Editor's note: This text-based course is a transcript of the webinar, Proprioceptive Rehab: 30 Practical Ideas And Interventions For The Neuro Patient, presented by Andrea Salzman, MS, PT.
Learning Outcomes
- After this course, participants will be able to identify three elements of active movement and balance training interventions to support ADL and IADL participation.
- After this course, participants will be able to identify a stance and steppage drill and progress it through 2-3 variations and the appropriate use of three passive movement training interventions for ADL support.
- After this course, participants will be able to list elements of three somatosensory stimulation training interventions and recognize the benefit of using a single “named” approach to proprioceptive training versus using an eclectic mix.
Introduction
Welcome back to those of you who have attended my previous courses. I'm excited to share a plethora of ideas with you today. One of the most valuable lessons I've learned in teaching is that learning occurs in stages: you gain a bit of knowledge when you hear it, more when you see it, even more when you do it, and significantly more when you tackle it as a challenge. There's a profound psychological inclination towards embracing challenges, and further learning comes when you teach and correct others.
While we may not cover all these aspects today, we'll play around with concepts, primarily focusing on active techniques. The bulk of today's session will be dedicated to active movement interventions. We'll explore various practical ideas, touching upon all 30 techniques and then some, emphasizing making them enjoyable, innovative, and grounded in evidence-based practices.
Today, we aim to breathe new life into these familiar routines, exploring ways to enhance them creatively.
Why Train Proprioception?
- Think of it this way.
- Kick back in your chair by the fireplace (move the cat) and start reading a truly engrossing book.
- To your right is a 12-ounce can of (insert beverage of choice).
- Intermittently, your hand reaches out for the can, brings it to your lips, and – after your body has registered a truly minor change in weight from drinking – returns it to hearth.
- All of this occurs without you registering that you did any of it.
Why is proprioception even a concern, you may wonder? Allow me to share how I approach this topic with my patients. While I may not consider myself an exceptional therapist, I deeply value human connection, storytelling, and the art of listening. When a patient expresses confusion, saying, "I don't understand why we're focusing on proprioception," I welcome the opportunity to engage them in a narrative that brings clarity.
Picture yourself in your favorite armchair by the fireplace, perhaps shooing away the cat to claim your cozy spot. You're engrossed in a book, completely immersed in the narrative. Beside you sits a 12-ounce can of your preferred beverage. As you read, you occasionally reach for the can, effortlessly bringing it to your lips for a sip. Without conscious effort, your body adjusts to the slight decrease in weight as you take a sip, and then you return the can to its place by the hearth. You remain absorbed in your reading, perhaps diving into a hefty tome like "War and Peace" (though maybe not enjoying it as much as you'd like!). The entire process unfolds seamlessly, almost unconsciously, without you actively registering each movement or interaction with the soda can.
- Now, imagine I sneak up next to you, grab the can, and take a huge gulp without you noticing.
- When next you reach out to grab the can, there is a moment when your brain has prepped your muscles to lift 12 ounces and your muscles apply too much force, resulting in a disjointed muscular effort to lift the can.
- For most of you, your body’s proprioceptive systems then perform a minor miracle and allow you to notice, halt and adjust… all in a fraction of a second.
- The rest of the drink is saved (our friendship, however, is toast).
- But what if your proprioceptive system was not functioning correctly?
Now, let's consider a scenario where I stealthily approach you from behind, swiftly grabbing the can and taking a hefty gulp without your notice, then returning it to its place beside you. As you reach out for the can again, there's a split-second moment where your hand begins to rise, but your brain swiftly receives feedback from various sensory receptors—the Golgi tendon organs, muscle spindles, and more. This intricate feedback loop signals a discrepancy between the expected weight (based on previous sips) and the actual weight of the can.
Instantly, your brain commands your muscles to halt and adjust, preventing you from exerting excessive force. It's a marvel of proprioception—a system that allows you to notice, correct, and adapt within a fraction of a second, ensuring the safety of your beverage (and perhaps our friendship, depending on your reaction!).
However, what if this proprioceptive system fails to function correctly? From patients with high ankle sprains to those with Parkinson's, multiple sclerosis, cerebral palsy, and individuals recovering from surgeries like total knee replacements, the impact can be profound. For instance, post-surgery, patients may remark that their knee doesn't "feel right." This disconcerting sensation arises because surgical procedures often disrupt proprioceptive feedback loops, requiring the body to recalibrate its understanding of movement and position.
Similarly, conditions like stroke, Parkinson's, and MS can impair proprioceptive function, complicating movement coordination and balance. With MS, the unpredictable nature of symptoms exacerbates the challenge, as sensations fluctuate over time.
So, what interventions can we implement to address these proprioceptive deficits?
- Proprioception has only been in our lexicon for slightly more than a century.
- The term was coined at the beginning of the 20th century in a book titled The Integrative Action of the Nervous System.
- Unfortunately, no one since that time has ever agreed what should be meant by the term.
- It’s a Latin-derived term -- which always helps add to the confusion -- but it was first crafted to stitch together the concepts of “oneself” (proprius) and “perception.”
(Sherrington, 1910)
Interestingly, the term "proprioception" has only been part of our lexicon for about a century. It was coined at the beginning of the 20th century in a book titled "The Integrative Action of the Nervous System." Despite its relatively recent introduction, there's been ongoing debate about its precise meaning. Different interpretations abound, leading to potential misunderstandings when discussing proprioception.
Let's establish a shared definition to guide our discussion to mitigate this confusion. Proprioception, derived from Latin roots, combines "proprio," meaning oneself, and "perception," referring to one's perception or awareness of oneself.
It's worth noting a fun linguistic tidbit: around 80% of words with three or more syllables are of Latin origin, adding a layer of complexity to our understanding. Essentially, proprioception encompasses our knowledge and perception of ourselves, a fundamental aspect of our sensory experience. Figure 1 is an illustration of proprioceptive concepts.
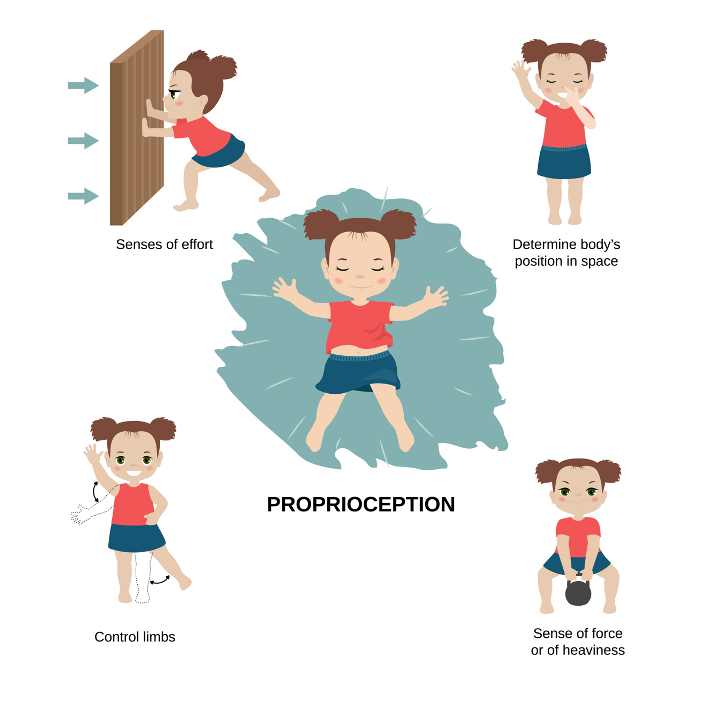
Figure 1. Illustration of proprioceptive concepts. Image: Continued (licensed from Getty Images).
- Proprioception is a great big amorphous blob of balance reactions, coordinated movement of limbs, and a perception of how our various parts function in relation to one another.
- A ballpark definition might read:
- “Our awareness of where our body parts exist in space, including a sense of location, space, and motion.”
(Sherrington, 1910)
Why should we train it? Figure 2 shows my son.

Figure 2. The author's son runs outside towards a puddle.
Imagine yourself running excitedly, almost feeling the anticipation of splashing into the water. When I visualize proprioception, I see it as this vast, shape-shifting entity encompassing balanced reactions, coordinated limb movements, and a deep understanding of how each part of our body functions in relation to the others. Remembering this interconnectedness, how every component communicates with the others is crucial.
For the duration of our session, let's adopt this broad definition: proprioception is our comprehensive awareness of our body parts' positions in space, incorporating a sense of location, spatial orientation, and motion. However, it's important to acknowledge the interchangeability—or sometimes the confusion—between proprioception and kinesthesia. Some argue that kinesthesia is a subset of proprioception, while others suggest it is synonymous. Our focus today will be on this holistic understanding of proprioception and its role in movement and coordination.
- It helps to think of proprioception as our body’s capacity to change our movements “on the fly.”
- The body takes note of other input – visual, tactile, and otherwise – and responds.
- Accurate movement of our limbs is dependent on a combination of the following:
- forward inputs sent from the brain to the body; and
- sensory inputs that can help modulate the forward commands.
- When proprioceptive sensory inputs are absent, the end result is a loss of direction and erratic judgment of the amplitude of movement.
Again, proprioception is our body's capacity to change our movements on the fly (Figure 3).

Figure 3. The author's son jumps into a puddle.
Indeed, our bodies constantly integrate sensory inputs—visual, tactile, and more—and respond accordingly. The brain sends commands to our limbs for precise movement, while sensory feedback modulates and refines these commands. Today, we'll delve into this intricate interplay between sensory inputs and motor responses.
When proprioceptive inputs are compromised or absent, the consequences can be significant. Movement becomes imprecise, directionless, and erratic. We struggle to gauge the extent and speed of our movements accurately. Consequently, falls become more frequent, and safety becomes a pressing concern. For individuals with conditions like high ankle sprains, the lack of proper proprioceptive feedback perpetuates a cycle of injury as the body fails to adjust and stabilize effectively. Understanding and addressing these proprioceptive deficits is crucial for improving movement quality and preventing complications.
- There is a conscious and an unconscious element to proprioception.
- Some academics use the term “kinesthesia” for the conscious elements and reserve “proprioception” for the unconscious ones.
- However, many people consider this a distinction without a difference.
- For the purposes of this course, we will consider the term proprioception as an all-inclusive of both.
(Konczak et al., 2009)
Proprioception encompasses both conscious and unconscious elements. While some academics delineate between proprioception and kinesthesia based on conscious and unconscious aspects, we'll take a more inclusive approach in this session.
Rather than getting bogged down in semantic distinctions, we'll treat proprioception as a comprehensive term, encapsulating both conscious and unconscious components. This allows us to focus on the broader understanding and practical applications of proprioception without getting mired in academic debate.
An Overview
- So, where to start? In 2015, a group of researchers (Aman et al) published a systematic review on proprioception which we are going to use to organize our discussion.
- The authors wanted to know which treatments commonly used in rehab were effective, so they started with a definition.
- Proprioceptive training is:
- an intervention
- that targets
- the improvement
- of proprioceptive function.
- It focuses on
- the use of somatosensory signals
- such as proprioceptive or tactile afferents
- in the absence of information from other modalities (such as vision).
- Its ultimate goal is
- to improve or restore
- sensorimotor function.
(Aman et al., 2015)
As someone with three decades of experience in therapy and currently serving as the director of Aquatic Therapy University, my journey has taken me through various roles, from skilled nursing departments to outpatient clinics. While I may not consider myself the best at any one thing, my curiosity drives me to continuously seek new knowledge and approaches.
Today, I want to explore proprioception through the lens of a systematic review I came across in 2015. Though the study may be a bit dated now, it provides a valuable framework for understanding the different methods of proprioceptive training. The authors sought to evaluate the effectiveness of various rehabilitation treatments, with a particular focus on proprioceptive training.
Let's start by dissecting their definition of proprioceptive training. According to the authors, proprioceptive training is an intervention aimed at improving proprioceptive function. It involves leveraging somatosensory signals, such as proprioceptive and tactile feedback, in the absence of input from other sensory modalities like vestibular and visual cues. While the definition may seem a bit circular, it underscores the importance of targeting proprioceptive function specifically in rehabilitation interventions.
The ultimate goal of this is to improve or restore sensory motor function.
- The researchers clumped the interventions into these categories:
- Categories:
- Active Movement/Balance Training
- Passive Movement Training
- Somatosensory Stimulation Training
- Combined/Multiple Systems
- Somatosensory Discrimination*
- *Aman et al also examined Somatosensory Discrimination, a category we will not explore today. It included interventions that focused on discrimination between opposing somatosensory stimuli. These discrimination tasks included haptic discrimination (e.g., active exploration of objects with the hand), tactile discrimination, wrist joint velocity discrimination, and wrist or ankle joint position discrimination.
The systematic review conducted by Aman et al. categorized the various proprioceptive training interventions into distinct classifications based on their findings. Today, we'll focus primarily on two of these classifications: active movement and balance training. This segment will constitute the bulk of our discussion, as these methods substantially improve proprioceptive function.
Additionally, we'll touch on passive movement training and somatosensory stimulation training combined in multiple systems. As therapists, we often employ an eclectic approach, incorporating various techniques to comprehensively address our patients' needs.
However, we'll not talk about somatosensory discrimination in this session. This category encompasses haptic discrimination, tactile discrimination, velocity discrimination, and position sense of the wrist and ankle. While these aspects are crucial in proprioception, we'll reserve them for future discussions and focus on the active movement and balance training methods today.
Active Movement and Balance Training
- The first category of proprioceptive training we will discuss is active movement and balance training. This category includes interventions that require participants to actively move a limb, a limb segment, or their entire body.
- Active Movement/ Balance Training*
- Balance training
- Multi-joint active movement
- Single-joint passive versus active movement
- Multi-joint passive versus active movement
- According to the study, therapists are advised to spend their time providing interventions that encourage active movements and balance training and not creating passive training scenarios.
- Because of this, we will focus most heavily on the Active Movement/ Balance Training category.
- *Almost half of the studies examined fell into the Active Movement/ Balance Training category.
The first category of proprioceptive training we'll delve into is active movement and balance training. Now, I'm not just talking about standing on one's feet when I refer to active movement and balance training. We'll explore many ideas, including techniques for getting on and off the floor, out of the tub, or in and out of bed. In fact, I've previously taught a class titled "Bed-Based Exercises," originally coined "Never Leave the Bed," focusing on exercises that can be performed entirely while in bed.
This category encompasses interventions that require participants to actively engage their limbs or entire body. Within this framework, we'll examine various subcategories, such as balance training, multi-joint active movement, and the comparison between passive and active movements at single and multi-joint levels.
The overarching message from the 2015 study—and one that I believe still holds true—is that therapists are encouraged to prioritize interventions that promote active movements and balance training over exclusively passive approaches. While passive training may have its place, the emphasis should be on encouraging active engagement. Later on, I'll share a comprehensive overview of available techniques, but for now, let's focus on the fundamental importance of active movement and balance training in proprioceptive rehabilitation. This is where your core strategies should lie.
- Many studies included in the systematic review made use of a huge variety of active balance activities, including:
- walking,
- single leg balance exercises,
- stance exercises,
- sit-to-stand exercises,
- standing, walking,
- stair-stepping activities,
- bouncing on stable and unstable surfaces, and
- sport-specific exercises.
Here are some of the things that they listed as active balance activities.
- All the studies showed improvement from pre- to post-balance intervention with a range of improvement spanning from 16% to 97%.
- Overall, balance regimens that lasted 6 weeks or longer were the most popular and showed the greatest potential.
- With that in mind, let’s look at some specific examples of Active Movement and Balance Training, including loads of newer trials that were not included in the 2015 systematic review.
In their review, all the studies examined showed some improvement from pre to post-balanced interventions, ranging from 16% to nearly 100%. Interestingly, balanced regimens lasting six weeks or longer were the most commonly studied and appeared to yield the most promising results. This underscores the importance of sustained and consistent interventions in achieving meaningful improvements in proprioceptive function.
An important aspect highlighted in the study was the potential pitfalls of discontinuing balanced interventions prematurely. While programs offered at assisted living and independent living senior centers led by occupational therapists, physical therapists, or fitness instructors can yield significant improvements in mobility, there's a caveat. Studies have shown that individuals who attend fewer than 50 training sessions and discontinue prematurely may inadvertently increase their safety and risk management problems. This paradoxical outcome occurs because improved mobility and confidence may lead individuals to take greater risks in their daily activities, which can result in accidents or falls.
Therefore, it's essential to consider the duration and continuity of balanced interventions to ensure their effectiveness in mitigating risks and enhancing overall function. Now, let's explore one of the specific examples highlighted in the study: stance and steppage exercises.
Active Movement and Balance Training: Stance and Steppage
- What is Stance and Steppage Training? Gait is comprised of alternating states of single-leg stance and stepping. Because of this, it makes sense to focus on both sides – stance and steppage – when addressing proprioceptive skill after a neuro event.
- Single-leg stability is a very important component of gait and transfers for all ambulatory individuals.
- While the dynamic limb is moving, the stance leg is required to fully support the body, often experiencing greater challenges in stillness than the moving limb does in action.
- Consider a car or a tub transfer that requires prolonged periods of single-leg stance; these unstable activities respond well to stance and steppage training.
- If not addressed, these activities can result in disastrous consequences, so they require special attention.
The significance of stance and steppage in maintaining gait and functional stability cannot be overstated. These movements, encompassing single-leg stance and controlled stepping, form the foundation of everyday mobility. Whether walking, transitioning between sitting and standing, or simply balancing, they constantly alternate between stability and controlled movement.
In rehabilitation, particularly after neurological events, addressing stability and mobility is crucial, even when full ambulation isn't achievable. Activities such as sitting on the edge of a bed or attempting to rise from the floor demand a strong focus on stability. I recall a poignant case where a patient with MS faced severe contractures and mobility limitations, prompting his overwhelmed wife to seek assistance.
Rather than immediately targeting mobility, we prioritized enhancing proprioceptive awareness and posture. Through weeks of static standing exercises and mindful breathing techniques, we aimed to improve his body alignment and stability. Emphasizing foundational stability and proprioceptive awareness yielded remarkable progress, eventually enabling him to walk to the bathroom—an inspiring testament to the effectiveness of patient-centered rehabilitation.
Single-limb stability is pivotal for various tasks, including car or tub transfers, which necessitate extended periods of single-leg stance. Neglecting to address this aspect can result in dire consequences, such as falls or injuries during transfers. Hence, it's imperative to ensure individuals can manage prolonged single limb stances safely, whether in rehabilitation settings or daily activities.
In my practice, I've encountered instances where patients become overly reliant on seated exercises, overlooking the importance of weight-bearing and standing stability. This oversight can create a false sense of security and heighten the risk of falls. Consequently, I've often needed to adapt rehabilitation plans and employ problem-solving strategies to address these challenges effectively.
Sample Drill: Single-Leg Static Holds
- SAMPLE DRILL: Single-leg static holds: This static activity is the foundational element for all single-leg stability drills to follow.
- The core exercise involves balancing the body weight on one leg at a time and maintaining a quiet stance. Perform this exercise with both eyes open and holding onto a stable surface
- The patient may be cued as follows: Stand on your left leg and raise your right foot off the ground. Flex (bend) your left knee slightly and hold that position for 2–3 seconds. Repeat with longer hold times. Repeat with the other leg.
- SAMPLE PROGRESSIONS:
- Remove hand hold
- Add a head turn
- Add arm swing
- Throw and/or catch a ball
- Close eyes
Here's a practical exercise focusing on single limb stance, a fundamental component for enhancing stability and proprioception. Occupational and physical therapy practitioners can collaborate to modify this drill to suit individuals' needs and advancement.
Engaging in a single-limb stance while performing everyday tasks like brushing teeth can heighten proprioceptive awareness. Encouraging the use of the non-dominant hand further stimulates diverse neural pathways, fostering cognitive and motor skill development.
To advance this drill, several considerations come into play. Starting with individuals using visual support, such as holding onto a countertop or utilizing assistance for balance, offers stability. As proficiency increases, minimizing visual input by closing eyes or fixing the gaze on a distant point challenges balance and proprioception further.
Surface stability is another aspect to address. Beginning on a stable surface like a bathroom floor provides a solid base for beginners. Progressing to an unstable surface, like a foam pad or balance board, introduces additional challenges, necessitating greater stabilization efforts.
Integrating arm movements can add complexity as individuals gain stability and confidence in single-limb stances. Alternating lifting each hand, reaching forward or sideways, or performing tasks like holding a toothbrush while brushing teeth can challenge balance and coordination.
Transitioning from a static single-limb stance to dynamic movements enhances proprioception and functional abilities. Incorporating activities such as toe taps, knee lifts, or subtle weight shifts while maintaining balance prompts individuals to adapt and adjust realistically.
Gradually extending the duration of single limb stances and increasing the complexity of accompanying tasks effectively advances individuals' abilities. Starting with shorter intervals and progressively lengthening duration fosters endurance and confidence.
By systematically adjusting these variables based on individuals' progress and capabilities, we can tailor the single limb stance drill to align with their specific rehabilitation objectives and facilitate functional independence.
A progression can be seen in Figure 4.

Figure 4. Example of single-leg static hold.
As individuals advance in single limb stance training, therapists can gradually reduce reliance on hand support to challenge balance and proprioception. This shift encourages greater weight-bearing on the standing leg and fosters stability.
Introducing head turns while maintaining a single limb stance disrupts the body's equilibrium, demanding increased proprioceptive input. By incorporating different head directions or alternating between eyes-open and eyes-closed positions, individuals can further challenge their balance and spatial awareness.
Incorporating cognitive tasks, such as naming objects in various directions or recalling specific visual cues, adds a cognitive aspect to proprioceptive training. This cognitive overlay prompts individuals to integrate sensory information with cognitive processing, enhancing overall functional capacity.
Including arm swings, reaching, or engaging in throwing and catching a ball while in single limb stance introduces dynamic movement patterns and heightens the challenge to balance control. Varying the direction and intensity of arm movements enables individuals to improve coordination and proprioceptive feedback.
Introducing unpredictable elements like random perturbations or sudden changes in movement direction simulates real-life scenarios and enhances reactive balance responses. This progression encourages individuals to adapt and adjust quickly, improving overall stability and fall prevention skills.
Lastly, closing the eyes during single limb stance eliminates visual input, necessitating individuals to rely solely on proprioceptive feedback for balance maintenance. This advanced progression further challenges proprioceptive awareness and serves as an effective method to assess and enhance balance control in diverse environments.
Clinical Pearl: "Embrace Failure"
- Idea: Build the assumption of failure into sessions.
- Reinforcement motor learning is an improvement in motor behavior driven by binary outcome-based feedback.
- After a movement's success or failure, the learner does not receive information about how the movement needs to be modified to succeed. He knows he failed or succeeded.
- Think “knowledge of results”.
- Either the person stays on one foot for 10 seconds -- or he does not. Success will lead him to stick with what works. Failure will lead him to recalculate and explore different movements.
- He will then select actions with the highest probability of success while avoiding actions with a lower probability of success.
(Leech et al., 2022)
Advocating for integrating the assumption of failure into therapy sessions may seem unconventional at first glance, but it aligns with the principles of motor learning. Motor learning encompasses various approaches, with reinforcement motor learning being a significant one. This form of learning involves improvements in motor behavior driven by binary feedback—success or failure—without detailed guidance on adjusting the movement.
Emphasizing knowledge of results over knowledge of performance is key to this approach. Knowledge of results focuses on whether the desired outcome was achieved rather than the specific execution of the movement. For example, success in a therapy session might entail maintaining balance on one leg for a set duration, while failure indicates loss of balance.
By structuring therapy sessions with the assumption of failure, therapists provide opportunities for patients to learn from their experiences. After each attempt, patients are encouraged to reflect on what transpired and why, facilitating a deeper comprehension of their movements and enhancing motor learning.
This approach is particularly valuable in settings like skilled nursing facilities, where patients may struggle with functional ability declines. By embracing failure as an integral part of the learning process, therapists empower patients to take charge of their rehabilitation journey and strive for meaningful progress.
Sample Drill: Forward and Backward Swings
- SAMPLE DRILL: Forward-backward swings (hip flexion/extension/ abduction/adduction): In this variation, an extension of the hip may provoke more co-contraction of the gastrocnemius/soleus and anterior tibialis muscles to stabilize the lower leg with the anterior/posterior motion. The patient is cued to maintain a stance on one leg while moving the other leg forward and back and side to side.
- SAMPLE PROGRESSION:
- Freeze with verbal (or gestural) cues at different positions
- Cross midline
- Perform Figure 8’s
- Move in unpredictable ways
- Vary the speed of movement
- Vary the amplitude of movement
Figure 5 shows forward and backward swings.

Figure 5. Example of forward-backward swings.
As you observe the movement from multiple perspectives, various ways enhance its complexity and challenge proprioception. As an occupational therapist, incorporating functional tasks such as pulling on pants or simulating stepping over obstacles with a gym hurdle can add practicality to the exercise. Introducing additional elements like weights, a balance pad, or dancing to slow music can further engage proprioceptive feedback.
Here's a sample progression to consider. Begin by incorporating a metronome to establish a rhythmic cadence, challenging individuals to synchronize their movements with the beat. Adding verbal or gestural cues to freeze at different positions introduces unpredictability and engages different brain areas.
Encourage direction changes and crossing midline to promote cognitive engagement while enhancing proprioceptive awareness. Activities like Simon Says or performing figure eights introduce variation in movement patterns, keeping the exercise dynamic and engaging.
Introduce unpredictable movements and adjust the speed and range of motion to further challenge proprioceptive skills. Games like Red Light Green Light can add fun while reinforcing proprioceptive awareness and responsiveness.
By layering these progressions systematically, therapists can create a dynamic and challenging environment that promotes continuous improvement in proprioceptive skills.
Clinical Pearl: "Repeat Without Repetition"
- Idea: Remember: Practice is a particular type of repetition…without repetition.
- According to Leech,
- practice does not consist of
- repeating the means of solution of a motor problem
- time after time, but
- in the process
- of solving this problem again and again
- by techniques
- we have changed and perfected
- from repetition to repetition.
- The participant must understand the goal and make intentional changes to their movements to solve the movement problem and achieve that goal.
- Think “knowledge of performance”.
(Leech et al., 2022)
The concept of "repeat without repetition" underscores the importance of practicing motor skills in a manner that facilitates learning and adaptation. Rather than mechanically repeating the same movements, the emphasis is on problem-solving and refinement with each repetition.
As per Leech's study, the essence of the practice lies in not merely repeating the same solution to a motor problem but in exploring different techniques and approaches to solve it. This approach encourages learners to actively refine their performance with each iteration, incorporating feedback and self-assessment to drive improvement.
Implementing this method involves providing knowledge of performance, where specific feedback is offered on various aspects of the movement, along with suggestions for enhancement. For instance, therapists may highlight how a particular movement affected the center of mass and recommend adjustments to mitigate such effects.
By prompting learners to critically evaluate their performance and adapt their approach from one repetition to the next, therapists can nurture skill development and prevent stagnation. This approach ensures that practice remains dynamic and conducive to continuous learning rather than being characterized by repetitive actions devoid of progress.
Sample Drill: Leaning
- SAMPLE DRILL: Leaning Drills: In this exercise, the abdominals and erector spinae will engage in oscillating stabilization of the trunk. In addition, the alternating leans may provoke co-contraction of the gastrocnemius/soleus and anterior tibialis muscles to stabilize the lower leg with the anterior/posterior motion.
- The patient may be cued as follows: Stand next to a wall, facing it. Place your palms against the wall and stand slightly away from it.
- Let go of hand contact with the wall and attempt to maintain a forward lean toward the wall without ever touching the wall. The lean should come from the ankles and not the hips or waist.
- Reposition yourself with your back to the wall. Repeat with backward lean.
- SAMPLE PROGRESSIONS:
- Move farther from the wall
- Lean closer to the wall (without contact)
I want to move on to variations that are real life. Figure 6 shows one of my favorite stability exercises.

Figure 6. Example of leaning drill.
The leaning drills described here are invaluable for stabilizing the trunk and engaging the abdominals and erector spinae. In these drills, individuals lean forward or backward from the ankles while maintaining proper posture, with chin and chest held up. Initially, hand contact with the wall aids in maintaining balance, but as individuals progress, they attempt the lean without support, relying solely on their ankle excursion for stability.
These drills may seem deceptively simple, but the subtle ankle movements required can pose a significant challenge. Participants are encouraged to imagine leaning in as if attempting to kiss a post-it note on the wall, emphasizing the forward or backward lean without bending at the waist.
Progressions for these drills include increasing the distance from the wall, reducing or eliminating hand contact, and extending the range of lean while maintaining proper form. The goal is to progressively challenge ankle stability and trunk control, leading to enhanced balance and proprioceptive awareness.
While these exercises may evoke humor with instructions to "kiss the wall" or humorous reactions to the challenge, their effectiveness lies in the nuanced ankle movements that contribute to overall stability and functional mobility. Incorporating these drills into therapy sessions, whether in a clinical setting or the pool, can yield remarkable improvements in balance and postural control.
Clinical Pearl: "Edgecraft"
- Idea: Find an edge of competency… and push past it.
- In 2010, I started taking innovative ideas from other fields and apply them to therapy. One of my favorites is the idea of edgecraft.
- Seth Godin coined the term “edgecraft” to describe a marketing technique for developing new and remarkable ideas by finding and pushing the edges of a product or service.
- We can do Edgecraft by finding and pushing past the edges of competency.
- Running out of progressions?
- Think “Edgecraft.”
(McGillicuddy, 2005)
The concept of "Edgecraft," inspired by Seth Godin's marketing principles, applies to therapy by pushing individuals to their natural boundaries of competency and then guiding them to surpass those edges. Just as successful companies play to their strengths and push beyond their limits, therapists can identify where clients naturally struggle and focus on pushing past those barriers.
In therapy sessions, the goal is to constantly challenge individuals at the edge of their capabilities. This means avoiding staying within their comfort zones and instead pushing toward the limits of their abilities. For example, if a client struggles with maintaining balance when leaning forward, the therapist may focus on exercises that require forward lean while providing support or guidance to ensure safety.
One application of Edgecraft in therapy is in-bed mobility exercises. Instead of practicing every aspect of bed mobility, therapists can pinpoint the moment clients typically falter, such as when transitioning from lying down to sitting up. By focusing on this challenge, therapists can design exercises and interventions to help clients overcome it, effectively pushing past their natural barriers.
Edgecraft encourages therapists to think creatively and strategically about pushing clients beyond their comfort zones while ensuring safety and progress. By identifying and targeting individuals' natural edges, therapists can facilitate meaningful improvements in functional abilities and overall independence.
Sample Drill: Golfer's Lift
- SAMPLE DRILL: Golfer’s Lift Drills: In this exercise, the entire weight of the body is stabilized on a single stance leg. In addition, the body’s center of mass rotates outside the body’s base of support and remains in flux throughout the drill.
- This exercise has been dubbed a golfer’s lift as it simulates a golfer leaning over and snagging a golf ball off the green.
- The patient may be cued as follows:
- Stand with one leg in front of the other. (If the patient cannot safely stand in a mock tandem stance, do not continue)
- Lean forward as you were going to pick up a small, light object (golf ball, keys) off the floor.
- Allow your back leg to lift up as you lean down, in order to maintain a neutral curve in your lower back.
- Return to standing and repeat with the other leg.
- SAMPLE PROGRESSIONS:
- Pick up smaller or flatter items
- Dip deeper or freeze during dip
Here's our sample drill, golfers lift, in Figure 7.

Figure 7. Example of a golfer's lift.
Picking up an object from the floor while balancing on one leg engages the entire body's stability and proprioception. It simulates real-life movements like reaching for objects or bending down to pick something up, requiring coordination and balance.
To progress this exercise in occupational therapy, you can introduce variations that mimic everyday tasks. For example, picking up smaller or flatter objects challenges precision and fine motor skills. Varying the object's height requires adjustments in reach and balance, further enhancing proprioceptive awareness.
In physical therapy, adding a mini-squat to the movement increases lower body strength and stability. Combining elements of a squat with the picking-up motion mimics functional movements like transitioning from sitting to standing. Freezing at different positions during the movement challenges balance control and promotes muscle coordination.
Modifications can be made for clients at different skill levels to suit their abilities. Beginners may start with larger, easier-to-reach objects and progress to smaller or more challenging items as they improve. Adjusting the depth of the squat or the distance of the reach allows for gradual progression based on individual capabilities.
To enhance the exercise further, incorporating a stability challenge by having clients hold onto a stable object, like a chair, while performing the movement adds an additional layer of difficulty. Requiring clients to lift their leg without pushing off the chair promotes balance and strengthens the muscles that maintain stability.
By tailoring the exercise to individual needs and skill levels and incorporating various progressions, therapists can effectively improve their clients' balance, coordination, and functional mobility.
Clinical Pearl: "Add a Layer"
- Idea: Don’t change what you are doing. Add a layer instead.
- Layers are easy ways to stick with the same concept but explore real-world scenarios to challenge the patient. Here are 13 layers for you to play with.
- Velocity
- Amplitude
- Endurance/ Work
- Feedback
- Supportive Device Used
- Assistance Given
- Developmental Sequence
- Regional Approach
- Variability
- Component Parts
- Task Attention
- Environmental Modification
(Fell, 2004)
Picture layers, not the kind you wear in winter, but layers of challenges and strategies that push boundaries and stimulate growth. This way of thinking started with inspiration from an article in 2004. Each layer adds a new dimension, a fresh perspective to our approach. But we're not talking about ordinary layers; we're talking about 13 layers of possibility, each one offering a unique angle to tackle therapy challenges.
Let's break it down. Velocity sets the pace, dictating the speed at which movements unfold. Amplitude expands horizons, stretching the limits of motion to new heights. Endurance and work test the limits of stamina, pushing the boundaries of persistence and effort. Feedback becomes our guiding compass, while supportive devices and assistance provide a safety net as we navigate uncharted territory. We can also look at developmental sequencing, tracing the footsteps of motor development. A regional approach zooms in on specific areas, directing focus, and variability adds a twist, shaking up routines with unexpected challenges. Breaking down into component parts dissects complex movements into manageable pieces, paving the way for mastery step by step. Task attention introduces cognitive elements, merging mind and body. Dual-task processing throws a cognitive curveball, testing multitasking skills and balance in tandem. Environmental modifications alter the landscape, transforming surroundings to simulate real-world scenarios and enhance adaptation. With each layer, therapy becomes a canvas for creativity and exploration.
Sample Drill: Step-Ups and Step-Overs
Step up and step over demo is shown in Figure 8.

Figure 8. Examples of step-ups and step-overs.
The drill of stepping over obstacles is a staple in every therapist's repertoire. As we guide our patients through this exercise, we ensure they traverse cautiously, mindful of each step to avoid missteps.
Picture this: standing at the base of the stairs, poised and ready. With one leg raised, the challenge begins—to tap the step without bearing weight. It's a delicate balance, a controlled maneuver akin to a dance with gravity. Shift the center of mass forward, tap, and then gracefully retreat. Repeat, aiming for the elusive target of eight taps in 20 seconds—a feat of skill and precision.
But why stop there? We can progress to add eccentric control—the art of lowering oneself down from the step. It's a test of strength and control. No more falling off the step; instead, we descend gracefully, like elevators traveling between floors.
Let's not forget variety. We can have them step over the box, return to the start, and change directions—forward, sideways, even backward. Each variation adds a layer of complexity, a new twist to keep the mind engaged and the body challenged.
Clinical Pearl: "Suck the Marrow"
- Idea: Find something that resonates with both of you… and stick with it.
- Have you ever taken an aerobics class with an instructor who introduced new moves WAAAAAYYYY too soon? That was me. After 16 counts of “high knees” I’d think, surely, they are bored. So I’d move on.
- Actually, most hadn’t even noticed that I had changed from “low knees” to “high.”
- The ones who had noticed were scrambling to visually assess and translate it to action.
- The quickest ones were doing “high knees” but had not gotten a rhythm.
- I was a terrible aerobics instructor.
- I am a decent therapist because I find something that works and stick with it long enough for us both to find our rhythm.
(Mikal-Flynn et al., 2018)
Embrace the challenge, and remember the wise words of wisdom: "Suck the marrow from the bone.'" As a proud Tennessean, I know something about making the most of every opportunity.
Let me break it down for you. You might call it bone broth, but we call it 'sucking the marrow.' Why spend five bucks on a container of bone broth when you can simmer your bones and extract all the goodness? It's like savoring every last drop of a delicious meal, lingering over that final taste because that's where the real flavor lies. So, when I teach my students, I always tell them: 'Whatever you're doing, do it halfway.'
At first, they're puzzled. 'What does that mean?' they ask. But then they give it a try. And you know what? They find a sense of calm, a deeper connection to the task. So I push them further: 'Now, whatever you're doing, cut it in half again.' It's about finding that sweet spot, that rhythm that resonates with the patient and the therapist.
Back in college, I was a standout aerobics student, but when I became a step aerobics instructor, I faced a new challenge. I'd lead the class through 16 counts of a move, and then I'd want to move on. Little did I realize that most of them hadn't noticed the change! Some were struggling to catch up, while others were lost in the rhythm of the music. You see, it's not just about keeping up; it's about finding your groove and enjoying the journey.
That's why I stick with what works. If lunges are hitting the mark, I don't abandon them. Instead, I add layers and nuances that keep the exercise fresh and engaging. It's like dancing to your favorite song; you don't want it to end once you find the beat. Step class might be a relic of the '90s, but the principle still holds true today: find your rhythm, and you'll find your joy."
Sample Drill: Squats
- SAMPLE DRILL: Squats: Squats are used to strengthen the quadriceps and gluteus maximus and challenge balance reactions throughout the body. An open pelvis squat is a great teaching tool, allowing the patient to feel the difference between “falling back” into a chair and squatting into a stable base.
- The patient may be cued as follows: Place your legs more than shoulder width apart with your hips externally rotated (point your toes outwards slightly). Squat down as if you are riding a low bike or motorcycle. Your weight should not pitch you forward or backward and your knees should not move forward of your toes. Hold this position for 3-10 seconds, and then push back to standing by driving the heels into the ground.
- SAMPLE PROGRESSION:
- Squats may be progressed by adding an “elevator” element and requiring the patient to stop on various “floors.”
Open pelvic squats are shown in Figure 9.
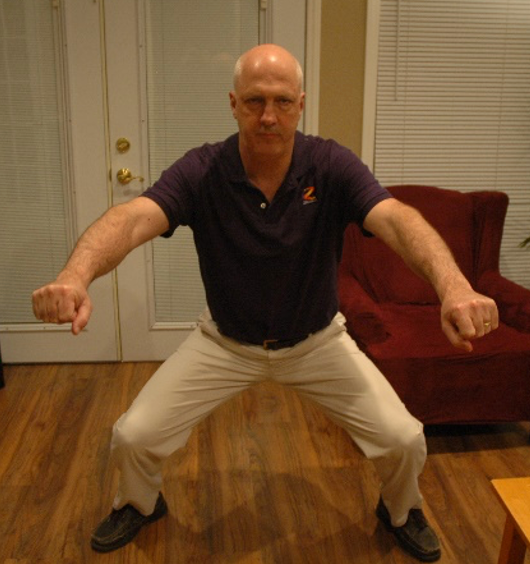
Figure 9. Example of an open pelvis squat.
"Imagine cruising down the highway on a low-rider motorcycle, the wind whipping past you as you lean into each turn. That's the feeling I want you to channel as you settle into this squat position," I tell my patients with a smile. If that doesn't resonate, I'll switch gears and paint a picture of camping in the woods, finding that perfect spot to sit around the campfire.
This open pelvis squat isn't just about getting low; it's about understanding the difference between plopping into a chair and engaging your muscles to lower yourself gracefully. "Feel the weight evenly distributed between your feet, like the steady hum of a motorcycle engine beneath you," I instruct. "Your knees shouldn't jut past your toes, and your back should stay straight as you lower yourself down."
We kick it up a notch once they've got the hang of it. "Now, push back up from that stance, driving through your heels," I encourage. It's all about that powerful contraction, feeling the strength in your legs as you rise.
But we're not done yet. We will take this squat to new heights – or rather, new floors. "Let's take an elevator ride," I propose. "Squat down to the first floor, then the second, and keep going until you reach the top. And don't forget to name each floor as you go – it's all part of the journey."
Clinical Pearl: “Seek the Athlete Within”
- Idea: They can all be adult-onset athletes. Treat them that way.
- Have you ever wondered why we expect so little from those at the “bottom” of the training spectrum?
- As a runner, my pace was described as glacial. But I made the biggest gains out of everyone I knew. Why?
- Because initial changes in strength, speed, flexibility, and power are gigantic compared to any gains made by highly trained individuals.
- Treat your patients like the athletes they are (or can be).
- Chart goals.
- Expect more.
- Push them to excellence.
- Use training tools and techniques like you would with any athlete.
(Brennan & Isaacs, 2018)
Tap into the athlete within. It's a mantra I live by when working with older individuals. Nothing irks me more than seeing them treated like delicate porcelain dolls. Even those with osteoporosis and osteopenia deserve to be treated as adult-onset athletes. I first encountered this idea in a reference somewhere, resonating with my own journey of discovering athleticism later in life.
Research backs this approach, showing that individuals at the bottom of the training spectrum often yield the most significant gains. I can attest to this firsthand. Joining a running club and participating in a "couch to marathon" program called Team in Training, I found myself among speedy, seasoned runners. My initial pace was a modest 13-minute mile, but I shaved it down to an impressive nine-minute mile through dedicated effort. While my pace improvement was substantial, those already closer to perfection saw smaller gains.
The principle applies to proprioceptive challenges as well. Individuals grappling with such issues can experience remarkable progress early on. Thus, I strive to instill in them a sense of athletic potential. I encourage them to jot down their goals in a notebook, setting tangible targets to track their progress. Expecting more and embracing moments of failure are integral to the journey toward excellence. I approach their rehabilitation with the same vigor and strategies as I would with any athlete, leveraging techniques to enhance proprioceptive skills and propel them toward success.
Sample Drill: Tandem Stance
- SAMPLE DRILL: Tandem Stance: Tandem stance is an excellent way to challenge stance stability bilaterally. In tandem stance, the patient must remain stable with a narrow base of support (both feet lined up one in front of the other).
- The patient may be cued as follows: Place your feet one in front of the other as if you were walking on a balance beam or tightrope. Hold your position without using your arms to keep your balance.
- SAMPLE PROGRESSIONS:
- Reducing space between feet so that the back foot touches the front
- Encouraging weight shift in an anterior-posterior direction
- Increase the amplitude of the weight shift, like the “Pirate ship” ride at the amusement park
- Close eyes
Figure 10 shows a tandem stance.

Figure 10. Example of a tandem stance.
Here are some progressions to challenge your patients further. Start by reducing the space between their feet so the back foot touches the front. This narrower stance makes maintaining balance much harder compared to the wider stance. Encourage them to shift their weight in an anterior-posterior direction, akin to the motion of a pirate ship ride at amusement parks. Cue them into this stance, liken it to being at the bow of the Titanic.
Clinical Takeaway for Stance and Steppage
- CLINICAL TAKEAWAY: Stance and steppage training is at the heart and soul of all balance training.
- These drills (and others like them) should be routinely introduced after neuro events because they work.
Figure 11 shows functional tasks for stance and steppage.

Figure 11. Examples of functional tasks for stance and steppage.
Let's incorporate daily activities into our training sessions. We'll simulate reaching into the dryer to grab clothes, practice donning a coat smoothly, and even rehearse chopping motions. Remember, stance and step training form the foundation of balance training. These drills should be regularly integrated into our sessions to enhance stability and mobility.
Active Movement and Balance Training: Unstable Surface Training
- What is Unstable Surface Training?
- It’s one thing to walk and balance on a stable surface; it’s quite another when the ground won’t stay still.
- Walking on an uneven or giving surface requires more – more flexibility, more strength, more agility and quicker reaction time.
- The foot and ankle complex is the first to encounter an uneven surface. The foot must make constant inversion and eversion corrections when walking on grass, rocks, or other unstable surfaces.
- Quick muscular responses to the changing foot position help to maintain balance and avoid a quick roll and sprain.
- If the ankle strategies, hip strategies, and steppage reactions in the lower extremities are inadequate or slow, then the person will be at risk for a fall.
Unstable surface training involves walking and bouncing on surfaces that lack stability, such as grass, rocks, pillows, or BOSU boards. When navigating these surfaces, the foot constantly adjusts to prevent imbalance, requiring frequent inversion and eversion corrections.
When discussing balance loss, it operates on a three-tiered support system. Ankle strategies are the first line of defense, where individuals use inversion and eversion movements to maintain balance without significant body movement. Next are hip strategies, characterized by swaying of the center of mass. Finally, steppage occurs when individuals widen their base of support to compensate for balance issues, indicating a lower level of proprioceptive control.
- Unstable Surface Training can be introduced as a more advanced method to train balance.
- It may be as easy as adding an unstable base to the Stance and Steppage drills just discussed – or more sport-specific ideas may be used.
- An outdoor unstable surface can be created using almost anything, including a slope, a grass field, or a rocky staircase.
- The following rehab equipment is often used to bring instability challenges indoors:
- Foam pads
- Rocker boards
- Wobble boards
- Biomechanical ankle platform system (BAPS) board
- BOSU Pro Balance Trainer
- Mini-trampoline
Unstable surface training can be introduced as a more advanced method, and you can use the same types of things that you did. It's like sitting on the side of the bed with a pillow, instead of having a nice firm surface underneath them.
Sample Drill: Steppage With Unstable Surface
- SAMPLE DRILL: Steppage with unstable surface: The patient can be positioned on an unstable surface and challenged to perform activities that require stepping.
- The patient may be cued as follows: Stand with your feet shoulder-width apart and perform forward/lateral lunges while maintaining your balance.
- Keep your stance knee slightly bent and hold your trunk upright.
- Don’t “fall” into these steppage drills.
- SAMPLE PROGRESSIONS:
- Add upper extremity arm swing, ball toss, head turn, or other dynamic UE.
- Vary speed and direction of above.
- Introduce tapping drills, bounces, jumps, tucks, plyometric, and sports-specific tasks, such as explosive leg presses, as tolerated.
You can have an unstable surface in standing, tall kneeling, kneeling, and so forth. Figure 12 shows using a throw pillow.

Figure 12. Example of stoppage using a throw pillow.
For example, a therapist can use a firm throw pillow with a towel over it. The challenge becomes immediately apparent as the patient stands barefoot on the towel-covered pillow. They must engage muscles to maintain stability with each movement, relying on proprioception to adjust their position.
The therapist can guide the patient through exercises, starting with basic movements like stepping over the pillow and gradually advancing to more complex tasks. Arm swings and head turns add layers of difficulty, requiring the patient to coordinate their movements while maintaining balance on the unstable surface.
As the session progresses, the therapist can introduce variations in speed and direction, prompting the patient to step to different points in an imaginary clock. With each change, the patient's muscles work harder to stabilize their body, honing their balance skills in real-time.
Tapping movements are particularly challenging, requiring precise control to maintain balance while shifting weight from one foot to another. The therapist encourages the patient to push their limits, incorporating bouncing, jumping, and plyometric exercises for those ready to tackle more advanced challenges.
Through it all, the therapist provides support and guidance, adjusting the difficulty level to match the patient's abilities and goals. Together, they explore the limits of balance and proprioception, unlocking new levels of strength and stability with each session.
Clinical Pearl: "Harness the Power of Touch"
- Idea: Touch changes everything, for good or ill.
- Have you ever asked yourself:
- What is the “Power of Human Touch”?
- Does “less physical assistance” always lead to progress?
- When I add physical contact, what happens?
- In 2023, Packheiser et al did a comparative systematic review and meta-analysis on touch. They found that:
- The more frequently the touch occurs the greater the positive health benefits.
- Shockingly, the session duration did not matter.
- There was no difference in the effectiveness of touch when it was provided by a health professional vs. a familiar person.
(Field, 2010; Grobbel et al., 2017; Packheiser et al., 2023)
Harnessing the power of touch as a therapist encompasses the profound impact physical contact can have on the therapeutic process. This notion was exemplified by an encounter with a clinical psychologist undergoing Watsu therapy, where touch elicited complex emotions. The psychologist, unable to engage in such tactile interactions in their profession, expressed both awe and frustration at the transformative potential of touch in therapy.
The therapist reflects on the inherent significance of touch, acknowledging its ability to evoke emotions, provide comfort, and foster a sense of connection. This underscores touch's pivotal role in facilitating healing and promoting well-being, whether through a supportive hand on the back or a gentle embrace in the water.
Drawing from recent research, the therapist highlights the findings of a systematic review and meta-analysis conducted in 2023. The study emphasizes that the frequency of touch, rather than its duration or the familiarity of the individual administering it, correlates with positive health outcomes. Touch emerges not only as a protective measure but also as a therapeutic intervention with the potential to enhance the therapeutic alliance and promote recovery.
In essence, the therapist encourages a deeper exploration of the profound implications of human touch within the therapeutic context. By recognizing and harnessing its power, therapists can leverage touch as a potent tool for healing and connection, transcending verbal communication to evoke profound therapeutic effects.
Sample Drill: Bridging on Unstable Surface
- SAMPLE DRILL: Bridging on Unstable Surface drills: Patients can be supine in hooklying, with feet placed on an unstable base (like the BOSU).
- The patient may be cued as follows: Lie on your back with your knees bent. Place your feet shoulder-width apart and perform a bridge (lift your hips). While holding the bridge, shift your weight from side to side.
- Shift your weight onto one leg and attempt to hold the other leg in a straight leg raise.
- Vary the amount of flexion and abduction of the straight leg. Reposition yourself with a new orientation on the device and repeat.
- SAMPLE PROGRESSION:
- Lift arms in the air during bridge
- Perform dynamic movements with one leg while bridging
- Execute an elevator drill (stopping on various “floors”)
Incorporating bridging exercises using props like a BOSU or a folded pillow can offer a dynamic challenge to enhance strength and stability. Patients can target different muscle groups and refine their motor control by shifting weight laterally or altering leg positions during bridging. Progressions such as lifting the arms or pushing down onto the surface further engage the trunk muscles, ensuring a comprehensive workout. You can again use the elevator concept to have them raise or lower slowly.
- SAMPLE DRILL: Quadruped on Unstable Surface drills: Patients can be positioned in a 4-point position on an unstable base.
- The patient may be cued as follows: Position yourself on hands and knees. Shift your weight from side to side and front to back.
- While balancing on 3 limbs, attempt to raise the other limb into the air. Vary the amount of flexion and abduction of the straight limb. Reposition yourself with a new orientation on the device and repeat.
- SAMPLE PROGRESSIONS:
- Rise from 4-point to a tall kneel position and then return to 4-point.
Sample progressions are using four-point or tall kneel.
Clinical Pearl: "BOGO Your Therapy"
- Idea: Make your therapy time do DOUBLE DUTY.
- There is probably not a patient on the planet who could not benefit from a little breathing work. Or guided imagery. Or relaxation cueing. Or speech drills. Or fine motor tasks.
- If your physical task is conducive to multi-tasking, BOGO your therapy.
- How, you ask? While you are doing bridges:
- Exhale fully while you descend
- Count to 5, using your “indoor voice” and ramping up to your “outdoor voice”
- As you descend, release your muscles and let your body “let go”
- As you prepare for another rep, use your foot intrinsics to attempt to grip the surface
(Goverover et al., 2018)
In essence, "BOGO your therapy" translates to maximizing the efficiency of therapeutic interventions by integrating multiple objectives into a single session. This approach encourages therapists to explore synergies between different disciplines, such as physical therapy, occupational therapy, and speech therapy, rather than working in silos. By borrowing techniques and insights from other professions, therapists can enhance the effectiveness of their interventions and provide holistic care to their patients.
For instance, during a physical therapy session focused on exercises like bridges, therapists can incorporate breath work and vocalization elements. By cueing patients to exhale fully during the bridge movement, therapists promote core stability and facilitate a more powerful inhalation afterward. Moreover, incorporating vocalization exercises during specific movement phases, such as counting or vocalizing sounds, can engage the vocal cords and respiratory muscles, benefiting patients with conditions like Parkinson's disease.
Additionally, therapists can target specific muscle groups or coordination skills by integrating tasks such as foot intrinsic exercises into the bridge movement. Therapists can enhance foot strength and proprioception alongside core stability by encouraging patients to grip a BOSU or pillowcase with their feet while performing the bridge.
Ultimately, "BOGO your therapy" underscores the importance of maximizing therapeutic opportunities and leveraging the synergies between different interventions to promote comprehensive rehabilitation and functional improvement.
Clinical Takeaway: Unstable Surface Training
- Clinical Takeaway: Unstable surface drills help move patients from the stability and predictability of the clinic to the “real world.” They can be used for patients positioned in standing or almost any other position (supine, prone, kneeling, quadruped, plantar grade). They are a versatile tool for progression.
Figure 13 shows examples of unstable surface training.

Figure 13. Examples of unstable surface training.
Mind Body Techniques
- Within the rehab world, there has been an increase in the amount of attention paid to more holistic balance-oriented exercises, like T’ai Chi and Yoga. Why?
- These ancient disciplines do not attempt to divide and conquer.
- There is no singular focus on strength, balance, or respiratory training – there is all of this wrapped up in a single package.
(Yang et al., 2007).
Mind-body techniques encompass holistic approaches such as tai chi and yoga, integrating elements like strength, balance, and breathwork into unified practices. Unlike traditional exercises that focus on isolated aspects of physical function, these ancient disciplines emphasize the interconnectedness of the mind and body, promoting overall well-being and balance.
The philosophy behind mind-body techniques revolves around unity rather than fragmentation. Instead of isolating specific muscles or movements, practitioners engage in activities that synchronize body movements with breath awareness and mental focus. This holistic approach aims to cultivate harmony between the physical, mental, and emotional aspects of an individual's being.
Research supports the effectiveness of mind-body techniques in promoting balance, reducing stress, and enhancing overall quality of life. By integrating these practices into rehabilitation programs, therapists can offer patients a comprehensive approach to improving their physical function and overall health.
Tai Chi/Qigong
- Tai Chi-Qigong, or Tai Chi as it is more popularly known, is an ancient Chinese exercise form designed to enhance balance and muscle tension regulation.
- Although the health benefits derived from practicing Tai Chi have been accepted in Chinese cultures, the specific effects of Tai Chi on biomechanics have not been studied in detail.
- Tai Chi-Qigong techniques enhance vestibular inputs, thereby increasing balance and steadiness in people who practice these techniques. Proprioceptive training effects with Tai Chi have been reported by many.
Tai chi, a widely practiced martial art and mind-body exercise, offers numerous health benefits that therapists should consider integrating into their rehabilitation programs. While tai chi classes and practices in parks are popular, therapists can extract specific elements to enhance vestibular inputs and improve balance and stability.
Proprioceptive training, which focuses on enhancing the body's awareness of its position and movement, is a fundamental aspect of tai chi, martial arts, and yoga. By incorporating elements of these disciplines into therapy sessions, therapists can capitalize on the proven benefits of proprioceptive training for rehabilitation.
While therapists may not implement entire tai chi routines or yoga sequences, they can selectively incorporate relevant components to address specific therapeutic goals. By doing so, therapists can leverage these ancient practices' holistic principles and effectiveness to optimize patient outcomes.
Yoga
- Yoga has long been practiced as a method of physical training. Yoga techniques that deal with increasing physical strength and flexibility have been described in ancient and modern Indian literature. Yoga exercises also include a component of regulated breathing (pranayama).
- People in various cultures have adopted yoga as a health restorative practice.
- Patients who have neurological complications feel incapable of working with treadmills or balance boards or resistance bands. Sometimes even mundane daily physical activities can seem like insurmountable challenges to them.
- And yet, in study after study, not only are patients able to successfully perform yoga postures, but they are able to derive neuromuscular facilitation from them.
(Mishra et al., 2012; Lawrence et al., 2015).
Yoga encompasses a diverse range of practices, and while some may argue about what constitutes "real yoga," the essence lies in the positions, flows, and regulated breathing techniques that can be adapted for therapeutic purposes. Patients with neurological issues often feel limited in their ability to engage with traditional rehabilitation tools like treadmills or resistance bands. However, introducing yoga poses and tai chi movements can provide an accessible and effective alternative.
Patients can derive neuromuscular facilitation benefits by incorporating these practices into therapy sessions. These movements improve physical strength and flexibility and enhance proprioception and balance, making them valuable tools in neurological rehabilitation. Therapists should explore the diverse range of yoga styles and tai chi movements to find approaches that best suit their patient's needs and abilities.
Clinical Pearl: “Name It and Claim It”
- Idea: Use the power of words to change everything.
- If I told you to stand with your legs in a front lunge and then asked you to hold your arms out to your side at shoulder height (see picture), would you go home and tell your spouse about it?
- If, instead, I told you, “Today, we mastered Warrior Pose”, would you go home and brag a little?
- Words have power. Use them.
(Wulf & Prinz, 2001)
"Name it and claim it" refers to using the power of words and storytelling to transform therapeutic experiences. By giving familiar movements and exercises evocative names or associating them with well-known practices like yoga poses, therapists can make them more engaging and memorable for patients. Instead of describing a movement as simply standing in a front lunge with arms to the side, framing it as mastering a warrior pose can instill a sense of accomplishment and motivation in the patient.
Moreover, employing adverbs (ly adverbs) to modify actions during therapy sessions can further enhance engagement and embodiment. For example, instructing a patient to perform a movement "angrily" or "sleepily" can elicit subtle but meaningful changes in their posture, facial expression, and overall demeanor, adding depth and variety to the therapeutic experience. Through these linguistic techniques, therapists can tap into the transformative power of words to enhance patient participation and outcomes.
Clinical Takeaway: Tai Chi and Yoga
- Clinical Takeaway: Short training periods in Tai Chi and Yoga show a rapid and favorable outcome in neuromuscular facilitation.
- This allows you to introduce small moments, flows and poses inside your current programming to determine if you can easily adapt these programs to patients with spasticity and other deficits.

Figure 14. Examples of yoga poses.
Motor Imagery
- What is motor imagery? Most of us think about an action before we do it. But what would happen if we thought about an action over and over, on a constant repeat? Would it improve our ability to execute the action? This question is at the center of the motor imagery intervention.
- This intervention imagines tasks multiple times before they are physically completed.
- When participants engage in motor imagery events, cortical activation can be seen through neuroimaging that is very similar to the activity that occurs when the motor task is performed.
- Motor imagery can be enhanced by adding elements from the 5 senses to the imagined activity, such as warmth, breezes, textures, smells, sounds, the weight of your limb, the space around you, the touch of your clothes, your environment (clinic, beach, park, home, school, work).
- Motor imagery. This is one of the techniques that I think nobody remembers to do, and it's dirt cheap, free, and it's very, very powerful.
(Monteiro et al., 2021; Agostini et al., 2021; Bezerra et al., 2022)
Motor imagery, a technique used by athletes and now increasingly in rehabilitation settings, involves mentally rehearsing physical actions before executing them. Just like athletes visualize their performance before a game, patients can mentally simulate movements, enhancing motor learning and performance. This practice helps activate brain pathways like physical movements, reinforcing neural connections associated with the desired actions.
When my daughter dribbles during normal daily tasks or practice, I tell her it is important to perfect her technique through mental rehearsal. The adage "practice does not make perfect, perfect practice makes perfect" highlights the significance of deliberate and accurate mental imagery in skill development. Encouraging my daughter to visualize dribbling correctly during practice reinforces that motor imagery can translate into improved performance during actual gameplay.
In rehabilitation, motor imagery can be incorporated into therapy sessions to enhance relearning and recovery. Patients can mentally visualize performing exercises or activities, reinforcing neural connections associated with movement patterns. By mentally rehearsing tasks multiple times before attempting them physically, patients can improve motor control, coordination, and overall functional abilities.
Clinical Takeaway
- Motor imagery helps patients show improvement in relearning tasks. Patients can perform tasks they had not been able to do for some time, perhaps due to cortical reorganization caused by motor imagery therapy. But this is not the only benefit to motor imagery. An interesting side effect is the fact that patients show a reduction in their fear of falling after a bout of motor imagery intervention.
- Clinical Takeaway: Motor imagery is cheap, quick, and has no downside. Add it to your repertoire, especially gait and upper extremity rehab. This technique is an easy one to introduce. No equipment is necessary, and relatively little time must be added to the treatment session. Motor imagery is associated with high patient adherence and patient satisfaction.
- Researchers suggest combining motor imagery therapy with conventional therapy to reach optimal results. No consensus exists on how many repetitions are most beneficial in creating positive outcomes. There appear to be little to no negative side effects from engaging in imagery.
Engaging in motor imagery events has been a fascinating aspect of my practice as a therapist. Through neuroimaging, we've observed cortical activation that mirrors the activity seen during physical movements, making it challenging to discern the difference solely through scans. To optimize motor imagery, I've found that incorporating sensory elements enhances the experience—whether it's imagining smells, textures, or the feeling of movement.
Encouraging patients to mentally simulate the sensations of a task, such as feeling the warmth of sunlight or the pressure of their body against a surface, can significantly enhance the effectiveness of motor imagery. This approach allows patients to mentally rehearse movements before physically performing them, facilitating the relearning of tasks and promoting confidence in their abilities.
One particularly intriguing observation has been the impact of motor imagery on reducing the fear of falling among patients. By mentally rehearsing movements and visualizing successful outcomes, individuals can effectively "practice" navigating challenging situations in a safe mental space. Over time, this process has led to a notable decrease in fear and increased confidence in their physical capabilities.
From a clinical standpoint, the benefits of motor imagery are undeniable. It's a cost-effective, efficient intervention with minimal downsides, making it a valuable addition to any rehabilitation program. I've integrated motor imagery techniques, particularly in gait and upper extremity rehab, with great success. Not only does the research support its efficacy, but it's also incredibly easy to introduce. It is well-received by patients, improving adherence and overall satisfaction with their therapy experience.
Mirror Therapy
- What is Mirror Therapy? Mirror therapy is a technique that uses visual feedback in an attempt to stimulate neuroplasticity. Although originally designed for patients who experienced phantom pain after amputation, it has been adapted for use with patients with hemiparetic limbs.
- In mirror therapy, we are using movements of the stronger body part to "trick the brain" into believing that movement is coming from the other limb, the weak or spastic side. In mirror therapy, the patient places the affected limb behind a mirror. The patient moves through rehab exercises with the unaffected arm reflected in the mirror. The concept behind this technique is that watching the movement reflected in the mirror stimulates mirror neurons (the same neurons that fire during motor imagery) and interacts simultaneously with the patient’s motor neurons.
(Tan et al., 2023; Geller et al., 2022).
Mirror therapy has been a technique that piqued my interest, although it's not widely practiced in my field. I recall an episode of a medical drama where mirror therapy addressed phantom limb pain in a patient, a concept that intrigued me greatly. Essentially, mirror therapy involves utilizing visual feedback to stimulate neuroplasticity, initially designed for individuals experiencing phantom pain after amputation.
While the original application was for amputees, mirror therapy has evolved to assist those with hemiparetic limbs, where one side of the body is weaker or affected by spasticity. It's a method that demands significant training and often specialized equipment. The idea is to employ movements from the stronger or unaffected side while using a mirror to create the illusion that the weaker side is also moving similarly.
By doing so, the brain is tricked into perceiving movement in the affected limb, fostering neuroplastic changes that could alleviate symptoms and improve function. While mirror therapy presents its challenges, particularly in terms of implementation and patient training, it holds promise as a non-invasive and innovative approach to rehabilitation for certain conditions.
An example of mirror therapy can be seen in Figure 15.

Figure 15. Example of mirror therapy.
You place the affected limb behind a mirror, and when the unaffected arm is reflected, you move through some rehab exercises. It stimulates what they call the mirror neurons, the same neurons that fire during motor imagery.
Clinical Takeaway
- Clinical Takeaway: Mirror therapy is coming into its own, but it requires training before implementation. Additionally, there is less to support its use early after a neurological event. Although mirror therapy appears to produce positive effects on post-stroke paresis, research showing benefit during the acute stage of rehab is limited.
Mirror therapy is coming into its own, but it requires some training before implementation. There's very little literature out there about using it early.
Constraint-Induced Movement Therapy
- What is Constraint-Induced Movement Therapy? This treatment technique, initially created for use with patients after CVA, was designed to couple restraint of the "unaffected" arm with intensive use of the affected arm. The hand itself is either mitted or placed inside a glove. The entire affected arm is sometimes placed in a sling or a splint. The goal is a forced usage of the affected arm.
- One of the original systematic review on this technique was conducted in 2005. Their study examined CIMT of the upper limbs for several outcomes for the post-stroke patient, including function, quality of life, costs, and satisfaction. They found results tended to favor CIMT groups for at least upper limb function, compared to either no treatment or alternative treatment plans.
(Hakkennes & Keating, 2005; Tedla et al., 2022; Abdullahi et al., 2021)
Constraint-induced movement therapy, a concept dating back to 2005, remains a notable approach, particularly in stroke rehabilitation. The essence of this therapy involves constraining the unaffected arm while intensively engaging the affected arm for extended periods, often up to five to seven hours a day. By doing so, the therapy aims to compel the utilization or attempted utilization of the affected limb while discouraging reliance on the unaffected limb.
The unaffected hand is typically restrained or encased in a glove, sometimes even immobilizing the entire arm within a sling (as seen in Figure 16). This restriction forces the individual to rely on the affected arm for daily tasks and activities, encouraging neural reorganization and motor recovery in the affected limb. Constraint-induced movement therapy is renowned for its intensive nature and is a testament to the principle of neuroplasticity, demonstrating the brain's ability to adapt and rewire after injury.

Figure 16. Client in a sling. Image: Continued (licensed from Getty Images)
The goal is forced usage of the affected arm. Some of the research shows positive benefits compared to no treatment or alternative treatment plans.
Clinical Takeaway
- Clinical Takeaway: Constraint-induced movement therapy has not yet been shown to render gold-standard effects. It requires a massive commitment of time and motivation, and many patients are lost to attrition during their clinical trials. This must be considered before suggesting its use.
The key takeaway regarding constraint-induced movement therapy (CIMT) is its potential for significant benefit in stroke rehabilitation. However, it's important to recognize that CIMT is not yet considered a standard approach following a stroke. While promising, its implementation requires a substantial commitment of time and motivation from patients and healthcare providers.
One notable challenge with CIMT is the high attrition rate observed in clinical trials, highlighting the frustrations and difficulties associated with sustaining participation in such intensive therapy. Therefore, while CIMT shows promise, it also underscores the need for ongoing research, refinement, and consideration of individual patient factors to optimize its effectiveness in stroke recovery.
Body Weight Supported Treadmill Training
- What is body weight supported treadmill training? Body weight supported treadmill training is performed when a patient is led through stepping on a treadmill with partial body weight support via a harness. This harness can be adjusted to provide trunk and pelvic support.
- Researchers set out to see if body weight supported treadmill training (BWSTT) is effective for improving gait in post-stroke patients. They found that all groups improved significantly overall, slightly favoring the BWSTT group.
(Atan et al., 2019; Mustafaoğlu et al., 2018)
Body weight supported treadmill training is oftentimes coupled with robotics. It's treadmill training performed when a patient is led through stepping on a treadmill with partial body weight support with a harness (Figure 17).

Figure 17. Client doing body weight supported training. Image: Continued (licensed from Getty Images)
Adjusting the harness and providing partial body weight support is a key feature of body weight supported treadmill training (BWSTT). By reducing the weight borne by the patient, therapists can facilitate a more controlled and supported environment for walking practice, particularly for individuals with mobility impairments. This approach has demonstrated promising outcomes in promoting gait recovery and functional improvement among patients with neurological conditions.
However, it's important to acknowledge the significant time investment required to set up and adjust the harness system during BWSTT sessions. While this setup time may not be directly billable, it plays a crucial role in ensuring the safety and effectiveness of the therapy. Experienced therapists may become more efficient in preparing for BWSTT sessions, but it remains a consideration in optimizing time management within clinical practice.
Clinical Takeaway
- Clinical Takeaway: A lower frequency of isolated BWSTT may be as effective as a higher frequency of conventional training in ambulatory post-stroke patients.
- BWSTT improved walking distance and balance ability, relieved fatigue, and reduced pain in patients with moderate to advanced Parkinson's Disease.
Passive Movement Training
- There are effective techniques that do not include active patient participation. One such category is “Passive Movement Training”. This category includes interventions that require some passive motion apparatus. All passive motion apparatus (PMA) are designed differently, but they all work in a nearly identical way. Many studies have shown a training effect with passive movement training, although it does not appear to be nearly as promising as Active Movement and Balance Training.
- Researchers interested in the benefits of “passive movement training” use various types of passive motion apparatus to try and train joint position sense (among other things). Some PMAs focus on a single joint, such as the knee, while others create multi-joint movements.
- Passive Movement Training
- Single joint passive movement
- Multiple joint passive movement
(Ren et al., 2017)
Passive movement training, while valuable, may not always be the primary focus of rehabilitation efforts due to its limitations compared to active interventions. These techniques typically require specialized equipment and primarily target joint position sense rather than range of motion. While they have shown some training effects, the evidence supporting their efficacy may not be as robust as that for active interventions.
One common example of passive movement training is continuous passive motion therapy, often used after knee surgery. However, proprioceptive training focuses on enhancing joint position sense rather than promoting passive motion. These techniques may target single joints, such as the knee, or involve movements across multiple joints.
While passive movement training can be beneficial, especially for patients who may have difficulty participating in active exercises, it's important for therapists to prioritize interventions that align with current evidence and maximize therapeutic outcomes.
Passive Knee ROM
- One research study studied the effects of PMT on healthy subjects to perform joint matching of their knees. The study volunteers received a treatment consisting of 60 repetitions of passive knee movement (ranging between 10°-100° at an average speed of 120°/second).
- During the passive movement sessions, the researchers wrapped an air splint around the limb to decrease tactile information. Still, the subjects were allowed to watch the knee flexion and extension take place.
- Did passive movement result in better matching? The participants showed a 37-47% improvement in their ability to match joint position after their training bout. This result appears to be one of the best responses to PMT recorded, as most other research teams found a training improvement of less than 25%.
(Ju et al., 2010)
Passive knee range of motion exercises, involving repetitive motion from 10 to 100 degrees at a relatively fast pace, have shown potential benefits in enhancing the ability to match joint positions from side to side. Studies on healthy subjects have indicated a roughly 25% improvement in this ability following such interventions. However, the long-term effects of these exercises have not been extensively studied, with most research focusing on immediate outcomes.
Passive Hand Mobilization
- Does Passive Movement Training need to be ongoing to produce results? In other words, does PMT need to be performed repeatedly – or is it possible to achieve results with a single session?
- Gobbo et al tackled this question head-on by examining whether a single 20-minute session of robot-assisted passive hand mobilization after a CVA would produce meaningful results. The researchers examined tissue perfusion (through near-infrared spectroscopy) and muscle tone (through the Modified Ashworth Scale). They also asked the participants about pain, stiffness, and joint “heaviness.”
- The results? Subjective complaints improved and so did perfusion and muscle tone. It appears possible that a single bout of PMT may indeed perform.
(Gobbo et al., 2017)
Is continual practice necessary to yield positive outcomes? In other words, is repetitive engagement required, or can a single session suffice? A notable study conducted in 2017 explored this question by examining the effects of a solitary 20-minute session of robot-assisted passive hand mobilization following a stroke. The study assessed parameters such as pain, stiffness, and joint heaviness, and observed improvements in pain reduction, decreased subjective complaints, enhanced perfusion, and improved muscle tone following one session. Although the study did not delve into the long-term implications, it demonstrated immediate benefits from a single intervention.
Passive Cycling
- In the aftermath of a CVA, many patients do not have the endurance to participate in long rehab sessions. Passive cycling is being pitched as a potential solution for patients who are too weak or medically incapable of active participation.
- Researchers believe that cycling motion can elicit sensory inputs, leading to beneficial changes in the cortical structures. The jury is still out, but it is possible that passive cycling, such as described in this study, may produce benefits work the effort.
(Nardone et al., 2017)
Regarding cycling, it often brings to mind continuous passive motion (CPM) where individuals are strapped in for a back-and-forth motion. In cases where patients are too weak or medically unable to participate actively, cycling may offer potential benefits. However, while the concept shows promise, further research is needed to determine its effectiveness.
Clinical Takeaway
- Clinical Takeaway: Passive Movement Training is used clinically in many physical medicine settings. However, it is currently more familiar to therapists for ROM purposes (such as a Continuous Passive Motion machine) than proprioception training. This is a specialized area of rehab requiring extensive equipment and training.
Passive movement training is utilized clinically, although it is often associated with addressing range of motion rather than proprioceptive training. However, practitioners should not dismiss it outright, especially if they have previous experience. While passive movement training may not directly target proprioception, exploring its potential benefits could still be worthwhile in certain cases.
Somatosensory Stimulation Training
- Passive movement training techniques are not the only interventions that require specialized equipment. Let’s move on to the next category of proprioceptive interventions: Somatosensory Stimulation Training.
- Somatosensory Stimulation Training includes interventions that use various forms of stimulation geared exclusively to somatosensation.
- Somatosensory Stimulation Training
- Functional electrical stimulation
- Vibration
- Vibration with active movement training
- Vibration with balance training
- Vibration and rehabilitation therapy
- Magnetic stimulation
- Acupuncture
- Thermal stimulation and movement training
Here are some things for somatosensory stimulation training.
Functional Electrical Stimulation
- What is Functional Electrical Stimulation? In recent years, functional electrical stimulation has been mentioned as an option for treating patients with reduced mobility, muscle weakness, and spasticity. In this intervention, electrical pulses stimulate the nerves to create contractions similar to those that occur naturally during exercise.
- Researchers have set out to investigate the outcomes of some common issues for the post-stroke patient -- shoulder subluxation, pain, and upper-arm motor function. They found that electrical stimulation worked well for shoulder subluxation when used early in treatment. However, there was little to no effect on pain or upper-arm motor function.
- Clinical Takeaway: Functional electrical stimulation is most thoroughly understood in the early stages of stroke rehabilitation. Research still needs to be done on incorporating FES into late-stage rehabilitation.
(da Cunha et al., 2021; Scally et al., 2020)
Functional electrical stimulation is gaining increased attention, particularly following cases like Christopher Reeve's, where individuals have made unexpected gains. FES involves using electrical pulses to stimulate nerves, inducing contractions like during exercise. It has been explored in addressing chronic shoulder subluxation, aiming to reduce associated pain. However, research on using FES in later stages of rehabilitation is limited, with the current focus mainly on early intervention for individuals with limited participation ability. For further insights, systematic reviews and meta-analyses on FES are recommended for review.
Vibration Therapy
- What is Vibration Therapy? There are two kinds of vibration therapy, whole body and localized. Both types of vibration are passive modalities in which something is done to the patient instead of the patient doing something actively. Whole body vibration therapy uses a platform that vibrates a patient who is passively sitting, standing, or lying on it. Localized vibration therapy uses a hand-held device which is positioned next to a body part. The research currently being done on vibration therapy looks at its ability to create muscle contractions and to cause the production of osteoblasts. Of all the somatosensory techniques studied by Aman, vibration training stood out from the crowd, with one study showing a 109% improvement.
(Park et al., 2018; Alam et al., 2020)
Vibration therapy comes in two forms: whole body and localized. In both cases, the therapy is passive, meaning that the individual receives the treatment rather than actively participating in it.
Whole body vibration therapy involves using a platform that vibrates while the patient sits, stands, or lies on it passively. On the other hand, localized vibration therapy utilizes a handheld device to administer targeted vibrations. Current research explores its efficacy in inducing muscle contractions and stimulating osteoblast production, which is noteworthy.
One notable study conducted by Ahman in 2015 demonstrated a remarkable 109% improvement with vibration therapy. Further details on this study are provided for reference.
Clinical Takeaway
- Clinical Takeaway: Passive exercises such as vibration therapy are a good option for those patients who might not be ready yet to progress to regular exercise. WBV training may provide a safe, alternative treatment method for improving the symptoms of stroke in patients.
- Vibration therapy can be integrated into your treatment plan as a stepping stone to further therapeutic exercise interventions.
Passive exercises like vibration therapy offer a valuable option for patients who may not be ready to advance to more active interventions. Apart from their practicality, these treatments are generating considerable interest due to their intriguing mechanisms. They represent a safe alternative for alleviating symptoms in stroke patients and could serve as a transitional tool towards more intensive rehabilitation strategies.
Combined Multiple Systems
- Physical medicine and rehabilitation has certainly come a long way from the early days of therapy. Technology is exploding and training options which were science fiction even ten years ago are finding their way into the mainstream. Therapists looking to motivate or encourage participation from clients may need to look no further than some of these multiple systems interventions.
- This category included interventions which either used multiple components of the categories (see prior) or used multi-sensory approaches.
- Combined/Multiple Systems
- Multisensory stimulation and active movement training
- Multisensory stimulation and balance training
- Somatosensory discrimination and active movement training
When integrating various therapeutic modalities, such as multisensory stimulation, balance training, and somatosensory discrimination, into a comprehensive treatment plan, aquatic therapy emerges as a highly efficient option. The aquatic environment offers a unique setting where multiple interventions can be seamlessly combined to maximize therapeutic outcomes within a limited time frame.
Aquatic Therapy
- What is Aquatic Therapy? Researchers have begun to examine the benefits of activities performed in an environment that combines sensory and motor stimulation.
- Aquatic therapy marries the benefits of skillful exercise and immersion. During mild to moderate intensity exercise, there is a 10-20% increase in blood flow in response to the uptick in cerebral neuronal activity and metabolism. The addition of hydrostatic pressure (during immersion) makes this more dramatic. Compared with exercise, water-based exercise induces an increase in middle cerebral artery blood flow, posterior cerebral artery blood flow, and partial pressure of expired CO2. In other words, the same exercises performed on land and in water do not produce similar results. The aquatic version augments cerebrovascular blood flow.
(Ghayour Najafabadi et al., 2022; Giuriati et al., 2021; Kottaras et al., 2021)
The minute you put someone in the pool, things happen to them. Figure 18 shows an example of pool exercises.

Figure 18. Example of pool exercises.
When engaging in mild to moderate-intensity exercise, the brain typically experiences a 10 to 20% increase in blood flow due to heightened cerebral neuronal activity. However, immersion in water triggers a remarkable surge in blood flow to the brain, amounting to approximately 250%. This significant augmentation underscores the potential benefits of aquatic therapy for individuals with conditions such as dementia and cognitive impairments, prompting extensive research in this area.
- Clinical takeaway: The therapeutic pool can provide a malleable environment to focus on proprioceptive training through active movement and balance training. Water can provide stability or instability, increasing or decreasing sensory input. It certainly provides a safe environment in which to fail with balance drills.
The clinical takeaway from aquatic therapy lies in its capacity to offer a flexible setting conducive to proprioceptive training. Moreover, the therapeutic pool is a safe environment where individuals can explore movements and exercises with reduced risk, fostering a sense of security amid therapeutic endeavors.
Robotic Assisted Therapy
- What is Robotic Assisted Gait Therapy? Robotic therapy, specifically robotics-assisted gait training, is a therapeutic intervention using robotic devices to assist patients. The devices help the patient walk without as much assistance from therapists.
- Robotics-assisted gait training devices typically consist of a harness to hold the patient over a treadmill while robotic attachments guide the legs through the walking motion.
(Staples, 2017; Baronchelli et al., 2021; Ren et al., 2017)
Figure 19 shows an example of treadmill training.

Figure 19. Example of treadmill training. Image: Continued (licensed from Getty Images)
Robotic-assisted gait training involves using robotic devices to guide and support a patient's legs through walking patterns while suspended over a treadmill by a harness. The robotics provide assistance and stimulation to help the individual replicate natural walking movements. This approach combines mechanical guidance with the patient's own muscle activation, facilitated by electrical signals, to enhance gait function. The body weight support provided by the harness allows patients to practice walking without bearing their full weight, making it a valuable tool in rehabilitation for individuals with impaired mobility.
- What about Wearable Robotics? Rehabilitation services – no matter how stellar – can only be provided for minutes out of every day. One promising area of study is the area of wearable robotics; these devices would be capable of cycling a patient through many cycles of active or passive movement therapy between sessions with a PT or OT.
- Clinical Takeaway: Most studies have shown beneficial effects of Lokomat on balance recovery for stroke survivors, at least comparable to conventional physical therapy. Many more study needs to occur.
Wearable robotics represent a promising avenue in rehabilitation, particularly for patients who require continuous support and stimulation outside of formal therapy sessions. These devices are designed to cycle patients through multiple cycles of active or passive motion during periods between their scheduled therapy sessions. Examples include the Lokomat, which targets balance recovery in stroke patients. Initial studies suggest that wearable robotics can yield benefits comparable to conventional physical therapy, as evidenced by the research highlighted in this study. However, further research is needed to fully understand the potential and efficacy of wearable robotics in rehabilitation.
Vibration Robotics
- The study by Cordo et al. (2009) used a specialized technique called assisted movement with enhanced sensation to treat paresis following a stroke. The researchers attached a robotic device that vibrated the tendons of the flexor and extensor muscles while rotating the ankle, wrist, or fingers. This was a form of localized vibration therapy.
- The researchers found that – to a large extent -- subjects complied with the testing. Based on these results, the researchers concluded that assisted movement with enhanced sensation, when used correctly, is a safe and effective way to increase strength in post-stroke patients with paresis.
(Cordo et al., 2009)
Vibration robotics combines the two things we've already talked about, wearable or interactive robotics, with the concept of vibration.
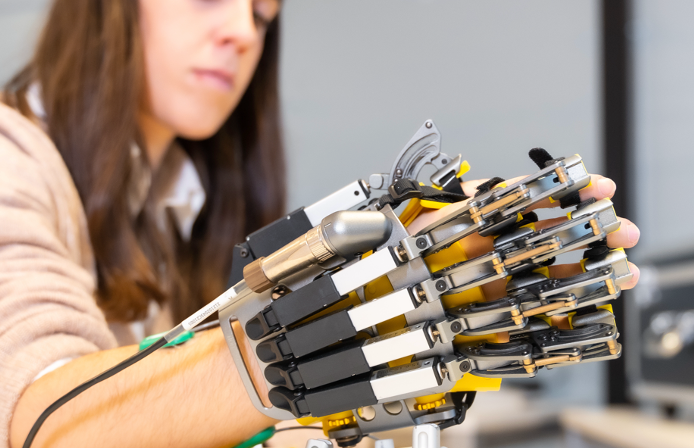
Figure 20. Example of a wearable robotic device. Image: Continued (licensed from Getty Images)
And so they have actually done studies that look at, does this effectively increase your strength? What does it do to your proprioception? So those are things that are currently under study.
- Clinical takeaway: Robotics applications are reaching beyond the experimental lab and into the clinic. Although most therapists today do not have access to these novel options yet, they are cropping up in clinical applications where neurologically impaired patients do intensive rehabilitation.
What's the takeaway? Robotics applications are fast reaching beyond the experimental lab and into the clinic, but most of us don't have access to them, so I am not spending much time on them right now.
Virtual Reality Training
- What is Virtual Reality Training? Virtual reality is the latest trend in video gaming. Virtual reality means different things to different people but a helpful way to define it was presented by Weiss et al (2004): Virtual reality is "the use of interactive simulations created with computer hardware and software to present users with opportunities to engage in environments that appear to be and feel similar to real-world objects and events.”
- Therapists can use computers to create a virtual 3D environment for patients to safely complete real-time tasks. The main categories include immersive virtual reality (which requires a head-mounted display setup) and non-immersive virtual reality (which does not). Immersive systems are very expensive and typically only used in research settings. Non-immersive systems do not require the hardware or software financial outlay and thus are more commonly used.
(Truijen et al., 2022; Li et al., 2021)
Virtual reality is the latest trend in video gaming. It's the use of interactive simulations created with computer hardware. An example can be seen in Figure 21.

Figure 21. Example of virtual reality. Image: Continued (licensed from Getty Images)
Virtual reality holds significant promise in rehabilitation, particularly for patients such as wounded warriors who may benefit from immersive 3D environments to complete therapeutic activities safely. There are two main types of VR systems: immersive and non-immersive. Immersive VR systems require a head-mounted display setup and offer a fully immersive experience, but these are typically found in specialized hospital or research settings. On the other hand, non-immersive systems do not require such elaborate setups and are more commonly used in rehabilitation facilities. These systems still provide valuable virtual environments for therapeutic activities but in a less immersive manner.
Clinical Takeaway
- Clinical Takeaway: Virtual reality training can add variability to therapy that may not be possible otherwise. Patients who participate in virtual reality therapy may experience higher motivation to complete therapy sessions than conventional sessions. However, access to virtual reality systems will limit the practical use of this intervention in the near future.
Virtual reality offers valuable variability and motivation in rehabilitation, especially for patients who traditional exercises may not inspire. Research suggests that VR can enhance motivation and engagement in therapy. However, its practical usage is limited due to the requirement for specialized equipment and setups, which are not readily available in most rehabilitation settings.
Gaming Console Systems
- What are Gaming Console Systems? Two popular systems, including motion sensation (the Nintendo Wii and the Xbox 360 Kinect), are routinely integrated into nursing home care, “homework” after skilled therapy, and even in the clinic. Why should therapists consider gaming as a viable rehab tool? In a word, neuroplasticity. After a neurological injury or insult, the brain attempts to restructure pathways and find a new way to do old things.
- In order for this to succeed, multiple factors have to fall into place. There has to be a method to obtain immediate feedback. There needs to be a motivational or reward element. There needs to be a means to repeat tasks as they are learned and mastered and eventually increase the task difficulty to progress. Motion-sensing gaming systems can provide all of these elements by engaging the user in “stories” or plots, assigning scores or points, and rewarding some behaviors and not others.
(Adie et al., 2017; Marotta et al., 2022)
Gaming console systems like the Nintendo Wii and Xbox Kinect are gaining popularity in clinical settings and as homework assignments after therapy sessions. These systems offer a fun and engaging way to promote neuroplasticity, helping the brain restructure pathways following neurological events or injuries. While some video games are designed to tap into addictive tendencies, when used appropriately, gaming provides immediate feedback and motivation, making it an effective tool for rehabilitation. Moreover, motor-sensing gaming systems offer immersive experiences with engaging stories and plots, enhancing patient engagement in therapy.
Clinical Takeaway
- Clinical Takeaway: Kinect and Wii immediately positively affect functional locomotion in people with PD. Compared with Kinect, Wii may be considered the best therapy for functional PD recovery.
Takeaway, there has been a little bit of research on the best system. For instance, they looked at patients with Parkinson's disorder and they said that "The Wii may be considered better than the Connect for providing functional recovery in Parkinson's."
Conclusion
- In order for patients to make gains in motor function after neurological loss, they must take advantage of the physiological and anatomical plasticity present in the nervous system.
- Scientists are currently investigating dozens of ways to expand the natural plasticity present.
- Novel “new frontier” experiments include:
- stem cell therapy,
- exogenous tissue engineering, and
- brain–computer interfaces.
- But the truth of it is that most people can’t wait. Therapists must use today’s available techniques to tap into neural plasticity to bring order to chaos. Good luck!
(Murao et al., 2023; Citro et al., 2023; Levett et al., 2023; Li et al., 2023; Dimyan & Cohen, 2011; Marasco & de Nooij, 2023)
In conclusion, patients seeking to regain motor function after neurological loss must harness the physiological and anatomical plasticity inherent in the nervous system. While advancements such as stem cell therapies, tissue engineering, and brain-computer interfaces offer promising avenues for rehabilitation, it's essential to recognize the enduring power of human touch and presence in therapy. While technology can facilitate neuroplasticity, therapists' hands, hearts, presence, and knowledge remain indispensable in guiding patients toward recovery. Embracing available technology while recognizing the profound impact of human connection is key to navigating the complex terrain of neurological rehabilitation. Now, let's address some questions.
Questions and Answers
Wouldn't providing perfect environments through virtual reality or aquatic therapy be great?
While VR systems and aquatic therapy can offer unique experiences, they also rewrite sensory input, which can be disorienting for some individuals. It's essential to consider how these interventions may affect proprioception and patient comfort.
What Wii games are commonly used for proprioceptive rehab?
Wii Sports games like bowling, tennis, baseball, and boxing are popular choices for proprioceptive rehabilitation. These games offer interactive experiences that engage patients in balance and coordination activities.
Is there a certification for therapists to utilize tai chi as part of therapy?
Several tai chi certification programs exist for therapists interested in incorporating tai chi into their practice. Organizations like Ai Chi offer aquatic tai chi programs specifically designed for therapy settings.
Any research on mirror therapy and cerebral palsy?
While there may not be specific research on mirror therapy and CP, therapists can explore resources like the Physiotherapy Effectiveness Database (PEDro) to find evidence-based information on proprioceptive training interventions for various conditions. PEDro provides access to systematic reviews, meta-analyses, and randomized controlled trials relevant to physical medicine and rehabilitation.
References
Abdullahi, A., Truijen, S., Umar, N. A., Useh, U., Egwuonwu, V. A., Van Criekinge, T., & Saeys, W. (2021). Effects of lower limb constraint induced movement therapy in people with stroke: A systematic review and meta-analysis. Frontiers in Neurology, 12, 638904.
Adie, K., Schofield, C., Berrow, M., Wingham, J., Humfryes, J., Pritchard, C., ... & Allison, R. (2017). Does the use of Nintendo Wii SportsTM improve arm function? Trial of WiiTM in Stroke: A randomized controlled trial and economics analysis. Clinical rehabilitation, 31(2), 173-185.
Agostini, F., Pezzi, L., Paoloni, M., Insabella, R., Attanasi, C., Bernetti, A., ... & Paolucci, T. (2021). Motor imagery: A resource in the fatigue rehabilitation for return-to-work in multiple sclerosis patients—A mini systematic review. Frontiers in Neurology, 12, 696276.
Alam, M. M., Khan, A. A., & Farooq, M. (2020). Effects of whole-body vibration on muscle strength, balance and functional mobility in patients with multiple sclerosis: A systematic review and meta-analysis. Journal of Musculoskeletal Research, 23(04), 2050019.
Aman, J. E., Elangovan, N., Yeh, I., & Konczak, J. (2015). The effectiveness of proprioceptive training for improving motor function: a systematic review. Frontiers in human neuroscience, 8, 1075.
Atan, T., TAŞKIRAN, Ö. Ö., Tokçaer, A. B., Karataş, G. K., ÇALIŞKAN, A. K., & Karaoğlan, B. (2019). Effects of different percentages of body weight-supported treadmill training in Parkinson's disease: a double-blind randomized controlled trial. Turkish journal of medical sciences, 49(4), 999-1007.
Baronchelli, F., Zucchella, C., Serrao, M., Intiso, D., & Bartolo, M. (2021). The effect of robotic-assisted gait training with Lokomat® on balance control after stroke: systematic review and meta-analysis. Frontiers in Neurology, 12, 661815.
Bezerra, P. T., Santiago, L. M., Silva, I. A., Souza, A. A., Pegado, C. L., Clécia, M., ... & Lindquist, A. R. (2022). Action observation and motor imagery have no effect on balance and freezing of gait in Parkinson’s disease: a randomized controlled trial. European journal of physical and rehabilitation medicine, 58(5), 715.
Brennan, S., & Isaacs, T. (2018). Fit at mid-life: a feminist fitness journey. Greystone Books Ltd.
Citro, V., Clerici, M., Boccaccini, A. R., Della Porta, G., Maffulli, N., & Forsyth, N. R. (2023). Tendon tissue engineering: An overview of biologics to promote tendon healing and repair. Journal of tissue engineering, 14, 20417314231196275.
Cordo, P., Lutsep, H., Cordo, L., Wright, W. G., Cacciatore, T., & Skoss, R. (2009). Assisted movement with enhanced sensation (AMES): Coupling motor and sensory to remediate motor deficits in chronic stroke patients. Neurorehabilitation and neural repair, 23(1), 67-77.
da Cunha, M. J., Rech, K. D., Salazar, A. P., & Pagnussat, A. S. (2021). Functional electrical stimulation of the peroneal nerve improves post-stroke gait speed when combined with physiotherapy. A systematic review and meta-analysis. Annals of Physical and Rehabilitation Medicine, 64(1), 101388.
Dimyan, M. A., & Cohen, L. G. (2011). Neuroplasticity in the context of motor rehabilitation after stroke. Nature Reviews Neurology, 7(2), 76.
Fell, D. W. (2004). Progressing therapeutic intervention in patients with neuromuscular disorders: a framework to assist clinical decision making. Journal of Neurologic Physical Therapy, 28(1), 35.
Field, T. (2010). Touch for socioemotional and physical well-being: A review. Developmental Review; 30(4): 367–383.
Ge, L., Zheng, Q. X., Liao, Y. T., Tan, J. Y., Xie, Q. L., & Rask, M. (2017). Effects of traditional Chinese exercises on the rehabilitation of limb function among stroke patients: A systematic review and meta-analysis. Complementary therapies in clinical practice.
Geller, D., Nilsen, D. M., Quinn, L., Van Lew, S., Bayona, C., & Gillen, G. (2022). Home mirror therapy: a randomized controlled pilot study comparing unimanual and bimanual mirror therapy for improved arm and hand function post-stroke. Disability and Rehabilitation, 44(22), 6766-6774.
Ghayour Najafabadi, M., et al. (2022). Aquatic therapy for improving lower limbs function in post-stroke survivors: A systematic review with meta-analysis.
Giuriati, S., Servadio, A., Temperoni, G., Curcio, A., Valente, D., & Galeoto, G. (2021). The effect of aquatic physical therapy in patients with stroke: A systematic review and meta-analysis. Topics in stroke rehabilitation, 28(1), 19-32.
Gobbo, M., Gaffurini, P., Vacchi, L., Lazzarini, S., Villafane, J., Orizio, C., ... & Bissolotti, L. (2017). Hand Passive Mobilization Performed with Robotic Assistance: Acute Effects on Upper Limb Perfusion and Spasticity in Stroke Survivors. BioMed research international, 2017.
Goverover, Y., Sandroff, B. M., & DeLuca, J. (2018). Dual task of fine motor skill and problem solving in individuals with multiple sclerosis: a pilot study. Archives of physical medicine and rehabilitation, 99(4), 635-640.
Grobbel, R., Cooke, K., & Bonet, N. (2017). Ethical use of touch and nurturing-restraint in play therapy with aggressive young children, as illustrated through a reflective supervision session. Touch in Child Counseling and Play Therapy: An Ethical and Clinical Guide. London, UK: Taylor & Francis.
Hakkennes, S., & Keating J.L. Constraint-induced movement therapy following stroke: a systematic review of randomised controlled trials. Aust. J. Physiother. 2005; 51:221–231.
Jain, A., Taylor, J., Sanzo, P., & Zerpa, C. (2017). The Effect of Tai Chi on Functional Lower Extremity Mobility and Strength, Ankle Proprioception, and Postural Adaptation in Older Adults. American Journal of Medicine and Medical Sciences, 7(6), 229-237.
Ju, Y. Y., Wang, C. W., and Cheng, H. Y. (2010). Effects of active fatiguing movement versus passive repetitive movement on knee proprioception. Clin. Biomech. 25, 708–712. doi: 10.1016/j.clinbiomech.2010.04.017
Konczak J., Corcos D. M., Horak F., Poizner H., Shapiro M., Tuite P., et al. (2009). Proprioception and motor control in Parkinson's disease. J. Mot. Behav. 41, 543–552. 10.3200/35-09-002
Kottaras, A., Lytras, D., Kottaras, S., & Iakovidis, P. (2021). Effect of Aquatic Physiotherapy on Functioning, Balance Performance, Motor Performance, and Health-Related Quality of Life in Patients with Parkinson's Disease: A Review of Structure and Dosimetry of Aquatic Exercise Programs. Critical Reviews™ in Physical and Rehabilitation Medicine, 33(1).
Lawrence, M., Celestino Junior, F. T., Matozinho, H. H., Govan, L., Booth, J., & Beecher, J. (2015). Yoga for stroke rehabilitation. The Cochrane Library.
Leech, K. A., Roemmich, R. T., Gordon, J., Reisman, D. S., & Cherry-Allen, K. M. (2022). Updates in motor learning: implications for physical therapist practice and education. Physical therapy, 102(1), pzab250.
Levett, J. J., Elkaim, L. M., Niazi, F., Weber, M. H., Iorio-Morin, C., Bonizzato, M., & Weil, A. G. (2023). Invasive Brain Computer Interface for Motor Restoration in Spinal Cord Injury: A Systematic Review. Neuromodulation: Technology at the Neural Interface.
Li, R., Zhang, Y., Jiang, Y., Wang, M., Ang, W. H. D., & Lau, Y. (2021). Rehabilitation training based on virtual reality for patients with Parkinson’s disease in improving balance, quality of life, activities of daily living, and depressive symptoms: a systematic review and meta-regression analysis. Clinical Rehabilitation, 35(8), 1089-1102.
Li, F., Zhang, D., Chen, J., Tang, K., Li, X., & Hou, Z. (2023). Research hotspots and trends of brain-computer interface technology in stroke: a bibliometric study and visualization analysis. Frontiers in Neuroscience, 17.
Marasco, P. D., & de Nooij, J. C. (2023). Proprioception: A New Era Set in Motion by Emerging Genetic and Bionic Strategies?. Annual Review of Physiology, 85, 1-24.
Marotta, N., Demeco, A., Indino, A., de Scorpio, G., Moggio, L., & Ammendolia, A. (2022). Nintendo WiiTM versus Xbox KinectTM for functional locomotion in people with Parkinson’s disease: A systematic review and network meta-analysis. Disability and rehabilitation, 44(3), 331-336.
McGillicuddy, K.M. (2005), "Free Prize Inside! The Next Big Marketing Idea (1st edition)", Journal of Consumer Marketing, Vol. 22 No. 4, pp. 234-235.
Mikal-Flynn, J., Anderson, L. S., & Hoffman, J. (2018). Posttraumatic growth and metahabilitation in recreational therapy practice: A strengths-based pathway to recovery. Therapeutic Recreation Journal, 52(3).
Mishra, S. K., Singh, P., Bunch, S. J., & Zhang, R. (2012). The therapeutic value of yoga in neurological disorders. Annals of Indian Academy of Neurology, 15(4), 247.
Monteiro, K. B., dos Santos Cardoso, M., da Costa Cabral, V. R., Dos Santos, A. O. B., da Silva, P. S., de Castro, J. B. P., & de Souza Vale, R. G. (2021). Effects of motor imagery as a complementary resource on the rehabilitation of stroke patients: a meta-analysis of randomized trials. Journal of Stroke and Cerebrovascular Diseases, 30(8), 105876.
Murao, M., Kondo, T., Hamada, R., Miyasaka, J., Matsushita, M., Otagaki, A., ... & Matsuda, S. (2023). Minimal important difference of the 6-minute walk test after allogenic hematopoietic stem cell transplantation. Disability and Rehabilitation, 1-8.
Mustafaoğlu, R., Erhan, B., Yeldan, İ., Hüseyinsinoğlu, B. E., Gündüz, B., & Özdinçler, A. R. (2018). The effects of body weight-supported treadmill training on static and dynamic balance in stroke patients: A pilot, single-blind, randomized trial. Turkish Journal of physical medicine and rehabilitation, 64(4), 344.
Nardone, R., Orioli, A., Golaszewski, S., Brigo, F., Sebastianelli, L., Höller, Y., ... & Trinka, E. (2017). Passive cycling in neurorehabilitation after spinal cord injury: A review. The journal of spinal cord medicine, 40(1), 8-16.
Packheiser, J., Hartmann, H., Fredriksen, K., Gazzola, V., Keysers, C., & Michon, F. (2023). The physical and mental health benefits of touch interventions: A comparative systematic review and multivariate meta-analysis. medRxiv, 2023-06.
Park, Y. J., Park, S. W., & Lee, H. S. (2018). Comparison of the Effectiveness of Whole Body Vibration in Stroke Patients: A Meta-Analysis. BioMed Research International, 2018.
Ren, Y., Wu, Y. N., Yang, C. Y., Xu, T., Harvey, R. L., & Zhang, L. Q. (2017). Developing a wearable ankle rehabilitation robotic device for in-bed acute stroke rehabilitation. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 25(6), 589-596.
Scally, J. B., Baker, J. S., Rankin, J., Renfrew, L., & Sculthorpe, N. (2020). Evaluating functional electrical stimulation (FES) cycling on cardiovascular, musculoskeletal and functional outcomes in adults with multiple sclerosis and mobility impairment: a systematic review. Multiple sclerosis and related disorders, 37, 101485.
Sherrington, C. (1910). The integrative action of the nervous system. CUP Archive.
Silva, S., Borges, L. R., Santiago, L., Lucena, L., Lindquist, A. R., & Ribeiro, T. (2020). Motor imagery for gait rehabilitation after stroke. Cochrane Database of Systematic Reviews, (9).
Staples, A. (2017). Should robotic assisted gait training be the new standard of care for balance treatment in chronic stroke? A meta-analysis (Doctoral dissertation, California State University, Fresno).
Tan, X., Ding, Z., Guo, C., & Sun, P. (2023). Re-evaluation of Mirror Visual Feedback Therapy for a Systematic Evaluation/Meta-analysis of Physical Function Re-education After Stroke. American Journal of Physical Medicine & Rehabilitation, 102(3), 229-234.
Tedla, J. S., Gular, K., Reddy, R. S., de Sá Ferreira, A., Rodrigues, E. C., Kakaraparthi, V. N., ... & Nambi, G. (2022, March). Effectiveness of constraint-induced movement therapy (CIMT) on balance and functional mobility in the stroke population: a systematic review and meta-analysis. In Healthcare (Vol. 10, No. 3, p. 495). MDPI.
Truijen, S., Abdullahi, A., Bijsterbosch, D., van Zoest, E., Conijn, M., Wang, Y., ... & Saeys, W. (2022). Effect of home-based virtual reality training and telerehabilitation on balance in individuals with Parkinson's disease, multiple sclerosis, and stroke: a systematic review and meta-analysis. Neurological Sciences, 43(5), 2995-3006.
Wulf, G., & Prinz, W. (2001). Directing attention to movement effects enhances learning: A review. Psychonomic bulletin & review, 8(4), 648-660.
Yang, Y., Verkuilen, J. V., Rosengren, K. S., Grubisich, S. A., Reed, M. R., & Hsiao-Wecksler, E. T. (2007). Effect of combined Taiji and Qigong training on balance mechanisms: a randomized controlled trial of older adults. Medical science monitor: international medical journal of experimental and clinical research, 13(8), CR339–48.
Citation
Salzman, A. (2023). Proprioceptive rehab: 30 practical ideas and interventions for the neuro patient. OccupationalTherapy.com, Article 5694. Available at www.occupationaltherapy.com
