Introduction
This is our second presentation in a series on therapeutic modalities. Besides my teaching at the university and being a researcher, I am also a clinic owner. Specifically to this course, I am an adjunct faculty member in the master of occupational therapy program at Cal State Dominguez Hills. The focus of this talk is going to be how ultrasound can be used in a treatment strategy specifically for the occupational therapist. I want everyone to consider, as we go over the modality of ultrasound, how this would fit into your general treatment strategy for patients with different conditions and how can you use it as one of the tools in your toolbox.
Agenda
- Module 1: Basic Science
- Module 2: Indications and Contraindications
- Module 3: Treatment Parameters
- Module 4: Treatment Application
- Module 5: Ultrasound Research
- Module 6: Device Hygiene
- Module 7: Documentation
The science, application, and research of ultrasound are very comprehensive. I did my best to try to find a balance between all three in this presentation. There are textbooks and research articles that go more in-depth into the topic. Consider this a nice, robust overview of this topic.
Module 1: Basic Science
History of Therapeutic Ultrasound
Before we get into the science, it is always great to look at the history of therapeutic ultrasound in Figure 1(Miller et al., 2012).
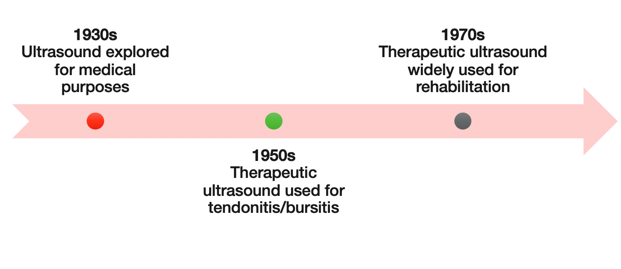
Figure 1. The history of ultrasound.
We can see that ultrasound was explored back in the 1930s for medical purposes. About 20 years later, they started to separate the different ultrasound waves and use it for imaging and some therapeutic purposes. In the 1950s, we started seeing the advent of therapeutic ultrasound being primarily used for tendinopathy or tendonitis and also bursitis conditions. Fast forward to the 1970s, we can see that the application of the technology was used worldwide. In the 1970s, it was used on a regular basis. There is a huge body of research that discusses the evolution and progression of therapeutic ultrasound technology.
Phases of Tissue Healing
- Things for the Occupational Therapist to consider!
- When is the optimal time to use US during a patient’s rehabilitation program?
- How will US enhance the tissue healing process and the patient’s overall recovery?
- The optimal sequencing of interventions (including US) in the patient’s rehabilitation program.
Another thing to consider is the phases of tissue healing with the use of US (See Figure 2).
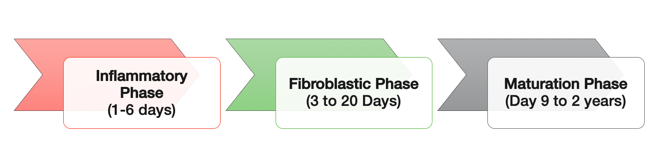
Figure 2. Phases of tissue healing.
Some of you may have taken the first presentation. In this, I stressed that if someone has surgery or an injury, the body interprets it the same way and goes through a process of healing. If you look in the literature, there are typically three phases. The inflammatory phase, fibroblastic phase, and then the maturation phase. this could be anywhere from one day all the way up to two years. Within each phase, I think it is important for the occupational therapist to consider three main points. The first point is when is the optimal phase to use ultrasound during a patient's rehabilitation program? I think that is important to determine. Consideration number two is how will ultrasound enhance the tissue healing process and the patient's overall recovery. Finally, what is the optimal sequencing of interventions with each client including ultrasound or modalities? These three points are important to consider.
Currently, there is a trend where modalities are not the primary treatment unless it is needed for a specific purpose. It is one piece of a comprehensive intervention strategy. It is important to facilitate and use your modalities correctly. You have to introduce the modalities at the right time within each phase to help facilitate healing. From an occupational therapist perspective and looking at the biopsychosocial model, you want to examine how ultrasound might create a quicker healing process.
It is important to remember these three considerations as we go through the lecture today because they are going to help drive your decision making. Your clinical decision making should include when and where to apply the modality to stimulate some physiological process. When I used to work in a clinic as an aide, everyone got ultrasound, a hot pack, and e-stim. As you know, there are some ethical concerns with that. Additionally, insurance caught on and are not paying very much now for modalities. Now, we use modalities to facilitate some type of outcome.
What is Therapeutic Ultrasound?
What is therapeutic ultrasound (Cameron & Sutkus, 2017)? Figure 3 shows an image of a basic ultrasound machine.
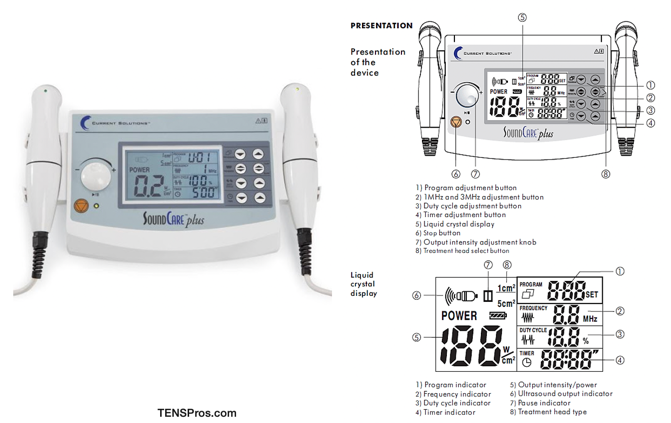
Figure 3. Basic ultrasound machine.
When we look at the image on the left, we can see that we have a normal digital display. Figure 4 shows the different types of sound heads on ultrasound.

Figure 4. Different sizes of ultrasound soundheads.
The therapeutic ultrasound soundhead is where the electrical current is converted to mechanical ultrasound energy. It comes out of the face or the flat part of the soundhead, and this is probably one of the most important pieces of the ultrasound equipment.
- Therapeutic ultrasound (US): High-frequency sound wave used to induce a biological response (> 20,000 Hz).
- Piezoelectric sound crystal:
- The transducer (applicator) has a crystal inside that creates the wave.
- AC electrical current to crystal = crystal expands and retracts (vibration)
- Changes in crystal = compression and rarefaction of wave
- Conversion of electrical to mechanical energy = US wave
Therapeutic ultrasound is a high-frequency sound wave used to induce a biological response. Inside the soundhead, or some people call it the transducer or the applicator, is a crystal (see Figure 5).
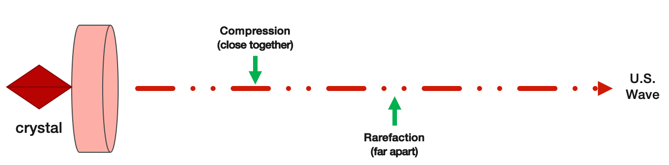
Figure 5. Crystal inside the soundhead.
There is a crystal in the metal part. The alternating electrical current is driven into the soundhead. As the AC current strikes that crystal, it causes the crystal to expand and retract which creates vibration. The change in the crystal results in the transmission of an ultrasound wave. The ultrasound wave that comes out replicates the compression and the refraction (or coming apart) of the crystal sound wave. This ultrasound wave has parts that are compressed and other areas that are apart or refracted. As the crystal is expanding and retracting, it produces this type of dynamic, consistent wave. The take-home for this slide is that because the crystal is moving and is driven by electricity, there is a conversion from electrical current to mechanical energy and that results in a compressed and refracted sound wave that is driven out of the soundhead.
Ultrasound Physics
- Attenuation: reduced energy as it passes through different body tissues
When the soundhead or the ultrasound wave is applied to human tissue. It goes through a process called attenuation. The term attenuation is a reduction in energy as it passes through the different body tissues. Attenuation can be seen in Figure 6.
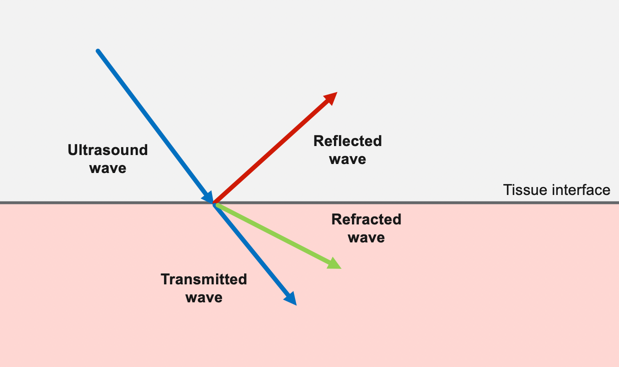
Figure 6. Attenuation of an ultrasound wave.
This shows the tissue interface. As the ultrasound wave strikes the skin, part of the wave reflects off of the skin, part of the wave refracts, and then the rest is going to be absorbed or transmitted into the deeper tissue. The ultrasound wave is going to be bouncing off the skin, but it is also going to be absorbed by the tissues. This whole process is called attenuation where the ultrasound wave is going to be reduced because some of the wave strength is going to be lost. This is why we always move the soundhead and why there are different settings to try to get into deeper tissues or more superficial tissues.
Ultrasound and the Body
- Tissue absorption- more energy is absorbed in the superficial tissues.
- High collagen tissues absorb the most energy
- Bone and cartilage may reflect the energy
There are different tissues of the body that absorb the ultrasound energy more than others. High collagen tissues absorb the most energy. Examples of high collagen tissues are ligaments, tendons, fascia, joint capsules, and scar tissue.
If you look at the body of ultrasound research, we see that ligaments and tendons do pretty well with ultrasound. More dense tissues like bone and cartilage tend to reflect the energy off of them. Ultrasound seems to do really well for these collagenous structures versus trying to go over bone or even cartilage. Another thing to consider is that muscle tissue is so dense. A lot of energy is lost in the muscle. Thus, heating up a muscle is not always effective.
Types of Ultrasound Waves
- Continuous (Thermal)
- Increased tissue temperature
- Affected by intensity, frequency, and tissue type
- Pulsed (Non-Thermal)
- Cavitation: Vibration of gas bubbles
- Stable = change in cell function, Unstable = tissue damage
- Acoustic streaming: Movement of fluids along the boundaries of cell membranes
- Increased fibroblastic activity, intracellular calcium
- Alterations in cell membranes activity and wall permeability
- Increased protein synthesis
- Cavitation: Vibration of gas bubbles
There are two types of ultrasound waves as seen in Figure 7.
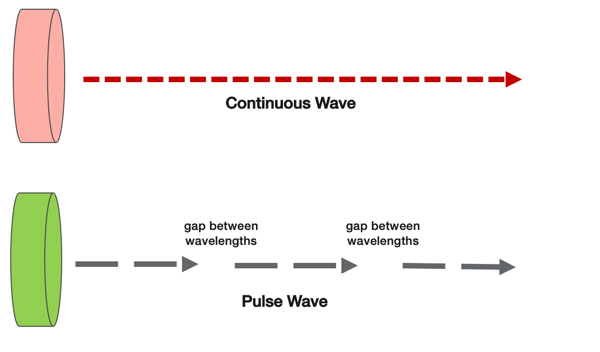
Figure 7. Here are examples of ultrasound waves.
Again, the ultrasound wave is created by a vibrating crystal. It transmits or shoots out an ultrasound wave from the soundhead. There are two types of waves. You can have a continuous wave where it's 100% moving all the time, and then if you look below on the diagram, you can have what is called a pulse wave or a pulsed wave. A pulsed-wave gives you a latent period or a rest period in between ultrasound waves. Depending on what your setting is for your ultrasound, you can use a continuous wave or you can use a pulsed wave to stimulate different physiological processes in the body.
Continuous (Thermal). Continuous is considered a thermal effect because the ultrasound wave is striking the tissues and is being absorbed at 100% consistency. There are many studies that have looked at continuous ultrasound and have shown that it heats the tissues locally a couple of degrees creating a thermal effect. If you have a goal of heating a patient's tissues, it is going to be affected by the intensity, or how strong you set the intensity, the frequency of the wave, and also the tissue type. A ligament might heat up quicker than a big, dense muscle.
Pulsed (Non-Thermal). Pulsed is non-thermal as there is a latent period or a rest period in between each sound wave that allows the tissues to cool down a little bit. This depends on the setting, and we will talk about that a little bit later. Pulsed non-thermal is mainly used to create a mechanical effect on the body. We are not trying to heat up the tissues as much with pulsed. There is always going to be a little bit of a temperature change because you are creating this effect, but we are not going to be doing this continuously. Our goal is to create some type of mechanical movement in the tissues and cellular structures.
Scientists have found two physiological responses from pulsed ultrasound. One is called cavitation, where you get vibration from the crystal moving and causing compression and refraction. As it strikes the tissue, it causes mechanical vibration. As the tissues are absorbing this pulsed energy, they are creating a vibration of gas bubbles inside the tissues. The goal is to create what is called a stable vibration by moving the soundhead, being safe, and not creating any instability where the settings are too high or the machine is faulty. We want stable cavitation where there are vibration and movement. Along with this cavitation, the pulsed ultrasound also creates what is called acoustic streaming. As the ultrasound wave is being absorbed by the tissues, it is stimulating the movement of fluids along the boundaries of the cell membrane. Scientists have found that this increases fibroblastic activity, intracellular calcium, and alterations in cell membrane activity and wall permeability. It also increases protein synthesis. There are two treatment strategies for therapeutic ultrasound. One is continuous thermal and the other one is mechanical non-thermal. The question is when and where would you use those settings in your patient's treatment strategy.
Mode of Heat Transfer
- Conversion (non-thermal energy to heat)
- Reflection
- Refraction
- Transmission
The mode of heat transfer is called conversion. We discussed this more at length in our first presentation. It is a conversion of electricity to mechanical energy. Non-thermal is typically a pulsed wave, and it is used for mechanical energy. Thermal is a continuous wave, and it is used to heat up the tissue.
Physiological Occurrences
As we look at some of the physiological occurrences, what happens with continuous thermal (Figure 8)?
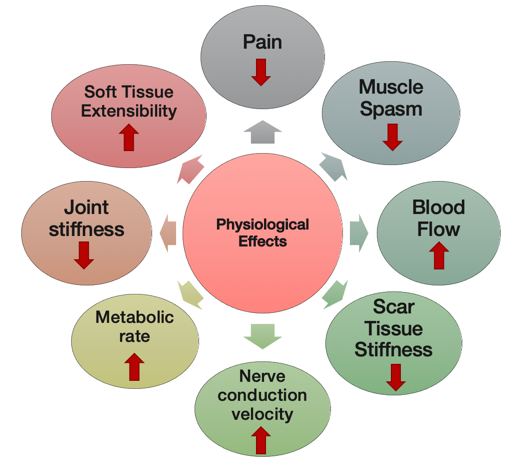
Figure 8. Ultrasound: Continuous/Thermal.
If we go clockwise along with the diagram here, we can see that research has suggested that ultrasound decreases pain and muscle spasm and increases blood flow locally. It can decrease scar stiffness, increase nerve conduction velocity locally, increase local metabolic rate, decrease joint stiffness, and increases soft tissue extensibility. Ultrasound is going to penetrate deeper than a superficial hot pack, but it is going to have similar effects. It is going to heat up the tissue and make things more pliable. Remember, even if you are using a continuous 100% cycle of ultrasound, you are still going to have a thermal and a mechanical effect. It does not go away. Both of them are going to have mechanical. Consider that many of these physiological responses are a combination of thermal and mechanical. Here are pulsed/non-thermal effects in Figure 9.
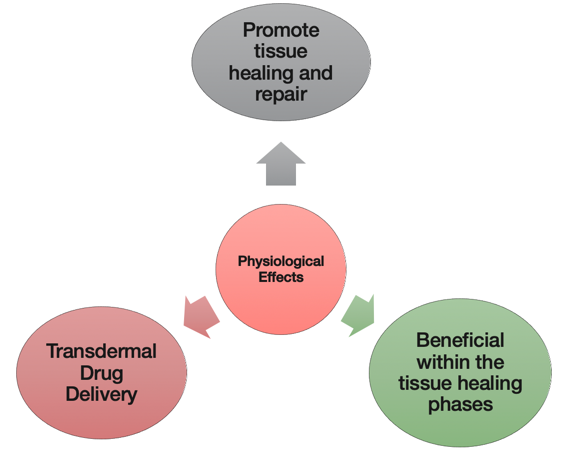
Figure 9. Ultrasound: Pulsed/Non-Thermal.
Pulsed/ non-thermal is used used to promote tissue healing and repair. It is beneficial within all the tissue healing phases. It can also be used to drive transdermal drug delivery or photophoresis. I am sure everyone here has heard of that before. This is where you take a nonsteroidal antiinflammatory or a corticosteroid, like a dexamethasone, and you put it in ultrasound gel to deliver it to the tissues. This is how pulsed ultrasound is to promote tissue healing and to drive medication versus creating a thermal effect.
Conducting Media
- Air is a poor conductor of ultrasound energy
- Conduction medium needed to maximize delivery to tissues
- Ultrasound gel
- Gel pads
- Mineral oil/cream
- Lotions
- Water immersion (avoid metal containers)
- Conduction medium needed to maximize delivery to tissues
Some type of conduction media or medium is needed to maximize delivery. Typically, we use ultrasound gel, a gel pad, mineral oil, different lotions, or you can do water immersion. Any of these mediums will help transfer the ultrasound wave into the tissues. When the ultrasound wave is conducted through ambient air, it gets struck with other particles, thus air is a poor conductor. The rule of thumb is to use some type of gel, oil, or lotion to be able to transfer it successfully into that tissue interface. Another conductor that is popular is water immersion. For example, you can stick someone's ankle in a plastic tub, and then you place the ultrasound soundhead in there. However, do not use a metal tub as the water turns into a complete conductor. Ultrasound gel is probably used the most.
Bottom Line
- Occupational Therapist considerations:
- Ultrasound transfers energy by conversion.
- Ultrasound creates thermal and non-thermal effects.
- High collagen tissues absorb US energy more than bone or cartilage.
- A medium is used to assist in the transfer of ultrasound energy into the body tissues.
Ultrasound transfers energy from the ultrasound head into the tissue interface by conversion. Ultrasound creates a thermal effect and a non-thermal effect. High collagen tissues absorb ultrasound energy the most, and a medium is needed to transfer it successfully into the tissues.
Module II: Indications and Contraindications
What are the indications and contraindications for ultrasound?
Clinical Indications
You can see there are several clinical indications.
- Pain modulation
- Treatment of soft tissue shortening
- Dermal ulcers
- Surgical skin incisions
- Tendon & ligament injuries
- Fractures
- Carpal Tunnel Syndrome
- Phonophoresis
Precautions and Contraindications
- Precautions
- Acute inflammation
- Epiphyseal plates
- Fractures
- Breast implants
- Poor mentation
- Contraindications
- Pregnancy
- Malignancy
- Nerves, veins, and eyes
- Joint cement and plastic
- Thrombophlebitis
- Pacemaker
- Reproductive organs
- Impaired sensation/circulation
Most of these follow along with a lot of the other modalities. You need to have caution with acute inflammation. Epiphyseal plates are also very controversial. There is a lot of older studies that say that if you use ultrasound over a plate, you might stimulate early growth and sealing of that plate. The standard of care is you stay away from that in a growing kid. Fractures are also a precaution, but there are some super low-level ultrasounds that are used to heal a fracture. We will cover that in a second. We also have breast implants and poor mentation as precautions. If the client lacks the cognitive ability or they cannot feel what is going on, then we would not use ultrasound to be safe.
For contraindications, you would not want to use on pregnant women. Ultrasound sonography is totally different. We need to be careful with doing therapeutic ultrasound over any type of malignancy, nerves, veins, and eyes. Joint cement and plastic are other controversial areas. Some doctors think it is ok to do ultrasound around a knee replacement, while others do not. I have used it before more in the popliteal fossa or the distal hamstrings, but I have never done ultrasound directly over a knee replacement approaching it from the anterior or lateral part where it is more superficial. Instead, I will use a hot pack in these situations if I want to soften tissue before manual therapy. Obviously, you would not want to use it with thrombophlebitis or any type of DVT. Additionally, it is contraindicated over a pacemaker, reproductive organs, or areas of impaired sensation or circulation. As a professional, you would screen first and make sure that any type of modality is safe for your individual client.
Adverse Events
- Precaution: Tissue/bone burn
- Keep soundhead moving
- Monitor throughout treatment
- Burns, standing waves, cross-contamination, cross-infection
The biggest adverse event is a burn. You have to keep the soundhead moving. Before you turn on the machine, move the soundhead. I do a little bit of legal expert work, and I have had several cases in the last 10 years where I was deposed as an expert where the person did not move the soundhead and burned the patient. We have to be cautious and vigilant, especially with ultrasound, because it is a very powerful modality. There are also standing waves that can affect the tissues if you leave it in one spot. We also have to think about these days about cross-contamination and cross-infection. Make sure you clean the soundhead and the skin. We will talk about this in the later modules.
Module III: Treatment Parameters
Thermotherapy
- Superficial Heat (Superficial < 2 cm depth)
- Moist heat (conduction)
- Contrast bath (convection)
- Hydrotherapy (convection)
- Fluidotherapy (convection)
- Paraffin bath (conduction)
- Deep Heat (Deep > 2 cm depth)
- SW Diathermy (conversion)
- Ultrasound (conversion)
Once we determine our treatment and if we want to go thermal or non-thermal, we are going to use different settings. Ultrasound is a deeper heat. In the first presentation of this series, we discussed superficial heat. Those only penetrate the skin and into the muscle maybe two centimeters or less. The deeper heat of ultrasound can go greater than two centimeters. Some research says it can go all the way down to five centimeters so ultrasound is considered a deep heat modality. If you are working around a bony area, you definitely have to keep that soundhead moving and have the controls set for more superficial tissues. We will talk about that next.
Ultrasound Parameters
I put a lot of information on ultrasound parameters on one concise slide in Figure 10.
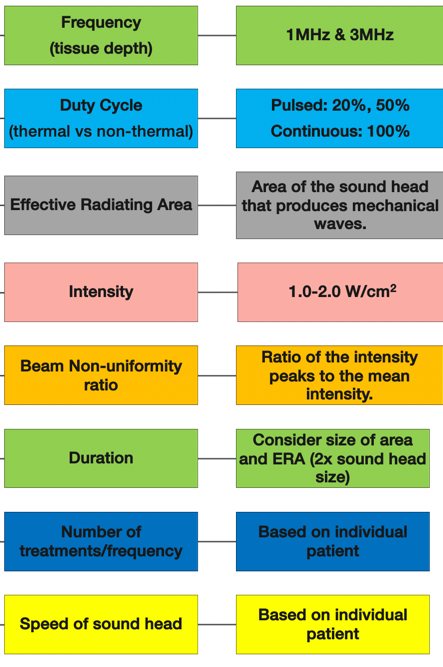
Figure 10. Ultrasound treatment parameters (Cameron & Sutkis, 2017).
If we start at the top, we are going to discuss the frequency. That is the speed of the ultrasound wave being transmitted out of the ultrasound head or the applicator. The duty cycle is the ultrasound wave whether it is continuous at 100%, 50%, or 20%. Are there rest periods in between the sound waves? The effective radiating area is the circular size of the sound wave coming out. Intensity is how high you turn up the machine. This determines the strength of the ultrasound wave. And then, there is the beam non-uniformity ratio. This looks at the sound wave that is coming out. It is not perfectly circular. The sound wave is asymmetrical with different shapes. When we move the soundhead, we are trying to make sure that the tissues are absorbing the sound wave, but we are not keeping it in one spot to cook our patient. That is important. The duration is how long each session should be. The number of treatments and frequency, and also the speed of the soundhead movement are also important parameters. We are now going to get into some of these right now to help you make good decisions when using ultrasound with your patients.
Frequency/Depth. Frequency is the speed of the ultrasound wave coming out of the soundhead. Figure 11 is a demonstration of this.
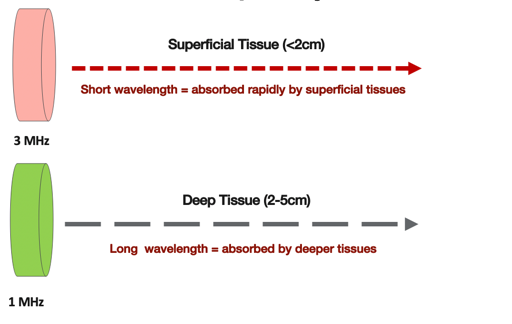
Figure 11. Speed of the ultrasound waves.
There are two common frequencies; three megahertz and one megahertz. Three megahertz is for superficial tissue. The sound wave is being transmitted rapidly out of the soundhead, and it is striking the tissue interface very fast with a short wavelength. As it is reflecting and refracting off the tissues in a rapid three megahertz frequency, the superficial tissues are absorbing it more than the deeper tissues. In general, the depth would be less than or equal to two centimeters or less.
If the goal of our treatment is to go deeper, then we would use a one megahertz setting. The sound wave is coming out of the ultrasound head at a slower frequency. That slower frequency allows more of the ultrasound wave to be absorbed by the deeper tissues. Studies over the years have shown that the deeper tissues, from two to five centimeters, tend to be affected more mechanically but also heat up. If you want to go thermal and heat up the tissue, then you should use one megahertz.
As an example, if you working around the elbow, you would use a three megahertz setting because that is superficial. If you are trying to get to something deeper like the patellar tendon, a lesion on the quadriceps, or some scar tissue on the quadriceps, these are a lot deeper. You may want to use a one megahertz setting because that is going to penetrate deeper. Another example is treating the thoracolumbar fascia, which is very thick and dense, in the lower back. One megahertz would be appropriate for a deeper setting plus a deeper effect. Try to keep these thermal and non-thermal and superficial and deep parameters in mind depending upon your goals and the physiological responses you are trying to stimulate. Figure 12 is another schematic showing the different depths.
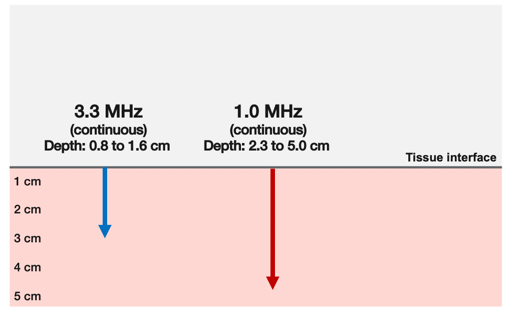
Figure 12. Depth of the ultrasound waves.
Some studies say that ultrasound can even go a little deeper so that is why I put the arrow a little lower.
Duty cycle. When we look at the settings on the machine, we call it the duty cycle.
- Duty cycle = duration of the pulse (time on)
pulse period (time on + time off)
The duration pulse is the time on versus the pulse period, which is the time on plus the time off. If you do a continuous duty cycle, your goal is to heat up the tissue. If you do a pulsed setting, you turn the machine on at 50%, then you are going to get like that one to one ratio. If you set it for 33%, 25%, or even 20%, this is where you are going to have different rest periods in between the sound waves. Figure 13 shows a good overview of the duty cycle.
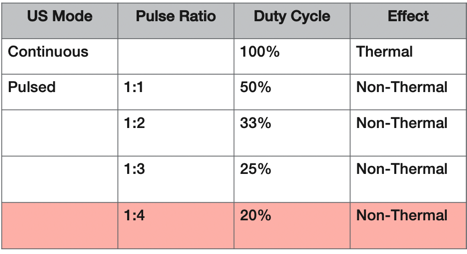
Figure 13. Overview of the duty cycle.
In this chart, 100% continuous means that the ultrasound wave comes out of the soundhead continuously. If you do a pulsed one to one, there is going to be 50% of the sound wave on and 50% off. For 33% pulsed, the ratio will have a one to two with one wave on, two waves off with a rest period in between. As we go from 50% down to 20%, we create a longer rest period in between those ultrasound pulse waves. The greater the gap, the less the tissue is going to heat up. The 20% pulsed parameter tends to be the gold standard for a non-thermal, pulsed ultrasound. If you want to use ultrasound in a more superficial area or drive medication, all the research is pointing to 20% because that has been shown over 20 or 30 years of research to produce the least amount of heat.
Many textbooks consider pulsed 50% as a non-thermal, but there has been some more recent research that has shown that 50% pulsed is strong enough, even though it is pulsed, to create thermal effects. This is not as much as continuous, but there are some temperature changes with 50% pulsed. Depending on the ultrasound unit you have, there are typically three or four settings where you can go continuous 50%, 25%, and 20% or some just go to 20%. It depends on what ultrasound unit you have, which gives you the settings. Figure 14 shows another schema of the duty cycle options.
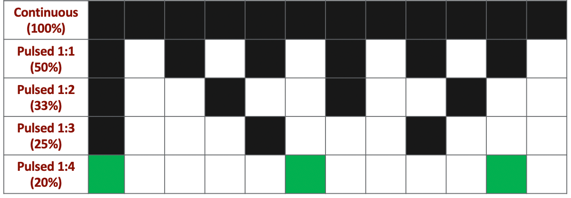
Figure 14. Duty cycle options.
This is going to come into play when you purchase more expensive ultrasound units. You want to look at the duty cycle and what settings you can use to go thermal or non-thermal, and continuous or pulsed. Keep in mind that while 50% might give you a little bit of warmth, 20% gives you the least amount of temperature increase because there is a rest period. The tissues get to cool down in between those ultrasound waves. Figure 15 shows what some researchers have put out as a prescription for pulsed ratios.
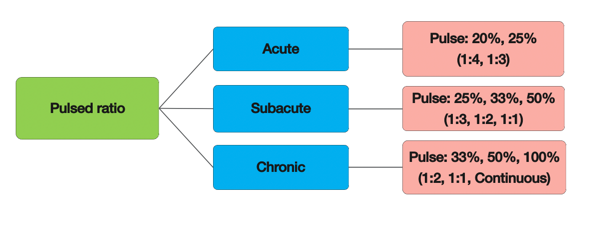
Figure 15. Prescriptions for pulsed ratios.
For an acute injury, you can use the lower level pulses at 20% and 25% because those will stimulate the mechanical effect but those will not heat up the tissues. As we talked about in the first presentation, sometimes people believe that heat can negatively or positively affect the healing process. If you have an acute injury, the standard right now for ultrasound is to use a lower level pole setting. Then as you progress to the subacute stage, you can go up to 50%. With a chronic injury, your duty cycle can be anywhere between 33% to 100%. This is one evidence-based algorithm that a lot of professionals use.
Effective radiating area. One of the most important aspects is the effective radiating area (ERA). It is the cross-sectional size of the ultrasound wave coming across the soundhead (Figure 16).
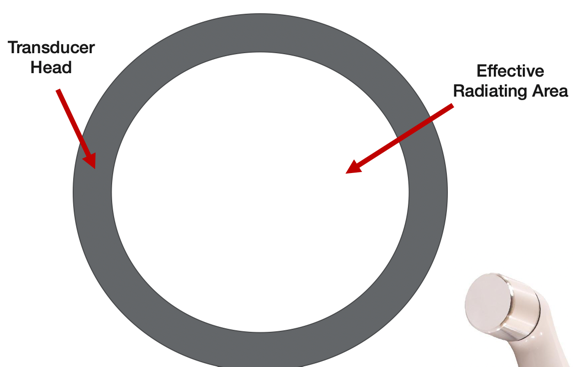
Figure 16. Effective radiating area.
The effective radiating area is how big the ultrasound wave is. This is going to determine the size of the treatment area. You always treat an area that is two times the size of the transducer soundhead.
- Treatment area in relationship to the US head size
- 2x size of the transducer head (faceplate)
- Common transducer sizes
- 1 cm²
- 2 cm²
- 5 cm²
- 10 cm²
e.g. Treatment Area = 10cm2 x 2 = 20cm2
For example, common sound heads are one, two, five, and 10 centimeters. I have even seen bigger ones. If you are following what is recommended in the research, typically, you are going to be treating a small area with your ultrasound. If you do a larger area, you are going to lose a lot of mechanical and thermal effects. And, the temperature increases from thermal only last anywhere between three to six minutes. Thus, the rule of thumb is to only go two times the size of your soundhead. If you are working on the elbow as an example, you are going to use a smaller soundhead. If you are working on something bigger like the thoracolumbar fascia, you might choose a little larger soundhead.
Intensity. Intensity is like the volume or strength of the wave.
- Intensity: Determines strength of the US beam
- Watts/square centimeter
- W/cm2
It is measured in watts per centimeter squared so please consider that when you chart. Here are some parameters for intensity in Figure 17.
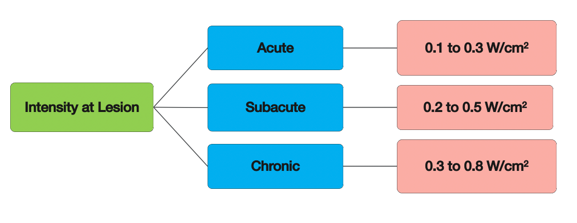
Figure 17. Parameters for intensity.
When you chart about an ultrasound treatment, you have to put in the intensity. For example, some research recommends a lower ultrasound level of 0.1 to 0.3 watts per centimeter squared intensity. Subacute can go up to 0.2 to 0.5, while chronic settings can go 0.3 to 0.8. However, the research is can be all over the map. In the next module, I will be able to give you some specific guidelines on general numbers, but this is one evidence-based algorithm used for intensity. Remember, the intensity is how strong the ultrasound beam or the wave is.
Beam Non-uniformity Ratio (BNR). There are going to be some asymmetries to the ultrasound wave. Scientists and the FDA created what is called the BNR, or the beam non-uniformity ratio.
BNR = special peak intensity
special average intensity
- BNR- The maximum point intensity on the transducer to the average intensity across the transducer surface
- Most common
- 2:1 and 6:1
- Low BNR ratio: more even energy distribution = less risk of tissue injury.
- Most common
The vibrating crystal inside the soundhead is sending out a continuous ultrasound wave. The energy particles are then compressed and refracted. When the ultrasound beam comes out, it is not going to be perfectly shaped like a laser. The above equation is the spatial peak intensity divided by the average intensity which gives us the BNR.
- Spatial average intensity:
Total Power (watts)
Area (cm2)
- Spatial peak intensity
- The greatest level of intensity anywhere within the beam.
The spatial average intensity is the total watts divided by the area. There is an asymmetrical sound wave that is compressing and refracting with the peak intensity in the center. See Figure 18 for an example of this.
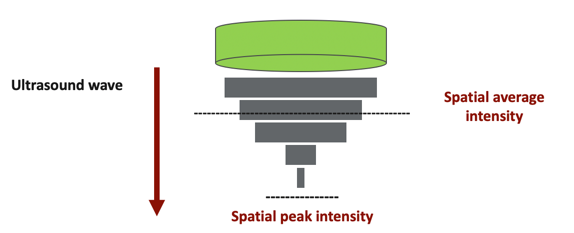
Figure 18. Example of the spatial peak intensity.
When it strikes the tissue interface, it is going to create a maximum point of intensity. The government and manufacturers decided that there needed to be a lower BNR ratio to avoid burning the tissues. The BNR is typically already taken care of when you buy an FDA approved unit in the United States.
- Soundhead motion avoids burns
- Longitudinal or circular patterns
- Speed: 4 cm/sec
- Total area: 2x size of ERA
However, it is also important to understand physics. If you leave the soundhead in one spot, an asymmetrical wave, that is compressing and refracting and striking the tissue interface, is going to create some hot spots. As it is striking the tissues, if the ultrasound unit does not have a low BNR, it can damage the tissue. This is what happened in some of the earlier models in the 1930s, 40s, and 50s. The ratio fixed inside the machine to create a more even ultrasound wave was not in place. Most commercial ultrasound units out there already have an approved lower ratio. You can be fairly confident that the ultrasound beam is more even. However, we can also control this by moving the soundhead.
Sound Head Motion (Speed).
- Soundhead motion avoids burns
- Longitudinal or circular patterns
- Speed: 4 cm/sec
- Total area: 2x size of ERA
The rule is to use a longitudinal or circular pattern. Your speed is going to be four centimeters per second, and your total area is going to be two times the size of your soundhead. There is some variability depending on what textbook or article you read. I move it quickly over superficial areas. You also want to monitor the patient and their feedback. If they feel the warmth, you either need to turn down the intensity, change the settings, or move the soundhead faster.
US Treatment Parameters
- Frequency: Superficial or Deep Tissue?
- Duty Cycle: Thermal or Non-Thermal?
- ERA: Size of treatment area?
- Intensity: 0.5 to 2.0 W/cm2 ? Patient feedback is important
- BNR: What tissues are you trying to affect? Be careful over superficial areas (e.g. ankle/foot)
- Soundhead Movement: 4 cm/sec (2x size of ERA)
- Tx Duration: Size of treatment area?
- Tx Frequency: Phase of tissue healing? Treatment Goal?
We need to look at all of these parameters. Again, you have to keep the soundhead moving because you know that that sound wave is pretty strong, and you want to move it four centimeters per second. The treatment duration is obviously going to depend on the treatment area, and the treatment frequency depends on the healing stage and the treatment goal. As everyone is different, it is really hard to have a standardized norm. I do want to give you a couple of tips that I use personally when I teach this. Most people use 100% for thermal, 20% for non-thermal. If someone is doing a larger area, they usually do five to six minutes per area. They may also do two treatments. I primarily use 1.0 watts per centimeter squared for both three and one megahertz. Sometimes if I am over a bony area, I will go down to 0.8. These parameters seem to produce the physiological effects that I want. Again, this is more clinical-based evidence from me and others that I consult with. I do move the soundhead more rapidly as I said over bony or superficial areas. If I am treating a big area, I might do five to eight minutes per area. This is also with your billable codes. The frequency depends on what I am trying to do. If I am doing phonophoresis, I might do it one or two times or if I am trying to heat up some tissue over time, or I might do it three to four times. Rarely do I do this treatment over several months or more than six times.
Bottom Line
- Occupational Therapist considerations:
- Treatment parameters need to match the intervention goal and should benefit the patient treatment.
- The OT must have a working knowledge of US parameters in order to provide safe patient treatment.
- The OT must consider the safety of using US with each patient.
The bottom line is that we need to match the treatment parameters with the intervention goals. Everybody needs to have a working knowledge of these parameters and what to set. We have to consider the safety of each patient. You also need to ask yourself the following questions. Why are you going to do it? What are you going to get out of the modality? You are looking at probably 15 minutes of a one-hour treatment on average. You have to ask yourself how this fits into the overall treatment strategy.
Module IV: Treatment Application
We have now gone over science, indications, contraindications, and the settings on the ultrasound machine. We also went over the goals of that. Now, how do we apply it?
Clinical Indications
These are the clinical indications that we talked about before.
- Pain Modulation
- Treatment of soft tissue shortening
- Dermal ulcers
- Surgical skin incisions
- Tendon and ligament injuries
- Fractures
- Carpal tunnel syndrome
- Phonophoresis
These are all of the conditions that the research has shown a positive efficacy with ultrasound. We also have to consider how to set the ultrasound to effectively treat these conditions. I am going to go in-depth about a few of these areas.
Pain Control.
- Intensity: 0.5 to 3.0 W/cm2
- Duty Cycle: 100% continuous (preferred)
- Duration: 3 to 10 min
- Frequency: 3 MHz or 1 MHz
- Speed: 4 cm/sec
- Total area: 2x size of ERA
These are the parameters for pain control as noted in the research. You use intensity of 0.5 to 3.0 at 100% continuous for a duration of three to 10 minutes with the goal of either superficial or deep tissue treatment at a speed of four centimeters per second and two times the size. The complicated pain neural matrix that we discussed in the first lecture in this series looked at stimulating the local mechanoreceptors, proprioceptors, and the nociceptive free nerve endings. You are going to be heating up the tissue and stimulate these areas. It may also stimulate the neuroendocrine system to release some endorphins. This is similar to when you take a hot shower. And again, with continuous, there may have a combo effect by stimulating through thermal and mechanical means. If you are trying to control pain, I think most likely it would be best to do this in the subacute fibroblastic phase. I always use pulsed in the acute phases. Again, the research is still kind of weak on that, but I think it is important to use the guidelines available.
Soft-Tissue Healing.
- Intensity: 0.5 to 1.0 W/cm2
- Duty Cycle: 20% pulsed (preferred)
- Duration: 3 to 10 min
- Frequency: 3 MHz (preferred)
- Speed: 4 cm/sec
- Total area: 2x size of ERA
Now for soft tissue healing, we get away from that thermal effect. We are using a lower intensity, but our duty cycle is 20% pulsed with a longer rest period in between waves. We are using vibration and mechanical input versus thermal. The research says three to 10 minutes with three megahertz the preferred setting. You are still at 4 centimeters/sec ERA and two times the size for the treatment area. The speed and total area are still the same, but what interesting is that according to the research, three megahertz was preferred. I am surmising that this has more to do with the superficial tissues. However, this might be different in the lumbar spine with the different layers of muscles and thoracolumbar fascia as noted earlier. You are going to have to take all this into consideration depending on the area you are treating. No one says that you have to use just one setting. For your own clinical evidence, try both and see how it works for your patient. Keep this all within the standard of care and make sure it is safe.
Soft-Tissue Shortening.
- Intensity:
- 3 MHz: 0.5 to 1.0 W/cm2
- 1 MHz: 1.5 to 2.5 W/cm2
- Duty Cycle: 100% continuous (preferred)
- Duration: 5 to 10 min
- Frequency: 3 MHz or 1 MHz
- Speed: 4 cm/sec
- Total area: 2x size of ERA
If you have soft tissue shortening or contractures, the research supports using both settings. For superficial, you are still going to use a lower intensity of 0.5 to 1.0 at 3 MHz. For deeper, you want to use 1 megahertz for deeper so that it will not heat up the superficial tissues as much. You can also turn up the intensity more, and they recommend 1.5 to 2.5 W/cm2. The duty cycle is going to be continuous as you are trying to heat up the tissue. They recommend a longer treatment time of five to 10 minutes per total area. If you are using a five-centimeter or 10-centimeter soundhead, you are going to be working in a small area. And again, we can use both frequencies. The speed of the soundhead is going to be consistent. These give you some guidelines to start with, and then obviously, you can adjust it accordingly. Some of the researchers actually promote getting the patient's feedback as you are turning up the intensity. I think this is interesting because as you are turning up the intensity, if they feel the warmth, typically you stop there. However, some of the experts like Michelle Cameron, a medical doctor who does a lot of studies, suggest that for some things that you go buy a subjective report. There can be a risk as the patient may not always pay attention. I always recommend starting by trying to warm up the tissue with the norms of 1.0 and see how it affects your treatments.
Ligament and Tendons.
- Intensity: 0.5 to 1.0 W/cm2
- Duty Cycle: 20% to 50% pulsed (recommended)
- Duration: 3 to 10 min
- Frequency: 3 MHz or 1MHz
- Speed: 4 cm/sec
- Total area: 2x size of ERA
When we look at ligaments and tendons, we know that they are superficial. However, like the glenohumeral joint, there are some deeper ligaments and structures. The research recommends a collective intensity of 0.5 to 1.0. Your duty cycle is going to be 20% to 50%. The duration is going to go three to 10 minutes, and the frequencies can be superficial or deep depending on your goals. The speed and the total area of treatment are going to follow the same rules.
Bone Fractures.
- Intensity: 0.15 W/cm2
- Duty Cycle: 20% pulsed
- Duration: 15 to 20 min
- Frequency: 1.5 MHz
- Speed: NA
- Total area: NA
- *Device: Specific device with application pads used over FX
Another interesting area is bone fractures. In Southern California, I deal with a lot of runners from school teams and professionals, and I see many stress fractures. More so recently, probably the last 20 years, they have debunked the precautions around fractures. The researchers have found that you can use a super low-intensity ultrasound. We are talking 0.15 at a 20% duty cycle. This causes a low-level mechanical vibration into the tissues. The frequency, however, is going to be faster than the 1.0. Using ultrasound at a moderate level frequency with low-level vibration has shown good efficacy for helping bone fractures to heal quicker. Most of the time if you are talking in simple clinical lingo, they call it a "bone stimulator." I have seen very good outcomes with different patients especially for shin splints and lower foot injuries. I have seen a few athletes who have stress fractures because they are growing and running 40 to 50 miles a week. In these cases, I do not feel that the stimulators work as effectively with the deeper tissues. In my opinion, for superficial fractures, from the knee down (tibial tuberosity, shin), there seems to be some good clinical evidence. These examples can apply to hand and wrist.
Carpal Tunnel Syndrome.
- Intensity: .1.0 W/cm2
- Duty Cycle: 20% pulsed
- Duration: 5 to 15 min
- Frequency: 1 MHz
- Speed: 4 cm/sec
- Total area: 2x size of ERA
One of the most widely studied musculoskeletal issues is nerve entrapment with carpal tunnel syndrome (CTS). There have been quite a few studies that have shown efficacy for ultrasound using a 1.0, 20% duty cycle, five to 15 minutes with a one megahertz setting. This is going deeper at the same speed in the area. I have heard of people using ultrasound for entrapments, like CTS, and at Guyon's canal. The take-home message is that the majority of research for carpal tunnel is saying that it works pretty well.
Set-up of the Ultrasound.
Here are the steps for the set-up of ultrasound as a review.
- Inspect and prep the treatment region
- Turn on the machine and set treatment parameters
- Apply media (gel or lotion)
- Place and move soundhead over the area
- Start device
- Administer treatment
- Recheck and clean area
Phonophoresis.
- Intensity: 0.5 to 1.0 W/cm2
- Duty Cycle: 20% pulsed (preferred)
- Duration: 5 to 10 min
- Frequency: 3 MHz (preferred) or 1 MHz
- Speed: 4 cm/sec
- Total area: 2x size of ERA
Phonophoresis is a great adjunct to help control inflammation and calm down tissues. These are the settings according to research. The only difference between this and the steps noted above is that you put the medication in the gel. We are trying to drive the medication into the tissues. If we go 20% for five or 10 minutes at a frequency of three megahertz, we can increase the permeability of the skin and the myofascial through the mechanical effects. Remember through mechanical acoustical streaming, we can increase the permeability. We open up the skin per se and drive the medication into it. Some studies have used one megahertz for deeper penetration, but in my opinion, three megahertz seems to be effective. Again, we keep the same speed and the total areas as our standards.
I believe that using phonophoresis and some type of NSAID or anti-inflammatory can be effective for many situations like chronic tendinopathy. I think phonophoresis has its value more so than ultrasound in some cases. This is what I am finding clinically in my practice. You put the medicine in the ultrasound gel and mix it in. Typically, a 1:4 ratio. You can use dexamethasone or a diclofenac anti-inflammatory cream as examples. Many times people will mix that with ultrasound gel to kind of create a medium, but you need to dilute the medication a little bit. Even though we are doing phono at a low-level, you still have to monitor for tissue interface irritation when you are driving in medication. You also have to go back to your basic screening of the patient's medications and make sure that you are not double-dosing them with an anti-inflammatory. I have had some clients on a prednisone pack because they are in a lot of pain. You do not want to use an additional steroid in this case. We need to be safe with our medication and chart it appropriately. There are some more legal risks to using medication. You want to be careful if they are on blood thinners, lack sensation, or if they are on other anti-inflammatories like a corticosteroid or an NSAID. Additionally, think about your clients with asthma or COPD. If they are taking an inhaler that has a steroid in it, this would also be double dosing them. Please consider all of these little nuances during your treatment as mistakes can be made.
Treatment Examples
Let's now get into some treatment examples. The next couple of slides are giving you an algorithmic approach to summarize some of the ideas in this section.
Soft Tissue Shortening.
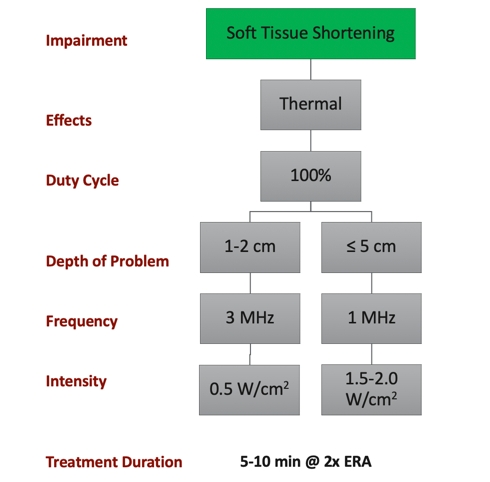
Figure 19. Example of treatment for soft tissue shortening.
If we are working on soft tissue shortening, the goal is to have a thermal effect, thus the duty cycle should be 100%. If the depth of the problem is superficial, we are going to go with three megahertz with a lower intensity. If it is a deeper lesion, we are going to go one megahertz with a higher setting. We know that we can go higher because it penetrates deeper. Our treatment duration on average is going to be five to 10 minutes. We want to use two times the ERA with a slow, nice even movement.
Delayed Tissue Healing/Prolonged Inflammation.
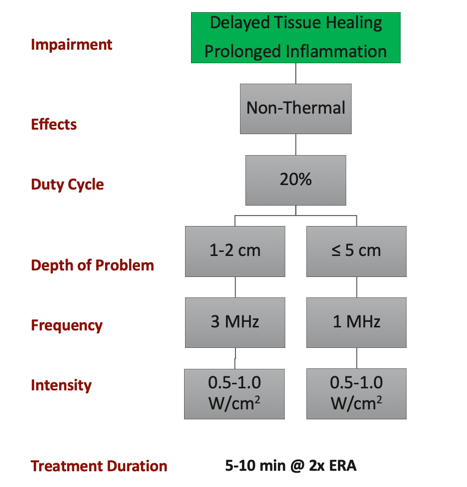
Figure 20. Example of treatment for delayed tissue healing and prolonged inflammation.
If we are trying to promote some type of tissue healing, we may want to try a non-thermal ultrasound. The recommendation in the research is to go as low as possible to 20%. Some units even go to 10%. If we go 20%, we know that there is a longer rest period. Theoretically, this is going to have a non-thermal effect. A superficial problem will follow the same rules, three megahertz 0.5 to 1.0. That should be up to five centimeters. We can go one megahertz, and we are still going to use a lower intensity. Treatment duration on average is going to again be five to 10 minutes. The other settings as far as speed and treatment area are going to stay consistent.
Integrative Treatments.
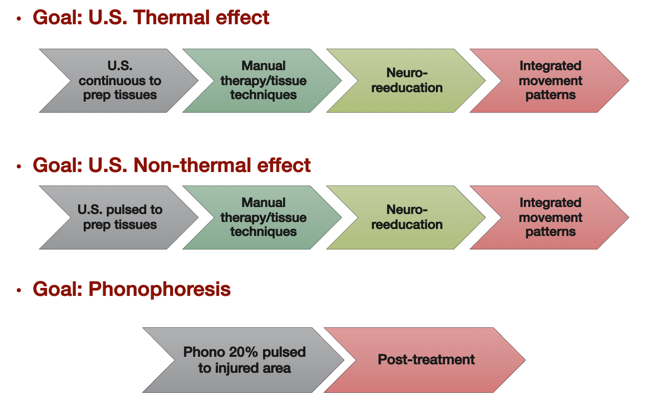
Figure 21. US integrative treatments.
Here are some integrative strategies. For example, if you are looking to create a thermal effect (insert any kind of condition you want), you can do some continuous ultrasound to prep the tissue and warm it up. Then, you can immediately jump into your manual therapies or your tissue techniques. Once you get the desired effect, you can do some neuro reeducation and some active motion movements. We are upregulating the nervous system. Remember, we prep the tissue, we treat the tissue, we reeducate locally to turn on those motor patterns, and then we integrate. This is my approach when I am treating a tight joint or contracted tissue. Now, if my goal is to have a non-thermal effect and I just want to promote healing (post-surgery, new injury), I am going to prep the tissue with ultrasound first. Then, I am going to do my manual therapies and tissue techniques. I might also get into some deeper tissues to get some movement in there. From there, I might try to reeducate if I gain some new range of motion. We want the brain to accept that new range of motion. Remember, neuro reeducation is when your patient is "downloading the software" to move more efficiently. Then from there, you integrate. The neuromuscular system gets activated, it upregulates, and they start to improve. These are two general recipes that I personally use when it comes to ultrasound. This is very individualized, and I do not on every single patient
Phonophoresis is interesting. Some clinicians do photophoresis first. In my humble opinion, if you are driving medication into the area, you want to keep the medication in the area as long as possible. Thus, I do not want to drive in medication and then do a manual treatment as this will flush out everything that I just pushed in there. When it comes to certain things like an acute injury or a flared up tendon, I like to do photophoresis last or post-treatment. I might start off with a hot pack to warm up the area and prep the tissue. This also usually relaxes and calms the patient if they are in pain. Then, I will do my manual treatments. Next, I reeducate and integrate. In the end, I might choose to do some cryotherapy to cool them down. We know that in the last lecture, we want to do this for about 10 minutes as the body reheats. I might have them stretch a little bit afterward. Lastly, I might have them do a phonophoresis session to put medication in and then go home and relax. Hopefully, this is going to help everything to calm down. This is the recipe that I have used before that has worked well with patients with plantar fasciitis and patellar and Achilles tendinopathies.
Bottom Line
- Occupational Therapist considerations
- US and Phono have some good utility for different MSK conditions.
- The current research provides some clinical guidelines.
- Treatment parameters should be chosen and adjusted based upon the research, treatment goals, and patient response to treatment.
- The OT must consider the safety of using these treatment methods with each patient.
The bottom line, when we talk about application, is that ultrasound and phono have good utility for different musculoskeletal conditions. The current research provides some clinical guidelines, and the treatment parameters should be chosen and adjusted based on what we talked about as far as research goals and the patient's response. We have to consider the safety of it first, and then when and where we should we apply it from there.
Module V: Ultrasound Research (2010-2020)
Evidence Summary
- The body of therapeutic ultrasound evidence is large with over 40 years of published studies.
- There is moderate evidence supporting the treatment of different MSK conditions. However, there are some studies that reported inconclusive results.
- This section will summarize the most relevant evidence from the past twenty years based upon common clinical questions.
As I mentioned at the beginning of the talk, there are 30 to 40 years of research that's out on ultrasound. The body of research is huge. I did an evidence-based appraisal going back 10 years as I think it is important to look at the current research and see how the evidence is applied. Let's look at some clinical questions.
Clinical Questions
Therapeutic Ultrasound.
1) Q: Does ultrasound decrease pain, increase joint ROM, and function after musculoskeletal injury or pathology?
- (+): Ultrasound had positive results for all outcomes
- 2019- Wu et al. Clin Rehabil (Knee OA)
- 2018- Ozgonenel et al. J Med Ultrasound (Knee OA)
- 2016- Zhang et al. Clin Rehabil (Knee OA)
- 2017- Yegin et al. Ultrasound Med Biol (Knee OA)
- 2010- Rutjes et al. Cochrane Database Review (Knee OA)
- (-): Ultrasound had weak to no results for all outcomes
- 2020- Ebadi et al. Cochrane Database Review (LBP)
- 2020- Karakas et al. Clin Rehabil (Knee OA)
- 2020- Papadopoulos and Mani. Int J Low Extrem Wounds (LE Pain)
- 2010- Shanks et al. Foot (LE MSK)
From 2010 all the way through 2019, most of the current research is on knee osteoarthritis, and all these studies reported favorable outcomes with decreased pain, increased range of motion, and increased functional measures, either functionally like gait or using a patient-related outcome measure. However, in 2020, a systematic review showed that ultrasound did not have positive outcomes with low back pain. Karakas and Papadopoul
