Editor's note: This text-based course is a transcript of the webinar, Interdisciplinary Approach To Stroke Rehabilitation: Acute Care And Inpatient Rehabilitation Phase, presented by Alaena McCool, MS, OTR/L, CPAM, Katherine George, PT, DPT.
Learning Outcomes
- After this course, participants will be able to:
- Examine 3 appropriate assessments to use during an acute care OT and PT evaluation based on the patient’s diagnosis.
- Analyze at least 3 appropriate interventions during the inpatient rehabilitation phase based on the patient's diagnosis and presentation of symptoms.
- Recognize the importance of the interdisciplinary approach between physical and occupational therapy and discuss how to implement collaboration strategies during case studies.
Content/Introduction
- Disclosures
- Introduction
- Stroke Overview
- Case Study Introduction
- Acute Care Rehabilitation
- Inpatient Rehabilitation
- Literature Update
- Case Studies
- Questions and Answers
Today, we will discuss an overview of stroke, including the definitions and medical management, and review interdisciplinary approaches to stroke rehab in acute and inpatient phases. We will also apply case studies throughout the presentation.
Why are we here talking about an interdisciplinary approach? When professionals from multiple disciplines come together to create a care plan for a patient, each professional has a slightly different perspective based on their specialty. This can help create a more comprehensive care plan and optimize patients' recovery. From a patient's perspective, their care plan is more consistent and harmonious.
There is also a massive amount of literature discussing why early mobility is better for all types of patients, including those post-stroke. Early mobility is generally safe and effective in promoting better outcomes, shortened lengths of stay, and improved functional mobility. For example, disciplines can split up mobility tasks where OT is working on bed-level ADLs and transferring them to the chair so that the PT can work on standing and walking. They can also work together for evaluations and treatments utilizing two skilled sets of hands. In this way, they can focus on the client's quality of movement, which is very important in the neurological population.
Many populations benefit from energy conservation, including stroke patients, especially in acute cases. Combining PT and OT in one session may sometimes be all that a patient can tolerate.
From a time management perspective, clearing a patient for other disciplines saves time and money. Communicating a patient's response to your session can help another therapist prepare, saving time.
Stroke Definitions
- Ischemic Stroke (87% of strokes)
- Obstruction in cerebral vasculature prevents brain tissue from getting oxygen and nutrients, causing cell death.
- Hemorrhagic Stroke (13% of strokes)
- Blood vessel rupture or leakage causes blood to flow into brain tissue
(Tsao et al., 2022)
Let's review some definitions, so we are all on the same page here. Ischemic strokes are due to an obstruction in the vasculature preventing the brain tissue from getting oxygen and nutrients. These obstructions can include blood clots or fatty buildup.
Hemorrhagic strokes are due to blood vessel rupture or leakage causing blood flow into the brain tissue, which causes cell death. This can be due to aneurysms or weakness in the vessel wall, uncontrolled hypertension, and the overuse of medications like anticoagulants. Eighty-seven percent of all strokes are ischemic, and 13% are hemorrhagic. Hemorrhagic strokes are more severe and have worse outcomes than ischemic ones.
Common Presentations
Here are some common presentations in this chart.
Middle Cerebral Artery | •Largest vessel branching from internal carotid artery •Supplying large areas of the frontal/temporal/ parietal lobes and basal ganglia | •Contralateral strength and sensory loss in face/arms > legs •Contralateral homonymous hemianopia •Aphasia with L sided MCA strokes •Neglect with R sided MCA strokes |
Anterior Cerebral Artery (ACA) | •Branching from internal carotid artery •Supplies portions of the frontal and parietal lobes | •Contralateral strength and sensory loss in legs > arms •Confusion, delayed response times, memory deficits •Apraxia possible |
Posterior Cerebral Artery (PCA) | •Branches from basilar artery •Supplies occipital and temporal lobes, thalamus | •Visual deficits •Contralateral strength and sensory loss •Aphasia with L PCA strokes •Neglect with R PCA strokes |
Vertebral Arteries/ Basilar Artery | •Vertebral arteries join to form basilar artery •Supplies posterior portion of brain including cerebellum and brainstem | •Vertigo, visual deficits, and speech deficits, balance and coordination deficits, including ataxia with cerebellar strokes •Strength, sensation, vision, swallowing, breathing, and arousal deficits with brain stem strokes |
As with all neurological conditions, most clinical presentations do not fit into a nice little box. It is nice to have basic knowledge about what to expect to help guide your evaluation process and decision-making. This is a general overview of what you should have in your head when you complete a chart review.
Next, we will go over the stages of stroke, including more definitions for your reference.
Stages of Stroke
- Hyperacute: 0-24 hours
- Acute: 1-7 days
- Early Subacute: 7 days-3 months
- Late Subacute: 4-6 months
- Chronic: 6 months+
We will mainly address the hyperacute, acute, and early sub-acute phases during today's presentation.
Stroke Quick Facts
- “Leading cause of serious long-term disability”
- Global Incidence: 11.71 million people
- U.S. Incidence: ~ 795,000 people
(Tsao, 2022)
Stroke is the leading cause of serious long-term disability. The incidence rates of strokes in the US and globally are very high, and one in four stroke survivors will have another stroke in their lifetime. Those with recurrent strokes tend to have higher mortality rates and worse functional outcomes.
- Readmission Rates (Leppert et al., 2020)
- 12-17% readmitted within first 30 days
- Up to 50% readmitted within 1 year
- Rehab Needs (Almhdawi et al., 2016; Leppert et al., 2020)
- Two-thirds of all stroke survivors need rehabilitation
- More than 80% present with UE deficits and/or gait deficits
Up to 17% of stroke survivors are readmitted within the first 30 days, and up to 50% within one year. There are many different reasons for these readmissions, including falls, fractures, recurrent strokes, and other medical complications. Two-thirds of all stroke survivors need rehab, and more than 80% end up with upper extremity and/or gait deficits.
Introduction to Case Study J.K.
- J.K. is a 67-year-old female presenting after an unwitnessed fall with acute right MCA stroke, left shoulder hematoma, left 4th rib fracture, and left pneumothorax
This is an introduction to J.K. We will follow J.K. throughout her recovery, which spans parts one and two of this course series.
She is a 67-year-old female presenting after an unwitnessed fall with an acute right MCA ischemic stroke. She has a left shoulder hematoma, a left fourth rib fracture, and a left pneumothorax.
Acute Care Rehabilitation
Acute Care Overview
- Care Team
- Physicians
- Nurses
- Respiratory Therapists
- Case Manager/Social Worker
- Rehabilitation Services
- Dietician
- Patient and Family Members
- Pharmacists
- Palliative Care Specialist
- Stroke Recovery Group Liaison
Many professionals are involved in the care of a patient after a stroke, and these can vary by facility.
Ischemic Stroke Management
- Revascularization
- Intravenous Tissue Plasminogen Activator (IV-tPA)
- Endovascular Thrombectomy (EVT)
- Blood Pressure Management
- Cerebral Edema/Intracranial Pressure Management
Medical teams will focus on revascularization for an acute ischemic stroke using IV-tPA or intravenous tissue plasminogen activator. It can be used within three to four-and-a-half hours of the patient's last known normal. They also provide endovascular procedures such as thrombectomies, which is the removal of a thrombus, or thrombolysis, which is the delivery of TPA directly to the clot. These procedures can be performed up to 24 hours after the last known normal.
Medical professionals also manage blood pressure after an ischemic stroke, as they need to be high for adequate perfusion. Blood pressure goals can be less than or equal to 220 over 120 within the first 24 to 48 hours.
Cerebral edema management and intracranial pressure management are also used with this population, as there is an increased risk for cerebral edema after a hemispheric infarct. Surgical interventions, such as placing an external ventricular drain or a decompressive craniectomy in severe cases, can be used.
Additional medical management is going to include the prevention of complications in recurrent stroke during hospitalization using diagnostic imaging, seizure prophylaxis, and encouraging early mobility.
- Therapy Implications
- Therapy holds post IV-tPA and EVT
- Blood pressure goals
- Surgical precautions
- External ventricular drain precautions
Therapy implications with ischemic strokes include therapy holds after tPA for 24 hours and after endovascular procedures are common. They use the femoral artery to access the vasculature system resulting in "lie flat" orders. The time for a therapy hold after the different endovascular procedures depends on your facility.
Monitoring blood pressure during sessions is essential. If blood pressure goes too high, we can cause another stroke or hemorrhagic transformation of their current stroke. If blood pressure is too low, there may not be enough pressure for perfusion to the brain. Blood pressure goals are not universal, and many factors go into making them. We always want to defer to our medical team. As therapists, we need to ensure that we get individualized blood pressure goals to manage them appropriately during our sessions. When blood pressure goals are high, as we would expect with an ischemic stroke, we need to use our clinical judgment regarding the appropriateness of therapy. Just because the doctors have set a blood pressure goal to keep systolic pressures between 180 and 220 does not necessarily mean that it is appropriate to work with a patient with a resting blood pressure of 210 over 105, as blood pressure increases with activities. Discuss with the medical team to weigh the risks and benefits of early mobility in the acute phase with these patients.
Surgical precautions are going to include helmets for craniotomies. Additional precautions will depend on the facility and the surgeon performing the procedures.
An external ventricular drain (EVD) is a tool that can be used to measure intracranial pressures and drain cerebrospinal fluid (CSF) or blood to lower intracranial pressures if needed. When the drain is open and actively draining CSF or blood, mobilization is contraindicated. The EVD must be clamped for mobility.
Hemorrhagic Stroke Management
- Control Bleeding
- Intracranial Pressure Management
- Surgical Intervention
For acute hemorrhagic strokes, the medical team is going to work on controlling bleeding and preventing hemorrhagic expansion with blood pressure management and the use of medications, platelets, or fresh frozen plasma. Figure 1 shows an example of a hemorrhagic stroke.
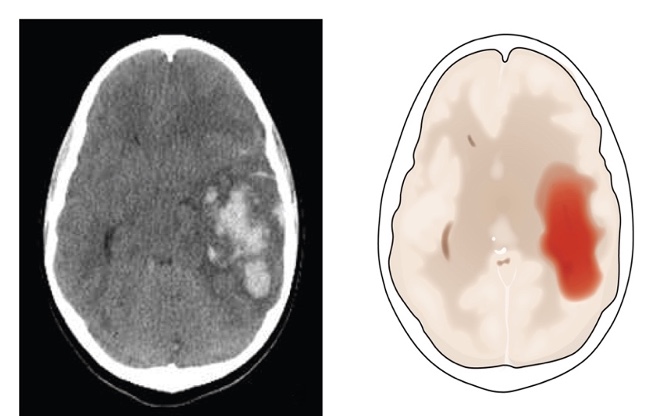
Figure 1. Examples of a hemorrhagic stroke on a scan.
There are typically strict blood pressure goals for these patients to prevent further bleeding. There are systolic goals of around 130 to 140.
Using EVDs or external ventricular drains to monitor and manage intracranial pressures after hemorrhagic strokes is associated with improved survival. You will see many patients with EVDs in neurologic ICUs.
There are surgical interventions to remove blood in the brain tissues and minimally invasive options such as burr holes. More invasive procedures, such as craniotomies and craniotomies, can be used depending on how much blood and where the blood is.
Additional medical management here will be the same for ischemic stroke and will include the prevention of complications and recurrent stroke during their hospital stay.
- Therapy Implications
- Blood pressure goals
- Surgical precautions
- External ventricular drain precautions
Therapy implications for a hemorrhagic stroke related to these medical procedures will include individualized blood pressure goals and constant blood pressure monitoring during sessions. Reduced blood pressure variability after hemorrhagic stroke has been shown to increase functional outcomes. We want to take extra precautions with this patient and keep their blood pressure within those recommended goals so as not to increase the risk of further bleeding.
Surgical precautions are similar to those for ischemic strokes, including using a helmet after craniotomies. Therapy holds will depend on the procedures that are being done.
Again, external ventricular drains must be clamped for mobility.
Acute Care Evaluation
- Medical Chart Review
- Patient Interview
- Objective Assessments
- Goal/Plan of Care
- Equipment/Orthotic Recommendations
- Discharge Planning
Alaena: We will discuss these topics for the acute care evaluation.
- Chart review
- Hospital Guidelines
- Lines and Tubes
- Diagnostic Imaging
- Past Medical History
- Hospital Course
- Precautions
The chart review starts with knowing your hospital guidelines, policies, and procedures. Guidelines can include the vital lab levels, vent settings, and when it is appropriate for us to go in and see the patient. Even if the labs are showing therapeutic, it is always important to talk to the nursing team to see if they are appropriate for therapy.
From the chart review, we will see the types of lines and tubes the patient has to better manage those. For example, if we know the patient has an EVD, we should check with nursing to see how their intracranial pressures are and if they can have the EVD clamped for treatment.
Diagnostic imaging includes X-rays, ultrasounds, MRIs, or CT scans. Due to the complexity of this population, sometimes things are missed by the medical team. For example, you may look at an x-ray and notice a potential scapular fracture. We need to reach out to the medical team to express our concerns. Our job is to not provide any more harm to this patient and to get them better.
The next one we will look at is past medical history like high blood pressure, strokes, surgeries, medical complexities, pain and pain tolerance, medications, and so on.
Lastly, we should know their precautions. Precautions can be specific to the surgeon if the patient has had surgery, but typically in this population, we will see the precautions that Katie previously discussed. If a patient receives tPA, they cannot participate in therapy for 24 hours post-thrombectomy, and there will be a lying flat order. Blood pressure parameters try to keep systolic below 140 to 160; however, this range may depend on a patient's medical history.
- Patient interview
- Include Family
- Home Setup
- Cognitive Assessment
- Prior Function Level
- Pain
The subjective patient interview should include family. You may ask the patient some questions, and family members can confirm that it is accurate. If the patient cannot provide information because of communication or cognitive issues, the family can provide that. If family members are not in the room, you go back into their chart post-session and try to contact the emergency contact number. If you still cannot contact them, the next step would be to reach out to a case manager to see if they have any information about the family.
The reason we want to do this is to confirm everything the patient is saying and have an accurate history of what the patient was doing before having the stroke. During this patient interview, we can learn about the home setup, including accessibility, like if there are any stairs to enter the house. We also want to determine family support.
Cognitive assessments can include informal questions like orientation and following commands or formal ones like the MOCA. We can also have the patient track objects in the room to see if there are any visual processing things going on. If at any time when doing these assessments, you suspect cognitive or communication deficits, a speech pathology referral may be indicated.
Prior level of functioning will include their ability to perform ADLs and IADLs, mobility, work, and leisure activities before the stroke.
Finally, if they are having pain or have a low pain tolerance, we can coordinate with nursing to have pain medication administered before our session.
Outcome Measures
Objective assessments will include range of motion, strength, ADLs, and mobility. However, the two lists show discipline-specific measures. We are not going to go through all of these, nor is this an exhaustive list of the assessments available. The assessments with the asterisks are highly recommended by StrokEDGE, Stroke Evidence Database to Guide Effectiveness, a template for measuring effectiveness and quality of evidence for outcome measures.
- Outcome Measures: OT
- Action Research Arm Test
- Box and Blocks Test
- Clock Drawing Test
- Modified Ashworth Scale
- Montreal Cognitive Assessment
- Motricity Index
- NIH Stroke Scale
- Orpington Prognostic Scale*
- Star Cancellation Test
- Stroke Rehabilitation Assessment of Movement*
- Outcome Measures: PT
- 5 Times Sit-to-Stand*
- 6-Minute Walk Test*
- 10–Meter Walk Test*
- Activities-Specific Balance Confidence Scale*
- Berg Balance Scale*
- Chedoke-McMaster Stroke Assessment
- Functional Gait Assessment
- Motricity Index
- NIH Stroke Scale
- Orpington Prognostic Scale*
- Postural Assessment Scale for Stroke Patients*
- Stroke Rehabilitation Assessment of Movement*
- Trunk Impairment Scale
https://www.neuropt.org/practice-resources/neurology-section-outcome-measures-recommendations/stroke
Above are the OT and PT lists. Again, we are not going to go through all of these, but rather we left these lists for your reference. The ones with the asterisks at the end are recommended through StrokEDGE and are the most up-to-date recent clinical practice guidelines.
Specialized Assessments
- Arousal
- Tone/Spasticity
- Sensation
- Coordination
- Visual Assessment
- Neglect/Inattention
- Sensory vs. motor vs. visual
- Cognition
Along with the OT and PT assessments, we are also going to look at other ones that are available specific to the stroke population to give a more accurate and thorough picture of the patient and capture what deficits are impairing their independence, ADLs, and mobility.
The first one up is for arousal. There are multiple assessments, with the more common one for acute care called the Glasgow Coma Scale or GCS. This is appropriate for a client with a low-level stroke and a way to show progress.
The next specialty assessment is for tone, and most likely, you will see PTs and OTs using something called the Modified Ashworth Scale. There is an upper and a lower extremity portion, and observations for synergistic patterns, clonus, and fixed posturing if noted. It is important to note that when you see anything out of the norm or these patterns, the focus should be on what impacts function.
For sensation, we look at proprioception, sharp/dull, discrimination, light touch, temperature, and stereognosis. Stereognosis is typically seen in lesions of the sensory cortex of the parietal lobe. Intact sensation is important for both function and safety. For example, if their sharp/dull discrimination is not intact when mobilizing, they can hurt themselves if they bump into something.
Coordination assessments can include testing for dysmetria, ataxia, tremors, and other movement disorders.
Visual assessments include visual acuity, an easy assessment to perform at the bedside. A therapist can have the client identify colors and numbers from items in the room, like a clock. Smooth pursuits, convergence, saccades, peripheral vision, and field testing can be tested by following a therapist's finger. Neglect and inattention can result from the sensory, motor, and visual issues.
Cognitive assessment includes tools like the MOCA (Montreal Cognitive Assessment), which can be assessed during ADLs or dual tasking during PT. It is important throughout all of these that you are collaborating with your counterpart. One discipline may see something, while the other may not. Depending on the time of day, a client may mask deficits easily, especially using different medications. By collaborating with your counterpart, you are going to obtain a fuller picture of the patient and be able to make the most appropriate recommendations for discharge while increasing that patient's independence.
Discharge Planning
- Functional Status
- Home Setup/Family Support
- Equipment Needs
- Services Required
- Collaborate
Discharge planning is going to start on day one. When making recommendations, you need to know if they are going to rehab (acute or subacute) versus home with outpatient therapies. Recommendations should also include understanding the client's current functional status related to ADLs, mobility, social factors, family support, and the home setup.
We need to know the accessibility of the home and available equipment, whether basic, like a sock aide, or something more complex, like a stair lift or a Hoyer lift.
We also need to know what services are required at discharge, like OT, PT, or speech.
The medical team needs to collaborate with the case manager to ensure there is an accurate picture of the patient and what the best course of action is.
Interventions
- OT
- ADLs
- Vision/Cognition
- ROM/Strengthening
- Mobility
- Orthotics
- Patient/Family Education
- PT
- Mobility
- ROM/Strengthening
- Seating and Positioning
- Assistive Devices/DME
- Patient/Family Education
OTs focus on ADLs, vision, cognition, range of motion, strengthening, mobility, orthotics, and patient and family education. PT focuses on mobility, range of motion, and strengthening as well. They may also work on seating and positioning, assistive devices, DME, and patient and family education.
- Short Length of Stay
- Line Management
- Discharge Planning
- Communication
Interventions are limited by the length of stay. You may only get one session with a patient, which would include the assessment and intervention. With limited time, you would focus on the biggest deficit impeding the patient's independence. However, suppose you can get more than one session, especially for patients in the ICU. In that case, interventions can be tailored towards whatever the discharge recommendation is and the patient's needs. For example, if we say the patient can go home, OT may focus on ADLS and DME, and PT may focus on stair training and household ambulation. We both will focus on client and family education.
The interventions may also be limited by lines and tubes, as these must be managed at all times. For example, we may need permission from nursing to unplug IV lines before mobility. They may also have drainage tubes or other unseen lines. I like to take a safety pin and pin their gown where that line or drain is to keep an eye on it.
As we said before, the interventions are tailored toward discharge recommendations. The patient may present differently in the a.m. versus p.m., one day to the next, which may affect discharge. Thus, communication is key within the medical team, case managers, nursing, and therapy. When you are thinking of changing or updating a discharge recommendation, it is imperative to have conversations with your counterpart to see if they agree. You also want to contact the case manager as soon as possible to make sure that there will be no issues with insurance or rehab bed availability. Working together and educating them about why you are changing the discharge recommendation will go a long way.
Other Considerations
- Policies and Procedures
- Complex Patients
- Insurance
Other considerations include hospital-specific policies and procedures, specifically in the ICU and early mobility. Knowing that some hospitals have a more conservative approach to therapy and working with people in the ICU is important. Based on the evidence, early mobility is key for better outcomes in this population. If you think rehab is not starting early enough in your facility, you may be able to advocate by presenting evidence to your rehab leadership.
With this population, there can be complex medical complexities, including contractures, comorbidities, and patients plateauing. The medical team may say a patient is too low-level, but in reality, the patient can do a lot. This is why communication is crucial. A chart review might not give an accurate description of what you see in the patient. On the opposite side of the spectrum, you may have a patient in such a fragile state that therapy is on hold. Then when you go back in, they require a reevaluation and a new discharge recommendation. This change may require communicating with your counterpart and case manager and educating the family, especially if they are overwhelmed.
Lastly, insurance can affect discharge recommendations due to their inability to pay, or you may need to see a patient more frequently to justify specific recommendations to insurance. Some insurances require a note to be placed in the chart within 48 hours of discharge. Other things can happen, like the patient needing a procedure or rehab will not accept them because of insurance.
Interdisciplinary Approach
- Co-Evaluations/Co-Treatments
- Screening for Other Disciplines
- Communication
- Education
- Supporting Other Disciplines
An interdisciplinary approach in the acute care setting is beneficial for time management, multitasking in the session for line management and interviewing, and safety. Treating alongside your counterpart also allows you to see the bigger picture of the patient from an ADL and mobility perspective, which you might not be able to do alone.
Screening for other disciplines is key. We are part of a medical team, especially in the acute care setting. If you see significant upper extremity edema or it is red and warm to the touch, you should alert the other disciplines. Things can be missed, so having an extra set of eyes is important.
We also want to communicate clients' responses to our sessions, including their cognition, range of motion, strength, and equipment recommendations or mobility devices. We also want to instruct others in the proper donning and doffing and wear time of orthotics, along with education to family and patients. We can discuss our treatment approaches and implement other disciplines' ideas if appropriate.
The more education, the better, but we need to be mindful that in this setting, typically, the patient and family are still in the active phases of coping and may have selective hearing. We can work with our counterparts to simplify education to maximize patient outcomes.
We also need to think about how we can support other disciplines. Can we add anything to our sessions that would make a difference? For example, as the PT is transitioning a patient to the chair, could they work on some seated upright tolerance and prep for seated ADLs for OT? Could the OT incorporate standing during an ADL task? These small adjustments to our sessions might help the patients meet their goals faster.
Case Study J.K.
- J.K. is a 67-year-old female presenting after an unwitnessed fall with acute right MCA stroke, left shoulder hematoma, left 4th rib fracture, and left pneumothorax s/p chest tube placement and intubation.
- Received tPA, thrombectomy completed
- PMHx: CAD, HLD, HTN, GERD, anxiety, current smoker
- PT Eval Order
- Placed 2 days post-admission
- Is this patient medically appropriate for PT Eval?
- Is any other rehab discipline appropriate?
Going back to our case study, J.K. is a 67-year-old female presenting after an unwitnessed fall with acute right MCA stroke, left shoulder hematoma, left rib fracture, and left pneumothorax status post chest tube placement and intubation. She received tPA, and a thrombectomy was completed. She has a past medical history of coronary artery disease, hyperlipidemia, hypertension, GERD, and anxiety, and she is a current smoker. A PT eval order was placed in the chart two days post-admission.
When we go through these case studies today, we will pick out specific discussion points to start thinking about what you would do in this specific scenario. The first point is whether the patient is medically appropriate for a PT evaluation. The patient received tPA upon admission, and it has been greater than 24 hours. They had a thrombectomy yesterday and, per the medical team, needed to lie flat for six hours. Currently, we are past that window. We would call up to the floor to ensure the pain is controlled because of the chest tube placement. We would also talk to a respiratory therapist to see about any plans for extubation, plans about weaning the patient, and if they are stable on the vent.
If all the answers to the questions are yes, they are appropriate to be seen. The next question would be if there is an OT or speech eval placed. Due to a right MCA, this patient likely has left upper and lower extremity weakness, sensory loss, visual deficits, and inattention.
- PT/OT Co-Evaluation
- Why?
- Requires increased assistance for mobility and proper positioning
- Likely to have decreased activity tolerance and endurance
- Early and aggressive mobility
- Why?
We would also assess if the patient is appropriate for a co-eval. If a patient has left upper extremity weakness, neglect, inattention, and requires increased assistance for mobility and proper positioning, they would benefit from several people assisting. We may also expect high pain and anxiety due to that left shoulder hematoma, left rib fracture, and post-chest tube placement. When a patient is intubated, they typically have decreased activity tolerance and endurance, and this patient has been on bed rest on top of all of that for two days. Atrophy of muscles can happen quickly, even lying in bed for an extra hour a day. It is beneficial to mobilize this patient to prevent further effects.
- Patient Interview
- Objective Assessments
- Mobility and ADLs
Katie: Continuing to discuss J.K.'s case, we will discuss how to implement interdisciplinary components of her co-evaluation. First, we can coordinate duties during the patient interview for efficient time management and for the prevention of fatigue, as the patient needs energy for the rest of the evaluation. We want to condense things as much as possible here. To do that, one therapist can begin the patient interview. In contrast, the other therapist works on rearranging the room, collecting necessary equipment, and speaking to the family if they are available, as our patient is intubated. The patient interview will be limited, and we will rely on the family to supplement information.
We can communicate and share information, like range motion and strength, to prevent overlapping assessments, unnecessary pain, and patient fatigue. For example, the PT will assess lower extremity strength, range of motion, sensation, and coordination. At the same time, the OT performs these same assessments on the upper extremities, and they share the information as it is pertinent to the other discipline and not because PTs only look at legs and OTs only look at arms. We are saying the two disciplines do not need to do both. Working together on these assessments and communicating during them will be important for the patient.
Next, we can intertwine PT and OT functional assessments to efficiently use time and equipment, reduce position changes, and conserve energy. This method looks at everything in supine, seated, and standing that needs to be done. We can also assess mobility with ADLs, like transferring to a bedside commode instead of the chair or walking to the sink instead of simply taking a few steps, turning around, and getting back into bed. We can work together to get more done within a session.
Lastly, during mobility and ADL assessments, we can provide increased assistance during mobility to maximize energy conservation and increase function by using two sets of skilled hands, this is especially true with an intubated ICU client like J.K. You are not going to assess for a home discharge at this point. Instead, you are prioritizing early mobility for improved outcomes. Extra skilled hands can also allow us to focus on the quality of movement. As a patient is mobilizing, we can work on the positioning of the hemiparetic extremity. And during ADL tasks in a seated position, one of the therapists can focus on helping that patient maintain an upright seated posture.
Now that we have discussed all the ways to implement an interdisciplinary approach during a co-eval let's walk through an example using J.K.'s evaluation. When we walk in, J.K. is in bed. One of the therapists performs the patient interview while the other therapist rearranges the room and manages the lines in prep for mobility. We split up the objective assessments and complete those. The OT performs supine ADLs like washing of the face. We will work together on rolling and transitioning from supine to sitting. The OT can perform a seated ADL while the PT assesses and assists with sitting balance. We can finish any objective assessments here, completing vision or coordination testing. After this, we do a sit-to-stand trial assessing balance and strength to see if J.K. is appropriate for standing mobility or ADLs.
After this, she needs a rest break; if you were alone, you may have to do that supine. With the extra set of hands, she rests while seated, allowing her to do more things after her rest break. One therapist can position themselves in the back of the patient to give her a solid backrest and maintain good upright positioning, which is important for respiration and pain management. Remember, she has a chest tube and rib fracture and is mechanically ventilated, so her positioning will be crucial.
While one therapist supports her during her rest break, the other can perform passive range of motion interventions or set up the room for the next piece of the assessment. After she takes her long rest break, we ambulate her five feet to the bedside commode, where the OT can further assess her seated balance and provide patient education. We can then do a stand pivot transfer to the bedside chair to work on positioning before the end of our session. This is a good example of how working together and intertwining our assessments allowed us to do more with J.K., which will ultimately benefit her recovery.
Our co-eval findings are that she is alert and oriented times three. She lives alone in a multi-level home and has identified that her daughter may be able to help her after discharge. She was independent at baseline, but she currently requires a mod to max assist for most ADLs and mobility tasks. She has deficits in almost everything, including strength, range of motion, sensation, balance, endurance, coordination, and vision, and she has left inattention. As such, the most appropriate discharge is to an acute or inpatient rehab setting, depending on how she progresses during her stay. Her pain limited her overall tolerance to the session, and we did not know if her daughter could help her after discharge. Both of these things will influence which rehab discharge plan we make.
- Plan of Care/Discharge Planning
- Pain management
- Contact family
- Discharge recommendation
- Goals
J.K. has high pain during mobility, a nine out of 10, and a three out of 10 at rest in sitting. We need to come up with a plan for pain management so that this patient can fully participate in her therapies. We also need to talk to other treating disciplines about timing mobility and ADL sessions with pain meds.
Contacting the family is important here. We need to figure out if assistance is going to be available since it is going to impact what discharge recommendation we make. We find out that her daughter will be able to live with her when she returns home.
J.K. was independent at baseline, is motivated, and her family will assist when she goes home. She could tolerate a 55-minute evaluation vented in an ICU, which is great. We do not have to have finalized discharge recommendations for this patient, but it is looking like acute rehab may be the way to go for her.
- Examples of Possible OT Goals:
- Patient will locate 3 items needed for toothbrushing task with items placed in all visual fields on a table with mod verbal cues to scan visual field as needed.
- Patient and caregiver will be educated and perform daily UE ROM without verbal cues to maintain ROM needed for dressing tasks.
- Patient will complete full upper body dressing task in supported sit with min A.
- Patient will sit EOB with supervision for 1 min without loss of balance in prep for seated ADL tasks.
- How Can PT Help Facilitate These OT Goals?
- Incorporate seated static and dynamic balance tasks in between mobility tasks
- Ongoing education, initiating techniques and cueing for L-sided attention during all tasks
- Perform exercises in a sitting position to work on endurance and sitting balance
- Check in with patient and caregiver to see if they are completing exercise programs
Some possible examples of OT goals include locating items needed for toothbrushing tasks using scanning techniques, performing an upper extremity range of motion program, completing an upper body dressing task, and increasing her static sitting balance in prep for seated ADLs.
PT can facilitate these goals by incorporating seated balance tasks throughout their session, educating her on techniques for scanning the environment during mobility and cueing her for left-sided attention during all tasks. When working on therapeutic exercises, the PT can have her perform them in a seated position to work on the patient's balance and endurance. And lastly, PTs can facilitate OT goals by checking in with her to see how she is doing with her home exercise programs and notifying OT of any issues.
- Examples of Possible PT Goals:
- Patient will perform supine <> sit toward R side, HOB flat and no bedrails, CG A and min cues or less for L UE management.
- Patient will perform sit <> stand using LRAD with CG A, min cues or less for L UE management.
- Patient will perform SPT toward L side with LRAD, mod A and mod cues or less for attention to L side.
- Patient will ambulate 15ft with LRAD and min A, mod cues or less for sequencing and attention to L side.
- How Can OT Help Facilitate These PT Goals?
- When transitioning to EOB for seated ADLs, practice toward R side with HOB flat
- Bring same AD to session when planning to work on standing ADL tasks or transfers
- Ongoing education, initiating techniques, and cueing for L-sided attention during all tasks
- Set up room so patient practices SPT toward L side when working on commode transfers/toileting
PT goals for J.K. include performing supine to sit towards the right edge of the bed, performing sit-to-stand transitions using the least restrictive assisted device, performing stand pivot transfers toward the left side, and ambulating with the least restrictive assisted device. OT can facilitate these PT goals by purposefully transitioning the patient toward the right edge of the bed when getting her up to work on seated ADLs or even purposefully transferring toward the left side when working on commode transfers. Also, the OT can help by bringing the same assisted device that the patient has been working on with PT to their sessions when planning to do standing ADLs or transfers. Lastly, the OT can continue educating the patient surrounding left inattention and trialing new techniques for the patient to maximize outcomes in both disciplines.
When we are talking about these goal slides, these are all examples. Each discipline should plan its session to help the client meet their goals and not focus on the other's agenda; however, having goals that align with the other discipline makes sense for the client. Being mindful of the patient's goals for other disciplines helps us build opportunities to increase the client's independence. These are small changes that are not disruptive but may help them to further meet their goals with the other discipline.
Inpatient Rehabilitation
We will now move into the nuts and bolts of the inpatient rehab phase.
Acute Vs. Subacute
- Acute
- Higher intensity and frequency of therapy
- Frequent physician involvement
- Shorter stays
- Subacute
- Lower intensity and frequency of therapy
- Less physician involvement
- Longer stays
Acute and general rehab centers have a higher intensity, more therapy, increased physician involvement, and shorter stays. Subacute rehabs have lower intensity and frequency of therapy. Typically, the session length is based on tolerance, and there are longer stays.
Inpatient Rehabilitation Overview
- Care Team
- Doctors/Physiatrists
- Nurses
- Case Manager/Social Worker
- Respiratory Therapy
- Rehabilitation Services
- Neuropsychiatry
- Psychologists
- Recreational Therapy
- Patient and Family Members
- Art or Music Therapy
Here is an overview of the care teams, which can vary based on the facility. Some have more, and some have less. It is important to know your care team members so that you can connect patients with them as appropriate.
Ongoing Medical Management
- Blood Pressure
- Pain Management
- Nutrition
- Mental Health
- Stroke Prevention
Medical management remains a very large part of their care in the inpatient rehab phase. Controlling blood pressure to prevent additional strokes, managing pain so that they can fully participate in their therapies, and ensuring that they are getting the appropriate nutrition to support the healing process are all part of medical management. Monitoring and screening for mental health concerns is another critical area. Lastly, we want to educate the client and family on stroke prevention and address habits like smoking, sedentary lifestyles, and unhealthy diets. This education also includes the medical management of risk factors like high blood pressure, obesity, and hyperglycemia.
Inpatient Rehab Evaluation
- Medical Chart Review
- Patient Interview
- Objective Assessments
- Goals/Plan of Care
- Equipment/Orthotic Recommendations
- Discharge Planning
The basic evaluation will look the same in all settings for PTs and OTs, but we focus on certain aspects in different settings. In the inpatient rehab phase, we will focus on the home setup and thorough assessments of impairments and functional deficits, which will drive our discharge planning.
Outcome Measures
Here are the outcome measures.
- OT:
- 9 Hole Peg Test
- Action Reach Arm Test
- Arm Motor Ability Test
- Assessment of Life Habits
- Box and Blocks Test
- Dynamometry
- Executive Function Performance Evaluation
- Fugl-Meyer Assessment of Motor Performance*
- Functional Independence Measure*
- Kettle Test
- Modified Ashworth Scale
- Orpington Prognostic Scale*
- Stroke Rehabilitation Assessment of Movement*
- Motor Activity Log-28
- Motor Evaluation Scale for Arm in Stroke Patients
- Motricity Index
- Short Form-36
- Wolf Motor Function Test
- PT:
- 5 Times Sit-to-Stand*
- 6-Minute Walk Test*
- 10–Meter Walk Test*
- Activities-Specific Balance Confidence Scale*
- Balance Evaluation Systems Test
- Berg Balance Scale*
- Chedoke-McMaster Stroke Assessment
- Fugl-Meyer Assessment of Motor Performance*
- Functional Gait Assessment*
- Functional Independence Measure*
- Motricity Index
- Orpington Prognostic Scale*
- Postural Assessment Scale for Stroke Patients*
- Rivermead Motor Assessment
- Stroke Rehabilitation Assessment of Movement*
- Trunk Impairment Scale
https://www.neuropt.org/practice-resources/neurology-section-outcome-measures-recommendations/stroke
Again, this is not an exhaustive list, but we left it here for your reference. The ones with an asterisk are highly recommended by StrokEdge, and we have provided the reference.
Functional Independence Measure (FIM)
- 18-item standardized test performed at admission and discharge
- Scored on an ordinal scale (1-7)
- Cognition Subscale
- Comprehension
- Expression
- Social Interaction
- Problem-solving
- Memory
- Motor Subscale
- Eating
- Grooming
- Bathing
- Dressing
- Toileting
- Bladder/Bowel Management
- Transfers
- Walk/Wheelchair
- Stairs
Here is an overview of the Functional Independence Measure (FIM). It is an outcome measure most commonly used in acute rehab. This is a breakdown of what it is and how it works. It is at least performed during eval and discharge in acute rehab settings, sometimes more depending on the facility. It captures aspects of cognition, ADLs, and mobility.
Interventions
- Motor Recovery
- Traditional approach
- Sensory stimulation
Alaena: As Katie said, the goal of our inpatient rehab is to get the patient home as independently and safely as possible by progressing deficits, educating the family, and increasing strength, with a special focus on ADLs from OT and mobility from PT.
Traditionally, this is accomplished by motor training, including strength training, range of motion, and mass practice to improve outcomes in stroke patients. However, what we know now is that sensory processing and integration are impaired in the stroke population, and this limits motor recovery. Consideration of these sensory deficits and limitations is important when treating this population.
Motor training is also not purely motor. Movement is the integration of motor and sensory information, so the next few slides will focus on the sensory stimulation approach, which consists of a combination of approaches to load the nervous system in multiple ways to get the most optimal outcome. All of these approaches are utilized by OTs and PTs, and as we go through them, we will highlight how we may use them a little differently within this setting.
First, we have sensory stimulation approaches. This is not a comprehensive list of therapeutic interventions but a summary of what we will focus on today. These interventions are used all the time by therapists, but we want to highlight them here to be intentional when choosing interventions with this population.
Sensory Stimulation
- Somatosensory Approaches
- Electrical stimulation
- Manual interventions
- Constraint-induced movement therapy
- Balance and postural training
- Visual Approaches
- Visual feedback/mirror therapy
- Addressing field loss or neglect
- Auditory Approaches
- Rhythmic stimulation
- Vestibular Approaches
- Reaching, gaze stabilization, balance, and postural training
- Multisensory Approaches
- Virtual reality
- Robotic-assisted training
- Combinations
Stroke patients have impairments in sensation and sensory integration. Sensory stimulation includes somatosensory, visual, auditory, vestibular, and multisensory approaches. In the following areas, we will break them down, including how PT versus OT can use them to obtain different outcomes. We will also discuss how they can work together to achieve optimal outcomes for the patient.
- Somatosensory Approaches
- Electrical Stimulation
- Manual Interventions
- Constraint-Induced Movement Therapy
- Balance and Postural Training
- Weight Bearing
For somatosensory approaches, we will discuss electrical stimulation, manual interventions, constraint-induced movement therapy (CIMT), balance and postural training, and weight bearing.
Electrical stimulation (e-stim) actively stimulates the paralyzed or affected muscle to get a certain response like increased strengthening or awareness. This can include a neuromuscular or sensory response. You can also use electrical stimulation with a functional task, which is recommended for both therapies. You might hear people call this a functional electrical stimulation approach. It should be used as an adjunct to other interventions.
An example is self-eating because it is a great task to break down and grade appropriately. We can stimulate muscle contraction on the affected bicep using a trigger. This means I am setting the stim up using certain parameters, frequencies, and pulse widths to get the muscle to do what I want it to do. Part of a self-eating task is bringing your hand towards your mouth. We can incorporate the electrical stimulation in elbow flexion and extension or a feeding activity that incorporates holding a spoon and bringing it to their mouth. PT could use functional stimulation differently, like with a Bioness FES, which is more of a robotic device.
We will talk a little bit more about e-stim in part two, but PTs often come out of school able to use them. In contrast, OTs may need to be certified to use electrical stimulation.
Next is manual interventions that combine interventions to improve sensory and positional awareness. It can be achieved through Proprioceptive Neuromuscular Facilitation (PNF) strategies, sensory reeducation such as vibration, and manual facilitations such as massage, stroking, or tapping.
Constraint-Induced Movement Therapy (CIMT) is an intervention to improve the use of the affected limb by restricting the unaffected one by using a glove, a mitt, a splint, etc. We will talk more about this intervention in part two of this series.
Balance and postural training increase sensory and positional awareness of the body. It includes different static and dynamic balance positions both in sitting and standing.
Weight-bearing will be discussed in more detail in a moment.
- Visual Approaches
- Visual Biofeedback
- Mirror therapy
- Addressing Field Loss or Neglect
- Visual Biofeedback
One visual approach is using biofeedback. This is getting feedback and using your vision using multiple devices. It can be as simple as having the patient intentionally watch a task being performed by a therapist and imitating it back, called learning by observing. It could also be the patient doing a task in front of the mirror and getting real-time feedback, or it could involve a higher-level device. For example, a device called a Vector™ gives an EMG reading.
Let's go back to that self-feeding example. You would put electrodes onto the client's bicep, and the machine picks up any EMG readings from the neurons within that muscle belly. So, if I ask the patient to contract, even if I do not see movement, the machine will pick up those readings. The therapist can create the threshold. When they hit the threshold, the stim turns on, and they get a full motor contraction.
When addressing field loss or neglect, research is very scarce, and most recommend using compensatory strategies.
- Auditory Approaches
- Rhythmic Stimulation
- Auditory Biofeedback
Auditory approaches are next, and this includes rhythmic stimulation and auditory biofeedback. Rhythmic stimulation uses music or another type of rhythm, like a metronome, during gait training to improve stride length and velocity. There is research on using the upper extremity with rhythmic stimulation, but again, research is scarce in that area. One way you could use it is by having a patient perform a bilateral upper extremity task while seated. The idea is to have the patient attend to their affected side.
Auditory biofeedback may enhance motor learning. We can add a sound to help them recognize correct or incorrect motor activities and positions. For example, during OT, I am trying to bring awareness to their left upper extremity during a bimanual task. I could place a bell on that hand for an auditory cue as they are doing a task or a balance activity with PT using a Wii Fit Balance Board. Or every time the patient is not weight-shifting appropriately, PT hits a buzzer so they know they must correct themselves.
- Vestibular Approaches
- Reaching
- Navigation
- Gaze Stabilization
- Balance and Postural Training
The vestibular system is associated with gait speed, balance, independence, wheelchair mobility, and reaching. As an OT, we do not learn much about vestibular training during our schooling. When I notice vestibular deficits, I collaborate with my PT or another senior therapist to fully understand how to address this central vestibular issue and go from there.
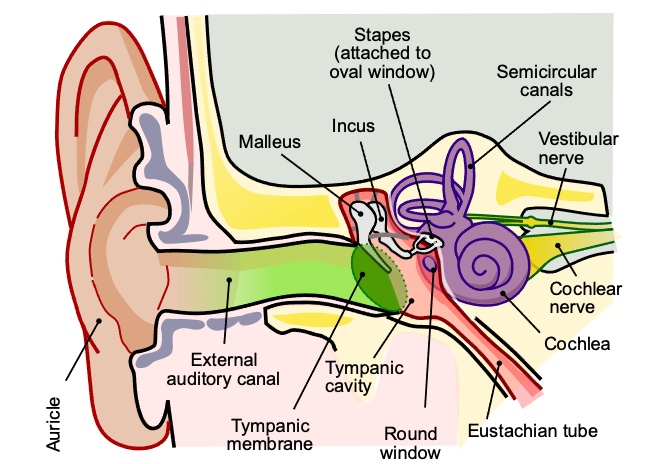
Figure 2. An overview of the inner ear.
- Multisensory Approaches
- Virtual Reality
- Robotic-Assisted Training
- Biofeedback
- Combinations
- Balance and postural training
A multisensory approach combines sensory reintegration using virtual reality, robot-assisted training, and biofeedback.
Virtual reality can improve upper or lower motor function, balance, mobility, and ADLs. However, it must be used with usual care, meaning it should not be the only thing in your treatment plan. You could add some e-stim or balance training while doing this activity. It also should not be done in every single treatment plan.
Robot-assisted training can be used to see improvements in balance, upper and lower extremity function, and midline perception. This intervention will be discussed more in detail in part two of this presentation. There are many robot-assisted options for OTs and PTs. Selecting the right one that is right for your clinic is important.
We have already discussed biofeedback and some of its applications.
Lastly, we can look at a combination of these approaches. For example, in balance and postal training, we use a combination of somatosensory, visual, and vestibular systems.
Weight Bearing
- Bone Mineral Density
- Sensory Retraining
- Balance and Postural Stability
- Spasticity and ROM
- Strengthen Muscles
- Improved Functional Performance
Now, we will take a deeper look into weight bearing. Weight-bearing has many benefits, including bone mineral density, sensory retraining, balance and postural stability, decreasing spasticity, increasing range of motion, strengthening muscles, and improving functional performance.
Increasing bone mineral density is vital because, in this population, there is an accelerated development of osteoporosis combined with high fall risk post-stroke. Due to decreased mobility and hemiparesis, disuse is a problem post-stroke.
Sensory retraining is important to bring awareness to joint subluxation through approximation and weight bearing.
Improper weight bearing leads to postural instability and sway. Bilateral weight bearing through the limbs increases strength.
Weight-bearing can also counteract dominant flexor synergy or spasticity to improve functional performance.
Figure 3 shows me in my clinic. Weight-bearing is applying pressure through the upper and lower extremities in various positions.

Figure 3. Weight-bearing in quadruped.
You could have the client complete weight-bearing prone on extended arms or with forearms propped, posterior prone sitting, anterior or lateral weight-bearing on walls, or while sitting, in quadruped, tall knee, or standing. Therapists can achieve these positions using different equipment. For example, during OT, if I do have an extra set of hands and have someone who cannot keep their elbow extended or follow directions, I may use some of the equipment and positions shown in Figure 4.

Figure 4. Different positions for weight-bearing through the arms.
As you can see in the very first one on the left, there is a slight asymmetry in the shoulders. We could get the patient into prone with a foam pad to assist with positioning.
Next, we are looking at a quadruped position, using a knee immobilizer on the left arm due to instability or weakness. You could also use e-stim to help. This allows a therapist to free up their hands to focus on approximating the shoulder joint or weight-shifting right and left at their hips.
Lastly, the last image shows weight-bearing through the forearms. Let's say we have a patient with an unstable wrist or pain in their arm. This position can get the same benefits of shoulder approximation. This prone position is also good for stretching flexor synergy patterns at the hips.
Katie: From a PT perspective, we will use weight-bearing tasks for the same purposes as OTs for strengthening muscles, sensory retraining, balance, and postural stability. Weight-bearing tasks can be performed in various positions depending on your patient's deficits and goals.
Looking at Figure 5, we can use these different positions.

Figure 5. More weight-bearing positions.
Using a ball or something underneath the patient to support their trunk allows the patient to focus more on their positioning versus simply holding themselves up in this position. In the middle, this patient seems to be leaning into the ball, looking for more support, which means that her knees are not underneath her hips. This is an ineffective position to work on weight-bearing. We may need to get a bigger ball or something more supportive to allow her to achieve the optimal position of her knees underneath her hips.
The far right image shows the client shifting her weight toward her strong side and away from her hemiparetic or weak side. We may need to facilitate a good weight shift toward the impaired extremity for strengthing and sensory input.
Task-Specific Training
- Principles
- Motor learning
- Experience-dependent neuroplasticity
- Shaping technique
- Example
- Self-feeding task
Alaena: Task-specific training has three principles, including motor learning, experience-dependent neuroplasticity, and shaping techniques. Motor learning refers to permanent changes in behavior because of practice and experience or the actual task at hand.
Experience-dependent neuroplasticity is the ability of the brain to reorganize itself in response to practicing a task, which includes varying environments and components of the task during other exercises or activities.
Shaping is a training method in which a motor or behavioral objective is approached in small steps by successive approximations. The task is made progressively more demanding as the patient's abilities enhance.
We are seeing much more in the research for task-specific training with OTs. Figure 6 shows an example of this with self-feeding.

Figure 6. Self-feeding task.
First, we look at the components of self-feeding, including reaching, grasping, grasp and release, elbow flexion, extension, supination, and pronation. We can start with the patient working on hand-to-mouth patterns and progress to cutting the food. She uses a universal cuff for the fork and curved plate, and her unaffected arm cuts. She also has a wrist brace and is practicing reaching. We could grade this activity by having her stand.
Gait Training
- High-Intensity Training
- Treadmill vs. Overground
- Body Weight Support
- Sensory Stimulation
- Improving Physical Activity
- FES and AFOs
Katie: The level of ambulation following stroke is a long-term predictor of participation and disability. We will talk about this more in part two of this presentation as there is so much research coming out about high-intensity training It is said to lead to improvements in gait speed, strength, and even outcome measures such as the Berg or the Six-Minute Walk Test when compared to traditional gait training.
Let's break down what we mean by high-intensity and traditional training. High-intensity training means mass locomotor practice at high aerobic intensities or 70 to 85% of age-predicted max heart rate for 45 to 60-minute sessions. In contrast, traditional gait training in an inpatient rehab setting averages only about 250 steps per session, with less than 5% of all sessions meeting recommended aerobic exercise thresholds. With high-intensity training, patients average thousands of steps per session. It is quite a big difference. Incorporating high-intensity gait training into your treatment plan for stroke patients is highly recommended throughout the literature.
Outcomes for treadmill and overground training are the same. You may see more improvements in gait speed using treadmill training. The use of body weight support during gait training benefits the stroke population. Still, it should not be used exclusively as the literature does not really support it as a primary treatment method.
Improving overall physical activity during non-therapy times has been shown to promote recovery of gait independence within the first-month post-stroke. Thus, it is important to work with your facilities to keep these patients active during non-therapy times, like with activity groups or wheelchair "walks" around the building.
The use of functional e-stim and AFOs are associated with improved muscle strength, increased gait speed, improved foot and ankle positioning during the gait cycle, improved dynamic balance and walking endurance, and improved overall mobility in patients post-stroke. We must think about recovery versus compensation when discussing functional e-stim and AFOs. Functional e-stim, such as the Bioness and walking aids, are mostly therapeutic and will promote motor recovery.
AFOs are typically chosen mostly as a compensatory strategy. However, research shows that the less restrictive AFOs can have therapeutic benefits by allowing for the activation of the gastrocnemius soleus and tibialis anterior.
In the acute and subacute phases of stroke recovery, we will choose interventions that promote the recovery of function. In the chronic phase, we use our clinical judgment based on the patient's presentation to decide whether we are promoting continued recovery or compensation.
Barriers
- Spasticity
- Contractures
- Movement Disorders
- Cognition
- Caregiver Support
- Home Setup
- Coping/Mental Health
Alaena: Now, we will touch upon barriers to discharge and intervention. We will look at the majority of these barriers, including spasticity, contracture, movement disorders, cognition, caregiver support, and home setup, in part two.
- Coping and Mental Health
- Coping (Rapoliene et al., 2018)
- More than 50% of survivors remain temporarily or permanently disabled
- Only 20% of survivors return to work
- Motivation affects outcome
- Depression (Tsao et al., 2022)
- Approximately 1/3 of stroke survivors
- Highest frequency in 1st-year post-stroke
- Associated with higher mortality and worsening function
- Coping (Rapoliene et al., 2018)
The one we will focus on today is coping and mental health. It is important to note that during an inpatient stay, the patient is still in the early days of a stroke. Depending on their length of stay in the acute care setting and the resources and support available, the patient and family may still be trying to process what this new diagnosis means for them or their loved ones.
Coping has five stages: denial, anger, bargaining, depression, and acceptance. As providers, we must be mindful of where that patient and family members are in the coping process, especially as we prepare them for discharge. Their coping stage is reflected in the goals and interventions. In general, we need to do a better job of addressing mental health at this stage of rehab. They may be angry, anxious, or depressed.
Here are some statistics. More than 50% of survivors remain temporarily or permanently disabled, and only 20% return to work. Throughout the literature, motivation is determined to affect mental health outcomes, especially depression. And approximately a third of stroke survivors are diagnosed with depression. We see the highest frequency of depression in the first year, which is associated with higher mortality and worsening function.
To help with this, we need to build positive relationships with the client, which has shown to be effective. We also need to educate the patient to address post-rehab uncertainty, even if it is a difficult conversation to have with them. We want the patient to become a specialist in their care by advocating and assisting in the therapy process. You can give them simple choices of what to do for the day or a "home" program they can do in their room. They can then educate the family on how to perform it.
Empowering and motivating patients has a huge impact on their overall care. We can provide specific feedback on actual improvements instead of the deficits. This patient has been in acute care, and now they are coming to an inpatient hearing, "It is going to be difficult to do XYZ when you go home." We want to highlight what they are doing well as this will have a huge impact on their psyche.
Lastly, we want to advocate for the patient by referring them to services through their medical team, like social work and neuropsych. A rehab hospital may have support groups or one-to-one peer interactions. Sometimes, it is easier to talk about what is going on with one person, especially someone who has been through it, versus a whole group. Be mindful that these patients are the experts in their care. Just because we see stroke patients, we do not know what they are going through. Finding someone to talk through things and discuss strategies will have a huge impact on their outcomes.
Literature Update
- Critical Window
- Enhanced neuroplasticity triggered by injury
- Largest functional gains in first 3-6 months post-injury
- CPASS study
- Gains in chronic stroke
- Enhanced neuroplasticity triggered by injury
The literature discusses neuroplasticity and the critical window timeline. This window is when the patient is going to make the most gains. This is constantly being researched and has changed throughout the years. Typically, the largest gains have a three to six-month mark. We can see gains from the chronic stroke population, but they are lower and not as intense. What we do not know is if these slower gains are because they are not in intense rehab or if this is just how the trajectory of that stroke diagnosis will go.
A current study called CPASS is moving into phase two clinical trials. It focuses on the upper extremity motor recovery and looks at intense therapy in the early acute care phase to see if this provides the most optimal outcomes. These neuroplasticity studies are crucial to know if gains can be made throughout this diagnosis.
Interdisciplinary Approach
- Co-Treatments
- Screening for Other Disciplines
- Communication
- Education
- Supporting Other Disciplines
To wrap up, we will look at the overall interdisciplinary approaches in in-patient care as they are necessary and beneficial. We know that co-treats are rarer in this setting, but sometimes they are needed.
We can screen for other disciplines and refer to them, like social work or psych.
In the setting, there is more of a focus on rehab services, so medical communication is super important. We can also observe our clients in different environments with our counterparts. We can support each other by talking through scheduling conflicts, goals of care, equipment recommendations, and how to don and doff different orthotic devices. Let's say PT goes on a community outing with patients. They can report how that patient navigated obstacles, reached for objects, or performed cognitively. Vice versa, if OT takes a patient out for a community outing, OTs can then communicate to the PTs on mobility, stair climbing, et cetera. Another example is that if PT sees patients in the morning, but the OT needs to work on ADLs, they may be able to switch times.
The next area is the education of the patient and family, again being mindful of their coping. We need to meet them where they are and provide an appropriate education for them right now. Some literature shows that carryover of home rehab programs is typically done when three or fewer exercises are included. We need to think of these same principles when educating families and patients. We must prioritize what we want them to hear for carry-over.
Lastly, we want to incorporate other disciplines' goals into our interventions to achieve optimal client benefits.
Case Study J.K.
- J.K. was discharged to acute rehab 12 days post-stroke. Hospital course complicated by respiratory status 2/2 PTX, intubated x6 days, and chest tube x10 days. Discharged on 2L 02
- Patient’s daughter will become primary caregiver and live with patient upon discharge. She can only take 2 weeks of leave from work
- A&Ox4, follows 2-step commands consistently, requires cueing for L inattention
- Mod to max A for all seated and bed-level ADLs
- CG/min A for sitting balance
- Mod/max A for transfers/gait with left lean
J.K. was discharged to acute rehab 12 days post-stroke. The hospital course was complicated due to her having a pneumothorax, being intubated for six days, and having a chest tube for 10 days. She was also discharged on two liters of oxygen.
We now know that the patient's daughter will become the primary caregiver and live with the patient upon discharge. However, she can only take two weeks of leave from work.
The patient is now alert and oriented times four and can follow 2-step commands consistently. They require cueing for left inattention, mod to max assist for all seated and bed level ADLs, contact guard to min assist for sitting balance, and mod to max assist for transfers and the gait with a left lean. In the acute care setting, J.K. had three OT and four PT sessions. Not much has changed from that acute care except for mild improvement in activity tolerance, balance, pain, and range of motion. Since not much has changed from the acute care to the inpatient setting, we will not go through a whole evaluation.
Case Study J.K. Goals
- Examples of Possible OT Goals:
- Patient will complete full upper body dressing task with min A.
- Patient will attend and use left UE for 75% of meal prep activity with 2 verbal cues as needed.
- Patient will be able to reach towards target with left UE in 2 out 5 trials accurately while in side-lying to increase strength needed for ADL and community reintegration.
- Patient will perform bed mobility with supervision to inc. independence needed for ADL tasks.
- How Can PT Help Facilitate These OT Goals?
- L UE approximation and use of L UE during tasks
- Reinforcing OT technique when putting on jacket or changing clothes
- Scapular PNF for proximal strength and stability
- Focus on bed mobility technique when transitioning on/off mat for exercises
Above are examples of OT goals and how PT may be able to support.
- Examples of Possible PT Goals:
- Patient will perform supine <> sit from R EOB independently with HOB flat and no bed rails.
- Patient will perform SPT toward both R and L sides from various height surfaces using SBQC requiring supervision, min cues for safety and L inattention.
- Patient will ambulate 100ft with SBQC and CG A, min cues for L inattention.
- Patient will ambulate over and around static obstacles in path with CG A using SBQC, mod cues or less for attention to L side.
- How Can OT Help Facilitate These PT Goals?
- Practicing SPT toward L side when working on commode transfers/toileting
- Bed mobility practice and techniques, practice bed mobility on/off mat
- Incorporate standing endurance and balance tasks such as standing ADLs into session
- Refrain from setting up environment prior to walking to the bathroom, try gift shop/cafeteria
Katie: These are examples of PT goals and how OTs can support them.
Case Study J.K. Interventions
- OT Interventions
- ADL Training
- Strengthening
- Vision Strategies
- Fine Motor Interventions
- Reaching
These are a few interventions that the OT used in J.K.'s case, working on strength, fine motor, and reaching using sensory motor approaches such as robot-assisted activities, e-stim, constraint-induced movement therapy, and mirror therapy. They worked on visual strategies such as techniques for left inattention, scanning the environment, and making checklists to ensure that the patient collected all the items needed for an ADL task, like toothbrushing. They also used a sticker on the patient's arm to improve attention during mobility and ADL tasks.
Ways that PT supported the OTs interventions include working on transfers, seated balance, and standing balance, and encouraging the use of the upper extremity, such as reaching for the bedrail and reinforcing the visual strategies implemented by the OT so that the patient gets more practice.
- PT Interventions
- Targeted Strengthening
- FES + High-Intensity Gait Training
- Obstacle Course
- VR for Balance
- Mobility Training
Again, this is not a complete list of PT interventions, but these are some areas to highlight. PT used therapeutic exercise with e-stim and PNF patterns and combined functional EIM with high-intensity gait training. They also used obstacle courses for balance and to reinforce left inattention during dynamic tasks and balance training with a VR device. They also worked in quadruped and tall kneeling positions for weight bearing and mobility training to address bed mobility transfers and stairs.
Ideas for ways the OT can assist with PT interventions include cueing for equal weight bearing during standing activities and using ADLs to work on static and dynamic balance. Of course, it is important to use the same assistive device that the patient has been working on with PT when performing transfers, standing ADLs, and continuing to work on strategies for vision and left inattention. As we've said previously, co-treatments in the acute rehab setting are certainly less frequent than in acute care, but there are scenarios where co-treats are appropriate.
- Co-Treatment Example
Let's talk about an example of a situation where a co-treat would be appropriate for a patient like J.K. The OT working with a patient has been trying to progress standing ADLs, but J.K. has not progressed much. She keeps losing her balance, her left knee buckles, and she cannot keep herself in an upright position long enough to complete an ADL. The OT looks through the recent PT notes to see what the PT has been working on and notices that PT has been working heavily on standing, balance, and gait using high-intensity gait training. She reaches out to PT to discuss the discrepancies of why the patient is doing so well with these standing activities in PT and not OT. They decide to work together to progress the standing ADLs for this patient. This is a great example of a time when a co-treat can benefit a patient.
Much is going on during a standing ADL task. For a standing ADL, they use an elevated table. The OT focuses on ADL activity, facilitating upper extremity coordination and motor control. In contrast, the PT focuses on balance and positioning, facilitating equal weight bearing and cueing to keep the left knee straight throughout the task. They may need to modify the ADL task if the task is too hard and advance as able.
Case Studies
Now, we will review four additional case studies.
Case Study 1
- Eval Findings in Acute Care
- Eye-opening but weak/fatigues easily, vertical and horizontal eye movements
- Minimal R cervical rotation in gravity eliminated plane, trace R upper trap contraction
- Communication established via eye movements when therapist holds eyes open
- A&Ox3 (name, place, time)
- Diagnosis: Locked-in Syndrome (incomplete form)
- Discussion Points
- Functional expectations
- Therapy goals
- Discharge planning
Case study number one is a 42-year-old male status post bilateral pontine infarcts. He initially presented with a Glasgow Coma Scale (GCS) of three, and the medical team deferred a therapy evaluation pending a family meeting about the goals of care. After a week, the family elects to trach and PEG the patient, and therapy orders are placed. Due to staffing, therapy cannot get in to eval this patient for another five days. The patient has begun opening his eyes when sedation is lowered. The medical team states that the patient is not doing anything other than opening his eyes, and they suspect locked-in syndrome.
Here are some discussion points. Is this patient appropriate for a PT/OT eval? When we are talking about a locked-in syndrome, the answer is yes. He may be a good candidate for a co-evaluation as he will have very low activity tolerance. We may only be able to turn off the sedation once, depending on his medical status.
The next point is how do we evaluate this patient? First, we will remove any sedatives or drugs used for the patient that may cause sleepiness. We want him awake so that we can work with him and see if we can establish communication.
Next, we are going to educate this patient. If it is a locked-in syndrome, cognition is typically intact, and the patient is probably scared to death. Telling them where they are, what happened, and why you are there will be helpful. Typically, we will see if a client can follow commands like thumbs up, wiggling their arm, wiggling their toes, or lifting their arm, but this will not work with a patient with locked-in syndrome. We need to work on basics like opening and closing their eyes, holding their eyelids open, and asking the patient to look up and down. Since vertical eye movements are typically preserved with locked-in syndrome, we want to see if they can do it consistently. We also want to see if they have other movements in their face or neck. Once we know whether or not they can follow commands, we can try to establish communication in the form of eye blinking if they have enough motor control over their eyelids to do that consistently or look up and down with or without holding their eyes open. If you find a way to communicate with a patient like this, make sure you are communicating with the entire team and leaving a sign at the bedside so that the patient can start to be involved in their care. Lastly, performing any objective measures that are appropriate, like sensation, reflexes, and any voluntary movement.
We find that this patient can open his eyes but is weak and fatigues easily. Vertical and horizontal eye movements are intact. He has some right cervical rotation and some right upper trap contraction. He can communicate with eye movements when the therapist holds his eye open. He can open his eyes, but he fatigues, so the therapist has to assist. He is alert and oriented times three, and the medical team diagnoses him with an incomplete form of locked-in syndrome.
What are some functional expectations for this patient? First, we want him to have the ability to communicate and direct his care. He will likely be dependent on all of his ADLs and mobility, but he does have the potential to gain independence and wheelchair mobility. Some therapy goals for this patient include maintaining enough range of motion for function in case he regains any additional control and tolerance for an upright position so that he sits safely in a wheelchair. We are going to be discussing upright positioning more on the next slide.
We want to establish an efficient form of communication involving speech therapy and OT. We can work with the strength and balance he currently has to help him to maintain eye-opening for long enough to communicate, stay awake, and improve neck movements so that he can potentially use something like a head array for wheelchair mobility down the line.
We can educate the family on a range of motion program and functional expectations and goals.
For discharge planning, we need to know if the client has family support and the proper home set-up to support them. They may need intensive therapy to get back as much function as possible, so we most likely will discharge them to an inpatient or an acute rehab setting if possible.
- Inpatient Rehab Interdisciplinary Plan of Care
- Upright tolerance
- Seating and positioning
- Contracture prevention
- Strength/endurance
- Self-directing care
- Education
- Family training
If this patient goes to acute rehab, what will his plan of care look like? The first goal may be upright tolerance to progress sitting and functional mobility in a wheelchair. This patient is essentially presenting like a quadriplegic, so hemodynamic stability in an upright position will be an issue. We may use a tilt table, compression stockings or wraps, and a tilt-in-space wheelchair to reposition his legs above his heart if his blood pressure drops while upright.
We may look at contoured seating in the wheelchair for proper positioning and pressure relief, as well as the use of powered mobility and a head array in the future.
To prevent contractures, we want to maintain his range of motion within normal limits throughout his entire body. As we think about function, we want to prioritize areas like his neck to be able to use a head array and other devices. His upper extremities may also get back some movement using a modified joystick like a goal post. We want to maintain hip, knee, and ankle range of motion to use a mechanical lift for transfers and for proper seating in a wheelchair.
Increasing his strength and endurance is imperative to gain some ability to control his environment. Again, we want to increase strength in his eye muscles, neck, and upper traps for communication and potential independent mobility.
We can collaborate with speech therapy to reinforce communication techniques and have them start to direct their care. We can also educate the patient and family in all areas of care, including pressure relief, seating, range of motion, and the use of equipment. We also want to involve case management and social work to help transition to accessible housing and other community resources such as outpatient programs, support groups, wheelchair vendors, et cetera.
Overall, this patient is a great example of an interdisciplinary approach because every single part of his care is interdisciplinary and involves therapists working together.
Case Study 2
- 55-year-old male with PMHx of uncontrolled HTN and chronic back pain s/p basal ganglia ICH with hemorrhagic expansion to thalamus. Patient has significant deficits, including R UE/LE hemiplegia, memory deficits, and speech deficits. Patient is max A for all mobility, and therapy recommended discharge to SAR post co-evaluation.
- Discussion Points
- Why the co-eval?
- What are some goals and interventions?
- How can opposite discipline support?
- Progression and plan to change to recommendation?
- Discussion Points
Alaena: Case study number two involves a 55-year-old male with a pre-medical history of uncontrolled hypertension, chronic back pain, and a status post basal ganglia intracranial hemorrhage with expansion to the thalamus. Patient has significant deficits, including right upper extremity and lower extremity hemiplegia, memory deficits, and speech deficits. Patient is max A for all mobility. Since this is still in the acute care setting, therapy has recommended discharging to subacute post-evaluation.
We decided to do a co-eval because of limited activity tolerance and more thorough mobility and ADL assessment with extra skilled hands. They have right upper and lower hemiplegia and speech and memory deficits. As such, getting them to follow commands is most likely going to be an issue. This person also has chronic back pain, which could also be an issue.
What are some goals and interventions for the specific patient? We will work with the patient and family to determine appropriate discharge recommendations. We need to determine if the family is available and if they are willing to provide the care. We also need to educate them about the rehab process and plan our goals accordingly to prepare for this transition.
OT interventions include range of motion, strengthening, ADLs at bed level and at the edge of the bed, and cognitive assessment. PT can be working on strength and range of motion as well and maybe some sit-to-stands from a chair to have a more stable surface.
Co-treats may be more appropriate to progress mobility and transfers to increase arousal and function. They may coordinate care where the PT gets the client out of bed using sit-to-stand equipment, and then the OT works with the client at chair level. The OT may also provide an orthosis, and PT can help reinforce the proper use and positioning during their sessions.
As this patient is in the early days of the acute care setting, we may recommend discharge to a subacute setting based on what we are seeing today; however, if they have good family support and the potential to progress, we may reassess our recommendation. We can also coordinate with the nurses to see if they can get the patient out of bed more frequently.
- Patient was in the hospital long enough to progress to acute inpatient rehabilitation. His therapy team has identified some barriers to progress and discharge.
- Discussion Points
- Patient is always in bed when not in therapy
- Significant time required for transitions, limiting intervention time
- Family will be taking patient home with 24/7 caregiver assistance, however not available during therapy times
- Discussion Points
This patient was in the hospital long enough to progress to inpatient rehab, but his therapy team identified some barriers to progress and discharge. He was always in bed. To combat this, we could try more co-treats at the beginning or back-to-back scheduling. We can also coordinate with nursing to get this patient out of bed in the morning and in the afternoon. We could also post a schedule on the wall, so the patient knows what is happening.
Another problem is that significant time is required for transitions, which limits intervention time. We can increase the patient's endurance to tolerate more time in the chair. OT can then focus more on seated balance activities, and PT does the standing activities to get more bang for our buck.
Lastly, the family has decided to go against therapy recommendations and take the patient home, but they are unavailable at therapy times or training. We could communicate and train other disciplines regarding techniques and cueing and leave a home rehab program. If all else fails, we can see if a case manager can let the family know how important it is for them to get training. The family may still be trying to copy and not fully understand what it means to be a caregiver.
Case study three and case study four are for you to reflect upon and brainstorm some of the things that we mentioned in the discussion points today.
Case Study 3
- 62-year-old female s/p L MCA infarct presenting with receptive and expressive aphasia and mild R UE weakness. Patient is ambulating around unit, but safety is a concern (requires CG/min A assistance for seated and standing ADLs). Family can provide part-time assist only.
- Discussion Points
- DC planning
- Demonstrate deficits
- Interventions
- Discussion Points
Case Study 4
- 76-year-old male s/p L PCA stroke demonstrating mild R UE/LE strength deficits and significant balance deficits, unable to sit EOB unsupported. Patient is appropriate for acute rehab but refusing rehab placement. Patient with good family support and is willing to d/c home at a wheelchair level. He and his family report they are willing to purchase any equipment recommended. Patient has 1st floor setup with ½ bath but 4 STE.
- Discussion Points
- Discharge recommendations
- Plan of care/goals
- Discussion Points
Please email us any questions as you go through case studies three and four.
Summary
- Interdisciplinary Approach to Stroke Rehabilitation
- Benefits
- Ways to Implement
We know that an interdisciplinary approach to stroke rehab is beneficial, as it helps our patients meet their goals and produces optimal outcomes. It is doable in all settings, and we can implement this approach by having verbal conversations with our counterparts about our treatments and recommendations. We can incorporate co-treat as appropriate and help each other in our interventions by incorporating the other discipline's interventions. It can be as easy as incorporating upper extremity weight bearing or increased awareness during a standing task. It does not have to be huge changes. It is being mindful and intentional of how we are using them during our treatment sessions.
An interdisciplinary approach helps with time management, builds confidence, and increases rapport. In part two of our series. We will be going over the quick stroke facts, bringing back J.K. to discuss the home, outpatient, and community settings.
Questions and Answers
What is the process of certification for an OTA to utilize e-stim?
It is the same certification or CEU course you can take to be certified in physical modalities. After taking the course, you must be supervised while using the modalities.
What is the best treatment for a patient who has shoulder subluxation?
This is a tough question as it is not black and white. We know that sensory and motor deficits come along with the stroke population, and there is not one intervention that fits all. Doing a combination of things like weight bearing and PNF strategies may help. The other aspect is knowing what phase of stroke they are in. You might see bigger gains in the acute subacute phase compared to the chronic phase. You will also want to provide them with a home program to help them at home for carryover.
Can you use e-stim interventions in a home health setting?
You can use e-stim in any setting and can bill appropriately, just like you would in an inpatient setting. You would bill for a neuromuscular strengthening depending on what you are working on using the e-stim. However, in a home health setting, you will need access to that equipment. Would you need your company to purchase that equipment or purchase it yourself?
Do you have any more information on FES devices and the upper extremity?
Most research on FES devices starts with the lower extremity. There are options for the upper extremity, but remember, whatever you do has to go back to ADLs. If you are doing FES for the biceps and hand-to-mouth control, you need to relate this to self-feeding.
Did you list all of the outcome measures recommended for acute care?
The list of outcome measures we left for you in each section includes recommended ones based on StrokEdge data and clinical practice guidelines. However, it is not an exhaustive list. There are other outcome measures used, such as the modified Barthel index. What you want to do is take a look at the most recent evidence for each outcome measure that you are using and make sure it is appropriate for the stroke population or whatever population and the chronicity of the patient. For example, is it appropriate to use with stroke patients in the acute phase of their recovery or in the chronic phase of their recovery?
References
Ahn, S., & Hwang, S. (2019). Virtual rehabilitation of upper extremity function and independence for stroke: A meta-analysis. Journal of Exercise Rehabilitation, 15(3), 358–369. https://doi.org/10.12965/jer.1938174.087
Almhdawi, K. A., Mathiowetz, V. G., White, M., & delMas, R. C. (2016). Efficacy of occupational therapy task-oriented approach in upper extremity post-stroke rehabilitation. Occupational Therapy International, 23(4), 444–456. https://doi.org/10.1002/oti.1447
Arya, K. N., Verma, R., Garg, R. K., Sharma, V. P., Agarwal, M., & Aggarwal, G. G. (2012). Meaningful task-specific training (MTST) for stroke rehabilitation: A randomized controlled trial. Topics in Stroke Rehabilitation, 19(3), 193–211. https://doi.org/10.1310/tsr1903-193
Ballester, B. R., Maier, M., Duff, A., Cameirao, M., Bermudez, S., Duarte, E., Cuxart, A., Rodríguez, S., San Segundo Mozo, R. M., & Verschure, P. F. M. J. (2019). A critical time window for recovery extends beyond one-year post-stroke. Journal of Neurophysiology, 122(1), 350–357. https://doi.org/10.1152/jn.00762.2018
Bolognini, N., Russo, C., & Edwards, D. J. (2016). The sensory side of post-stroke motor rehabilitation. Restorative Neurology and Neuroscience, 34(4), 571–586. https://doi.org/10.3233/rnn-150606
Borschmann, K. (2012). Exercise protects bone after stroke, or does it? A narrative review of the evidence. Stroke Research and Treatment, 1–12. https://doi.org/10.1155/2012/103697
Conforto, A. B., Dos Anjos, S. M., Bernardo, W. M., Da Silva, A. A., Conti, J., Machado, A. G., & Cohen, L. G. (2018). Repetitive peripheral sensory stimulation and upper limb performance in stroke: A systematic review and meta-analysis. Neurorehabilitation and Neural Repair, 32(10), 863–871. https://doi.org/10.1177/1545968318798943
Dromerick, A. W., Geed, S., Barth, J., Brady, K., Giannetti, M. L., Mitchell, A., Edwardson, M. A., Tan, M. T., Zhou, Y., Newport, E. L., & Edwards, D. F. (2021). Critical Period After Stroke Study (CPASS): A phase II clinical trial testing an optimal time for motor recovery after stroke in humans. Proceedings of the National Academy of Sciences, 118(39). https://doi.org/10.1073/pnas.2026676118
Felipe, F. A., de Carvalho, F. O., Silva, É. R., Santos, N. G. L., Fontes, P. A., de Almeida, A. S., Garção, D. C., Nunes, P. S., & de Souza Araújo, A. A. (2020). Evaluation instruments for physical therapy using virtual reality in stroke patients: A systematic review. Physiotherapy, 106, 194–210. https://doi.org/10.1016/j.physio.2019.05.005
Gelaw, A. Y., Janakiraman, B., Teshome, A., & Ravichandran, H. (2019). Effectiveness of treadmill assisted gait training in stroke survivors: A systematic review and meta-analysis. Global Epidemiology, 1. https://doi.org/10.1016/j.gloepi.2019.100012
Greenberg, S. M., Ziai, W. C., Cordonnier, C., Dowlatshahi, D., Francis, B., Goldstein, J. N., Hemphill, J. C., Johnson, R., Keigher, K. M., Mack, W. J., Mocco, J., Newton, E. J., Ruff, I. M., Sansing, L. H., Schulman, S., Selim, M. H., Sheth, K. N., Sprigg, N., & Sunnerhagen, K. S. (2022). 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: A guideline from the American heart association/American stroke association. Stroke, 53, e282-361. https://doi.org/10.1161/str.0000000000000407
Herpich, F., & Rincon, F. (2020). Management of acute ischemic stroke. Critical Care Medicine, 48(11), 1654–1663. https://doi.org/10.1097/ccm.0000000000004597
Hosseini, Z.-S., Peyrovi, H., & Gohari, M. (2019). The effect of early passive range of motion exercise on motor function of people with stroke: A randomized controlled trial. Journal of Caring Sciences, 8(1), 39–44. https://doi.org/10.15171/jcs.2019.006
Huseyinsinoglu, B. E., Ozdincler, A. R., & Krespi, Y. (2012). Bobath Concept versus constraint-induced movement therapy to improve arm functional recovery in stroke patients: A randomized controlled trial. Clinical Rehabilitation, 26(8), 705–715. https://doi.org/10.1177/0269215511431903
Jin, M., Pei, J., Bai, Z., Zhang, J., He, T., Xu, X., Zhu, F., Yu, D., & Zhang, Z. (2021). Effects of virtual reality in improving upper extremity function after stroke: A systematic review and meta-analysis of randomized controlled trials. Clinical Rehabilitation, 36(5), 573-596. https://doi.org/10.1177/02692155211066534
Johnston, T. E., Keller, S., Denzer-Weiler, C., & Brown, L. (2021). A clinical practice guideline for the use of ankle-foot orthoses and functional electrical stimulation post-stroke. Journal of Neurologic Physical Therapy, 45(2), 112–196. https://doi.org/10.1097/npt.0000000000000347
Juckett, L. A., Wengerd, L. R., Faieta, J., & Griffin, C. E. (2019). Evidence-based practice implementation in stroke rehabilitation: A scoping review of barriers and facilitators. American Journal of Occupational Therapy, 74(1), 7401205050p1. https://doi.org/10.5014/ajot.2020.035485
Kattenstroth, J. C., Kalisch, T., Sczesny-Kaiser, M., Greulich, W., Tegenthoff, M., & Dinse, H. R. (2018). Daily repetitive sensory stimulation of the paretic hand for the treatment of sensorimotor deficits in patients with subacute stroke: RESET, a randomized, sham-controlled trial. BMC Neurology, 18(1). https://doi.org/10.1186/s12883-017-1006-z
Laver, K. E., Lange, B., George, S., Deutsch, J. E., Saposnik, G., & Crotty, M. (2017). Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews, 11. https://doi.org/10.1002/14651858.cd008349.pub4
Leppert, M. H., Sillau, S., Lindrooth, R. C., Poisson, S. N., Campbell, J. D., & Simpson, J. R. (2020). Relationship between early follow-up and readmission within 30 and 90 days after ischemic stroke. Neurology, 94(12), e1249–e1258. https://doi.org/10.1212/wnl.0000000000009135
Lin, D. J., Finklestein, S. P., & Cramer, S. C. (2018). New directions in treatments targeting stroke recovery. Stroke, 49(12), 3107–3114. https://doi.org/10.1161/strokeaha.118.021359
Lura, D. J., Venglar, M. C., van Duijn, A. J., & Csavina, K. R. (2019). Body weight supported treadmill vs. overground gait training for acute stroke gait rehabilitation. International Journal of Rehabilitation Research, 42(3), 270–274. https://doi.org/10.1097/mrr.0000000000000357
Mack, A., & Hildebrand, M. (2022). Education and training interventions for caregivers of people with stroke. The American Journal of Occupational Therapy, 76(3). https://doi.org/10.5014/ajot.2022.0763004
Maggio, M. G., Latella, D., Maresca, G., Sciarrone, F., Manuli, A., Naro, A., De Luca, R., & Calabrò, R. S. (2019). Virtual reality and cognitive rehabilitation in people with stroke. Journal of Neuroscience Nursing, 51(2), 101–105. https://doi.org/10.1097/jnn.0000000000000423
Mehrholz, J., Thomas, S., & Elsner, B. (2017). Treadmill training and body weight support for walking after stroke. Cochrane Database of Systematic Reviews, 8. https://doi.org/10.1002/14651858.cd002840.pub4
Mekbib, D. B., Han, J., Zhang, L., Fang, S., Jiang, H., Zhu, J., Roe, A. W., & Xu, D. (2020). Virtual reality therapy for upper limb rehabilitation in patients with stroke: A meta-analysis of randomized clinical trials. Brain Injury, 34(4), 456–465. https://doi.org/10.1080/02699052.2020.1725126
Moore, J. L., Nordvik, J. E., Erichsen, A., Rosseland, I., Bø, E., Hornby, T. G., Barkenæs, T., Bratlie, H., Byhring, M., Grimstad, I., Hågå, M., Halvorsen, J., Henderson, C., Mbalilaki, J.-A., Rimehaug, S.-A., Sæther, K., Tomren, T., & Vergoossen, K. (2020). Implementation of high-intensity stepping training during inpatient stroke rehabilitation improves functional outcomes. Stroke, 51(2), 563–570. https://doi.org/10.1161/strokeaha.119.027450
Moore, J. L., Potter, K., Blankshain, K., Kaplan, S. L., OʼDwyer, L. C., & Sullivan, J. E. (2018). A core set of outcome measures for adults with neurologic conditions undergoing rehabilitation. Journal of Neurologic Physical Therapy, 42(3), 1. https://doi.org/10.1097/npt.0000000000000229
Nascimento, L. R., Boening, A., Galli, A., Polese, J. C., & Ada, L. (2021). Treadmill walking improves walking speed and distance in ambulatory people after stroke and is not inferior to overground walking: A systematic review. Journal of Physiotherapy, 67(2), 95–104. https://doi.org/10.1016/j.jphys.2021.02.014
Papanagiotou, P., & Ntaios, G. (2018). Endovascular thrombectomy in acute ischemic stroke. Circulation: Cardiovascular Interventions, 11(1). https://doi.org/10.1161/circinterventions.117.005362
Pathak, A., Gyanpuri, V., & Dev, P., Dhiman, N. (2021). The Bobath Concept (NDT) as rehabilitation in stroke patients: A systematic review. Journal of Family Medicine and Primary Care, 10(11), 3983. https://doi.org/10.4103/jfmpc.jfmpc_528_21
Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., Biller, J., Brown, M., Demaerschalk, B. M., Hoh, B., Jauch, E. C., Kidwell, C. S., Leslie-Mazwi, T. M., Ovbiagele, B., Scott, P. A., Sheth, K. N., Southerland, A. M., Summers, D. V., & Tirschwell, D. L. (2019). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 50(12). https://doi.org/10.1161/str.0000000000000211
Qian, J., McDonough, D. J., & Gao, Z. (2020). The effectiveness of virtual reality exercise on individual’s physiological, psychological and rehabilitative outcomes: A systematic review. International Journal of Environmental Research and Public Health, 17(11), 4133. https://doi.org/10.3390/ijerph17114133
Ranner, M., Guidetti, S., von Koch, L., & Tham, K. (2018). Experiences of participating in a client-centred ADL intervention after stroke. Disability and Rehabilitation, 42(25), 3025-3033. https://doi.org/10.1080/09638288.2018.1483434
Rao, A., Barrow, E., Vuik, S., Darzi, A., & Aylin, P. (2016). Systematic review of hospital readmissions in stroke patients. Stroke Research and Treatment. https://doi.org/10.1155/2016/9325368
Rapoliene, J., Endzelyte, E., Jaseviciene, I., & Savickas, R. (2018). Stroke patients motivation influence on the effectiveness of occupational therapy. Rehabilitation Research and Practice. https://www.hindawi.com/journals/rerp/2018/9367942/
Ravichandran, H., Shetty, K. S., & Janakiraman, B. (2022). Effect of gait-specific weight-bearing interventions on physical performance among subjects with stroke: A systematic review and meta-analysis. Journal of Stroke Medicine. https://doi.org/10.1177/25166085221115605
Sharififar, S., Shuster, J. J., & Bishop, M. D. (2018). Adding electrical stimulation during standard rehabilitation after stroke to improve motor function: A systematic review and meta-analysis. Annals of Physical and Rehabilitation Medicine, 61(5), 339–344. https://doi.org/10.1016/j.rehab.2018.06.005
Shimizu, N., Hashidate, H., Ota, T., & Yatsunami, M. (2019). Daytime physical activity at admission is associated with improvement of gait independence 1 month later in people with subacute stroke: A longitudinal study. Topics in Stroke Rehabilitation, 27(1), 25–32. https://doi.org/10.1080/10749357.2019.1649916
Solbakken, L. M., Nordhaug, M., & Halvorsen, K. (2022). Patients’ experiences of involvement, motivation and coping with physiotherapists during subacute stroke rehabilitation – a qualitative study. European Journal of Physiotherapy. https://doi.org/10.1080/21679169.2022.2032825
Spencer, J., Wolf, S. L., & Kesar, T. M. (2021). Biofeedback for post-stroke gait retraining: A review of current evidence and future research directions in the context of emerging technologies. Frontiers in Neurology, 12. https://doi.org/10.3389/fneur.2021.637199
Stinear, C. M., Lang, C. E., Zeiler, S., & Byblow, W. D. (2020). Advances and challenges in stroke rehabilitation. The Lancet Neurology, 19(4), 348–360. https://doi.org/10.1016/s1474-4422(19)30415-6
Tashiro, S., Mizuno, K., Kawakami, M., Takahashi, O., Nakamura, T., Suda, M., Haruyama, K., Otaka, Y., Tsuji, T., & Liu, M. (2019). Neuromuscular electrical stimulation-enhanced rehabilitation is associated with not only motor but also somatosensory cortical plasticity in chronic stroke patients: an interventional study. Therapeutic Advances in Chronic Disease, 10. https://doi.org/10.1177/2040622319889259
Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Alonso, A., Beaton, A. Z., Bittencourt, M. S., Boehme, A. K., Buxton, A. E., Carson, A. P., Commodore-Mensah, Y., Elkind, M. S. V., Evenson, K. R., Eze-Nliam, C., Ferguson, J. F., Generoso, G., Ho, J. E., Kalani, R., Khan, S. S., Kissela, B. M., . . . Martin, S. S. (2022). Heart disease and stroke statistics-2022 update: A report from the American Heart Association. Circulation, 145(8). https://doi.org/10.1161/cir.0000000000001052
Vahidy, F. S., Donnelly, J. P., McCullough, L. D., Tyson, J. E., Miller, C. C., Boehme, A. K., Savitz, S. I., & Albright, K. C. (2017). Nationwide estimates of 30-day readmission in patients with ischemic stroke. Stroke, 48(5), 1386–1388. https://doi.org/10.1161/strokeaha.116.016085
Voinescu, A., Sui, J., & Stanton Fraser, D. (2021). Virtual reality in neurorehabilitation: An umbrella review of meta-analyses. Journal of Clinical Medicine, 10(7). https://doi.org/10.3390/jcm10071478
Wattchow, K. A., McDonnell, M. N., & Hillier, S. L. (2018). Rehabilitation interventions for upper limb function in the first four weeks following stroke: A systematic review and meta-analysis of the evidence. Archives of Physical Medicine and Rehabilitation, 99(2), 367–382. https://doi.org/10.1016/j.apmr.2017.06.014
Xiong, Y., Wakhloo, A. K., & Fisher, M. (2022). Advances in acute ischemic stroke therapy. Circulation Research, 130(8), 1230–1251. https://doi.org/10.1161/circresaha.121.319948
Citation:
McCool, A., & George, K. (2022). Interdisciplinary approach to stroke rehabilitation: Acute care and inpatient rehabilitation phase. OccupationalTherapy.com, Article 5564. Available at www.OccupationalTherapy.com

