Introduction and Outline
Hello, and thank you all for attending this presentation. Lymphedema is one of the most misunderstood diagnoses by the general public, patients, and healthcare professionals, including doctors. My hope is that this presentation will help you to assess and treat this disorder.
- COURSE OUTLINE:
- Lymphedema: What is it?
- Lymphatic System Anatomy
- Lymphatic System Pathophysiology
- Stages of Lymphedema
- Risk Factors
- Assessment
- Treatment
- Risk Reduction
- Summary and Questions
My course outline is to define lymphedema, review anatomy and pathophysiology, list the stages of lymphedema, identify risk factors, provide assessment/treatment ideas, review risk reduction, and at the end, answer any questions you may have. Let's get started.
Lymphedema: What Is It?
- Abnormal accumulation of protein-rich fluid in the tissues
- Increased swelling occurs, resulting in a blockage
- Causes increased inflammation and limb size due to lymph vessel overload of fluid
What is lymphedema? It is an abnormal accumulation of protein-rich fluids in the tissues because of disruption or damage. Increased swelling occurs, resulting in a blockage that causes increased inflammation and limb size due to the lymph vessels being overloaded with fluid.
- Chronic disease which can be Primary or Secondary
- Primary: Hereditary
- Secondary: after surgery, radiation, or other trauma; Filariasis – spread by infected mosquitoes
- Lymphedema may occur in the arm, leg, breast, neck, face, and genitals.
It is a chronic disease that people have to live with once they are diagnosed. It can be primary or secondary. Primary is hereditary, and it can come on at different stages, even as infants or toddlers. Or, it can appear later on in the teenage years.
Secondary lymphedema is what most of us think about. This happens after surgery, radiation, or other kinds of trauma. Most people associate it with breast cancer surgery, but it can happen with other types of surgeries.
There is another secondary type of lymphedema, which is called filariasis. This is spread by infected mosquitoes mainly in Africa, Asia, and some different Caribbean islands. It is a horrendous disease. With filariasis, the lymphedema is usually very severe.
I am sure many of you have seen people with arm or leg lymphedema, but it also can occur in the breasts, the neck, the face, and the genitals.
- Lymphedema Affects Millions
- Up to 10 million Americans
- Hundreds of millions worldwide
- More lymphedema in the U.S. than MS, MD, ALS, AIDS, and Parkinson’s combined
It affects millions of people, up to 10 million Americans, and hundreds of millions worldwide. I had no idea about these numbers until I started learning about lymphedema. There is more lymphedema in the United States than multiple sclerosis, muscular dystrophy, ALS, AIDS, and Parkinson's combined.
Lymphatic System Anatomy
- Lymphatic organs consist of lymph nodes, lymph vessels, thymus gland, spleen, and tonsils.
- Lymphatic vessels run parallel to the veins and are part of the circulatory system.
- Transports and filters excess fluid from the tissues, taking it back to the circulatory system.
This is the anatomy of the lymphatic system, as seen in Figure 1.
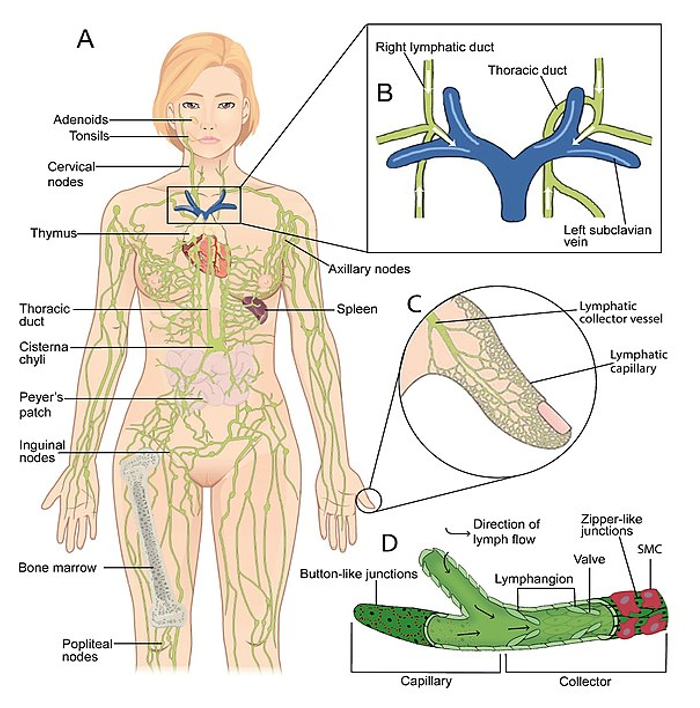
Figure 1. The lymphatic system (SGUL lymres, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons). Click here to enlarge the image.
The lymphatic organs consist of the lymph nodes, the lymph vessels, the thymus, the spleen, and the tonsils. The lymphatic vessels run parallel to the veins in the arms and the legs, which are part of the circulatory system. They transport and filter excess fluid from the tissues taking it back to the circulatory system.
- Lymphatic vessels:
- Lymph capillaries – larger than blood capillaries
- Walls made of flat endothelial cells that overlap, allowing opening and closing, so fluids are absorbed – anchoring filaments
- Increased interstitial fluid pulls on anchoring filament, opening the endothelial cell junction, allowing fluid in – it closes when the pressure has equalized.
- Lymph capillaries – larger than blood capillaries
The vessels are made up of various compartments, as seen in Figure 2.
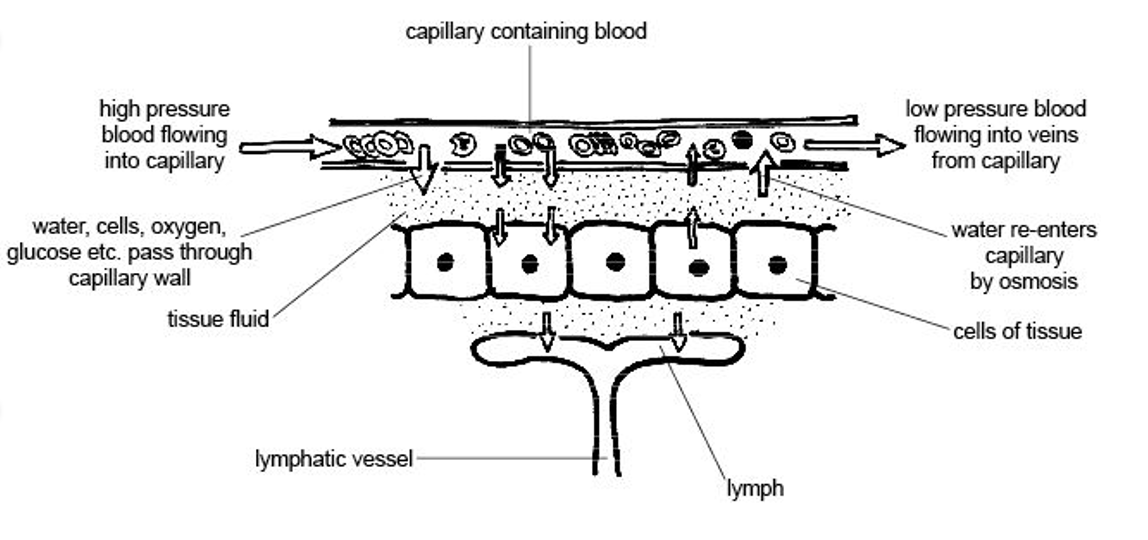
Figure 2. Lymph capillaries (The original uploader was Sunshineconnelly at English Wikibooks., CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons). Click here to enlarge the image.
The lymph capillaries are larger than the blood capillaries, which you will see in another picture. The walls are made of flat endothelial cells that overlap and allow opening and closing to absorb the fluids. These are called anchoring filaments. The increased interstitial fluid pulls on the anchoring filaments to open up a cell junction. This allows the fluid to come in. It is like opening the door, and then it closes when the pressure has equalized.
- Lymph Vessels
- Lymphatic capillaries
- Pre-collectors
- Lymph collectors
- Lymph nodes
- Lymphatic trunks
With this picture of the lymphatic system in Figure 3, you can see the lymphatic vessels up close.
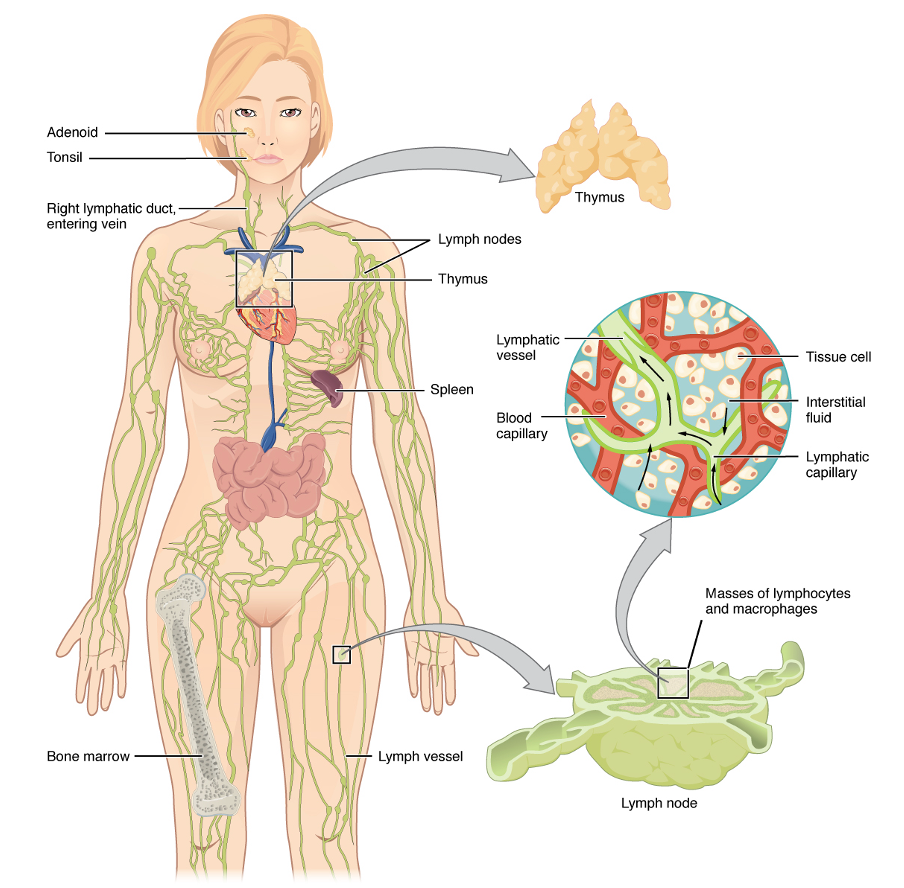
Figure 3. Lymphatic system overlayed on a female body with close-ups of the different components (SGUL lymres, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons). Click here to enlarge the image.
These are the blood capillaries and the lymph collector highlighted on the right side of the image. The lymph then goes to the lymph nodes and filter to the lymphatic trunks. Eventually, it will flow to the subclavian vein.
- Pre-collectors – located between the capillaries and collectors, carrying fluid and act as a bypass
- Collectors – run parallel on arms and legs, transport distal to proximal, directing the fluid flow
- Lymphatic Trunks
- Upper body: Jugular, subclavian, supraclavicular, parasternal
- Lower body: lumbar trunks and gastrointestinal trunk
The pre-collectors are located between the capillaries and the collectors. They carry the fluid and act as a bypass before you get to the collectors. The collectors run parallel on the arms and legs, which I showed in the other picture. This transports the lymph distal to proximal. The lymph and the lymph vessels only flow in one direction, so they are an open-ended system. The lymphatic trunks in the upper body include the jugular, subclavian, supraclavicular, and parasternal. In the lower body, it is the lumbar and gastrointestinal trunks.
- Ducts:
- Thoracic Duct
- Collects and transports 75% of the fluid (2-4 liters daily)
- Largest lymphatic vessel ~ 1-5 mm diameter and 40 cm long
- Right Lymphatic Duct
- Right venous angle – collects 25% transported daily fluid
- Thoracic Duct
Next, you have the ducts. The lymphatic duct is on the right, and the thoracic duct is on the left. The thoracic duct collects 75% of the fluid transported, and it gets filtered back out. This is about two to four liters of fluid daily. The thoracic duct is the largest lymphatic vessel in the body at 40 centimeters long. It spans from the cervical spine area, around the supraclavicular fossa, and down into the abdominal area. It perforates through the diaphragm on its way down to the abdominal area. The right lymphatic duct goes through the right venous angle, and it collects 25% of the daily fluid.
- Lymph Collecting Vessels
- In general, the superficial lymphatic collecting vessels in the skin travel with superficial veins.
- Deep lymphatic collecting vessels of the trunk and digestive viscera travel with the deep arteries.
There are superficial and deep lymphatic collecting vessels (Figure 4).

Figure 4. Overview of the lymph collecting vessels. Click here to enlarge the image.
The deep lymphatic vessels are the ones that go up the trunk and into the digestive viscera. They travel along with deep arteries. Today, we are talking about the superficial lymphatic collecting vessels in the skin. These travel with the superficial veins. You can see the superficial veins and lymph nodes highlighted in green in Figure 4.
- Lymphatic Fluid
- Contains:
- Proteins, water, RBC, WBC, lymphocytes, fats – intestinal, chyle waste products, and other foreign substances
The lymphatic fluid contains protein, but it also has small amounts of water, red blood cells, white blood cells, lymphocytes, fats, waste products, and foreign substances.
- Lymph Nodes:
- 600-700 in the body
- Largest number in abdomen and head and neck
- Function:
- filtering system to get rid of debris, produce WBC (lymphocytes), which assist in fighting infections, helping the immune system, and regulates the amount of protein in the lymph vessels
The lymphatic system/lymph nodes filter all these things out. There are 600-700 lymph nodes in the body. That is a huge number of lymph nodes that help with our immune system. The largest number are in the abdomen, head, and neck. Many people think that the majority of the lymph nodes are found in the axillary and inguinal areas, but that is not where the largest accumulation is. They function to filter the system to get rid of the debris that we talked about earlier, to produce lymphocytes, which help fight infections and regulate the amount of protein in the lymph vessels.
- Watersheds: areas on skin separating territories
- Sagittal (median)
- Horizontal (transverse)
- Inguinal
- Axillary
- Anastomoses
- Quadrants
Suami, H., and Shinaoka, A. (2019) The methodology of lymphatic anatomy studies in a cadaver model: an overview. Plast Aesthet Res, 6:33. http://dx.doi.org/10.20517/2347-9264.2019.46
Watersheds, quadrants, and anastomoses are areas that we utilize for manual lymphatic drainage. The watershed areas are areas on the skin that separate the different territories (Figure 5).
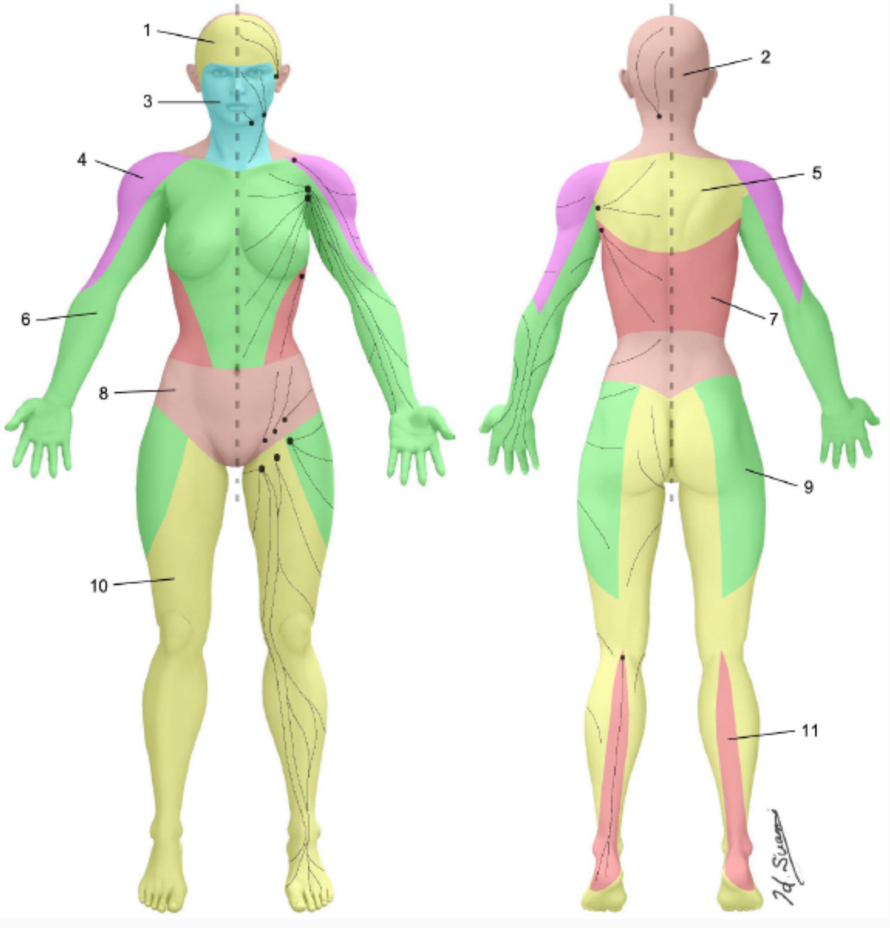
Figure 5. Watershed areas. Click here to enlarge the image.
The sagittal watershed is basically anterior and posterior, and the horizontal watershed is transverse. Then, you have inguinal and axillary watershed areas. These are because there are certain ways that we move the fluid when we do manual lymphatic drainage.
The quadrants are also important. The upper quadrant would be the whole right upper quadrant on that side, front and back, and the left upper quadrant. Then, you have the lower right quadrant and the lower left quadrant.
Anastomoses are areas from one side to the other or up and down. When you are draining fluid from someone with lymphedema, they typically have one area where the lymph nodes are blocked or damaged. Say it is on the right side. You would need to activate the left side, have the anastomosis from the right shoulder axillary area, and move it over to the left side. You do want to push more fluid into the right side. One of the anastomoses would be axilla to axilla. Another would be from the inguinal to the inguinal, and these are front and back. Another would be from the axilla down to the inguinal. Thus, these are different pathways that we can use when we are performing manual lymphatic drainage.
Lymphatic System Pathophysiology
- “Lymphatics absorb, transport, and recycle proteins and other waste products from the interstitial fluid before re-entering bloodstream.”
- Body is made up of 60% water, mostly inside or around the cells. Veins and lymphatics work together to remove the extra fluid.
- Lymph capillaries located just beneath the skin
- Collect fluid and return it to the circulatory system and heart
The pathophysiology is that the lymphatics absorb, transport, and recycle proteins and other waste products from the interstitial fluid before re-entering the bloodstream. Our body is made up of 60% of water, mostly inside and around the cells. The veins and the lymphatics work together to remove the extra fluid. The veins carry about 80 to 90% of that fluid, and the lymphatics carry the other 10 to 20%. The lymph capillaries, as I mentioned before, are located beneath the skin. This is important to know as the lymphatic system is very superficial. When we do perform the lymphatic drainage, you do not need to apply very much pressure. It is a very gentle type of massage. Figure 6 is another picture showing this.
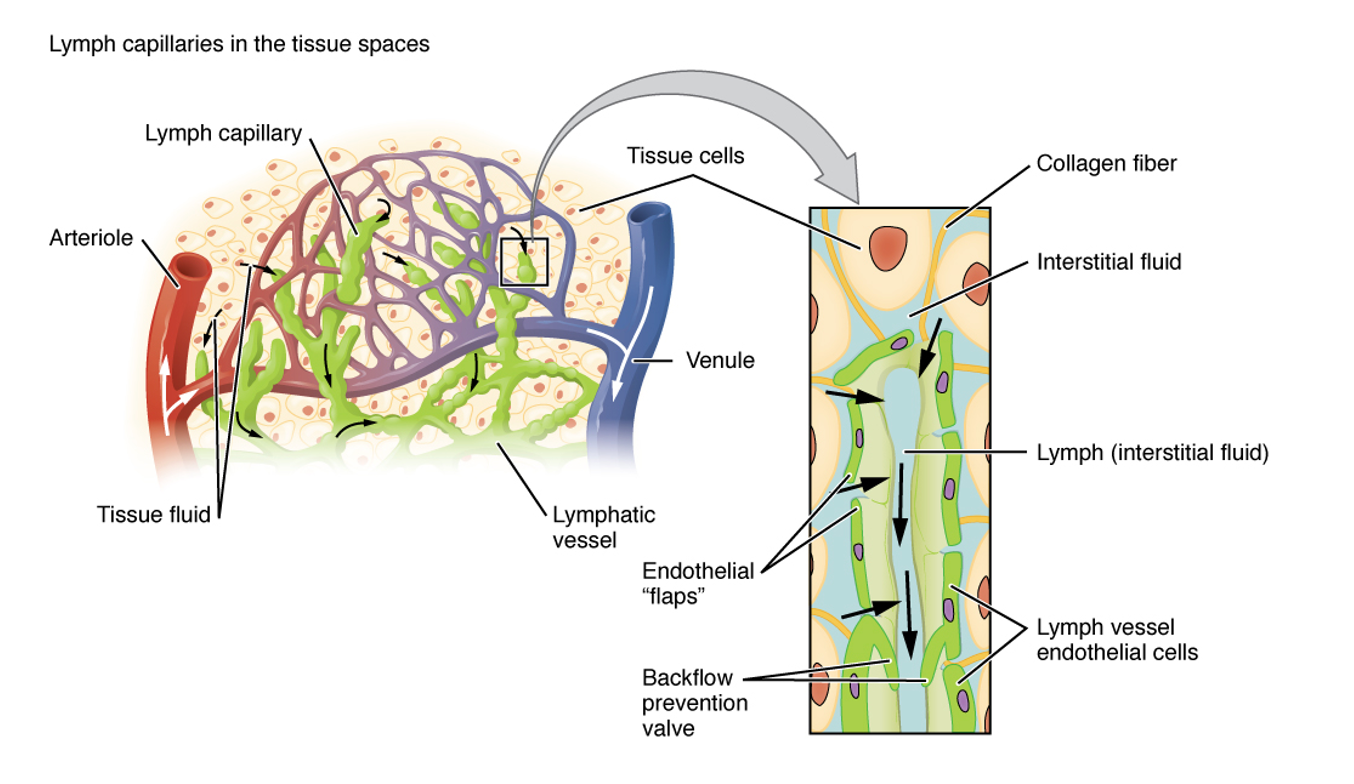
Figure 6. Manual lymphatic drainage overview with a close-up of the vessels. Click here to enlarge the image.
The interstitial fluid is blue, and the lymphatics are green. You can see the veins and the arteries in this image and how close these systems are to each other.
- Constant exchange of fluids in the body.
- Starling’s Equilibrium: Ernest Henry Starling (1866-1927)
- “The ultrafiltration force and reabsorption force are equivalent since all fluids that have entered the interstitium return back to the blood capillary, creating a perfect balance of forces.”
I would be remiss if I did not talk about Ernest Henry Starling. His description of equilibrium was, "The ultrafiltration force and reabsorption force are equivalent since all fluids that have entered the interstitium return back to the blood capillary, creating a perfect balance of forces."
- The lymphatic system works by interstitial pressure (IP)
- As fluid increases, the IP increases in lymph capillaries
- With damaged lymphatics, fluid builds up in interstitial space
- When water is removed from interstitial fluid leaving proteins, more water is attracted and pulled in from the blood capillaries
- decreased return of water through the veins
- decreased reabsorption
- Increased tissue swelling
Our lymphatic system works by interstitial pressure. As the fluid increases, the interstitial pressure increases in the lymph capillaries. If you have damaged lymphatics, the fluid builds up in that space. When water is removed from the interstitial fluid, leaving proteins in that space, more water is attracted and pulled in from the blood capillaries. Proteins act as a magnet toward the water. If water has been transported through the venous system and the proteins are left in there and not taken up into the lymphatics, they just sit there and keep attracting more water. This, in turn, decreases the return of water through the veins, decreases reabsorption, and increases tissue swelling.
- Lymphatics are a one-way open-ended system.
- Lymph capillaries have overlapping endothelial cell flaps
- As fluid accumulates in the tissue, it pushes the lymph collector flaps inward, allowing fluid to flow in
- Fluid enters the lymph capillary balancing the interstitial pressure
- As the pressure inside increases, the flaps press outward, closing the gaps and preventing backflow.
The lymphatics are a one-way open-ended system, while the circulatory system is a closed system. It goes back to the heart and returns. The lymph capillaries have overlapping endothelial cell flaps, which I touched on in the anatomy portion. As the fluid accumulates in the tissue, it pushes the lymph collector flaps inward, allowing the fluid to flow in. The fluid enters the lymph capillary balancing the interstitial pressure. As the pressure increases, the flaps press outward, closing the gaps and preventing the backflow.
- The segments of the lymph collectors are called lymphangions – they perform autonomic contractions called lymphangio activity
- frequency depends upon lymph volume and autonomous regulation of the sympathetic nervous system
- this allows transport of the lymph fluids to the lymph nodes and larger vessels, draining via the subclavian veins
The collector section of the lymph vessels is called a lymphangion. They perform autonomic contractions called lymphangio activity. The frequency of it depends upon the lymph volume and the autonomous regulation of the sympathetic nervous system. There are six to 10 contractions per minute at rest, but if we increase our exercise and movement, it increases to 10 times that amount. This is good in a normally balanced system as it allows transport of the lymph fluids to the lymph nodes and into the larger vessels draining via the subclavian veins. If it is damaged, the contractions are not happening because there is a blockage somewhere. This is why manual lymphatic drainage is important to move that fluid along manually.
- Physical trauma of any type may injure the lymph system altering the healthy balance.
- Insufficiency of the lymph vessels to move the fluids and wastes
- Protein-rich fluid accumulates, causing blockage and swelling
- Changes in the interstitial cells with increased proteins making the tissues more susceptible to infections and fibrosis
Physical trauma of any type may injure the lymph system altering the healthy balance. Insufficiency of the lymph vessels impacts the moving of fluids and waste. Protein-rich fluid accumulation causes blockage and swelling. And, changes in the interstitial cells with increased proteins make the tissues more susceptible to infections and fibrosis.
- Common causes-Disruption of the Lymphatic System may occur from:
- Cancer treatments
- Infection
- Trauma
- Scar Tissue from Radiation
- Venous Insufficiency
One common cause of lymphedema and disruption of the lymphatic system is cancer treatments. This is probably what most people think about when they hear lymphedema of an arm. This is because lymph nodes may have to be removed, or the lymphatics are damaged somehow. An infection can also cause lymphedema. One of the examples that I was talking about in the beginning was filariasis. This is an infection from bacteria. Trauma can definitely impact the lymphatic system because it lies so close to the surface of the skin. Scar tissue from radiation is another common cause. Sometimes people have surgery and then have radiation therapy and are fine until a few months after the radiation. This is because of all the damage that was done to the tissue. The tissue becomes fibrotic, and the lymphatics are damaged. You may also see lymphedema with venous insufficiency.
Stages of Lymphedema
- Stage 0: Latent
- Swelling not apparent
- Impairment of lymph transport capacity
- May report feeling of heaviness and tightness
- Stage I: Reversible
- Early accumulation of protein-rich fluid
- Pitting edema
- Elevation decreases swelling (no fibrosis)
- Stage II: Spontaneously irreversible
- Pitting edema increased
- Edema needs more than elevation to decrease
- Late-stage, onset of fibrosis
- Stage III: Lymphostatic Elephantiasis
- No pitting – fibrosis and sclerosis
- Skin changes – papillomas, hyperkeratosis
There are stages 0 through III of lymphedema. When someone gets diagnosed, the doctor usually diagnoses them with a particular stage. Stage 0 is called the latent stage. There is no swelling. People usually come in and say they feel heaviness or tightness in their arm, leg, or whatever body part it is. Sometimes, it is in the breast area. There is no objective, identifiable edema that can be seen, but there is some impairment of the lymphatic transport capacity. However, it is not something that can be seen or picked up right away.
Stage I is called reversible. It is usually the pitting edema you see in an extremity that will go down when you elevate the limb. No fibrosis has formed yet, but there is an early accumulation of protein-rich fluid.
Stage II is called spontaneously irreversible. At this point, you cannot totally reverse the lymphedema, but you can definitely control it. The pitting edema is increased, and the edema needs more than elevation to decrease it. This is when you need to incorporate complete decongestive treatments.
Stage III or late stage is the onset of fibrosis and is called lymphostatic elephantiasis. There is no pitting, and the tissue is fibrotic and sclerotic. You see skin changes like papillomas (blisters) and hyperkeratosis. I have never seen papillomas in the arm. In the leg, these are bubbly areas of water as the fluid has nowhere to go. Hyperkeratosis is when you see dark, leathery type skin.
The first three slides are all my patients, the last two are not (Figure 7).

Figure 7. Examples of the different stages of lymphedema. Click here to enlarge the image.
In the first image on the left, this is stage 1. There is some pitting edema. With a compression sleeve, glove, self-care, and manual lymph drainage, this went down, and eventually, it went away. What I am treating her for right now is scar tissue around her breast area.
The middle two pictures are stage 2. One is less edematous, so more early stage 2, and the other is mid to later stage 2 (white t-shirt). The woman in the top picture (bed sheet) did fantastic with compression wrapping, a compression sleeve, and manual lymph drainage. Now and then, her arm lymphedema flares up, and then she comes back for treatment. She is very good at performing her own self manual treatments and her own self-care. In the lower picture, this man in the white t-shirt had a mastectomy of his right breast with resulting lymphedema in the right arm. It was treated, and he got somewhat better, but then it blew up again. He has an excellent program now, so hopefully, that will remain at bay.
These last two pictures are of what you would call stage 3 with the large upper and lower extremity. It is very debilitating and depressing for the patients.
Lymphedema Risk Factors
- Risk Factors:
- Increased # lymph nodes removed
- Radiation therapy
- Postoperative seroma formation Infection
- BMI greater than or equal to 30
- Over-exercising too early post-operatively
It is important to understand what the risk factors may be for getting lymphedema. The first one is the number of lymph nodes removed. After an axillary dissection because of breast cancer, they may have to remove many lymph nodes. One sentinel node is considered zero to four lymph nodes. The percentage would be about a 6% risk of getting lymphedema with this number of node removal. If you have more, then you have a 15 to 25% chance of getting lymphedema.
Other risk factors include radiation therapy, postoperative seroma formation infection (from the fluid that builds up around a drain), a BMI equal to or greater than 30, and over-exercising too early postoperatively.
Lymphedema Assessment
- Medical and Patient History
- Pain
- Sensation
- ROM and Strength
This first part of the assessment would be taking a medical history, as you typically would do. Typically, these clients have a significant medical history and complications as well. Some patients are very good at reporting their history, and others are not. If you have access to their chart, that is good to review before they come in.
Pain can be assessed using any pain scale, like a zero to 10 rating. Generally, with lymphedema, people do not complain of pain. It is more of a heaviness, tightness, and discomfort.
I am fortunate with my assessments that I have an hour, but I know not everyone gets that. Even within an hour, sometimes there is no time to do a sensation evaluation. If I do not check it on the first visit, I do it the next time. Breast cancer patients can be on a drug like Tamoxifen, and the side effects are chemo-induced peripheral neuropathy.
You would also evaluate range of motion and strength. I look at their functional range of motion on the first day. With breast cancer, you see many frozen shoulders because they often stay in a protective position. It often depends on how long it takes for the person to get into therapy.
- Edema measurements:
- Circumferential - tape measure every 4 cm
- Perometer - optoelectric
- Sozo – bioelectrical impedance
- L-Dex – lymphedema index used to measure fluid
The major difference between a normal OT assessment and one for lymphedema is the focus on edema. This is really the key to assessing lymphedema. The basic one is a circumferential measurement. This is the gold standard for the arm and legs. You would measure every four centimeters up the leg or the arm, depending on where they have the lymphedema. If the lymphedema is in the breasts, head, or neck, there are other ways to measure that. I use a tape measure. I have also had the opportunity to use the Sozo. I have not used the Perometer. The Perometer is another form of assessment. It is optoelectric and measures the fluid. The Sozo is bio-impedance spectroscopy (BIS) technology. This monitors the body composition and hydration of a person. The L-Dex (lymphedema index) is the score used to measure the fluid. This way, you can have consistent objective measurements.
- Perometer
- Harmless light beams measure the limb
- Calculates volume measurements in mls
This is a picture of the Perometer (Figure 8).

Figure 8. A perimeter by Pero-System.
You would place the arm through the rectangle, and then the machine would calculate the volume measurements in milliliters. This is a higher-tech assessment, but a tape measure works perfectly fine. This is the Sozo via a company called ImpediMed (Figure 9).

Figure 9. Sozo spectroscopy. Click here to enlarge the image.
I am mentioning this because I do not think any other company out there does this. It can pick up lymphedema even when a client is in stage 0. This is when they just feel heaviness and tightness, and there is nothing measurable. This machine picks up the extra-cellular fluid and compares the at-risk limb to the non-involved limb. You wet the foot and hand metal plates and then have the clients step (without shoes and socks) on the metal pieces. The clients also put their hands on the hand plates (See the middle picture). The iPad has a program in it that is used to record the patient's information like their height and weight. The client stands on this device for 30 seconds, and it calculates out the L-Dex score. It compares the right and left sides.
- Diagnostic Testing:
- MRI
- CT scan
- Doppler Ultrasound
- Lymphoscintigraphy
- Radionuclide imaging of lymph system using a dye which shows blockages
Various diagnostic testing can be performed to assess for lymphedema, like an MRI, CAT scan, or a Doppler ultrasound. An ultrasound is used more often if the doctor thinks there may be a DVT or chronic venous insufficiency. The lymphoscintigraphy is where they use dye to show blockages. I went to a conference in Boston where I took these pictures (Figure 10).

Figure 10. Pictures of a lymphoscintigraphy where dye is injected into a cavader arm. Click here to enlarge the image.
We were able to see cadaver arms that were injected with the dye to show the blockages of the lymphatic system on radio nuclei imaging. This is probably the best of all the techniques to find where the blockage in the system is.
Lymphedema Treatment
- Complete Decongestive Therapy or CDT includes:
- Manual Lymphatic Drainage (MLD)
- Compression Wrapping and Garments
- Remedial Exercises
- Skin and Nail care
- Self Care Management Education
Manual Lymphatic Drainage (MLD)
The gold standard is complete decongestant therapy or a CDT as we refer to it. It includes manual lymph drainage, compression wrapping and garments, remedial exercises, skin and nail care, and self-care management education. I want first to start talking about manual lymphatic drainage (MLD). Manual lymphatic drainage is a drainage system where we are helping to move the fluid from an area where it is congested or blocked to an area where it is not. As I tell all my patients, we are trying to activate the lymph node areas that are healthy and good and appropriately move the fluid. You can move it away from the affected limb. I have the patient lay supine. You would start with opening up or activating the supraclavicular fossa above your clavicle on each side. Then, I work with the abdominal area. There is a particular order of what you do with your motions that you can see in an upcoming video. Along with the treatment in the abdomen, I have my patients do diaphragmatic breathing as this can help move the fluids down. If you remember, the thoracic duct originates in the area of the supraclavicular fossa and travels down through the diaphragm to the abdomen. It helps with the drainage of the fluid, and it is a relaxing technique. Clients can close their eyes and do their breathing while you are performing the hand techniques for the massage.
For example, for a client with lymphedema in their left upper extremity, I would go over to the left side first and activate the lymph nodes in the axillary area and then come over to the right inguinal area because I am prepping the area to move the fluid from the left area. In the affected arm, you would activate areas on the forearm on both sides, the antecubital fossa, the wrist, the hand, and the fingers, and then move the fluid back up. You are rerouting the fluid. How I have heard it explained is that it is like a traffic jam. If you are stuck on the highway, you have to find a new exit route.
The gold standard for treatment is five days a week for two to four weeks, which I know is hard for many people to do. However, that is the gold standard to maximize the treatment and get the edema down in the limb. Obviously, if people cannot do that, we try to do what is best for both the patient and their medical condition. Use your professional judgment.
Compression Wrapping and Garments
Compression wrapping and garments can be seen in Figure 11. These are just some examples.

Figure 11. Client with right arm in a compression sleeve and another picture showing compression wrapping of a left arm.
You can also do compression wrapping on the legs. Additionally, there are compression garments for the head and neck. For an arm, you start with the fingers and wrap one layer of the ace wrap (beige material) over the hand and wrist. Then, you would start your next one from the wrist up over the elbow. The next bandage would go from mid-forearm up over the shoulder. Finally, you would put a last one over the whole thing. With this, you are creating a compression gradient. The client will have low resting pressure in the wrapping and high working pressure, which means that when they are moving their arm, they will have a better flow of the fluid.
As far as the fit of the compression sleeve (in the left picture), some facilities will measure for compression sleeves themselves, while others will refer to specialists for that. In my facility, we refer people out because there are two wonderful places nearby. They have been doing it for years. We do give our recommendations of what we think they need. The garment has to be a certain percentage of pressure. Many people end up with 20 to 30 millimeters of mercury pressure. It can also be as high as 30 to 40 or as low as 15 to 20. The most common is 20 to 30, but it all depends on the person's limb, lymphedema, and the stage that they are in.
The compression sleeve in Figure 12 is a pretty fancy purple and white flower design. They used to only make a tan color, but now they have various colors and designs. They even have ones that look like a tattoo sleeve. You need to make sure that they are getting the right amount of pressure for their lymphedema.
Remedial Exercises
We start with the active assistive exercises. You want to make sure they have good endurance for the activity because people who have had cancer, for example, may not. Even if the lymphedema is not from cancer treatments and is from something like chronic venous insufficiency, these people can still have very low endurance. You have to grade the activity depending on what they can tolerate, and you do not want to overload the lymphatic system.
Skin and Nail Care
You need to do a lot of education in this area to ensure that people do not end up with infections. If they get an infection, it can blow up their lymphedema because of the protein-rich fluid in the interstitial fluid area. This can be a breeding ground for bacteria. All my patients make sure they put on some kind of lotion at least once a day, if not twice because the skin tends to be dehydrated with lymphedema.
Self-Care Management Education
Self-care management education includes teaching them how to perform their self manual drainage. This is not quite as involved as what we do, but I give them a handout. It has the general motions they should go through at least once a day, if not twice. I also educate them on how to wrap their own compression wrapping and the care of their compression garments. The garments need to be replaced every six months because they stretch out.
Other Treatments
- Other Treatments may include:
- Scar and fibrotic tissue management
- Lymphatouch
- Kinesiotape
- Progressive resistive strengthening/Yoga
Another treatment is working on their scar and fibrotic tissue. Figure 12 is a bag with foam cubes that I made.

Figure 12. Net bag with soft foam cubes.
You just cut little pieces of foam and put them in a net. Then, you put it over the scar or fibrotic tissue that is really hard and dense. I also use this for lacerations. Once the tissue heals, if the client still has some swelling and some hard tissue, I will put this over the tissue and put a sleeve over it. Clients feel that this is comfortable, and it helps soften up the tissue. Another thing you can use is a piece of silicone which comes in little pads. You can just cut a piece and lay it over the fibrotic tissue or the scar tissue. I also have people wear it at night time.
Other treatments are the Lymphatouch and Kinesiotape. Progressive resistive strengthening is a little different than the remedial exercises as you are adding strengthening exercises. I also find a lot of people benefit from yoga. There are many studies about using yoga after cancer and lymphedema. It provides good breathing and stretching.
Figure 13 is a picture of a Kinesiotape technique.

Figure 13. Black Kinesiotape from fingers up to the upper forearm.
I love this method called the fan. The anchor would be up on the upper forearm. You want to pull the fluid towards the anchor. You would lay down the anchor up in this area, and then you would cut the fan pieces to go on the palmar side over the intrinsic. This would draw the fluid up through that area, through the elbow where the lymph nodes are, and continue up the arm. Sometimes, I will continue it all the way up to the shoulder. This helps to remove fluid out of the hand. I use that same technique for a lot of my wrist fractures who have edema in their hands.
Figure 14 shows the Lymphatouch.

Figure 14. The Lymphatouch.
This is a suction machine. It has different size cups that go on it. On the screen, you can choose the amount of intensity of the suction, and you can also choose a pulsating or a continuous option. This helps with manual lymph drainage. I use it more to suction continuously to suction a scar tissue area or fibrotic area. It works really well, and the patients really like it. You start at a lower intensity where you can hardly feel it and gradually build it up. It also helps when people have hypersensitivity.
Video: Manual Lymphatic Drainage (MLD)
- Modified for post-operative edema
- Proximal to distal
- Light superficial pressure
In this video, I perform a very shortened version of manual lymphatic drainage. This is what I would do if she was a regular post-operative patient, not a lymphedema patient with edema. This is to give you an idea of what you could do. You are not supposed to be performing manual lymphatic drainage unless you have had 135 training hours and have attended one of their conferences. The courses that are offered are usually nine days long with prior intensive work on the computer. It is very intensive training for the certification. This is not to say that you cannot use the portions of it as long as you know what you are doing.
In general, you are going to be moving proximally to distally with light superficial pressure. I am going to play the video now.

This is a short video on how you would do Manual Lymphatic Drainage for post-operative edema. So since this is an introductory course and you have to be a certified lymphedema therapist to work with lymphedema, I want to show a short video and just be able to show you a couple of things that you would do if you want to move swelling, say from a risk fracture or any other kind of injury of the hand or the distal arm. And thank you, Pat, for being my here, my patient. So I would start up in the axillary area where the lymph nodes are, and you would do a circular or a stationary circle, and you're going towards the axilla, so your motion is like a C. And then you go into the axilla. I'm not going to do it as long as I would typically do it, 'cause I just want to show the general area that you would cover. And then, you're going to move the fluid from medial to lateral towards the deltoid area. So you would typically do about five to seven repetitions in each spot, and then you would do what's kind of pump motion. So you're pushing that fluid up, and you always want to go proximal to distal, but you're doing the distal part of the proximal segment, and you're moving that up, so then you'll do this part and move it up. Okay. And then you would go to the antecubital fossa where there are lymph nodes in that area as well, and you would work on that. And then you would go to the lateral epicondyle. So basically, what you want to do is activate all the areas where there are lymph nodes or larger area lymph nodes so that then you can drain the fluid in that direction. And then we'll go to the medial epicondyle area and do the same thing. And then you're going to do the forearm from the risk to the elbow, and you're going to do a little scoop, so you're moving the fluid towards the elbow. And then you're going to do the other side, and I'm just going to do some stationary circles that way. Then you're going to go to the wrist, and you want to clear the wrist, and you want to go towards the area of the ulna. Both sides, and then you're going to do the dorsum of the hand, and then you would do each individual finger, you'd be doing some circular motions for each of the fingers. Then you would turn the hand over, and you want to drain the fluid from the middle of the palm towards your right hand, going towards the ulna side, and your left hand going towards the medial side. And then from there, you're really just going to move the fluid back up, whether you want to do it in your stationary circles or you want to do like a little effleurage and just move everything back up. But that's the way you would generally do the manual drainage for post-op edema.
- Risk Reduction
- Skincare :
- Avoid trauma and injury to reduce infection risk
- Careful nail care and shaving, apply daily moisturizer to skin
- Protect skin with sunscreen and insect repellent
- Wear gloves with activities like gardening, tool use, detergent use
- If scratches/ punctures occur, wash with soap and water, apply antibiotics, and observe for signs of infection
- **Avoid injections/blood draws in affected limb**
It is important to understand the risk factors we went over and then provide information to your patients about risk reduction. Risk reduction involves many different areas. We always give a large handout, so all the patients have all this information. They need to avoid trauma and injury to reduce infection, be careful with nail care, and avoid injections and blood draws.
- Avoid Limb Constriction
- Blood Pressure; avoid at-risk or edematous extremity
- Wear non-constrictive clothing and jewelry
- Avoid carrying heavy bags on the at-risk or edematous extremity
- Compression Garments
- Well-fitting with no tight or “tourniquet-like” areas
- Provide support of the limb with a compression garment for strenuous activity, except if open wounds or poor circulation in the limb
They also should avoid limb constriction like with a blood pressure cuff or constrictive jewelry or clothing. Compression garments should be well-fitting.
- Activity / Lifestyle
- Gradual progressive exercises modifying duration and intensity
- Take frequent rest periods during activity to allow for recovery
- Monitor extremity during and after activity for any changes
- Maintain optimal weight as obesity is a risk factor
All activities should be progressive so as not to overwhelm the system. It is also important to take frequent rest periods.
- Extremes of Temperature
- Use common sense when using heat therapy – ie. Sauna, hot tub, or hot packs – never use longer than 15 minutes.
- Avoid exposure to extreme cold, which can be associated with rebound swelling or chafing of skin
- ** Contact MD immediately if any increased symptoms of rash, itching, redness, pain, increased temperature and swelling, and fever **
They should avoid extreme temperatures. They need to use their common sense. If something is bothering them, they should stop. Ensure that the patients are aware of all of these things and that they contact their doctor immediately if they have any increased symptoms of rash, itching, redness, pain, increased temperature, swelling, and fever.
Lymphedema Contraindications
- Untreated metastatic cancer, malignant disease
- Acute inflammation with infection – i.e., cellulitis
- Untreated thrombosis (DVT)
- Acute allergic reaction
- Cardiac insufficiency (CHF), Cardiac decompensation (Cardiac Edema)
The five most important contraindications for MLD are untreated metastatic cancer, acute inflammation with an infection like cellulitis, an untreated DVT, acute allergic reaction, and cardiac insufficiency. You do not want to increase the fluid load back to the heart if they already have a cardiac issue.
Goals of CDT
- GOALS of CDT:
- Early Intervention – identify “at-risk” persons early on when it’s a fluid imbalance, not fibrosis
- Risk Reduction – evidence that maintaining a healthy weight and lifestyle is useful
- Volume reduction - measurable and visual feedback
- Infection Management – educate on skincare to protect against bacteria
- Fibrotic Management – fibrosis inflames the skin, increasing temperature a few degrees
- Quality of Life- breast cancer patients
The goals of CDT are first early intervention to try to identify any people that are at risk. You want to catch things early on and treat them right away. Other goals include risk reduction, volume reduction, infection management, fibrotic management, and quality of life. Per numerous studies, many breast cancer survivors say that after the fear of getting cancer again, their second fear is to get lymphedema.
For quality of life, it is important to treat lymphedema and give the patients the knowledge and information they need because it is a lifelong disease that they have to learn to manage. I want to thank everyone for your time and attention to this presentation. Hopefully, more therapists will become CLTs to treat this debilitating condition.
Questions and Answers
Can you summarize the functions of the lymphatic system?
The function of the lymphatic system is to collect fluid, transport it, and get rid of the waste and debris through the lymph nodes. It also supports the immune system as the lymphocytes are produced in the lymphatic system.
Can any change be expected 30 years post-mastectomy, either positive or negative?
The tissue can become a little more dense or fibrotic if not taken care of and managed. You will also have typical aging processes occur as well.
Why is light touch the best to help transport fluids out of the area?
This is because the lymphatics live right underneath the skin. You do not want to put too much pressure because you can further damage the lymphatic collectors and the capillaries.
References
Available in the handout.
Citation
Grenus, L. (2021). Upper extremity reconstructive surgery for tetraplegia: The role of OT. OccupationalTherapy.com, Article 5452. Available at www.OccupationalTherapy.com
