Editor's note: This text-based course is a transcript of the webinar, The Bariatric Client And The OT Role, Part 2, presented by Jennifer Phillips
OTD, OTR.
Learning Outcomes
- After this course, participants will be able to identify at least two ways that occupational therapy can assist clients and children with obesity with 100% accuracy.
- After this course, participants will be able to identify at least two factors to evaluate prior to assisting an obese client with transferring with 100% accuracy.
- After this course, participants will be able to identify at least two variables that affect safe patient handling when working with an obese client in 1/1 trials.
Introduction
Thank you for joining me for part two. In part one, we discussed the background of obesity and bariatric care and the comorbidities associated with that, including childhood obesity. Today, we will focus more on occupational therapy, evaluation and treatments, safe patient handling, and bariatric equipment.
Poll
Before delving into our presentation, I would like to initiate a brief poll that aligns with a study we will explore further in this webinar.
What are the factors that most significantly affect your ability to work with clients dealing with obesity?
The options are stigma, equipment, safe patient handling, time, or a lack of education on our part, specifically insufficient knowledge about obesity. Based on the results, it appears that a majority, 55% of you, highlighted safe patient handling as the primary concern, with equipment following closely behind. These insights are valuable, and we will delve into both of these aspects in greater detail during the course of today's discussion.
OT and Obesity
- As clients with obesity face many barriers to occupational performance, occupational therapy practitioners can bring a holistic and client-centered approach to assisting clients with obesity.
- This includes participating in and enjoying healthy routines, weight management, and assisting clients in achieving goals in affected occupations (Reingold, & Jordan, 2013).
Clients facing obesity encounter numerous barriers to occupational performance. Occupational therapy, with its foundation in activity analysis, provides a holistic and client-centered approach. The literature on occupational therapy interventions for obesity highlights the impact on various occupations.
Occupational therapists play a vital role in identifying and addressing challenges in affected occupations. The focus is on what matters most to the client, including participation in healthy routines, weight management, and achieving goals in their chosen occupation. A client-centered approach empowers individuals with obesity to overcome barriers and improve their overall quality of life.
Assessments
- Barthel Index: A detailed activity of daily living scale
- Katz Index of Independence in ADL: A 6-item activity of daily living scale
- Brody Instrumental Activities of Daily Living Scale (IADL): 8-item instrumental activity of daily living scale
- Canadian Occupational Therapy Measure (COPM): Assessing self-perceived performance throughout occupational therapy intervention
Various assessments are available, and I've selected four commonly used in-home care settings. The Barthel Index is a comprehensive scale focusing on activities of daily living (ADLs), providing detailed insights into specific areas that require attention.
The Katz Index of Independence, a succinct six-item ADL scale, offers a more generalized yet quick assessment tool. Similarly, the Brody Instrumental Activity of Daily Living Scale, an eight-item scale, concentrates on instrumental ADLs. This scale is particularly valuable for assessing areas beyond basic self-care.
The Canadian Occupational Therapy Measure (COPM) stands out as a self-perceived performance assessment tool. It allows clients to express their perceived needs and priorities in terms of occupational performance. This tool proves especially valuable in understanding the client's perspective and tailoring occupational therapy interventions to address their specific concerns and goals.
OT and Obesity Study
In addition to complexities being found with this population, research revealed a need for occupational therapy practitioners to facilitate improved participation in daily meaningful occupations. So again, the literature supports this both for adults and for children. And we'll get into both later on.
- A study in Australia was conducted reviewing barriers to treatment of occupational therapy when working with clients with obesity through the use of a survey.
- A significant barrier was weight-related stigma impacting social, leisure, and work (Lunt, 2022)
Let's discuss a relevant Australian study that correlates with the recent poll findings. The study aimed to uncover barriers to occupational therapy treatment for clients with obesity through a survey. The poll we just conducted briefly highlighted equipment and safe patient handling as primary concerns, aligning with the study's results. The Australian research emphasized weight-related stigma as a significant barrier, notably affecting social, leisure, and work-related occupations.
The survey involved 80 occupational therapists, constituting a substantial and representative sample for analysis. The identified impacted occupations included social, leisure, and work-related activities, highlighting the pervasive influence of obesity on various aspects of an individual's life.
As occupational therapists, we possess the necessary skill set to address these challenges. The Canadian Occupational Therapy Measure (COPM) emerges as a valuable assessment tool in this context. Utilizing the COPM allows us to pinpoint specific barriers clients perceive, enabling tailored interventions to enhance their engagement in social, leisure, and work-related activities.
- Occupational therapy has been identified to assist clients with obesity through “health promotion and prevention, increasing physical activity, modifying diet, and decreasing the impact of obesity” (Lunt, 2022, p 403)
- Impact of obesity, including associated health conditions, psychosocial, and stigma
Occupational therapy plays a vital role in assisting clients with obesity through health promotion and prevention, a newly added category in the Occupational Therapy Practice Framework (OTPF). This category is particularly relevant, encompassing strategies to increase physical activity, modify diet, and mitigate the impact of obesity. Addressing the impact involves considering the associated comorbidities, both mental and physical, and finding ways to alleviate their effects.
Within the realm of health promotion, occupational therapists can contribute significantly to decreasing the impact of obesity on various fronts. This includes addressing associated health conditions, psychosocial aspects, and combating stigma. The holistic nature of occupational therapy allows us to tailor interventions that encompass both the physical and mental well-being of clients.
Moreover, an essential aspect of an interprofessional approach involves collaborating with other disciplines. In the context of modifying diet, for instance, working in tandem with a dietitian can prove highly effective. Occupational therapists can contribute to the collaborative effort by assisting with developing grocery lists, fostering healthy routines, meal planning, and cooking. However, recognizing the specialized nature of nutrition, involving a dietitian ensures a comprehensive and targeted approach to address nutritional aspects effectively. This interdisciplinary collaboration reinforces the holistic support offered to clients dealing with obesity, acknowledging the diverse dimensions of their health and well-being.
- Results indicated that occupational therapists in Australia were conducting most of their interventions of
- ADLS
- pressure management
- equipment
- home modifications (Lunt, 2022)
The same study highlighted that occupational therapists in Australia predominantly focused their interventions on activities of daily living (ADLs), pressure management, equipment, and home modifications. It is noteworthy to explore collaborative opportunities with other disciplines, especially in areas such as pressure management, where nursing expertise can be instrumental.
Given the heightened risk of wounds in individuals dealing with obesity, involving nursing professionals in pressure management interventions is crucial. Occupational therapists, often involved in patient bathing and dressing, can contribute valuable observations to support nurses in conducting comprehensive skin assessments. This collaborative effort aims at preventing pressure sores and addressing the unique needs of this population.
Moreover, the study underscores the significance of interventions to prevent pressure-related issues. Occupational therapists can play a pivotal role in implementing equipment and home modifications tailored to address these concerns, ultimately influencing participation in ADLs. Recognizing the multifaceted nature of interventions, this study underscores the importance of a comprehensive approach that leverages the strengths of different disciplines to enhance the overall well-being of clients dealing with obesity.
- OTs also reported addressing:
- motivation
- self-esteem
- anxiety
- coping with stigma
- discrimination
- psychosocial strategies
- These OTs identified that the most significant barrier to treatment was not feeling educated enough to work with clients with obesity and access to bariatric equipment (Lunt, 2022)
The study also revealed that OTs included a mental health component in their treatments. This encompassed addressing motivation, self-esteem, assisting with anxiety, and coping with obesity-related stigma, whether within the healthcare system or the general public. The study underscores the importance of incorporating a psychosocial approach when working with clients dealing with obesity.
Recognizing the potential past negative experiences with healthcare professionals, building a trusting relationship becomes a pivotal aspect of intervention. Establishing trust is essential to demonstrate advocacy for clients and provide support on their healing journey. This is particularly pertinent as the study identified a significant barrier to treatment: the perception of not feeling adequately educated to work with clients with obesity and challenges in accessing bariatric equipment. This aligns with the poll findings and highlights the need for comprehensive education on obesity at the foundational level of occupational therapy training.
Moreover, the research emphasizes that healthcare workers and caretakers face an elevated risk of work-related injury due to factors associated with obesity. These factors include education and training, as well as difficulties in referencing written procedures and protocols. This underscores the importance of ongoing education and training to equip healthcare professionals with the knowledge and skills needed to address the unique challenges presented by clients dealing with obesity.
Safe Patient Handling
- The research expresses that healthcare workers and caretakers have a greater risk of work-related injury due to factors associated with obesity, including education and training, and an inability to reference written procedures (Cowley & Leggett, 2011).
My research initially centered on safe patient handling, a topic close to my heart due to a work-related injury early in my career. Experiencing firsthand the impact it had on my ability to practice as an occupational therapist fueled my commitment to preventing injuries for others in our field, especially considering the vulnerability within the healthcare setting.
The literature consistently underscores that when working with clients dealing with obesity, there is an increased risk of work-related injuries for healthcare professionals. Another critical aspect highlighted is the lack of ability to reference written procedures and protocols, a factor that poses challenges in ensuring the safety of both therapists and clients.
In light of these findings, it becomes imperative for healthcare facilities to establish and implement safe patient handling protocols. If such protocols are not in place, there is an opportunity to take proactive steps. Forming a dedicated team or coalition to develop and institute these protocols can be a constructive approach. By addressing these concerns, we contribute to creating a safer and more supportive environment for occupational therapists and other healthcare professionals, ultimately enhancing the quality of care provided to clients dealing with obesity.
- Surveys were conducted for physical and occupational therapy practitioners, revealing that 71% of injuries were due to manually lifting clients.
- The size of the client contributed to the injuries reported, including lower back injuries (Darragh, Campo, and King, 2012).
The research conducted by Darragh, Campo, and King involved surveys of both physical therapy and occupational therapy practitioners, capturing insights from approximately 1,158 professionals. The findings shed light on a significant aspect of occupational therapy practice – the risk of injuries associated with manually lifting clients.
Clinicians reported that 71% of injuries were attributed to the manual lifting of clients, highlighting the physical strain associated with this aspect of the profession. Furthermore, the size of the client emerged as a contributing factor to reported injuries, particularly those affecting the lower back. Notably, lower back injuries were identified as the predominant type of injury in this study.
These findings underscore the importance of having proper equipment and adequate time to accommodate the unique needs of clients, particularly those with larger body sizes. Ensuring occupational therapists have access to suitable tools and resources not only promotes the well-being of the practitioners themselves but also safeguards the health of the clients they serve.
- Shape and size of the client
- Cooperation level
- Level of mobility
- Pain
- Comfort and dignity considerations (Hignett & Griffiths, 2009)
- Factors that impact safe patient handling related to staff
- Effective communication
- Access to policies and training
- Lack of staffing
- The environment
- Access to equipment and accessible furniture (Hignett & Griffiths, 2009)
The study identified several factors that significantly impact the ability to complete safe patient handling, encompassing both client-related and staff-related considerations. In terms of clients, factors such as shape and size, cooperation level, mobility, level of pain, and considerations for comfort and dignity during transfers were found to be influential.
The shape and size of the client, along with their cooperation level and mobility, directly affect the ease and safety of patient handling. Additionally, the level of pain experienced by the client plays a crucial role in these procedures. Comfort and dignity considerations, including the appropriateness of room setup, chairs, gowns, and privacy measures, were also highlighted as critical components.
Staff-related factors contributing to safe patient handling included effective communication among team members, particularly essential in scenarios requiring co-treatment or collaboration between multiple staff. Access to policies and training was identified as an area where improvements are needed, with a lack of consistent training being noted in the literature.
Other staff-related factors included a staffing shortage, potentially hindering collaborative efforts and the overall environment's suitability for patient transfers. Adequate room setup, space for transfers, and accessibility to equipment and furniture were underscored as crucial considerations.
Despite time constraints and productivity standards, prioritizing a comprehensive assessment of these factors before initiating patient transfers is emphasized. This proactive approach not only mitigates the risk of work-related injuries for staff but also ensures the safety and well-being of clients, particularly those dealing with obesity. Balancing efficiency with these critical considerations is vital for creating a safe and supportive environment for both occupational therapists and their clients.
- It is imperative that therapists be educated on how to not only operate ceiling lifts, but all types of bariatric equipment and furniture to protect themselves, and the clients that they facilitate.
- The use of bariatric lifts and ceiling lifts may reduce the chances of work-related injury.
Ensuring therapists are well-versed in the operation of various bariatric equipment and furniture is crucial for safeguarding both their well-being and that of the clients they serve. Proficiency in using bariatric lifts, including ceiling lifts, is particularly important to reduce the risk of work-related injuries when working with individuals dealing with obesity.
Ceiling lifts, in particular, are highlighted as an ideal choice for this population in the literature. However, there is a noticeable gap in training regarding the use of bariatric equipment and lifts. Bridging this gap through comprehensive education and training is essential to enhance therapist competence and promote the safe and effective use of these specialized tools.
In an effort to address this need, I will be sharing a resource later in the webinar. This resource aims to empower therapists with the knowledge and skills required to navigate the challenges associated with bariatric care, ensuring a safer and more supportive environment for therapists and their clients.
- 134 healthcare workers were surveyed across 5 VA hospitals on work perceived work-related injury with a focus on the influence of body weight of the patient
- Healthcare workers reported manually handling a bariatric patient about one time a week.
- A bariatric lift can accommodate 1100lbs and air-assisted transfer mats can accommodate up to 1200lbs (Galinksy et al., 2021)
The study conducted by Galinsky et al. focused on surveying 134 healthcare workers across five VA hospitals in the U.S., with a particular emphasis on perceived work-related injuries, considering the influence of the body weight of the patient. Notably, the research highlighted that healthcare workers reported manually handling a bariatric patient approximately once a week, without utilizing equipment for assistance.
The frequency of manually handling a bariatric patient once a week translates to at least four patients a month over time. This consistent manual handling places a significant burden on healthcare workers and increases the risk of injury over the long term. It's essential to consider the cumulative impact on the well-being of healthcare professionals engaging in such practices.
In contrast, bariatric lifts and air assistive transfer mats offer safer alternatives. Bariatric lifts can accommodate up to 1100 pounds, providing a secure means of transferring patients. Similarly, air assistive transfer mats, with a weight capacity of up to 1200 pounds, offer a more ergonomic and less physically demanding approach to patient transfers.
Reflecting on the weight capacity of these lifts and mats compared to the demands of manually handling a bariatric patient, the importance of adopting safer practices becomes evident. Even with the support of multiple personnel or equipment like ceiling lifts, the strain on healthcare workers could still be substantial. These findings underscore the necessity of prioritizing the use of appropriate equipment to minimize the risk of work-related injuries and promote the well-being of healthcare professionals.
- Healthcare workers reported injuries with the use of a ceiling lift (the patient leaning back during the lift), and manually rolling bariatric patients
- Despite this information, healthcare workers have reported having access to the equipment, but not using it due to:
- time constraints
- difficulty following safe patient handling protocols and policies.
- In settings where healthcare workers had more time, more bariatric equipment was utilized, and less work related injury was reported. (Galinksy et al., 2021)
The study reported an incident where a healthcare worker was injured while using a ceiling lift. The injury occurred when the patient leaned back during the lift, affecting the clinician. This serves as a crucial reminder that, even with the use of lifts or equipment, healthcare workers are still at risk of injury. It emphasizes the importance of understanding the setup and proper use of equipment to ensure both patient and clinician safety.
Other reported injuries were associated with manually rolling bariatric patients, a task that could be addressed by utilizing air transfer mats, providing a safer alternative for patient movement.
Interestingly, despite having access to equipment, healthcare workers reported not using it. This was attributed to time constraints and challenges in adhering to safe patient handling protocols and policies. This finding is concerning, as it reflects a potential gap in implementing available resources that could enhance safety.
Advocating for more time when working with bariatric clients emerges as a crucial consideration. In settings where healthcare workers had more time, there was a higher utilization of bariatric equipment, and fewer reported work-related injuries. This correlation highlights the importance of allocating adequate time for safe patient handling practices, not only for the well-being of healthcare professionals but also to mitigate the financial costs associated with work-related injuries and subsequent time away from work. It underscores the need for prioritizing comprehensive training, sufficient time, and the utilization of available equipment to enhance the safety of both clinicians and patients.
- NIOSH guidelines from the CDC suggest that the maximum weight to be lifted by a caregiver or professional should be no more than 35 pounds. However, the new recommendation is that even lifting 35 pounds is a risk to the body and that the overall goal of safe patient lifting programs should be to avoid manual lifting whenever possible (Centers for Disease Control and Prevention, 2017).
- It is recommended that when working with clients with obesity to avoid manual handling whenever possible.
The current lifting protocol provided by the National Institute for Occupational Safety and Health (NIOSH) guidelines from the Centers for Disease Control and Prevention (CDC) emphasizes that the maximum weight to be lifted by a caregiver or professional should not exceed 35 pounds. However, a recent shift in recommendations suggests that even lifting 35 pounds poses a risk to the body. The new emphasis is on the overarching goal of safe patient handling programs: avoiding manual lifting whenever possible.
This recommendation holds particular significance when working with clients who have obesity. The statistics in today's discussion highlight the increased likelihood of getting hurt during manual lifts, underscoring the importance of minimizing such practices whenever feasible. While it may not always be ideal or practical to entirely avoid manual lifting, a proactive approach to reducing its frequency is crucial.
Additionally, recognizing that clients with obesity, like any other individuals, possess valuable insights into their bodies and movement capabilities is vital. Consulting with the client to understand how they navigate their movements in a safe and comfortable manner can inform safer transfer strategies. This collaborative and client-centered approach promotes a sense of empowerment for the client and contributes to injury prevention and overall well-being.
Environment
- Besides education being a barrier for occupational therapists, the environment in which occupational therapy practitioners work with clients who have obesity requires improvement.
- The literature indicated that a disservice has been done in managing this population, as well as to the occupational therapy practitioners who treat them, by having limited access to the proper environment, tools, and education to effectively treat these clients.
The literature underscores that the environment in which occupational therapy practitioners work with clients who have obesity needs improvement. A common theme in the literature is the limited access to the proper environmental tools and education necessary to effectively treat this population. This limitation poses challenges for occupational therapists and does a disservice to the clients in managing this specific population.
The lack of access to essential equipment emerges as a notable barrier, consistent with concerns expressed in previous discussions. Inadequate access to necessary tools hampers optimal care delivery, creating challenges for both healthcare workers and their clients. Recognizing this as a significant barrier emphasizes the need for comprehensive solutions to address the environmental shortcomings hindering effective treatment for clients with obesity.
Improving the environment in which occupational therapy practitioners operate is essential to ensure better outcomes for clients.
- Not only may healthcare staff have hesitancies when working with clients with obesity, but the clients themselves shared their fears of being transferred if the equipment was not well suited to their size. They also feared that essential equipment, such as toilet seats, had the ability to break at any moment. (Forhan, 2008)
Healthcare staff hesitancies when working with clients with obesity are paralleled by the fears expressed by the clients themselves. These individuals articulated concerns about the transfer process if the equipment was not well-suited to their size. Additionally, they harbored anxieties about the potential breakage of essential equipment, such as toilet seats, contributing to an overall apprehension.
Putting oneself in the shoes of these clients, it becomes evident that feeling unsupported and unsafe in a healthcare setting can be a significant barrier to the healing process. The worries about equipment suitability and durability create a tangible impact on the overall patient experience. Addressing these concerns is crucial to ensuring that clients, particularly those with obesity, feel supported, secure, and confident in their healthcare environment. Establishing an environment that fosters trust and reassurance is foundational to effective care and positively influencing the well-being of individuals seeking treatment.
- Furthermore, a client’s privacy was a factor that had been intruded upon due to the hospital gowns being too small (Forhan, 2008).
- With staff shortages and a lack of bariatric equipment present, clients with obesity are less likely to be assisted with position changes impacting skin integrity.
- Clients with obesity themselves felt neglected due to these reasons (Forhan, 2008).
The issue of privacy intrusion for clients with obesity was exacerbated by hospital gowns being too small, a factor that can significantly impact the patient's sense of privacy. To address this challenge, a practical strategy involves tying two gowns together before entering the room, especially if bariatric gowns are not readily available. This improvisation aims to enhance the privacy and comfort of the client, offering a solution in the absence of specialized clothing.
However, staff shortages and the lack of bariatric equipment further compound the challenges faced by clients with obesity. Insufficient support and infrequent checks on bariatric patients can result in skin integrity issues, potentially leading to wounds. The findings indicate that clients with obesity may feel neglected due to these systemic issues, perceiving disparities in treatment options and experiencing a sense of being treated differently.
In the spirit of client-centered care, it becomes imperative for healthcare professionals to ensure that clients with obesity receive equal attention, time, and treatment options.
- In a synthesis about patients' and health care professionals’ perceptions of obesity, “health professionals often lack the physical equipment and technical resources to deliver care to obese patients, further compounding the situation and impeding the professional’s ability to provide best practice care,” (Mold & Forbes, 2011, p. 140).
- This synthesis also discovered that clients with obesity felt the following accommodations were found to be lacking for this population:
- Gowns
- Tables
- Equipment
The synthesis by Molds and Forbes delves into the perceptions of both patients and health professionals regarding obesity. It highlights a critical challenge faced by health professionals, where the lack of physical equipment and technical resources impedes their ability to provide optimal care to patients with obesity. The absence of these essential resources further complicates the situation, negatively impacting the healthcare professionals' capacity to deliver best-practice care.
The synthesis also reveals that clients with obesity perceive several accommodations to be lacking, including gowns, as discussed earlier, and tables and equipment in general. This underscores the importance of comprehensive risk assessment before working with patients, regardless of their body size.
Safe Patient Handling Risk Assessment
- To reduce work-related injuries, a risk assessment can be completed prior to transferring a client with obesity. This includes assessing the following:
- The environment
- The client
- The healthcare worker
- Work organization (Libre Texts, 2020)
The importance of conducting a thorough risk assessment before working with a patient, particularly those with obesity, cannot be overstated. Various risk assessment tools are available, and a resource focusing on safe patient handling is provided at the end of this webinar.
Taking the time before entering the room or the home to assess key factors is crucial. This includes evaluating the environment, considering aspects such as available space, the involvement of family members, the suitability of chairs, and the presence of tubing or wires. A comprehensive assessment of the client's physical condition is essential, examining factors such as strength, balance, and the ability to sit unsupported on the edge of the bed. Testing manual muscle strength helps gauge the client's capabilities and informs the transfer approach.
Assessing the healthcare worker is equally important. Considering their experience level, familiarity with working with clients with obesity, and any personal perceptions or stigma is critical. Understanding the healthcare worker's background and mindset contributes to a more effective and collaborative approach.
Lastly, evaluating the work organization involves reviewing policies and procedures related to safe patient handling. This includes assessing the organization's support for using bariatric equipment and whether adequate time is allocated. Understanding the organizational culture and commitment to safe practices informs the overall risk assessment.
Bariatric Equipment Needed
- The evidence literature by Forhan (2008) displays that there are barriers to the accessibility of these necessary tools and that the potential for occupational therapy services is limited due to this, (Forhan, 2008). The research indicates that the bariatric population requires the following:
- specialty beds
- toilets
- shower benches
- adaptive equipment for activities of daily living
- large blood pressure cuffs
- bed levers
- leg lifters
- sliding sheets
- bariatric seating (Bakewell, 2007)
- space accommodations
- hallway accommodations
- bariatric wheelchairs
Forhan's evidence literature underscores the barriers and limited accessibility of necessary tools for occupational therapy services, particularly for the bariatric population. The research emphasizes the need for specialty equipment to address the unique requirements of individuals with obesity, including specialty beds, toilets, shower benches, and adaptive equipment for activities of daily living.
Specialty tools for the bariatric population include sock aids, bariatric toileting aids, lifters, long-handled sponges, and larger blood pressure cuffs. The study also delves into specialty bed levers, leg lifters, sliding sheets, airside transfer mats, bariatric seating, space accommodations, hallway accommodations, and bariatric wheelchairs. These tools play a crucial role in ensuring safe and effective care for individuals with obesity.
The research extends to nursing assistants' injuries and associated costs. Between 2009 and 2013, 122,000 nursing assistants reported musculoskeletal disorders in the U.S., making it the occupation with the highest number of such disorders. The estimated cost of these injuries amounted to $1.6 billion. Transferring and transporting patients, especially in wheelchairs or beds, contribute significantly to these injuries. Sudden stops and quick turns during transportation threaten healthcare workers' musculoskeletal health.
Recognizing the increasing demand for bariatric equipment, a study evaluated the effectiveness of a power drive feature in moving bariatric beds without manual effort from healthcare workers. This innovation aims to reduce the physical strain associated with manually moving bariatric beds, contributing to healthcare professionals' overall safety and well-being.
Bariatric Equipment Study
- “From 2009 to 2013, 122,000 nursing assistants reported musculoskeletal disorders in the US; more than any other occupation” (Wiggerman, 2017 p. 59).
- Estimated cost of these injuries are 1.6 billion dollars
- Often, this can be attributed to not only transferring the patient, but also transporting them around the hospital via wheelchair or bed.
- Various factors attribute to injury, such as sudden stops or quick turns. More so with a client with obesity (Wiggerman, 2017)
The study conducted by Wiggermann introduced a device designed to assist therapists in pushing beds without the need for manual effort. This device, equipped with a power drive feature, aimed to alleviate the physical strain typically associated with manually moving beds. The study involved a small sample size, comprising 10 participants who experienced both a manual bed and a bariatric bed equipped with the demonstrated powered drive feature.
- With the rise of more clients requiring bariatric equipment, such as a bariatric bed, a study was conducted to see the effectiveness of a powered drive feature to move the bed so this would not need to be done manually by a health care worker.
- The study had 10 participants with use of a manual bed and a bariatric bed with the powered drive feature.
- The author discovered that less pull and push force by the participant was used with use of the powered drive feature (Wiggerman, 2017)
The study by Wiggermann revealed that participants utilized less pull and push force when utilizing the powered drive feature on the bariatric bed than manually moving the bed. This finding suggests that incorporating such innovative features can significantly reduce the physical strain on healthcare professionals during routine activities, such as moving beds.
While the frequency of implementing these features in hospitals may vary, the study underscores the potential benefits of healthcare worker well-being and injury prevention. Including such features could be a proactive measure to mitigate the risk of musculoskeletal injuries associated with common tasks in patient care settings. The provided image offers a visual representation of this innovative powered drive feature.
Cost
- Due to the high associated cost of bariatric equipment, many facilities are also lacking the equipment prior to accepting a bariatric client making it a dilemma for the healthcare workers that are working with the individuals.
- For instance, the cost of a bariatric bed is $8,900 compared to an average bed costing $3,000. (N.S.W Nurses & Midwives' Association, 2011).
- The standard cost of an average patient’s room, including furniture, costs approximately $24,000.
- Comparatively, a bariatric size room costs approximately $55,000 indicating a significant difference. (The Advisory Board Company, 2014)
The costs associated with bariatric equipment pose a significant challenge for many healthcare facilities, leading to a dilemma where patients are accepted before ensuring the availability of suitable equipment. This financial consideration influences decision-making processes within facilities. For instance, a bariatric bed can cost around $8,900, a substantial increase compared to the average hospital bed, which costs approximately $3,000. Similarly, the standard cost of furnishing an average patient's room is around $24,000, while a bariatric-sized room costs approximately $55,000, nearly double the standard cost.
These financial considerations impact the ability of hospitals and SNFs to become designated bariatric centers of excellence. While there is an increasing desire to accommodate bariatric patients, the high costs associated with specialized equipment and facilities can create barriers.
Case Studies: Marie and Carl
Moving on to treatment, we will discuss three case studies: Carl, Marie, and Carson. Carl, we'll see him in a hospital; Marie, we'll see her in her home; and Carson, we'll see him between home and school.
Marie
- Marie is a 75-year-old woman diagnosed with morbid obesity, endometrial cancer, hypertension, type II diabetes, incontinence, gallbladder disease, anxiety, history of sexual abuse, and depression. She was just discharged home from the hospital after having two blood transfusions due to severe anemia. She currently has a stage III wound under her inner skin folds. She lives with her husband in a single-family home, who suffered a stroke two years ago and is wheelchair-bound. Her prior level of function was ambulating with a walker, assisting her husband with ADLs/IADLs, driving, and she was independent with all ADLs. She currently is unable to transfer alone, ambulate, or complete any ADLs, making her primarily bed-bound. She has three children: one who is incarcerated, a supportive daughter, and a son who she has a difficult relationship with as he feels his parents should be in a nursing home. When you evaluate her, she is depressed and not motivated to work with you. She voices that the treatment she received at the hospital was different than other patients, and she feels that all “healthcare workers are the same.”
Marie, a 75-year-old woman, presents a complex case with multiple comorbidities, including morbid obesity, endometrial cancer, hypertension, type two diabetes, incontinence, gallbladder disease, anxiety, and a history of sexual abuse. She has recently been discharged from the hospital after receiving two blood transfusions due to severe anemia. Currently, she faces challenges such as a stage three wound under her inner skin folds. Marie resides in a single-family home with her wheelchair-bound husband, who suffered a stroke two years ago. Her recent decline in health has left her primarily bedbound, unable to transfer independently, ambulate, or perform instrumental activities of daily living (IADLs). This is a notable change from her prior level of function, where she was ambulating with a walker, assisting her husband with ADLs and IADLs, driving, and maintaining independence with all ADLs.
Marie's social dynamics add further complexity to her situation. She has three children, with one currently incarcerated. She has a supportive daughter, but her relationship with her son is strained, as he believes his parents should be in a nursing home.
Upon evaluation, Marie expresses feelings of depression and lacks motivation to engage in therapy. She attributes her reluctance to work with healthcare professionals to a perceived difference in treatment during her hospital stay, leading her to believe that all healthcare workers are the same.
The multifaceted nature of Marie's health issues, combined with the challenging family dynamics and her psychological state, requires a comprehensive and tailored treatment approach to address her physical and emotional well-being.
Carl
- Carl is a 58-year-old male who just underwent bariatric surgery and is being seen in the step-down unit at the hospital. His comorbidities are as follows: morbid obesity, depression, binge eating disorder, night eating syndrome, hypertension, sleep apnea, gallbladder disease, and type II diabetes. He currently has a stage II sacral wound. He lives alone in an apartment building complex and has a pet pug. His prior level of function was that he could transfer from his wheelchair to his bed and/or toilet with the use of a walker, but he was not safe in doing so. He works as a computer designer and recently had to stop due to medical limitations. He has a supportive sister who is available to assist him, but she is highly anxious about his needs and how he will continue living alone to support himself. When you approach him at his hospital bed, he is unengaged and self-conscious as the current gown he is wearing is too small for him. He does not want to bathe or get up today because he feels he does not have the equipment he needs to do so.
Carl, a 58-year-old male, has recently undergone bariatric surgery and is currently in the step-down unit at the hospital. His list of comorbidities includes morbid obesity, depression, binge eating disorder, night eating syndrome, hypertension, sleep apnea, gallbladder disease, and type two diabetes. A stage two sacral wound further complicates his health situation. Carl resides alone in an apartment complex and shares his living space with a pet pug. His previous level of function involved transferring from his wheelchair to his bed or toilet with the assistance of a walker, though it was not a safe practice. He previously worked as a computer designer but had to discontinue due to medical limitations.
Carl's support system includes a supportive sister, but she expresses high anxiety about his needs and his ability to continue living alone and self-supporting. Upon approaching him at his hospital bed, Carl appears unengaged and self-conscious, exacerbated by the discomfort of wearing a gown that is too small for him. Additionally, he expresses reluctance to bathe or get up, citing a lack of necessary equipment.
This case highlights Carl's physical and psychological challenges post-bariatric surgery, as well as the need for a supportive environment and appropriate equipment to facilitate his recovery and daily activities. Developing a treatment plan must address both his physical limitations and emotional well-being, while also considering his sister's concerns and anxieties regarding his ability to live independently.
- Carson is a 12-year-old boy who lives with his parents, his 10-year-old sister Carla, and his grandmother. Carson weighs 125 lbs and is 56 inches in height, placing him in the 98th percentile compared to boys his age, and a calculated BMI of 26.9. Carson has been diagnosed with obesity by his pediatrician and is at risk for having obesity and other comorbidities as an adult. Carson's parents work full-time, and his grandmother cares for him and Carla after school. Carson's grandmother has difficulty walking far distances as she is awaiting hip replacement surgery. When Carson and Carla come home from school, she makes them a snack, and they have screen time after doing their homework. Recently, Carson has not wanted to go to school because he is getting bullied for his weight. Mom and Dad are concerned about his weight and his mental health.
Carson, a 12-year-old boy, resides with his parents, 10-year-old sister Carla, and his grandmother. Weighing 125 pounds and measuring 56 inches in height, Carson falls into the 98th percentile for boys his age, with a calculated BMI of 26.9. His pediatrician has diagnosed him with obesity, putting him at risk for potential comorbidities in adulthood. Both of Carson's parents work full-time, and his grandmother assumes caregiving responsibilities for him and Carla after school. However, she faces mobility challenges while awaiting hip replacement surgery.
After school, Carson and Carla are provided with snacks by their grandmother, followed by screen time after completing their homework. Recently, Carson has expressed reluctance to attend school due to bullying related to his weight. His parents are increasingly concerned not only about his physical health but also his mental well-being.
This case emphasizes the multifaceted challenges faced by Carson, encompassing physical health, potential comorbidities, family dynamics, and the impact of bullying on his mental health. Developing an effective treatment plan for Carson involves addressing both his weight-related concerns and the emotional toll of bullying, while also considering the family's schedule and the mobility constraints faced by his grandmother.
Treatment Strategies for Carl and Marie
We will start with reviewing treatment strategies for Carl and Marie, as shown in Figures 1 through 4. We'll then move on to Carson in the next section.
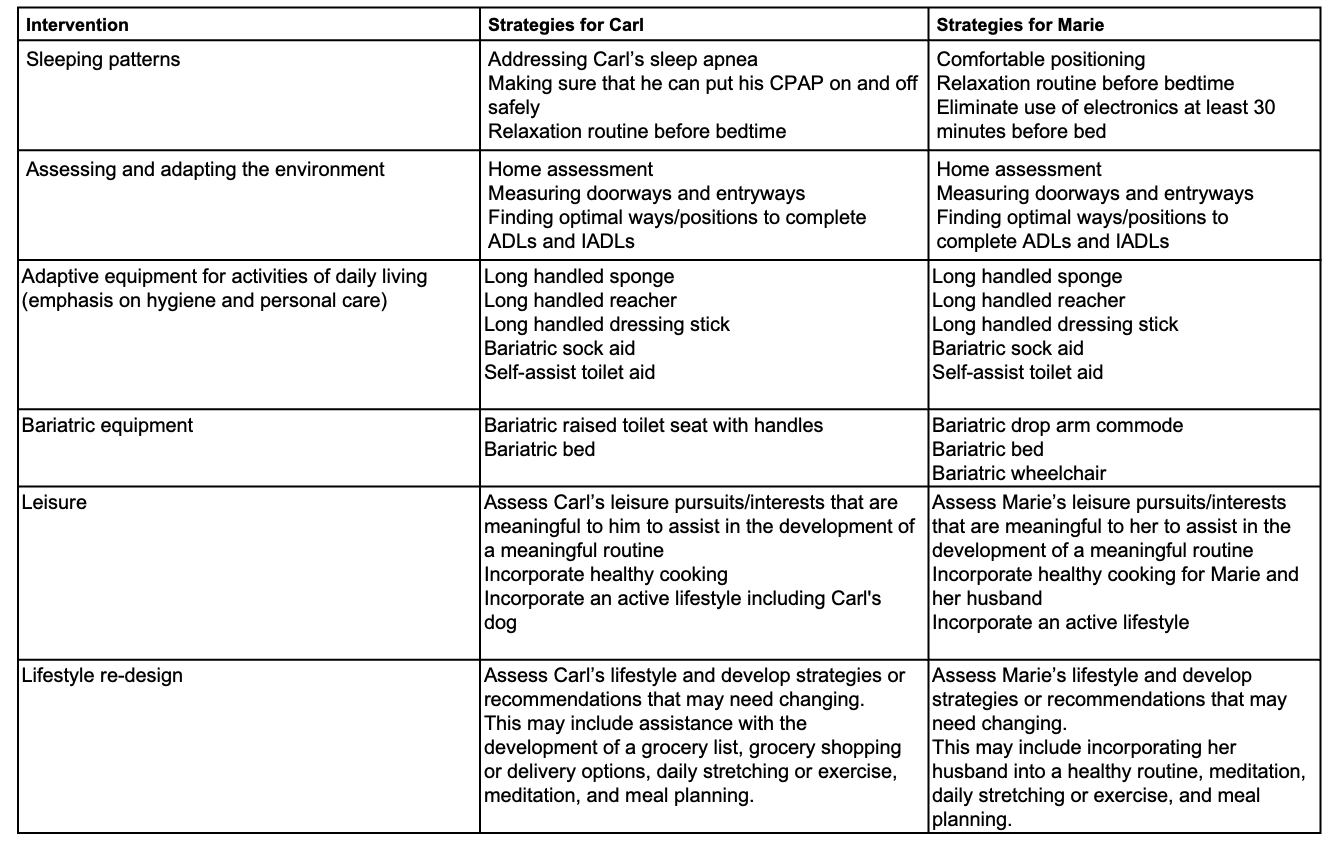
Figure 1. Treatment strategies for Carl and Marie, Chart 1. (Click here to enlarge the image.)
In formulating a comprehensive treatment approach for Carson, a 12-year-old boy grappling with obesity and facing bullying challenges, the strategy encompasses various facets of his well-being. The goal is to address both his physical health and mental resilience, acknowledging the impact of bullying on his overall quality of life.
Starting with Carson's physical health, a key focus is implementing a balanced and nutritious diet. The approach involves encouraging healthy eating habits, emphasizing portion control, and introducing nutritious snack options. Additionally, there's an emphasis on promoting regular physical activity tailored to Carson's preferences and considering any existing health conditions or comorbidities. This approach aims to foster a positive relationship with food and exercise, laying the foundation for a healthier lifestyle.
Simultaneously, attention is given to Carson's mental health and the challenges posed by bullying. Open communication channels are established to provide a safe space for him to express his feelings and experiences. Collaborating with the school, anti-bullying measures are put in place, and emotional support is offered. In some cases, involving a mental health professional may be considered to help Carson navigate and cope with the stress induced by bullying.
Family dynamics play a crucial role in the intervention. Parents are actively involved, contributing to a nurturing home environment. Resources and guidance are provided to address bullying concerns, and the focus is on supporting Carson's emotional well-being within the family context.
Education and empowerment are key components of the approach. Carson is educated about the importance of a healthy lifestyle without fostering a negative body image. Empowerment tools are provided to help him respond confidently to bullying situations, building resilience and self-esteem.
Recognizing the significance of peer and social support, efforts are made to facilitate positive peer interactions. This may involve group activities or support groups aimed at fostering a sense of belonging and camaraderie. Carson is encouraged to engage in activities aligned with his interests, contributing to positive social interactions.
Collaboration with the school is vital. Efforts are made to create a supportive environment by informing teachers about Carson's challenges and needs. Advocacy for inclusive practices and anti-bullying initiatives within the school community contributes to a holistic and supportive educational experience.
Regular health monitoring is integrated into the approach, ensuring Carson's physical well-being is consistently assessed. This proactive measure allows for the tracking of any changes or developments, with an emphasis on maintaining a positive attitude toward health and well-being.
In summary, the treatment approach for Carson is designed to be holistic, encompassing physical and mental health, family dynamics, education, empowerment, and social support. This approach aims to provide a comprehensive and effective intervention to enhance Carson's overall well-being through collaboration with parents, schools, and mental health professionals.
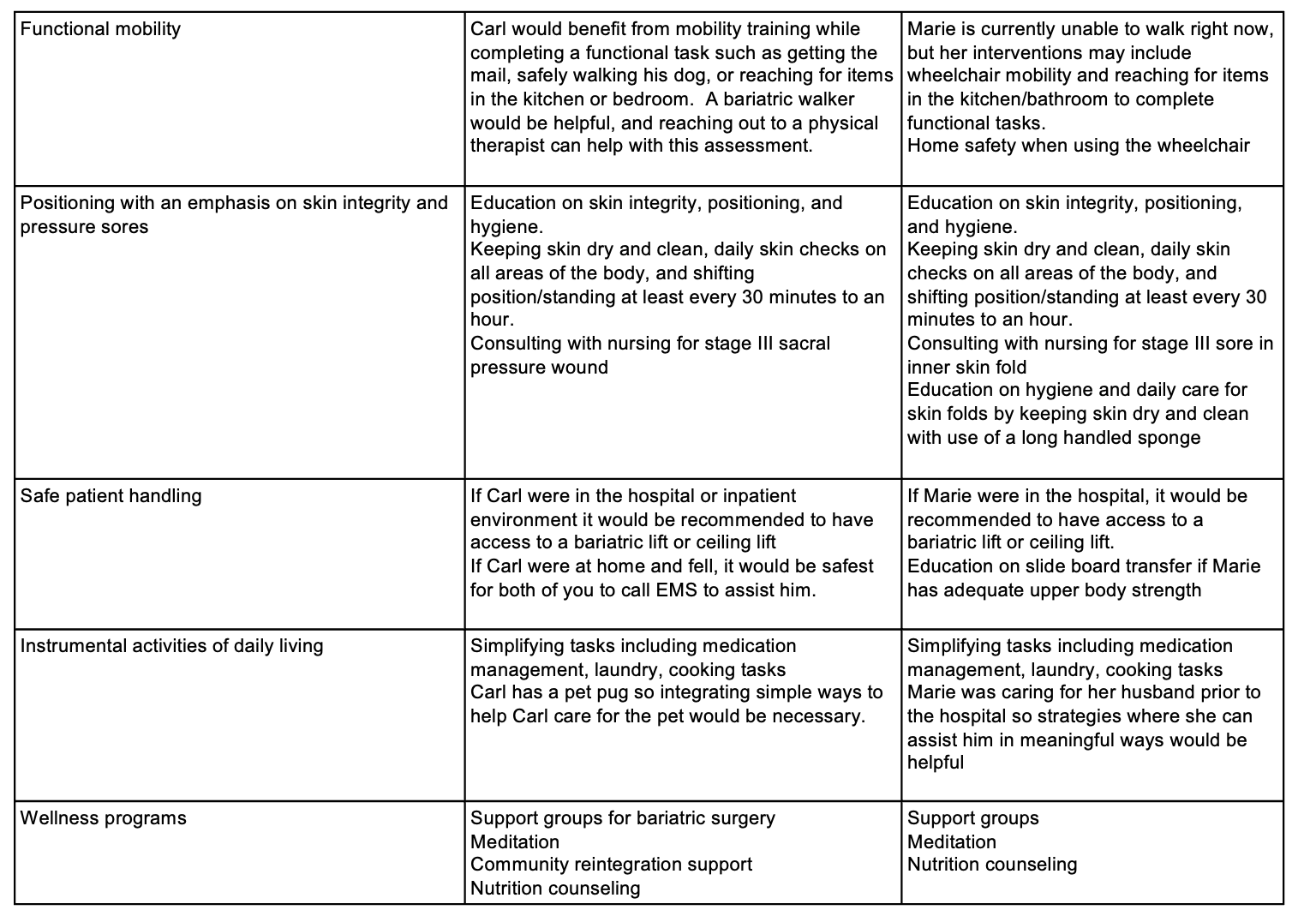
Figure 2. Treatment strategies for Carl and Marie, Chart 2. (Click here to enlarge the image.)
For Carl, incorporating functional tasks into his routine, such as getting the mail, walking or wheeling his dog, or reaching for items, becomes a pivotal part of his intervention plan. Introducing a bariatric walker and collaborating with a physical therapist further enhance his mobility assessment. As he transitions home, the support of a bariatric walker and the integration of functional tasks contribute to his overall well-being.
Marie, currently unable to walk, receives interventions focused on wheelchair mobility and performing tasks in the kitchen and bathroom. Home safety considerations become crucial, addressing challenges like doorways and accessibility. Emphasis on skin integrity and pressure sore prevention involves education, daily skin checks, and regular repositioning. Skin protection is prioritized with the use of an air-relieving mattress for her hospital bed. Collaboration with nursing is paramount for managing the stage three sacral pressure wound and ensuring appropriate care.
Safe patient handling measures are tailored to each individual. For Carl, accessing a bariatric or ceiling lift in an in-patient setting or calling EMS at home is recommended. Marie, with her strength considerations, receives education on sideboard transfers. Employing a risk assessment before handling tasks ensures patient and practitioner safety.
Instrumental activities of daily living (IADLs) involve simplifying tasks like medication management, laundry, and cooking for Carl and Marie. Integrating strategies for pet care, considering Carl's pug and Marie's responsibilities towards her husband, requires thoughtful planning and support.
Wellness programs focus on psychosocial aspects, including support groups for bariatric surgery, meditation, nutrition counseling, and community reintegration support. A holistic psychosocial approach is integrated into the care plans, considering Carl and Marie's unique needs and challenges.
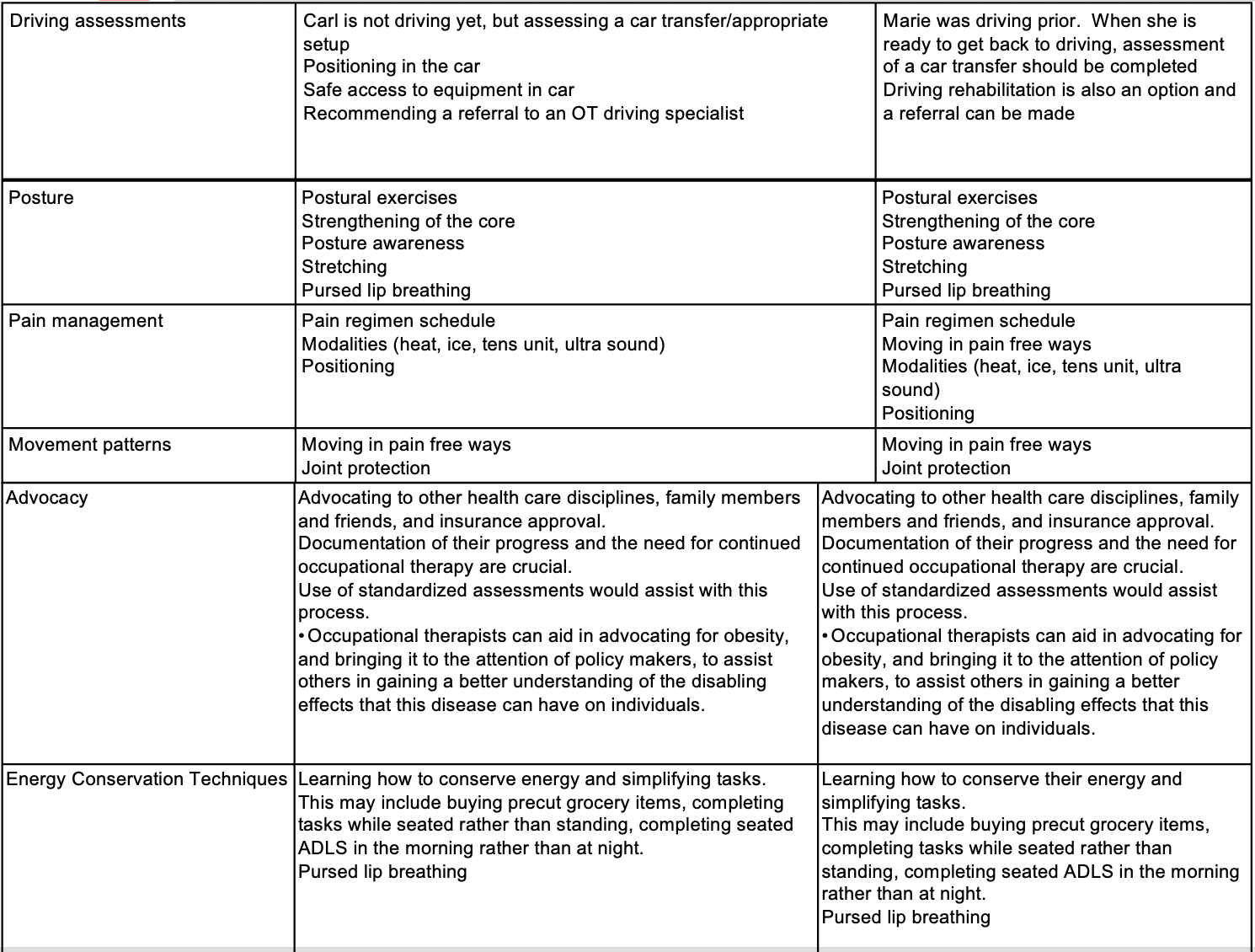
Figure 3. Treatment strategies for Carl and Marie, Chart 3. (Click here to enlarge the image).
For Carl and Marie, assessing their potential return to driving is significant. Even though Carl is not currently driving, evaluating a car transfer and ensuring safe access to the vehicle is essential. Referring an occupational therapist (OT) driving specialist can provide valuable insights. Similarly, when Marie is ready to resume driving, a referral to a driving specialist is recommended, and practicing car transfers can be beneficial, ensuring safety.
Posture exercises are crucial in maintaining skin integrity and core strength necessary for transfers. Incorporating postural awareness, core strengthening, stretching, and purse-lip breathing contributes to physical well-being and mental health. Pain management strategies are vital, including appropriate medication schedules and careful consideration of modalities. Focusing on comfortable positioning, assessing movement patterns, and suggesting pain-free ways to navigate their environments help protect joints and enhance mobility.
Advocacy is a pivotal role for healthcare professionals, especially in the context of clients with obesity. Collaborating with other healthcare disciplines, engaging family members, and advocating for insurance approvals for durable medical equipment (DME) become crucial. The use of standardized assessments aids in the advocacy process, ensuring proper support for individuals with obesity. Advocating for policies addressing obesity at the policy-making level contributes to creating an environment that supports the needs of these individuals.
Energy conservation techniques, such as preparing precut grocery items and organizing activities of daily living (ADLs) in the morning, help manage fatigue and optimize energy levels. These strategies aim to enhance Carl and Marie's overall well-being and functional independence.
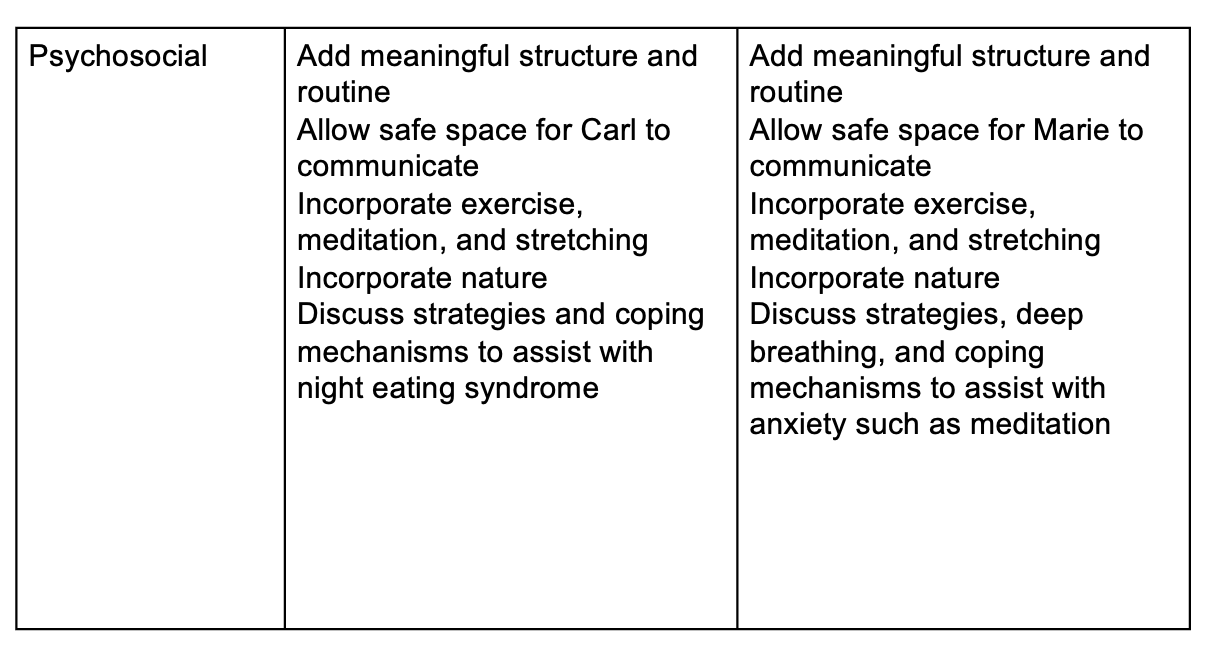
Figure 4. Treatment strategies for Carl and Marie, Chart 4.
A psychosocial approach is also important in developing a trusting relationship and adding meaningful structure and routine. This allows a safe space for both Carl and Marie to trust you and enjoy doing occupational therapy and trying to achieve the goals together.
Childhood Obesity and OT/Carson Case Study
- Family and occupation-based interventions (Orban, Erlandsson, Edberg, Onnerfalt, & Thorngren-Jerneck, 2014)
- Parents as positive role models for a healthy lifestyle
- Cooking as a family
- Physical activities that are adapted to the child (Reingold & Jordan, 2013)
- Exercising together
Addressing childhood obesity requires family-centered interventions, and in Carson's case, involving his parents, grandmother, and sister is crucial. Despite the grandmother's limited mobility, finding creative ways to engage the family in physical activities is essential. Implementing a structured routine after school, such as an exercise book or checklist, encourages regular physical activity for Carson and his sister.
Cooking as a family provides an opportunity to instill healthy eating habits. Including Carson in meal planning and preparation can promote a sense of responsibility and awareness about nutrition. Encouraging positive role modeling by parents sets the foundation for a supportive environment.
- Grocery shopping together and creating healthy grocery lists
- Implementing healthy family lifestyles
- Eating meals and snacks at the table
- Eating meals together as a family
- Spending more time together as a family
- Healthy sleeping habits and adequate sleep
- Implementing healthy beverages
Additional suggestions involve engaging in grocery shopping together and creating nutritious grocery lists. Implementing healthy family lifestyles includes emphasizing the importance of eating meals and snacks at the table, especially for Carla and Carson to avoid consuming snacks in front of screens. Encouraging family members to eat meals together fosters a sense of unity and has positive implications for overall health.
Prioritizing healthy sleeping habits and ensuring adequate sleep is crucial for Carson's well-being. Assessing Carson's current routine as an occupational therapist allows for tailored interventions that consider his unique needs and challenges. Implementing healthier beverage choices further contributes to promoting overall well-being.
- Parents spending more time with their children
- Implement a healthy lifestyle and physical activity at a young age
- Reduce screen time
- Wellness programs in the classroom and school environment (Sanders, 2015)
- Physical routine in the classroom
- Academic breaks throughout the day and around transition times
Introducing positive changes to routines and creating more meaningful activities for Carson and his family aligns with the occupational therapy approach. Focusing on implementing a healthy lifestyle and encouraging physical activity from a young age is essential. Reducing screen time is a crucial aspect of promoting overall well-being.
Wellness programs can be integrated within the classroom, and physical routines can be incorporated into the academic day, with breaks around transition times. These strategies aim to create a supportive environment considering Carson's unique needs.
Supporting Carson's parents in advocating for him at school is crucial, especially given his bullying challenges. Exploring possibilities such as implementing an anti-bullying program or incorporating education on childhood obesity could contribute to a more inclusive and supportive school environment. Activities like planting a school garden offer opportunities to introduce healthy food concepts and foster a positive relationship with nutrition.
- Increasing the child’s awareness of the body
- Healthy cooking group
- Nutrition education and healthy food and beverage choices (Reingold and Jordan, 2013).
Increasing Carson's awareness of his body and its nutritional needs is valuable in promoting a healthier lifestyle. Collaborating with a dietitian can provide essential insights into making informed food choices that fuel the body with energy. Introducing a healthy cooking group involving Carson, his sister, grandmother, parents, and friends can create a supportive environment for learning and practicing nutritious meal preparation.
Providing nutrition education on healthy food and beverage choices further empowers Carson to make positive decisions about his diet. These efforts aim to instill lifelong habits that contribute to his overall well-being.
- Encouraging co-occupations among the child and parent(s)
- Encouraging children to have various routes of self-expression, such as art/craft projects, to increase self-esteem and confidence
- Teaching children to use words such as “above average weight” rather than harmful words
- Advocacy for decreasing access to vending machines that have unhealthy food and beverage choices (Northrop, 2014)
Fostering co-occupations between Carson and his parents, such as engaging in weekend hikes or physical activities, can strengthen their family bond while promoting a healthier lifestyle. Encouraging diverse forms of self-expression, such as engaging in arts and crafts, contributes to building Carson's self-esteem and confidence.
Moreover, teaching children positive and neutral language, like "above average weight" instead of potentially harmful words, promotes a supportive and inclusive atmosphere. Language plays a crucial role in shaping perceptions, and using respectful terminology can help Carson develop a positive self-image.
Additionally, advocating for reducing access to vending machines that offer unhealthy food and beverage choices is crucial. Evaluating Carson's environment at home and school can provide a comprehensive understanding to implement effective changes.
- Single-family households have been associated with a higher BMI rate in children.
- Children who have experienced divorce, have a higher risk of obesity.
- Encouraging co-parenting.
- Meeting with each parent individually to establish healthy routines and occupations to keep the family and child healthy (Northrop, 2014)
I would like to share insights from a few studies that specifically highlight single-family households being associated with a higher BMI rate in children. Additionally, there's evidence indicating that children who have experienced divorce are at a higher risk of developing obesity. As occupational therapists, our role in such cases would involve encouraging co-parenting while meeting individually with each parent. This approach aims to establish healthy routines and enjoyable occupations for both parents, contributing to the overall health and well-being of the family and the child.
- Research has supported that fathers have an influence on a child’s eating patterns.
- Research has also documented that mothers tend to be more aware of what their child is eating (Salemonsen, Langeland, & Holm, 2023)
- It is important to incorporate both parents into OT treatment involving obesity.
This study highlights the importance of involving both parents in interventions for childhood obesity. Acknowledging the influence of fathers on a child's eating patterns and the heightened awareness of mothers regarding their child's diet is crucial information. As healthcare professionals, understanding and incorporating both parental perspectives in occupational therapy treatments for obesity is indeed essential for comprehensive and effective care. This approach ensures a more holistic understanding of the family dynamics and contributes to the overall success of the intervention.
- A study in Norway was conducted to research fathers’ perceptions of childhood obesity regarding their own children and preventing further weight gain to see how healthcare professionals can best support fathers in this role.
- Results indicated that fathers expressed “1) alternating between concern, helplessness, and responsibility, 2) Needing acknowledgment, and flexible and tailored professional support, (Salemonsen, Oma Langeland, & Lise Holm, 2023 p 4)
A study in Norway was conducted to research fathers' perceptions of childhood obesity regarding their own children and preventing further weight gain to see how healthcare professionals can best support fathers in this role.
- Fathers expressed:
- protecting their child’s self-esteem
- stigma
- trying to be sensitive to their child’s feelings
- worries of contributing to obesity
- worries of appearing shameful
- fear for their child and their health
- recognizing their own eating behaviors and noticing these behaviors in their child (Salemonsen, Oma Langeland, & Lise Holm, 2023)
The study results provide valuable insights into the multifaceted emotional experiences of fathers regarding childhood obesity. It's significant to note their alternating feelings of concern, helplessness, and responsibility, emphasizing the need for acknowledgment and flexible professional support.
The fathers' dedication to protecting their children's self-esteem, their sensitivity to the stigma associated with obesity, and their recognition of their role in modeling positive behaviors underscore the complexity of their involvement. Addressing their worries, fears, and self-awareness regarding eating behaviors is crucial for effective support.
As healthcare professionals, understanding these emotional nuances is key to tailoring interventions that resonate with fathers, fostering a positive and supportive environment for the child and the family. It reinforces the importance of a holistic approach in addressing childhood obesity within the family context.
- Fathers expressed that these feelings did hinder their ability to assist their child with obesity, and for losing weight as well as even speaking with their child about obesity.
- It also impacted their ability to say no to unhealthy food to their children as it appeared as a form of punishment (Salemonsen, Oma Langeland, & Lise Holm, 2023)
The fathers also expressed that their feelings did hinder their ability to assist their children with obesity and losing weight or even speaking about obesity to their children. Additionally, the fathers also expressed that it did impact their ability to say no to unhealthy food to their children as it appeared as a form of punishment.
- OT can assist fathers with:
- providing structure
- a healthy meal time and routine
- supporting fathers/parents in positive reinforcement and eliciting positive emotions
- supporting fathers/parents in being a positive role model
- supporting healthy occupations
- supporting positive mental health(Salemonsen, Oma Langeland, & Lise Holm, 2023)
I think OTs can assist fathers with providing structure, healthy mealtimes and routines, educating in positive reinforcement and emotions, and being a positive role model to support healthy occupations as well as mental health practices.
Video Resources
- Childhood obesity prevention through telehealth in schools
- https://www.youtube.com/watch?v=2T485z4d4dI
- Ceiling lift transfer
- https://www.youtube.com/watch?v=_bgCOOMYBDg
- Air slide/transfer mat
- https://www.google.com/search?q=airslide+for+lateral+transfer+you+tube&oq=airslide+for+lateral+transfer+you+tube&gs_lcrp=EgZjaHJvbWUyBggAEEUYOTIJCAEQIRgKGKABMgkIAhAhGAoYoAEyBwgDECEYjwLSAQg3MzQ3ajBqN6gCALACAA&sourceid=chrome&ie=UTF-8#fpstate=ive&vld=cid:e178ee28,vid:u0tjtK_4gOE,st:0
Here are some resources that may be helpful to you.
Risk Assessment Example
- https://med.libretexts.org/Bookshelves/Nursing/Clinical_Procedures_for_Safer_Patient_Care_(Doyle_and_McCutcheon)/03:_Safe_Patient_Handling_Positioning_and_Transfers/3.03:_Patient_Risk_Assessment
This is the link to the risk assessment.
Resources
- Resource with case studies about working with clients who have obesity and need bariatric care
- http://sizewise.com/clinical-education
- Resource for bariatric equipment
- https://www.safety.duke.edu/ergonomics/sphm/sphm-bariatric-resources
- Resource for ordering bariatric equipment
- https://www.amsdme.com/Catalog/Online-Catalog-Category/905/Bariatric-Equipment
- Resource for ordering bariatric equipment
- http://www.alimed.com/bariatrics/
Here are some resources on obesity and bariatric care, as well as some advocacy and support group links.
Summary
Thank you for joining me today. If you would like to reach out to me, please don't hesitate to do so at my email. I would love to hear from you.
References
Available in a separate handout.
Citation
Phillips, J.(2023). The bariatric client and the OT role, part 2. OccupationalTherapy.com, Article 5670. Available at www.occupationaltherapy.com
