Shoshana: In this session we are going to go over the effects of sensory issues on visual and sensory processing in children and adults with traumatic brain injury. This is not just for our clients, this may be an undiagnosed or misdiagnosed issue in yourselves as well, and I will explain that as we go along.
Traumatic Brain Injury (TBI) Changes
Physical Changes
Some of the physical changes that occur in traumatic brain injury are:
- Paralysis and motor planning
- Loss of motor coordination and agility
- Abnormal movement patterns
- Structural imbalances
- Tremors and spasticity
- Headaches/migraines
- Fatigue and weakness
- Seizures
- Oral motor dysfunction
There can be paralysis and motor planning issues, loss of motor coordination and agility, abnormal movement patterns, structural imbalances in the body (right/left side, top/bottom, front/back), tremors and spasticity, headaches and migraines, which is a major one that we are going to talk about, fatigue and weakness, seizure disorders, and oral motor dysfunction. I am sure if any of you work in this area, you can name a host of other ones.
Cognitive Issues
The cognitive issues which will come up a lot in this presentation can include:
- Attention deficit
- Poor concentration and memory
- Communication
- Problem solving
- Socialization and communication
- Difficulties initiating and planning activities
- Impulsivity and difficulty problem solving
- Poor judgment and reasoning
- Visual stress and visual distortions
- Sensory modulation and tolerances
We can see an attention deficit disorder, with either very hyper or low energy and spacey. There can also be poor concentration and memory, decreased communication skills for expressive and receptive language, and poor problem solving. When you cannot understand what people are saying accurately, you cannot express yourself and socialization and communication become very difficult. They may also have trouble initiating and planning activities, so there may be a lot of anxiety and fear that goes along with this. Many people will pull back from society and relationships. We also see impulsivity, difficulty with problem solving, and poor judgment and reasoning. They may have poor safety awareness. For example, driving a car may be extremely difficult, and they may not be able to do it anymore. There can be visual stress and visual distortions, which we are going to go over in this presentation, and poor sensory modulation and tolerances.
Behavorial Issues
Some of the behavioral issues include:
- Agitation and irritability
- Anxiety
- Verbal and physical aggressiveness or passivity
- Impulsivity
- Depression
- Difficulty with interpersonal relationships
They may have agitation and irritability, anxiety, verbal and physical aggressiveness or passivity, impulsivity, depression, and difficulty with interpersonal relationships. Isolation is a big issue as well.
Functional Issues
There are also many functional issues.
- Academic or work related tasks
- Computer use, writing, reading, copying
- Ambulation
- Driving
- Sports
- ADLs
- Environmental: patterns, lighting, accessibility, safety
Many of the issues are seen in those with concussions in the sports area. There can be problems with academic or work-related tasks, computer use, writing, reading and copying. We will take a closer look at these issues and talk more about the glare sensitivity, like reading on a white background. There can also be issues with ambulation, stair climbing, going on escalators, uneven surfaces, driving, riding a bicycle, sports performance, and activities of daily living. These deficits could be from mild to severe. If anybody has read the book Stoke of Insight by Dr. Jill Bolte Taylor, she describes how even just grabbing a spoon was a major task for her after her massive stroke at the age of 28. As a neuroscientist, she was able to describe, when she achieved function many years later, what it was like to be locked in a body that did not work, and how every little task that we automatically do became a major ordeal and effort to re-learn. Environmental variables, such as patterns, lighting, accessibility, and safety need to be addressed.
Causes of TBI
Some of the causes of traumatic brain injury include:
- Strokes
- Tumors
- Disease
- Toxins
- Near drowning
- Electrocution
- Head trauma: falls, sports injuries, and vehicle accidents
- Any forceful blow to head or neck
Many of these you probably know, but we will go over this. Traumatic brain injuries can be caused by strokes, ischemic or hemorrhagic, tumors, disease, toxins, drowning and hypoxia, electrocution, and head trauma, like falls, concussions, sports injuries, vehicle accidents, and other accidental issues. Additionally, any forceful blow to the head or neck can cause a traumatic brain injury. Sometimes people do not even know that they have incurred a traumatic brain injury because they do not get it checked it out or receive medical care. Often, they do not lose consciousness or have a headache. Many issues may come up like visual distortions that are identified with learning or other types of issues. These also may be related to an old injury or a recent injury. Brain scans can identify old injuries.
Incidence of TBI
The incidence of TBI is pretty high. These are some of the statistics.
- 1,500,000 new cases of TBI reported each year (Centers for Disease Control)
- 50,000 to 110,000 are severely disabled (National Institutes of Health)
- 5.3 million Americans living today with TBI (NIH)
- Visual stress and visual perceptual problems are reported by many people with TBI. It affects reading, math, working at a computer, depth perception, safety, comfort, and many other tasks involving balance and vision.
Many TBIs go unreported and can manifest in things like learning and emotional issues. These are the main issues that I work with as an Irlen Diagnostician and occupational therapist, working in the area of visual sensory processing disorders.
Symptoms Related to Light Sensitivity and Visual Stress
There can be many issues related to light sensitivity and visual stress.
- Attention deficit
- Strain or fatigue
- Poor depth perception
- Light sensitivity
- Inefficient reading
- Slow reading rate
The major one is an attention deficit. This may not be related to a brain injury especially if someone has had ADD or ADHD prior to the brain injury. This can include problems with concentrating and sustained attention while reading or doing schoolwork. Individuals may have difficulty staying on task and may need to take more breaks than normal. They do not work efficiently. They may need to look away from the task often, which also can impact efficiency. They can become restless, fidgety, or tired, because they are working much too hard to stay on task. People who cannot manage these symptoms can become impulsive, argumentative, or they can just check out and become spacey.
Strain or fatigue is another major issue because they are working so much harder than other people to stay on task or to receive information and modulate that information from the environment. It can be overwhelming. Tension, fatigue, sleepiness, and headaches can also occur when reading or other visually stressful tasks. Strain can interfere with reading for pleasure, studying, doing math tasks, listening, or expressing one's self.
Often, with a brain injury, the eyes do not work together well. They may start to only use one dominant eye and can lose depth perception. The inability to accurately judge distances or spatial relations is affected as well. They may be unsure of their body in space, and kinesthetic awareness can be impacted. Examples are proprioception on escalators, moving through hallways, navigating stairs, and using their body for more skilled performances like sports, dancing, and driving. They may get dizzy or nauseous, and this can also produce handwriting problems, especially when copying from the board or from a PowerPoint, which is using near and far vision.
One major thing that we address is light sensitivity. This is often not diagnosed, even by eye doctors. It can cause intolerance to glare. Fluorescent lighting is probably the worst lighting that we could have, and it is in most schools and office buildings. Bright lights are also an issue. If there are bulbs that are not sconced or recessed, the bright, glary light can be extremely stressful, especially at night. When driving at night, signage often has bright LED lights, and these can be extremely stressful to the eyes. Sunlight and glare ofr of windows or shiny surfaces such as marble and whiteboards can be problematic. Often, we do not realize how much that light on a bright, white background, like PowerPoints, computer screens, or whiteboards, can be stressing a large population of people, not just those with traumatic brain injury. There can be discomfort or difficulty working under bright or fluorescent lights or using a computer screen. I did not realize that l had Irlen Syndrome, or Scotopic Sensitivity Syndrome (light sensitivity), until I went to my training to be an Irlen Screener 15 years ago. Out of a 35 year career in education and occupational therapy, and most of that time working under fluorescent lighting, I did not realize that some of my antsy-ness, lack of concentration, and fatigue, that I was experiencing, had a lot to do with the type of lighting that I was working under. I learned that I had some visual distortions thate were impacting my ability to stay focused during reading. Using a customized piece of colored plastic, I was able to see things clearly even with my glasses. This had nothing to do with acuity (I have worn glasses since age 6), but it had to do with the way my brain was processing light. When you have a brain injury, brain processing becomes compromised even more. For example, the individual may have had a learning issue prior to the brain injury, but it can be exacerbated and they may not be able to compensate as they did when younger or healthier. Another tip is to be careful when using fluorescent lighting. A better option are lamps with LED lights, if you like energy efficient lighting. Old incandescent lights and natural light are actually the healthiest options for the human eye. Try different lighting situations for you and your client.
Inefficient reading is another area to address. Not everybody who has these issues has a reading problem. However, for those with reading issues, you can see positive changes immediately when you change the lighting or you use some of the accommodations that we will describe. To test this, you want age appropriate reading material with as much print as possible and not too big because that makes it easier to see beyond the distortions. Visual distortions can make the brain perceive the dots as moving. It might be hard to choose the correct answer as a result. It can progressively get worse, and you will see more and more mistakes. Reading maps, diagrams, and music notes can also be extremely stressful. I see a lot of musicians who have to read very complicated musical scores that have difficulties. Often, people will memorize if they are able to do that, and just look at the musical score for cuing. Problems may also include print that shifts, shakes, blurs, moves, doubles, disappears and becomes difficult to perceive. Additionally, there are some very bizarre visual perceptual distortions that people have described to me that are beyond even the more common ones that I see. If you have had this all your life, or if it becomes an issue and you do not know what to call it, people may say it is not real. However, it is real as it is how your brain is processing light and not a functional issue of they eye. Later, we will go over that and look at some of the research on that.
Slow reading rate can be seen as a problem with tracking, correctly identifying words, or having the ability to skim-read. Some of my clients went to a developmental optometrist or a visual neurologist as a child, and they were diagnosed with convergence insufficiency, accommodative stress, binocular issues, or tracking issues. Perhaps it was not a functional issue after all, but rather a brain processing issue that was causing fatigue and affecting those muscles of the eyes and the way that the information was being transmitted.
Allopathic and Integrative Treatments
There are many treatments available (Figure 1), and one piece of the puzzle may not be the whole picture.
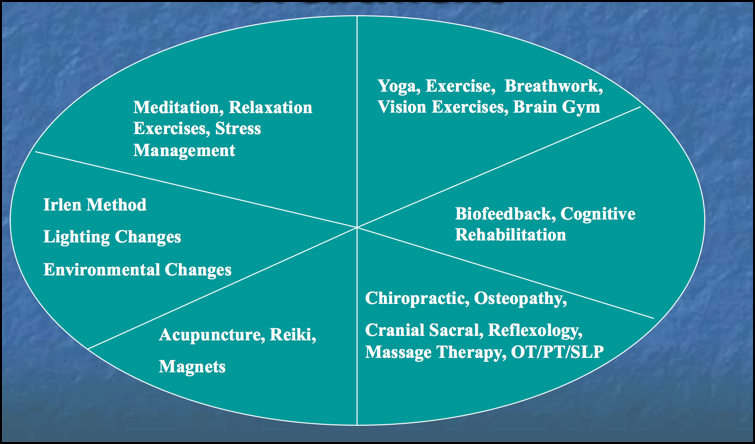
Figure 1. Examples of treatments.
For example, I might recommend stress reduction techniques that they can do at home, in a class, or they can go to another practitioner. Some of these are not for everybody. Sometimes you can reach your goals quicker by eliminating the visual stress, which we will describe today. It can also be a lot cheaper if you are paying out of pocket for a lot of these other things. Visual stress and light sensitivity are easy to assess. We can then eliminate it as a factor and go on to other areas. But once you eliminate that visual sensory overload, so much in the body can be remedied and more quickly.
Visual Stress and Distortions
We are going to overview visual stress and distortions, Visual Irlen Syndrome or Scoptic Sensitivity Syndrome, in this talk. Through the retinal system and the parvocellular and magnocellular cells, light and imagery is transmitted to the occipital cortex so that the brain can process the information. When this process is under stress, it can affect all the other sensory systems in the body. It can also affect your emotional balance and well-being, and produce anxiety, depression, manic depression, and other cognitive and emotional issues. It can block fluid transmission of hormones and affect body functions, like your sleep/wake cycle and your immune system.
Blurry vision and visual distortions are a problem as is depth perception. Many of my clients have fender benders, a problem parking, and changing lanes when they drive. They also bump into corners of walls, furniture, and even people. Distortions can occur where there are white spaces in between the words as in Figure 2.
Figure 2. Examples of white spaces. (©1987 Perceptual Development Corp.)
It can be mild to severe. With sustained attention and focus, it can become worse. As a child, I had this issue. However, I was an art major in high school and thought I was making that happen as part of my creativity. My attention would be diverted, and when the teacher would call on me to read out loud, I would not know where I was as I was so involved in the patterns on the page. If I blinked my eyes or shifted my body, it would go away. Once you release the stress, that can take it away, but it might come back. This picture is a static view of something that is always changing, and it can go from worse to severe. This distortion is called washout in Figure 3.
Figure 3. Example of "washout." (©1987 Perceptual Development Corp.)
It actually looks like the typeset is not clear and not even. As you read across the page, it can change. It can go from dark and clear to washed out. The letters can start disappearing on the edges in peripheral vision. It can be very frustrating to try to stay focused and see the letters clearly if this gets more severe. This is an example of "blurry," and this is the one that is often misdiagnosed as acuity (Figure 4).
