Pam: Thanks for joining me today. I am really excited to be talking to you on a topic that is near and dear to my heart. One of the things I want to highlight and focus on today is intervention. In many continuing eduation classes, we discuss best practice strategies and assessment, but there is often still the question of what is the best intervention according to the evidence. Hopefully, you have had the opportunity to participate in all of the lectures that have gone on this week as part of this virtual aging conference.
Aging in Place
The conference has focused on this theme of aging in place, and with each one of our presentations, we have emphasized that aging in place is the ability for a person to live in their own home and community, independently, safely, and comfortably, regardless of age, income, or ability level (CDC, 2013). This is the goal of most people in today's society. Occupational therapists, with our skills, talents, and distinct approach to looking at the person, as well as the environment and occupation, have a skillset that no other profession has to effectively help our clients achieve this goal. Again, we are going to focus on intervention, but we have to get through the first steps.
First Steps
I would like to re-emphasize, from our earlier talks this week, this idea that the best practice strategy for starting this process is to start with your client. Finding out what your client wants to do, what they need to be able to do, and what they are expected to do to age in place. This may seem obvious, but it is very individualized based on the person.
There are a variety of methods that we and other professionals use to identify what people want to do, need to do, and expect to do. In my own clinical experience, I find that occupational therapy practitioners rely heavily on self-report. Believe it or not, self-report is actually a pretty reliable tool to use with clients who are cognitively intact or for people who have a higher level of functioning. There is evidence, however, that a combination self-report and performance-based measures are more likely to identify some hidden barriers or some opportunities to strengthen a person's ability to be successful in their own home. One of the best practice strategies is to follow up a self-report measure with performance assessment.
Performance assessment is something that we do best and not duplicated by many other professionals. We can add insight to an inter-professional approach that can provide a brighter picture in terms of the client's strengths and opportunities. In addition to thinking about combining a self-report and performance approach, the other thing that we have to think is if we are going to use a non-standardized or a standardized approach. Unless you are driven by your reimbursement or by your place of work to use a particular assessment, you can decide what type of tools that you use to gather information. From an evidence-based perspective, the ones that have the strongest evidence and use a standardized approach are the Canadian Occupational Performance Measure (COPM), the Activity Card Sort (ACS), the Performance Assessment of Self-care Skills (Pass), and the In-Home Occupational Performance Assessment (I-HOPE). We are not going to be focusing on all of these tools today, but I want to highlight that these are tools that are effective for helping us to identify strategies for aging in place.
Intervention
Once we have completed our assessment, we now have the choice of deciding how we intervene. As occupational therapy practitioners, we are pretty lucky. We have a variety of intervention approaches that we can consider to help our clients age in place. I am using the AOTA Occupational Therapy Practice Framework (OTPF III) as a guideline fo the language and the descriptions. The reason for this is that if you want to look at this material further you can refer back to this reference to help you in understand these different approaches. The four intervention approaches that I would like to focus on today are:
•Promote health
Restore
When we think about remediation or restoration,we are trying to change the client or the person. We are helping them to regain a skill or an ability that has become impaired. The client could have reduced range of motion, endurance, balance, weakness, or attention. We are trying to engage the client in a restorative intervention to help them get back to where they were before the incident or the event. When occupational therapy practitioners use restoration as an intervention, our activity may be impairment-focused or occupation focused. Most studies suggest that occupational therapists heavily rely on restoration as an intervention approach. What is more variable is whether we focus on the impairment or we focus on the occupation as seen in Figure 1.
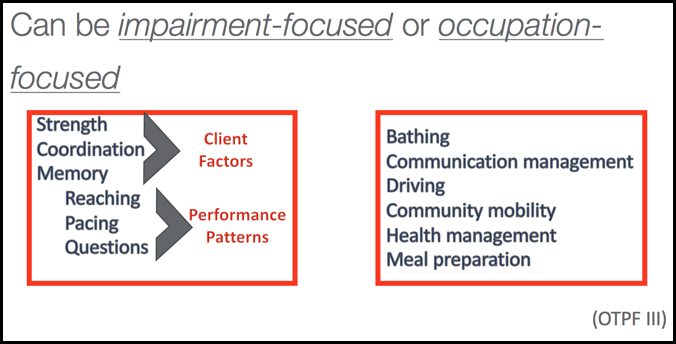
Figure 1. Impairment versus occupation focus.
If we are focusing on the impairment, we may be focusing on client factors such as strength, coordination, or memory, or we could be looking at performance patterns such as reaching, pacing, or asking questions. That is one strategy, but we could also be focusing on restoration by using occupation as an intervention in addition to the outcome. An occupation-based focus might be using bathing. During bathing, I provide the "just right" support, cuing, and modifications to help that client to get stronger for bathing within the context of bathing. Another example is I may be working with my client on communication management. Perhaps, they are having difficulty with memory and remembering what phone number they need to dial for an emergency. We practice that to reduce the impairment with the occupation for the occupation. Some other examples of occupation-based focuses might be driving, community mobility, health management, or meal preparation. All of these are common ADL's or IADL's that occupational therapy practitioners can work on that are occupation focused with the intent of helping the client to be able to regain the skill that they lost.
Now does the literature tell us about restoration? There is strong evidence that under the right circumstances, and I emphasize the right circumstances, that older adults can reduce some of their impairments. What we know though, however, is that older adults with chronic conditions may have less potential to reduce impairments. For example, if your client has pain related to severe or advanced arthritis and they are not going to have a joint replacement, doing exercise may or may not improve or reduce that impairment. In order to reduce impairment in older adults, it requires motivation and sufficient time and intensity. For any of you who exercise regularly, you know that going to the gym three times a week for two weeks probably is not going to make a significant impact. This is the same with our clients. While restoration is a really good approach for a certain group of people, the literature tells us that it has to be sustained over a long period of time. Someone who is exercising or being physically active needs to do it all the time or every day. And, to reduce the impairment, it may take six weeks to three months to make a difference. If you are only going to see someone for four visits, is it realistic to think that spending your time exercising with that person and not focusing on the occupation is going to result in a favorable outcome? You are not going to get them sufficiently stronger or significantly reduce the impairment in a very short amount of time. I am not saying restoration is bad, but we have to think about it from an evidence perspective of what is the biggest bang for the buck. How are we going to most effectively help someone age in place if we only have a brief interlude with that client?
Case Example: Restore
Last winter, Mrs. R., who is 85, acquired a bad cold that turned into pneumonia. She was hospitalized for four days and then was sent home with home health services. At baseline, Mrs. R. demonstrated decreased strength and required minimum assistance with self-care. Five weeks later, and after occupational therapy three days per week plus a home program, Mrs. R. regained her strength and endurance to become independent with self-care like she was before she got pneumonia. This case is a good example that Mrs. R.'s weakness was related to disuse because of her illness, hospitalization, and bed rest while she was sick. Mrs. R. does not have a chronic condition that caused the weakness but rather an acute condition that resolved itself. In this case, five weeks was sufficient time as her baseline was not max assist. Her baseline was minimum assistance, and in five weeks working on her occupations and having a home program that included some strengthening and endurance activities, she was able to regain her ability to complete her IADL's and ADL's the way that she did them before.
Modify
The second approach I would like to talk about is the idea of modifying. I think that this is where we have our greatest strength as occupational therapy practitioners. I think we do this better than anyone else, and it really provides us with the greatest opportunity to help people to age in place. Modifying includes changing the environment and or the activity demands to enable performance of a desired occupation. By the nature of what modify means, it automatically forces us to be occupation-based. We can change the environment like moving a bed to the first floor to eliminate the need to use stairs. Or, we can change activity demands. We can make activity easier or add a piece of adaptive equipment such as a reacher or a sock aide. Modify includes compensation and adaptation, and again, by nature, it is occupation based.
Based on evidence and our clinical skill, we select the approach to modify in a few different scenarios. We may choose to use it when the impairment is considered permanent or not expected to improve like when someone has a chronic condition. The other time we might choose modification is when there is limited access and/or time for the restorative approach. There is strong evidence that this approach, when used with older adults, can reduce ADL and IADL disability. We are targeting the thing that is causing them limitation. If someone has difficulty with bathing, we address bathing through a modified approach to reduce the disability directly. This approach may still some require time and resources to implement changes depending on the strategy or need for new learning. For instance, if I am giving a client a sock aide, I need to be sure that they have the capacity to learn how to do something new and have adequate time to practice.
Are the terms compensation and adaptation interchangeable? Do they mean the same thing or are they distinct terms? The Occupational Therapy Practice Framework does not delineate one versus the other, and they are interchangeable in most OT literature, including the addition to the OTPF and the most recent edition of Willard and Spackman. The good news is you can approach your client either way. You can use them as distinct approaches or you can use them interchangeably. In certain practice settings or with certain populations, you may find that these terms are used as two distinct terms. I previously worked with a long-term care population with cognitive impairment. In this environment, compensation and adaptation were used as two distinct terms. Compensation is where we are doing something that the client still has to use new learning; whereas, adaptation is the idea of an environmental change without new learning. For example, compensation might be that sock aide that my client has to learn. Adaptation might be that I teach a caregiver, who is feeding their loved one with end-stage Alzheimer's disease, that if they feed them on the left side, as opposed to the right, the person can swallow more easily. In the second example, I am not changing the client but the environment. For the record, there is no delineation anywhere that compensation and adaptation are distinct, but you may see this in your own practice setting or you may use it to be able to guide your clinical reasoning if you are working with clients that have very diverse abilities.
Case Example: Modify
Mr. B. is 71 years old, and he has chain-smoked for 45 years. He now has severe chronic obstructive pulmonary disease, or COPD, and is on oxygen. However, even with oxygen, his shortness of breath limits his ability to prepare his own meals and complete his laundry which is in the basement. The occupational therapy practitioner suggests that Mr. B. uses a stool while he is preparing his meals at the kitchen counter and washing dishes in the sink. This would be a compensatory strategy. Mr. B. might take a little bit longer at first because he is used to doing everything standing, but he can now do it without shortness of breath. We are teaching Mr. B. to use this different strategy to reduce effort for the task. For laundry, the occupational therapy practitioner could suggest using a laundry bag, which would be a compensatory strategy to reduce effort transporting items up and down the stairs. I worked with a client who used a laundry bag as a backpack. It educed their effort, and they were able to use the handrails. Mr. B. could also consider purchasing an apartment size washer and dryer for the main floor of his home. If you are using compensatory and adaptation as distinct approaches, as I mentioned on the previous slide, the washer and dryer moved to the main floor would be an adaptation because we are not doing anything to Mr. B. We are just changing where he needs to go to access the washer and the dryer.
My guess is that probably all of you use these approaches on a regular basis, but you may not think about them. I think we need to start thinking about them because then we can advocate for what we are doing that is skilled and distinct when we explain this to others and document our services. The third approach I would like to talk about is this idea of prevention.
Prevent
Prevention is when we educate older adults on strategies to reduce the likelihood of difficulty in ADL or IADL. When we think about preventative approaches, often they include both restorative and modification features. An example of a prevention strategy would be to remove clutter and increase lighting in the home to reduce falls risk in someone who has impaired balance or vision, but who has not had a fall yet. We know that this approach is based on the evidence. This approach is very warranted and successful with older adults who are at high-risk for decline. This is sometimes what we call secondary prevention. We take someone who is high-risk, and we intervene before the client has that acute event. We do not seem to do this as much in occupational therapy as other disciplines. If someone has an ambulation problem or they trip, they are referred for physical therapy to get stronger or learn how to use a cane. Does occupational therapy get a referral because someone forgot to turn off their stove? We should. This would be a good example of a secondary prevention.
