Introduction
It is an honor to be back here on OccupationalTherapy.com. It is always a pleasure presenting with you all, so thank you so much for having me back. I am excited about the timing of this course because September is Childhood Cancer Awareness Month. The way I will be presenting today is under the assumption that participants have already watched Part I as this will make much more sense to you if you are familiar with stem cell transplantation. I will provide you with a quick review of the definition of stem cell transplant before we get started.
Refresher on Pediatric SCT (Stem Cell Transplantation)
Stem cell transplantation is a general broad term that includes stem cell transplantation and bone marrow transplantation. Essentially, it is a medical procedure that may be necessary to replace an unhealthy immune system. There are different reasons this may occur. One of those reasons is due to a disease or condition like leukemia. Stem cell transplants may be warranted if an individual's immune system is weakened following treatment for cancer. Things like chemotherapy and radiation therapy can wear down the immune system requiring stem cell transplantation.
Types of SCT
- Now considered the standard of care for many populations
- Two main types:
- Autologous (patient is “donor”)
- Allogeneic (matched related or unrelated donor)
- Matched related (sibling, close family member)
- Unmatched unrelated (national registry)
- Umbilical cord (“cord blood” taken from the placenta)
- Two main types:
(ACS, 2016)
There are two main types of stem cell transplantation. Most of us are familiar with autologous. Autologous or auto stem cell transplantation is when the recipient and donor are the same person. Allogeneic stem cell transplant occurs when another donor is involved. This person may be related or unrelated. There are many different types of allogeneic transplants. Sometimes, it is a matched related donor like a sibling or close family member. An unmatched related donor may also be identified through the national registry. Umbilical cord transplants are also performed where the cord blood is taken from the placenta. Today, we are seeing more and more allogeneic transplants because the anti-rejection medication is improving helping these to be more effective and successful in the long run.
- Mini-transplants (non-myeloablative)
- Reduced-intensity conditioning (RIC)
- Syngeneic stem cell transplant: identical sibling
- Half-matched transplant
- Human leukocyte antigens (HLA) and histocompatibility testing
(ACS, 2016)
Other types of transplants are known as mini-transplants or non-myeloablative. These may be appropriate for individuals who cannot tolerate the more intensive, full stem cell transplantation. If the goal is not to completely eradicate the disease, this may be the type of transplant that is warranted for that individual. Another type is a syngeneic stem cell transplant. This is when there is an identical sibling available to be the donor, and they are a perfect match. Half-matched transplants or mismatched transplants occur when the human leukocyte antigens (HLA) or the blood typing (histocompatibility) are not the exact same. As I mentioned before, these are becoming more common because anti-rejection medication is becoming more effective today.
What I hope to highlight for you today is a more clear picture of what individual clients, with the different types of transplants, may look like and what may happen when we meet them at a different point in their process.
Meet Henry
Occupational Profile
- Age: 3 months
- Lives in 4th-floor walk-up apartment with his two moms in Brooklyn, New York
- Diagnosis: Severe Combined Immune Deficiency Syndrome (SCIDs)
- Referral
- Placed by pediatric SCT nurse practitioner in an acute care cancer specialty institute
Henry is a three-month-old male, who lives in Brooklyn with his two moms in a walk-up apartment building. Henry was diagnosed with Severe Combined Immune Deficiency Syndrome after his newborn uniform screening panel. This is now a national requirement. The reason for this change is that when SCIDs is caught early enough, a child's chance for survival is very good. They need to be treated at three and a half months of age or younger. So, it is critical that we identify this disease very early. Many of these kids used to be diagnosed when they became symptomatic, and at this point, it was too late. The success rate for treatment early on is good. SCIDs or Severe Combined Immune Deficiency is what a lot of people refer to as the "bubble boy syndrome." Essentially, children diagnosed with SCIDs are born without an immune system or an inefficient immune system. In Henry's case, the goal was to perform a stem cell transplantation before the age of three months, which they were able to do. His referral for occupational therapy was placed by the stem cell transplant team and a nurse practitioner in the acute care oncology setting. Although SCIDs is not a malignancy or a type of cancer, many of these children are treated with stem cell transplantation which primarily occurs in a cancer specialty institution. This is where you may meet many kids like Henry in your practice.
SCT & Medical Treatment Plan
- Mediport placed
- Preparative/conditioning regimen:
- Not necessary
- 10/10 HLA-matched related donor
- Sister
- Cells injected into bloodstream
- IVIG
He received a mediport after he was admitted to the hospital. A mediport is placed in the chest and used for many different reasons. In children like Henry, it can be used for frequent lab draws and to administer medication. Henry did not require the preparative or conditioning regimen that some babies diagnosed with SCIDs do. He was lucky that he had a twin sister who happened to be a 10 out 10 HCLA-matched donor for him. The chance of rejection was a bit lower for him thus a preparatory regimen was not required. Thus, Henry did not go through the intensive chemo and intensive radiation therapy that some other children do. He did receive IVIG, which is intravenous immunoglobulin. IVIG is multiple blood products from multiple donors with the intent is to boost the immune system. The medical team may ask us to hold therapy if it is the child's first time receiving IVIG. There also tends to be a high reaction rate. Once a child has received that type of boost and tolerated it well, usually it is okay to treat them while IVIG is running. Henry received his stem cell transplant via a peripheral IV, and there were no intensive complications.
Lab Values and Special Considerations
- Day “0”
- Day -2 → day +2 following SCT
- Protective isolation
- Thrombocytopenia
OT was referred for Henry on day zero. Day zero is the actual day of the stem cell transplantation. Figure 1 a visual representation of Henry's treatment roadmap.
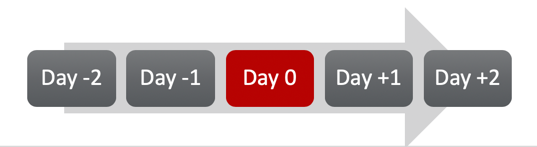
Figure 1. Henry's treatment roadmap.
Day minus one is the day before his stem cell transplant, and day plus one is the first day after and so on. Any treatment that occurs when there is a stem cell transplant scheduled is included on this roadmap timeline, and everything is dated as being pre or post-stem cell transplantation. On the day of the transplant, there is always a lot of anticipation and anxiety on the family's part. The stem cell transplant is simple (yet not simple), and it is a single transfusion. Sometimes, the process is very quick, while other times it may last a little bit longer. Some medical teams may want you to hold therapy on the day of stem cell transplantation if there is a specific complication they are worried about. For example, if the child receives the stem cell transplant early in the morning, they may want to closely observe them for any complications after. Conversely, if they are scheduled for the stem cell transplant later in the day, occupational therapy could coordinate with nursing to complete an evaluation. Every client is different. At the end of the day, we are always going to collaborate with nursing to determine what the most appropriate thing is.
Kids are usually premedicated about 30 minutes before the transplant with antirejection medication, maybe Benadryl, to prevent any kind of reaction. It is important to be mindful of the timing of your evaluation around that. It is also important to remember that in the two days before and after, clients most likely will experience some pretty severe thrombocytopenia and neutropenia because their immune system essentially is pretty much knocked out. They are very prone to infection so we need to be very mindful of that when we work with them. During this time, you are not going to take any toys in the room that have been used by other clients, and it is best to minimize things that you add to the room to prevent that infection.
OT Evaluation
In Henry's case, he was evaluated early in the day before his transplant.
- ROM – WFL
- Decreased strength/endurance
- Sensory processing
- Visual-motor - WFL
- Cognition - WFL
- Decreased play skills
- Decreased motor skills
- Decreased ADL participation
- Assessments
- PedsQL
- PDMS-2
- AIMS
His range of motion was within functional limits. Because of his newly placed mediport, he was not encouraged to reach overhead. And, at three months, he was not going to be stretching too much anyway. It is good to give the family expectations and specific parameters. Many times after mediports have been placed, one of the activity parameters is to avoid reaching overhead or avoiding shoulder abduction beyond 90 degrees. We need to be mindful of this restriction when we are positioning the client. Sensory processing is also important to assess. I think it is always important to ask families if there have been any changes in tolerance for different types of sensation. This is primarily important for children who have received chemotherapy and radiation due to some of the side effects. In Henry's case, his sensory processing was within functional limits as well as his cognition and visual-motor control. He localized to auditory and visual stimulation consistently. He was appropriate in his facial expression and emotional responses. However, there was some concern about his play skills, motor skills, and ADL participation. After the mediport was placed, Henry experienced decreased tolerance for changes in position, and his moms were not as comfortable with putting him in a prone position. They did not want to hurt him, and they were not sure if that was a safe and acceptable position. I would ask the medical team first, but in my experience, there has never been an issue putting a child, Henry's age, in prone especially when supported with some type of towel roll or wedge. And of course, this activity is always supervised. Promoting those different positions is really important with a mediport.
In the area of ADL participation prior to his stem cell transplantation, he was primarily breastfed. Unfortunately, it is recommended that breastfeeding be discontinued for many of these clients. The reason is because they do not want anything to be passed on from the mother to the baby that could compromise their immune system in any way. So, Henry had to adjust to bottle-feeding as well as getting used to drinking formula. This was a significant change.
For standardized assessments, it is tricky because there is not a lot of normative and standardized data on the pediatric oncology population. We really have to pull assessments from different areas of practice. I like to use the Pediatric Quality of Life or the PedsQL to get more information. I use this primarily as a screening tool to get a better idea psychosocially how the child and family are doing. This can let us know if another type of referral is needed and if there are other areas we can work on. In Henry's case, his moms were particularly anxious about handling him and managing him in the hospital with all the lines and tubes. The Peabody may be appropriate for him as well, and also the AIMS, the Alberta Infant Motor Scale. This would be my primary focus for a child like Henry, especially since he is having some difficulty with his motor skills. I would want to monitor and screen those very closely. Thus, if his development slows slightly while he is admitted to the hospital for the procedure, I could continue to follow him and take objective data of his motor skills moving forward. Also, the COPM, or the Canadian Occupational Performance Measure, would be helpful to use with his moms and interview them to get an idea of some of what their goals are for the therapy process.
OT Intervention
- Assist in fostering development of age-appropriate motor skills
- Play and environmental exploration
- Maximize independence
- Educate caregivers
- Discharge recommendation:
- EI services
Henry's primary concerns were positioning and motor and play skill development. When receiving a stem cell transplant, individuals have private rooms in the hospital. As a result, we can recommend how to set the room up to maximize the client's exposure to different settings for play. In his case, he did not have many options outside his bed or crib because he was so young. An extra mat in the room might be helpful. I know this can be tricky depending on the resources where you work, but this can be another great play surface. Some families are willing to even go buy those big puzzle mats that you can wipe off and clean. You can get them at Target and Walmart. This, however, cannot be used by any other children, and it has to be a material that can be cleaned.
After setting up the environment that was conducive for play, a realistic play schedule can be provided to Henry's moms. This can help his parents to feel empowered to be responsible for promoting playtime. They could be educated on how to transfer Henry safely to the mat and allow him to move in a different way than he did in his crib for most of the day. It is also important to encourage them to bring in alternative seating like a well-positioned baby seat. Another component is to bring in age-appropriate toys to provide him with varied sensory experiences. He was only exposed to people fully gowned, gloved, and masked during his hospital admission. And at three months old, this was a crucial stage where he was learning a lot of new skills quickly. Development is really rapid at this stage, and hospitalization can be a barrier. It is so important to create sensory alternatives for kids like Henry to open up their world a little bit and to maximize their independence.
Typically, I recommend putting a child like Henry on the schedule twice a week. The child will then need to be reevaluated every couple of weeks to see how things are going. If you find that the child becomes more fatigued and has less energy, you may want to increase that frequency. However, I would say this is a pretty typical schedule for a child admitted for this type of procedure at that age.
Upon Henry's discharge, early intervention services were appropriate. Following this type of procedure, motor delays are something you want to keep a close eye on. There can be late-term effects that are well-documented following stem cell transplantation.
