Kathleen: It is my sincere pleasure to be back with you all and presenting on this topic.
Introduction
State Survey Guideline
Here are state survey guidelines that relate to long-term care which is where I think we see most of our restraints. The requirements of participation for long-term care were updated over the last couple of years, and they are called F tags and are listed below. All of these are guidelines that relate to physical and chemical restraints particularly F604 and F605.
- F600 Free from Abuse and Neglect
- F602 Free from Misappropriation/Exploitation
- F603 Free from Involuntary Seclusion
- F604 Right to be Free from Physical Restraints
- F605 Right to be Free from Chemical Restraints
The requirements of participation for long-term care were updated over the last couple of years, and they are called F tags and are listed above. All of these are guidelines that relate to physical and chemical restraints particularly F604 and F605.
Additional state survey guidelines say:
- The responsibility of IDT (interdisciplinary team) to assess and provide the least restrictive environment
- The facility must design interventions to minimize medical symptoms, and identify and address problems causing the medical symptom
Medicare Regulations
I want to now get into the actual Medicare regulations.
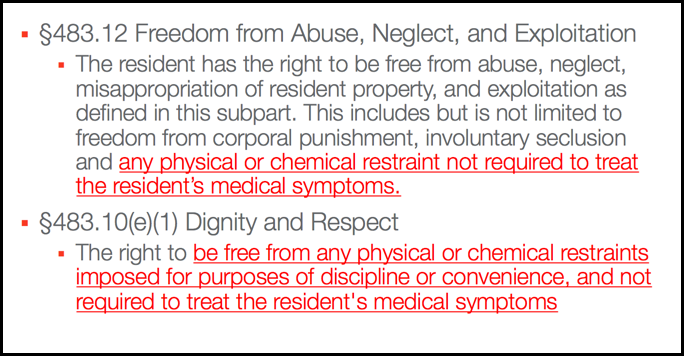
Figure 1. Medicare regulations 483.12 and 483.10 (e) (1).
The first one is 483.12, Freedom from Abuse, Neglect, and Exploitation. The resident has the right to be free from any physical or chemical restraint, not required to treat the resident's medical symptoms. I know this sounds pretty basic, but interestingly enough, the definitions are pretty specific. The next is 483.10, subsection e1. This states that the resident has the right to be free from any physical or chemical restraints, imposed for purposes of discipline or convenience. This again is not required to treat the resident's medical symptoms. Next is 483.12, subsection a2.
Figure 2. Medicare regulation 483.12 (a) (2).
The facility needs to ensure that the resident is free from physical or chemical restraints for discipline or convenience, and they must use the least restrictive alternative for the least amount of time and document ongoing re-evaluation of the need for restraints. There is nothing in the requirements that say we have to be restraint free. Somebody could potentially have a restraint provided that it is, in fact, the least restrictive restraint. The takeaway here is that when you look at what CMS or Medicare wants and what the state survey guidelines state, the facility needs to minimize the use of restraints and design interventions to minimize the medical symptoms and the problems that might be the reason why we are applying the restraint. Often as therapists, we get referrals or requests to look at a restraint. This is not really our role. It needs to be an interdisciplinary process.
Physical Restraint Definition
Physical restraint is any manual method, physical or mechanical device, equipment, or material that is attached or adjacent to the resident’s body, cannot be removed easily; restricts freedom of movement. To break it down, let's look at these words:
- Convenience
- Discipline
- Freedom of movement
- Manual method
- Medical symptom
- Position change alarms
- Removes easily
Convenience is defined as the result of any action that has the effect of altering a resident's behavior such that the resident requires a lesser amount of effort or care, and it is not really in the person's best interest. Discipline is defined as any action taken for the purpose of punishing or penalizing a person. Freedom of movement means that any change in position or place or part of the body that the person is able to control. This is really important because if the person does not have a movement that you are taking away, then why are we using the restraint in the first place? It may not be considered a restraint if we are not truly restricting freedom of movement. Manual method means to hold or limit voluntary movement by a method of contact or physical restraint. A medical symptom is an indication or a characteristic of a physical or psychological condition. Position change alarms can be viewed as restraints. Finally, "removes easily" means that the physical or the mechanical device can be removed intentionally by the resident in the same manner in which it was placed. Let's say somebody is using a lab buddy, and through the course of fidgeting with that throughout the course of the day, they remove it. That is not intentional; they have to be able to remove it by request or upon command. It also needs to be removed in the same way that staff would remove it. If it is a bed rail, they need to be able to put that bed rail down the same way that staff would put that bed rail down.
Examples of Restraints
Some examples of things that would be considered restraints are:
- Bed rails that keep a resident from getting out
- Placing a chair close to a wall to prevent rising
- Using a concave mattress
- Tucking in a sheet tightly so it prevents movement
- A chair that prevents rising
- Devices such as trays, tables, cushions, bars, belts
- Hand mitts, soft ties, vests
- Holding a resident down
- Enclosed framed wheeled walker that cannot be opened
- Some position change alarms
We often use bed rails or different things as "enablers" to help a person roll or move. Is that a restraint? The question becomes are we preventing them from getting out of bed or taking away some movement that potentially they would have by putting that enabler in place? If the answer is yes, then it is considered a restraint even though it is still an enabler or a positioning device. Other examples are placing a chair or a bed too close to the wall so that it prevents the person from getting up from a chair, putting them on a concave mattress so they cannot get out of bed, tucking in a sheet so tightly that they cannot get out, or fastening their clothing in a way so that it restricts their movement. Placing somebody in a chair like a beanbag or a recliner that prevents them from getting up is another one I have seen. Using devices like a tray or a table in front of the patient that they cannot move away are also considered restraints. Arm restraints, hand mitts, vests are other restraints. Holding someone down in response to behavioral symptoms during the provision of care is obviously a form of restraint. Placing a person in an enclosed frame like a Mary Walker where they cannot exit the device is also a restraint. Lastly, position change alarms are another form of restraint that we will talk about in a second.
- Reclining geri-chair
- Upright geri-chair with a lap tray
- Devices that “hold” resident in the chair
- Seat belt, not self-releasing
- Lab buddies that cannot be removed
Any device that holds the residents in the chair like a reclined position or lap trays is a form of restraint. This includes seat belts that are not self-releasing or that the person cannot release and also lab buddies.
Examples of Convenience
We cannot apply restraints solely for the purpose of discipline or convenience. Additionally, the facility is prohibited from getting permission from the resident or the resident representative for the use of restraints when it is not really necessary to treat the resident's medical symptoms. On the flip side, family members cannot come to the facility and request restraints. Surveyors are looking for a medical condition that requires the use of the restraint. Examples of convenience that are not acceptable include:
- Staff are too busy to monitor the resident
- The resident does not exercise good judgment
- Staff state the family has requested
- Not enough staff
- Temporary staff do not know the resident
- Lack of staff education regarding alternatives
- Teaching the resident a lesson
- Preventing wandering
- In response to confusion or combative behavior
Staff may state that the resident is in the restraint because they are too busy to monitor them, or they think that the resident does not exercise good judgment and do not wait for assistance. Another reason may be that the family has requested it because they are afraid that their loved one is going to fall. There may not be enough staff on a particular shift, or it could be a new or temporary staff member using the restraint that does not know the patient and how to deal with behavioral symptoms. There also could be a lack of education. There could be negative feelings toward the resident, and they want to teach the resident or the patient a lesson so they put them in a restraint. It might be in response to wandering, confusion, or combativeness. They may need to hold the person down to provide care. This particular example differs from an emergency situation where staff would briefly hold a person down for the purpose of providing medical care in a life-threatening situation. All of these are unacceptable.
Chemical Restraint Definition
Chemical restraint is when a medication is used to treat a medical symptom. The facility needs to use the least restrictive alternative for the least amount of time, provide ongoing reevaluation, and not use that medication for discipline or convenience. This is a hot topic right now for Medicare. They are looking at psychotropic medications that might be used for convenience, or where there is not a medical symptom. Facilities are strongly encouraged to address these. In this case, the definitions for physical and chemical restraints are not any different; convenience and discipline are the same. Indication for use is defined as a documented clinical rationale for administering a medication based on the assessment of the patient. There are therapeutic goals, and then it also needs to be consistent with the manufacturer's recommendations, evidence-based practice, medication references, and clinical studies.
Examples of Medications Considered Chemical Restraints
Some examples of medications that could be considered chemical restraints are those listed below.
- Antipsychotics
- Antidepressants
- Antianxieties
- Sedatives
An example would be a medication to calm down the resident. Another example is where the staff recommends to the physician that the resident is administered a medication to prevent behaviors. These behaviors may be things like wandering into somebody's room, calling out, or yelling. Staff may be frustrated with a resident who is continually requesting staff assistance or always putting on the call light. Nursing may want medications to subdue or sedate the resident when they do not have enough staff, or they restrict the patient to a sitting or lying position by sedating them. They may want the medications to subdue clients during ADL routines. In these examples, the staff did not really assess the patient's behaviors and look at non-pharmacological options.
Double Restraints
A double restraint is just what you think it is, two restraints. It could be two physical, two chemical, or one of both. This is a serious concern for us. Keep in mind that if the person is able to remove that restrictive device upon command or request, it would not be considered a restraint. Again, it has to be in the same manner that it was applied or taken off by a staff member. Documentation is key, and it needs to be a team effort.
Restraint Related Issues
Let's now go through some restraint-related issues.
Reasons for Restraint Use
- Confusion and cognitive impairment
- Weakness and debilitation
- Climbing out of bed
- Getting up out of the wheelchair
- Falls
- Inability to follow weight bearing precautions
- Wandering within the building
- Wandering outside the building
- Inability to maintain a sitting position
- Pulling out tubes or catheters
- Physical aggression
- Yelling and calling out
- Lack of knowledge about restraints
We see restraints used because folks are climbing out of their bed, getting up out of their wheelchair and falling, wandering, or pulling out their tubes. They may have aggression or are calling out. Rather than applying a restraint, we need to figure out what the root cause is and address that.
Physical Risks Associated with Restraints
There are many physical risks associated with restraints.
- A decline in physical functioning
- Dependence in ADL/mobility, strength, balance, ROM
- Respiratory complications
- Skin breakdown
- Incontinence or constipation
- Injuries
- Accidents such as falls, strangulation, or entrapment
There can be a decline in physical functioning. We can also see skin breakdown, particularly in the area where this restraint is. If it is a seat belt and somebody's shirt rides up, we may see rashes or some wounds in those areas. There can be issues with both the respiratory and digestive systems because the person is not getting up and moving. There can also be accidents like strangulation or entrapment. Poor appetite, dehydration, edema, decreased blood volume, decreased bone mass, and decreased metabolism may be some issues that are seen.
Psychosocial Impact from Physical Restraints
There can also be a psychosocial impact from physical restraints.
- Agitation, aggression, anxiety, delirium
- Social withdrawal and depression
- Feelings of shame
- Loss of dignity, self‐respect, and identity
- Dehumanization
- Panic, feeling threatened or fearful
- Feelings of imprisonment
- Increased anger, combativeness, hostility
There can be dehumanization or feelings of shame. There can also be a loss of confidence, feelings of helplessness, feelings of being imprisoned, social withdrawal, loss of dignity, and disorientation. The list could go on and on.
Psychosocial Impact from Chemical Restraints
There is also a big impact from chemical restraints.
- Subdued, sedated, or withdrawn
- Asleep during hours that he/she would not normally be
- Limits to functional capacity
- Loss of autonomy, dignity, self-respect, and orientation
- Confusion, cognitive decline, withdrawal, depression
- Decreased activity levels, including social activities
- Decline in skin integrity
- Decline in continence level
- Weight loss if missing meals
These issues are very similar to what we have already seen with the physical restraints. The person can be subdued, sedated, and withdrawn. There is a loss of autonomy, dignity, and self-respect. There is also a decline in mobility. We might get called in for these folks for "behavior issues." It is important that all facilities know the effects of the medications on their patients. If the medication has a sedating or subduing effect, and it is not administered to treat a medical symptom, that medication is a chemical restraint. The client may be subdued intentionally or unintentionally. It might be a side effect that we were not anticipating. In the case of unintentional chemical restraint, the team needs to go back and review the plan.
Resident Rights
Residents have the right to be free from any physical or chemical restraints imposed for the purpose of convenience or discipline and not required to treat the medical symptoms. This is taken directly from the regulations.
Restraint Myths
Here are some of the myths related to restraints.
- Restraints prevent falls and injury.
- Restraints safeguard residents from harm.
- The facility is at risk if restraints are not used.
- A resident feels secure when restrained.
- Restraints decrease the risk of falls.
- There are no other alternatives.
- Restraints can substitute for nursing care.
- Restraints are effective to manage resistance and control behaviors.
There are more falls with restraint use because folks are trying to get out of them. For example, they are climbing up over the bed rails, over the edge of the bed, sliding underneath restraints, etc. There can also be the risk of strangulation. There are many other alternatives to restraints, and they cannot substitute for good nursing care.
