Introduction
This is our third presentation in a series on therapeutic modalities. I would love to thank the fantastic team at OccupationalTherapy.com for providing me the opportunity to present on these topics. I also want to welcome everyone back who has attended the first and second courses. Today, we are going to be talking about a very comprehensive subject, electrotherapy. I am going to package this comprehensive topic into a two-hour presentation and provide an overview of key points. I will be discussing the different types of electrotherapy and how to apply this to different patients or clients. There are textbooks that go way more in-depth. Please consider this as more of an evidence-based overview of all the different electrotherapy modalities. I am an adjunct faculty in the MSOT program at California State University, Dominguez Hills. All that we will be talking about today will be framed for the occupational therapist, looking at the biopsychosocial model and how we can progress a client's rehabilitation strategy using electrotherapy.
Agenda
- Module 1: Basic Science
- Module 2: Indications, Precautions, Contraindications, and adverse effects
- Module 3: Treatment Parameters
- Module 4: Electrodes, Placement, and Patient Hygiene
- Module 5: Electrotherapy Application
- Module 6: Documentation
In Module 1, we are going to cover the basic science and the physics behind e-stim modalities. Module 2 will look at potential precautions, contraindications, and adverse events. Module 3 will review the treatment parameters. This is how you set up the machine. Module 4 will look at the interface between the e-stim machine and the patient and the use of the electrodes. We will also talk about electrode placement and patient hygiene.
The application of the different e-stim modalities will be next in Module 5. There are four main categories of e-stim. You are trying to depolarize the motor neuron to get a muscle contraction or number two is you are trying to control pain. The third category is tissue healing, and number four is using it as biofeedback. Those are really the four main categories: activate a muscle, decrease pain, heal tissue, and provide some biofeedback. There are many different machines that fall into these four categories. I will break this down into more simple categories and will highlight what we have to do to get the desired effect within those categories within Module 5. Module number 6 is going to go over documentation. Throughout each of these modules, we will be reflecting on the current evidence as well.
Module 1: Basic Science
History of Electrotherapy
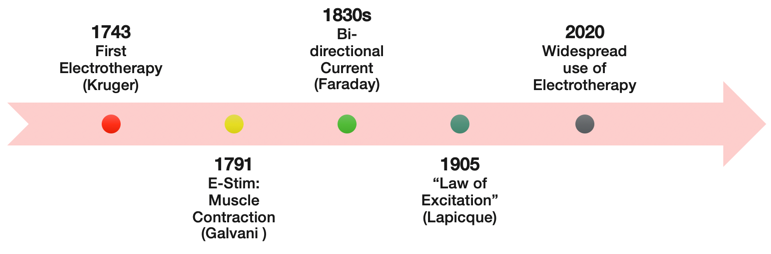
Figure 1. Timeline of electrotherapy.
The first documented form of electrotherapy used therapeutically was in 1743. As we fast forward to 1791, we see that Galvani came up with the muscle stimulator. Faraday used a bi-directional current in 1830, and then in 1905, Lapicque founded the Law of Excitation. Now in 2020, there are many forms of electrotherapy, e-stim, that are used all over the world for different purposes. Figure 2 shows an earlier use of this technology.

Figure 2. Early use of electrotherapy.
Phases of Tissue Healing
- Things for the Occupational Therapist to consider:
- When is the optimal time to use electrotherapy during a patient’s rehabilitation program?
- How will electrotherapy enhance the tissue healing process and the patient’s overall recovery?
- The optimal sequencing of interventions (including e-stim) in the patient’s rehabilitation program.
Are you going to use it pre-manual therapy? Are you going to do it post-exercise? Where does e-stim fit into your rehabilitation strategy? Right? Here is a look at the phases of tissue healing in Figure 3.
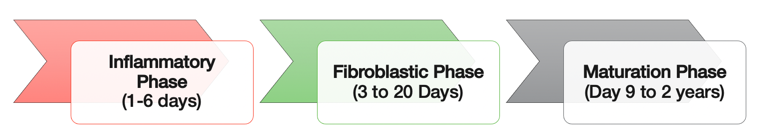
Figure 3. Phases of tissue healing and timeline.
Based on the patient's healing process and all the factors that you found in your evaluation, how is e-stim going to be beneficial to them?
We also use e-stim for pain control with TENS units. In the first presentation in this series, I talked about pain science and the pain neuro-matrix. How are you going to affect your patient? Are you trying to activate a muscle? Are you trying to control pain? How is this going to facilitate and/or progress them through it? I have been in practice for almost 20 years. Back in the day, everyone got e-stim and ultrasound. Now, we have progressed from that and only use e-stim modalities to help us with our treatments. It is an adjunct to a comprehensive strategy.
What is Electrotherapy?
- Basic Definition
- A group of modalities that use an electrical current to induce a physiological effect on the body.
- Electric current: A flow of charged particles
- Electrons and Ions
- Electric current can flow in one or both directions
- Electric current can flow between the anode (+) and cathode (-) (Figure 4)
- Cathode = active electrode

Figure 4. Electric current flows between the positive anodes and negative cathodes.
(Cameron & Sutkus, 2017)
Electrotherapy is a group of modalities that use electrical current to induce a physiological effect on the body. It is based on an electrical current through the body. It is that simple. As the electrical current flows through the body, it creates a mechanical effect. You can also stimulate other tissues and the central nervous system to create opioid responses. The basic foundation is that you have a positive (anode) and a negative (cathode) electrode. The electricity will either go one way or back and forth between these electrodes. This is why when you look at e-stim machines, there is a channel one and a channel two. There is also a red wire and a black wire. In general, the cathode (negative) is the active electrode and where you are going to feel the most tingling.
Electrotherapy Nomenclature
- Direct current (DC): A continuous stream of charged particles flowing in one direction.
- Alternating current (AC): A continuous, sinusoidal, bidirectional flow of charged particles.
- Frequency (rate): Number of cycles (for AC) or pulses (for PC) that occur per second.
- Hertz (1 Hz = 1 cycle/second) or pulses per second (pps)
- Amplitude (intensity/strength): The magnitude of the current flow.
- Amps or volts
- Phase: Period when electrical current flows in one direction.
- Pulse: Period when electrical current flows in any direction. May include one or more phases.
When we look at nomenclature, there are quite a few terms we have heard over the years. Direct current (DC) is defined as a continuous stream of charged particles and flows in one direction. Alternating current is similar to what we get when we plug something in. It is a continuous sinusoidal, bidirectional flow of charged particles. It goes from positive to negative, but it is continuous. When we look at the frequency or the rate (speed), it can be described as the number of cycles or the number of pulses. This is typically described in Hertz or pulses per second. We will cover this in the coming slides, but I wanted to plant the seed now. The amplitude is the intensity or the strength of the tingling. This is defined as the magnitude of the current flow. You are turning up the intensity of the machine, and it is measured in amps or volts. This depends on what type of unit you have in your clinic. The phase is the period where the electrical current flows in one direction. Lastly, we have a pulse or a period where electrical current flows in any direction. This may include one or more phases. When charting, you want to document what machine you used, the frequency, amplitude, and the pulse/seconds. I will share some examples of this later in this talk.
When we apply an electrical current to a person, they are obviously going to have some type of efferent sensations that go up to the brain. You can see these in Figure 5.
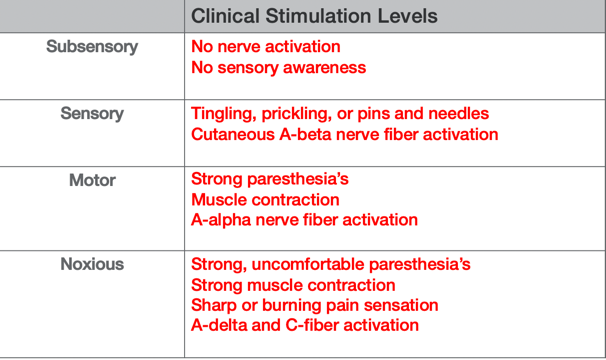
Figure 5. Sensory chart adapted from Behrens, Beinert. Physical Agents Theory and Practice. 2015. FA Davis
There are typical sensations from different clinical stimulation levels. One is sub-sensory where there is no nerve activation or sensory awareness. There is a sensory level where the patient may feel tingling, prickling, pins, and needles, and that may be more of a continuous nerve fiber activation. There is also a motor one where they are going to feel those paresthesias and also get a visible motor contraction. Finally, there is noxious stimulation where it is very painful. E-stim covers all four of these. We want the patient to feel a strong tingling, but we do not want it to be painful. Obviously, we want to depolarize an alpha motor neuron, then we want to go into the motor level.
Current is a continuous flow, and there are three different classifications: direct current, pulsed, and alternating. Let's go over those now.
Direct Electrical Current
- Direct Current (galvanic): A continuous unidirectional flow of charged particles.
- Device: Battery
- Not used often due to the discomfort.
- Electrodes: one anode (+) and one cathode (-) for the entire treatment
Direct current (Figure 6) is defined as a continuous unidirectional flow of particles. It typically comes from a battery. It is not often used as it is very uncomfortable as the electrical current flow goes simply from the positive to the negative in a continuous manner. Figure 6 shows an example of that.
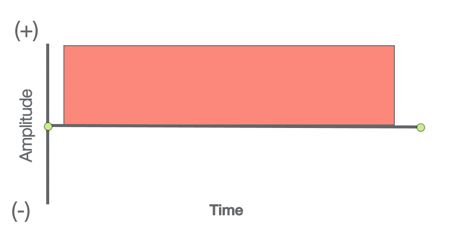
Figure 6. Example of a direct electrical current.
We see the amplitude over a period of time. The direct current is also unidirectional. The center line is zero with the height representing amplitude or the intensity. To make it higher, you turn the machine up.
Pulsed Current
- Pulsed Current: An interrupted flow of charged particles. The current flows in a series of pulses separated by a period of no current.
- Unidirectional or bidirectional
- Device: Battery or wall.
- Electrodes: AC or DC
Pulsed current (Figure 7) can be both unidirectional or bi-directional. It can go back and forth between the electrodes instead of going one way. Instead of going from positive to negative or negative to positive, it can bounce back and forth between those. Typically, these devices are battery-powered, or they come out of the wall. A pulsed current is defined as an interrupted flow of charged particles in between the pulses. Basically, we have the tingling as it comes on, it turns off, it comes on, it turns off, etc.
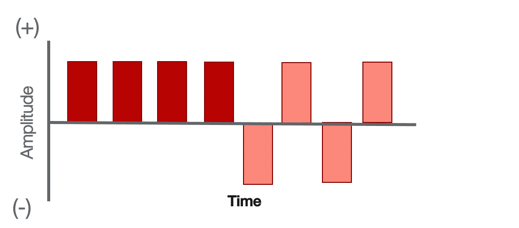
Figure 7. Example of pulsed content.
Now, depending on your pulse width, the client may feel it turn off or they may not. It depends on the sensory level what you feel, but the point about pulsed current is it's not a continuous flow, there's a gap or a rest period in between pulses. And I think that that's important to define because a lot of pulsed currents are used and they have some good research behind them. I want everyone to understand that the pulsed current is that it could be unidirectional or bi-directional, and there is a rest period or a kind of a latency period in between pulses,
Alternating Electrical Current (AC)
- Alternating Current: A continuous sinusoidal, bidirectional flow of charged particles.
- Device: Wall.
- Current flows back and forth between polarities.
- Electrodes: change polarity throughout treatment
We can see here as we go up and down in Figure 9. It is a continuous sinusoidal or an oval bi-directional flow of charges. It is continuous and does not stop. Typically, these are done out of a wall like a wall unit, but we could see that if you hooked up two electrodes, the electrical current would just bounce back and forth between negative and positive electrodes (Figure 8).
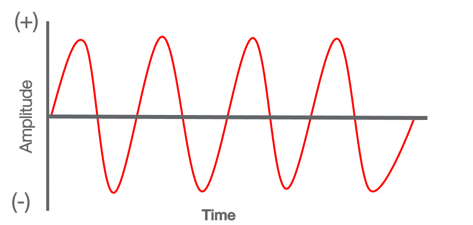
Figure 8. Example of alternating current.
The patient may not feel the electrical current go back and forth, and they may just feel the active electrode called the cathode. Many patients say, "I just feel it in one electrode." However, with an alternating current or some type of bi-directional current, understand that the current is going back and forth between those two electrodes. We now dig a little bit further where we have defined AC current. pulsed and DC current (Camerson & Sutkus, 2017). Those are the big things. There are also some subtypes of AC currents that we need to understand.
AC Current-Inferential Current (IFC).
- Interferential Current: Two different AC currents are delivered across an area by the same device via 2 channels.
- Interference is caused when the two waveforms intersect.
The first one is actually my favorite, is interferential current, and we will simply call it IFC to be quick. IFC is interesting because it is considered an alternating current, but it is unique where they use two channels. If you look at the diagram below, and I will lay this out (Figure 9).
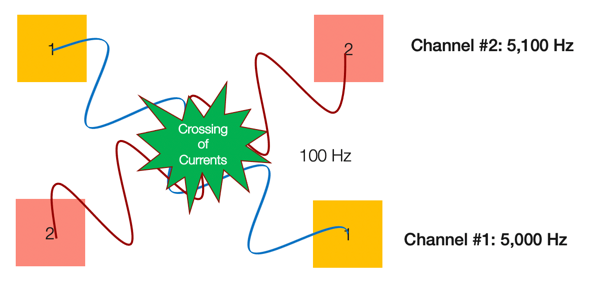
Figure 9. Example of interferential current.
IFC requires a second channel with a different positive and negative frequency: 5,100 Hertz. For set-up, you set up four pads with two different channels and then cross those over the target area. In the example, you can see the electrode currents are crossing over. Once you turn on the machine, these alternating currents are going to be sending two different currents back and forth between channel one and channel two. When they intersect each other, they are going to cause a disruption in that area and a low-level stimulation of 100 Hertz.
Over the years, I have gotten some really good results with controlling pain with interferential current especially postoperatively or during an acute inflammatory phase. I will target the area of injury like an ankle sprain with this type of set-up. If I cross the area with the two channels, and I turn on the interferential, I create a disruption of the pain fibers. This could be considered the gate theory of pain or whatever philosophy you want to look at as far as pain science. I am going to create a disruption in that area and confuse the nervous system to help it to accommodate. Accommodation is where the body gets used to it. We are going to fatigue those nerves and accommodate it via these two waveforms crashing into each other and creating this disruption. I think interferential is great technology. I prefer it out of all of the electrical currents I have used over the years. I have a portable unit that I use. They come in many forms, but something to consider if you are looking for really good pain control. Here is another diagram here of the two channels in Figure 10.
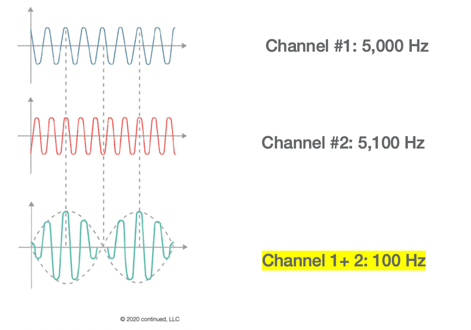
Figure 10. Another example of interferential current.
There are two AC, continuous waveforms with one slower and one faster. Once you cross them together, they are going to crash into each other and develop this interference in the target area. Additionally, the net Hertz is going to be a lower value so the patient may not feel it as much. This is what I like about it. You can turn up the intensity, and for some reason with interferential and those two channels crossing, they do not feel it as much like a TENS or some of the other units.
AC Current- Premodulated Current.
- Premodulated Current: AC current with sequentially increasing and decreasing current amplitude.
Another waveform or another AC current is called pre-modulated. This is already set in the machine where the AC current goes through these sequential increases and decreases of amplitude as seen in Figure 11.
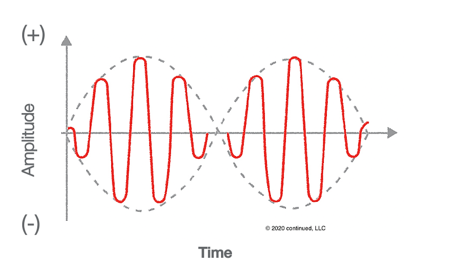
Figure 11. Example of a premodulated current.
The patient is going to feel the tingling increase, decrease, increase, decrease. At the sensory level, they are going to be feeling this modulation or this adjustment in the current flow while the machine is on.
AC Current- Russian Protocol.
- Russian Protocol: AC current designed for muscle strengthening.
- Frequency of 2500 Hz delivered in 10-ms-long bursts with 50 bursts per second, with a 10-ms interburst interval between bursts.
Our last AC current is called the Russian protocol (Figure 12).
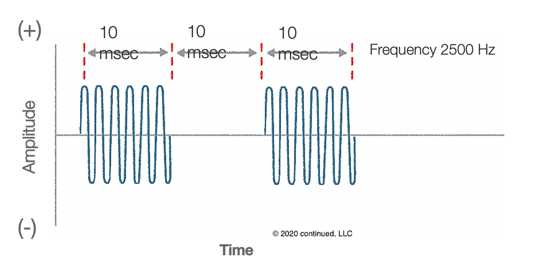
Figure 12. Example of Russian protocol.
It is going to turn on for 10 seconds, and then turn off for 10. There is going to be a burst of electrical current and then a break. It is designed to activate the motor neurons by depolarization using this frequency. So, if you are trying to strengthen a muscle that has been denervated or atrophied, the Russian protocol is a great one to use. Over the years, I have found that it can be uncomfortable because of that burst mode. A lot of your newer combo units that have like eight or 10 waveforms will have this. It is pretty standard with a lot of new machines.
We talked about the different currents so now let's look at the different waveforms: monophasic and biphasic (Cameron & Sutkus, 2017).
Waveforms
Monophasic Current.
- Monophasic Current: An intermittent unidirectional current
- Pulse current
- Electrodes: one (+) and one (-) electrode
Monophasic has that break in between so it is intermittent. You have a period or a pulse where you feel the tingling turn on, it may turn off, turn on, turn off, etc. The patient may or may not feel that depending on how much rest period you give in between. If you are using a monophasic current for trying to strengthen the muscle, you might do 15 seconds on and five seconds off (Figure 13).
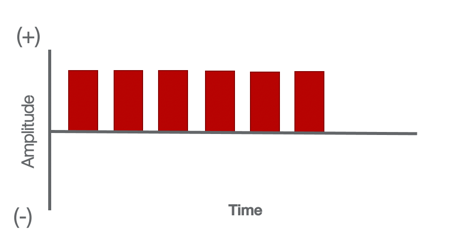
Figure 13. Example of a monophasic current.
The client is going to feel the tingling come on and then feel it come off. You want them to volitionally contract while that is happening. Monophasic currents are typically where the electrical current goes from one electrode to the other in one direction and not back and forth.
Monophasic: High-Voltage.
- Hi-Voltage Current: A monophasic waveform made up of pulses, each composed of a pair of short, exponentially decaying waves that travel in the same direction.
- Pulse current
- Electrodes: one (+) and one (-) electrode
A modified monophasic current is called hi-voltage. It is interesting because you have this sudden spike with a quick increase in amplitude with a quick drop (Figure 14).
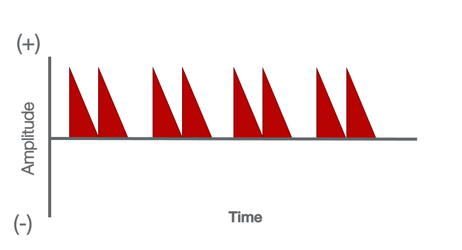
Figure 14. Example of a modified monophasic current.
It goes from like zero to 50 and then backs down to zero. It is intermittent, but hi-voltage has been used for things like strengthening and tissue healing. We know it is a pulsed current, and we know that the current goes one way because it is monophasic. Hi-voltage is going to feel a little bit stronger than some of the different waveforms that are used. This is something to consider because a lot of times clinicians will shy away from monophasic currents as they are more painful. Many people prefer biphasic as it is less strong but still gets the same physiological effect.
Biphasic Current.
- Biphasic Current: An intermittent bidirectional flow of charged particles. Electrodes change polarity.
- Symmetrical: Both phases and the total current are the same.
- Balanced Asymmetrical: Different phases. The total current is the same.
- Unbalanced Asymmetrical: Different phases and total current.
In this waveform, the electrical current goes back and forth between electrodes with changing polarities. It moves back and forth, and we have three different subtypes of biphasic currents. We have symmetrical where the waveforms are very symmetrical. We also have a balanced asymmetrical where one pulse may be one shape, and then the next pulse might be a shorter one. The third one is called unbalanced. One waveform might be more intense, and as it changes to the other, it might be a shorter waveform. These can be seen in Figure 15.
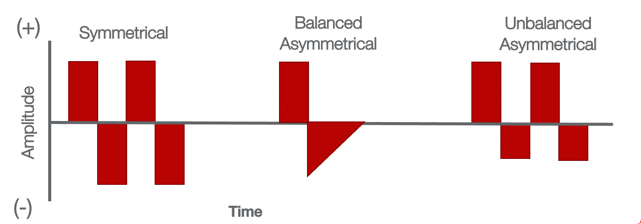
Figure 15. Types of biphasic currents.
Depending on the protocol that you use, you may program the machine to do a balanced asymmetrical or unbalanced based on your desired physiological effect. The patient is not going to feel that the waveforms are asymmetrical. The client may just feel the tingling. Depending on the protocols, the research, and what your machine can do, you will program that for the desired effect. Biphasic has different currents that work on the body in different ways. In summary, we defined what e-stim is. We talked about the different currents. We also talked about the different waveforms. We are now going to take a look at the physiological effects.
Physiological Effects
- E-Stim: Nerve depolarizing requires a specific amplitude and duration (strength/duration curve)
They all have different physiological effects on the body.
- Depolarize Sensory Nerves (AP)
- Depolarize Motor Nerves (AP)
- Ion Effects from Direct Current
- Mechanical Effects/Chemical Effects
E-stim focuses on depolarizing either the motor nerve, the alpha motor, or some type of afferent mechano-receptor or nociceptive pain fiber. It can also be used to drive medication like iontophoresis. Typically, this is a direct current. As we are sending electrical current into the body, we are going to be getting local mechanical effects, vibration, cellular movement, a neuroendocrine response, and chemical changes. We are still going to have all the basics with all the waveforms and different currents. Remember with all the currents and waveforms, you are going to be impacting the client in different ways. However, what are you going to do with that electrical stim modality? Are you trying to activate the muscle? Are you trying to activate the nerve fibers? Are you trying to drive medication? Are you trying to heal? Are you trying to give biofeedback? When you are sending a current into the body, you need to have a reason and make that part of your treatment plan.
Depolarizing sensory nerves vs. motor nerves.
- Sensory Nerves: Lower amplitude/ short pulse duration.
- Pulse duration: 50 to 100 µs (50 to 100 x 10-6 sec)
- Amplitude: Depends on patient tolerance and desired effect.
- Motor Nerves: Higher amplitude/ longer pulse duration.
- Pulse duration:
- Very small muscles: 100 to 125 µs (100 to 125 x 10-6 sec)
- Most muscles: 150 to 350 µs (150 to 350 x 10-6 sec)
- Amplitude: Depends on patient tolerance and desired effect.
- Rheobase: Minimum amplitude with long pulse duration to produce AP in any tissue (units of current amplitude).
- Chronaxie: Minimum duration it takes to stimulate the tissue at 2x rheobase intensity (units of time or duration
- Pulse duration:
If you are trying to activate a sensory nerve to say decrease pain, you would use a lower amplitude with a shorter pulse duration. This would be like 50 to 100 microseconds. The amplitude is going to be lower because you do not want to stimulate the motor fibers. If you are trying to activate a motor nerve to get a muscle contraction, then obviously you would have a longer pulse duration and turn up the intensity or the amplitude. In general, research says that if you are going to try to activate very small muscles like in the hand or the face, you would use a 100 to 125 pulse duration. Other muscles are anywhere between 150 to 350. Stimulating muscles are not going to be as comfy or relaxing as activating a sensory nerve for pain. As you turn up the intensity on any machine, you are eventually going to drive so much current into the area that you are going to depolarize a bunch of nerves both motor and sensory.
On that note, there is a term that I want to familiarize you with called rheobase. Rheobase is defined as the minimum amplitude with a long pulse duration to produce an action potential in any tissue. Another term is chronaxie. Chronaxie is the minimum duration it takes to stimulate the tissues at two times the rheobase intensity. These two terms are used in all the science textbooks. We will talk more about this in the coming modules, but I want everyone to understand the basic settings to activate sensory and motor fibers.
Ionic Effect.
- DC current (Ionto) is used to repel ionized drug molecules to increase transdermal drug penetration.
- Ion Flow: Like charges repel; opposite charge attract
There is also an ionic effect. Sometimes, we can use a direct current with this iontophoresis to drive the medication into the skin through a transdermal route. If you are using Dexamethasone or using lidocaine, you would flip the leads on your machine so that the ion flow was positive to positive. It is going to repel those ions and push them into the skin. We are using the basic concept that ion flow, like charges, repel and that opposite charges attract. Your dispersion pad with iontophoresis could be positive, which has the medication, and then you make sure you set the machine to repel the ions of the medication to the other electrode. This will help to drive that medication into the skin and into the myofascial tissues. Remember, it is a direct current, but it does not feel very good. Again, this is mainly meant to drive medication through that transdermal route.
Mechanical Effects/Chemical Effects.
- Tissue healing/cellular activity
- Galvanotaxis (cell movement)
- Cell activation
- Antimicrobial effect
- Enhanced circulation
We can use some of the mechanical and chemical effects to heal tissue. Like I mentioned before, we get cell movement called galvanotaxis and cell activation that can affect the mitochondria. There can also be an antimicrobial effect and enhanced circulation.
Bottom Line
- Occupational Therapist considerations:
- E-Stim Currents:
- DC: Iontophoresis (low level), muscle contraction
- AC: Pain control or muscle contraction
- Pulsed: Pain control, muscle contraction, and tissue healing
- Biphasic: Most common waveform used in electrotherapy. Symmetrical most comfortable and good to activate large muscles
- Treatment goal should determine desire physiological effect
- E-Stim Currents:
Direct current is typically iontophoresis, but it can also be used for muscle contraction. AC currents are mainly used for pain control and muscle contraction. Pulsed currents are mainly used for pain, muscle contraction, and tissue healing. When we talk about waveforms, biphasic is the most common because it seems to feel the best. Remember the treatment goal should determine the desired physiological effect.
Module II: Indications, Precautions, Contraindications, & Adverse Events
Clinical Indications
- Pain modulation
- Promotion of tissue healing
- Improving muscle strength
- Improving motor control
- Transdermal drug delivery
- Biofeedback
There are many clinical indications for e-stim as noted above. Those are the big categories. Obviously, there are more treatment areas like functional electrical stimulation.
Precautions and Contraindications
- Precautions
- Cardiac disease
- Poor sensation
- Malignant tumors
- Skin irritation
- Poor mentation
- Open wounds
- Contraindications
- Pacemaker
- Carotid sinus
- Nerves, veins, and eyes
- Unstable arrhythmia
- Thrombophlebitis
- Pregnancy
- Impaired sensation/circulation
We covered a lot of these areas in the first two presentations. Many are similar to this modality as well. Specifically though for e-stim, we need to use a little bit more precaution with a pacemaker. If you look at some research, there are studies that have shown that you can use electrical stim with the new insulated, tech-savvy pacemakers and defibrillators, but in general, most clinicians consider a pacemaker as a contraindication. There are also a couple of studies that have used e-stim during the later stages of pregnancy. There is still some controversy around that because of Braxton Hicks contractions. Those are the two areas that are debatable. E-stim has been used during birth to help calm down the pain versus using opiates. For me clinically, I like to err on the side of caution, and I do not try to risk it.
Adverse Events
- Burns
- Skin reaction from electrode adhesive
- Cross-contamination
- Cross infection
- Tissue burn/skin irritation
- Electrodes should be in good condition
- Each patient gets their own electrodes
- Monitor throughout treatment
Then we move to adverse events like burns, skin reactions, cross-contamination, and cross infection. These are pretty straightforward. The electrodes should be in good condition. Each patient should also get their own electrodes, and they need to be monitored throughout the treatment. Besides all my teaching and my research, I also do some legal work. Two weeks ago, I had a brand new case where a female patient had surgery on her knee. The physical therapist was using EMS to get a muscle contraction. The patient said that he used the same electrodes for over a month. In one of her last sessions, she felt a big burn in her quad with a red bruise. She came home and experienced a lot of pain. She went to the doctor, and they found out that she had a third-degree burn in her quad from the electrical stim unit. We are currently in discovery. As I read the notes and learning more and more, but at this point, I have come to the professional conclusion as an expert that the standard of care was breached by using outdated old electrodes. We will talk more about electrodes later, but for some reason, that old electrode caused a hot spot in the electrode and that caused a third-degree burn. The patient had to have surgery where they opened up the muscle and clean it all out. As an expert for the PT board of California, I get these types of cases on a yearly basis. It is so important to monitor throughout treatment. This goes for all modalities including hot and cold packs. I am getting a least five to six cases a year when it comes to unsupervised, busy clinicians.
Bottom Line
- Occupational Therapist considerations:
- The precautions and contraindications discussed are not all-inclusive and others may exist.
- Screen the patient before Tx will ensure a safe session.
- Patients may find e-stim painful.
- Try a shorter pulse duration and increase amplitude slowly over time.
- Try using larger electrodes
- Consider other treatments if the patient cannot tolerate after modifications.
Make sure you understand your precautions and contraindications, screen the patient, and be safe. If the client finds e-stim to be painful, try a shorter pulse duration and increase the amplitude slowly over time. Or, you can try using bigger electrodes. And again, if they cannot tolerate it, move on, and try something else.
Module III: Electrotherapy Parameters
This is an important module because this is how you program the machine. Most machines are preset, but you need to know what is going on when you set it because most machines only give you simple settings of pain, strengthening, and so on. We need to know how the electrical waveforms are programmed in each machine.
Phase
- Phase: Period when electrical current flows in one direction
- Phase duration: How long the phase lasts in microseconds (10−6 seconds)
Remember the phase is a period when the electrical current flows in one direction (Figure 16).
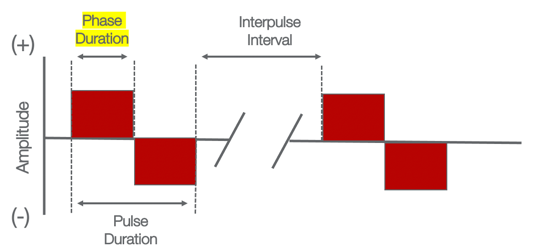
Figure 16. Example of a phase.
The phase duration is how long it lasts, and a phase duration could be on either side. It could be monophasic or even biphasic. And, it could be on both sides.
Pulse
- Pulse: Period when current flows in any direction.
- Pulse duration (width): The time from the beginning of the first phase of the pulse to the end of the last phase.
- Microseconds (10−6 seconds)
A pulse is when we are charting pulses per second. It is a period of time. As you can see in Figure 17 at the bottom, you can see it is a period of time that includes the phases.
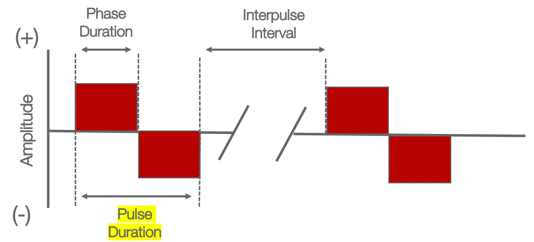
Figure 17. Example of a pulse.
This does not matter where the current flows. It is a period of time that includes the phases. You could have a pulse duration of 100 or 200 sec, and that may include two or three different phases. Remember, the pulse duration helps us understand if we are trying to stimulate the different tissues. We can see that the biphasic uses a shorter pulse duration to make it more comfortable for people. I think it is a big one to hang on to because the pulse duration, shorter or longer, may stimulate different tissues at different times.
Interpulse Interval
- Interpulse interval: Amount of time between pulses
When we look at the interpulse interval, this is the latent period or the rest period in between the different pulses. You can have a pulse that comes on for 10 seconds and then you have an interval of five seconds, and then the pulse turns on again. Interpulse intervals are the break between pulses or spikes in the current (Figure 18).
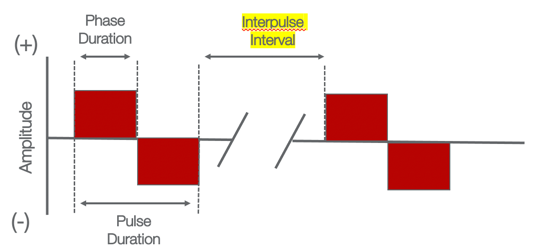
Figure 18. Example of an interpulse interval.
Frequency
- Frequency (rate): The number of cycles (for AC) or pulses (for PC) that occur per second.
- Hertz (1 Hz = 1 cycle/second) or pulses per second (pps)
Frequency is important because it is the number of cycles for AC or the number of pulses for pulsed current. Most of the time we chart it as pulses per second (Figure 19).
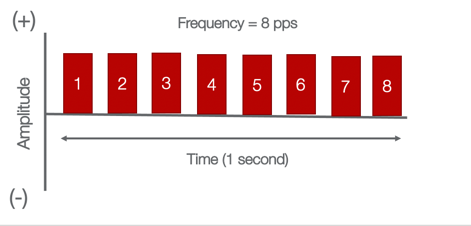
Figure 19. Example of frequency or pulses per second.
If we have these intermittent spikes, we would chart that the frequency was set at eight pulses per second. Thus, the waveform is going to have a very rapid increase, decrease, and then break repetitively. This is going to determine your physiological effect.
Amplitude
- Amplitude (intensity/strength): The magnitude of the current.
- Amps or Volts (E.g. range of 1 to 10)
The magnitude is set in amps or volts. If you look at a typical unit, this is usually one through 10 (See Figure 20).
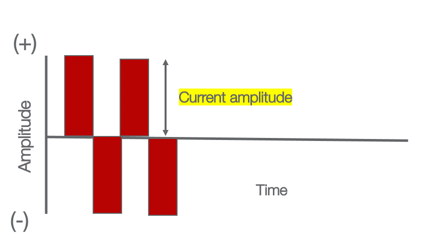
Figure 20. Example of amplitude.
The higher the column is the higher the intensity or amplitude.
On/Off Time
- On/off time: Amount of time current is on and off
- E.g. Muscle stimulation devices
- Ratio:10 sec on/50 seconds off = 1:5 on:off ratio or time.
Another thing to consider is your on and off time. This is typically used with a muscle stimulator. You are trying to activate the motor neuron but you cannot keep it on all the time because you are going to fatigue the muscle and perhaps create a spasm. Neuromuscular electrical stimulating units, NMES units, will have a specific on and off time. This is similar to that interpulse period, but this is really a defined on and off period. Figure 21 shows this.
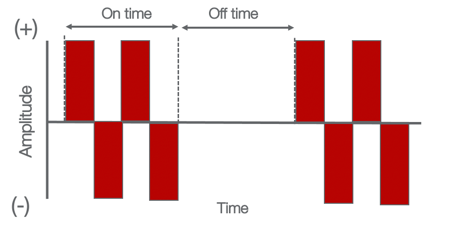
Figure 21. Example of on/off time.
The off time is when the muscle can rest and regenerate adenosine triphosphate or ATP. Remember that most electrical stimulators have a preset or a custom set of on and off times.
Ramp Up/Ramp Down Time
- Ramp up/ramp down time: The time it takes a current to increase from zero to maximum amplitude.
Figure 22 the maximum amount of time for the current to ramp up and then back down.
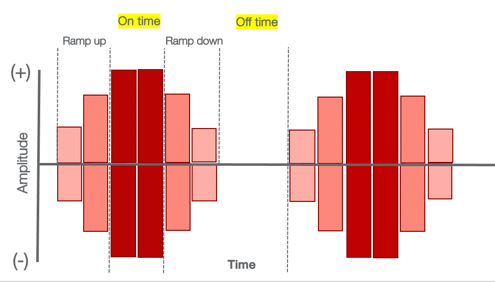
Figure 22. Example of ramp up and down time.
Ramp times are a great way to get the patient during muscle stimulation to actively contract the quad, hold it for that 10 seconds, and then relax it as an example. You should set your ramp time to allow the person to recognize the tingling and to volitionally contract the muscle, hold it at that maximum voluntary contraction (MVIC), hold it, and then start to relax it as the tingling ramps down. You then give them a break to recover, and then you go through the same cycle. I love using ramp up and ramp down times because that does not fatigue the patient as much. If I have a post-op patient like an ACL repair with atrophy in the quads, I love to use electrical muscle stim early on to get them to activate. Once they are able to activate the muscle, they get that motor pattern returned and then progress to active assist-active motion. In the early phases of reeducation or if you have somebody who has some type of neurological disorder, you are trying to get them to activate.
Bottom Line
- Occupational Therapist considerations:
- Different e-stim modalities have different settings that require the clinician to have a working knowledge.
- Matching the e-stim modalities with the phase of tissue healing and patient needs will optimize treatment.
- Accommodation: Nerve becomes gradually less responsive to e-stim over time. Treatment may require periodic adjustments (e.g. increase amplitude, etc.)
When we talk about parameters, different units have different settings. The manual will give you the settings. If you work with other professionals, they may show you their protocols as well. You need to chart all of these parameters. You to this number one to protect yourself legally. Number two is another clinician should be able to pick up your chart or click on your chart in an EMR to replicate the treatment.
If you are using e-stim on a patient over time, they will start to have accommodation. That means the nerves and tissues in the area may become less responsive. They become used to it. You may have to change your amplitude or the pulses per second. I have had this happen before. I will go and check in on someone and they say they do not feel it anymore. I will then turn up the amplitude. The body is always going to accommodate the electrical stimulation so you should actively monitor this and make adjustments as you need.
Module IV: Electrodes, Placement, Patient Hygiene
Electrodes
- The interface between the patient and the e-stim machine
- Common types of electrodes:
- *Disposable flexible adhesive electrodes (self-adhesive)
- Re-usable carbon-impregnated silicone rubber electrodes (need conduction gel)
- Electrodes embedded in conductive fabric (gloves or garments)
- Water immersion
Electrodes are the interface between the patient and the e-stim machine. There are a lot of different electrodes that are out there. You get what you pay for. You can go on Amazon and buy cheap, disposable, and flexible ones. There are also reusable carbon ones. There also electrodes that are permanent. These are the old-school ones with conductive fabric. You put gel on these. Lastly, there are ones that you can use in water. I had a therapist who used water immersion electrical stim in a metal hydrocollator. This obviously was not a great idea. Again, you get what you pay for. Electrodes can be very expensive in a clinical setting, and insurance does not pay for them. In my opinion, for patient safety, you need to buy good quality, reusable electrodes. I do not use a ton of e-stim in my practice, but when I do, I use nice electrodes.
Electrode Hygiene
- Hygiene: Patients get their own electrodes. Renew every month.
- Shelf-life: Electrodes last the longest if good quality, stored on a plastic sheet, and sealed in a plastic bag.
- Dried out electrodes: Current delivery is less uniform causing uneven current density. The areas with good conductivity will have a higher current which can cause a skin burn.
Everyone should have their own electrodes. In fact, you can punch a couple of holes and stick these in their exercise chart. And, in my opinion, you should renew these every month. In my practice, I sell some products like foam rollers, stretching straps, e-stim machines, and electrodes. If you can circumvent the cost of electrodes by selling some basic products like Biofreeze and some basic stuff in your clinic, then you can circumvent the cost. This is how I did it in my practice, and it works out pretty well because it covers costs for all your basics.
It is generally recommended that you store them on a plastic sheet and seal them in a bag so that the adhesive does not dry out. Died-out electrodes can cause issues. This is what happened with a recent legal case. The electrode dried out, and the current delivery was not uniform through the two-by-two electrode. Thus, the electrode had a hotspot and caused a third-degree burn in the client's quad area. Remember, electrodes are your interface. When we are multitasking or supervising techs, we have to make sure to control the most important variable which is patient safety by using good electrodes. I am getting these cases coming through that are a result of simple mistakes.
Electrode Shape/Size
- Shape/Size: The electrode size, shape, and type should depend on the treatment goals, treatment area, and desired physiological effect.
- Minimize burns: 2 x 2-inch electrode or higher ( 2 x 4-inch preferred)
The shape and size of the electrode definitely affect the treatment area. Look at the pictures in Figure 23.
Figure 23. Examples of electrode shapes and sizes.
On the left, you might choose to use a smaller electrode, whereas, you may want to use larger electrodes on a bigger area like the back. It depends on your goal and waveform.
Electrode Placement
- Distance: Electrodes close together = superficial current
(Cameron & Sutkus, 2017)
The distance of the electrode makes a huge impact on the tissues (Figure 24).
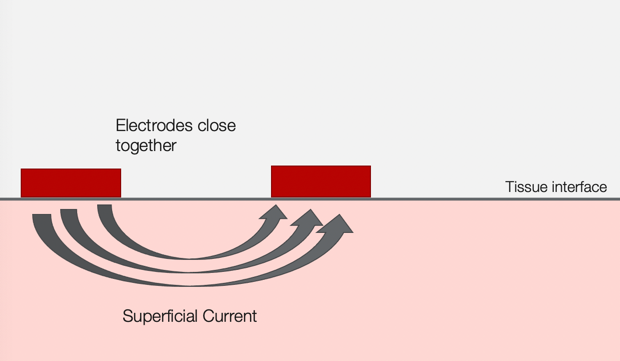
Figure 24. Example of superficial current.
Here is the rule of thumb: If the electrodes are closer together, the electrical current is going to be more superficial. And, if it is a DC current, it is going to go one way, and if it is an AC current, it is going to bounce back and forth. You may choose to do this over the bony areas like the ankle or the hand. You may want to put the electrodes close together and want to use a smaller 2 x 2 electrodes.
If you are treating a larger area like the low back and based on the anatomy, you might need a deeper current to get through the thoracolumbar fascia, the lats, et cetera. In these cases, you are going to spread out the electrodes as in Figure 25.
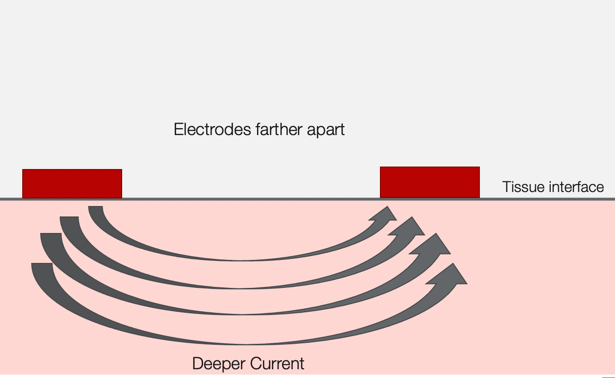
Figure 25. Example of deeper current.
You might want to also use the larger two by four or larger electrodes. The distance of your electrodes needs to reflect your desired outcome.
Tissue Impedance
- Tissue impedance (resistance to current flow)
- Tissue type: Impedance/conduction vary with different tissues
- Tissues (high water content):
- Decrease impedance and increased conductivity.
- Tissues (high water content):
- Tissue type: Impedance/conduction vary with different tissues

Figure 26. High water content tissues.
- Tissues (low water content):
- Increases impedance and slow down conductivity

Figure 27. Low water content tissues.
When we look at tissue impedance, this is the resistance to current flow. For example, if we are working the lower back, we know that the electrical current has to travel through multiple tissues.
And, different tissue types have different impedance and conduction properties. Tissues with high water content decrease resistance and they increase conductivity. Electrical stim modalities are good for the deeper skin layers, nerves, and muscles. In tissues with low water content, the resistance is increased, and it slows down the connectivity of the current. This includes bone, fat, tendon, fascia, and epidermis. Thus, you have to consider what your target tissue is and the desired outcome.
You also need to factor in electrode placement. This is an important take-home point because regardless of what current you use, biphasic, monophasic, or waveforms, it is not going to matter unless you properly place the electrodes. Again, if you are going to go into deeper tissue like the lumbar spine or the quadricep, then you are going to distance the electrodes for a deeper effect. If you are wanting a more superficial application, you are going to move the electrodes closer together. You may also hist some tissue impedance and need to make adjustments. We need to be thinking about these factors whenever we apply the modality. We can write directions out in the chart or make a diagram. You then want to check the application if you are supervising an aide.
- Recommendations
- Try and reduce impedance as much as possible in order to use the lowest intensity for patient comfort.
- Impendence can be reduced by:
- Cleaning the patient's skin prior to treatment
- Removing excess hair around the treatment area
- Warming the treatment may reduce impedance
- Adipose tissue: an area with increased adipose may require a higher amplitude or intensity to create the desire response. This may be painful for the patient. E-stim should be D/C’d if too painful.
Here are some recommendations. You can reduce impedance by doing some other best practices. Cleaning the skin is an obvious one. It is also important to use new, proper electrodes and remove excess hair around the treatment area. Sometimes warming up the treatment area can reduce impedance because it increases blood flow. Lastly, we need to look at adipose tissue as it slows down the current. Adipose is an insulator so if you are targeting an area with a lot of adipose, you may need to increase the amplitude to create the desired response.
Patient Hygiene
Here are some best practices that we talk about. Steps one through six. We've used a similar scenario for all the other presentations, but I'm going to go through one through five right now (Figure 28).
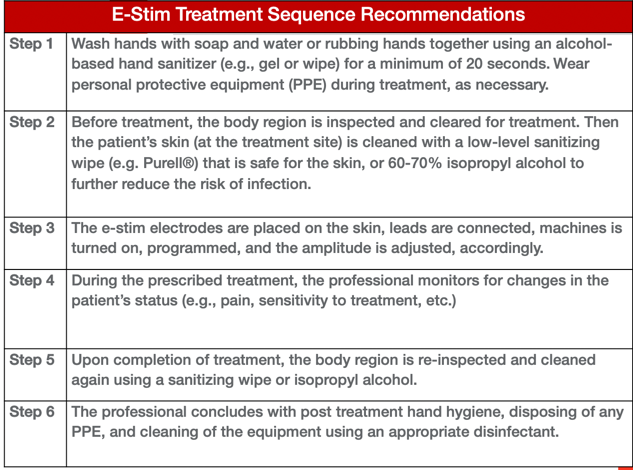
Figure 28. Steps for using e-stim.
First, you need to wash your hands and wear PPE. Number two is you need to prep the area of the patient's skin. Whenever I apply e-stim to an area, I wipe the area with an alcohol wipe. Step three, I apply electrodes, hook up the lead wires, program the machine, and then adjust the amplitude. Step four, I monitor them during the prescribed treatment time. If I am using ice or heat, I make sure there is no water to decrease cross-contamination. Remember, even an ice bag or a gel pad can carry bacteria. Once the treatment is completed, I am going to reinspect the area and wipe everything off. I will also wipe off the machine and discard the PPE. For the electrode leads, you can simply wipe those off and let them dry. I would not do like the metal part but just the plastic outer covering.
Bottom Line
- Occupational Therapist considerations
- Electrode distance should match the target tissue depth
- Patients get their own electrodes (never share)
- Defective or old electrodes can burn the patient
- Monitor patient throughout each e-stim treatment
- Following the recommended e-stim treatment sequence to help prevent any adverse events (e.g. cross-contamination, burns)
In summary, especially for this unit, we understand that electrode distance should match the target depth. Again, for safety and sanitation, patients get their own electrodes as defective older electrodes can burn. You need to monitor them throughout and follow the prescribed treatment sequence. The big step in that whole sequence is wiping off the patient's skin before you apply the electrodes in order to reduce contaminants like sweat from prior intervention.
Module V: Electrotherapy Application
Muscle Contraction
- Terms:
- Neuromuscular Electrical Stimulation (NMES)
- Functional Electrical Stimulation (FES):
- *Simulation of muscle contractions
- Goal: Depolarize nerve and stimulate nerve AP
- Waveforms:
- Strengthening/re-education: Biphasic pulsed/Russian protocol
- Spasm reduction: Biphasic pulsed/Russian protocol
- Edema control: Biphasic pulsed/Russian protocol
- Denervated muscles Direct current
E-stim for muscle contraction in its essence has several terms. A lot of times people call it NMES or neuromuscular electrical stimulation. It is also called a muscle stimulator. If you are doing a functional activity like with someone post-stroke or with a spinal cord injury, this might be termed FES. There are portable electrical stimulators that turn on a muscle in a synchronous fashion. The different waveforms that can be programmed in these machines are biphasic, pulsed, or the Russian protocol to build strength. Strengthening protocols do exist, and yes, you can improve someone's isometric strength and their concentric eccentric strength, but there are limitations. Nothing replaces someone actually working out. However, if you have somebody who has had surgery, has been sedentary, or are atrophied, you can strengthen and reeducate. The preferred waveforms for these instances are biphasic or Russian. Biphasic seems to be the most comfortable for a lot of different things.
Muscle stimulators are used for spasm reduction, edema control, and a denervated muscle. Sometimes they do a direct current which is much more powerful and can be much more uncomfortable for patients. Again, you can see the utility of a biphasic current where the current is going back and forth between the electrodes. This is more comfortable and is more efficacious than some of the other currents.
- Indications: Healthy individuals and MSK conditions
- Muscle strengthening (Type 1 and 2)
- Post-ACL reconstruction
- Post-TKA
- Patellofemoral Syndrome
Sports
Now when we look at specific indications for muscle contractions, it is used for muscle contraction of Type 1 or Type 2 muscle fibers, post-ACL reconstruction, post total knee, patellofemoral, sports performance, and cardiovascular performance. Those are the main indications for healthy individuals and individuals with musculoskeletal or MSK conditions.
- Indications: Cardiac and Neurological Conditions
- Cardiothoracic surgery
- Cardiac disease; pulmonary diseases (COPD)
- Post-stroke
- Spinal cord injury
- CV performance
Muscle stimulators have also been used with cardiac and neurological conditions. There have been studies that have used this to help strengthen people with cardiopulmonary diseases, post-stroke spinal cord injury, and also cardiovascular performance for people who have had surgery. It is interesting to see how muscle stimulators or e-stim has been used in the early years for a more athletic population. Now, it is being used more for cardiac and neurological cases to help keep the muscles strong and people more functional and active.
- NMES devices:
- Portable units
- Small/large combo units
Figure 29 shows some of the different devices.

Figure 29. Examples of different devices.
Standard EMS devices have only two channels (on the left). We also have a large combo unit that plugs into the wall. This is a brand called the InTENSity Select Combo. This has like six or 10 different waveforms. These manufacturers are trying to get smaller, more portable, and use rechargeable batteries. The advantage for us is we can use one portable unit and have access to six or 10 different waveforms. I think that is great. Many of these combo units will have Russian and NMES settings that you can program for your desired effect for each patient. The table in Figure 30 goes over some of these parameters.
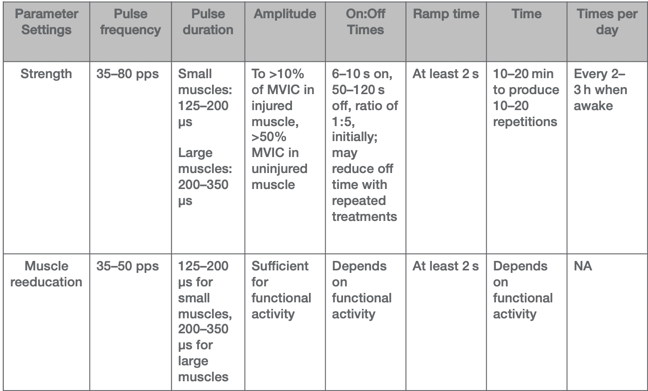
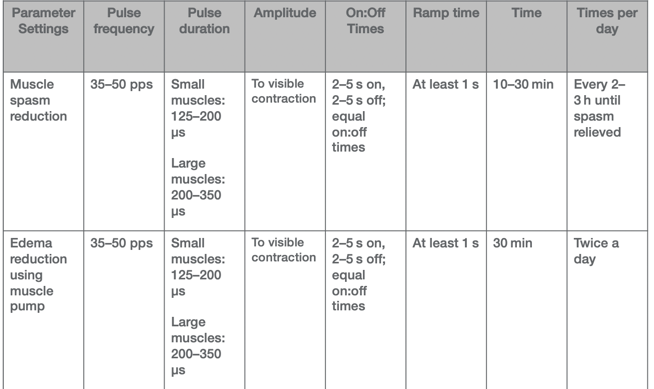
Figure 30. Treatment parameters for different diagnoses.
I have compi
