Gina: Thank you all of you for attending this webinar.
Health, Wellness and OT
Nutrition and health are very hot topics these days. How can OTs become involved and integrate this into their practice settings? Health and wellness, in general, have become a lot more at the forefront of occupational therapy. In 2008, AJOT published an article that outlined how OT services could be part of a promotion of health and the prevention of disease and disability. It mentioned specifically how OT could be used in primary and secondary prevention. Primary prevention is how can OTs prevent chronic illness before there is a diagnosis, and secondary prevention is how can we prevent, halt, or slow the progression of the disease after it has been diagnosed. The article specifically mentioned that OTs can work in education and training regarding eating habits, activity level, and prevention of secondary disability, especially with obesity. Many other studies have elaborated on this concept of OTs having a unique role in prevention and health promotion.
A very recent journal article from this past February in the Journal of Environmental Research in Public Health brought this issue again to the forefront. This is really important as now we are listed in journals outside of OT journals. This article was titled, Preparing Physical and Occupational Therapists to be Health Promotion Practitioners: A Call for Action. It stated how practitioners can be part of health-focused care, and it mentions nutrition optimization. Another piece of the article was that OT practitioners, when they got to OT school, especially if they were trained recently, learned about disease prevention and health promotion as part of their course content. However, out in the field and within practice, occupational therapists are not always treating with that prevention mindset. How can we address that gap between what current entry-level providers are learning in school and providing that knowledge to clients to establish healthy eating habits and other health-promoting behaviors?
OT Practice Framework
I also wanted to go to the OT Practice Framework because that is the backbone of our profession. In the framework is "Achieving health, well-being, and participation" in life through engagement in occupation. It is an overarching statement that describes "the domain and process of OT" and the keywords of health and well-being, along with participation in life, are found throughout. My question is, "If health and well-being are so prevalent in the backbone of our profession, and if dietary habits and patterns in many cases influence that piece of health and well-being, why are we as clinicians not paying more attention to that? I feel like this is one of the most important things that an OT can do to support client health and well-being throughout multiple settings.
Where is Nutrition Mentioned in the Practice Framework?
If you look even a little bit deeper in the OTPF, there is a list of categories and nutrition is there, albeit a bit buried. There is also a list of IADLs and one of the sub-categories is called health management and maintenance. Some of the descriptions they use have to do with "Developing and managing routines for health and wellness promotions such as physical fitness, nutrition, decreased health risk behaviors, and medication routines." One thing I wanted to share on the side is that that the OTPF is in the process of being revised, and there has been some discussion about taking health management and maintenance out of IADLs and renaming it health and wellness self-care or health and wellness self-management. This change would be listing it as its own occupation because this is a piece of daily routines for many, and it is at the forefront of healthcare right now.
Many OTs ask, "If I do health or nutrition activities with a patient, how do I bill that?" The answer is straightforward. These routines are listed under health management and maintenance, which is an IADL. If it is a client-centered focused activity, it could also be billed under therapeutic activities. These are just a few ideas. Of course, if there are health and nutrition interventions that could also be billed as a group, you can do that as well.
I am now going to pass the microphone to Yanet, who I have had the pleasure of working with for the past several months on a project that relates to community-dwelling participants focusing on nutrition amongst other health behaviors in group settings.
Participant Video-Lifestyle Medicine
Yanet: The information that I will be sharing with you is a result from my master's level research and other occupational therapy students, under the guidance of Dr. Donna Man, at Eastern Washington University. We developed a 10-week class program where we educated community participants on how to make health behavior changes. In every class, we had a meal-preparation activity, where we showed participants how to cook healthier and introduced them to foods that they might not have known about.
As part of my fieldwork work placement, I am delivering these courses to four community agencies. Two of them are taught in English and two in Spanish. Although this is a very non-traditional setting, it is an emerging practice area for occupational therapists. I think that these programs can also be modified so that they can be provided at an adult inpatient or outpatient setting. If you have some interest or would like to know more about this program, please contact either Gina or myself for more information on the class.
We are going to see a video of a father and a son wanting to improve their eating habits. The father currently lives with his son, who is requires assistance with IADLs. He had a CVA a few years ago and is receiving occupational therapy and physical therapy for strengthening as well as speech therapy for some residual expressive aphasia. Prior to his CVA, he was very fluent in English, but due to this event, he is only able to communicate in Spanish. In the video, he will be speaking Spanish. His son, who has switched to a plant-based eating diet several years ago, has been very supportive in helping his father make some changes around his nutrition. Let's go ahead and watch that video now.
Video 1

I hope that you were able to identify that there are many factors that are playing a role in the father's current behavior. He mentioned that he wants to eat healthier to feel better. His CVA was a cue for him to start making some changes in his lifestyle, especially around nutrition. There are some personal factors and motivation for him to feel better because he mentioned how his weight right affects his mobility. He has a lot of pain in his knees, and so he wholeheartedly believes that by changing his nutrition and eating healthier, he can feel better and gain more independence in his daily activities. Besides having a great support system from his son and all of these internal factors that are motivating him, there are many other factors that are playing a role in his health-behavior change. As occupational therapists, the best thing for us to understand is that this process is very complex.
Behavior Change Models
I want to introduce you to a few behavior-change models that exist.
Transtheoretical Model (Stages of Change)
The first one is a Transtheoretical Model, otherwise known as the Stages of Change (Prochaska, DiClemente, & Norcross,1992). This model identifies six Stages of Change where we can identify what stage a participant is in and how ready they are to adopting a health behavior change.
Health Belief Model
Then, we have the Health Belief Model (Rosenstock,1974). This model identifies four additional factors that influence health behavior change. The first one is susceptibility. If I believe that my current behavior is going to make me susceptible to a disease, this is going to influence my ability to make a health behavior change. The next is severity. If I believe that my behavior is going to lead to severe outcomes, like a disability, that is also going to play in my favor. And, if I believe that by making a health behavior change, the benefits are going to outweigh the barriers, that is also going to increase my chances of making a health behavior change in my life.
At the end of the presentation, we have resources that will directly lead you to more information on these models. Unfortunately, we cannot dive in too much, but these models have existed independent of each other.
Dynamic HEALT²H Model
As a result of our qualitative data from our research, we developed the Dynamic HEALT²H Model, where we integrated these two existing models together.
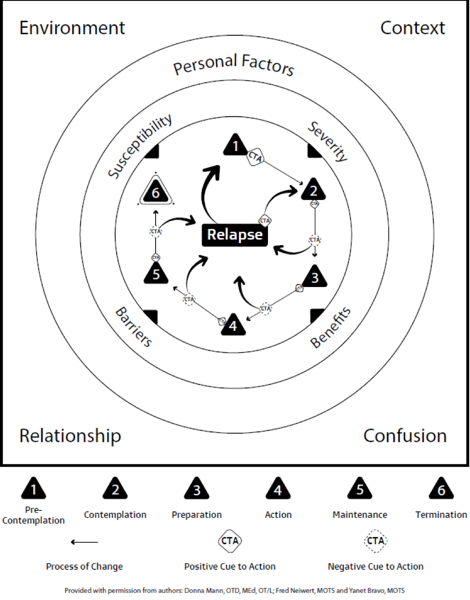
Figure 1. Dynamic HEALT²H Model.
In the center, we have the Stages of Change, one through six. They are explained here at the bottom. Then, the second layer is the Health Belief Model, the four factors that are further influencing this center process. As part of our model, we also figured that there are a lot of other factors that are playing a role in our behavior which include personal factors. Personal factors can be those internal influences that affect a health behavior change process like motivation, self-efficacy, and current habits. We also found that the environment and context also play huge roles in the health behavior change process. As occupational therapists, these terms are not new for us. We know how much our environment and our context play a role in our behavior. We also included "relationship" and "confusion" down here at the bottom. A supportive relationship, with our family and friends, can also foster a health behavior change process. As far as the term confusion, there is a lot of new information on nutrition as this tends to change a lot. For example, there are a lot of new fad diets that can make it very difficult for our patients or clients to make decisions around their nutrition. On a bigger scale, all of these factors play a huge role in the Stages of Change and how susceptible a person can be at adopting a health behavior change. I know that this diagram can be a little confusing and hard to digest at first glance, but we created an acronym to help occupational therapists implement different strategies within interventions to help facilitate that health behavior change process.
The Dynamic HEALT²H Model can be applied to various behaviors like physical activity, sleep, and stress management. For the sake of this presentation, we will be applying it to nutrition. As I mentioned, we have the acronym HEALT²H, which is capitalized. There is a little exponent because there are two Ts in this acronym.
Holistic Approach
The H is for a holistic approach. We need to be sensitive to personal and environmental factors that can influence behavior change. Every patient is going to be different, and there are going to be various personal environmental factors that are playing a role. In the case of our participant, the father relocated from Venezuela. There were a lot of environmental changes, not only in his lifestyle but in his nutrition as well. His personal factors and motivation of wanting to feel better are also affecting the behavior change process. As occupational therapists, we need to remember to apply this holistic lens to each individual to help influence this process.
Evidence-based Approach
"E" is for an evidence-based approach. As occupational therapists, we know we need to look at the evidence for our interventions. This is not only using evidence but also helping our patients evaluate the evidence for themselves so that they can be active agents in their health behavior change process. When we are looking at the evidence, the only diet that research has shown to reduce or reverse heart disease was called the whole food plant-based diet. We have a resource there for you to look more into this diet and what it entails. Gina will be providing some more nutrition tools and resources for you to access so that you can apply to your practice.
Antibody Metaphor
"A" is for antibody metaphor. Much like we need booster vaccines to prevent infectious diseases, our patients and clients will need boosters of interventions from different healthcare professionals, not just occupational therapists, along with the path towards health behavior change for the prevention of non-communicable or non-infectious diseases. One of the most important things is to educate our clients and patients is that relapse is going to occur. However, we can integrate prevention activities over time to maintain the disease prevention process. I am going to go back to that diagram of the Dynamic HEALT²H Model again. As you can see in the Stages of Change, we have what is called cue to action. This is where we need to incorporate different activities and interventions that are going to be stage-matched and best received by our patients based on how ready they are on adopting a health behavior change. There are going to be a lot of opportunities for us to put in those into booster vaccines of interventions to help our patients get back on the wagon when they do relapse.
Lifestyle Medicine
Lifestyle medicine was the framework of care delivery that we used when providing the program. This is a concept from the American College of Lifestyle Medicine that is comprised of physicians and other healthcare providers who are committed to the prevention of chronic diseases. Lifestyle medicine focuses on treating the causes of disease rather than the symptoms of the disease. It is no secret today that non-communicable diseases such as cardiovascular disease, diabetes, coronary artery disease are lifestyle related and can be prevented through things like nutrition, physical activity, stress and sleep management, and social relationships. Lifestyle medicine really encompasses that holistic approach as well as how we educate our participants on various areas to help improve overall health and wellness.
Therapeutic Relationship
The first T is for the therapeutic relationship. I know this term is not new to any of you that are listening today. Each patient and client is different so the way that we interact with them is going to be different. Utilizing a unique approach helps to foster the therapeutic relationship between the therapist and the client. This also helps to facilitate the health behavior change process at various stages.
Team Approach
The second T is for team approach. It is important to have interprofessional collaborations. This way we can seek the expertise from other professionals to deliver the highest level of care possible. This collaboration can be with dieticians, physicians, psychologists, nurses, and even exercise physiologists. We can all work together and provide those booster shots along the way because we are not going to be with our patients at every step of the way. The team all needs to be focused on improving health and wellness at every step of the way.

