Introduction
Thank you. It is really great to be here today. When I became an occupational therapist, I had never thought I would be involved in pelvic health. I thought when I entered OT school that I would be a hand therapist. As I got exposed to many different things, I became influenced by all the different topic areas.
My introduction to pelvic health emerged during the first year of my practice as I noticed that most of the people I was working with were not breathing well. They were breathing very inefficiently, and I started a program on breath. And in my learning about breathing, I discovered something exciting. We are all familiar with the respiratory diaphragm. The pelvic floor muscles make up the pelvic diaphragm. As I began to learn more about the pelvic floor, I learned how it helps with more efficient breathing and how it impacts our overall health and wellbeing. It is really vital for our ability to engage in occupations.
I also started to discover that within the broad category of pelvic health, there are different types of pelvic health issues, some of which are epidemic. Many people are dealing with incontinence, prolapse (women), and different pelvic health issues.
To give you an example of the need, I have been involved with a local community health center in New York City for about 20 years. I run several groups. About 15 years ago, I was approached about doing a pelvic health program. Many poo-pooed the idea because they said, "Who's going to come?" Finally, they gave in. After they sent out the information, the next day, they called and said, "We filled that group. Would you be willing to do another group?" I said, "Yes." The next day, they filled another group. We wound up filling four groups of 25 people. There was also a waiting list of 75 or more people. The community health center had never had a response to a program like that before. This goes to show that there is a tremendous need. The need is seen by how many incontinence underwear commercials for men and women we see. We tend to think of pelvic health mainly as a women's health issue because more women have pelvic health issues than men; however, men also have issues.
Pelvic Region: A Lot Happens Down There
- Elimination
- Sexual function
- ________________________________
- Center of balance
- Femoral joints
- Intimate relationship between tailbone and head in terms of mobility and flexibility
- Key muscles for postural alignment pass through the pelvis.
When I ask a group of people, "What goes on to the pelvic region?" people can usually identify the two items above the line, elimination, and sexual function. As a therapist, you would probably be able to identify most of the points below the line. We certainly know from anatomy and kinesiology that our center of balance is in the pelvic region. If the center of gravity is in the pelvic region and movement is restricted due to pain or other reasons, this can greatly impact balance.
We also know that the femoral joint is part of the pelvic region. Many times when people have pelvic health issues, they have hip issues as well. I will skip down to that last bullet point to talk about key muscles for postural alignment. These pass through the pelvis. Thus, there is an intimate relationship between the tailbone and the head regarding mobility and flexibility. If the pelvic region is restricted, not only will there be balance issues, but there will also be mobility restrictions. When we start to look at the pelvic region and are dealing with someone with incontinence, this could also impact other areas. I will help connect these dots as we go along.
When I first started thinking about pelvic health, it was framed around pelvic floor disorders or dysfunction. Then, I realized words influence our thinking, so I shifted my thinking and started to reframe it as pelvic health issues. Again, I never went into OT thinking I would work in pelvic health. Hopefully, you will agree by the end that this is an important area of practice, even if you are not interested specifically in things like incontinence. Remember, the pelvic floor relates to core dysfunction. If there are problems with the pelvic floor, there is also going to be core dysfunction.
Pelvic Health Issues: Core Dysfunction
- Urinary Incontinence
- Fecal Incontinence
- Constipation
- Prolapse
- Painful Urination
- Dyspareunia
- Erectile Dysfunction
- Levator Ani Syndrome
- Coccydynia
- Pudendal Neuralgia
"Pelvic health issues" is an umbrella term for some of the above conditions. There are a large number of people dealing with pelvic health issues. Let's take a minute to look at how the pelvic floor relates to our core. Core strengthening is a popular term today. Most people think about the transversus abdominis or the abdominal muscles when they think about the "core." However, if you are only thinking about strengthening the abdominals, you are missing an important piece of the puzzle, and this can cause an imbalance.
Think about holding a tube of toothpaste. If you hold it vertically and squeeze the middle, the toothpaste will pop out the top and the bottom. So, if you are only thinking about the abs in terms of core function, you can create dysfunction because the core is made up of the abdominals in the front, the respiratory diaphragm at the top, multifidus muscles in the back, and the pelvic floor or the pelvic diaphragm in the bottom. All of these muscles need to work together ultimately for core function.
Core Functions
- Core-Distal Connectivity
- Posture
- Balance
- Spinal Stability
- Shock Absorption
- Breathing
What are these core functions? Figure 1 shows an overview of core functions.
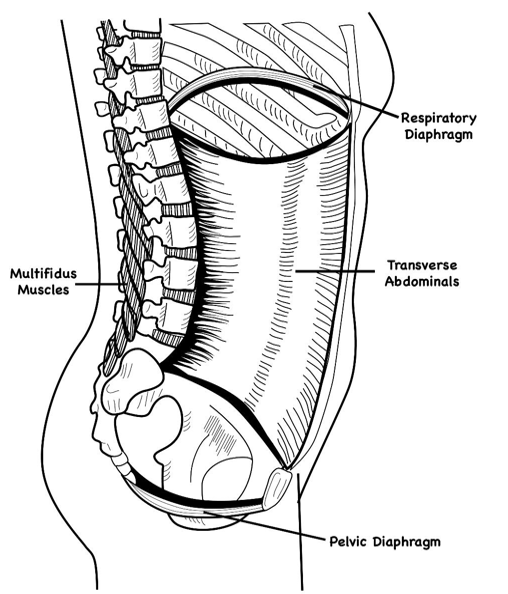
Figure 1. Four areas of core function: respiratory diaphragm, transverse abdominals, pelvic diaphragm, and multifidus muscles. Click here to enlarge the image.
The core functions are vital for spinal stability, shock absorption, core distal connectivity, meaning we need proximal stability for distal mobility, posture, and balance. It is also essential for our breathing. When you and I breathe, the respiratory diaphragm descends when we inhale, pushes on the abdominal organs, presses down on the pelvic diaphragm. As we breathe in, the respiratory and pelvic diaphragms move down. When we breathe out, they go up. There is this up and down movement that is referred to as the dance of the diaphragm. If the pelvic floor is not functioning in the way it should, every breath will be shallower.
Pelvic health has a direct relationship to our ability to breathe. Aside from the core that we just looked at, Figure 2 shows a drawing looking at the pelvic floor.
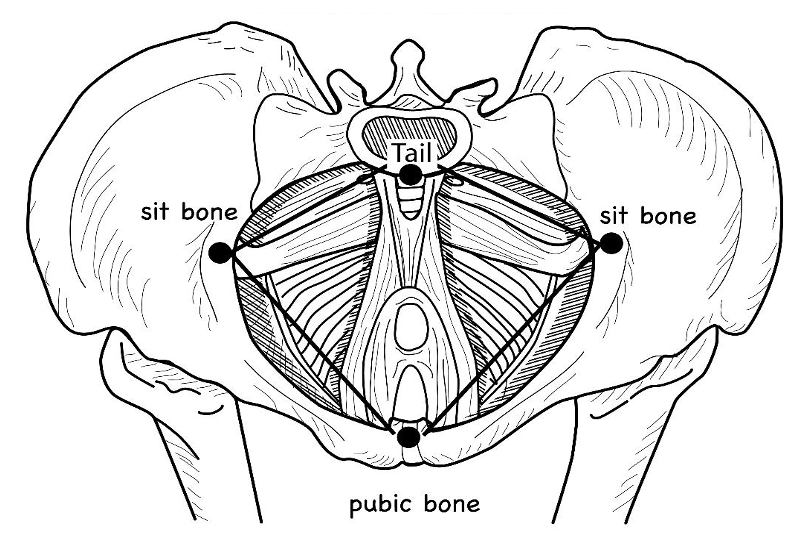
Figure 2. The pelvic floor with the tail bone, sit bones, and pubic bone forms a diamond shape. Click here to enlarge the image.
The pelvis is shaped like a bowl, with the pelvic floor muscles shaped like a hammock. You can also see that it is a diamond-shaped space with borders consisting of the tailbone, the pubic bone, and the two "sit" bones. Part of the work we are going to do today is experiential. I will take you through the lecture, and then the last 30 to 40 minutes will be experiential with a handout on the steps. These landmarks define where the pelvic floor is so that people can sense and feel it in the work we will do, and we will come back to this picture later on.
Figure 3 shows both the male and female anatomy from a bottom-up view.
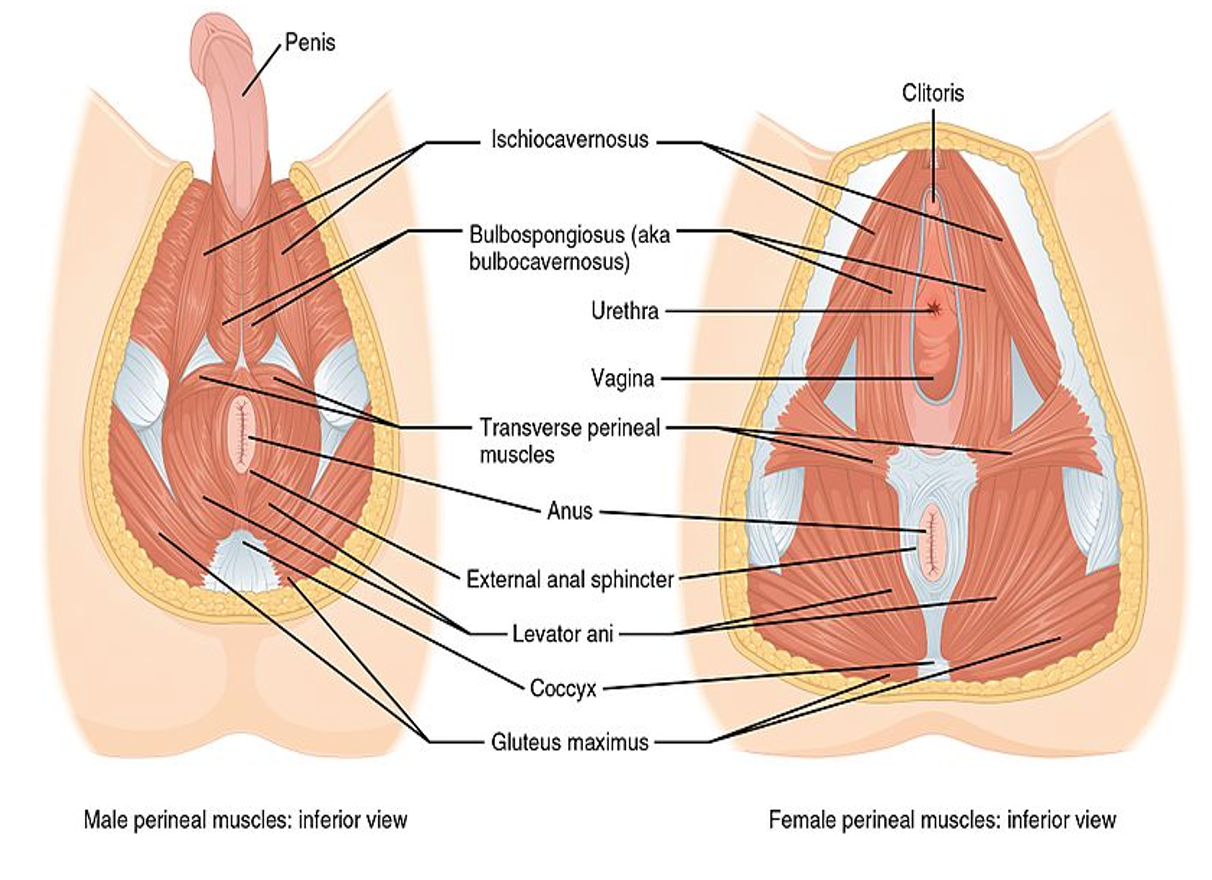
Figure 3. A bottom-up view of the male and female pelvic anatomy and musculature. Click here to enlarge the image.
Here is another picture looking from the bottom up of both the male and female anatomy to see the pelvic floor muscles. I am going to focus on the female anatomy on the right. The urogenital triangle includes the urethra and the vagina. These muscles are more superficial and are the weaker muscles of the pelvic floor. The muscles in the back portion of the pelvic floor, as a group, can be referred to as the levator ani muscles. These are deeper, more powerful muscles that are involved with postural control. At the bottom, you can see that the muscles almost fan out from the tailbone.
I am not going to talk much about Kegels today. These are the muscles that you squeeze to stop urine flow. The goal is to get people to contract these. However, the deep, powerful muscles in the back are so much easier to engage. Oftentimes, people engage these when doing a Kegel exercise instead of focusing on the muscles in the front. I will take you through an exercise that will help you make the distinction between the front and back.
The pelvis is also shaped like a bowl, as we talked about. Every time I see drawings of a female pelvis, it always makes me think of a bowl of fruit. The fruit represents the organs that sit inside the pelvis. The muscles support these organs, including the bladder, the uterus, and the rectum. There are also abdominal organs on top of that. As I said, when we breathe in, the respiratory diaphragm pushes downward on those pelvic floor muscles. That is a lot of force coming down. If those muscles are weak, everything gets very lax. Or, if they are too tight, it can restrict normal movement and the dance of the diaphragm. The pelvic floor is under a lot of pressure all the time. Thus, those muscles need to be healthy and supple enough to respond to the demands of daily living.
What do I mean by supple? Supple means the ability of the muscles of the pelvic floor to lengthen and shorten. All of us need that capacity. Every muscle needs to lengthen and shorten. When a group of muscles or a particular muscle loses that ability, this leads to dysfunction.
Let's look at some of the functions. In Figure 4, you can see that the pelvic floor muscles support the organs.
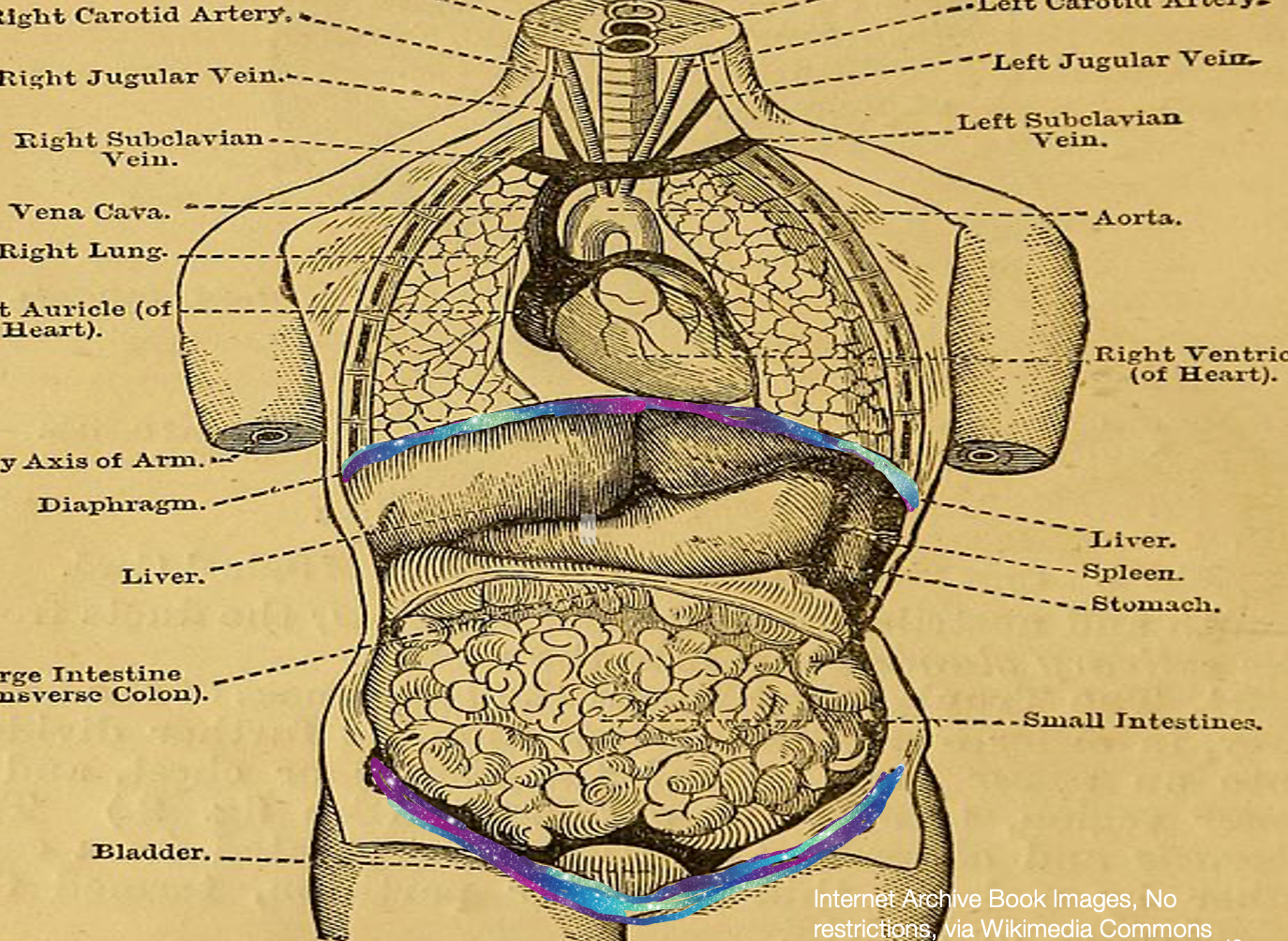
Figure 4. Anatomical image with the pelvic floor and diaphragm highlighted. Click here to enlarge the image.
Pelvic Floor Functions
- Support organs – vagina, bladder, rectum, and intestines
- Maintain continence
- Allow elimination
- Stabilize and support joints of hips and pelvis
- Sexuality
- Birthing
- Breathing (Hurry Call)
They help us maintain continence, allow elimination, and stabilize and support the joints of the hips, the pelvis, and even the back. The pelvic floor is the floor of the core. Good core coordination is vital to the stability of all those joints in the back. If those muscles are too tight, there can be a lot of sexuality issues as well as birthing and breathing issues.
Let's do a quick experiential. I want you to sit back all the way back in your chair and allow yourself to breathe as if you were going to sleep. Do not try to control your breath. Just let it come and sense how low the breath seems to go. Get a feel for that and where you sense the movement. Next to the bullet that says breathing, I have added the wording, "hurry call." I want you to imagine that you are sitting on a plane. You have to pee, and all of a sudden, you need to get up to go. Suddenly, you hit turbulence, and the pilot says, "I'm sorry, but you have to stay in your seat." You would contract to help yourself hold. I want you to do that contraction, hold those muscles for as long as you can right now and see how that affects your breathing. Go ahead and see what you notice. Now, breathe normally again and relax those muscles. You probably should have noticed that when those muscles are tight, it makes the breath much shallower. So, if you are walking around with tight pelvic floor muscles, you are breathing with a much shallower breath. And, if those muscles relax, the same would be true as well.
Some Common Causes of Pelvic Floor Dysfunction
- Stress and tension
- The pelvic floor can be weak from lack of muscle control OR habitual contraction.
- You need both contraction and relaxation of the pelvic floor for functional strength.
- The pelvic floor can be weak from lack of muscle control OR habitual contraction.
- Childbirth injuries
- Hormonal fluctuations
- Couch potato syndrome - less active, so overall muscle tonus and strength decrease
Stress and tension are big factors in pelvic floor dysfunction. Remember, these are muscles as we use our bodies. Regular stress/tension can make muscles get very tight. Or, if we do not utilize those muscles, they can get relaxed. A lot of pelvic dysfunction is due to weakness. Remember, a lax muscle or a tight muscle will not work optimally. Muscles need the ability to shorten and lengthen. Both situations, whether it is a lax or a tight muscle, can create pain and discomfort. Additionally, childbirth injuries and hormonal fluctuations can cause pelvic floor dysfunction. If you are a couch potato and do not do much, pelvic muscles will get out of shape by not being used.
- Surgeries –
- Hysterectomy
- Prostatectomy
- Total hip replacement – 64-72%
- Abdominal operations - C-sections
- Lumbar spinal fusions, laminectomy, discectomy
- Bladder suspensions
- Obesity
- Trauma due to accidents, fractures of hips or pelvis, sexual abuse
- Excessive exercise, especially abdominal crunches
Common surgeries can also create issues with the pelvic floor like a hysterectomy, prostatectomy, and a total hip replacement, especially the posterior lateral version. This is because the obturator internus attaches to the pelvic floor. Here is what is interesting. People that have hip dysfunction or need a hip replacement typically have pelvic floor dysfunction. I used to believe a long time ago that many people develop pelvic floor issues after hip replacement surgery. However, the evidence shows now that hip dysfunction creates problems in the pelvic floor, which ultimately, down the road, can lead to a hip replacement. Some of that data shows that up to 64 to 72% of pelvic floor issues may also contribute to hip dysfunction.
Abdominal operations like lumbar spinal fusions, laminectomies, discectomies, and bladder suspensions can contribute to dysfunction of the pelvic floor. Obesity can also cause pressure on those muscles and have the muscles do a lot of work. Of course, there is also trauma like broken bones and damaged muscles. Excessive exercise, like abdominal crunches, can cause a decreased balance between the respiratory diaphragm and the pelvic floor abdominals and back muscles. Focusing strictly on those abdominals can create pelvic floor disorders because of all that increased pressure.
- Neurological conditions – MS, CVA, SCI, Parkinson’s
- Pain – low back pain
- Musculoskeletal dysfunction
- Low back/Sacroiliac dysfunction
- Sacral pain
- Groin or Pubic pain
- Piriformis syndrome
- Pudendal Neuralgia
- Tension Myalgia of Pelvic Floor
- Coccydynia
- Levator ani syndrome
- Sexual/Emotional Abuse
Neurological conditions can cause issues, including MS, strokes, spinal cord injury, and Parkinson's. People with chronic back pain can also have pelvic floor disorders. I have many friends that are PTs. They find that people with back pain come back months later with back pain again. However, if they deal with low back pain and incorporate the pelvic floor for the coordination that I was talking about, they have much more success in the long run than people that do not think about the pelvic floor.
Musculoskeletal dysfunction may be involved as the pudendal nerve can have pressure on it. It is a small space with a lot crammed into it. Increased pressure on the nerve can create pain as well as discomfort. The muscles in the pelvic region can get tight, which leads to coccydynia or levator ani syndrome.
Let's not forget about sexual and emotional abuse. These can be huge factors contributing to pelvic floor dysfunction. Pelvic floor muscles are innervated by the sympathetic nervous system much more so than the parasympathetic system. Thus, the stress in our lives greatly impacts the pelvic floor muscles.
Women
- Pelvic Inflammatory disease infection and inflammation in
- Pelvic cavity
- Vulvodynia (10-28%) J Sex Med 2016;13:291e304
- Chronic vulvar discomfort – burning, irritation, pain with penetration
- Vaginismus
- Inability to penetrate the vaginal opening due to spasms
- Dyspareunia (10-20%, 45% after menopause)
- Painful intercourse
- Prolapse (40%)
- Descent of the vaginal wall, uterus, uterus, rectal organs
I mentioned that I work in a community health center called the Carpus Center. When I am doing presentations of 100 people or more, it is usually predominantly women. I say, "How many of you in this room know what prolapse is?" If it tends to be a group of younger women, only three or four out of 100 will know what that is. About 40% of women will deal with prolapse at some point in their lives. Let's go to the top, and I will come back to prolapse. The urethra is very short as compared to a man's. Thus, women are more susceptible to infection. Vulvodynia is where the vulva can have a lot of pain, burning, and irritation in the vulva. And, if there is penetration, it could be excruciating. Oftentimes you do not know the cause and the data. In fact,10 to 28% of women experience that. That is a lot of women. Take, for example, America. Of 330 million Americans, half are women.
Vaginismus involves the muscles around the vagina. They get so tight that there could be no penetration. Even putting a tampon can be very painful. Dyspareunia is where there can be penetration and intercourse, but it is painful. It is a mild diversion of vaginismus. Ten to 20% of women are dealing with this or have dealt with it, and 45% of those are after menopause. As I mentioned before, there is also prolapse, and about 40% of women have or will deal with that. There are also different types of prolapse.
Figure 5 shows that the uterus has dropped down into the vagina.
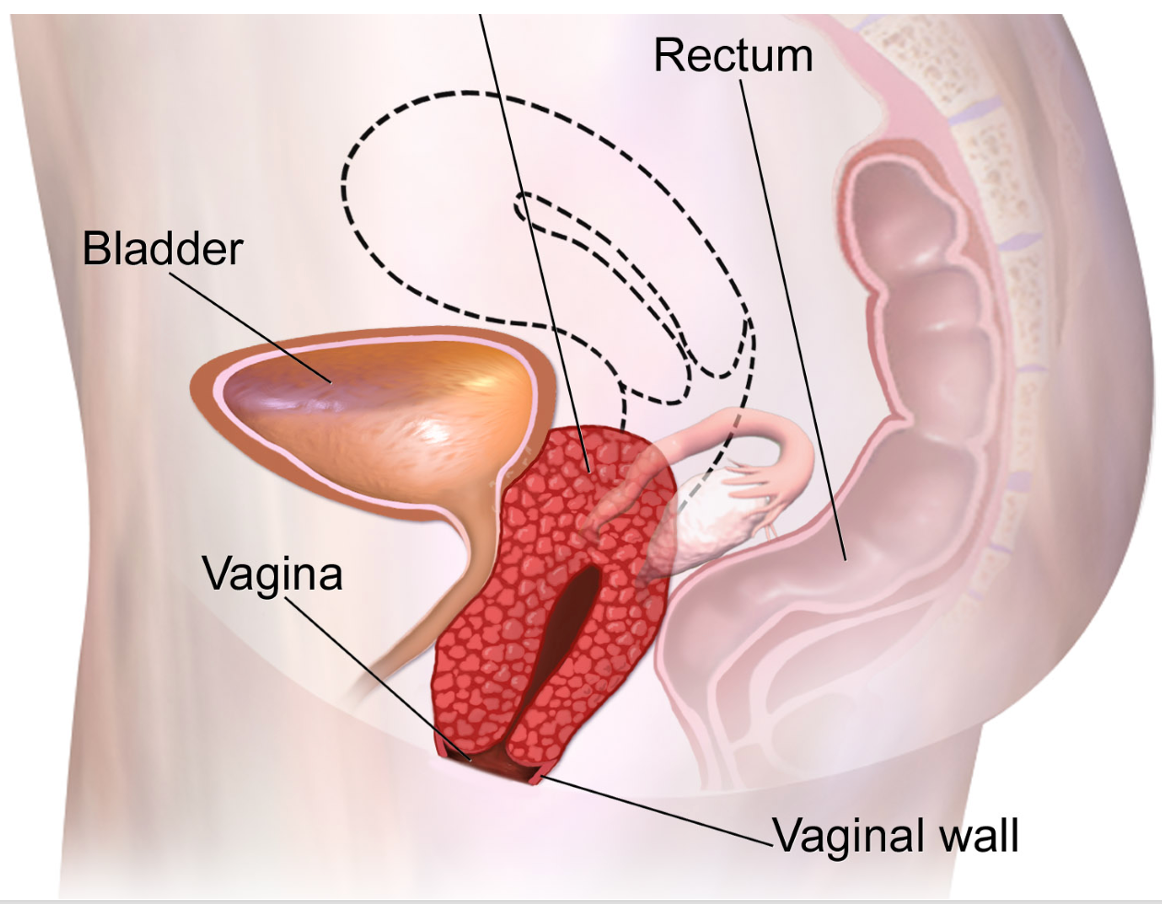
Figure 5. The uterus is dropped down in the vaginal area. Click here to enlarge the image.
The bladder and rectum can also down into the vagina as the ligaments and muscles become weak over time, allowing the organs to descend. There are four different stagings to categorize how far the organ has descended. In the first two stages, there is a lot of the work that I will talk about today that can help a woman. It is also important for women to think about prevention by doing pelvic health work throughout their lives. The last option would be surgery.
- Endometriosis
- Tissue similar to uterine tissue is found outside the uterus – ovaries/fallopian tubes, bladder, bowel, intestines, colon, appendix, and rectum
- Dysmenorrhea
- Painful periods, menstrual cramps
- Diastasis Recti
- Also known as abdominal separation; it happens when rectus abdominus pull apart from their attachment, the linea alba
Lastly, there is endometriosis, painful periods, and diastasis recti. This is where the abdominal muscles can separate. These also fall under the category of pelvic health.
Men
Prostatitis
- Prostatitis (8-10%)
- Inflammation of the prostate gland. There are 4 different types:
- Acute bacterial prostatitis
- acute infection – fever, chills, pain in the lower back and genital area, painful urination
- Chronic bacterial prostatitis
- recurrent infection – may be caused by incomplete urinary evacuation
- Chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CPPS)
- Typically, due to myofascial pain syndrome or nerve inflammation – 3 months or more of pain in the pelvic region
- Asymptomatic inflammatory prostatitis
- No genitourinary symptoms, but higher levels of white blood cells
- Acute bacterial prostatitis
- Inflammation of the prostate gland. There are 4 different types:
An enlarged prostate is a big issue for men (Figure 6).
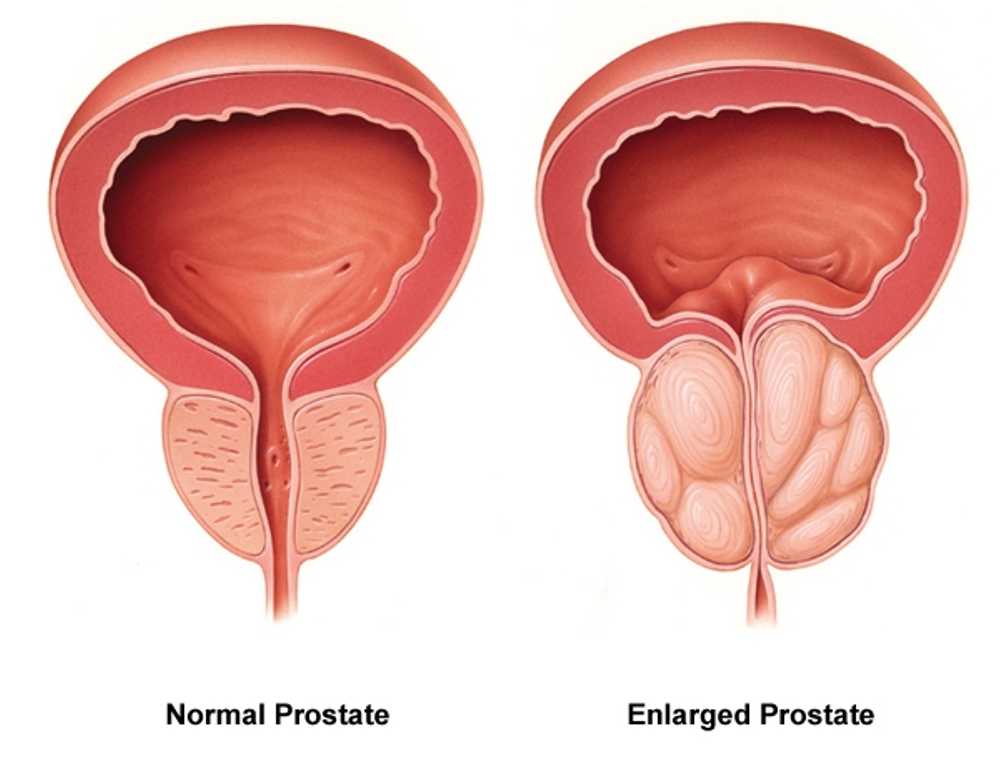
Figure 6. Image showing an enlarged prostate on the right side, causing a narrowing of the urethra.
If you look at the picture on the left, you can see a normal prostate. It is much smaller than the one on the right. The urethra goes right through the prostate. As the prostate enlarges, it begins to restrict the urine that can pass through. Now, for men, this can happen with normal aging. The urine flow gets slower, and that is true for me. I am 66 now, and my urine stream is much slower today than when I was in my twenties. This is normal. The problem is when it slows down too much. This can back up and lead to infection and pain.
When the prostate enlarges, there can be different types of inflammation. There are acute bacterial and chronic bacterial. When men go to a urologist, they are often given antibiotics because the urologist or another type of physician will say, "It is bacterial." The chronic non-bacterial type is also referred to chronic pelvic pain syndrome. A musculoskeletal issue typically causes pain in men versus bacteria or an infection. Men are given antibiotics when instead, the myofascial pain can be addressed. If it is treated properly, the pain will go away.
Erectile Dysfunction
- 25% under 40, 70% at age 70
Men can also have erectile dysfunction. From all of the commercials, we know that this is prevalent, with about 25% of men under 40 dealing with this and 70% at age 70. When I give you these percentages, these are in the middle of several different research studies that have been done. With any type of research, the way a question is asked is going to influence the numbers. These are the mid-range numbers. It could be even a little bit higher or a little lower.
Children
- Diurnal and nocturnal enuresis
- Diurnal 20% < 7, 14% > 7
- Nocturnal 5-10% <10
- Encopresis (bowel incontinence)
- 4% children between 5 and 6, 1.6% 11-12
- Chronic constipation
- Painful urination or defecation
- Urinary retention
- Vesiocoureteral reflux (retrograde flow of urine)
I am not going to focus on kids today, but kids also deal with pelvic health issues. They have day and night urinary incontinence, bowel continence, chronic constipation, and urinary retention. This impacts not only the child's self-esteem but also the dynamics of the family. If you are interested in pediatrics, pelvic health should be something that you are thinking about. I will talk about a model that we can all use whether we are working in pediatrics, adults, or geriatrics.
Bladder and Bowel Disorders in Men and Women
- Bladder
- Interstitial Cystitis (IC) – painful bladder syndrome (PBS)
- Urethral Syndrome – urethral pain, burning, and sensitivity during urination
- Urgency-Frequency Syndrome – irritation of the bladder
- Bowel
- Constipation
- Irritable Bowel Syndrome (IBS) – encompasses a group of symptoms such as abdominal pain, bloating, frequent bowel movements
- Inflammatory Bowel Disease (IBD) – includes Crohn’s disease and ulcerative colitis
Here are some other bladder and bowel disorders in men and women. There is interstitial cystitis or painful bladder syndrome. Again, there are no known causes. There are also urethral syndrome, frequency syndrome, and different types of constipation.
Types of Incontinence
Now, I want to spend a few minutes delving into the different types of incontinence because it is a huge issue, as we all know. Figure 7 shows a diagram showing these types.
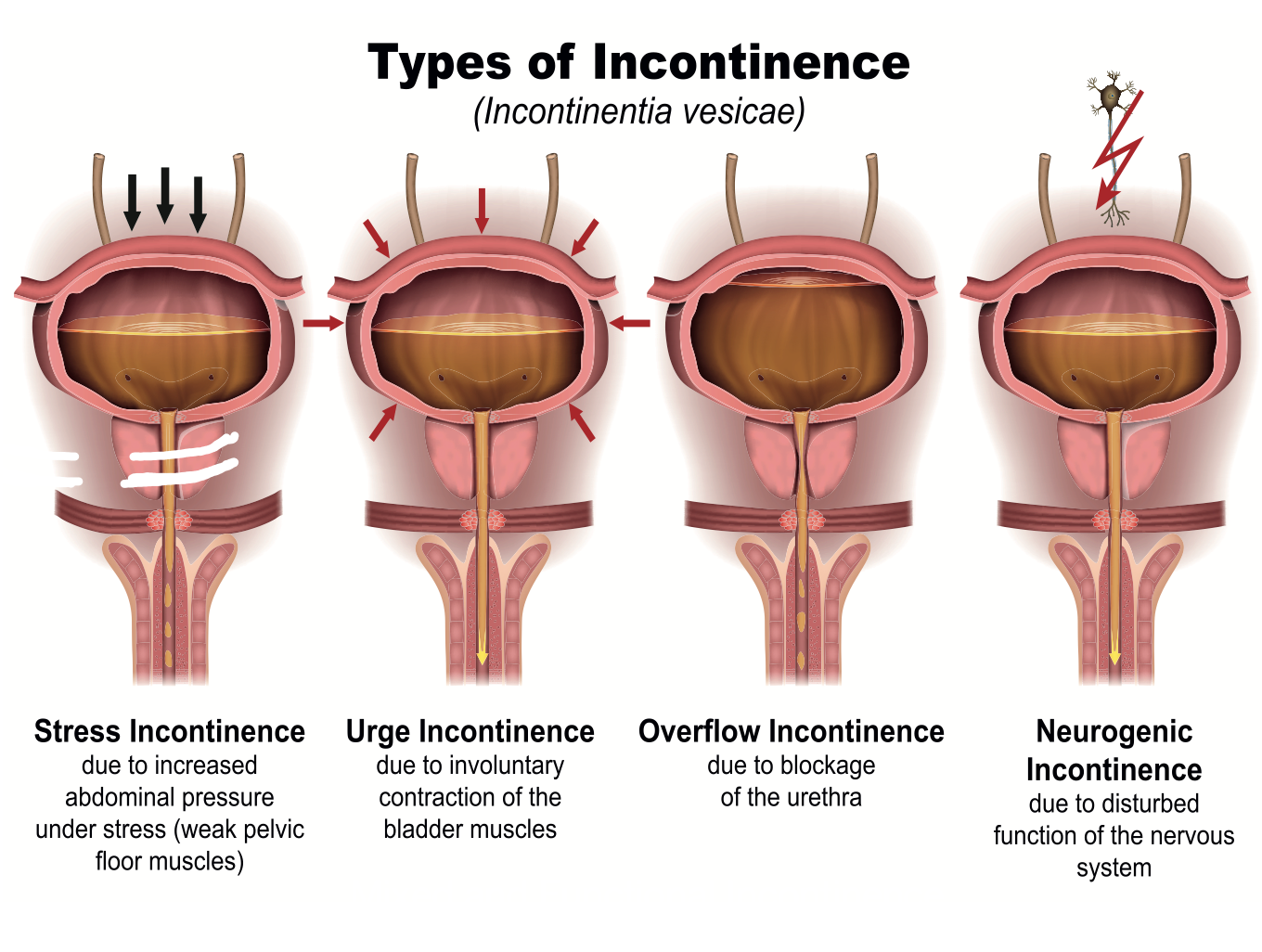
Figure 7. Types of incontinence including stress, urge, overflow, and neurogenic. Click here to enlarge the image.
Stress Incontinence
On the left, you can see an illustration for stress incontinence. The urethra goes through the prostate, pelvic floor muscles, and sphincter. When somebody has stress incontinence, the pelvic floor muscles become weak. For women, this may be due to childbirth, with the muscles becoming weak. If somebody coughs, sneezes, laughs or pushes against something heavy to move it, there can be increased intraabdominal pressure. You see can see this illustrated by the arrows pushing down in the pictures. For example, if you cough, this force pushes down the bladder, and urine leaks out. That is stress incontinence or a muscular weakness issue.
Urge Incontinence
Urge incontinence is something different. This is when the bladder begins to contract before it is full. Normally, the bladder is smooth muscle tissue. When relaxed, it is like an empty balloon. It has sensory receptors built into the tissue. When things normally work as the bladder begins to fill and reaches a certain point, the receptors send information to the brain. "Okay, bladder, you were relaxed, and now you are filling. Now, I want you to contract." It is an urge we feel. Also, "Hey, sphincter muscles, you were a little bit contracted to keep any overflow from leaking out. I want you to relax as the bladder starts to contract to allow the urine to come out." However, with urge incontinence, the bladder begins to contract before it is full. People are usually rushing when this happens. It is also called the "key in the door" syndrome. As they get the key in their home lock, they lose urine as they anticipate going to the bathroom. With stress incontinence, it is a little bit of urine, while with urge incontinence, it is a much larger volume of urine.
Overflow Incontinence
There is also overflow incontinence. This can be due to a blockage like an enlarged prostate. Urine begins to leak out.
Neurogenic Incontinence
There are different neurological issues, like Parkinson's, where the communication between the brain and the bladder is askew. This is similar to what happens with urge incontinence.
Mixed Incontinence
Another type of incontinence that was not listed in the image is mixed incontinence. Mixed incontinence is when somebody has at least two types of these incontinences happening at one time. The most common version of mixed incontinence is stress and urge incontinence. When someone has stress incontinence with increased intra-abdominal pressure, they make a little urine when they cough, sneeze, etc. As this starts happening regularly, they start to come up with strategies. "Hmm, if I'm leaking a little bit of urine, I will start to pee more frequently throughout the day." They think that peeing more often will leave less urine in their bladder so that they are less likely to leak. However, the problem with that is, it does not work. Instead, it creates urge incontinence. The brain starts to go, "Oh, you want me to contract when I'm only partially full?" The person who started with only stress incontinence due to muscular weakness now develops urge incontinence. This is a good example of where clients did not have the right information and created another issue for themselves. People may also limit their fluids. "If I do not drink as much, this will help." This leads to dehydration.
Prevalence of Urinary Incontinence
- 37% of women report UI (stress & urge)
- 86% of this population have stress incontinence
- Average Age:
- 48 - SI
- 55 - Urge
- 61 – Mixed
- A majority of suffers remain untreated
If we look at women, the prevalence of urinary incontinence is very high, with close to 40% of women reporting issues in this area. Stress incontinence is definitely the more common. You can see the breakdown by age, with 48 for stress incontinence, 55 for urge incontinence, and 61 for mixed, but it happens at all ages. You could have somebody with mixed incontinence in their thirties. Studies show that about 40% of women who have had at least one child in their mid-thirties have dealt with or are dealing with stress incontinence. And a majority of the sufferers remain untreated.
Causes
- Chronic UTI, bladder stones, and polyps
- Diuretics
- Atrophic vaginitis
- Diet – caffeine, co2 beverages, alcohol, spicy and tomato-based food
- Neurogenic bladder – SCI, BI, or disease that interrupts nerve conduction
- Overhydration
- Medications – heart, blood pressure, muscle relaxants
We have all seen those Depends and other kinds of adult diaper commercials. I have no issue with people wearing a product like that as a starting point as they start to use strategies that will help them. However, those commercials do not talk about getting control and resolving the issue, only managing it. I do not want to make somebody dependent on a diaper because, ultimately, people can have tremendous success.
When we are working with someone who has urge incontinence, diet can be a factor. Caffeine, carbonated beverages, alcohol, and spicy foods can be contributing factors. I typically tell the client to stop one of those at a time to see if things resolve.
Chronic UTIs can also be a problem with women due to their shorter urethras. Diuretics are also problematic. As women get older, the lining of the vagina gets much thinner, and for some reason, that tends to be an issue.
The neurogenic bladder can be impacted by over-hydrating. Then, of course, there are medications. Some heart and blood pressure medications and muscle relaxants can contribute to urge incontinence. You need to take a broader look and see how many of those factors might be coming into play.
Psychological, Role, and Societal Burden of Incontinence
- Physical Effects
- Bacterial and fungal infections
- Incontinence dermatitis
- Skin tears/pressure ulcers
- Falls & Fractures
- Pain
- Sexual dysfunction
- Psychological Effects
- Anxiety
- Depression
- Loss of self-esteem
- Shame
- Social Isolation
- ADL Effects
- Bladder management
- Functional mobility
- Sexuality
- Leisure participation
- Job performance
- Sleep
- Societal Effects
- Institutionalization
- 16.4 billion/year incontinence care
- 1.1 billion/year
I want to start to focus on OT and the bridge between occupational therapy and pelvic health. I want to make the case where we, as occupational therapists, have unique training that will serve this population very well. I want to stick with incontinence as an example. We are going to look at the physical, psychological, and societal factors that come into play.
Physical Effects
What are some of the physical effects of incontinence? They can get infections, leakage, and skin issues like ulcers. How many people do we know have rushed to the bathroom and fallen? There can also be pain with the different types of bladder issues. It can also lead to sexual dysfunction.
Psychological Effects
If a person is worried about leaking, they may start to restrict activity. "Can I do that activity? Will there be bathrooms nearby? What clothing should I wear?" They start to get anxious, which engages the sympathetic branch of the autonomic nervous system. It has a direct, powerful connection to the pelvic floor muscles. If somebody is dealing with incontinence, it could cause them to disengage and lead to dysphoria, sadness, and depression over time. They can have a loss of self-esteem. Think about it. If a person is going to be intimate with a partner and has stress incontinence or is worried about leaking, this can cause shame and social isolation. They begin to limit their activities because of these different factors. Ultimately, this gets back to sexual dysfunction.
ADL Effects
For ADLS, we often deal with bladder management and functional mobility. We are experts at dealing with all things associated with making people safe in their homes, especially if they have mobility issues. Sex is an important part of an ADL routine. Leisure participation is affected by the disengagement piece associated with leaking. We want to help people get back to engaging and back to being intimate. It can also impact job performance. If a person is getting up to go to the bathroom at night and is sleep-deprived, how does this impact their job performance? We know sleep deprivation leads to cognitive issues over time.
Societal Effects
The societal cost is tremendous. It is estimated that billions of dollars go toward incontinence care. For some older adults, incontinence can lead to institutionalization.
The Gold Standard in PFD Rehabilitation
The gold standard and working not just with incontinence, but all the other types of pelvic floor issues that I've been talking about can be seen in Figure 8.
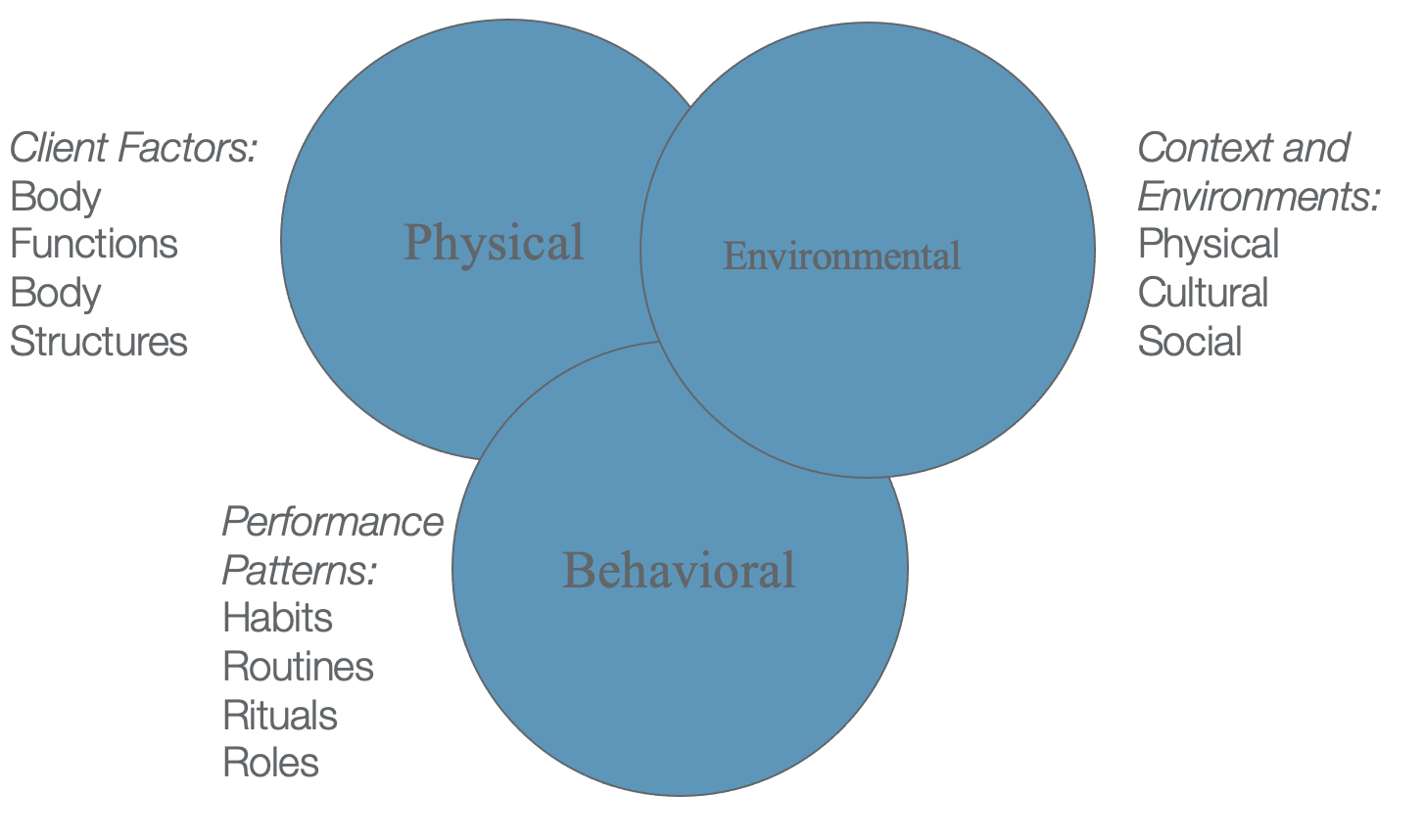
Figure 8. The three areas of pelvic floor dysfunction rehabilitation including physical, environmental, and behavioral factors.
For incontinence, the gold standard addresses the physical, environmental, and behavioral factors. For example, somebody with stress incontinence may have weak muscles, behavioral issues like we talked about, and environmental/physical factors. Does the person rush to the bathroom a lot at night? Are the pathways clear? Is there adequate lighting? Can the person manage their clothing properly? If the person has bad arthritis or incoordination issues, are they wearing the proper garments?
While we should be addressing the physical, behavioral, and environmental factors, more emphasis goes on the physical and less on these other two. In the outer part of Figure 8, you can see the OT framework. We address client factors, body functions, body structures, and behavioral issues. We also look at the persons' habits, routines, rituals, roles, and environment. We not only look at the physical environment but also their culture and social issues. Our basic training has prepared us very well to deal with pelvic health issues. Of course, we do need some additional specialized training to work in pelvic health.
Physical
- When addressing incontinence, an occupational therapy practitioner may:
- Provide preparatory activities to address underlying body structure issues
- Manual therapies
- Biofeedback
- Therapeutic exercises – strength, flexibility, coordination
- Functional activities – strength, flexibility, coordination/ context
As an OT, what would you do to address the physical? When addressing incontinence as an OT, you might use preparatory activities to address underlying body structure issues. There are manual therapies that necessitate additional training. This is where you work directly with the pelvic floor muscles. Biofeedback uses different kinds of electrodes to educate people on how to work with the muscles. Therapeutic exercise works on improving strength, flexibility, and coordination. Remember, it is not just about the pelvic floor muscles. We want to address the whole core and other parts of the body that influence the pelvic region.
Functional activities can do almost everything that therapeutic exercises do. I will give you some examples of that, especially when we get into the experiential part of this talk. As OTs, we do not want just to use exercise as a treatment. We call our exercises therapeutic exercises or preparatory activities to prepare the person for function. We want the body and pelvic floor muscles to support a person throughout the day regardless of their activity.
Environmental
- When addressing incontinence, an occupational therapy practitioner may:
- Focus on mobility and environmental issues limiting quick, safe access to the bathroom
- Height of toilet
- Offer suggestions on garment management for clients dealing with arthritis or incoordination
When addressing incontinence, OTs can focus on the client's mobility and environmental issues for safe access to the bathroom, such as the height of the toilet. I will have a couple of slides about that in a little bit. Higher toilets make it easier to go from sitting to standing, but they can contribute to more constipated people. This can make it hard for the pelvic floor muscles to relax. I will cover this in more detail soon. We can also make suggestions on garments. We work with so many people that have incoordination, whether from neurological or orthopedic reasons.
Behavioral
For behavioral factors, we can talk with the client about modifying their medication schedule if medications contribute to incontinence. We can work with them on planning, voiding, and a liquid intake schedule for bladder retraining. For example, when somebody has urge incontinence and loses a lot of urine from their bladder contracting too soon, I have them get into a routine when they go to the bathroom. I have them count how many seconds ("one Mississippi, two Mississippi...") it takes them to go to the bathroom. And then, after two or three days, I have them come up with an average. "I go to the bathroom every hour and 35 minutes. I pee for nine seconds on average." From there, we work on retraining their bladder with a voiding plan by slowly increasing the amount of time between visits to the bathroom. Over time, we want to train the bladder and the brain to hold on to the urine for longer periods of time. This is looking at treatment from a behavioral and environmental point of view by being very methodical.
Here is something I want you to think about in the next couple of days. We should pee for at least eight to 10 seconds. If you are, on average, peeing for less than 10 seconds, you are probably peeing too often. You would want to retrain your bladder to go for longer periods of time.
We also want to collaborate on strategies for engaging in social and leisure activities. You can let the clients know that they can wear diapers temporarily, but there are things we can do to figure out a better way. I was working with a guy who had Parkinson's and incontinence. He wanted to go to a wedding, but he was worried about going. I worked with him, and we practiced with the specific garments he would wear that day. We found out about the bathroom at the restaurant. I had his son, who took him to the wedding, go to the bathroom first to make sure everything looked as described. They were comfortable with it, and he was able to go over the wedding and celebrate with his family and friends. He had a great time and was successful. We can help clients alleviate their stress and figure out ways for people to make these things work.
When people are dealing with pain, we can help them as we are well-educated in different relaxation and pain management strategies that can be helpful to them.
Cognitive
There can also be cognitive issues. For example, someone who has dementia may not see a white toilet seat in a white room. However, if you put a red toilet seat on top of the toilet, this can help. Both of my parents had dementia. My mom could not find the toilet, but once I changed the color of the toilet seat, she could find it.
Interventions
- Bladder Training/Timed Voiding – increase intervals between voiding by instructing a person to avoid urge…follow a planned schedule
- Biofeedback – learn to relax the Detrusor muscle and abdominal muscles while contracting sphincter muscles
- Pelvic Floor Exercises
- Functional Activities
- Environmental Adaptations
- Clothing Adaptations and Management
There are many different ways that we can support people using a holistic approach. We look at the physical, behavioral, and environmental factors. Above is a list of interventions. We just talked about bladder training and timed voiding. Biofeedback is used if the muscles are weak. We can also instruct in pelvic floor exercises, which I will demonstrate in a little bit. As mentioned earlier, we can use functional activities, environmental adaptations, and clothing adaptations to support this population.
- Medications – Anticholinergics such as Ditropan, Detrol, Enablex can calm an overactive bladder
- Medical Devices
- Urethral insert
- Pessary
- Surgeries
- Sling procedure – uses body tissue or synthetic material to create a pelvic sling/hammock around the urethra and bladder neck
- Bladder neck suspension – provides support to the urethra and bladder neck
- Artificial urinary sphincter – a ring-like device placed around the bladder neck. When the valve is pressed, the ring is deflated.
We do not deal with medications, but it is important to know that if somebody has urge incontinence, they may have medications. Some of these medications have nasty side effects, and I have discovered that some of them can impact memory. The gentleman with Parkinson's was really affected by his urge incontinence medication. Eventually, the doctor took him off of the medications, and he did very well within a one to two-month period.
There are also medical devices that can be helpful, like a urethral insert. I have never used it, but it is like a tiny little tampon that can be pushed into the urethra to block dripping. There is a pessary for women. It looks like a diaphragm that you would use for birth control. It is inserted into the vagina, and it puts pressure against the urethra to stop leakage.
And when things are really not so good, different kinds of surgeries can be done to help people who have not benefited from these other approaches.
Optimum Position for Opening Bowels
What is the optimal position for bowel movements and for people who are constipated? I work with many people who are constipated. Many use medication. Think about how many people around the world squat when they go to the bathroom. Before toilets, people squatted to go to the bathroom. The joke goes that the guy that invented the toilet invented constipation.

Figure 8. Proper squatting position for bowel elimination.
Here is why squatting works. There is a muscle called the puborectalis represented in Figure 9.
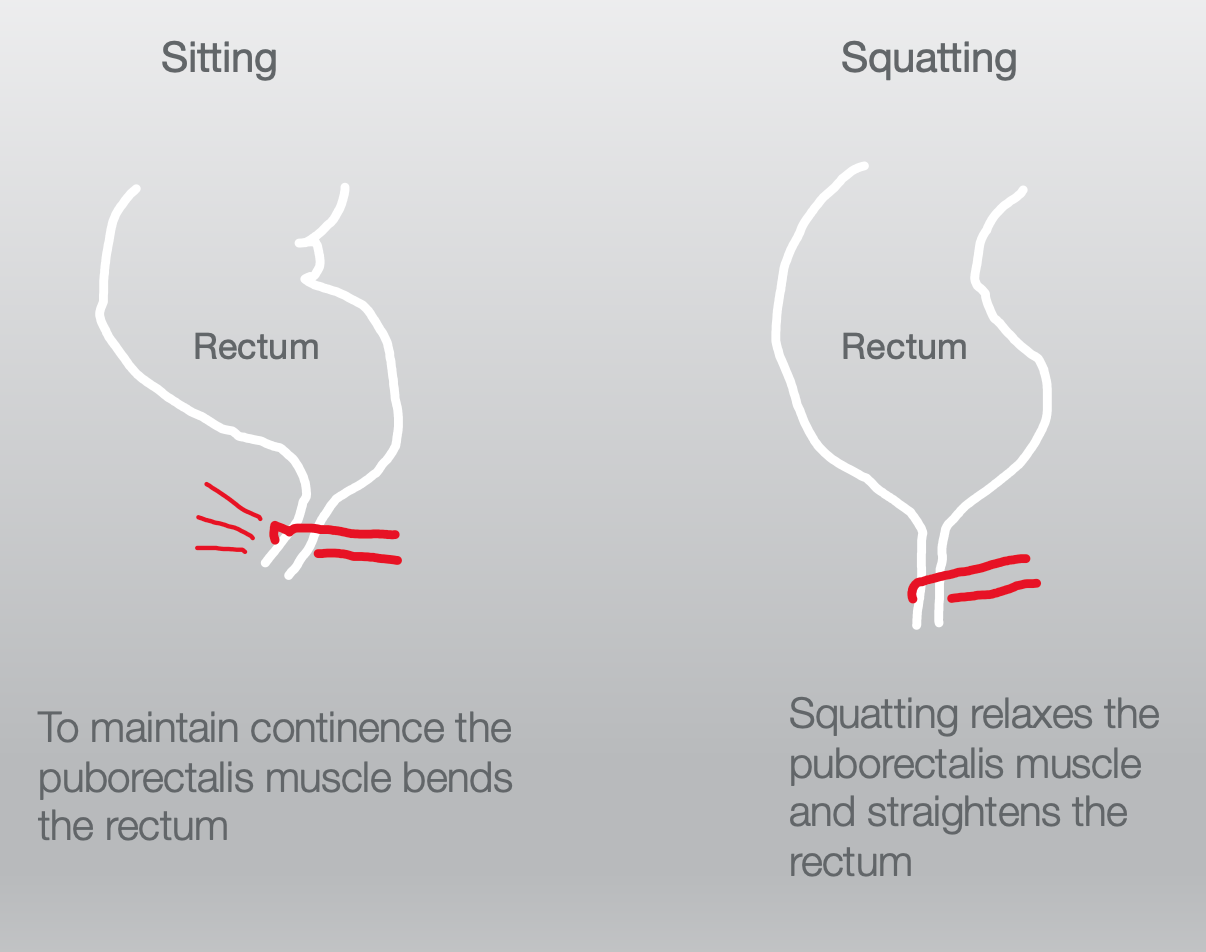
Figure 9. The position of the puborectalis muscle during sitting and squatting. Click here to enlarge the image.
If we sit on a toilet, the puborectalis pulls on the anus and creates a bend. When you are sitting on the toilet, the anus is like a bent straw when you are trying to poop. But, when we squat, the puborectalis relaxes and becomes like a straight straw to allow the feces to come out more easily. Many products elevate your feet to bring your knees higher than your hips when you sit on the toilet. You want to make sure that the person you are working with is cognitively intact enough not to leave whatever device under their feet when they try to stand. Some products move out of the way when you go to stand.
Towards the beginning of our talk, we talked about how the pelvic floor is part of the core. When there are issues with the pelvic floor muscles, there can be core dysfunction. This influences the coordination between the other muscles. It is never about the strength and flexibility of any one muscle. Every muscle needs strength and flexibility. More importantly, how you use and coordinate that strength and flexibility is crucial. Often, there is an overemphasis on the pelvic floor and not the core.
PLISSIT Model
I want to now talk about the PLISSIT model, which many of us have learned about as an approach to sex and sexuality during recovery. This was developed by Jack Anon and can be seen in Figure 10.
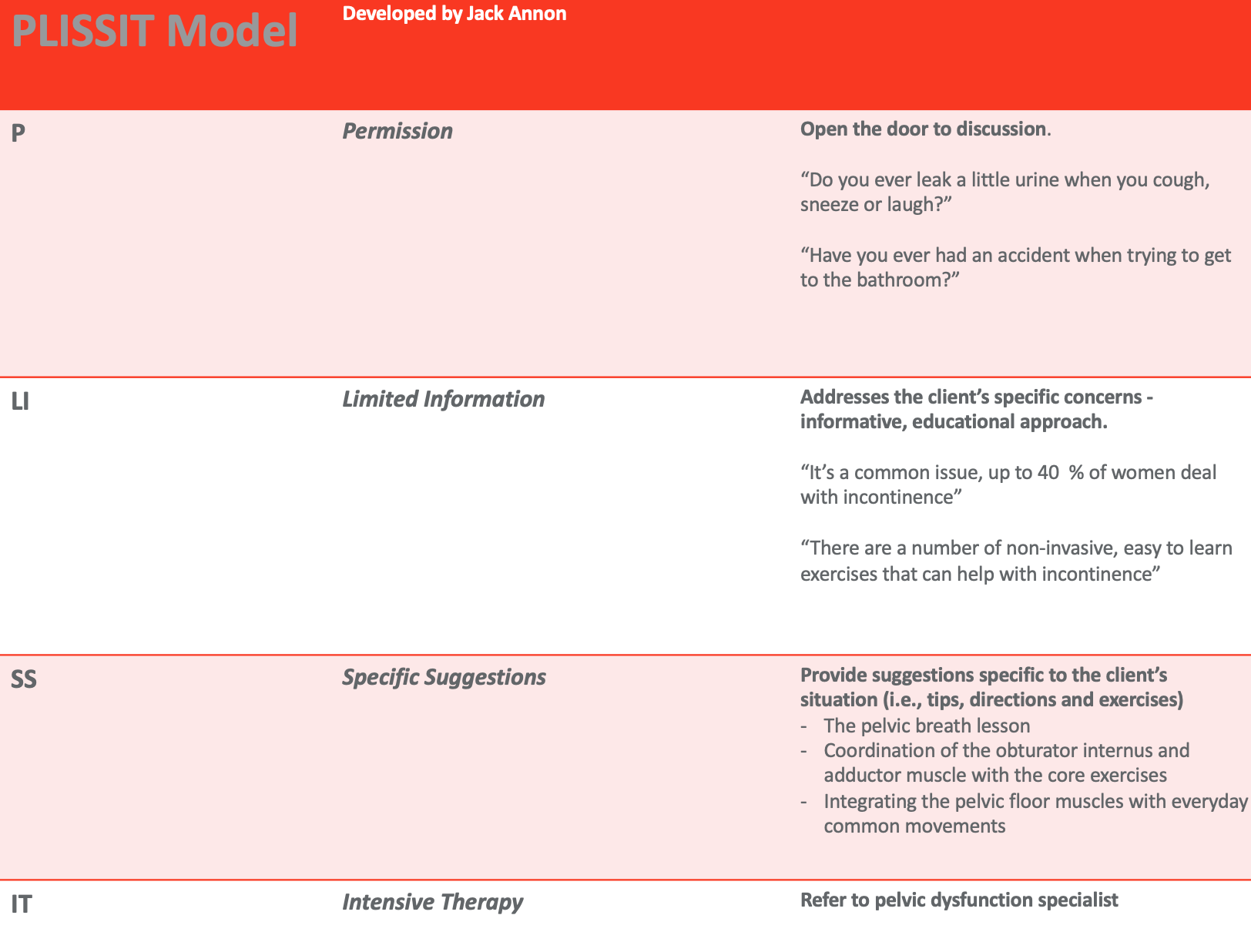
Figure 10. Overview of the PLISSIT Model. Click here to enlarge the image.
The "P" means we give the person permission, the "LI" is limited information, SS are specific suggestions, and IT is intensive therapy. I want to talk through this model in terms of pelvic health. We work with people all the time on ADLs, with one of the areas being toileting. Regardless of our interest in pelvic health, we could ask a simple question like, "Do you leak a little urine when you cough, sneeze, or laugh?" Or, "Have you ever had an accident trying to get to the bathroom?" These are just examples, but they are a way to open the door to a discussion. Even if you are not interested in pelvic health, many people deal with these problems. We need to be able to help them or refer them to somebody that can. This is similar to someone who needs a specialized wheelchair. We can send them to a seating and positioning expert. You may not want to deal with incontinence, but you need to direct them to someone who can help. Thus, I really believe we should all be asking this question or similar questions during that initial evaluation.
The next step would be limited information. Let's say the person does have issues when you ask the question. We can respond, "It's a common issue. You're not alone as up to 40% of women deal with incontinence." Also, you can share, "There's a lot of non-invasive, easy to learn exercises that can help you. You do not have to be dependent on that diaper." I feel that every OT should do this.
The next step is to make specific suggestions. "Today, after spending a little time with me, I'm going to teach you a pelvic breath lesson." This is on your handout because this is the foundation of all the work that I do. I will explain why in a little bit. Other specific exercises are a part of my pelvic health program.
The IT is intensive therapy. Many times the issue is beyond our skill set. It could be somebody who has been abused (sexual or physical abuse) or too complicated. We would then need to find a specialized person for the intensive therapy. We all can do the first two steps, and many could even do the first three steps. However, we all need to refer to that fourth step unless that is all you do and you become highly skilled and trained in this area.
Let's talk again about OT moving into pelvic health or even an area of practice within our profession that becomes well entrenched. For example, when Mary Warren first started talking about low vision, AOTA poo-pooed it. Now, low vision is such an integral part of who we are and what we do. We all learn about low vision, and there are even low vision experts. We all can do a certain amount with clients, and then if it gets a little bit beyond our skillset, we refer to another OT who is specialized.
AOTA's Centennial Vision
During the hundredth anniversary of occupational therapy, AOTA reached out to stakeholders (therapists, people receiving OT, legislatures, insurance companies, payers, etc.) and asked for feedback on the demographics, science, technology, and health care for the next one hundred years. Another question was asked, "What are things that we need to change or that could be obstacles? The bottom quote, "Rigid adherence to the status quo," means that if OT does not grow and evolve, then our profession may ultimately, in the long run, die. All professions need to evolve and grow. Look how much OT has changed, and again, low vision is a good example.
I bring this up because I submitted an article years ago to OT practice on pelvic health. It was accepted, and then all of a sudden, they said, "No, we can't accept that." They even gave me a publication date. They changed their mind saying, "This is really PT, not OT." I talked to them about it, rewrote the article, and addressed some concerns. They accepted it again and gave me a publication date, but they kicked it out again as the practice committee said, "It's not really OT." I got a little frustrated, and I reached out to the practice committee. I let them chat and tell me why they thought it was not OT. I disagreed and stated that pelvic health falls within our framework. Ultimately, they agreed with me. The reason I tell you that is because there was that resistance to change. This happens in life, not just in AOTA. And, if we look at the number of people with this issue, this is an area of practice that we are well-positioned to serve.
Charles Christiansen, the vice-president around this time, had this quote, "There are no facts about the future, only possibilities. These possibilities arise from our knowledge of trends, from our experiences and from our imagination about how the world could be...our vision of these possibilities helps us create the future we want."
Vision 2025
AOTA came out with Vision 2025. Occupational therapy maximizes health, well-being, and quality of life for all people, populations, and communities through effective solutions that facilitate participation in everyday living. From what I have shared with you, many people deal with pelvic health issues and are forced to disengage and not fulfill their roles. Their routines are greatly altered.
Mary Reilly
I hope many of you are familiar with this quote from Mary Reilly. "Man through the use of his hands, as they are energized by mind and will, can influence the state of his own health" (Mary Reilly, 1962). When I was in OT school, it really moved me the first time I read this, "Man through the use of his hands, as they are energized by mind and will, can influence the state of his own health." And I love that quote. It's still. I can get emotional if I sit and think about those words. I am framing it to read, "Man through the use of his body, as energized by mind and will, can influence the state of his own health." I put the body there because I am sure Mary Reilley used the term "hands." After all, that is a unique feature of human beings. I am sure she meant the whole body.
Back in the day, people would draw a line through the body saying that OTs work from the waist up, PTs from the waist down. Remember, AOTA was initially resistant to thinking about OTs and pelvic health. On Facebook, there is a private group called OTs for Pelvic Health. There are almost 3,000 members at this point. I remember when that group started several years ago, it was minimal. There is another group WomensHealth4OT that has over 4,000 members. Occupational therapists are moving into issues of pelvic and women's health. We are a profession of predominantly women. Why would we not think about women's health? If a mother has just given birth and has pelvic floor issues with leaking or pelvic pain, she may have trouble lifting her child from the stroller or putting them on the changing table. They may develop varicose veins, carpal tunnel, or whatever. Wouldn't it be nice to know that you, as an OT, would be able to help this mom on a broader level? Remember, we may not do it all, but it is important to ask the right questions and refer them if they need more help.
Easy Does It: An Occupational Therapy Based Pelvic Health Program
- 8-week program
- 1X/week for 1½ hours
- Handouts provided on all of the lessons
- Assessments
- Kings Health Questionnaire
- Limitations in daily activities, personal relationships, emotions, sleep/energy, general questions on how bladder problems impact on quality of life
- Personal Activity Scale
- Participants select 2 activities that are important to them and rate their current satisfaction and performance
- Weekly Check-in
- pelvic pain
- the benefit of today’s session
- how many times did you experience leakage
- how would you rate the impact of your leakage on your everyday life
- how frequently have you practiced
- Kings Health Questionnaire
I want to take a few minutes and tell you a little bit about a group I have been doing. It is the "Easy Does It: An Occupational Therapy Based Health Program." I have been working for a while now in pelvic health and have pulled together many different activities and people. I work one-on-one, and pelvic health is a small part of my practice now. However, I like to do groups in the community and just did a project with students from SUNY Downstate, where I teach. It was an eight-week quality assurance project where we worked with 12 older adults. It turned out that the group happened to be all older women, even though this was open to people of all ages. We are going to do the study again this fall and make it bigger. For this study, we did it through Zoom because of COVID, and people were given handouts.
We did three assessments at the beginning. The first was the King's Health Questionnaire. This is used in a lot of pelvic health research, and it is excellent. We kept it to incontinence because, as a study project, we did not want to deal with all pelvic health issues. However, all the techniques I used in this group could be used for all the different types of pelvic health issues I have already alluded to. The King's Health Questionnaire looks at how incontinence limits daily activities, personal relationships, emotions, sleep, and in general, how the bladder problem impacts their quality of life. It is based on a Likert scale. Then, we used a personal activity scale, sort of like a modified Canadian Occupational Performance Measure. We had people identify two activities that were impacted by incontinence and rate them on a 10-point Likert scale. They rated their current performance and satisfaction with these activities. We did a pre and post-test for the King's Health Questionnaire and this personal activity scale. After each session, we also gave them a 10-point Likert scale to reflect on their pelvic pain and other questions. How do you feel today? How do you rate the benefit of this session? How would you rate the impact of your leakage on your everyday life? We also had them think about how frequently they practiced? We wanted to know who practiced and who did not.
We found that after eight weeks, everybody improved significantly, and the more people practiced, the better they did. In the group, I had particular lessons as opposed to exercises that we did. We are going to do some in a few moments. And then informally, we addressed behavioral issues. For example, we would talk about the distinctions between stress and urge incontinence. I gave everybody a home safety checklist to look at their homes and see what things might be going on that would be risk factors like rushing to get to the bathroom. We addressed the behavioral and environmental factors. The lessons themselves were specific to the body structures and functional level.
I want to add this little quick snippet. In the seventh week, one of the participants said, "Can I talk about the elephant that is in the room?" I thought, "Oh gosh, what is she going to bring up?" She says, "We've been talking about the pelvic floor for all these weeks, and we haven't focused on sex." I said, "Thank you for bringing that up." So, I asked the group of all older women over 65, "Do you think that this should be a group that focuses on sex and sexuality." Unanimously, they said, "Yes." I share that only because I do a lot of work in geriatrics. We tend to think that older adults are thinking about sex or that it is not that important to them.
The group context works extremely well. One of the key things about pelvic health is social isolation. People in the group were able to support each other and share ideas. We are starting to reach out to urologists, gynecologists, and OB-GYNs that are part of the medical center and trying to broaden the population of people in terms of age. Again, we want to keep it to incontinence issues for this particular
