Gomez-Peralta F, Abreu C, Cruz-Bravo M, et al. Relationship between "a body shape index (ABSI)" and body composition in obese patients with type 2 diabetes. Diabetol Metab Syndr. 2018;10:21. Published 2018 Mar 20. doi:10.1186/s13098-018-032, 3-8
Corbyn, C. & Rush, A. (2010). Challenges of wound management in bariatric patients. Wounds UK. 6(4), 62-71.
Gallagher, S. (2004). Panniculectomy: More than a tummy tuck. Nursing, 34(12), 48-50.
Garzillo EM, Monaco MGL, Corvino AR, et al. Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training. Int J Environ Res Public Health. 2020;17(14):4971. Published 2020 Jul 10. doi:10.3390/ijerph17144971
2018. Guidance on Managing the Manual Handling Issues of Service Users with Bariatric Needs. [ebook] Available at: <https://healthservice.hse.ie/filelibrary/staff/guidance-on-managing-the-manual-handling-issues-of-service-users-with-bariatric-needs.pdf> [Accessed 1 May 2021].
Editor, B., 2009. Patient Transferring Challenges: Bariatric Times. [online] Bariatrictimes.com. Available at: <https://bariatrictimes.com/patient-transferring-challenges/> [Accessed 1 July 2021].
Hwang J, Kuppam VA, Chodraju SSR, Chen J, Kim JH. Commercially Available Friction-Reducing Patient-Transfer Devices Reduce Biomechanical Stresses on Caregivers' Upper Extremities and Low Back. Hum Factors. 2019 Nov;61(7):1125-1140. doi: 10.1177/0018720819827208. Epub 2019 Feb 22. PMID: 30794442.
Hales, C., Curran, N., & de Vries, K. (2018). Morbidly obese patients’ experiences of mobility during hospitalisation and rehabilitation: A qualitative descriptive study. Nursing Praxis in New Zealand, 34(1), 20-31.
Dockrell S, Hurley G. Moving and handling care of bariatric patients: a survey of clinical nurse managers. Journal of Research in Nursing. 2021;26(3):194-204. doi:10.1177/1744987120970623
Laurie D. McGinley and JoAnn Bunke. Bariatric Nursing and Surgical Patient Care. Dec 2008.255-260.https://doi.org/10.1089/bar.2008.9951. Published in Volume: 3 Issue 4: December 6, 2008
McClean K, Cross M, Reed S. Risks to Healthcare Organizations and Staff Who Manage Obese (Bariatric) Patients and Use of Obesity Data to Mitigate Risks: A Literature Review. J Multidiscip Healthc. 2021;14:577-588. Published 2021 Mar 8. doi:10.2147/JMDH.S289676
Collins, Felicia. Implementing a Safe Patient Handling and Mobility Program to Prevent Staff Injury [DNP Scholarly Project]. Greenville, NC: East Carolina University; July 2020.
Jones, Dennis DNP, RN, CCNS∗; Martinez-Amezcua, Pablo MD, MHS†; Pandian, Vinciya PhD, MBA, MSN, RN, ACNP-BC, FAAN, FAANP‡ Utilization of Resources by Patients Who Are Morbid and Super Obese Admitted to a Tertiary Care Center, Journal of Patient Safety: June 2020 Volume 16 - Issue 2 - p 143-148 doi: 10.1097/PTS.0000000000000655
Citation
Pandya, R. (2022). Guide to bariatric transfers and manual handling. OccupationalTherapy.com, Article 5509. Available at www.OccupationalTherapy.com
