Editor's note: This text-based course is a transcript of the webinar, Skilled Nursing Facility Interventions: Interdisciplinary Collaboration Between Therapists And Certified Nursing Assistants, presented by Brittany Horvath, MS, CCC-SLP, CDP.
Learning Outcomes
- After this course, participants will be able to compare and contrast the terms interdisciplinary, interprofessional, and multidisciplinary.
- After this course, participants will be able to identify areas of clinical practice where interdisciplinary collaboration can be improved.
- After this course, participants will be able to recognize knowledge gained to clinical practice with multidisciplinary team.
Introduction
Hello and welcome everyone. I am looking forward to discussing interdisciplinary collaboration today.
Aging Population
- Growth of the aging population
- 65+ will double
- 85+ will triple
- Utilization of skilled nursing facilities
- 1.3 million in nursing homes
- 113% increase in referrals versus home health
The United States Census Bureau forecasts a notable demographic transformation, envisioning a doubling of Americans aged 65 and older from 2020 to 2060, constituting 23% of the total population. A particularly striking aspect of this shift is an anticipated threefold increase in individuals aged 85 and older during the same period. This demographic surge outpaces the projected growth in the supply of healthcare professionals, encompassing generalists, geriatricians, and specialists, presenting formidable challenges in ensuring adequate healthcare for the burgeoning adult and geriatric populations.
The escalating elderly demographic is accompanied by a rise in chronic, life-limiting, and progressive diseases, impacting both physical and psychological well-being. Consequently, families and caregivers grapple with an escalating burden when providing care for their elderly loved ones at home, prompting an increased reliance on skilled nursing and long-term care facilities. In 2017, the Centers for Disease Control and Prevention (CDC) estimated that approximately 1.3 million people reside in skilled nursing facilities. Notably, there was a 113% surge in referrals from hospitals post-pandemic, underscoring the strain on acute care settings attributable to staffing shortages.
IDT Team in SNF
- Social worker
- Registered dietician
- Nurse
- Medication aide (CMA)
- Nursing assistant (CNA)
- Occupational therapist (OT)/Occupational therapy assistant (OTA)
- Physical therapist (PT)/Physical therapy assistant (PTA)
- Speech-language pathologist (SLP)
- …and more
As the population admitted to skilled nursing facilities rises, the complexity of their care also intensifies. Patients with higher acuity and multiple comorbidities necessitate collaboration among healthcare professionals from various specialties.
Course Overview
- Healthcare is dynamic and multifaceted
- Collaboration is key
- Course Overview
- Key definitions
- Importance of collaboration
- Barriers to collaboration
- Components of successful collaboration
In the dynamic healthcare landscape, the pivotal elements of effective communication and collaboration are crucial pillars for maintaining care quality, elevating patient outcomes, and mitigating healthcare costs.
Within skilled nursing facilities, the synergy between certified nursing assistants (CNAs) and therapists assumes paramount importance in delivering comprehensive and patient-centered care. Addressing unique patient needs, therapists make substantial contributions to overall well-being, while CNAs dedicate their efforts to fulfilling daily basic requirements. The objectives of this course encompass an in-depth exploration of the dimensions inherent in therapy and CNA roles. Emphasis is placed on underscoring the significance of collaboration, identifying potential barriers, proposing effective communication strategies, and presenting ideas to foster successful interdisciplinary collaboration within healthcare facilities. This collaborative approach aspires to optimize patient care, enhance outcomes, and streamline the delivery of healthcare services.
Key Definitions
- Collaboration-Key features: More than one discipline, partnership, negotiating, and powersharing
- Interdisciplinary-Broad term (Most familiar): Key features: shared decision-making and goal-setting, communication, joint problem-solving, and mutual respect
- Interprofessional-More narrow terminology: Key features: communication, shared decision-making and goal-setting, joint problem-solving, and mutual respect
- Multidisciplinary- Key Features: Practicing in silos, communication may be filtered through a single entity
In collaboration, key definitions shape our understanding of the cooperative processes involved. Collaboration is characterized by the involvement of multiple individuals or disciplines working together toward a shared goal. Conversely, partnership is defined as a dynamic sharing and negotiation of power and ideas, often entailing conflict management. Interdisciplinary collaboration brings together individuals or teams from different backgrounds to collectively address complex problems or achieve common objectives. It encompasses shared decision-making, effective communication, joint problem-solving, mutual respect, and an emphasis on efficiency. Interprofessional collaboration, a related concept, involves members of various professions contributing their knowledge and expertise to tackle challenging situations, sharing common features with interdisciplinary collaboration. Although the terms "interdisciplinary" and "interprofessional" collaboration are frequently used interchangeably, this presentation adopts "interdisciplinary" as a broad and encompassing term due to its widespread familiarity and usage.
Within skilled nursing facilities (SNFs), interdisciplinary teams (IDTs) typically include essential members such as social workers, registered dietitians, nurses, certified medication aides (CMAs), certified nursing assistants (CNAs), and the therapy team. The therapy team comprises occupational therapists (OTs), occupational therapy assistants (OTAs), physical therapists (PTs), physical therapy assistants (PTAs), and speech-language pathologists (SLPs). While other roles are undoubtedly crucial, this discussion will predominantly delve into the relationship between certified nursing assistants and OTs, OTAs, PTs, PTAs, and SLPs.
Importance of Collaboration
- IDT collaboration is important because
- Increased patient outcomes
- Increased quality of care
- Decreased healthcare spending
- Decreased length of stay
- Examples:
- Contracture management
- Fall prevention
- Independence
- Quality of life
Interdisciplinary collaboration within healthcare holds critical importance for various reasons, as evidenced in existing literature showcasing positive impacts on patient outcomes and the overall quality of care. Furthermore, this collaborative approach has been associated with favorable effects on the healthcare system, manifesting in reduced spending and shorter lengths of hospital stays. In the context of skilled nursing facilities, where successful outcomes are paramount, the collaboration between therapists and certified nursing assistants (CNAs) emerges as a linchpin for achieving these positive results. Conversely, a lack of collaboration can lead to detrimental consequences, negatively affecting patient outcomes, independence, and overall quality of life.
Illustrating the tangible benefits of collaboration, consider the area of contracture management. Joint contractures, prevalent in long-term care, are linked to risk factors such as neurologic disease and impaired mobility, correlating with poor outcomes and diminished quality of life. A study by Lamm et al in 2022 revealed that the highest risk of developing limb contractures occurs within the first five years of admission to a long-term care facility, with prevalence rates ranging from 0.7% to 3.2% for upper limbs and 0.3% to 6% for lower limbs per year. Collaboration between charge nurses, CNAs, and the therapy team becomes paramount in mitigating the risk of state regulatory issues and, more importantly, preventing the development of contractures in patients.
In another critical aspect, fall prevention, Gillespie et al's Cochrane review in 2022 indicated that around 30% of individuals aged 65 and above experience falls each year, a percentage that rises to 50% in those over 85. Given the multifactorial nature of fall risk, collaboration and communication between disciplines play a pivotal role in decreasing these risks. This includes addressing overall deconditioning, cognitive impairments, visual impairments, nutrition, and hydration. Sharing knowledge between therapists and CNAs benefits the individual patient and can enlighten CNAs to identify and address similar barriers with other patients. Fall prevention extends beyond physical considerations, incorporating cognitive and communication factors often overlooked in education and training.
Effective communication also extends to patient-specific needs, as demonstrated in scenarios where verbal commands may not be effective but tactile and visual commands prove successful. Sharing such insights between therapists and nursing colleagues minimizes the risk of falls and frustration for both parties. A meta-analysis by Lee and Hee (2016) reinforced the positive impact of exercise programs on fall prevention in skilled nursing facilities. Additionally, combining exercises with environmental modifications and assistive devices was found to enhance the effectiveness of fall prevention programming. Moreover, incorporating cognitive retraining and toileting programs, guided by collaborative efforts between CNAs and therapy, has demonstrated success in urinary incontinence management, further contributing to fall prevention.
Beyond addressing specific issues, collaboration between CNAs and therapists positively influences patients' activity levels throughout the day, promoting overall independence. Recognizing that patients may spend limited time in therapy, ensuring they remain active during the rest of the day is crucial to sustaining the gains made during therapy sessions and improving physical and cognitive functioning. This holistic approach aligns with the expectations of insurance companies and contributes to an enhanced quality of life for the patients.
Seeking insights from colleagues on the significance of interdisciplinary collaboration, their perspectives reaffirmed its critical nature in achieving positive outcomes in patient care.
- “IDT collaboration is an important aspect of patient-centered care in order to provide a multidisciplinary goal-oriented treatment approach. Communication with other disciplines helps to keep all team members informed, allowing for each discipline to provide the best care. IDT also helps to bring organization to the plan of care, preventing duplicate goals and builds trust with the patient.” – Stefanie J., PT, DPT
- “Teamwork makes the dream work! Without IDT the patient would not receive intervention reinforcement. I think it would take significantly longer for them to reach their goals.” – Paige A., OTR
Stephanie, a physical therapist, underscores the pivotal role of Interdisciplinary Team (IDT) collaboration in fostering patient-centered care through a comprehensive, goal-oriented treatment approach. The cornerstone of this approach lies in effective communication with team members from various disciplines, ensuring that each member is well-informed and able to contribute to the provision of optimal care. Stephanie emphasizes that IDT brings a sense of organization to the plan of care, averting redundant goals and establishing a foundation of trust with the patient.
Paige, an occupational therapist, succinctly captures the essence of IDT collaboration by stating, "Teamwork makes the dream work." She emphasizes that without the collaborative efforts of the IDT, patients would lack the reinforcement needed for their interventions, significantly impeding their progress toward achieving goals. Paige contends that poor collaboration exacerbates the inherent challenges of the healthcare landscape, potentially prolonging the time it takes for patients to reach their desired outcomes. In essence, the sentiments expressed by both Stephanie and Paige underscore the indispensable nature of interdisciplinary collaboration in navigating and optimizing patient care within the complex healthcare environment.
Barriers to IDT Collaboration
- Hierarchical structures
- Lack of clear roles and responsibilities
- Communication challenges
- Time constraints
- Cultural and organizational differences
- Ego and professional identity
- Lack of education and training
- Resistance to change
- Resource constraints
- Practicing in silos
- Resident complexity
- Differences in perceived vs. actual encouragement
Barriers to effective Interdisciplinary Team (IDT) collaboration are multifaceted and can significantly impact patient care. One prevalent barrier is the existence of hierarchies within healthcare organizations. Traditionally, these hierarchies can create power imbalances, where certain professions, such as physicians or therapists, may be perceived as power holders. Unclear delineation of roles and responsibilities within the team can lead to confusion and conflicts, with team members, like Certified Nursing Assistants (CNAs), uncertain about expectations, patient functioning, and leadership in specific situations. Effective communication is crucial in mitigating these challenges and sustaining IDT collaboration.
Communication barriers further compound collaboration challenges between CNAs and therapy teams. Differences in language, including unfamiliar medical terminology, can lead to misunderstandings, errors, and a lack of trust among team members, patients, and their families. High stress, time-sensitive environments, and productivity standards limit opportunities for collaboration between therapists and CNAs, hindering discussions on patient care and coordination of services. Additionally, cultural, organizational, and disciplinary differences contribute to tensions within IDT, impacting effective communication and collaboration.
Personality differences, strong professional identities, and a fear of losing autonomy may breed resistance to input from other disciplines. Variations in formal education within the same discipline can hinder effective IDT collaboration, as some may lack training in the necessary skills. Resistance to change and input from others poses additional challenges. Staffing shortages in healthcare, a pervasive issue, limit resources and impact the assembly and maintenance of IDT teams, affecting patient care and outcomes.
The trend toward healthcare specialization can create silos within departments or specialties, impeding collaboration. Algrain's warning in 2010 about this phenomenon, highlighting its potential to lead to poor patient outcomes and confusion, remains relevant. The complexity of patients admitted to skilled nursing facilities, often with multiple comorbidities, further complicates collaboration efforts. Patient refusal to participate and differences in perceived versus actual encouragement present additional hurdles. Studies reveal instances where nursing staff completed patients' activities of daily living (ADLs) without proper encouragement, emphasizing the gap between perception and observed behavior.
In a case study, these barriers come to life, illustrating the challenges faced by IDT teams and the potential repercussions on patient care and outcomes. The importance of addressing these barriers becomes evident in ensuring the effectiveness of interdisciplinary collaboration in healthcare settings.
Unsuccessful Collaboration: Case Study #1
- Mr. E is a 36-year-old male who suffered an anoxic brain injury. He arrived at the skilled nursing facility on a Thursday night. Evaluations by PT, OT, and SLP were completed the following morning.
- He presented as follows:
- Max assist x2 for bed mobility and transfers
- Dependent for ADLs due to contractures
- PO diet (puree/nectar), though he has a PEG tube
- Speech is severely dysarthric; he can speak 1-2 semi-intelligible words per breath
Mr. E, a 36-year-old male, was admitted to the skilled nursing facility following a several-month-long hospital and inpatient rehabilitation stay. His admission on a Thursday night was swiftly followed by evaluations from Physical Therapy (PT), Occupational Therapy (OT), and Speech-Language Pathology (SLP) on Friday morning. During the evaluations, Mr. E's condition was assessed as follows: he required maximum assistance, with support from two individuals, for bed mobility. His dependence on others extended to Activities of Daily Living (ADLs) due to existing contractures in his hands, which were evident upon admission. Dietary considerations included a puree diet and nectar-thick liquids, complemented by a PEG tube. Furthermore, his speech was severely dysarthric, with only approximately 50% intelligibility, allowing for the expression of one to two words per breath. This comprehensive evaluation forms the foundation for the interdisciplinary collaboration needed to address Mr. E's complex needs and enhance his overall quality of life.
- Verbal communication to nursing staff: Hoyer lift, “feeder”, splints to both hands, puree/nectar until MBSS, and utilize simple yes/no questions for basic wants and needs.
- Monday morning:
- Family upset
- Not out of bed all weekend, no splints
- Not consistently assisted with meals
- Not allowed additional time to respond
- Family upset
The interdisciplinary collaboration for Mr. E faced an immediate challenge in effective communication and coordination of care. Following the evaluations, the therapists conveyed a concise verbal update to the charge nurse and the Certified Nursing Assistant (CNA), emphasizing the need for a Hoyer lift and assistance with feeding due to Mr. E's condition. Specific instructions were provided to use yes/no questions for a basic understanding of his wants and needs.
However, by Monday morning, a family member expressed dissatisfaction, awaiting meetings with the Director of Nurses and the Director of Therapy. The concerns raised were substantial – Mr. E had not been mobilized from bed throughout the weekend, his splints were not in use, consistent assistance with meals was lacking, and there was a failure to allow additional time for him to respond to questions due to the exclusive use of yes/no format.
- Reflect on:
- Your communication with nursing after treatment or evaluation
- Facility and state rules regarding communication
- Whiteboard
- Stickers
- EMR use
When contemplating this example and delving into effective communication strategies to enhance Interdisciplinary Team (IDT) collaboration, it's essential to reflect on the nature of communication with Certified Nursing Assistants (CNAs) post-evaluations and treatment sessions. Additionally, it's crucial to consider the facility and state regulations governing communication practices. Does your facility employ whiteboards for conveying important information? Is there a sticker system in place? And are therapists allowed to input information directly into the Electronic Medical Records (EMR)?
Unsuccessful Collaboration: Case Study #2
- Mrs. F is a 72-year-old female who was originally admitted to the SNF eight months ago after a right middle cerebral artery stroke. She is now a long-term resident due to a lack of caregiver support available at home.
- Mrs. F has the following deficits: poor decision-making and problem solving skills, lack of insight, left sided weakness, visuospatial deficits, and poor short-term memory.
- Recently referred to therapy following a fall
We're also going to look at Mrs. F., a 72-year-old female who was admitted to the skilled nursing facility eight months ago following a right MCA stroke. She's now a long-term care resident due to the lack of caregiver support at home. She has the following deficits from her stroke.
Poor decision-making skills and problem-solving skills, a lack of insight into her deficits, left-sided weakness, visual-spatial deficits, and poor short-term memory. She was recently referred to therapy due to having a fall.
- After evaluation by PT and OT, it is determined that Mrs. F would benefit from:
- Rehabilitative therapy with PT and OT
- Concomitant restorative nursing therapy
- Increased opportunities to attend facility activities
- Written and verbal communication provided to nursing team and CNAs; no visual aids or demonstration provided
After thorough evaluations, PT and OT recommended rehabilitative therapy for the patient. In conjunction with this, they suggested incorporating restorative nursing exercises and increasing the patient's engagement in facility activities. The recommended exercises were communicated to the nursing staff verbally and in writing. However, it's important to note that no visual demonstration accompanied the instructions due to the unavailability of the CNA, and the written instructions lacked accompanying pictures. This absence of visual aids could potentially impact the clarity and understanding of the prescribed exercises, highlighting the need for comprehensive communication methods in interdisciplinary care.
- What can go wrong in this scenario?
- Communication breakdown
- Lack of visual aids or demonstration
- Carryover
- Communication breakdown
- Misunderstanding of responsibilities
- CNA received limited guidance
- CNAs may not recognize the significance of certain exercises
- Prioritize other tasks
In this scenario, several potential issues can arise, primarily centered around communication breakdowns and the absence of visual aids during the therapeutic plan dissemination. The therapist communicated the plan verbally and in writing; however, the lack of a visual demonstration and accompanying pictures introduces potential challenges.
Firstly, there is a risk of misunderstanding responsibilities. The Certified Nursing Assistants (CNAs), tasked with executing the plan and administering exercises, might perceive the guidance as limited due to the absence of a visual demonstration. The written instructions, although present, may be challenging to interpret for those unfamiliar with the specific verbiage or exercise techniques. This can lead to a breakdown in the transfer of information, where staff members may not pass along crucial details, hindering the seamless implementation of the prescribed plan.
Furthermore, without a visual demonstration, the significance of the activity may not be fully recognized by the CNAs. This lack of awareness could result in the de-prioritization of the exercises, potentially leading to incomplete or inadequate execution. The absence of a clear visual guide might impact the overall understanding of the therapeutic plan, potentially compromising its effectiveness in the absence of a comprehensive and universally understandable communication method.
- What can go wrong (continued)…
- Lack of follow-up/inadequate monitoring
- Therapy may assume exercises are being completed
- CNAs may not feel comfortable approaching therapists
- Patient frustration and deterioration
- Lack of physical activity can contribute to a decline in mental state, psychosocial well-being, and quality of life
- Can increase dependence on others for basic care needs
- Lack of follow-up/inadequate monitoring
If there is a lack of follow-up between the therapists and the CNAs or if the CNAs feel hesitant to approach the therapists with questions or concerns, it creates a potential for miscommunication and negative outcomes.
The therapists may assume that the prescribed exercises are being implemented by the CNAs, leading to potential frustration on the part of the therapists if this is not the case. This lack of clarity and feedback can contribute to a divide between disciplines, impacting the overall collaborative environment within the healthcare team.
Moreover, the ramifications extend beyond professional frustrations. Being at the center of the care plan, the patient might experience frustration due to the potential deterioration of skills resulting from inadequate exercise. The negative impact on the patient's mental state, stemming from limited physical activity and cognitive stimulation, can lead to increased dependency on assistance for basic care needs. This compromises the therapeutic plan's effectiveness and adversely affects the patient's overall well-being and quality of life. Therefore, ongoing communication and collaboration between disciplines are crucial to ensuring the successful implementation of care plans and positive patient outcomes.
- Reflect on:
- Your communication with CNAs regarding splinting and exercises – how can it be easier?
- Goal writing in maintenance plans or exercise programs
- Facility and state rules regarding visual aids
- How can follow-up and check-ins be facilitated?
Reflecting on the case study, it's essential to consider the communication dynamics between therapists and Certified Nursing Assistants (CNAs) regarding therapy-specific needs, such as splinting, maintenance programs, toileting programs, and feeding strategies. Effectively conveying the significance of movement and exercises is crucial, and the communication method, including visual aids and demonstrations, plays a pivotal role.
Firstly, evaluating the efficiency of communication is crucial. Are therapy-specific needs being effectively communicated to CNAs? Is the education on the significance of movement and exercises clear and comprehensive? Demonstrating exercises to CNAs, where applicable, can enhance understanding and implementation.
Understanding facility and state rules regarding visual aids and communication is also vital. Does the facility have guidelines on using visual aids in patient care? Are therapists allowed to demonstrate exercises visually, and what tools or platforms are permissible for such demonstrations?
Facilitating follow-up and check-ins is a key aspect of ensuring ongoing collaboration. Regular team meetings or huddles can provide a structured discussion forum on patient progress, and barriers, and address any questions or concerns. Open lines of communication and an approachable atmosphere are essential for fostering teamwork.
However, barriers can exist within specific facilities and teams. Time constraints, varying levels of familiarity with therapeutic terminology, and differences in work cultures between therapy and nursing staff can pose challenges. Establishing a collaborative culture that encourages questions and feedback can help overcome these barriers.
To prevent failures in communication, therapy and nursing teams must establish effective channels. This involves clarifying roles, providing clear instructions, utilizing visual aids when necessary, and implementing regular check-ins to review patient progress and address concerns. These elements contribute to a collaborative and patient-centric approach to care, fostering a positive and supportive working environment.
Components of Successful Collaboration
- What is needed?
- Build rapport
- Knowledge and respect of roles and responsibilities
- Clear and effective communication
- Cross-training and education
- Competencies
- Importance of out of bed activity
- Working through barriers
- Practice!
- Develop a feedback mechanism.
- Involving CNAs in problem-solving
- Conflict resolution and management
- Celebrate successes!
Successful collaboration relies on several key components, each creating a positive and efficient working environment. Establishing strong interpersonal relationships builds trust and promotes a positive team dynamic. A clear understanding of individual roles and responsibilities is crucial to preventing confusion and ensuring a smooth workflow within the team. Transparent and effective communication, utilizing familiar language and diverse channels, is the backbone of cohesive teamwork.
Cross-training and education opportunities contribute to a comprehensive understanding of each team member's role, fostering a more knowledgeable and adaptable workforce. Ensuring team members possess the necessary competencies is paramount for maintaining overall efficiency and delivering quality care.
Recognizing the importance of out-of-bed activity is essential, as it promotes mobility and mental health among patients. Providing CNAs with the skills to navigate barriers in patient care ensures effective problem-solving and contributes to successful collaboration. Regular practice reinforces learned skills, maintaining proficiency in therapists' and CNAs' roles.
Establishing a feedback mechanism allows for continuous improvement by providing insights into processes and fostering a culture of collaboration. Encouraging the active involvement of CNAs in problem-solving instills a sense of ownership and contributes to collaborative resolution. Conflict resolution skills are vital to ensure disagreements do not impede collaboration, fostering an environment where conflicts lead to constructive solutions.
Lastly, celebrating successes, regardless of size, is crucial to reinforcing team morale and cultivating a positive working culture. These components work together to create a collaborative and patient-focused care environment.
Build Rapport
- Get to know your colleagues
- Find level ground
- Ellingson (2003) – rapport increases when you discuss personal lives and work complaints
- Find level ground
First and foremost, building rapport is a fundamental aspect. Taking a moment to introduce oneself, inquire about the names of the CNAs, and address them by name creates a foundation for a positive relationship. Despite the constraints of a busy schedule, investing a few minutes in greeting and getting to know the CNAs can significantly impact collaboration and, consequently, patient care.
An illustrative example highlights the importance of such interactions. In an experience, a CNA preferred specific greetings, expecting a personalized "good morning" or "good afternoon" along with her name. While seemingly trivial, adhering to this preference became a simple yet effective way to establish respect and rapport. Despite its simplicity, it demonstrated an understanding of individual preferences, contributing to a more positive working relationship.
Research by Ellingson in 2003 underscores the significance of personal connections in the workplace. Colleagues discussing personal lives or finding common ground in work-related discussions, such as addressing staffing concerns or scheduling issues, contributed to improved relationships on the floor. This emphasizes that building rapport involves professional interactions and acknowledging and respecting personal preferences, fostering a collaborative and harmonious working environment.
Define Roles and Responsibilities
- Decreases overlap, gaps, and misunderstandings
It is imperative to be attentive to potential confusion surrounding roles and responsibilities within the healthcare team. Actively engaging in understanding and defining the roles and responsibilities of each team member is vital to minimize overlap, address gaps, and prevent misunderstandings.
There are instances where, for example, a therapist may work with a patient on ADLs in the morning, and it's crucial to communicate the rationale behind the schedule. Clear communication with CNAs, explaining that these ADLs are specific to certain days, can alleviate misconceptions and contribute to a shared understanding. This not only prevents misunderstandings but also enhances trust, both from the patient and their family members, in the collaborative efforts of the team.
While not delving into exhaustive details, the non-exhaustive list of responsibilities for therapists and CNAs displayed on your screen (Figure 1) serves as a reference point for understanding the diverse roles within the healthcare team. Defining these roles promotes clarity, streamlines workflows, and contributes to effective collaboration in patient care.
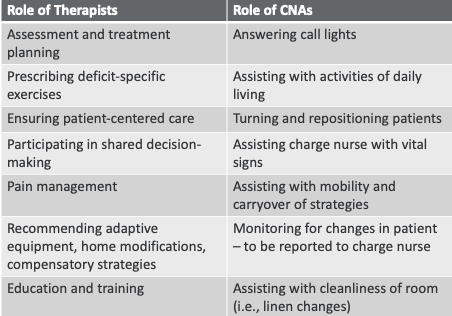
Figure 1. Table of the role of therapists versus CNAs.
The roles of therapists and CNAs are dynamic and subject to constant evolution based on the demands of specific facilities and the broader healthcare environment. Unprecedented situations, like those witnessed during the COVID-19 pandemic, may lead to therapists temporarily taking on roles traditionally fulfilled by CNAs, exemplifying the adaptability required in the healthcare field. While such instances may not be the norm, they underscore the flexibility inherent in our roles to meet the diverse needs of the facility.
In this ever-changing landscape, therapists also find themselves engaged in tasks like answering call lights and potentially changing linens, particularly when assisting patients in the morning. These activities, while not core to traditional therapy roles, contribute significantly to rapport-building and cultivating collaborative relationships. Acknowledging the broader spectrum of responsibilities fosters a sense of shared purpose and teamwork.
Despite working alongside CNAs, it's crucial to recognize that their understanding of therapists' intricacies may be limited. While therapists gain insights into the daily responsibilities of CNAs through collaboration, the reciprocal understanding may not be as comprehensive. Therefore, fostering open communication and offering insights into the nuances of therapeutic practices can enhance mutual understanding and strengthen collaborative efforts within the healthcare team.
Clear and Effective Communication
- Facilitates regular and timely exchanges
- Decreases misunderstandings
- Goal: message from sender = message heard by receiver
- Communication strategies
- Effectiveness vs. efficiency
- Ways to improve
- Be approachable!
- Clear, concise, understandable
- Preparation and organization
- Know your audience
- Exhibit active listening
Successful collaboration hinges on establishing clear communication channels to facilitate regular and timely exchanges of information, thereby reducing the likelihood of misunderstandings. The goal of communication is to ensure that the message conveyed by the sender aligns with what the receiver comprehends. However, achieving this alignment can be challenging, and efficiency in communication doesn't always equate to effectiveness.
Efficiency, exemplified by leaving a note at the nurse's station, may fall short in effectiveness if the message is misplaced or overlooked during shift changes. Conversely, while waiting to educate the next shift's Certified Nursing Assistants (CNAs) may be effective, it might not be the most efficient use of time. Striking a balance between efficiency and effectiveness is crucial.
Improving communication effectiveness involves being approachable and creating a level playing field, acknowledging the time constraints therapists and CNAs face. Clarity, conciseness, and understandability are key attributes of effective communication. Using medical terminology judiciously and adapting communication to the audience's knowledge level, from physicians to patients, ensures that information is easily digestible.
Active listening plays a pivotal role in effective communication, fully engaging with a communication partner and summarizing or asking relevant questions to demonstrate understanding. For instance, responding to a CNA's report about a patient's right knee buckling with active listening assures the CNA that their concerns are acknowledged and will be addressed, even within the therapist's time constraints. This approach fosters a culture of reciprocal understanding and collaboration within the healthcare team.
Cross-training and Education
- Therapists knowledge of nursing > nurses knowledge of therapy
- Knowledge = Power = Patient Outcomes
- Importance of activity (physical and cognitive)
- Practice!
- Hands-on demonstrations
- Simulation
- Working through barriers
- Task modification and approach
- Do it early!
In the realm of healthcare collaboration, building rapport stands out as a foundational element. Even in our hectic schedules, taking a moment to introduce ourselves and learn about the CNAs we work with can go a long way. An example from my experience involves a CNA who insisted on a specific greeting. A simple shift from a generic "hello" to a personalized "good morning, [insert name]" built rapport and, surprisingly, impacted patient care positively. Research by Ellingson in 2003 emphasizes that personal connections among colleagues enhance teamwork, and discussions about personal and work-related matters contribute to better relationships.
Roles and responsibilities, often a potential source of confusion, demand proactive clarification. I've encountered instances where the lack of communication led to CNAs expecting daily repetition of morning ADLs after a therapy session. Articulating our plans and reasoning minimizes misunderstandings and fosters trust among all parties. While I won't delve into every detail, I've found that having a shared understanding of responsibilities (Figure 1) helps create a smoother collaborative environment.
Our roles in healthcare are dynamic, especially during challenging periods like the COVID era. Therapists might find themselves taking on responsibilities typically handled by CNAs. Recognizing and appreciating these role shifts, such as assisting with changing linens or responding to call lights, aligns with teamwork and contributes to rapport-building.
Clear communication channels are crucial for effective collaboration. I've learned that the efficiency of communication doesn't always guarantee its effectiveness. Leaving notes for the nursing staff might be efficient, but it doesn't ensure the message reaches everyone. Instead, investing time in face-to-face communication, despite being less efficient, can be more effective in relaying important information.
Cross-training and education are imperative, and I've witnessed situations where visual education significantly enhanced understanding. In a recent survey by Novec et al (2023), nurses expressed a perception gap between therapy and nursing. Bridging this gap involves mutual education on roles, goals, and insurance constraints. Sharing insights into therapy practices, insurance nuances, and length of stay expectations enlightens CNAs, empowering them to contribute meaningfully to patient care.
Early training offers numerous advantages. Advocating for patients to move to long-term care rooms early, allowing therapists to train CNAs multiple times. This not only aids continuity but also ensures that, as therapists, we can continue to provide necessary insights even after the formal therapy sessions conclude.
Active listening is a powerful tool in practice sessions. Acknowledging the concerns or updates from CNAs and summarizing our understanding builds trust. In one instance, a CNA flagged an issue with a patient's knee buckling, and through active listening, I assured her I would address it promptly after my ongoing evaluation.
Cross-training also extends to teaching CNAs how to navigate barriers with patients who may resist assistance. In my experience, providing examples of task modifications and emphasizing the impact of small adjustments in approaching patients helps CNAs overcome challenges without confrontation.
Effective collaboration involves these intertwined elements — building rapport, clarifying roles, establishing clear communication, and continuous cross-training. These practices, rooted in real-world examples, contribute to a positive, collaborative environment, ultimately benefiting patient outcomes.
Other Ideas
Here are some other ideas in Figure 2.
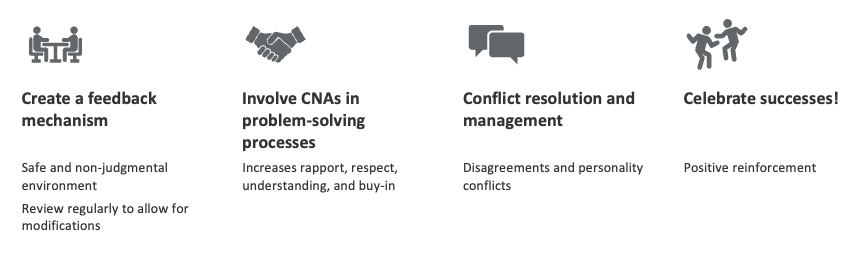
Figure 2. Graphic of other ideas for collaboration.
Establishing an effective feedback mechanism is like creating a bridge between therapists and CNAs, allowing for a dynamic exchange of insights. Think of it as a two-way street where both parties actively engage in providing and receiving feedback. Picture this: regular reviews of this feedback mechanism from a leadership perspective ensure continuous improvement in collaborative processes, making it akin to performing routine maintenance on the bridge for seamless travel.
Active listening is the cornerstone of this process. Imagine an instance where therapists and CNAs engage in open conversations, making eye contact, verbally engaging, and truly understanding each other's perspectives. It's like tuning the instruments of the orchestra to ensure everyone is in harmony, creating a symphony of collaboration.
Let's delve into problem-solving, a joint venture where therapists and CNAs come together to navigate challenges. Consider a scenario where a patient's toileting preferences need attention after therapy hours. By involving CNAs in the discussion, the team addresses the problem and strengthens their bond. It's akin to a brainstorming session where everyone contributes to finding the best solution, fostering a sense of shared responsibility.
Transition to conflict resolution and management are the tools in the toolkit for constructively addressing disagreements. Picture it as a compass guiding the team through potentially tricky situations, ensuring a smooth journey even when the terrain gets rough. Learning about one's emotional expression becomes crucial here, like understanding the weather conditions for a safe journey.
Finally, celebrating successes acts as the fuel that keeps the collaborative engine running smoothly. Think of it as regularly servicing the engine, ensuring it runs efficiently. Small gestures, such as providing Halloween candy or acknowledging CNA Week with treats, act as pit stops that refuel the team's energy. Picture a team event, like a potluck or cook-off, where therapists and CNAs not only bond but witness the progress of patients. It's a celebration of teamwork and mutual respect, like the victory lap after completing a challenging race.
What Are Professionals Saying: Video 1
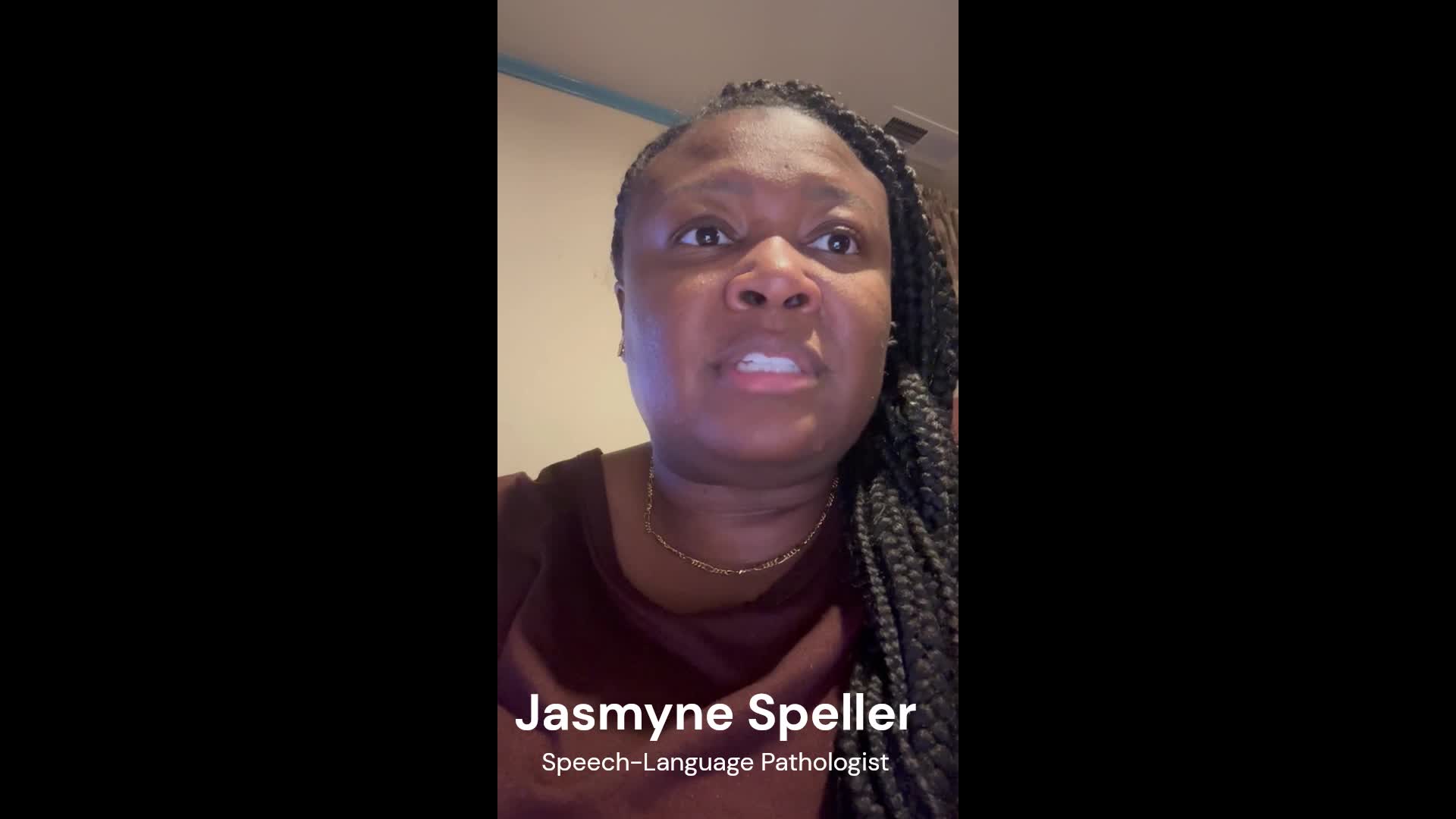
This is Jasmyne Speller. She's a speech-language pathologist in Georgia. She has over a decade of experience in skilled nursing. Half of that time she spent as the rehab director and she will give us some of her thoughts on interdisciplinary collaboration.
What Are Professionals Saying: Video 2
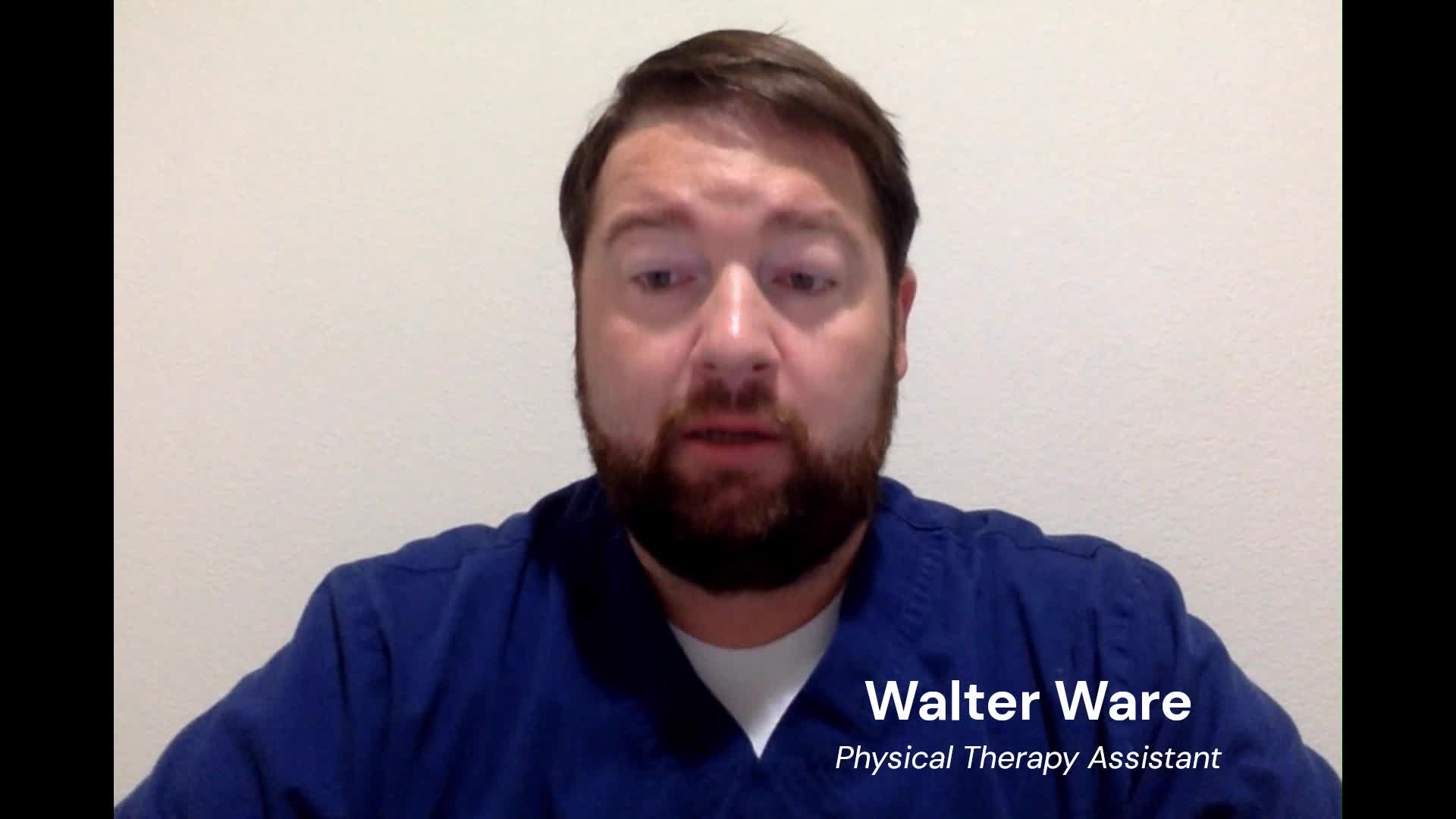
This is Walter Ware. He is a physical therapy assistant. Walter was a key component in his rehab team and was an excellent example of cultivating a culture of teamwork with the CNAs.
- Good leadership and set protocols help to improve IDT collaboration. Predetermined set expectations of staff and weekly meetings can help improve communication between team members” – Stefanie J., PT, DPT.
This quote is from Stephanie, whom we heard from earlier. She states good leadership and set protocols help to improve IDT collaboration. Predetermined set expectations of staff and weekly meetings can help improve communication between team members.
Successful Collaboration- Organization
- Encourage organizational leadership support
- Interdisciplinary rounds
- Standardized care protocols and competencies
- Patient-centered care
- Communication
- Leadership
- Conflict management and resolution
- Transparency and teamwork
- Inclusive care planning
- Quality improvement projects
Within organizational collaboration, the adage "it starts at the top" is acknowledged, but the emphasis lies on the effectiveness of interdisciplinary team (IDT) collaboration being most impactful on the floor and moving upwards. Encouraging support from organizational leadership for IDT collaboration is crucial, and individuals can set an example for effective collaboration within their teams. Several strategies are proposed to foster organizational support:
Despite potential time constraints for therapists or CNAs, organizational leadership can play a pivotal role by initiating regularly scheduled rounds. These rounds would involve discussions on patient progress, current level of function, treatment plans, goals, and discharge planning. Introducing specific protocols or checklists can further engage employees in determining their competency levels and ensure collaborative care.
Recognizing employees' skill sets is essential for collaborative care. For instance, considering the communication styles of therapists—some extroverted and hands-on, while others are introverted and contribute in different ways—can help assign roles effectively. This approach enhances the collaborative dynamic within the team.
Simulated competency training for conflict management and resolution can be beneficial. By practicing these skills in a controlled setting, team members can develop effective strategies for handling conflicts when they arise.
Ensuring each team member understands their role and responsibilities within collaborative care promotes transparency and effective teamwork. Clear communication of contributions fosters an environment where everyone understands how they contribute to the overall goal.
Providing regular opportunities for therapists and CNAs to learn and discuss relevant topics related to patient care, discipline-specific matters, or facility-specific initiatives is vital. This ongoing education contributes to improved collaboration, reduced errors, and streamlined processes.
Including CNAs and therapists in developing care plans enhances collaboration. Discussing initiatives aimed at improving collaboration within teams and facilities becomes more effective when all involved parties contribute to the planning process.
By implementing these strategies, organizations can create a culture that supports and values interdisciplinary collaboration, ultimately leading to improved patient outcomes, reduced errors, and enhanced teamwork.
Successful Collaboration- Students
- Ideas for student clinicians
- Allow them to spend time with other disciplines
- Benefits of Interprofessional Education
- Development of stereotypes
- Silo-type thinking
- Cooperation and interaction
Incorporating students into the collaborative process and providing them with an understanding of the importance of interdisciplinary teamwork involves offering opportunities for cross-training and exposure to various disciplines. For instance, a friend teaching graduate-level speech-language pathology shares an innovative approach. Twice a semester, her students engage in cross-training with nursing students during simulation labs. This fosters insight into each other's disciplines and provides valuable hands-on experience in diverse fields.
Another example is drawn from a speech-language pathologist's experience. Whenever physical or occupational therapy students were present, they were invited to observe modified barium swallow procedures. This exposure proved enlightening for these students, offering insights into practices beyond their primary field.
Starting cross-training initiatives during undergraduate and graduate programs and extending them into externship experiences, yields numerous benefits. Literature suggests that introducing interdisciplinary collaboration early in education helps negate the development of stereotypes, reduces silo-type thinking, and cultivates a willingness to interact and cooperate with other professions. Preparing students with a collaborative mindset equips them to positively influence their future workplace, contributing to creating and nurturing a collaborative care environment.
Successful IDT Collaboration: Case Study #1
- Mr. E is a 36-year-old male who suffered an anoxic brain injury. He arrived at the skilled nursing facility on a Thursday night. Evaluations by PT, OT, and SLP were completed the following morning.
- Max assist x2 for bed mobility and transfers
- Dependent for ADLs due to contractures already forming in his hands on admission
- PO diet (puree/nectar), though he has a PEG tube
- Speech is severely dysarthric; he can speak 1-2 semi-intelligible words per breath
In reconsidering Mr. E's case, where collaboration faced challenges due to communication breakdowns, exploring avenues for enhancing success is crucial. Effective communication with CNAs is pivotal, and understanding facility and state regulations regarding visual aids is essential. To improve collaboration, incorporating multiple communication channels is recommended. This may involve utilizing whiteboards or electronic means for clear and visible instructions. Regular team meetings or huddles can provide opportunities for verbal communication and clarifications.
Moreover, incorporating visual aids such as diagrams or infographics alongside written instructions can enhance understanding, catering to different learning styles. Establishing a structured follow-up system, where therapists routinely check in with CNAs, can address concerns, ensure comprehension, and create an environment conducive to questions and feedback.
Facilitating training sessions that include visual demonstrations of exercises and care techniques can bridge gaps in understanding. Acknowledging the significance of movement and exercises and conveying this effectively to CNAs can foster a shared commitment to patient well-being. Creating an open and collaborative atmosphere, where all team members feel valued, can significantly enhance the likelihood of successful collaboration and improved patient outcomes.
- What can make this case more successful?
- Involve the CNA in a portion of the evaluations.
- Natural way to complete demonstration and hands-on training as well as education
- Allow feedback to flow easily in both directions
- Communicate with the following shift
- According to facility and state regulations
- Whiteboard
- Stickers
- EMR?
- Orders?
- According to facility and state regulations
- Involve the CNA in a portion of the evaluations.
- Is what you are already doing working? GREAT!
In optimizing collaboration for cases like Mr. E, involving CNAs actively in the evaluation process can be transformative. Initiating communication with CNAs beforehand and informing them about the evaluation schedule creates an environment of shared responsibility. For instance, coordinating with CNAs to be present during evaluations at specific times of the day, as exemplified by your colleague's practice at 7:00 AM, sets clear expectations and facilitates their involvement.
Having CNAs present during evaluations opens avenues for immediate collaboration. It enables real-time education, return demonstration, and feedback. This collaborative approach empowers CNAs to understand the therapy goals, actively participate in care strategies and allows them to express any concerns or discomfort. Addressing such concerns promptly fosters a collaborative and supportive atmosphere.
Understanding facility regulations on communication methods is essential. Whether utilizing whiteboards, electronic medical records (EMR), or other channels, aligning communication practices with the facility's guidelines ensures consistency. Additionally, seeking input from CNAs on the most effective means of communication for smooth transitions between shifts contributes to a more streamlined and efficient process. The collaborative effort becomes a shared commitment to patient care and outcomes by actively involving CNAs in the evaluation and communication processes.
Successful IDT Collaboration: Case Study #2
- Mrs. F is a 72-year-old female who was originally admitted to the SNF eight months ago after a right middle cerebral artery stroke. She is now a long-term resident due to a lack of caregiver support available at home.
- Mrs. F has the following deficits: poor decision-making and problem-solving skills, lack of insight, left-sided weakness, visuospatial deficits, and poor short-term memory
- Recently referred to therapy following a fall
To enhance the collaboration in Mrs. F's case, several strategies can be implemented to ensure the effective execution of her maintenance plan and exercises. Recognizing that CNAs might hesitate to approach the therapist or initiate exercises, fostering a culture of open communication is crucial. Actively encouraging CNAs to voice their concerns or seek clarification without fear of judgment can significantly impact the success of the maintenance plan.
Regular check-ins or huddles between therapists and CNAs could provide a structured platform for communication. Therapists can offer clarifications, address concerns, and provide ongoing education during these sessions. This collaborative approach ensures that CNAs feel supported and empowered to engage confidently in the exercise program.
Moreover, incorporating visual aids or simple reminders in Mrs. F's living space can be a non-intrusive way to keep both CNAs and Mrs. F informed about the prescribed exercises. Whether it's a whiteboard in the room or a designated section in the patient's chart, having a clear and accessible reference for the exercise plan reinforces consistency.
Additionally, creating a feedback loop where CNAs can share observations about Mrs. F's progress or any challenges they encounter further enhances collaboration. This two-way communication ensures that adjustments can be made to the maintenance plan if needed and reinforces the shared responsibility for Mrs. F's well-being.
- What worked for Mrs. F?
- Therapy sessions initially in a room or hall
- Training and education with staff
- In areas easily observable by staff
- Engaged CNAs in sessions for training on prescribed exercises
- The program was written with time constraints in mind.
- Built into ADLs
- The program was written with time constraints in mind.
- Resulted in:
- Completion of exercise program
- Communication between CNA and therapist
- Gains for Mrs. F
- Therapy sessions initially in a room or hall
In a more collaborative example, the therapist initially began their therapy sessions in the patient's room and in the hallways, inviting the CNAs to participate for short periods here and there between the care of their other patients so that they could be educated on the exercises that were prescribed as part of the patient's "home exercise" program.
Since the success of that program is dependent upon the CNAs helping the patient complete it, the goals and exercises were written with the CNA's time constraints in mind. For example, the patient aimed to do ten sit-to-stands. During their training sessions, the OT explained to the CNA that they didn't have to do that in the middle of their shift or take extra time, but rather wrap it into their daily care. So when transferring the patient from the bed to the toilet, have her do more than one sit to stand, or from the bed to the chair, have her do more than one sit to stand. After that interaction, the CNA felt more comfortable approaching the therapist when an issue arose, when the patient started to decline to do exercises or when the patient wanted to do more than what they were currently doing.
The CNA would also stop the therapist in the hallway to celebrate when the patient made progress and that CNA took pride in being a part of the bigger picture and getting the patient back to what she once was.
Summary
- Collaboration can have positive impacts on:
- Patient outcomes
- Facility and healthcare system
- However, it requires:
- Commitment
- Shared focus
- A harmonious and productive environment
- Sometimes we must be proactive in building
In conclusion, the substantial benefits of improved collaboration between therapy professionals, certified nursing assistants, and all nursing staff underscore the significance of fostering teamwork, effective communication, and a collective commitment to delivering optimal patient care. Implementing a range of collaboration strategies outlined can contribute to an enhanced working environment and, more crucially, to an elevated standard of care. The ultimate objective is to establish a harmonious and productive setting where therapists' expertise complements that of nursing counterparts, working collaboratively to empower patients to achieve their goals. This collaborative approach is pivotal in promoting positive patient outcomes and overall well-being.
Questions and Answers
How can I involve certified nursing assistants (CNAs) more effectively in therapy sessions and ensure they understand the goals and exercises prescribed?
To involve CNAs effectively, consider conducting joint training sessions where therapists demonstrate exercises and explain goals. Schedule these sessions to align with the CNAs' availability. Emphasize the importance of their role in supporting patients' therapy plans. Use real-life examples and practical scenarios relevant to their daily responsibilities. Encourage open communication, allowing CNAs to share their concerns or ask questions. Celebrate successes together, fostering a sense of accomplishment and teamwork.
References
Ahlgren B. (2010). Dissolving the patient Bermuda triangle. International Journal of Care Pathways, 14(4), 137-141. https:/doi.org:10.1258/jicp.2010.010025
American Speech-Language Hearing Association. (n.d.). SLPs in long-term care. Retrieved October 17, 2023 from https://www.asha.org/slp/healthcare/longtermcare/#:~:text=According to data collected by, work in skilled nursing facilities.
Bendowska, A. & Baum, E. (2023). The significance of cooperation in interdisciplinary health care teams as perceived by Polish medical students. International Journal of Environmental Research and Public Health, 20, 954. https://doi.org/10.3390/ijerph20020954
Boscart, V. M., Heckman, G. A., Huson, K., Brohman, L., Harkness, K. I., Hirdes, J., McKelvie, R. S., & Stolee, P. (2017). Implementation of an interprofessional communication and collaboration intervention to improve care capacity for heart failure management in long-term care. Journal of Interprofessional Care, 31(5), 583-592. https://doi.org/10.1080/13561820.2017.1340875
Centers for Disease Control and Prevention. (2022). Nursing home care. Retrieved October 11, 2023, from https://www.cdc.gov/nchs/fastats/nursing-home-care.htm
Colwill, J. M., Cultice, J. M., & Kruse, R. L. (2008). Will generalist physician supply meet demands of an increasing and aging population. Health Affairs, 27(3), w232-w241. https://doi.org/10.1377/hlthaff.27.3.w232
D'Amour, D., Ferrada-Videla, M., San Martin Rodriguez, L., & Beaulieu, M. D. (2005) The conceptual basis for interprofessional collaboration: Core concepts and theoretical frameworks. Journal of Interprofessional Care, 19(1), 116-131. https://doi.org/10.1080/13561820500082529
den Ouden, M., Zwakhalen, S. M. G., Meijers, J. M. M., Bleijlevens, M. H. C., & Hamrs, J. P. H. (2017). Feasibility of DAlly NURSE: A nursing intervention to change nursing staff behaviour towards encouraging residents’ daily activities and independence in the nursing home. Journal of Clinical Nursing, 28(5-6), 801–813. https://doi.org/10.1111/jocn.14677
de Souto Barreto, P., Morley, J. E., Chodzko-Zajko, W., H Pitkala, K., Weening-Djiksterhuis, E., Rodriguez-Mañas, L., Barbagallo, M., Rosendahl, E., Sinclair, A., Landi, F., Izquierdo, M., Vellas, B., Rolland, Y., & International Association of Gerontology and Geriatrics – Global Aging Research Network (IAGG-GARN) and the IAGG European Region Clinical Section (2016). Recommendations on physical activity and exercise for older adults living in long-term care facilities: A taskforce report. Journal of the American Medical Directors Association, 17(5), 381–392. https://doi.org/10.1016/j.jamda.2016.01.021
Ellingson, L. (2003). Interdisciplinary health care teamwork in the clinic backstage. Journal of Applied Communication Research, 31(2), 93-117. https://doi.org/10.1080/0090988032000064579
Gilbert, J. H., (2005). Interprofessional learning and higher education structural barriers. Journal of Interprofessional Care, 19, 87-106. https://doi.org/10.1080/13561820500067132
Grant, M., Elk, R., Ferrell, B., Morrison, R. S., & von Gunten, C. F. (2009). Current status of palliative care- Clinical implementation, education, and research. CA: A Cancer Journal for Clinicians, 59(5), 327-335. https://doi.org/10.3322/caac.20032.
Hudson, J. N., Lethbridge, A., Vella, S., Caputi, P. (2016). Decline in medical students’ attitudes to interprofessional learning and patient-centeredness. Medical Education, 50, 550-559. https://doi.org/10.1111/medu.12958
Kuk, N. O., Zijlstra, G. A. R., Bours, G. J. J. W., Hamers, J. P. H., Tan, F. E., S., & Kempen, G. I. J. M. (2017). Promoting functional activity among nursing home residents: A cross-sectional study on barriers experienced by nursing staff. Journal of Aging and Health, 30(4), 605-623. https://doi.org/10.1177/0898264316687407
Kuo, H., Lin, K., Lan, C., & Li, I. (2017). Activities of daily living trajectories among institutionalized older adults: A prospective study. Journal of Clinical Nursing, 26(23-24), 4756-4767. https://doi.org/10.1111/jocn.13828
Lam, K., Kwan, J. S. K., Kwan, C. W., & Chi, I. (2022). Factors associated with development of new joint contractures in long-term care residents. Journal of Post-Acute and Long-Term Care Medicine, 23, 92-97. https://doi.org/10.1016/j.jamda.2021.05.036
Morley, L. & Cashell, A. (2017). Collaboration in health care. Journal of Medical Imaging and Radiation Sciences, 48(2), 207-216. https://doi.org/10.1016/j.jmir.2017.02.071
Morris, Z. S., Wooding, S., & Grant, J. (2011). The answer is 17 years, what is the question: Understanding time lags in translational research. Journal of the Royal Society of Medicine, 104(12), 510-520. https://doi.org/10.1258/jrsm.2011.110180
Morrison, R. S., & Meier, D. E. (2004). Palliative care. The New England Journal of Medicine, 350(25), 2582-2590.
Motivation, communication, and negotiation. Lombardi D.N., & Slonim A.D. (Eds.). (2014). Manual of healthcare leadership: Essential strategies for physician and administrative leaders. McGraw Hill.
Novak, L. S., Jewell, V. D., Gerg, M., Thinnes, A. (2023). Education and perceptions of post-therapy maintenance programs in long-term care: A mixed methods exploratory study. The Open Journal of Occupational Therapy, 11(2), 1-11. https://doi.org/10.15453/2168-6408.2004
Schot, E., Tummers, L., & Noordegraaf, M. (2020). Working on working together. A systematic review on how healthcare professionals contribute to interprofessional collaboration. Journal of Interprofessional Care, 34(3), 332-342. https://doi.org/10.1080/13561820.2019.1636007
Singh, R., KÜÇÜKDEVECİ, A. A., Grabljevec, K., & Gray, A., (2018). The role of interdisciplinary teams in physical and rehabilitation medicine. Journal of Rehabilitation Medicine, 50(8), 673-678. https://doi.org/10.2340/16501977-2364
Sloane, P. D., Zimmerman S., & D’Souza, M. F. (2014). What will long-term care be like in 2040? NC Medical Journal, 75, 326-330. https://doi.org/10.18043/ncm.75.5.326
Spaulding, E. M., Marvel, F. A., Jacob, E., Rahman, A., Hansen, B. R., Hanyok, L. A., Martin, S. S., Han, H.-R. (2021). Interprofessional education and collaboration among healthcare students and professionals: A systematic review and call for action. Journal of Interprofessional Care, 35(4), 612-621. https://doi.org/10.1080/13561820.2019.1697214
Stulick, A. (2023, March 27). Skilled nursing vs. home health: Referral trends shift due to acuity, staffing shortages, regulation. Retrieved October 11, 2023, from https://skillednursingnews.com/2023/03/skilled-nursing-vs-home-health-referral-trends-shift-due-to-acuity-staffing-shortages-regulation/
U.S. Census Bureau. (2020). U.S. Census Bureau projections show a slower growing, older, more diverse nation a half century from now. Retrieved October 5, 2023, from https://www.census.gov/newsroom/releases/archives/population/cb12-243.html
U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. (2017). National and regional projections of supply and demand for geriatricians: 2013-2025. Rockville, Maryland. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/geriatrics-report-51817.pdf
Vaseghi, F., Yarmohammadian, M. H., & Raeisi, A. (2022). Interprofessional collaboration competencies in the health system: A systematic review. Iranian Journal of Nursing and Midwifery Research, 27, 496-504. https://doi.org/10.4103/ijnmr.ijnmr_476_21
Verbeek, H., Zwakhalen, S. M. G., Schols, J. M. G. A., Kempen, G. I. J. M., & Hamers, J. P. H. (2020). The living lab in ageing and long-term care: A sustainable model for translational research improving quality of life, quality of care, and quality of work. Journal of Nutrition, Health, & Aging, 24(1), 43-47. https://doi.org/10.1007/s12603-019-1288-5
Vespa, J., Medina, L., & Armstrong, D. (2020). Demographic turning points for the United States: Population projections for 2020 to 2060. Retrieved October 4, 2023, from https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf
Vestergaard, E., & Nørgaard, B. (2018). Interprofessional collaboration: An exploration of possible prerequisites for successful implementation. Journal of Interprofessional Care, 32(2), 185-195. https://doi.org/10.1080/13561820.2017.1363725
World Health Organization. (2020). Palliative care. Retrieved October 4, 2023, from https://www.who.int/news-room/fact-sheets/detail/palliative-care
Citation
Horvath, B.(2023). Skilled nursing facility interventions: Interdisciplinary collaboration between therapists and certified nursing assistants. OccupationalTherapy.com, Article 5665. Available at www.occupationaltherapy.com