Learning Outcomes
- After this course, participants will be able to identify the symptoms of caregiver burnout.
- After this course, participants will be able to list the main factors that contribute to caregiver burnout.
- After this course, participants will be able to identify resources for caregivers.
Introduction
Hello everyone. I am excited to be here and have some excellent information for you. Caregivers work so hard to provide for their loved ones.
References
Here are the references used to compile this information in Figure 1.
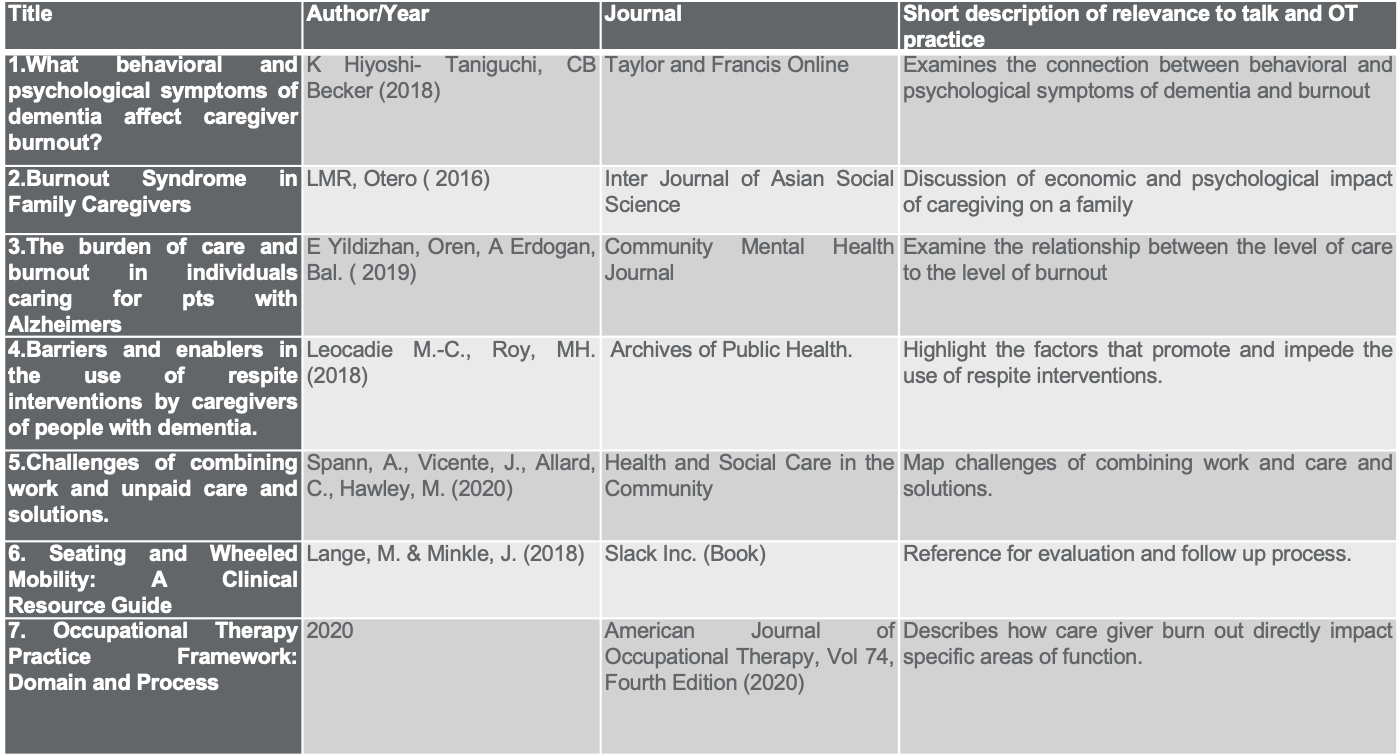
Figure 1. The references used for this talk. Click here to enlarge the image.
Here are some references that I used to create this talk.
Holistic Caregiver Impact
- 7 Dimensions of Well Being
- Physical – A balance of strength, flexibility, and endurance in your body. Helps prevent disease, adds quality of life, and length of life.
- Intellectual – Engaging in creative and stimulating activities that maintain and increase the function and capacity of your brain.
- Environmental – Sense of safety, comfort, and connection with your physical surroundings.
- Vocational – Using your gifts, talents, and experiences to produce income, provide a service, and impact others.
- Social – Fostering personal connections and nurturing relationships that establish social networks and support systems.
- Emotional - Overall positive state of being that encompasses satisfaction, meaning, and purpose.
- Spiritual – A connection to a set of core beliefs and values that provide you with structure, boundaries, and peace.
As occupational therapists, we pride ourselves on being the champions of holistic wellness. That is the main reason why I wanted to become an occupational therapist. What makes up the whole person? There are seven dimensions of well-being. The first is physical, a balance of strength, flexibility, and endurance in our bodies. It helps prevent disease, promotes quality of life and how well you feel. How does your back feel? I am getting a little bit older, and my knees are not as good as they used to be. When someone asks you how you feel, they typically ask about physical well-being. Intellectual well-being is engaging in creative and stimulating activities that maintain and increase the function and capacity of the brain. Perhaps you love listening to favorite podcasts. Like me, you may like to read or listen to Audible. Environmental is your sense of safety, comfort, and connection where you are. This is making a cozy space to destress. When mom closes the door to her office, the kids know not to bother her. Vocational wellness is how we use our gifts, talents, and experience to produce income and provide a service. Fostering personal connections with people is the social part of well-being. You meet up with your friends for happy hour on Friday or go to a mom group. Emotional well-being is an overall positive state of being that encompasses your satisfaction, meaning, and purpose. The last one is spiritual, or a connection to a set of core beliefs and values that provides you with structure, boundaries, and peace.
Caregivers must tap into each one of these seven areas of well-being. Many caregivers say that these seven areas of well-being are impacted. We can then understand why burnout is common, and I want to say unavoidable. Here is a numerical illustration in Figure 2.
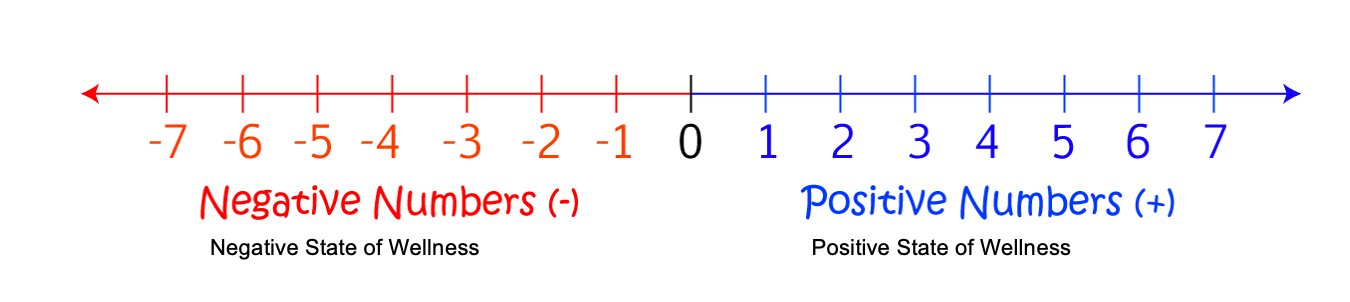
Figure 2. Number line to identify a state of wellness.
The class title is "Preventing Caregiver Burnout." However, I am not magic and do not think "prevent" is a good word. We need to strive for is decreasing burnout. We will now jump into and talk about more of these areas of well-being and then discuss how it affects our caregivers directly.
Physical Wellness Impact
- Changes in sleep patterns
- Getting sick more often
- Exhaustion
- Changes in appetite, weight, or both
- Using alcohol and/or sleep medications too much
- Headaches
- Digestive Issues
The first is physical wellness. Caregivers often have changes in sleep patterns and physical sicknesses like viruses, colds, and other diseases. They may have exhaustion, changes in appetite, weight gain or loss, increased use of alcohol, headaches, and digestive issues. If you could make a mental note of how a caregiver looked for a month, you would probably be able to see some visible signs of caregiving taking a toll on their physical wellness.
Intellectual Wellness Impact
- Difficulty concentrating
- Difficulty completing tasks
- Hesitancy trying new or challenging things
- Difficulty solving daily life situations
An intellectual wellness impact includes difficulty concentrating, completing tasks, or hesitating to try new things because why would they want to "add one more thing to my plate." It may even be a preferred task, but they are unwilling to add more activities. They may also display difficulty solving daily life situations.
Social Wellness Impact
- Withdrawal from friends and family
- Loss of interest in activities
- Becoming unusually impatient, irritable, or argumentative with patient and others
There may be a withdrawal from family and friends. We are going to talk about this later. They need to tap into community and social support as it is essential. Social wellness is something that we have to pay special attention to because this is one of the ways that we can help caregivers gain a little bit of their time and balance back. They may display a loss of interest in activities and become unusually impatient and irritable.
Environmental Wellness Impact
- Disorganized at home and work
- Decreased cleanliness of the home
- Decrease time spent out of the home
For environmental wellness, their home may show decreased organization and cleanliness. They may also start to spend most of their time in their home.
Spiritual Wellness Impact
- Decreased “faith”
- Feeling of abandonment by God
- Feelings of being disconnected to their inner self (sense of loss of self)
They may have decreased faith. Many caregivers begin to question why their God or whoever they serve would allow this caregiving burden as their fate. They may experience feelings of abandonment by God and being disconnected from their inner self. They may wonder, "Who am I?" or, "Am I only a caregiver?" They may lose touch with who they are and the things they enjoy.
Vocational Wellness Impact
- Decreased performance of work responsibilities
- Problems interacting with co-workers
- Decreased job satisfaction
- Financial Instability
The impact of vocational wellness may manifest as decreased performance at work, problems interacting with co-workers, reduced job satisfaction, and overall financial instability.
Emotional Wellness Impact
Caregivers may have many of these symptoms.
- Feeling blue, cranky, hopeless, and helpless
- Feelings of wanting to hurt yourself or the person for whom you are caring
- Depression
- Anxiety
Caregivers and patients may exhibit the following symptoms.
- Caregiver
- Headaches
- Sleep Disturbances
- Heart Disease
- Anxiety
- Unhealthy Weight Loss or Gain
- Poor Medication Management
- Digestive Issues
- Dizziness
- Irritability
- Muscle Tension and Pain
- Patient/Loved One
- Headaches
- Sleep Disturbances
- Heart Disease
- Anxiety
- Unhealthy Weight Loss or Gain
- Poor Medication Management
- Digestive Issues
- Dizziness
- Irritability
- ADL impairment
- Fall Risk and Falls
- Behaviors
- Pain
- Incontinence
- Decreased Skin Integrity
How can we realistically, without intervention and resources, expect our caregivers to do an excellent job at taking care of their loved ones if we do not help with some of these symptoms?
Defining Caregiver Burnout
- Caregiver Burnout:
- A state of physical, emotional, and mental exhaustion
- Affects ADLs and IADLs
- Not an episode but a cycle
- Not preventable but can be drastically mitigated
Caregiver burnout is a state of physical, emotional, and mental exhaustion that begins to affect a person's ADLs and IADLs. A warning sign is when a caregiver is not taking care of themselves. They may come to the clinic disheveled or mention that they have missed work for many days. They may also complain of headaches a lot. One thing that we need to understand is that burnout is not an episode or a one-time thing. It is a cycle, and it is our job as occupational therapists to give them the tools and the resources to disrupt, slow down, or pause that cycle. Caregiver burnout is not preventable, but it can be drastically mitigated.
OT Impact
- Research shows that occupational therapy intervention:
- Decreases behavioral symptoms
- Decreases psychological symptoms
- Decreases caregiver’s report of distress and anger towards client’s behaviors
Research shows that occupational therapy intervention decreases behavioral symptoms, and we will dig into this important topic a little more later. When we can reduce the behavioral symptoms of our clients, it decreases caregiver burnout. The second thing is that we can decrease psychological symptoms as well. By helping caregivers, we hear fewer reports of distress and anger directed at their loved ones. These are comments like, "He does it on purpose. He knows it irritates me, and he still does it. I don't know why he continues to do that." We can educate our caregivers, so they understand the behavior better. This is one of the areas where occupational therapists are highly impactful.
Correlates for Burnout
- Number of Behavioral Symptoms (2 or more)
- Level of Assist (mod A or greater)
- Gender (greater reports in females)
- Age (greater in younger caregivers)
- Relationship to client
- Ethnicity (greater reports in White/Caucasian)
- Education level
There are some correlates of burnout. The number one indicator for an eventual burnout is the number of behavioral symptoms in a loved one. Alzheimer's disease and other mental health conditions in loved ones are more stressful on caregivers than dealing with those with physical impairments. Even if the loved one is max to total assist physically but cognitively intact, their caregiver has a lower propensity for burnout than the caregiver of a loved one who has two or more behavioral symptoms.
A loved one needing moderate assistance or more is another correlate for burnout. Females also have a higher propensity for burnout than males. We have also seen that younger caregivers are at a greater risk of experiencing burnout than older caregivers. For example, if you have a husband caring for a wife or what we see most often, a wife caring for a husband, there has been time to accept their role. However, a younger caregiver, like a daughter caring for her father, may feel that she has been unfairly thrust into a role for which she was not prepared. This is why we see a more significant and higher propensity for burnout for younger people than older people.
The relationship with the client is another one. Burnout is lower for spouses versus other relatives like a daughter/son or a niece/nephew. When the relationship is not as close as a spouse's, the propensity for burnout is higher.
There are also greater reports of burnout in Caucasians and those with a higher education level.
(Cook, Snellings, & Cohen, 2018)
Burnout Measures and Assessments
- Caregiver Self Assessment Questionnaire https://www.healthinaging.org/tools-and-tips/caregiver-self-assessment-questionnaire
- Caregiver Burden Self Assessment https://www.agingcare.com/documents/caregiver_burden_assessment.pdf
- The Center for Epidemiologic Studies Depression Scale (CES-D) https://www.chcr.brown.edu/pcoc/cesdscale.pdf
- The Zarit Burden Short Forms https://www.oncozine.com/wp-content/uploads/2018/11/ZBI-12_Form.pdf
There are several burnout measures that you can easily access for free. You want to prep your caregiver before assessing them, as caregivers often feel judged. When you begin to ask them questions like, "Do you feel resentful?" you may get an adverse reaction, or they may not tell the truth. Make sure that you give them at least a session's notice before implementing one of these. You can say, "This is an assessment that we give all of our caregivers. Often people answer say they have depression, are teary, or have some resentment." You want them to not be on guard and feel comfortable
I like the ones that are a little bit shorter. While none of them is too long, I like the ones that are about 18 to 20 questions. Once you start asking anyone more than 20 questions, they may begin to feel standoffish. Take the time to peruse the assessments yourself and see what you think about it.
One good thing about several is that they can be self-assessments. If your clients will not sit down with you, they may be willing to the assessment with them or click on a computer link later. They then may talk to you about what they found at a later date.
Number 1 Correlate: Number of Behaviors
The number one correlate for caregiver burnout is the number of behaviors in a loved one. A patient that consistently spits, screams, or is rude might be tolerated for 45 minutes of an OT session; however, the caregiver has to be with the client all the time. I am sure you can see why this is the number 1 correlate without a study reporting it. This is where OTs can come into play.
An approach called "The DICE Approach" is shown in Figure 3.
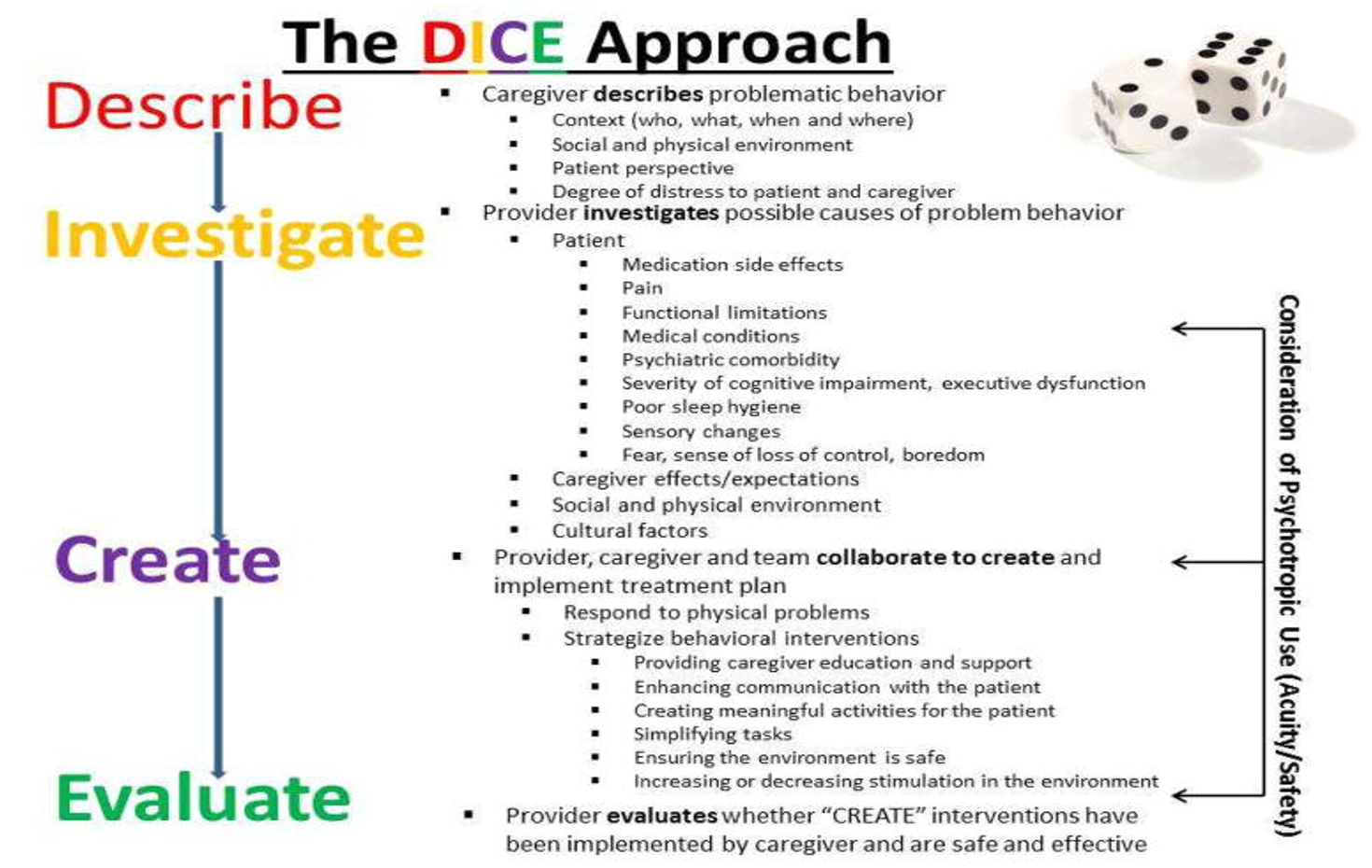
Figure 3. Overview of DICE. Click here to enlarge the image.
It methodically breaks down how we look at a person exhibiting behaviors. At each step, there is something that we can do for intervention, even if it only changes the behavior slightly.
Describe
The first part of the DICE is "describe" as we listen to the caregiver as they describe the problematic behavior. We are looking for context and key players. When does it happen? Is it in the morning or the afternoon? Is it only with the daughter or the paid caregiver? We need to take good notes because we will be looking for parallels and differences.
We also want to look at the social and physical environment and the patient perspective. Often, as clients are non-verbal or cannot clearly articulate their needs and wants, we do not gain their perspective on an issue. We cannot skip that step.
The degree of distress of a behavior to a patient and caregiver is another factor. Let's say there are five behaviors. One of them may not bother the caregiver too much, but another may get under her skin. As we begin to create our care plans and treatment interventions, we can tackle the most pressing issues and then work our way down.
Investigate
For "investigate," we look at things like medication side effects. We can get nursing and the doctor involved. We can also assess pain, functional limitations, psychiatric comorbidities, the severity of the cognitive impairment, and poor sleep hygiene. We are digging into all of the factors contributing to the behaviors.
We can then come up with an intervention plan with tailored activities. We want to tap into something the client is familiar with to limit as much new learning as possible. With cognitive impairment, new knowledge is more challenging to maintain or achieve. We are going to have greater success with familiar activities.
We also want to simplify tasks and change the environment if needed. We do is not want to change too many things in the patient's environment at once because that can be more disruptive.
Create
As part of "create," for example, we may change the positioning of the client's chair, but we are not going to move the chair to a different room. We only want to change one or two things in the person's environment at a time. It can be more disruptive than helpful if we change more than that.
Evaluate
The last correlate is "evaluate." We then evaluate what works based on our observations and the caregiver's experience. We ask very measurable things like the number of times the behavior has presented itself. If it is not working, we go back to create and try it again. By decreasing or eliminating one or two behaviors (two or more increases burnout), we may significantly impact burnout. What if we mitigate those behaviors, so only one behavior gets under the caregiver's skin through the DICE Approach? Or have we decreased the frequency or severity of the behaviors? Even one successful behavior that we have mitigated or reduced can give a caregiver up to an hour of their life back. If someone told me every day that I could have an hour of my life to do me, I would be all for it.
Number 2 Correlate: Level of Assist
- ADL retraining
- IADL
- Transfer Training
- Bowel and Bladder Management
- Medication Management
The next correlate is the level of assist.
ADL Retraining
If we can get Mr. Johnson independent on putting on his pants, his caregiver may be able to sit and have a cup of coffee in the morning before she has to prepare dad's breakfast. If we can get Ms. Williams independent or minimal assistance managing her bowel and bladder, perhaps we can give her daughter time to walk around the block. A decrease in assistance increases the time a caregiver spends on their self-care and self-management.
IADL
Can we get a client interested in a hobby or sit down for 15 minutes and perform a tailored activity? What interests, hobbies, or community activities can we get our clients involved in to help our caregivers have more time throughout the day?
Transfer Training
Many caregivers express the pain in their backs and shoulders from transferring clients. Often, most caregiving training is completed in the last week of care. If we start intensive transfer and caregiver training early on, this can help caregivers feel more prepared.
Bowel and Bladder Management
Bowel and bladder management is often overlooked. We need to dive into the specific details of why our clients are incontinent. Is it stress or mixed incontinence? We could start a bowel and bladder management schedule or take the client to the bathroom at specific intervals. We can also make slight changes to how much fluid we give them and at what times. There may be medications that can help. Can we bring in some e-stim? We need to include bowel and bladder management goals as this can ease the caregiver's role.
Medication Management
Is the client cranky or sleepy during certain times or after certain medications? We can work with nursing and the physician to see if we can switch or modify medication schedules to make them more manageable and helpful.
Other OT Intervention Areas
- Stress Management Techniques
- Caregiver education (including basic understanding of nature of dementia)
- Maintenance Programs
- Environmental Modifications
- Health Promotion
Stress Management Techniques
We can say to our caregivers, "I know that you're at the edge, but I promise you, there are some things that you can do to back yourself away from that edge." Many of them do not buy it, but we have to sell it. It could be certain things like taking deep breaths, walks, and sensory regulation. We think of sensory regulation with kids with autism, but it can also work for stress management. For example, they could go to a trampoline park. You could explain how it is essential to put weight through joints for good sensory input and endorphins. You could encourage cardio activities and have them write down some small goals regarding activities for stress management. Another idea is journaling.
Caregiver Education
We talked about this a little bit, but I want to stress this again. One statistic says only 47% of caregivers feel they have received adequate training to perform major caregiving tasks, including catheter management, transfer training, and wound care. One of the huge reasons for that is the tendency to pack in most caregiver training into the last week of therapy. We have to change this philosophy and start early with our training. Make a point to include caregivers in as many sessions as are practical and possible. If they work, we may have to schedule this later in the day. If we can do this on an ongoing basis, we get the caregivers well-versed about what they will be doing independently and alone.
Maintenance Programs
We do not want to burden the caregiver by giving them an overly structured, complex maintenance program. I like to provide maintenance programs for range of motion and things of that nature that they can incorporate into their ADLs or activities that they are already doing. "While you are helping him with this, this is how I want you to range his hip and his shoulders." Or, "While you are bathing your dad, I want you to look at his skin for signs of breakdown." We need to incorporate these activities into the ADLs that are already going on in a natural routine.
For the exercise and maintenance programs that need to be separate, we need to ensure the caregiver is clear on the goal and comfortable carrying out the program. Once they are proficient in the program, we have to make sure that it is as simple as possible. No maintenance or exercise program should take more than 15 minutes for the caregiver to do in one sitting.
Environmental Modifications
You can suggest environmental modifications, but remember you do not want to do too many all at once. What adaptive equipment or durable medical equipment can they use? The best-case scenario is to complete a home evaluation, but you can give the caregiver a printed-out home eval with clear instructions if you are not able. In the age of smartphones, caregivers can take pictures or video a home evaluation.
Health Promotion
- Link our pts and caregivers with community resources:
- Respite
- Veterans’ services – can be admitted to hospitals
- Adult day services
- Area Agency on Aging
- Senior centers
- Alzheimer’s associations
- Funding options
- *partner with social workers
It is crucial to connect caregivers with community resources. About 85% of family caregivers in the United States do not receive any respite care. They may need help understanding what respite is, what organizations provide this service, how much it costs, how they can tap into it, and also give them permission that it is okay. Many caregivers feel guilty when they need a respite, but we need to let them know it is a safe and smart option. Veterans (or even spouses of veterans) can be admitted to VA hospitals for specific lengths of time for a respite stay.
Adult daycares range anywhere from $65 to $85 a day in most places. For some people, this is not a consistent option for them. However, they may use it once a week to attend Bible study or an exercise class. You may help them identify a practical cadence of using the adult day service. Long-term care insurance may pay for adult day services, but many clients want to reserve this benefit.
The Area Agency on Aging has so many different benefits. I have a friend taking care of her mom with early-onset Alzheimer's, and it has blown my mind what resources are provided. For example, last week, they provided someone to do some lawn care for her. She had a fallen tree, and they helped her clean it up. They also provide sitters at low to no cost and many other resources. Many senior centers have free programs. Clients who only need a low level of assistance or have mild cognitive deficits are good candidates for senior centers and Alzheimer's Associations.
There are other funding options like nonprofit agencies that provide caregiver grants. That same friend that I mentioned received a grant that allowed her to take her mom to one of those adult daycares for a month. We also need to make sure that we partner with social workers to ensure that we have tapped into all available resources in a particular area. You may also need to do a Google search for funding options in your area or empower the caregiver to do some research to see what is available.
How To Make It Billable
- CPT CODE 97633 Sensory integrative techniques to enhance sensory processing and promote adaptive responses to environmental demands, direct (one-on-one) patient contact, each 15 minutes
- CPT CODE 97535 Self-care/home management training (e.g., activities of daily living [ADLs] and compensatory training, meal preparation, safety procedures, and instructions in use of assistive technology devices/adaptive equipment), direct one-on-one contact, each 15 minutes
- CPT CODE 97537 Community/work reintegration training (e.g., shopping, transportation, money management, avocational activities and/or work environment/modification analysis, work task analysis, use of assistive technology device/adaptive equipment), direct one-on-one contact, each 15 minutes
- CPT CODE 97530 Therapeutic activities, direct (one-on-one) patient contact (use of dynamic activities to improve functional performance), each 15 minutes
- CPT CODE 97129 Therapeutic interventions that focus on cognitive function (e.g., attention, memory, reasoning, executive function, problem-solving, and/or pragmatic functioning) and compensatory strategies to manage the performance of an activity (e.g., managing time or schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact; initial 15 minutes
- CPT CODE 97116 Gait training (includes stair climbing)
- CPT CODE 97112 Neuromuscular reeducation of movement, balance, coordination, kinesthetic sense, posture, and/or proprioception for sitting and/or standing activities
https://www.theraplatform.com/blog/408/cpt-codes-occupational-therapy
Next, how do we make it billable? First, we need to make sure that we document what is happening. This is another reason it is so important to get our caregivers to come to our sessions. These are the codes that you can use. Everything that we discussed can fall under one of these categories. If you are doing environmental modifications, that can go under self-care, community integration, or even therapeutic activities. If we are drilling down to the overstimulating or understimulating behaviors, we can put that under 97633.
Sample Goals
- Goal 1: Caregivers will be able to describe signs that resident has unmet physical needs (hunger, bathroom, pants too tight, etc.) with MI, using written guide as needed.
- Goal 2: Caregivers will be able to describe at least 3 specific strategies to meet resident needs at her cognitive ability level with MI, using written guide as needed.
- Goal 3: Caregivers will use identified cues to support resident adherence to safety precautions 80% of the time with post-training and implementation of a striking visual cue.
- Goal 4: Caregivers will demonstrate ability to set up environment (bed positioned at lowest level, commonly used items in reach and visible) 100% of the time post-training to reduce pt risk of falls.
- Goal 5: With implementation of a striking visual cue, resident will orient to the bathroom with CGA and have no instances of urinating in inappropriate locations over a period of 2 weeks.
- Goal 6: With use of environmental modifications, caregiver training, or spaced retrieval, resident will wash hands thoroughly after using the bathroom at least 50% of the time
- Goal 7: Post-implementation of a visual reminder, resident will demonstrate ability to follow 3 fall prevention strategies related to her environment (such as clutter picked up off of floor) with SUP 80% of the time.
- Goal 8: After bathroom has been labeled and using striking/recognizable visual cues, resident will distinguish bathroom from other rooms in home and urinate in the correct room 100% of the time.
These are eight sample goals that you can use and plug and play for your specific client's needs.
Tips and Tidbits
- Explain the concept of sinkers and swimmers
- Embrace a culture of “no unsolvable problems”
- Stress schedules
- Teach systems
- Encourage responding vs. reacting
- Get assistance from family and friends
- Encourage support groups
- View caregiver as your secondary client
We need to explain the concept of sinkers and swimmers to our caregivers. This is a simple premise that in caregiving, you do not float. I have never met a caregiver that said, "Oh, this is so easy. I love every moment of it." There are no floater caregivers, but there are sinkers and swimmers, and we see both. I have seen clients, caregivers, and families who are stressed, depressed, constantly overwhelmed, and live in a constant state of feeling overwhelmed financially and time-wise. I have also seen caregivers with similar situations who have been able to methodically and strategically handle their situation without severe stress levels. We can encourage them that through the systems and resources that we are giving them, they can swim.
We also need to tell them that there is no unsolvable problem. I am confident that you have had a patient or caregiver that has said, "Oh, that's not going to work," when you have given them a suggestion. You provide them with community resources, and they say, "He is not going to go," or "I just don't feel comfortable." For transfer training, they may say, "Well, I don't like it that way." We have to convince and empower them that there is no unsolvable problem. We may not be able to fix it, but it is worth the effort if we can change, alter, or decrease it slightly.
We need to stress schedules. Often, caregivers say that there is no time for themselves. This is because they try to do everything at once without any boundaries. Clients need basic schedules for their days. Systems are different than schedules. A schedule says when, but a system says how. If a schedule says breakfast is at 9:00, then the system says each day I wake dad up an hour before breakfast because he does not handle transitions well. Or, the schedule says a doctor's appointment at 1 pm, but the system says, "Every time I have to schedule an appointment for my dad, I always schedule it in the evening because I know he is hard to get out the door in the morning."
Systems make the schedules flow. When educating caregivers, we need to stress the importance of implementing both a schedule and system which encourages responding versus reacting. Every behavior, incident, or situation that catches you off guard, you were not prepared or "scheduled" for it. And, when caregivers are off guard, they will act quicker, be more irritable, and make errors. Instead, we need to teach caregivers to be responders. For example, when packing the car, if you know your dad gets a little bit edgy at this time, have a distraction like a snack. We want our caregivers to be prepared with forward-thinking.
It is also essential for caregivers to get assistance from family and friends. Many of my caregivers are afraid to be burdens to others. We need to start helping them tap into their community resources of family and friends. Ask them to make a list of people they think would be open to helping them. We can then take that list and help them develop how they would ask for assistance. "Is there a day that you think you could help me?" And if the family member agrees to twice a month, you can then help frame the assistance needed. "Can you come and sit with dad?" We can help them think through different situations and make a loose schedule of other caregivers to help them.
We also need to encourage them to find support groups. We can be supportive, but we are not in their shoes. Other caregivers can be some of the most refreshing resources because it validates their emotions in a way that we cannot.
We need to view our caregivers as secondary clients. If we are dependent on the caregiver for our client's health, we need to make sure that the caregivers are well. They may be checking skin integrity every two hours or maintaining a home program, so we want the caregivers to be healthy.
Self-Care is Survival
Self-care is survival for our caregivers. We can teach our caregivers specific ways to tap into self-care.
- Physical:
e. Nutrition
In the physical area of wellness, we can ask how they are sleeping. The caregivers must be getting at least six hours of sleep consecutively. Can we help them find a way to tap back into getting better sleep? Are they stretching, walking, and exercising? What is their diet? I know you are thinking, "How can I do all that and bill for it?" When we get a caregiver into a session and talk about the patient's physical needs, including their sleep regimen, why can't we also speak to the caregiver about their sleep regimen? If we are talking about applying a gait belt and safely walking the client, can't we also ask, "How are you? How many steps are you getting in a day?" We are making this billable because we have incorporated the caregiver into the session.
- Emotional:
d. Journaling
For emotional, are they journaling? Are they going to therapy?
Social:
d. Positive social media
Social boundaries are a big one. Are they feeling empowered to say no to things to give them more time? What support systems do they have?
- Spiritual:
e. Sacred space
We can teach them about meditation and mindfulness. We may even do this with the client and incorporate the caregiver.
- Intellectual:
e. Establishing goals
Are they feeding their hobbies and creativity? As we look for activities for our clients that keep them busy, occupied, and stimulated, we can also talk to our caregivers about their hobbies and activities.
- Environmental:
c. Be intentional about enhancing the “feel” of home
We can work with the clients and caregivers in their environment.
- Vocational:
d. Change positions, schedules, or roles if necessary and possible
Systems and schedules to keep themselves more organized in their environment. Vocationally, they may change their position and role at work if necessary to keep up with their caregiving role.
Summary
- You can’t pour from an empty cup. Fill yourself up first.
Remember, caregivers cannot pour from an empty cup, so they must fill themselves up first. Being a full-time or even part-time caregiver requires self-care for survival.
Questions and Answers
Do you believe that females experience more burnout because females are expected to do more than males?
I wish I knew how many men were on the call before answering this question, but my honest answer is yes. For many, it is a cultural expectation. Some men are taking great care of their moms or spouses. However, it is often the daughter's role in the family to be more of the direct caregiver for mom and dad over the brothers. There are more women in the older age groups for spousal caregivers, so they are typically found in a caregiving role.
Have you ever been in a caregiver role and implemented any of these techniques?
My best friend has been a caregiver for two people. Her grandmother passed about two years ago, but she still cares for her mom. She moved from Chicago to become a full-time caregiver for her grandmother and mom. That is my closest experience. One of the situations that I remember is when her grandmother was experiencing her most significant decline and struggled with pain, muscle tension, and headaches. She asked if I could come over and help her. She was having trouble transferring her. I showed her some simple and basic transfer techniques. Her response was, "Oh my God, no one has ever shown me this, and my grandmother gets OT and PT services." The therapists were working with the grandmother on many different things but did not take the time to practice transfers with her. Sometimes we overlook incorporating caregivers into the treatment plan.
Can you talk more about how to help the caregiver who thinks they cannot be helped or who is resistant?
We have to stress that we have seen other people in the same or similar situations. Here is a standard script I use, "I've worked with people who have had a mom (or other loved one) who had as many behaviors as your mom's exhibiting. The difference between them and you is that they tried some of these techniques, and we problem-solved together." You want to encourage them to try.
I also like to refer to this as "pockets." "If you had small pockets of relief in your day, would that help?" I think that sometimes caregivers believe in totality. "If you can't fix mom, then you can't help me." We have to tell them, "No, I can't fix mom, but I can make mom a little bit easier to get along with around lunchtime because we have identified that is when she is most cognitively in tune and has the most strength. All the things you want to do with mom, do them at this time." You are not fixing but providing pockets of relief. Sometimes, you may not get a breakthrough, but if you have established a good enough rapport, they will start to problem-solve with you.
Do you consider someone in assisted living a caregiver? I have found this to be a different level of stress.
There are different levels of caregiving. There is a full-time caregiver or a person who does not have consistent assistance from anyone. They may get a couple of hours of nursing a couple of days a week, but a full-time caregiver is a person primarily in the home providing care. A person who lives with their spouse in assisted living is also considered a caregiver. Their level of stress is less. I like to correlate stress to how much time a person spends caregiving. If, for example, a person is a part-time caregiver, we can expect their caregiver burnout to be slower than someone providing full-time care.
References
Cook, S.K., Snellings, L. & Cohen, S.A. Socioeconomic and demographic factors modify observed relationship between caregiving intensity and three dimensions of quality of life in informal adult children caregivers. Health Qual Life Outcomes 16, 169 (2018). https://doi.org/10.1186/s12955-018-0996-6
Hiyoshi-Taniguchi, K., Becker, C. B., & Kinoshita, A. (2018). What behavioral and psychological symptoms of dementia affect caregiver burnout? Clinical gerontologist, 41(3), 249–254. https://doi.org/10.1080/07317115.2017.1398797
Leocadie, M. C., Roy, M. H., & Rothan-Tondeur, M. (2018). Barriers and enablers in the use of respite interventions by caregivers of people with dementia: an integrative review. Archives of public health = Archives belges de sante publique, 76, 72. https://doi.org/10.1186/s13690-018-0316-y
Otero, LMR. (2016). Burnout syndrome in family caregivers of dependents. International Journal of Asian Social Science, 6(1): 12-20. ISSN(e): 2224-4441/ISSN(p): 2226-5139
Spann, Alice & Vicente, Joana & Allard, Camille & Hawley, Mark & Spreeuwenberg, Marieke & Witte, Luc. (2019). Challenges of combining work and unpaid care, and solutions: A scoping review. Health & Social Care in the Community, 28. 10.1111/hsc.12912.
Yıldızhan, E., Ören, N., Erdoğan, A., & Bal, F. (2019). The burden of care and burnout in individuals caring for patients with Alzheimer’s disease. Community mental health journal, 55(2), 304–310. https://doi.org/10.1007/s10597-018-0276-2
Citation
Rollins, M. (2021). Preventing caregiver burnout. OccupationalTherapy.com, Article 5493. Available at https://OccupationalTherapy.com
