Editor's note: This text-based course is a transcript of the webinar, Human-Interfacing Robots For Functional Upper Extremity Rehabilitation, presented by Ashley Gatewood, OTR/L, CSRS.
Learning Outcomes
- After this course, participants will be able to analyze the types of robotic technology currently available in occupational therapy practice in terms of primary drive systems, patient safety, movement planes, and inclusion of cognitive, visual, and motoric activities.
- After this course, participants will be able to apply the ability to determine the specific clinical benefits provided by current robotic technology for integration into treatment planning to support functional activities.
- After this course, participants will be able to evaluate the current available robotic technology capabilities and limitations, including an understanding of the basic drive systems, set-up requirements, kinematic supports, movement facilitations, and environmental considerations in clinical environments across multiple settings.
Introduction
Hello, everyone. Thanks for being here. I will give a history lesson about robots and then proceed to clinical applications.
What is a Robot?
A robot is a device capable of automatically carrying out complex actions. It can articulate motions in multiple degrees of freedom and move freely within itself in a programmable way. A robot can also resemble a living creature capable of moving independently. Whether it moves on wheels, walks, or grasps objects, it navigates through different planes of action. Robots do not have to interact directly with humans; they can operate in industries, build cars, or assist in rehabilitation.
First Robots in History
The first robot in history dates back to 3000 BC. The Egyptians used a human figurine to strike a bell, simulating a clock to indicate the time. This early form of automation was akin to the bell towers we are familiar with today. The Egyptians created their first robot to demonstrate automation and movement. Thus, the concept of robots began long ago and evolved through history.
George Devol developed the first industrial robot in the 1950s in Louisville, Kentucky. His invention, a universal automation device, laid the foundation for modern robotics. Devol and Joseph Engelberger are often considered the fathers of robotics. They began with large-scale robots designed to perform various tasks, primarily in industrial settings. Today, when people think of robots, they often envision the ones that build cars, package products, and handle numerous tasks in manufacturing and logistics.
In 1958, Stanford created the first academic mobile robot, Shakey. Shakey was the first robot on wheels and was named for its clunky, unsmooth movements, which caused it to shake and make a lot of noise.
What is a Rehabilitation Robot?
Today, I want to emphasize the importance of rehabilitation robots and their significance for us as occupational therapists in the clinic. Rehabilitation robots are crucial because they objectively measure the amount and type of assistance provided during therapy. They track and adapt to changes in our motor functions and movements throughout the treatment, whether we are working with different objects or engaging in various training activities.
These robots serve as professional tools, providing physical support by offloading weight from a patient's limb or body part, whether the lower or upper extremities. They also help stimulate muscles and provide proprioceptive input, essential for neuroplasticity. This stimulation helps us jumpstart neuroplastic principles, facilitating better patient outcomes.
First Medical Robots
The first medical robot was introduced in 1980, primarily for surgical purposes, such as hip surgeries. By 1985, more surgical robots emerged, including the Puma 560, which was used in operating rooms for procedures like inserting needles into the brain for biopsies, reducing the risk of human error due to tremors. In 1994, the FDA approved a robotic arm called the Aesop 1000, a voice-controlled endoscopy tool. Over the years, medical robots have become more sophisticated. In 2006, the Mako robot was FDA-approved and became more prevalent in operating rooms. Most notably, in 2000, the Da Vinci robot was introduced and has become the most commonly used surgical robot today, widely recognized even by those outside the medical field.
First Rehabilitation Robots
Rehabilitation robots began with the first patent for a movement apparatus, a machine driven by electric motors to guide and support stepping motions, primarily for the lower extremities. In 1989, the MIT Mantis emerged from the MIT lab. Known today as the bionic in-motion device, the Mantis served as the first prototype, eventually evolving into the advanced bionic devices we see on the market now.
Virtual Reality and Robotics
With the advent of virtual reality (VR) and robotics, technology has become ubiquitous today. Whether through TV or video games, we frequently hear about VR, which immerses users in virtual environments using headsets. VR is increasingly integrated into robotic systems, enhancing their capabilities and applications. This convergence allows for more immersive and interactive experiences in various fields, including rehabilitation, where VR can complement robotic therapy by creating engaging and dynamic treatment environments.
Virtual Reality (VR) vs. Non-Immersive VR (NVR)
There are two types of virtual reality: immersive and non-immersive. Immersive VR involves goggles similar to those used for video games, fully immersing the user into a virtual environment. This type of VR is often used for applications like pain management and promoting smooth movements. However, immersive VR can be visually taxing and may cause issues like vertigo, making it challenging for some patients or individuals in the community.
Non-immersive virtual reality, on the other hand, uses technology to create a computer-generated environment without fully immersing the user. This type is displayed on a TV screen or computer monitor, allowing users to interact with the virtual environment without wearing goggles. In this setup, the user's arms or legs act as controllers, enabling them to engage with the VR content through the robotic system, whether for upper or lower extremity rehabilitation.
Benefits of Virtual Reality Workspaces
The benefits of virtual reality (VR) in rehabilitation are significant, particularly when comparing gamification to traditional functional exercises. While some might view VR as just games, it creates a computer interface that immerses users in a virtual environment, providing valuable visual feedback and enabling multitasking.
VR allows users to translate movements in the virtual world, requiring them to perform specific physical actions to achieve tasks. For example, moving an arm from right to left on the screen translates to real-life functional movements. This process promotes repetition and task-oriented activities, which are crucial for neuroplasticity and recovery in neurological rehabilitation.
Research shows that in traditional outpatient settings, patients may perform only 32 repetitions to facilitate upper extremity recovery. In contrast, VR combined with robotics can facilitate 200 to 300 repetitions within 30—to 45 minutes. This higher activity rate leads to more effective recovery in a shorter time span, which is especially important given the trend of shorter inpatient stays.
Virtual Reality and Rehabilitation
Although from 2017, one of the research articles I referenced remains highly relevant to our current use of virtual reality and robotics in therapy. The study focused primarily on upper extremity rehabilitation, conducting 72 trials. The significant finding was the higher dose of therapy observed in the group using VR and robotics compared to the control group.
This finding underscores the primary takeaway: VR and robotics enable a higher volume of therapeutic activity, which is crucial for improving patient outcomes more efficiently. Given the shorter windows available in inpatient settings, the ability to provide more intensive therapy in a limited timeframe is invaluable. This increased volume of activity helps patients recover better and faster, highlighting the importance of integrating VR and robotics into rehabilitation practices.
Rehabilitation Robotic Landscape
Now, let's break down the rehabilitation robot landscape by looking at typical lower and upper extremities systems.
For lower extremities, you'll often see suspension harness systems like those from Reo and Jacamar, commonly called the Locomote. These suspension robotic leg trainers focus on gait training and achieving reciprocal patterns. The harness provides support to ensure safety and reduce the risk of falls during therapy.
The ARMAO Power is a commonly used robot for upper extremities. This device can perform gravity elimination and is a non-immersive system, with feedback provided on a screen rather than through a VR headset.
On the left, we have the Burt® upper extremity robot, which operates in all functional planes and can eliminate gravity within those planes to meet the patient's needs. On the right is the Bionik device, previously mentioned, which focuses on tabletop activities and emphasizes horizontal movements, such as protraction and retraction. Both devices (Figure 1) are crucial for upper extremity rehabilitation, each serving different functional requirements and therapy goals.

Figure 1. Examples of robotic devices.
The application of robots to deliver therapy represents perhaps the most significant development in rehabilitation since the invention of the pulley. As occupational therapists, we are accustomed to using pulley mechanisms to assist patients with spinal cord injuries or any neurological injuries that require off-weighting the arm to facilitate movement.
Today's rehabilitation robots offer similar advantages. They allow us to off-weight our patients' arms, enabling them to achieve more movement than they thought possible. During passive range-of-motion exercises, patients may feel that their therapist is moving their arm rather than recognizing their own muscle activation. However, when placed in a robotic system, patients can independently realize their movements, which boosts their motivation and participation.
These systems provide numerous benefits, including increased repetitions and enhanced sensory input—tactile, visual, or proprioceptive. This comprehensive feedback helps drive functional gains, making rehabilitation more effective and encouraging for our patients.
Rehabilitation Robotic Landscape Considerations
Again, the key consideration is ensuring that the upper extremity function moves effectively. As we know, the upper extremity is complex and impacts every aspect of our roles, whether children or adults. The arm is a vital and highly intricate part of our body, making it essential to focus on rehabilitation.
Despite its importance, there is a notable lack of research within our field for upper extremities. However, there has been rapid progress in the design of robotic exoskeletons. This growing interest leads to more research and a deeper understanding of the benefits of robotics in therapy. Research indicates that robotic therapy can provide more intense and beneficial outcomes for the shoulder, elbow, and wrist.
Fewer robots are designed specifically for hand therapy due to the intrinsic complexity of hand movements. However, advancements are being made, and we anticipate some innovative devices emerging in the next few years to enhance hand therapy. These developments will significantly contribute to our ability to provide comprehensive and effective rehabilitation for the upper extremities.
Advantages of Rehabilitation Robots
The advantages of rehabilitation robots are numerous, and while it may seem repetitive, it's crucial to emphasize their significant benefits. The most important advantage of robotic systems is their ability to provide intense repetitions without overburdening therapists. A study from last year highlighted that one of the most common injuries among occupational therapists is back injuries. This is understandable, given the awkward positions we often find ourselves in while supporting a patient's neurological shoulder, moving their arm appropriately, or maintaining their posture. These positions can sometimes contort us into what feels like a pretzel, leading to strain and injury.
Robotic systems help mitigate this by allowing us to place patients in a system that eliminates gravity and supports high repetitions and functional movements. Essentially, they act as a second set of hands, enabling us to focus on other critical aspects such as manipulating the shoulder blades, improving posture, and providing additional tactile cues. This multifaceted approach is often challenging on a mat, where our ability to manipulate both the patient's and our own bodies is limited.
Another significant advantage is the motivation factor. Surprisingly, even older patients find themselves motivated by these systems. I recall a personal experience with an 85-year-old patient who initially disliked video games. However, a competitive nature emerged once she started using the robotic system. She became determined to beat her score from the previous day, driven by the tangible sense of movement and progress. She could see and feel her arm moving, which was far more encouraging than being told she had movement.
Rehabilitation robots are also suitable for all levels of mobility. Whether a patient is flaccid or regaining full range of motion and strength, these systems provide the necessary support and strength training. This versatility makes them invaluable in modern rehabilitation, enhancing patient outcomes and therapist well-being.
Rehabilitation Robotic Types and Designs
Let’s now delve into the design features and types of robots available on the market. I won't cover all the available options but will provide a broad overview to help guide your research if you're considering these systems for your clinic or hospital.
There are two main types of robots in rehabilitation: those focused on Activities of Daily Living (ADL) support and those designed for therapeutic purposes.
Figure 2 shows an example of an ADL support robot: the Myomo.

Figure 2. Example of a person using the Myomo. (https://myomo.com/)
This device is essentially a robotic orthotic that patients can wear. It assists with grasping and releasing objects, bending the elbow, and supporting the arm. For instance, as shown in the picture, a patient can use it to hold and cut an orange, facilitating tasks like cooking or other daily activities. Although some of these devices may be bulkier than others, they provide substantial support for completing ADLs.
Examples of therapeutic robots, ARMEO Power and the Burt, are shown in Figure 3.

Figure 3. Examples of the ARMEO Power and the Burt.
Both of these robotic systems can accommodate patients who are fully flaccid or those with a full range of motion. They provide gravity elimination to support various therapeutic exercises. Despite their similar functionalities, these two devices operate on different drive systems, a detail we'll explore further.
This broad overview gives you a starting point for understanding the types of rehabilitation robots available and how they might be integrated into your clinical practice.
Types of Devices
Within rehabilitation robotics, there are different types of devices, each driven by distinct mechanisms. Understanding these variations can help you choose the right robotic system for your clinical needs.
Active devices can move the limbs in various planes. For instance, some upper extremity robots can move in all four planes, while others may be limited to two. The choice depends on the specific requirements of the therapy.
Passive devices can also move the limbs but are designed to resist movement when exerted in the wrong direction, ensuring safe and correct motion patterns.
Haptic devices interface with users through proprioceptive forces and the sense of touch. They provide feedback through vibrations or other tactile sensations, which can help patients understand and correct their movements.
Coaching devices track movement and provide feedback. Many robotic systems have detailed tracking capabilities, offering reports on the range of motion, strength, and overall activity. They can monitor patients' progress through various metrics, such as scores, repetitions, and session usage, allowing therapists to tailor interventions based on detailed data.
These features ensure that therapy is effective and tailored to the patient's needs, providing valuable insights for therapists and enhancing patient outcomes.
Types of Mechanical Design
The mechanical design of rehabilitation robots also varies, with three main types: end effector-based, exoskeleton-based, and planar-based.
End effector-based devices attach to the patient's limb only at the most distal segment, ensuring that the actions are not overly constraining. This design allows for a more natural range of motion, as seen in devices focusing on hand or foot movements.
Exoskeleton-based devices have a mechanical structure that mirrors the skeletal structure of the arm or leg. These robots have multiple connection points for lower extremity devices, such as hips, knees, and feet. This design provides comprehensive support and alignment, facilitating complex movements and rehabilitation.
Planar-based devices, typically end effector-based, move in a specific plane, either one or two. These are generally considered the low-tech side of rehabilitation robots, focusing on simpler, more controlled movements within a single or dual plane. This type of device is useful for targeted rehabilitation exercises that require precise control.
Each type of mechanical design offers unique advantages, allowing for a wide range of therapeutic applications tailored to the patient's specific needs.
Human-Interfacing Drive Systems
Although I am an occupational therapist by trade, I've learned a bit about the engineering aspects to better understand these robots' mechanisms.
Some robots are gear-driven, similar to the gears in a clock. In this design, smaller gears interact with larger ones to create movement, which allows for a significant push force. These robots might appear larger and clunkier, but they still operate smoothly and often include a speed reducer to control the motion.
Another common mechanism is belt-driven systems, which also feature teeth like gears. These systems use belts with teeth to transfer motion, providing a balance of precision and strength.
The most common type of gear used in robots today is harmonic drives. These allow for smoother and more functional movement, allowing robots to perform tasks with greater fluidity and precision. Harmonic drives have significantly enhanced the performance of modern rehabilitation robots, making them more effective in facilitating therapeutic exercises.
The next type of mechanism is cable-driven systems. When we think about cables, we should imagine a pulley system. In these systems, the cables act push-and-pull, creating very smooth movements. Unlike gear-driven systems, cable-driven robots do not have motors or gears; instead, they rely entirely on pulley motion. This design results in exceptionally smooth and fluid movements, almost like floating on a cloud.
Cable-driven systems offer robust movement with minimal backlash and less noise. They provide a calm and smooth motion, which feels more natural and human-like. Just as our arms move freely and fluidly, cable-driven systems mimic this kind of natural movement, making them highly effective for rehabilitation tasks that require gentle and precise control.
Another mechanism used in rehabilitation robots includes the flex and harmonic drives. These systems also incorporate a gear teeth design, enabling them to produce high gear ratios. This design allows for fast movement, making them highly efficient in executing precise and rapid motions. However, the complexity of their gear rotations and the intricacies involved in their manufacturing make these systems more expensive to design and produce. Despite the higher cost, their efficiency and precision make them valuable in applications requiring swift and accurate movements.
Another mechanism you will encounter in our industry is the four-bar linkage system. Unlike other designs, these systems do not involve gears. They can be somewhat bulky and may have pinch points, which could pose a risk or hindrance for patients. However, despite these drawbacks, four-bar linkages are excellent for providing automatic robotic support.
These systems are particularly effective for achieving a passive range of motion across various movement planes and accomplishing high repetitions. For practical understanding, think of riding a bike, which operates on a similar four-bar linkage principle. This mechanism allows for smooth, repetitive motion, making it suitable for certain rehabilitation tasks and prioritizing consistent and repetitive movements.
While not commonly used in upper extremity prosthetics, three other types of mechanisms are worth noting as technology is rapidly evolving. First, direct drive systems are generally weak, bulky, and expensive.
Another mechanism uses hydraulic and pneumatic systems. These use fluid power to generate movement but are also prone to fluid leakage, which can lead to contamination. Because of these issues, they are not favored for upper extremity prosthetics.
Finally, magnetic levitation offers small ranges of motion because the components must remain within the magnetic field. This limitation means that large movements are impossible with magnetic levitation systems, making them less suitable for upper extremity applications. While these technologies are not currently prevalent, advancements may change their relevance.
Main Movements (Degrees of Freedom) of the Upper Extremity
- Arm flexion/extension
- Arm adduction/abduction
- Arm internal (medial)/external (lateral) rotation
- Elbow flexion/extension
- Forearm pronation/supination
- Wrist flexion/extension
- Wrist adduction (ulnar deviation)/abduction (radial deviation)
- Hand grasp/release
The main movements we observe in the upper extremities are numerous, reflecting the arm's complexity and wide range of motion (Figure 4).
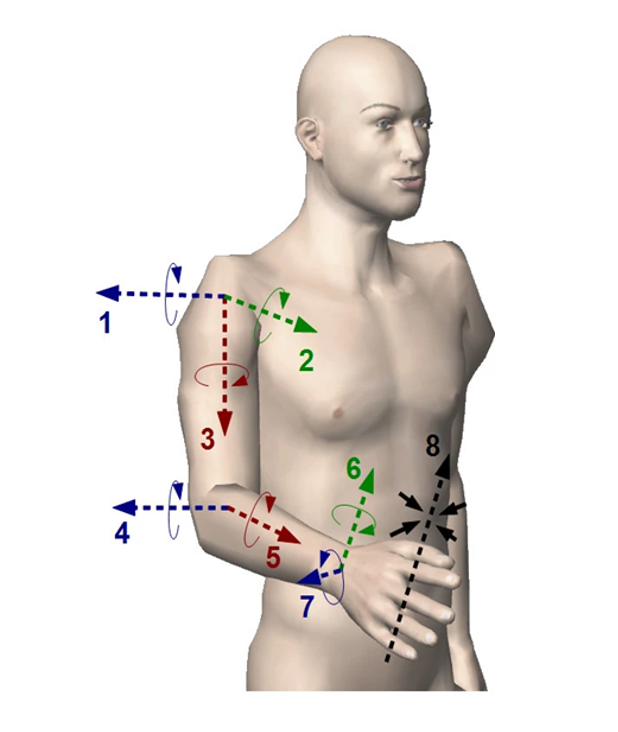
Figure 4. Main movements in the upper extremity.
Our arm's degrees of freedom include the shoulders, elbows, hands, and wrists. Specifically, we look at movements such as arm flexion and extension, arm abduction and adduction, external and internal rotation, elbow flexion and extension, forearm pronation and supination, wrist flexion and extension, wrist abduction and adduction, and, crucially, grasp and release.
Understanding these movements is essential when evaluating the capabilities of different prosthetic systems. The hand, in particular, remains an area of rapid development. Over the next few years, we anticipate significant advancements in prosthetic devices that better mimic natural hand movements. Some current devices already incorporate hand movements, primarily focusing on grasp and release and, in some cases, supination and pronation.
As technology progresses, we expect these devices to become even more sophisticated, enhancing the intrinsic functionality of the hand. This prosthetic evolution promises to improve the range of motion and dexterity available to users, making the devices more effective and lifelike.
Human Arm- 7 Degrees of Freedom (DOF)
As shown in Figure 5, there are seven degrees of freedom in different planes.
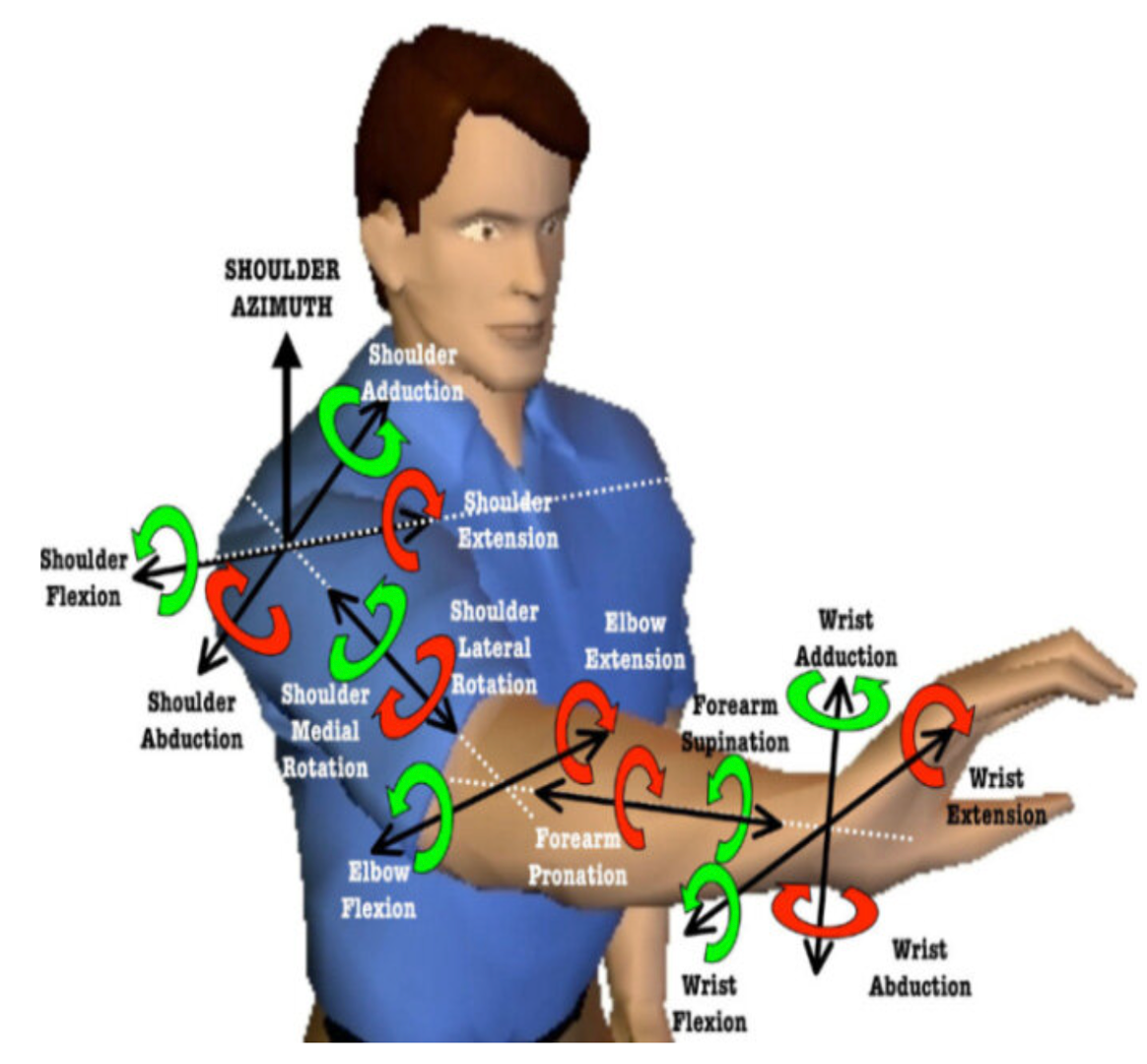
Figure 5. Illustration of the degrees of freedom in an upper extremity.
This gives a human picture of what it means.
Main Movements (Degrees of Freedom) of the Upper-Extremity Translation to Robotics Challenge
We're translating the human arm into robotics as shown in Figure 6.
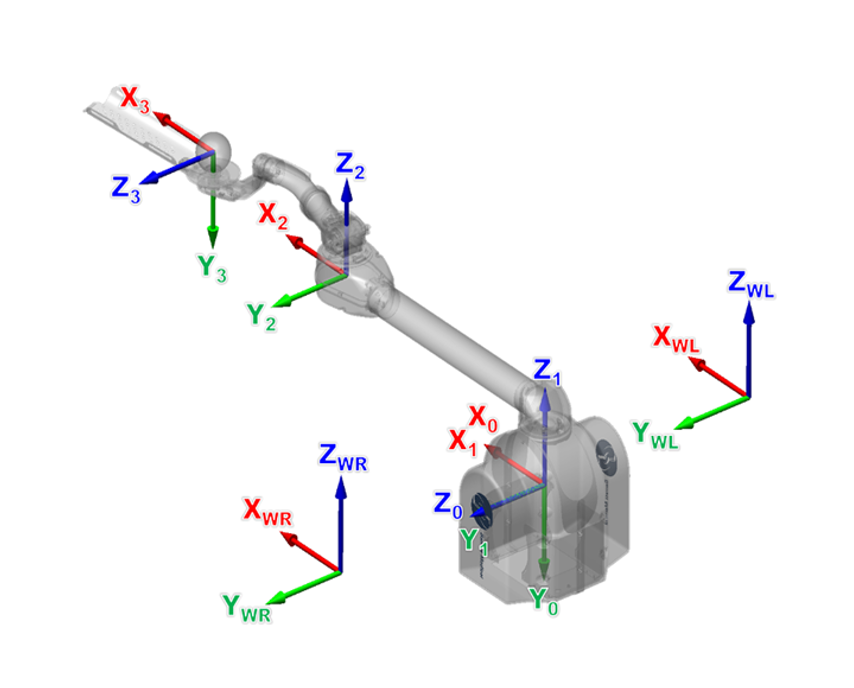
Figure 6. This illustration shows the translation of the degrees of freedom to the Burt. (Barrett Technology)
The Burt can facilitate nearly every aspect of arm movement. It's free and not bulky in that sense.
Movement Planes
The arm can move freely throughout the planes of movement. Specifically, with the Burt upper extremity robot, we have two degrees of freedom at the shoulder and one at the elbow. In reality, the shoulder has four degrees of range of motion, so the robotic system can be adjusted to closely mimic natural movement. This flexibility allows us to fine-tune the range of motion, though it must sometimes be limited for safety reasons.
It is important to balance maximizing the range of motion and ensuring safety. Given the range of movements we can achieve, it's crucial to consider positioning and support for the patient. The challenge lies in making all these motions happen while ensuring the robot supports the patient in the best and safest way possible. This requires accounting for factors like subluxation, impingement, and pain.
Most robots on the market today can achieve a variety of planes of movement. For instance, the Burt can operate in all five planes, including the parasagittal plane. Robots designed for gravity elimination can operate in all four primary planes, though tabletop models are limited to the transverse plane. When selecting or using systems in your clinic, consider the movement planes needed for each patient. This helps decide which system to use based on the specific movements the patient needs to work on, streamlining the treatment process.
What Movement Planes Do Robots on the Market Have?
I've broken down the movement planes to give you an idea of the most common robots you'll see in clinics today (Figure 7).
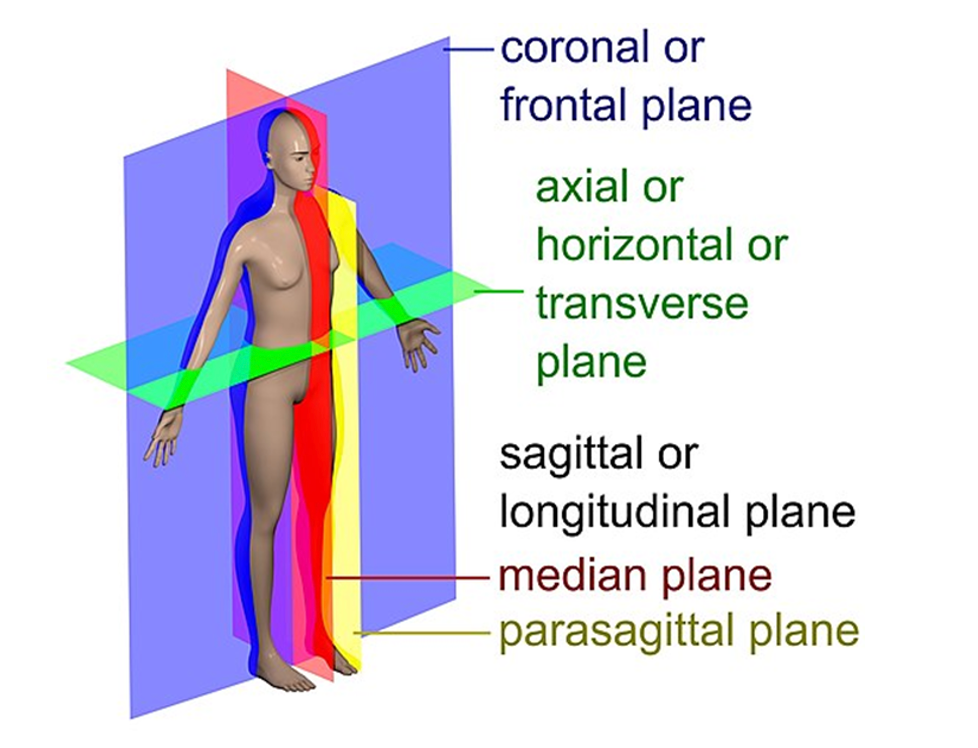
Figure 7. Illustration of the movement planes on the body.
The Burt robot offers three primary planes of movement, and with proper positioning, it can cover most of them. The Bionik operates in two planes, transverse and sagittal, while Harmonic Bionics covers three planes. The ARMAO Power also works in three planes.
The ARMAO Spring technically has zero planes since it is not robotically driven, but you can still access the planes manually. The Diego operates in one plane with two passive, non-robotic sides, combining robotic systems with passive pulleys. These are some of the most prevalent robotic systems you'll encounter in clinical settings today.
Orientation Vs. Position
Another important aspect to consider with robotics and positioning is the distinction between orientation and position. Imagine you're holding a cup of water. If the cup remains fixed in your hand, you can move your hand around, changing the position, but the orientation of the cup remains the same. However, when you bring the cup to your mouth and tip it, the position and orientation change. Figure 8 illustrates a robotic arm.
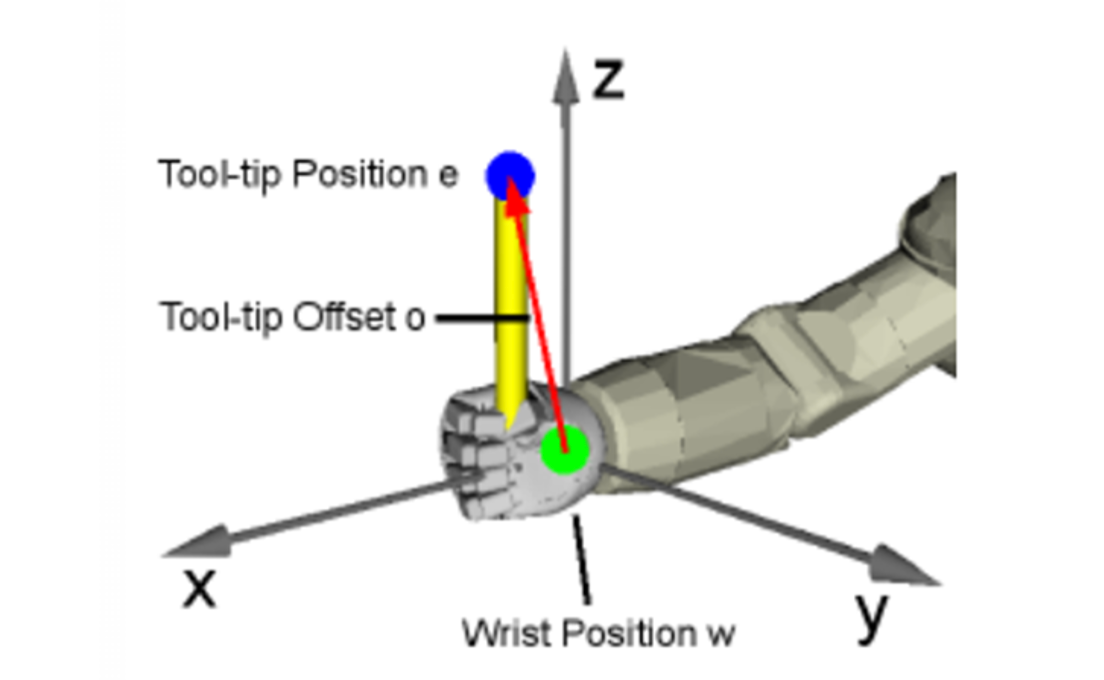
Figure 8. Orientating and positioning with a robotic arm.
In robotics, this concept allows us to decide whether to fix our hands on an object or perform multidirectional positional changes. This capability is crucial for working on activities of daily living (ADLs) or functional tasks. Many robots can facilitate actions like bringing a cup to your mouth, essential for rehabilitation and daily activities.
The current drive in robotics, especially from an occupational therapy perspective, focuses on enhancing functionality. Our main goal is to make these robotic systems more functional, helping patients perform everyday tasks more effectively. This push towards increased functionality aligns with our primary objectives in clinical settings, aiming to improve patient independence and quality of life.
Human and Robotic Workspaces
Figure 9 shows the Burt, an upper extremity robot.
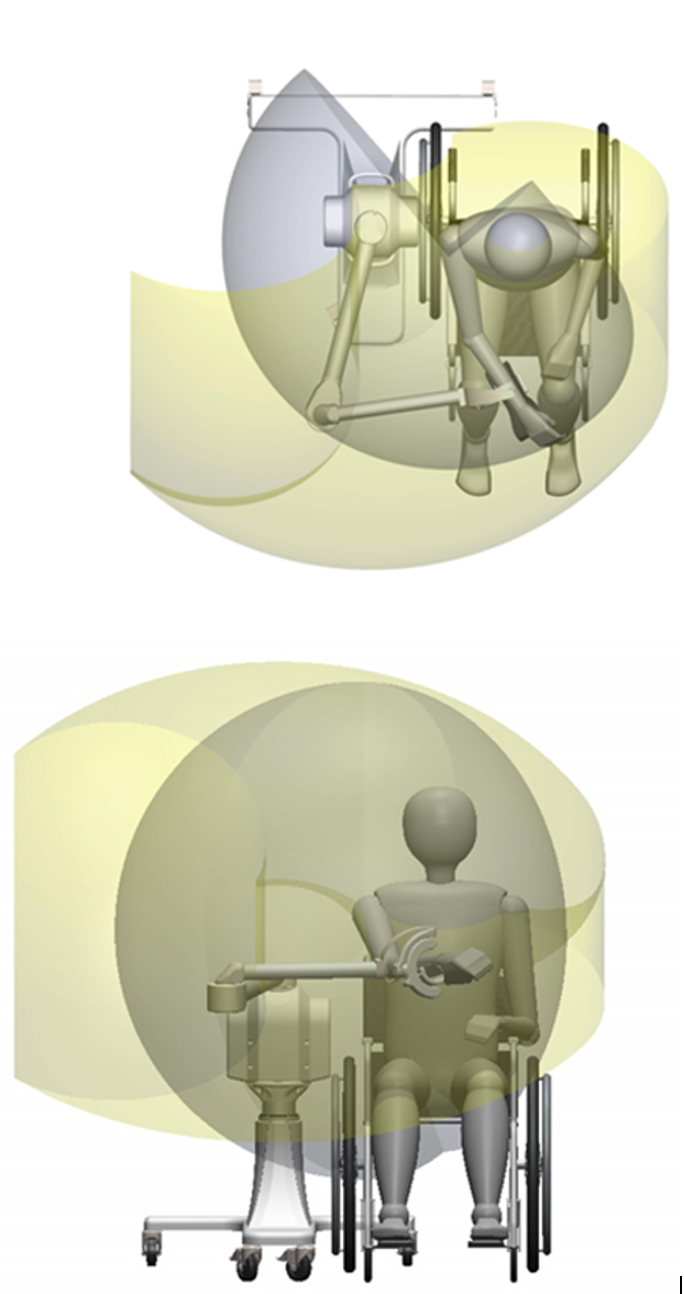
Figure 9. Examples of the range of motion with the Burt.
The yellow area represents the full range that Burt can achieve and accomplish. In contrast, the gray area indicates what we can safely accomplish while sitting in Burt, considering certain restrictions to prevent patients from hitting themselves in the face or legs. These safety parameters ensure that patients stay within a functional range, although the robot's range of motion far exceeds that of a human arm.
This capability means we are not limited to a small workspace; we can use as large a workspace as the patient can physically manage. Even patients with minimal movement can participate in tasks because the robot can be set to assist them. They do what they can, and the robot moves them through the full range of motion. This setup provides tactile sensation, repetition, and simultaneous visual and physical feedback, which enhances neuroplasticity.
It's important to emphasize that robotics in therapy is not about replacing the therapist. Many therapists, myself included when I first started, have concerns about this. However, robotics is an additional tool in our toolbox. They protect our bodies and maximize the effectiveness of therapy sessions for our patients.
We'll take some time to explore the clinical benefits of using robotics in therapy, ensuring you understand how they can enhance your clinic's offerings and improve patient outcomes.
Clinical Benefits with Safety as a Priority
How can it help you as a therapist, and how can it help your patients? The number one clinical benefit is safety. Safety is paramount when treating a patient, whether transferring in the bathroom, to a bed, or to a mat.
A significant safety feature in some of these systems is back drivability. For instance, the Burt upper extremity robot has back drivability. This means that if I need to override the robot, I can do so without it resisting. I can stop it mid-exercise if the patient is having a medical event. Although all robots have an emergency stop, back drivability allows me to manually stop the robotic arm and safely remove the patient without the robot fighting back. Thanks to its low torque motor, the robot stops because it senses my resistance.
Considering these safety mechanisms is essential because we deal with medically involved patients. We must ensure it's safe if they have a medical event, such as low blood pressure. Positional support is also crucial. For patients with strokes, subluxation can be a significant contraindication, but proper support within the system can help. The Glenohumeral joint must be in a neutral position to avoid offsetting and sliding, ensuring it’s supported.
Additional tools like electrical stimulation (e-stim) can enhance treatment by providing support and sensory feedback. For patients with neglect, the system can increase spatial awareness and sensation of arm movement, improving proprioceptive input and posture.
Therapist safety is also critical. We are at high risk for back injuries, especially when handling flaccid upper extremities that can be heavy. Robotics help offload the weight, allowing us to focus on other aspects like posture and recovery without straining our bodies. The robots assist in safely managing patient movement, reducing the physical burden on therapists and enhancing the effectiveness of therapy sessions.
Clinical Benefits of Assessment
The next topic is assessments. These assessments evaluate volitional mobility, range of motion, strength, cognition, and other functional tasks. Some robotic systems also incorporate balance assessments, providing feedback on visual processing abilities.
These assessments evaluate tracking, visual discrimination, and depth perception skills. They utilize various validating measures, enhancing the assessment process. For instance, the Burt system includes a trail-making assessment. Instead of pen and paper, patients perform the assessment on the screen using their arm, offering another dimension to the evaluation.
Robotic systems also enhance cognitive assessments through multi-step tasks. For example, a shopping game where patients use their arms to navigate a shopping cart and find items from a list, or a laundry task where they sort clothes and distinguish between bleach and detergent on a screen. These activities help patients practice and improve their skills in a safe environment, ensuring better carryover to real-life tasks.
These virtual tasks can serve as practice if a patient is unsafe in the kitchen or laundry room. They provide opportunities for patients to learn and apply skills such as money management or math in a controlled setting. This repetition and practice aim to facilitate real-life application. For example, sorting laundry on a screen can help a patient perform the task in a real-life scenario.
Reiterating these points emphasizes the benefits of integrating robotic assessments and training activities into therapy. They offer a bridge between practice in a safe, controlled environment and application in daily life, enhancing overall treatment outcomes.
Clinical Benefits in Treatment
The clinical benefits of robotics treatments are numerous, particularly for neurological patients, where repetition is crucial. Robotics significantly increases repetition, cognitive engagement, and motivation, contributing to mass practice. Combining robotics and non-immersive VR facilitates mass practice more efficiently than traditional OT sessions. This efficiency allows for 30 to 40 minutes of robotic therapy, leaving ample time to focus on ADLs and other necessary treatments.
Robotics also help decrease compensatory strategies. When patients begin to regain movement, they often compensate with improper techniques, such as shoulder hiking or using their whole body to move their arm. For instance, the Burt robot has a locking plane feature, which locks the patient into a specific plane, like horizontal adduction/abduction or shoulder flexion/extension. This prevents shoulder hiking and encourages smooth, functional movement patterns.
Another significant benefit is the quality of movement. Robotic movements are smooth and natural, providing support that feels like natural arm movement. This smoothness is essential, as clunky or jumpy movements can feel unnatural and hinder progress. These robots support the development of strength and coordination, offering resistance to increase strength and engaging patients in more interactive and motivating activities than traditional exercises like Therabands.
Robotics also improve reaction time and coordination, as patients must respond to tasks on the screen. Additionally, setup time is a critical factor. Efficient systems allow for quick setup, maximizing the time available for therapy. Systems that take too long to set up can consume valuable therapy time.
Gravity compensation or full elimination is another vital feature. Many robotic systems provide gravity elimination, making the patient's arm feel weightless and allowing them to focus on their movement without the burden of their arm's weight. This feature is particularly beneficial for patients with limited strength or movement control.
In summary, integrating robotics into therapy offers numerous clinical benefits, including increased repetition, cognitive engagement, decreased compensatory strategies, smooth and natural movement support, improved strength and coordination, efficient setup times, and gravity compensation. These advantages enhance therapy sessions' effectiveness and efficiency, ultimately improving patient outcomes.
In addition to the benefits already discussed, robotics in treatment offers several more advantages. One significant benefit is the ability to use guided patterns to perform functional tasks and activities of daily living. Many robotic systems are moving towards more ideal practices, allowing for open and closed-chain activities. These systems enable therapists to manipulate objects within the game space, making tasks harder or easier, adjusting the level of screen activity, and placing items on the right or left side of the screen based on patient needs.
The sensory feedback provided by these systems is also invaluable. For example, the Burt robot offers haptic feedback, providing tactile sensations like tapping and buzzing when performing a task correctly. This haptic feedback and visual cues, such as balloons or other celebratory graphics, enhance patient engagement and motivation.
Robotic systems also prepare patients for other skill sets through gamified functional activities. Driving games, for example, improve reaction times, while grocery store navigation tasks help with spatial awareness and decision-making. These activities are engaging and practical as they translate to real-life scenarios.
Finally, robotics in therapy effectively addresses range of motion, ensuring that patients work through their full range of movement in a controlled and supportive environment. This comprehensive approach supports overall functional recovery, making robotics a powerful tool in therapeutic settings.
Summary
To reiterate, these are the learning objectives I hope you can now achieve. You should be able to analyze the types of robotic technology currently available in OT practice, considering aspects such as drive systems, patient safety, movement planes, and the inclusion of cognitive, visual, and motor activities. Additionally, you should be able to apply your understanding to determine the specific clinical benefits of current robotic technology and integrate these benefits into your treatment planning to support functional activities.
Furthermore, you should now be able to evaluate the capabilities and limitations of current technology. This includes understanding the drive systems, setup requirements, kinematic supports, and movement facilitation. Finally, you should be able to consider how these technologies fit into your clinical environment and across different settings.
Thanks for your time and attention today.
Questions and Answers
Is there any particular movement on the machine that you like the best?
One of my favorite aspects of using robotic technology, especially for the upper extremities, is quickly getting most patients active and engaged. As we know, recovery often progresses from proximal to distal, so starting with the shoulder is crucial. Seeing patients achieve that initial shoulder movement is incredibly rewarding. It seems to unlock their enthusiasm and motivation, sparking further progress.
For example, the first movements I often see patients perform are protraction and retraction. Watching them punch away with excitement as they gain control over these movements is a testament to the effectiveness of robotic therapy. This initial success can lead to positive outcomes as their confidence and engagement grow.
Reflecting on my earlier experiences, our tools were quite antiquated compared to now's advanced technology. Treating stroke or spinal cord injury patients with today's robotic systems would be an exciting and significantly more effective experience.
What characteristics, like range of motion and muscle strength, would allow patients to benefit from robotics?
To determine whether a patient is appropriate for robotic therapy, it's essential to consider their movement level. If the robot can perform full robot assist, it can accommodate patients with trace or no movement.
Patients with trace movement can engage in activities within their limited workspace, such as playing games on the screen. This minimal level of engagement can be crucial for maintaining motivation and involvement in their rehabilitation process.
You would set up the workspace for patients without movement and put the robot in full robotic mode. In this mode, the robot performs the movements for the patient, guiding them through the range of motion and activities. This ensures that even patients without any voluntary movement can still benefit from the therapeutic exercises and activities, receiving the necessary sensory and proprioceptive feedback to aid their recovery.
By tailoring the robotic settings to the patient's capabilities, you can provide effective therapy that maximizes their potential for improvement, regardless of their initial movement level.
How do you charge for this technology?
It all depends on the specific circumstances. When charging for a device, I typically coded it as neuromuscular re-education, especially since most of my patients were neuro patients. However, depending on the treatment provided, you can also code it as a therapeutic activity.
For general deconditioned patients, I used these systems for cardio training within a controlled environment to avoid overexertion. Neuromuscular re-education is an ideal choice for coding, given the nature of the therapy and the patient population I primarily worked with.
How do clinics or SNFs obtain these systems?
In my experience, incorporating robotics into the clinic involves thorough research and effective communication with management. When I was in the clinic, I would conduct detailed research on the available robotic systems, considering both high-tech and low-tech options that fit within a range of budgets. It's essential to understand the financial constraints of your facility, as budgets can vary widely.
Once I had gathered sufficient information, I would present my findings to my manager, highlighting the potential benefits for patient outcomes and how these technologies could be integrated into our treatment plans. Demonstrating enthusiasm and a clear understanding of the technology's impact on patient care is crucial. This approach not only helps to get management on board but also assists in navigating the budgeting process.
For those high-level discussions, it's important to emphasize the technology's evidence-based benefits. Show how it can enhance patient engagement, improve functional outcomes, and potentially increase the efficiency of therapy sessions. Tailoring your pitch to address the concerns and priorities of decision-makers, such as CEOs and other higher-ups, can significantly influence their support for investing in these technologies.
By presenting a well-researched proposal and aligning it with your facility's strategic goals, you can effectively advocate for the adoption of robotic systems and ultimately enhance the quality of care provided to your patients.
References
Brochard, S., Robertson, J., Médée, B., & Rémy-Néris, O. (2010). What's new in new technologies for upper extremity rehabilitation? Current opinion in neurology, 23(6), 683–687. https://doi.org/10.1097/WCO.0b013e32833f61ce
Brunner, I., Skouen, J. S., Hofstad, H., Aßmuss, J., Becker, F., Pallesen, H., Thijs, L., & Verheyden, G. (2016). Is upper limb virtual reality training more intensive than conventional training for patients in the subacute phase after stroke? An analysis of treatment intensity and content. BMC neurology, 16(1), 219. https://doi.org/10.1186/s12883-016-0740-y
Bureau of Labor Statistics, U.S. Department of Labor. (2023, September 12). Low clinical burden-therapist physical safety (back injuries). Retrieved from https://www.bls.gov/iif/nonfatal-injuries-and-illnesses-tables/case-and-demographic-characteristics-table-r100-2020.htm
Carrico, C., Chelette, K. C. 2nd, Westgate, P. M., Salmon-Powell, E., Nichols, L., & Sawaki, L. (2016). Randomized trial of peripheral nerve stimulation to enhance modified constraint-induced therapy after stroke. American journal of physical medicine & rehabilitation, 95(6), 397-406. https://doi.org/10.1097/PHM.0000000000000476
Conroy, S. S., Whitall, J., Dipietro, L., Jones-Lush, L. M., Zhan, M., Finley, M. A., ... & Bever, C. T. (2011). Effect of gravity on robot-assisted motor training after chronic stroke: A randomized trial. Archives of Physical Medicine and Rehabilitation, 92(11), 1754-1761. https://doi.org/10.1016/j.apmr.2011.06.016
Conroy, S. S., Wittenberg, G. F., Krebs, H. I., Zhan, M., Bever, C. T., & Whitall, J. (2019). Robot-assisted arm training in chronic stroke: Addition of transition-to-task practice. Neurorehabilitation and Neural Repair, 33(9), 751-761. https://doi.org/10.1177/1545968319862558
Edwards, D. J., Cortes, M., Rykman-Peltz, A., Chang, J., Elder, J., Thickbroom, G., Mariman, J. J., Gerber, L. M., Oromendia, C., Krebs, H. I., Fregni, F., Volpe, B. T., & Pascual-Leone, A. (2019). Clinical improvement with intensive robot-assisted arm training in chronic stroke is unchanged by supplementary tDCS. Restorative neurology and neuroscience, 37(2), 167–180. https://doi.org/10.3233/RNN-180869
Gandhi, D. B., Sterba, A., Khatter, H., & Pandian, J. D. (2020). Mirror therapy in stroke rehabilitation: Current perspectives. Therapeutics and clinical risk management, 16, 75-85. https://doi.org/10.2147/TCRM.S206883
Gillen, G. (Ed.). (2015). Stroke rehabilitation. Elsevier Health Sciences. https://www.sciencedirect.com/book/9780323172813/stroke-rehabilitation
IRF.org
Karunakaran, K. K., Pamula, S. D., Bach, C. P., Legelen, E., Saleh, S., & Nolan, K. J. (2023). Lower extremity robotic exoskeleton devices for overground ambulation recovery in acquired brain injury-a review. Frontiers in Neurorobotics, 17, 1014616. https://doi.org/10.3389/fnbot.2023.1014616
Kimberley, T. J., Samargia, S., Moore, L. G., Shakya, J. K., & Lang, C. E. (2010). Comparison of amounts and types of practice during rehabilitation for traumatic brain injury and stroke. Journal of rehabilitation research and development, 47(9), 851–862. https://doi.org/10.1682/jrrd.2010.02.0019
Klopcar, N., et al. (2007). A kinematic model of the shoulder complex to evaluate the arm-reachable workspace. Journal of Biomechanics, 40(1), 86-91.
Krebs, H. I., Hogan, N., Aisen, M. L., & Volpe, B. T. (1998). Robot-aided neurorehabilitation. IEEE Transactions on Rehabilitation Engineering, 6(1), 75.
Lang, C. E., MacDonald, J. R., & Gnip, C. (2007). Counting repetitions: An observational study of outpatient therapy for people with hemiparesis post-stroke. Journal of Neurological Physical Therapy, 31(1), 3-10. https://doi.org/10.1097/01.npt.0000260568.31746.34
Laver, K., George, S., Thomas, S., Deutsch, J. E., & Crotty, M. (2015). Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews, 2, CD008349. https://doi.org/10.1002/14651858.CD008349.pub3
Laver, K. E., Lange, B., George, S., Deutsch, J. E., Saposnik, G., & Crotty, M. (2017). Virtual reality for stroke rehabilitation. The Cochrane database of systematic reviews, 11(11), CD008349. https://doi.org/10.1002/14651858.CD008349.pub4
Lee, S. I. (2020). Estimating upper-limb impairment level in stroke survivors using wearable inertial sensors and a minimally-burdensome motor task. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 28(3), 601-611. https://doi.org/10.1109/TNSRE.2020.2966950
Maciejasz, P., Eschweiler, J., Gerlach-Hahn, K., & Jansen-Troy, A. (2014). A survey on robotic devices for upper limb rehabilitation. Journal of neuroengineering and rehabilitation, 11(3). https://doi.org/10.1186/1743-0003-11-3
Miranda, J. G. V., Daneault, J. F., Vergara-Diaz, G., Torres, Â. F. S. O. E., Quixadá, A. P., Fonseca, M. L., ... & Bonato, P. (2018). Complex upper-limb movements are generated by combining motor primitives that scale with the movement size. Scientific reports, 8(1), 12918. https://doi.org/10.1038/s41598-018-29470-y
MIT 77 Massachusetts Avenue Laboratory. (2023, September). Rehabilitation robotics. MIT. https://the77lab.mit.edu/rehabilitation-robotics
Oubre, B., Daneault, J. F., Jung, H. T., Whritenour, K., Miranda, J. G. V., Park, J., Ryu, T., Kim, Y., & Lee, S. I. (2020). Estimating upper-limb impairment level in stroke survivors using wearable inertial sensors and a minimally-burdensome motor task. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 28(3), 601-611. https://doi.org/10.1109/TNSRE.2020.2966950
Purton, J., Sim, J., & Hunter, S. M. (2023). Stroke survivors' views on their priorities for upper-limb recovery and the availability of therapy services after stroke: A longitudinal, phenomenological study. Disability and Rehabilitation, 45(19), 3059-3069. https://doi.org/10.1080/09638288.2022.2120097
Reinkensmeyer, D. J., & Boninger, M. L. (2012). Technologies and combination therapies for enhancing movement training for people with a disability. Journal of neuroengineering and rehabilitation, 9, 17. https://doi.org/10.1186/1743-0003-9-17
Rodgers, H., Bosomworth, H., Krebs, H. I., van Wijck, F., Howel, D., Wilson, N., ... & Shaw, L. (2019). Robot assisted training for the upper limb after stroke (RATULS): A multicentre randomized controlled trial. The Lancet, 394(10192), 51-62. https://doi.org/10.1016/S0140-6736(19)31055-4
Rohrer, B., Fasoli, S., Krebs, H. I., Hughes, R., Volpe, B., Frontera, W. R., ... & Hogan, N. (2002). Movement smoothness changes during stroke recovery. Journal of neuroscience, 22(18), 8297-8304. https://doi.org/10.1523/JNEUROSCI.22-18-08297.2002
Stoykov, M. E., & Madhavan, S. (2015). Motor priming in neurorehabilitation. Journal of neurologic physical therapy, 39(1), 33-42. https://doi.org/10.1097/NPT.0000000000000065
The increasingly important role of robots in rehabilitation. (n.d.). Retrieved from https://ifr.org/post/the-increasingly-important-role-of-robots-in-rehabilitation
Citation
Gatewood, A. (2024). Human-interfacing robots for functional upper extremity rehabilitation. OccupationalTherapy.com, Article 5709. Available at www.occupationaltherapy.com.
