Editor's note: This text-based course is a transcript of the webinar, The Bariatric Client And The OT Role, Part 1, presented by Jennifer Phillips
OTD, OTR.
Learning Outcomes
- After this course, participants will be able to identify the various comorbidities of obesity and how they relate to occupational therapy.
- After this course, participants will be able to recognize obesity-related stigma and sensitivity programs.
- After this course, participants will be able to list at least 2 ways obesity impacts an individual.
Introduction
Thank you for the warm welcome. What we cover today represents part one of our discussion. Please also check out part two, as I delve deeper into the intricacies of the topic. During our discussion, I encourage you to consider at least two ways obesity can significantly impact an individual.
General Statistics
- In the United States, 41.9 percent of adults have obesity and 20 percent of children ranging from 2-19 have obesity (Trust for America's Health, 2023).
- Obesity has become common among adults, but in the United States particularly, the incidence of obesity in children exceeds that of other chronic conditions (Pediatrics, 2018).
Delving into general statistics, it is noteworthy that in the United States, 41.9% of adults grapple with obesity, while 20% of children aged two to 19 find themselves in a similar predicament. Reflecting on the initiation of my research journey in 2015, it is evident that the predominant focus was on adult obesity. However, over the ensuing years, a perceptible shift has occurred, with an increasing emphasis on the issue of childhood obesity.
The prevalence of obesity among adults has reached a concerning level, yet the United States witnesses a particularly distressing scenario where the incidence of obesity in children surpasses that of other chronic conditions. This statistic serves as a poignant revelation, underscoring the severity of the issue within the pediatric population. Consequently, my research trajectory underwent a transformation, evolving from an initial focus on adults to a broader and more nuanced exploration that encompasses the challenges faced by children grappling with obesity.
- According to the CDC in America, from 1999-2000 to 2017-2018 obesity increased from 30.5% to 42.4% (Centers for Disease Control and Prevention, 2020)
- Not only have rates of obesity increased at alarming rates, but severe obesity in America has risen from 4.7% to 9.2% (Centers for Disease Control and Prevention, 2020)
Drawing on data from the Centers for Disease Control and Prevention (CDC) in the United States, a concerning trend emerges. From the period spanning 1999-2000 to 2017-2018, the prevalence of obesity has surged significantly, catapulting from 30.5% to a staggering 42.4%. This substantial increase underscores the pressing nature of the issue over the past two decades. It is worth noting that similar concerns are echoed globally, with the United Kingdom, for instance, reporting higher obesity rates compared to the United States.
Notably, the escalation in obesity rates is not confined to a general increase but extends to severe obesity as well. In America, the incidence of severe obesity, defined by a Body Mass Index (BMI) of 40 or higher, has witnessed a notable rise from 4.7% to 9.2%. This troubling surge in severe obesity prompts a deeper examination of its implications, a topic we will delve into further during the latter part of this webinar.
Statistics
- Obesity has been established to be recognized as an increased fatality rate for COVID-19, especially in countries such as the United Kingdom, where 50% of adults have obesity.
- Individuals with obesity are at increased risk of COVID-19 infection and complications even with vaccination, as some studies have provided information that vaccination is less effective for people with obesity due to inflammation and metabolic imbalances (Fu, Lin, Zhu, & Ye, 2023).
The global impact of the COVID-19 pandemic has been particularly pronounced for individuals grappling with obesity, with heightened fatality rates documented, notably in countries such as the UK, where 50% of adults contend with this health challenge. The pandemic served as a stark wake-up call, especially within the healthcare sector, prompting a reassessment of vulnerabilities and necessitating innovative approaches to care.
Throughout the pandemic, clients with obesity faced distinct challenges, notably in the context of positioning. The frequent use of the prone position, a crucial element in patient care during that time, posed a significant obstacle for individuals with obesity, as they often encountered difficulties being positioned in this manner. This added layer of complexity underscored the intricate nature of care for this demographic.
Beyond the increased susceptibility to COVID-19 infection and complications, the advent of vaccinations, while a welcome development, revealed further disparities. Studies have indicated that the effectiveness of vaccination for individuals with obesity may be somewhat compromised due to underlying inflammation and metabolic imbalances. Thus, from the onset of the pandemic, where clients with obesity faced positioning challenges, to the current vaccination phase, this population continues to grapple with distinct disadvantages in their healthcare journey.
OT and Obesity
- It is due to this recent growth of obesity within the United States that it is becoming necessary to address the difficulties that occupational therapy practitioners encounter in clinical practice.
The burgeoning prevalence of obesity in the United States has underscored the imperative to confront the challenges faced by occupational therapy practitioners in clinical practice. My initial foray into research in 2015 revealed a notable dearth of literature connecting occupational therapy with the discourse on obesity. At that time, much of the available research predominantly centered on nursing and its intersection with obesity. This discrepancy posed a challenge in discerning the specific contributions and considerations within occupational therapy.
However, there has been a discernible shift over the past few years. A growing body of literature now addresses the role of occupational therapy in the context of obesity, signifying an expanding awareness of the profession's significant potential in aiding individuals dealing with this health challenge. As we delve into this discussion, it is clear that occupational therapy has a meaningful role in supporting and assisting those affected by obesity, and the evolving landscape of research reflects an increasing recognition of this crucial intersection.
Definitions
- Being overweight is defined as having a body mass index (BMI) of 25 or higher (World Health Organization, 2021)
- Obesity- having a body mass index (BMI) of 30 or higher (Mata, Mikkola, Loveland, & Hallowell, 2015)
- Childhood obesity- having a BMI-for-age of 95% percentile or greater and being overweight at 85%- 95% percentile (Centers for Disease Control and Prevention, 2021)
Before delving further into our discussion, let's review some pertinent definitions. Being overweight is characterized by a body mass index (BMI) of 25 or higher. On the other hand, obesity is identified when an individual has a body mass index of 30 or higher. In the context of childhood obesity, it is defined by a BMI for age at or above the 95th percentile, while being overweight falls within the 85th to 95th percentile.
It's important to note the distinction between being overweight and having obesity according to BMI definitions. One can be classified as overweight without meeting the criteria for obesity. This differentiation sets the stage for exploring the nuances between these classifications and their respective implications as we continue our discussion.
- Extreme obesity- having a BMI of 40 or higher (Mata, Mikkola, Loveland, & Hallowell, 2015)
- Mega obesity- having a BMI of 70 or more (Bennet, 2008)
- Bariatric- services are provided in prevention, treatment, and research to individuals with obesity (Forhan, 2008)
Expanding our understanding of obesity-related classifications, it's essential to consider additional definitions. Extreme obesity is identified when an individual's BMI reaches 40 or higher, indicating a severe level of adiposity. Mega obesity takes this a step further, denoting a BMI of 70 or more, signifying an even more pronounced and challenging health condition.
Complementary to these classifications, the term "bariatrics" encompasses a range of services dedicated to the prevention, treatment, and research associated with individuals dealing with obesity.
Predicted BMI and Health Care Related Costs
- There is a direct link between healthcare costs associated with obesity and bariatric care.
- Since 2012, there has been a dramatic increase in healthcare costs related to obesity.
- In 2012, BMI-related healthcare costs were around 55 million.
- With no reduction in obesity, it is predicted to be close to 63 million.
- Even with a 5% reduction in obesity, by 2027, the cost of healthcare-related services is predicted to be 59 Million (Phit America, 2017).
Addressing the healthcare landscape associated with obesity and bariatric care introduces a significant financial dimension. The specialized requirements, including bariatric beds, lifts, and additional staffing, contribute to elevated costs in comparison to conventional healthcare services. The necessity for more than one staff member and extended time investments further underscore the economic implications associated with the care of individuals grappling with obesity.
Examining the trajectory of healthcare costs related to obesity since 2012 reveals a substantial escalation. Back in 2012, BMI-related healthcare costs were estimated at approximately 55 million. However, without a reduction in obesity rates, projections indicate an alarming surge, nearing 63 million. Even with a modest 5% reduction in obesity—an optimistic scenario given current trends—the anticipated cost by 2027 is projected to be around 59 million.
These figures signal an urgent need for proactive measures within the healthcare community to grapple with the impending financial challenges associated with obesity-related care. This includes not only strategic planning for increased costs but also ensuring access to essential equipment to guarantee the safety of both clients and healthcare professionals engaged in the care of individuals with obesity.
Socioeconomic Status (SES)
- Low SES status can be correlated with obesity. For instance, access to health care, health food options, and safe access to exercise options such as parks or gyms makes it difficult for an individual with obesity to attain a healthy lifestyle. (Forhan, Obesity and Health Occupation, 2008)
- Homebound clients with obesity have difficulties with finding work, and maintaining the productivity standards, referred to as presenteeism making it challenging for those with obesity to maintain a meaningful profession (Reingold, & Jordan, 2013).
The intersection of socioeconomic status (SES) and obesity introduces a complex dynamic, with notable correlations between low SES and the prevalence of obesity. The challenges faced by individuals with obesity in attaining a healthy lifestyle are magnified in low SES areas, where barriers to access healthcare, nutritious food options, and safe exercise spaces are more pronounced.
There are "food deserts" in these regions, highlighting the lack of access to healthy food, the prevalence of fast-food options, and a dearth of parks or gyms. The implications are far-reaching, as individuals in low SES areas may find it challenging to adopt healthier dietary and exercise practices.
Furthermore, the demands of long working hours in such environments may hinder individuals from engaging in physical activities or preparing nutritious meals. Time constraints often lead to opting for quick, albeit less healthy, food choices. This confluence of factors underscores the intricate relationship between socioeconomic circumstances and the ability to maintain a healthy lifestyle.
Home-bound clients with obesity encounter additional hurdles in their professional lives. Challenges in finding work and meeting productivity standards, known as presenteeism, present formidable barriers. Beyond attendance issues, the pervasive stigma associated with obesity further compounds the difficulties, affecting not only workplace dynamics but also limiting potential job opportunities. This multifaceted impact emphasizes the need for comprehensive strategies to address the socio-economic determinants that contribute to the challenges faced by individuals with obesity.
- Childhood obesity is affected by SES status with less prevalence found in households with higher education (Prevention, 2019).
- “Obesity prevalence is 18.9 % among children and adolescents aged 2-19 years in the lowest income group, 19.9 % among those in the middle income group, and 10.9% among those in the highest income group” (Prevention, 2019, p1).
Examining the influence of socioeconomic status (SES) on childhood obesity reveals a concerning trend, with a notable discrepancy in prevalence based on household income and education levels. The statistics paint a stark picture: among children and adolescents aged two to 19 years, obesity prevalence is strikingly high at 18.9% in the lowest income group, 19.9% in the middle-income group, and significantly lower at 10.9% in the highest income group.
This data underscores the profound disparities that exist, revealing an almost 10% difference in obesity prevalence among households with varying income levels.
Prevalence: CDC 2021
The CDC outlined some graphs that we will review in the next few slides, including the prevalence of obesity over the years, Figure 1.
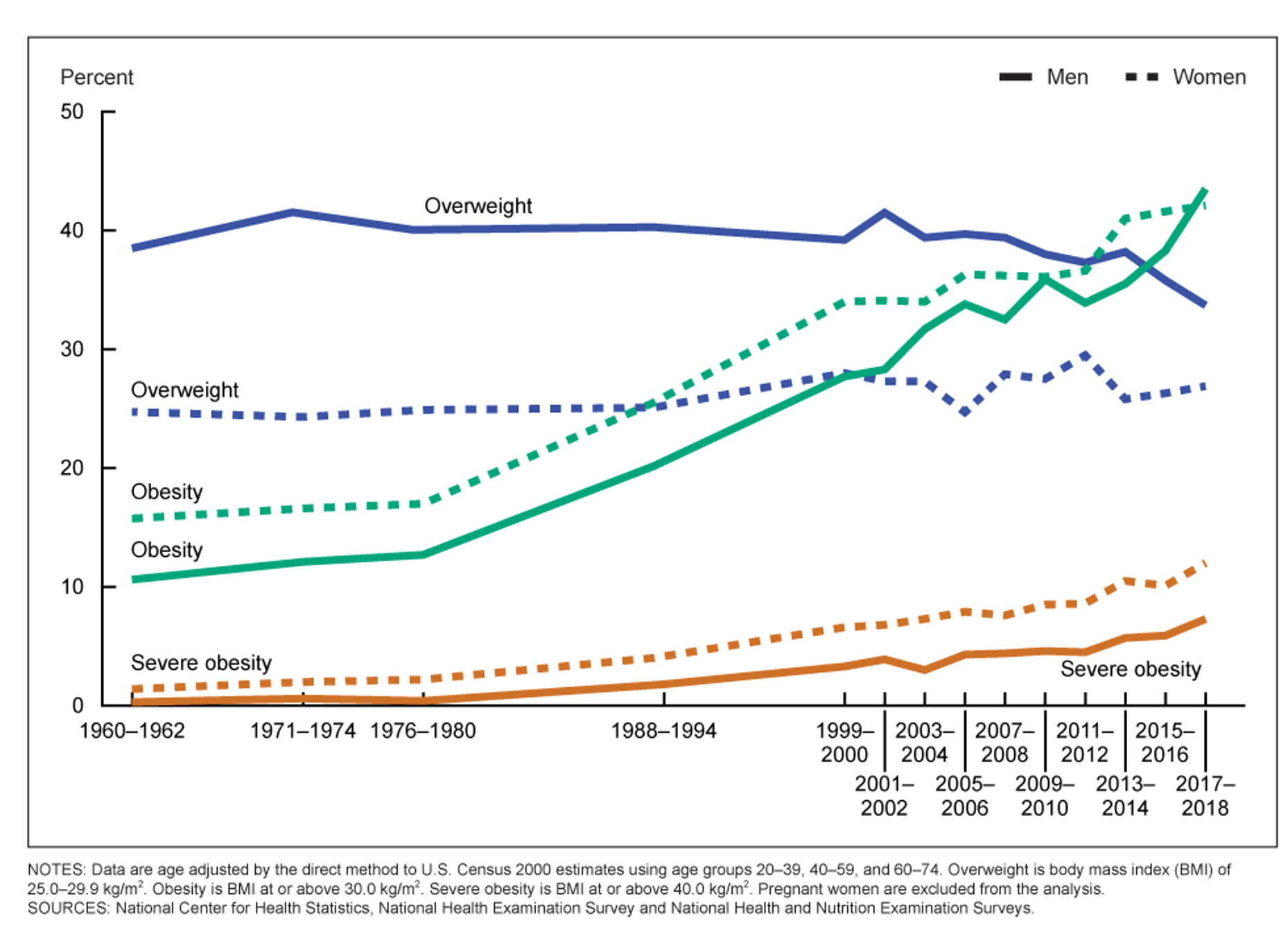
Figure 1. Prevalence of obesity over the years (Click here to enlarge the image).
The graphical representation vividly illustrates the trends in obesity, severe obesity, and overweight across different decades, with the solid line representing men and the dotted line representing women. Notably, the trajectory for severe obesity, depicted in orange, reflects a striking shift from nearly zero in the 1960s to a discernible upward trend in recent years. This transformation highlights the evolving landscape of severe obesity, underscoring the need for a deeper understanding of the factors contributing to this surge.
Similarly, the ascent in obesity rates over the past decade is unmistakable, emphasizing the urgency of addressing this health concern. The data reveals a steep incline, indicating a significant increase in the prevalence of obesity, particularly noteworthy in the context of public health.
Contrastingly, the graph portraying overweight trends, particularly for men in the 1960s, reveals a relatively high prevalence, hovering around 40%. However, in recent years, there has been a decline, potentially indicative of a shift where individuals who might have been classified as overweight in the past are now falling into the category of obesity. This intriguing observation prompts a deeper exploration of the dynamic relationship between overweight and obesity rates, shedding light on the evolving patterns in body weight categorization over time.
Figure 2 shows a graph for children.
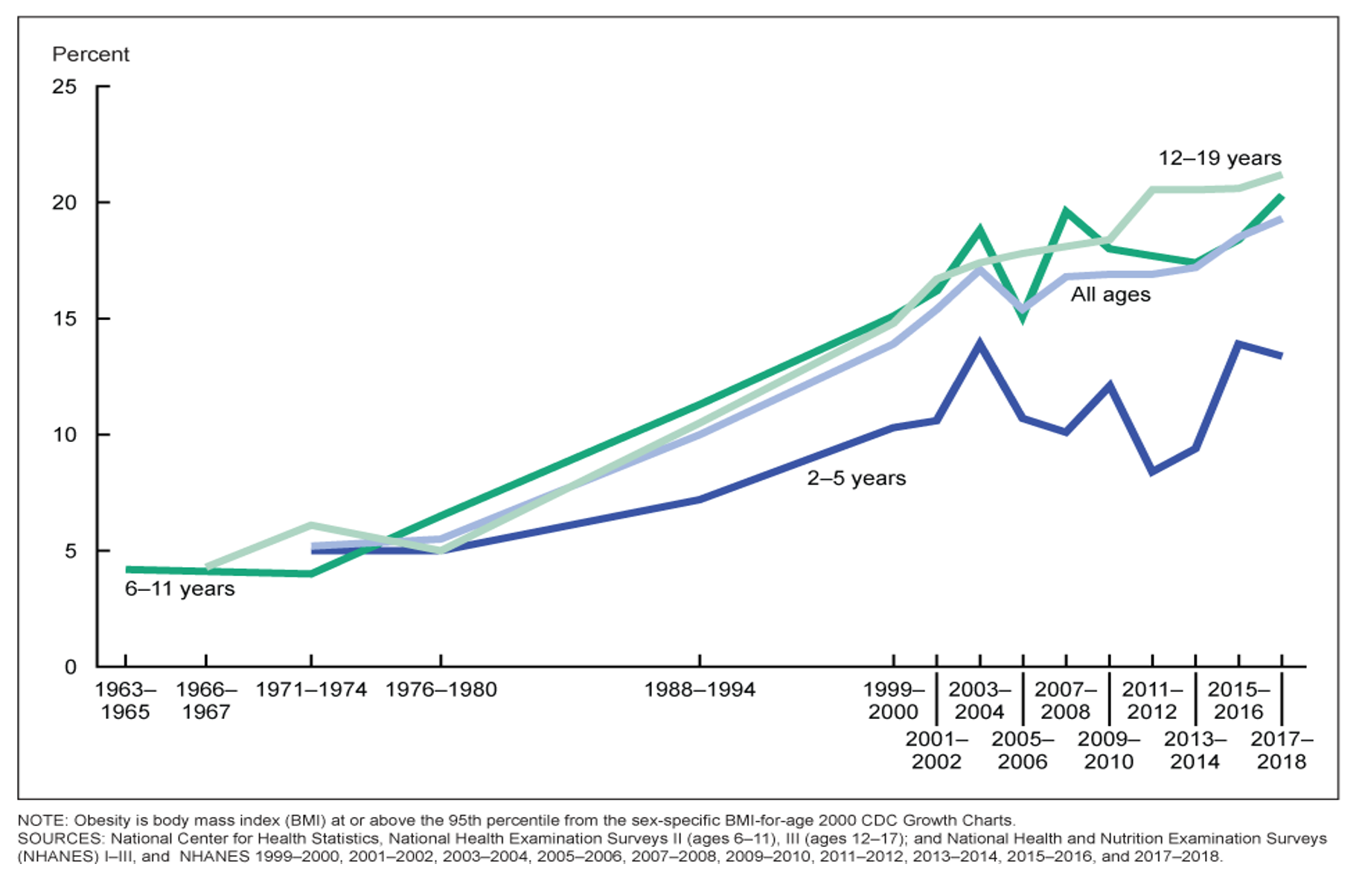
Figure 2. Prevalence of obesity in children over the years (Click here to enlarge the image).
The continuation of the graphical representation further accentuates the concerning trajectory of obesity prevalence over the years, commencing from the 1960s and now nearing 20%. A noteworthy observation is the highest prevalence occurring in the age range of 12 to 19 years. This age group exhibits the most pronounced rates of obesity, signaling a critical area of focus for intervention and preventive measures.
Figure 3 shows a depiction of obesity by state.
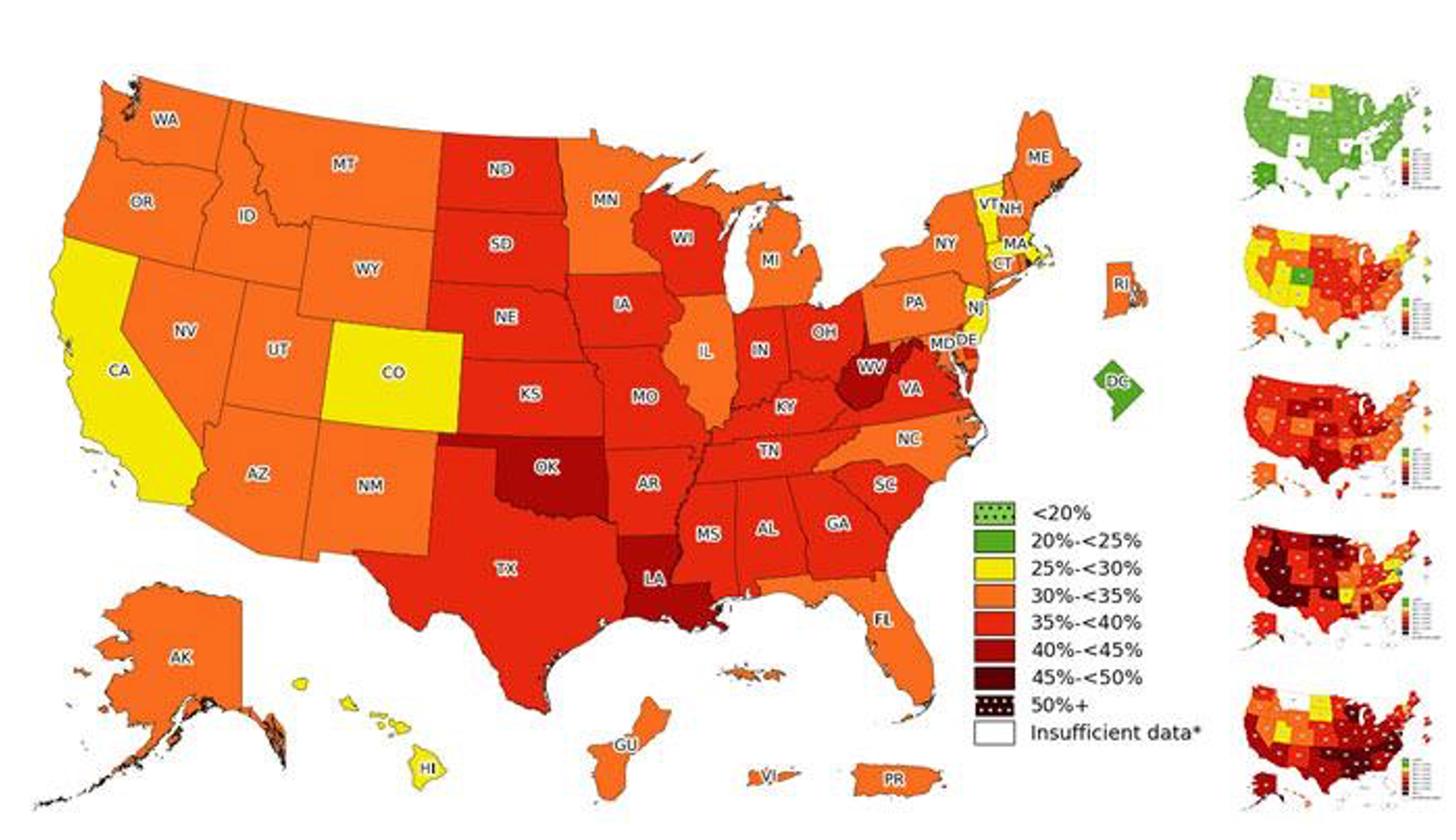
Figure 3. Graph of obesity by state (Click here to enlarge the image).
The prevalence map developed by the CDC provides a visual representation of the obesity landscape across the United States in the current year, 2023. The dotted green, representing a less than 20% prevalence, is notably absent across the entire map. Delaware is the only state with a prevalence falling within the 20 to 25% range, indicating a relatively lower incidence of overweight or obesity.
Moving into the yellow category (25 to 30%), a handful of states find representation, but the majority of the map is dominated by orange, red, and dark red categories. States outlined in dark red, with a 40 to 45% prevalence, including Oklahoma, Louisiana, and West Virginia. This configuration underscores the concentration of higher obesity rates in specific regions.
Considering the trends and the current state of obesity prevalence, the projection for the future is concerning.
Comorbidities
- This complex population has various associated health and psychological comorbidities that impact occupational therapy evaluation and treatment.
- People who have severe mental illness are at a higher risk of obesity (Conn, Bourke, James, & Haracz, 2019).
There are various comorbidities associated with this population, including psychological comorbidities as well as physical comorbidities. Additionally, people who have severe mental illness are at a higher risk of obesity. This may be due to medications, possible lack of activity, or access to gyms or areas where they can work out.
- Cardiovascular disease: conditions that can lead to heart attack, stroke, or chest pain due to narrowed or blocked blood vessels. Heart rhythm and heart muscles can also be affected and are considered an aspect of heart disease (Mayo Clinic, 2017).
- Hypertension: high blood pressure that can lead to heart disease due to the pressure of blood against the arteries (Mayo Clinic, 2017).
- Arteriosclerosis: thickening of the blood vessels that carry oxygenated blood to the body, which can prevent adequate blood flow to the body (Mayo Clinic, 2017).
- Renal failure: kidneys are unable to filter waste from the blood, such as metabolic waste, leading to impaired kidney function (Mayo Clinic, 2017).
- Gallbladder disease: inflammation of the gallbladder often caused by gallbladder stones that prevent bile from exiting the gallbladder (Mayo Clinic, 2017).
- Osteoarthritis: wearing down of protective cartilage over time. Most commonly seen in the hands, knees, hips, and spine (Mayo Clinic, 2017).
- Incontinence: inability to control the bladder (Mayo Clinic, 2017).
- Sleep apnea: sleep disorder in which periods of breathing stops and starts. This can occur for seconds or minutes, and sometimes for thirty times a night (Mayo Clinic, 2017).
- Metabolic disorders: when energy developed from food ingested in interrupted due to chemical imbalances or diseased organs (MedlinePlus, 2016).
- Endometrial cancer: cancer associated with the lining of the uterus, which is often diagnosed early due to abnormal vaginal bleeding (Mayo Clinic, 2017).
- Breast cancer: cancer developed from growths of cells of the breast that are uncontrollable (Breastcancer.org, 2017).
- Prostate cancer: cancer occurring in the prostate, which is responsible for seminal fluid (Mayo Clinic, 2017).
- Colon cancer: cancer occurring in the large intestine (Mayo Clinic, 2017).
- Heart disease: any condition affecting the function of the heart (Nordqvist, 2016).
- Type II diabetes: the body is not using insulin properly and depends on the pancreas to make extra insulin, affecting glucose levels in the body. Usually, this is associated with high blood sugar due to a lack of insulin (American Diabetes Association, 2017).
- Pain limitations: being limited physically or mentally due to a condition or illness that causes discomfort or suffering (Forhan, 2008; Foti & Littrell, 2004).
The spectrum of comorbidities associated with obesity encompasses both physical and psychological dimensions, creating a multifaceted health challenge for individuals within this population.
Cardiovascular disease emerges as a significant concern, manifesting in conditions such as stroke, chest pain, and hypertension. The relationship between obesity and hypertension is particularly noteworthy, as the increased pressure of blood against the arteries can contribute to the development of heart disease.
Arteriosclerosis further adds to the cardiovascular implications, thickening blood vessels and potentially impeding adequate blood flow, leading to conditions like stroke. Renal failure, impacting the kidneys and their ability to manage metabolic waste, becomes another dimension of concern.
Gallbladder disease, osteoarthritis, and incontinence are additional comorbidities, with obesity exacerbating pre-existing conditions and potentially causing more pain. Sleep apnea, a common occurrence among individuals with obesity, is characterized by interruptions in breathing, further complicating health outcomes.
Metabolic disorders are closely linked to obesity, as are various forms of cancer, including endometrial, breast, prostate, and colon. Notably, the correlation between high obesity rates and diabetes prevalence, particularly evident in states like Louisiana, Oklahoma, and West Virginia, underscores the interconnected nature of these health challenges.
The impact on pain limitations is profound, with conditions like osteoarthritis intensified by the extra weight, affecting joint functionality and mobility. This, in turn, poses challenges in safe movement and weight-bearing activities. The intricate web of obesity-related comorbidities highlights the necessity for comprehensive and interdisciplinary approaches to address the diverse health needs of this population.
Psychological Comorbidities
- Depression: mood disorder caused by consistent feelings of sadness, lack of motivation, and/or interest (Mayo Clinic, 2017).
- Anxiety: thoughts of persistent worry, tension, and recurring thoughts that may hinder a person from attending social events or that may produce physical symptoms such as rapid heartbeat (American Psychological Association, 2017).
- Sexual abuse: sexual activity that is unwanted, or consent that is not given for sexual behavior. Abuse may include the use of force or threats and/or taking advantage of an individual (American Psychological Association, 2017).
- Substance abuse: excessive use of chemical substances that leads to an inability to control the use of it leading to physical and mental dysfunctions (Healthy.Aging.org, 2016).
- Verbal abuse: use of words to cause harm towards a person or withholding a response to establish control or enforce nonexistence (Croft, 2016).
- Physical abuse: intentional, unwanted physical behavior that comes in contact or close contact with an individual (National Domestic Violence Hotline, 2016).
- Binge eating disorder: consuming large amounts of food with an associated feeling of inability to stop eating/lack of control, which becomes a regular occurrence (Mayo Clinic, 2017).
- Personality disorders: possessing a “rigid and unhealthy pattern of thinking, functioning, and behaving” (Mayo Clinic, 2017 para 1). Difficulty with being relatable to others and difficulty with perceiving situations affecting daily relationships and life. A person with a personality disorder may be unaware of their difficulties because it may seem very natural to them.
- Anorexia: eating disorder caused by low body weight in which an individual may have a fear of gaining weight interfering with their daily lives. Anorexia is also associated with binging and purging (Mayo Clinic, 2017).
- Bulimia: eating disorder in which an individual will binge on eating large amounts of food, and then purge to rid the extra calories consumed. This may be completed by excessive exercise, forced vomiting, or the use of laxatives (Mayo Clinic, 2017).
- Alcohol abuse: problems with controlling drinking that affect daily life and relationships as well as physical problems, and continuing to drink when these problems arise (Mayo Clinic, 2017).
- Night eating syndrome: eating most calories at night or throughout the night (Bell, 2016).
- Low self-esteem: feeling incapable and unworthy about oneself, and/or having a lack of self-respect (Roberts, 2012).
- Poor body image: distorted perception of one’s shape. A person with poor body image may feel uncomfortable in their own skin, and/or self-conscious (National Eating Disorders.org).
Psychologically, comorbidities include depression, anxiety, and personality disorders. Sexual, verbal, and physical abuse, as well as substance abuse, can be prevalent.
Individuals with obesity may also exhibit addictive behaviors. Interestingly, once weight is lost, these behaviors may transition to other forms of addiction. Binge eating disorder, characterized by consuming large amounts of food with an associated feeling of inability to stop eating or lack of control, can be a regular occurrence. Various eating disorders, including anorexia and bulimia, are not exclusive to weight loss attempts but represent forms of disordered eating, impacting individuals with obesity. Alcohol abuse is another manifestation of addiction, while night eating syndrome involves consuming most calories at night or throughout the night.
Low self-esteem and poor body image are significant psychological challenges associated with obesity. Addressing these dimensions requires a holistic approach, recognizing the intricate connection between mental health and weight-related struggles.
Interventions should extend beyond physical health to encompass the multifaceted aspects of an individual's well-being.
- Common psychological themes that appeared within the literature post-bariatric surgery include:
- transferring of food addiction to other forms of addiction (Mata et al., 2015)
- defense mechanisms such as self-protection, including social withdrawal and isolation (Daus, 2001)
Common psychological themes that appeared within the literature post-bariatric surgery include transferring a food addiction to other forms of addiction, as I mentioned, and then defense mechanisms such as self-protection, including social withdrawal and isolation.
- Oppositional behavior: insulting or demoralizing others, which often tends to be directed towards health care workers (Bennet, 2008).
- Some clients achieve positive gains within the first year after surgery, and then many experience a setback after the first year with the remission of comorbidities such as DM, sleep apnea, and hyperlipidemia (Smith, et al., 2019).
Oppositional behavior can be directed towards healthcare workers.
Some may have positive gains within the first year after surgery but have a setback with a remission of the comorbidities such as diabetes, sleep apnea, and hyperlipidemia. This specific statistic is correlated with age. So, if somebody completed the bariatric surgery when they were older, they were more likely to have a setback after the first year of this surgery.
Stigma
- When working with clients, families, and caregivers, it is important to recognize our biases and how they may impact treatment approaches.
- An additional knowledge gap was attained, where all healthcare fields require additional training. The evidence literature discovered that there is a common stigma associated with obesity and that sensitivity is a critical part of bariatric care (Fruh et al., 2017)
Obesity-related stigma holds a significant place in my journey towards focusing on doctoral studies in obesity and bariatric care. A pivotal moment occurred while working with a patient over 500 pounds in a skilled rehab facility. The lack of adequate equipment for her size resulted in a challenging situation that should have been avoided. On a Saturday with limited staff, the struggle to facilitate her basic needs, like accessing the bathroom, underscored the inadequacies in our preparedness.
The experience was profound, with at least eight people crammed into her room, attempting to provide support and exposing her to intense embarrassment. The prevailing atmosphere in the hallway further exacerbated the situation, revealing a lack of warmth and acceptance. Witnessing the impact on her care and the emotional toll it took on the patient ignited my determination to explore ways healthcare professionals, including occupational therapists, can better understand and address their own biases and stigmas when working with individuals affected by obesity.
Recognizing this knowledge gap in the literature, I advocate for sensitivity training across all healthcare fields. Acknowledging and addressing biases can significantly improve the quality of care provided to individuals with obesity. It's imperative for healthcare professionals to be cognizant of their own prejudices and strive towards creating an environment that fosters empathy, respect, and understanding for this population.
- In a synthesis by Mold and Forbes (2011) about obesity-related stigma in healthcare, the following key themes were recognized as factors that impacted the treatment of clients with obesity:
- powerlessness
- treatment avoidance
- psycho-emotional functioning
- professional attitudes
- confidence and training
- health contact time
- differences in treatment options
The synthesis on obesity-related stigma in healthcare, drawn from the perspectives of clients with obesity, sheds light on crucial themes that impact their experiences within the healthcare system.
Clients with obesity commonly reported feelings of powerlessness, perceiving a lack of control over their treatment and healthcare journey. Treatment avoidance emerged as a prevalent theme, with individuals sensing reluctance or delay in engagement from healthcare professionals. They often felt relegated to the last treatment of the day, experiencing a disadvantage in their interactions with healthcare providers. The impact extended to their psycho-emotional functioning, with reported feelings of vulnerability and emotional distress.
A pervasive theme was the perception of a lack of professional attitudes among healthcare professionals. Clients felt that healthcare providers exhibited insufficient confidence and training in dealing with obesity-related concerns. This translated into decreased health contact time and limited access to diverse treatment options, further contributing to their sense of disenfranchisement.
These insights underscore the profound impact of obesity-related stigma on individuals seeking healthcare. For healthcare professionals, awareness of these dynamics is crucial, especially considering the vulnerability of patients in healthcare settings. Recognizing the potential barriers clients with obesity face, both in seeking care and participating in their healthcare, is pivotal. The importance of fostering a welcoming and inclusive environment cannot be overstated, as it plays a fundamental role in facilitating positive healthcare experiences and outcomes for this population.
- This stigma also affects children and adolescents and can begin at a young age leading to an increase in bullying and victimization affecting:
- life participation
- social participation
- poorer academic performance
- self-harm behaviors
- suicidal ideation (Pediatrics, 2018)
- Obesity related stigma in children can also be received by teachers. A recent study revealed that educators have lower academic expectations of students with obesity (Pediatrics, 2018).
Obesity-related stigma doesn't spare children and adolescents, impacting them from a very young age and permeating various aspects of their lives. The consequences are far-reaching, leading to bullying and victimization, which significantly affects their life and social participation. Disturbingly, this stigma has been linked to poor academic performance, self-harm behaviors, and suicidal ideation among children and adolescents.
The roots of obesity-related stigma are planted early in life, creating a trajectory that may persist into adulthood, with potential long-term consequences. Notably, this stigma isn't limited to peer interactions; it can also be interactions with teachers. A study uncovered lower academic expectations from educators for students with obesity. This finding is particularly impactful, as it not only contributes to the perpetuation of stigma but also implicates the future educational and academic performance of children with obesity.
For pediatric therapists working in schools, this underscores the importance of a thoughtful and empathetic approach, recognizing the potential challenges faced by children with obesity. Addressing obesity-related stigma in educational settings is crucial for fostering an environment that supports the well-being and academic success of all students, regardless of their weight or body size.
- Clients with obesity not only encounter stigma and bias within healthcare, but also within the general public, the media, and by employers, (Forhan, Obesity and health occupation, 2008).
- Additionally, Leemhis and Cozzolino (2010) specifically surveyed occupational therapy practitioners revealing alarming results.
- The survey revealed that 67.1% realized that critical statements regarding a client’s weight within the healthcare workplace were evident.
- Approximately half of the occupational therapy practitioners that worked in a variety of settings were found to have a negative bias associated with obesity (Leemhis & Cozzolino, 2010).
The pervasive issue of obesity-related stigma extends beyond healthcare settings, affecting individuals in the general public, media, and workplaces. Portrayals of people with obesity in ads, commercials, and movies contribute to shaping societal perceptions, influencing how the public views individuals with obesity.
An intriguing study by Leemhis and Cozzolino delved into the perceptions of occupational therapy practitioners regarding obesity. Surveying 145 OTs, the findings were revealing. A significant 67.1% acknowledged the presence of critical statements regarding a client's weight within the healthcare workplace, shedding light on the prevalence of weight-related biases in this professional setting. This statistic is notably high, emphasizing the need for awareness and interventions within the occupational therapy community.
Additionally, the study highlighted that approximately half of the OTs working in various settings exhibited a negative bias associated with obesity. This insight underscores the impact of societal biases on professionals within the occupational therapy field. The study, encompassing both OTs and COTAs across diverse settings, illuminates the need for targeted efforts to address and mitigate obesity-related stigma within the occupational therapy profession.
Sensitivity Programs
- In order to prevent and assist with the associated stigma, sensitivity programs are being implemented for students and healthcare workers and are acquiring positive outcomes.
- The following techniques to reduce obesity-related stigma include:
- modules (Falker & Sledge, 2011)
- online programs (Hague & White, 2005)
- role playing
- in-person lectures (Vacek, 2007)
- advocate against obesity-related stigma (Pediatrics, 2018)
Various sensitivity programs have been initiated, demonstrating positive outcomes among students and healthcare workers. These programs utilize diverse strategies to reduce stigma and enhance understanding, fostering a more empathetic and inclusive approach.
One effective strategy involves the incorporation of educational modules. These modules provide comprehensive information about obesity, unraveling its complexities, and shedding light on the profound impact of associated stigma.
Leveraging the flexibility and accessibility of online platforms is another impactful approach. Online programs disseminate information and interactive content, reaching a broader audience and allowing participants to engage with the material at their own pace. This method facilitates a more inclusive learning environment.
In-person role-playing exercises offer a hands-on and immersive experience. Simulating real-world scenarios enables participants to gain insights into the challenges faced by individuals with obesity, fostering empathy and promoting a deeper understanding of their perspectives.
Traditional in-person lectures also play a crucial role in sensitivity programs. These lectures delve into various aspects of obesity, including its associated stigma, and emphasize cultivating a supportive environment. They serve as a platform for open discussions and exchanging perspectives among participants.
Furthermore, advocacy programs tailored specifically for pediatrics have been introduced. These initiatives underscore the importance of combating obesity-related stigma, particularly in the context of children and adolescents.
Sensitivity Programs: Children
- Education provided on obesity and the comorbidities associated with obesity
- Avoid associating phrases such as “an obese child” and use “a child with obesity” instead (Pediatrics, 2018).
- Avoid associating words including: “fat,” “weight problem,” “extremely obese,” and use “body mass index” or “weight” instead as they are more neutral words (Pediatrics, 2018).
- Become involved at school by including parents, teachers, and administrators.
- Search for where obesity-related stigma can develop from within the family and/or friends of the child.
- Have an accommodating environment including appropriate sized seated options (Pediatrics, 2018).
- Positive role playing
In childhood education, there's a distinctive but equally valuable emphasis on educating about obesity and its associated comorbidities. The key is to ensure that staff and individuals working with children are well-informed about obesity and its implications. It's encouraged to adopt language sensitivity, refraining from phrases like "obese child" and opting for "a child with obesity" instead. Similarly, words such as "fat," "weight problem," and "extremely obese" are replaced with more neutral terms like "body mass index" or "weight."
Sensitivity programs for children extend beyond the classroom, involving parents, teachers, and administrators. The goal is to bring attention to potential areas where obesity-related stigma may develop. Research often points to family and close friends as sources of stigma, emphasizing the importance of identifying root causes.
Creating an accommodating environment plays a pivotal role in addressing obesity-related stigma. This includes providing appropriately sized seating options and incorporating positive role-playing scenarios. Notably, changes in healthcare settings, such as offering various seating options at doctor's appointments in the U.S., reflect an evolving awareness and commitment to making everyone feel comfortable and respected, irrespective of their body size.
This is a bariatric suit in Figure 4.

Figure 4. Example of a bariatric suit.
This can be used for sensitivity training. It could be used in academia if you're trying to teach students how to use a lift or how to transfer a client with obesity or work with a client. This can also be used for somewhere in healthcare where you're trying to educate your staff on what it might be like to be of this size and working with healthcare professionals. So this is being frequently used as a part of sensitivity training as well.
People First Language
- Avoid labeling an individual with obesity with the disease
- For example, say “the patient affected by obesity” rather than “the obese patient”
It is important to avoid labeling an individual with obesity with the disease. For example, say, "the patient affected by obesity" rather than "the obese patient."
Conclusion
- Statistics
- Definitions
- Comorbidities
- Stigma
- Sensitivity Programs
Here is an overview of what we discussed. In conclusion, I want to ask a few interactive questions to see your responses.
1) Within your practice, how has the rise of obesity impacted the care that you provide for your clients, your families, your caregivers, or your own health? Here are some responses/themes:
- Lack of access to proper equipment
- Increase in back injuries
- Lack of mechanical lifts
- Lack of training
- Hard to complete ADLs
- Emotionally and physically challenging
- Mental health issues
- Need support post-surgery
- Exercises and therapeutic activities are often limited to bed
- Safe handling issues
- Lack of manpower
- Need more staff
- Diabetes management
- Home health hard
- Increased health cost
- Poor hygiene
- Slower gains
- Discharges held up due to transportation issues
2) What strategies could you use to reduce obesity stigma at work?
Here are some responses/themes:
- Educating caretakers
- Patient-first verbiage
- Current research
- Positive statements about progress
- Encourage administration for obesity training for staff
- Support for newer therapists
- Encourage body positivity
- Practicing empathy
- In-services on bariatric equipment
- Brainstorming with family
- Client-centered treatment
- Emphasis on patients' abilities versus their inabilities
- Understand the individual's background, circumstances, and level of education
References
See additional handout.
Citation
Phillips, J.(2023). The bariatric client and the OT role, part 1. OccupationalTherapy.com, Article 5669. Available at www.occupationaltherapy.com
