Overview
- Unique Value of OT in Critical Care
- Prevention of Hospital-Acquired Deficits
- Outcome Measures
- Evidence-Based OT Interventions
- Role of Advocacy
- Q&A
Meghan: Hi, everyone, and thank you for attending our webinar. Lyndsay and I are excited to share our knowledge with you. Before we dive into OT's role in critical care, I wanted to take a moment to explain why it is important and why we are so passionate about promoting OT's presence within the critical care environment. First, there has been a recent shift in patient care that advocates for long-term recovery and overall quality of life for survivors and their families of critical illness. The abundance of research and literature recognizing therapy's role in recovery is much more prevalent than before. Examples are early mobility and including the therapist during spontaneous awake trials or delirium prevention and the overall awareness of how a therapist can have a profound impact on patient recovery during the most critical stages of illness. Evidence suggests that an occupational therapist in critical care can contribute to recovery in areas such as functional outcomes, length of stay, and delirium prevention. With the information that you will learn through our webinar today, we hope you, as clinicians, also feel empowered to promote OT's role and unique value for all survivors of critical illness. In my opinion, our biggest barrier is our role comprehension and understanding. What I mean by that is a lot of people we work with from day to day do not truly comprehend what we do as occupational therapists. Educating our team members on our role in the ICU is crucial because OTs can have such a significant impact on patients' early success, survival, and overall quality of life. With that being said, I hope you enjoy our webinar today on OT's role in critical care, and more importantly, I hope you feel empowered to promote, protect, and spread awareness on the services that we as a profession can provide for our patients. I also hope you feel confident to administer strategic outcome measures and deliver evidence-based treatment interventions.
Unique Value of OT in Critical Care
- Holistic
- Physical, cognitive, psychological
- Client-centered
- Interventions that are meaningful to the patient
- Person-Environment-Occupational Model
- Intimate understanding of the transactional relationship between each component
Lyndsay: Hello, everybody. This first part is diving in a little bit to the unique value of OT in critical care. The core of the profession of OT has always been holistic. We are not just looking at one specific body system or a functional deficit, but we really want to see how all of the body systems work together. Then, using that information from our holistic view, we want to create client-centered interventions that are meaningful to the patient. The piece that is important to the critical care environment for me is the Person-Environment-Occupation Model. We have in-depth theoretical training in the PEO model. We understand the intimate relationship between each person's ability levels, the occupations that they want to perform, and then the environment in which they are performing those occupations. Nothing can be more abnormal than an ICU environment. It is either sensory overload or sensory deprivation, and it usually has some component of immobility to it or a loss of consciousness due to different medications. We, as OTs, have a very in-depth understanding of that transactional relationship and can help patients progress through their ICU stay within this understanding.
Hospital-Acquired Deficits
About 10 years ago, the Society of Critical Care Medicine identified that patients who experience stays within the ICU have new or worsening physical, cognitive, or psychological symptoms. They determined that this cluster of symptoms is post-intensive care syndrome (Desai, Law, & Needham, 2013).
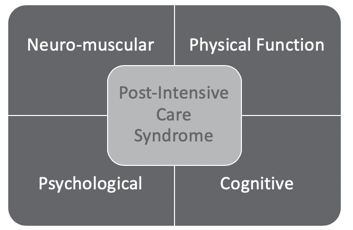
Figure 1. Post-Intensive Care Syndrome.
Post intensive care syndrome occurs in 50 to 70% of ICU survivors. It manifests in four specific domains that we will then utilize throughout the rest of our presentation. These four domains are neuromuscular, physical functioning, psychological, and cognitive. As we progress through this presentation, we will identify each of these four domains and outcome measures that can be used to assess each of these four domains. Then, we will break down specific interventions for these domains.
Neuromuscular
- Critical Illness Polyneuropathy & Myopathy
- Diffuse atrophy
- 85-95% of ICU survivors experience persistent weakness
- Also- impaired deep tendon reflex, sensory loss, foot drop, and heterotopic ossification
(Desai, Law, & Needham, 2013)
This includes any sort of critical illness, polyneuropathy, myopathy, or diffuse atrophy. Diffuse atrophy is present in 85 to 95% of ICU survivors. It is also called ICU-acquired weakness. This might be a term that you guys have heard before. Risk factors for neuromuscular deficits include sepsis, multi-organ dysfunction, or any periods of immobility or bed rest, which is obviously pretty common in the ICU due to the critical nature of a patient's medical state. The neuromuscular impairments are also associated with decreased functional independence as well as decreases on the Six-Minute Walk Test. All of these are pretty imperative for people to be able to perform ADLs, IADLs, and functional mobility.
Physical Function
- Impairment in ADLs & IADLs
- ADLs: >50% of ICU survivors requiring assistance in the first year after an illness
- IADLs: >70% of ICU survivors requiring assistance in the first year after an illness
- Decreased 6-min walk distance
(Desai, Law, & Needham, 2013)
As you can see, 50% of ICU survivors experience deficits in ADL independence in the first year of their illness status post-discharge from the ICU, and 70% of ICU survivors experience deficits in IADL performance. Symptoms of this are impairments in ADLs and IADLs, as well as a Six-Minute Walk Test. Risk factors include ICU-acquired illnesses, increased age over the age of 65, or pre-existing impairments with IADLs. Psychological symptoms include depression, post-traumatic stress disorder, and anxiety. Risk factors for all of these include delusional memories of the ICU, which is common during delirium. We will talk about this a little bit later on in the presentation. Other risk factors include sedation, the presence of restraints, and increased time on a mechanical ventilator.
Psychological
- Depression
- Occurs in more than 1 in 3 ICU survivors
- Independently associated with severity of executive dysfunction
- Risk factor: delirium
- Post-traumatic Stress Syndrome
- 60% of ICU survivors
- Risk factor: delirium
- Anxiety
- Experienced by up to 85% of patients in the ICU
- 62% of patients experience anxiety up to a year post-discharge
(Desai, Law, & Needham, 2013)
This all relates to impairment in physical functioning which then translates to some of these symptoms here. As you can see, depression occurs in about 1/3 of ICU survivors, and it is independently associated with the severity of executive functioning. Also, post-traumatic stress syndrome, or post-traumatic stress disorder, is present in 60% of ICU survivors. Anxiety is experienced in up to 85% of ICU survivors with 62% experiencing anxiety symptoms one-year post-discharge. These acute symptoms are being carried with them out into the community as they return to their premorbid lifestyle.
Cognitive
- Impairments in memory, attention, & executive functioning
- 70-100% of ICU survivors at hospital discharge
- 46-78% of ICU survivors at 1-year post-discharge
- Impairments in executive functioning are associated with higher rates of depression
(Desai, Law, & Needham, 2013)
Lastly, there are cognitive impairments related to the ICU including impairments in memory, attention, and executive functioning. Risk factors for these impairments include ICU delirium, periods of sedation, as well as any sort of hypoglycemic event that has been experienced during their ICU stay. And, 70 to 100% of ICU survivors will experience some sort of cognitive impairment below their baseline level of performance at their time of discharge, and almost 1/2 to 3/4 will experience continued cognitive deficits, at one-year post-hospital discharge.
Now, I am going to pass it over to Meghan to go a little bit more in-depth on some outcome measures within these four domains.
Outcome Measures
Meghan: Let's talk about outcome measures. The ability to evaluate and measure a patient's current level of function is extremely valuable to any clinician. It helps inform patients about their own recovery, helps identify patients who may require rehabilitation interventions, and also it allows therapists to monitor that responsiveness to such interventions. To highlight why evaluating a patient's current level of function is so important, I would like to share a few statistics from a recent article published in the Journal for Critical Care (Perry et al., 2017). ICU survivors with multi-organ failure are susceptible to physical morbidity with up to 30% muscle loss within the first 10 days of their ICU admission. I think this is really eye-opening. Another huge statistic that I took from that article is the prevalence of ICU-acquired weakness is 25 to 40% of all patients intubated over 48 hours. That, to me, is so alarming. Weakness and physical functioning are predictive of subsequent length of stay, post-discharge survival, healthcare utilization, quality of life, and the ability to return home. Therefore, the need for occupational therapists to have a way to objectively measure a patient's ability to engage in functional activity, while being admitted to the critical care unit, is extremely important. Through the use of outcome measures, we are able to inform patients and their families on projected recovery, identify patients who may require rehabilitation interventions, and monitor even the sickest patient's response to our robust OT interventions.
The evaluation of physical function is complex and is influenced by multiple interacting factors including strength, range of motion, proprioception, balance, cognition, and psychological issues. It is a very unique environment in the ICU. Factors that are very specific to the ICU such as sedation, the severity of illness, and mechanical devices play a role and influence how accessible a patient may be. So, determining the specific purpose of assessing function is important. For example, if your purpose is to evaluate intervention efficiency, you want to consider that specific effect of the intervention and match it with an instrument that will evaluate the effect. Before we start going into specific outcome measures, I think we really need to talk about factors that we should consider when choosing an outcome measure as outlined in Figure 2.
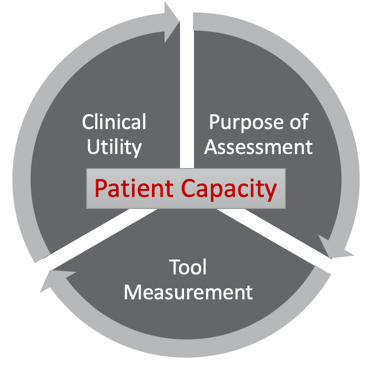
Figure 2. Outcome measure factors (Perry et al., 2017).
First, we need to look at the purpose of the assessment. Are you trying to show an increase in independence with self-care, improved level of arousal, ability to follow one-step commands, or looking at the level of orientation to determine if a patient has emerged out of the post-amnestic state? Whatever your primary aim is you want to be sure you use an appropriate instrument to evaluate that domain.
Another critical component, when choosing an outcome measure is the measurement properties. Is your tool reliable, is it valid, and does it demonstrate change? For example, will it show if a low-level patient is responsive to a very specific intervention? The instrument should illustrate change over time and must have a limited floor-to-ceiling effect across the expected evaluation time points. It is very important to be able to detect clinically meaningful changes over time, regardless if you or your peer is administering the assessment. Patients who are surviving any kind of critical illness may have very small gains, but if it is appropriate to advocate for an acute rehab setting, it is so important to make sure you are illustrating markers of success.
The third factor to consider when choosing an outcome measure is clinical utility. Be mindful of the cost, the training, the equipment, and the expertise required. As I move forward to educate you on some valuable assessments, I want you to dive a little deeper and be sure it is practical for your specific settings. Lyndsay and I want you to be set up for success, and we want this to be a useful component of your daily practice. Do your due diligence and make sure that the assessment you choose is right for the culture, utilization of therapy services, and the level of expertise that you are currently working with.
Finally, therapists should always consider a patient's capacity when choosing an outcome measure for the ICU. Instruments and assessments will always be dependent on the patient's effort. I typically never make "always" comments, but this is true. Please always consider if the assessment is feasible. Is the patient is alert, can they follow instructions, and do they have any premorbid deficits that may impact their motivation? All things are connected, therefore, it is important to stop and think about "the why." You are going to hear me talk about "the why" a lot during this talk. If we can justify what we are doing, then the world is our oyster. Why are you choosing this assessment for this patient at this time? When we talk about "the why," we have a much greater ability to utilize our time and evaluate patients efficiently and effectively. If you would like a more in-depth conversation on this topic of what outcome measure to choose and these four very important components, please look at our reference page. The article by Perry et al. (2017) that outlines this whole process.
Now that we have discussed the important factors to consider when choosing an outcome measure, I would like to now educate you on some robust outcome measures specific to the ICU. Hopefully, you will be able to implement them in your practice as soon as you return. Talking about outcome measures can be dry so I really want you all to understand my approach today. I will not be talking about the sensitivity, specificity, inter-relater reliability, or validity of any assessment, but I have provided links to every single outcome measure that I will be discussing and resources from our reference page. Please feel free to navigate each instrument's statistical properties on your own time. Instead, I really want to discuss the clinical significance of how each measure can offer recommendations for evidence-based interventions. Again, I want you to leave this webinar with the why and know that the instrument that you choose works for your practice because of very specific reasons.
Physical Function
- Basic:
- Manual Muscle Testing (MMT)
- Dynamometry
- Advanced:
- The Clinical Frailty Scale
- https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-016-0292-4
- Functional Status Score – ICU
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5292321/
- ICU Mobility Scale
- http://www.scielo.br/scielo.php?pid=S1806-37132016000600429&script=sci_arttext
- The Clinical Frailty Scale
- Additional Outcomes:
- Physical Function in ICU
- Chelsea Critical Care Physical Assessment Tool
(Perry et al., 2017)
I have broken out the outcome measures into basic and advanced. For a basic assessment, you can always manual muscle test or test grip and pinch using a dynamometer. I am not going to talk about those because I feel like we know them like the back of our hand. They do not often show very minute growth in patient recovery. What I will talk about in much more depth is the Critical Frailty Scale, the Functional Status Score - ICU, and the ICU Mobility Scale because I think these have a lot of power in the critical care setting.
Critical Frailty Scale. This is an excellent tool used by OTs in the ICU. This clinical scale is mostly used to obtain a baseline assessment of frailty and measures a sum of eight core frailty indicators. These are weakness, fatigue, weight loss, low physical activity, balance, gait speed, and visual impairments. Also, there is a note of cognitive impairments. Please look at the questionnaire to have a stronger grasp of what I am talking about. The Clinical Frailty Scale is an excellent way to get a snapshot of how your patient was navigating life before being admitted. One very important detail about being a therapist in any setting is acknowledging and being realistic that a patient may have been frailty prior to their admission. They have higher mortality and morbidity rates and may require institutionalization at discharge. Therefore, getting all the background information can be very useful when assessing the prognosis of a patient in a therapeutic context and using a standardized approach for assessing physical function in the ICU is highly recommended. Additionally, using the Clinical Frailty Scale can help with writing appropriate goals for recovery and rehabilitation.
The Functional Status Score-ICU (FSS-ICU). The FSS-ICU is a physical function measure specifically designed for the ICU and includes five functional tasks: rolling, transferring from supine to sit, sitting at the edge of the bed, transfer from sitting to stand, and walking. Each task is evaluated on an eight-point ordinal scale very similar to the Functional Independence Measure (FIM), ranging from zero (not able to perform at all) and seven (completely independent). This scale has excellent responsiveness to small gains and is an excellent tool to predict the duration of post-ICU hospital length of stay. This measure has also been proven to have a strong predictive value to discharge location. For example, in the category of a survivor discharged to home, there were much higher FSS-ICU scores associated with those patients as opposed to those survivors discharged to subacute rehab. For patients with multiorgan failure and at high risk for hospital-acquired deconditioning, the FSS-ICU is an excellent instrument to use to demonstrate an increase in muscle strength and functional capacity. In my personal practice, I have also found the FSS-ICU to be helpful to help me triage my caseload and help me focus on the right patient at the right time based on who would benefit most from my intervention.
ICU Mobility Scale. The final outcome measure I would like to discuss that measures physical functioning is the ICU Mobility Scale. This instrument is a widely used scale that evaluates mobility sub-domains. It measures a patient's mobility status starting with their ability to follow commands culminating in the distance walked in two minutes. It is on a 10-point scale with zero representing a patient requiring total assist for rolling or passive range of motion exercises, a five representing a patient's ability to progress to stand or shuffle through standing to sitting in a chair (a bed-to-chair transfer), and finally, the score of 10 demonstrates the patient's ability to walk from either a bed or a chair at least five yards, without an assistive device. I love this measure because it is easy to communicate the results within an interdisciplinary team. It is also a great tool for peer-to-peer handoff, and it offers context to physical positioning during self-care. We all know washing your face supported in long sit in a bed is absolutely not the same as washing your face standing at the sink. Therefore, when you use the ICU mobility scale, you provide more depth to a patient's physical abilities during times of self-care.
I just unloaded a lot of information so I want to take a step back and focus again on the big picture. When we evaluate physical function, using the Clinical Frailty Scale helps you grossly understand the patient's premorbid status and allows for a much more realistic goal-writing. The FSS-ICU is an excellent measure to assist with prognosis. It has proven to have strong predictive values for discharge disposition, therefore an essential tool during the early stages of recovery. Finally, the ICU Mobility Scale is great because it provides context and objective information during self-care interventions. It can demonstrate progress in an objective way so that team members and insurance companies can see how your patient is actively making progress during your sessions. When you use instruments like the Clinical Frailty Scale, FSS-ICU, and ICU mobility scale, you gain such a great depth of knowledge about your patient's physical function. It is important to know where a patient came from (Clinical Frailty Scale), where they potentially could be going (FSS-ICU), and then track their progress during intervention so that you can provide a rich description to properly illustrate the story of a patient recovery (ICU Mobility Scale).
Cognitive & Psychosocial
Let's shift gears and chat about outcome measures that directly look at the cognitive and psychological components of recovery. Screening for mental capacity should start from day one of admission and include assessments such as pain, sedation, and delirium status.
- Basic:
- Richmond Agitation Sedation Scale (RASS)
- https://www.mdcalc.com/richmond-agitation-sedation-scale-rass
- Confusion Assessment Method (CAM –ICU)
- https://www.researchgate.net/figure/Confusion-assessment-method-for-the-ICU-CAM-ICU-Flow-sheet_fig1_303790119
- Montreal Cognitive Assessment (MoCA)
- https://www.parkinsons.va.gov/resources/MOCA-Test-English.pdf
- Richmond Agitation Sedation Scale (RASS)
www.improvelto.com/coms
Richmond Agitation Sedation Scale (RASS). This is a tool that ICU clinicians can use to determine the level of consciousness of a patient. The original purpose of the RAAS was to avoid under and oversedation. The use of the RAAS scale is recommended to ensure that the ICU team speaks the same language regarding the intensity of a patient's sedation. On the link provided, you will see a 10-point scale with four levels of anxiety or agitation and one denoting a common alert state. A patient who scores a four-plus describes a patient who was combative and potentially unsafe to engage in therapy, while a three-minus describes a patient who is moderately sedated. This means eye-opening to voice but really no eye contact. Verbal stimulation is mostly required at this stage, but sometimes physical touch is needed. The RAAS can lead occupational therapists to make informed decisions that not only maximize patient safety during therapy but also the best types of interventions to use. The RAAS provides all ICU team members with a standardized way of accurately documenting patient status pre, during, and post an OT intervention. This scale also opens up the door to some powerful clinical conversations during patient recovery. With increased use, we can speak and establish a culture where all clinicians are talking the same language. Earlier in this webinar, Lyndsay educated us on the significance of hospital-acquired deficits. We learned about the profound effect that post-intensive care syndrome has on patients who survive a critical illness. One thing that always sticks out to me is 60% of patients who survive the ICU admission all share one common risk factor, and that is delirium. Therefore, this webinar would not be complete without a quick discussion of the CAM-ICU.
The Confusion Assessment Method (CAM-ICU). This is the gold standard for delirium. Delirium is a common, serious, and potentially preventable source of morbidity and mortality. Delirium can affect as much as 50% of elderly hospitalized patients. The CAM was developed to improve the identification and recognition of delirium. It is intended to enable all clinicians to identify delirium quickly and accurately. Therefore, it is highly recommended for occupational therapists working in acute care to assess for delirium during every OT session. If we establish a daily routine, modify the environment, and engage patients in functional task practice, research indicates that we can have an impact on the overall incidence of delirium. If we target that elderly patient population, we can decrease mortality, decrease the length of stay, decrease costs, deescalate the rate of long-term cognitive impairment, and finally, increase a patient's ability to return back to independent living. I think it is so powerful. Please assess for delirium every patient every time. We cannot afford not to.
Montreal Cognitive Assessment (MoCA). Let's dive a little bit deeper into a patient's current level of cognitive abilities and talk about the MoCA assessment. This is a great option. It is a screening tool designed to detect mild cognitive dysfunction. This screening tool, however, can offer clinicians insight into the following five categories: executive function, memory, attention, language, and abstract thinking. The MoCA may be administered by anyone who understands and follows instructions. However, only a healthcare professional with expertise in the cognitive field may interpret the results. This screen allows clinicians to identify specific domain areas of impairment, and then follow up using functional evidence-based treatment interventions. Knowing exactly where a patient is struggling is essential so you can utilize the time you have in your session wisely. Training in how to administer the MoCA is offered in the link provided.
With the ability to assess several cognitive domains using the RAAS, CAM-ICU, and MoCA creates a much clearer picture of where your patient is in their recovery. You will be armed with that knowledge to implement specific evidence-based treatment interventions to allow your patient to have a better outcome. Now, while I still have your attention, let's talk about more advanced outcome measures for the cognitive and psychosocial areas of recovery. Strength should never be the sole guide for determining a patient's need for therapy. As occupational therapists, we need to understand this. This is using a holistic approach and looking at the whole person to help an ICU survivor recover.
- Advanced:
- Hospital Anxiety and Depression Scale (HADS)
- http://www.svri.org/sites/default/files/attachments/2016-01-13/HADS.pdf
- JFK Coma Recovery Scale (CRS)
- http://www.tbims.org/combi/crs/CRS form.pdf
- Glasgow Outcome Scale- Extended (GOS-E)
- https://www.researchgate.net/figure/Glasgow-outcome-scale-GOS-and-Glasgow-outcome-scale-extended-GOSE_tbl2_272176279
- Hospital Anxiety and Depression Scale (HADS)
When an individual has their independence taken away from them and is admitted to a critical care unit, their prognosis may have many ambiguities and can cause a lot of emotional distress.
Hospital Anxiety and Depression Scale (HADS). This is a self-reported questionnaire (14 questions) designed to identify depression and anxiety. You will see items are rated on a four-point severity scale, one scale is for anxiety and the others for depression. A score equal to or greater to 11 is indicative of a positive sign. However, the true beauty of this scale is its simplicity, speed, and ease of use. This has a role in everyday ICU practice and all patients with mild to severe symptoms of anxiety or depression should absolutely be further psychologically evaluated by a professional in that field. By using this scale, we have a better grasp of what our patients are experiencing and now have the ability to advocate for these individuals with much more robust, objective information. This information also allows us to use our empathetic use of self to foster better relationships and rapport with our patients we are helping to recover.
JFK Coma Recovery Scale (CRS). I feel compelled to also talk about the JFK Coma Recovery Scale in today's webinar because of the unique role OTs can have on its administration. This scale is used to assess patients within a disorder of consciousness. The subscales include auditory response, visual motor, oral motor, communication, and levels of arousal. The lowest scale of each subscale represents reflexive activity. The highest level represents behaviors that are mediated by cognitive input. Patients who have sustained traumatic brain injuries, strokes, or brain tumors are appropriate for this assessment. When I work in the Neuro ICU, I love using this scale. It not only guides me by tapping into a patient's abilities at the earliest stages of recovery, but it also can be used to monitor the emergence of a minimally comatose state. For example, if your patient has a high score under the auditory section, modifying his or her environment by allowing the patient to listen to low tempo music may help activate areas of the brain involved with memory, cognitive function, and emotion. Listening to music is an excellent preparatory method to engage patients and increase their level of arousal. In 2006, Doctor Khan did a research study using music-listening for ICU patients. He concluded that music was a feasible way to reduce brain dysfunction and increase activity in areas of memory, potentially helping regain cognitive function. This might be something you would never know if you did not use the JFK Coma Recovery Scale. The JFK Coma Recovery Scale is so powerful for our neurological patients in the ICU. It offers us a pathway that we as occupational therapists can travel to administer evidence-based interventions. Even patients who have a current disorder of consciousness, we can help them to recover.
Evidence-Based OT Interventions
Lyndsay: Similar to the beginning part of the presentation, we are going to break up the interventions into the four domains that are impacted by critical care.
Neuromuscular
- Early Mobility & Engagement
- Increase muscle strength
- Reduce the incidence of ICU-acquired weakness
- Increase incidence of independent functional status at hospital discharge
(Schweickert et al., 2009)
We know that early mobility and early engagement help increase muscle strength. They reduce the incidence of that ICU-acquired weakness that we were talking about, as well as, increase the incidence of independent function at the time of hospital discharge. When it comes to these different interventions, our unique value as rehabilitation clinicians, specifically occupational therapy practitioners, is our clinical judgment to grade the activity. We know that we cannot have one intervention that is going to be appropriate for all of our patients. We really need to come in, utilize some of those outcome measures that Meghan was talking about, do some of our informal screens and functional assessments, and decide what intervention meets the needs of that specific patient.
We want it also to be client-centered and meaningful. To do so, we need to grade the activity. If you have a patient that has a profound weakness and is not really able to tolerate a whole lot of out of bed activities, whether from a physical perspective, a hemodynamic issue, from an agitation issue related to their diagnosis, or a medical situation, we have a couple of options to help them engage in mobility and activity. This all depends on your specific site. Here at our hospital, we have access to a tilt table that allows for progressive upright positioning. You can then incorporate some sort of meaningful task. We also have access to a cycle ergometer for seated or supine cycling. For some of our moderate to higher-level patients, something as simple as transferring to a commode for normal bowel-bladder management can be a profound benefit to that patient's functional progress. For higher-level patients, if they are able to tolerate ambulation or static/dynamic standing for a prolonged period of time, they can go into the bathroom or to a shower nearby for ADLs. You can use your clinical judgment to grade activities to what is appropriate.
Physical Function
- Early Rehabilitation
- ADL re-training
- Functional transfer training
- Sleep hygiene
- Communication
(Campbell, 2014)
Physical function is our bread and butter. We want patients to engage in meaningful activity as early and as often as possible. Early rehabilitation for us can be ADL retraining and establishing a routine. Nothing is more off-putting to a routine than an admission to a hospital, especially an admission to a critical care unit. Patients lose all sense of control, normal routines, and oftentimes, their natural circadian rhythms for sleep-wake cycles. OTs can have a profound impact as we look at that person-environment-occupation interaction. We need to create some sort of normalcy for patients.
Functional transfer training is where we can partner with physical therapists as well as nursing. We know that an intervention completed once a day is not as powerful as an intervention done multiple times a day. One of our roles is to empower not only the patient but also our colleagues and ancillary staff to help carry over plans of care that we have established.
Sleep hygiene is another area where we can partner with our nursing colleagues for improvement with sleep-wake cycles. This can be by creating some sort of routine, establishing breaks throughout the day for rest or lower stimulation, as well as, frequent engagement so that patients are not sleeping due to boredom or inactivity.
Communication is a great area for us to collaborate with our speech-language pathology colleagues. This can be via adaptive communication whether it is writing or using iPads which is what we use here at our hospital. We need to help our clients to communicate. This, in turn, will help in other domains for decreasing anxiety, depression, and also increasing a patient's ability to participate in their own medical plans of care. What is more powerful than being able to communicate what you want to be done to your own body?
Psychological
- Delirium prevention & management
- Detection
- Management
- Environmental Modifications
- ADL engagement
- Sensory regulation (visual, auditory, etc).
- ICU Diary
- Reduction in anxiety and depression
- Adaptive Communication
- Leisure engagement
(Parker, A., Sricharoenchai, T. & Needham, 2013; Clancy et al., 2015)
Unfortunately, delirium is extremely prevalent within critical care. It also carries with it some pretty profound deficits that persist for patients long after they are discharged from the hospital. As Meghan mentioned, the detection of delirium is key. Routine administering of the CAM-ICU needs to be done every session so that we can detect delirium early and start different management strategies to help decrease the severity and the length of the delirium. In order to manage delirium, environmental modification is one strategy. If the environment is understimulating, we can open the blinds, turn on the lights, and increase the patient's head of the bed so they are able to participate in daily activities. We can always provide the patient with their hearing aids, glasses, and dentures to try to regulate the sensory input. Conversely, if the environment is overstimulating and somebody is presenting with hyperactive delirium, we can inject soothing sounds, turn the lights off, and give patients rest breaks to try to decrease their agitation, which can be extremely psychologically detrimental for a patient.
Another option is the ICU diary. This is one that I have used for several years in my own clinical practice and absolutely love. When somebody comes into the ICU and they have lost control, they have a huge change in function. They are not able to engage in normal daily activity, leisure activity, work, normal family relationships, and those premorbid roles and routines. These are paused or gone for the foreseeable future. Being able to utilize the ICU diary to report emotions and feelings can be very helpful in reducing anxiety and depression. I also really like to use it from a cognitive perspective which I will talk about next.
Again, communication comes in here. We know if patients are not able to adequately communicate, they can have higher rates of anxiety within their hospital stay. This is another area that should be addressed as soon as possible. For example, someone with profound weakness might not be able to hit a standard call light to alert the nurse if they need something. We can come up with adaptive communication strategies. Adaptive call lights can play a huge part in our interventions to provide a little bit of control and independence and safety for that patient.
Lastly, leisure engagement is great, specifically, if patients have family and friends that frequently visit. We can create a routine for leisure engagement. These are things they enjoyed engaging in prior to hospitalization. It can increase their overall feelings of happiness and decrease some of the anxiety and depression.
Cognitive
- Delirium prevention & management
- Early cognitive engagement
- ICU Diary
- Puzzles
- Word search, crossword puzzle, maze
- Re-orientation activities
(Clancy et al., 2015; Alvarez et al., 2017)
Again, delirium prevention and management are important. The longer the delirium persists the more severe cognitive deficits persist post-hospitalization. It is crucial to use early cognitive engagement like the ICU diary. I like to use it in conjunction with the orientation log. The orientation log assesses 10 areas of a patient's orientation from location, date, time of day, the reason for admission, and current functional deficits. This gives us a good insight into where a patient might be disoriented. We can also use the ICU diary to have the patient create a written log of what has happened each day. This can then be used as a compensatory strategy for short-term memory, recall, and orientation.
In our hospital, we offer various puzzle books. I also will print off word searches, crossword puzzles, mazes, and anything that requires sustained attention to help the patient engage in something that might take their mind off of what's going on around them. Re-orientation activities are great as well. This can be something as simple as putting a clock or a calendar at their bedside or having a family member come by and have a conversation about what happened at church that day. You can get pretty creative with some different strategies.
- Remain holistic
- Interventions should not be utilized in isolation
- Emphasis on “occupation”
The takeaway is to remain holistic. We want to know how those four domains affect the patient (see Figure 3).
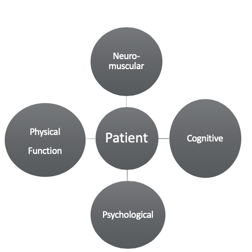
Figure 3. Four domains affecting the patient.
The environment affects the patient and their progress. We really do not want to choose one intervention and use that in isolation. Early mobility, engagement in ADLs, engagement in out-of-bed activities are all important. I think the power of OT is that we are holistic and client-centered, and that is what research is beginning to show. Early mobility is not the key to good outcomes, but it is an early engagement in life. We want to make that person as independent and fulfilled as possible. Just because a person can walk 100 feet does not mean you can take care of yourself, balance your checkbook, or take care of your child at home. We want to treat the person as a whole person and not just one of the four domains.
Advocacy
- The Role of OT is evolving !!
- Emerging evidence suggests the input from an Occupational Therapist can result in:
- Reduced Delirium
- Reduced Hospital Length of Stay
- Return to work at an earlier stage for both patients and caregivers due to reduced dependence
- Reduce patient morbidity as a result of earlier rehabilitation
- Emerging evidence suggests the input from an Occupational Therapist can result in:
(Brummel et al., 2014; NICE, 2009b; Alvarez et al., 2017)
Meghan: I think we all know now the role of occupational therapy is clearly involved in critical care units. In recent years, the value of occupational therapy has been recognized. Again, educating all interdisciplinary team members on how we can assist with ICU survivors' recovery is imperative. Lyndsay really just hit it home. It is not about how far you can walk or how you can move, but rather it is about how you engage in your life and how you sustain a quality of life that is important to you. Showing the impact that occupational therapists have in ICU recovery is absolutely major. Let's be the ones to positively influence the culture of our critical care recovery units. I hope after today you move forward with the knowledge that we can make a difference.
Questions and Answers
Can these assessment scales be used in skilled nursing facilities with low-level clients?
Excellent question. I would like to say at this time that our area of expertise is ICU. I do know the JFK Coma Recovery Scale is feasible to use in many different settings, but if you really want to dive a little deeper, I would use the links and do your own kind of self-study for that.
Are other OT clinicians being trained or given only expectations to focus on mobility?
I can only speak about our facility, and I would say no. We have autonomy as clinicians to do what we know is best from an evidence-based perspective based on our clinical judgment. We are definitely very engaged with mobility but also take it a step further for overall engagement with ADLs, leisure, et cetera.
Do you both have a further in-depth course regarding these topics?
Thank you so much for that. We actually did for occupationaltherapy.com last year, do a presentation on ICU delirium, which I know is available through the catalog (Occupational Therapy's Role in Delirium Assessment, Prevention, & Management within the Intensive Care Unit, course #4013). I would take a look at that.
If a patient or family member asked you to explain what an OT is, what do you tell them?
I find this to often be a difficult question to answer simply. I usually say, "My role is to help your family member engage in life to the best of their ability and engage in what they want to engage in." I am very straightforward, and I will not make them brush their teeth every day if that is not something that they are passionate about.
Do you have any suggestions for any free assessments that are used in the ICU?
I would say the majority of them are free. There are only maybe one or two you actually have to pay for. We tried to make this not only a feasible educational experience but something you can implement tomorrow. The other thing that I found when I was learning about these is YouTube has really cool links to how to administer them. If you do not feel comfortable asking a team member, you can always use the Internet as your guide
How many assessments do you typically complete on evaluation?
You really need to think about the capacity of the patient so I would not say that there is a blanket answer. With that being said, I would definitely do the CAM-ICU and the RAAS with every patient, every time.
The JFK Coma Recovery Scale is mainly used for traumatic brain injuries. Can it be used for others?
Great question. It is only valid for traumatic brain injuries, strokes, and brain tumor patients.
How many patients do the OT staff see in an eight-hour day? It seems like these tests would take time to administer and interpret.
I think this is a great point to bring up because it does seem overwhelming. When you get comfortable with all of the assessments, they are very quick to administer with the exception of the JFK Coma Recovery Scale. You just need to feel comfortable with them. In the neurological ICU, a 24-bed unit, I see anywhere from eight to 12 patients on my caseload and realistically treating six to seven.
Do you have any examples of leisure activities that you have used in an acute care setting?
Medication management is an IADL that I typically do, I also think that handwriting is important to do for check preparation. Sewing and crocheting tend to be very popular with the elderly population. Counting is also very nice to sustain attention. People love to color, and they have adult coloring books for that.
How can we improve OT referrals to ICU patients?
This is a huge one and one that I feel very passionate about. Physicians do not necessarily understand what OTs can offer. I have scheduled in-services with different providers to educate them on our role. I have also posted a handout. "Does this person have delirium? Are they at risk of delirium? Are they having decreased independence with ADLs? If yes, please consult the OT." I operate under the belief that we should be over consulted rather than under consulted. We can then utilize our expertise to decide who we see and the timing to intervention. I also find a lot of times physicians will wait until the patient is no longer sedated or no longer intubated to get OT involved. I want to be involved day one and then I can monitor their medical properties to see if and when they are appropriate for therapy.
References
Algeo, N., & Aitken, L. M. (2019). The evolving role of occupational therapists in adult critical care in England. Irish Journal of Occupational Therapy.
Alvarez, E.A., Garrido, M.A., Tobar, E.A., Prieto, S.A., Vergara, S.O., Briceno, C.D., & Gonzalez, F.J. (2017). Occupational therapy for delirium management in elderly patients without mechanical ventilation in an intensive care unit: A pilot randomized clinical trial. Journal of Critical Care, 37.
Campbell, C. (2014). The role of occupational therapy in an early mobility program in the intensive care unit. Special Interest Section Quarterly: Physical Disabilities, 37(1).
Clancy, O., Edington, T., Casarin, A., & Vizcaychipi, M.P. (2015). The psychological and neurocognitive consequences of critical illness. A pragmatic review of current evidence. Journal of the Intensive Care Society, 16(3), 226-233.
Costigan, F.A., Duffet, M., Harris, J.E., Baptiste, S., & Kho, M.F. (2019). Occupational therapy in the ICU: A scoping review of 221 documents. Critical Care Medicine, 47(12), 1014-1021.
Desai, S.V., Law, T.J., Needham, D.M. (2011). Long-term complications of critical care. Critical Care Medicine, 39(2). doi: 10.1097/CCM.0b013e3181fd66e5
Karnatovskaia, L.V., Johnson, M.M., Benzo, R.P., & Gajic, O. (2015). The spectrum of psychocognitive morbidity in the critically ill: A review of the literature and call for improvement. Journal of Critical Care, 30, 130-137.
Parker, A., Sricharoenchai, T. & Needham, D.M. (2013). Early rehabilitation in the intensive care unit: Preventing physical and mental health impairments. Current Physical Medicine and Rehabilitation Reports, 1(4), 307-314.
Parry, S. M., Huang, M., & Needham, D. M. (2017). Evaluating physical functioning in critical care: considerations for clinical practice and research. Critical Care, 21(1), 249.
Pohlman, M. C., Schweickert, W. D., Pohlman, A. S., Nigos, C., Pawlik, A. J., Esbrook, C. L., ... & Schmidt, G. A. (2010). Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Critical care medicine, 38(11), 2089-2094.
Schweickert, W.D., Pohlman, M.C., Pohlman, A.S., Nigos, C., Pawlik, A.J., Esbrook, C.L. … & Kress, J.P. (2009). Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomized controlled trial. Lancet, 373, 1874-1882.
Van der Ploeg, R. J., Fidler, V., & Oosterhuis, H. J. (1991). Hand-held myometry: reference values. Journal of Neurology, Neurosurgery & Psychiatry, 54(3), 244-247.
Wilcox, M.E., Brummel, N.E., Archer, K., Ely, E.W., Jackson, J.C., & Hopkins, R.O. (2013). Cognitive dysfunction in ICU patients: Risk factors, predictors, and rehabilitation interventions. Critical Care Medicine, 41, S81-S98.
Citation
Laxton, L. & Morrow, M. (2020). Acute care back to the basics: OT's role in critical care. OccupationalTherapy.com, Article 5155. Retrieved from http://OccupationalTherapy.com

