Michelle: Thank you very much for joining us today. Regardless of age or diagnosis of our clients, there is always a degree of risk of developing pressure injuries. Pressure injuries have a lot of very negative medical consequences that can also lead to quite a bit of pain for our clients. It is far easier to prevent the development of pressure injury than it is to treat it afterward and so this becomes a very critical part of our wheelchair-seating strategy.
We will be covering pressure injuries, the current definitions, and the etiology, the causes of these. As this has changed over the years, we are going to look at some of our most recent definitions and staging explanations. We are going to explore strategies to prevent pressure injury development within wheelchair seating by matching client parameters to product options. Then, we will wrap up with a case study.
Pressure Injury Definition
You have probably heard many different terms being thrown around: pressure wounds, bedsores, pressure ulcers, pressure sores. The current definition via the National Pressure Ulcer Advisory Panel is pressure injury, even though this advisory panel has the word ulcer within its title. Here is their definition:
“A pressure injury is localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue.”
Pressure Injury Statistics
Some of these statistics can be a little dated as it takes a while to get more recent information. Available statistics show that about 450,000 people or more have pressure-related wounds. They are reported annually among wheelchair users and hospitalized patients. These numbers are a little misleading as they are reported by hospitals and other institutions, and wheelchair-related pressure injuries and bed-related pressure injuries are often lumped together. Some of those people may have only a pressure injury related to bed or wheelchair. There could also be a combination of contributing factors. It costs nearly $40,000 on average to treat a pressure-related wound, and that is when hospitalization is required. Hospitalization is not always required, but it can be.
Other Definitions
There are other definitions that I wanted to list because these are quite important in our discussion of pressure injuries.
- Ischemia – Impaired blood supply to the tissue
- Tissue deformation – a change in the shape of tissue from one condition to another
- Hypoxic - a condition where tissue cells are deprived of an adequate supply of oxygen
- Tissue necrosis – premature death of tissue cells
- Normoxic – a condition where tissue cells have an adequate oxygen supply for life-sustaining function
- Apoptotic cell death- normal process programmed cell death in tissue
- Perfusion/reperfusion – the flow of blood through the circulatory system (perfusion) and the restarting of flow after a period of no flow (reperfusion)
These are terms that can come up when you are working with a client who already has an injury or needs wound care. Ischemia is impaired blood supply to the tissue. When there is not enough blood supply, there can be tissue death. Tissue deformation is quite important, particularly in more recent pressure-related research. Tissue deformation is a change in the shape of the tissue from one condition to another, and this is often in response to shear forces. This is a change or distortion to the tissues during that shear. Hypoxic is where tissue cells are deprived of an adequate supply of oxygen and can often be seen in combination with ischemia. You might see these terms used interchangeably at times. Tissue necrosis is the premature death of any tissue cell. Normoxic is a condition where tissue cells have enough oxygen to sustain their functioning. Apoptotic is a normal process where cells die. Our cells are constantly dying and then regenerating. There is constant remodeling going on in our body. It is natural for some of our cells to die every day. Necrosis is when there is the premature death of tissue cells. Finally, we have perfusion and reperfusion where we have the flow of blood through our tissue. When we do not have compression of the cells, the blood can perfuse those tissues. This delivers crucial oxygen and other nutrients and takes away any toxic or dead material. Reperfusion is the restarting of flow after a period where that flow is limited. Let's say there is compression of the tissue, and then that is relieved like with a weight shift. That is an example of reperfusion.
Pressure Injury Causes
What causes a pressure injury to develop?
Pathways to Tissue Damage
There are two main pathways to tissue damage. There has been much research about pressure over the years, and more recent research in the last five years, that has specifically defined these two pathways.
Ischemic. The ischemic pathway is the most known to us. The tissue is compressed and that leads to a deformation of the cells and a lack of adequate blood supply. This compression happens between a bony prominence like the ischial tuberosity of the pelvis and a support surface like a cushion. It can lead to damage to the cells. Research has shown us that this damage can take up to six hours to occur. This varies tremendously between clients.
Deformation. There is also a second pathway called the deformation pathway. This is where the cells are actually deformed, usually by a combination of pressure and shear. Shear forces are when two surfaces move in opposite directions, and this leads to distortion of tissue. For example, if a client is sitting in their seating system and they are sliding into a posterior pelvic tilt or reclining, this can lead to this deformation of tissue. A combination of compression and shear force can lead to cell damage in minutes to hours. This is very critical because we have always known that there are some clients that for whatever reason tend to be very very prone to pressure injuries, while others do not. Some clients have sat on a very poor surface for maybe 20 years and have never had a pressure injury. This may be one reason along with other contributing factors.
Contributing Factors
In addition to the aforementioned pathways, we know that the following factors can increase a person's risk.
- Heat
- Moisture
- Poor pressure distribution
- Lack of sensation
- Incontinence
- Poor hygiene
- Poor nutrition
- Prior pressure injuries
- Immobility
- Friction
- Shear
- Inactivity
- Decreased mental status
Heat and moisture are big culprits, and they are hard to address in a seating system. Depending on the seating system, there can be quite a bit of heat that builds up. Moisture can be a result of incontinence or perspiration. A combination of heat and moisture provides a breeding ground for bacteria that can lead to pressure injury development. Poor pressure distribution along seated surfaces can lead to pressure points, and ultimately, increased compression of the tissues. Lack of sensation means the client does not realize that they need to change positions. Most of us change our position frequently. If I am not comfortable, my body says, "Hey, move," and that helps reperfuse those tissues. Incontinence not only leads to moisture, but it actually changes the pH of the skin and that makes the client more at risk for developing pressure injuries. Urine and fecal matter change the pH of the skin, and this toxic combination can quickly lead to skin breakdown. Poor hygiene is certainly a contributing factor as well. It is important to keep the skin clean and dry as much as possible. Poor nutrition impacts skin and tissue integrity, as well as healing. If this client has ever had prior pressure injuries, those areas are always at higher risk. Immobility in general means the client is not moving around and reperfusing those tissues. Friction can impact skin integrity and usually involves a degree of shear forces again. Inactivity also means we do not have the same level of blood flow. Lastly, if someone has some cognitive impairments, they may be less likely to reposition themselves.
Pressure Injury Staging
A big part of understanding pressure injuries is being aware of staging. Pressure injuries are staged or categorized usually by a wound care specialist. Even though I know these stages, remember these stages, I defer to that wound care specialist. This is their job, and they are really good at determining the stage of the wound is involved, and as a result, what treatment is appropriate. All of these images are used with the permission of the National Pressure Ulcer Advisory Panel.
Normal Skin
Let's take a moment to look at normal skin in Figure 1.
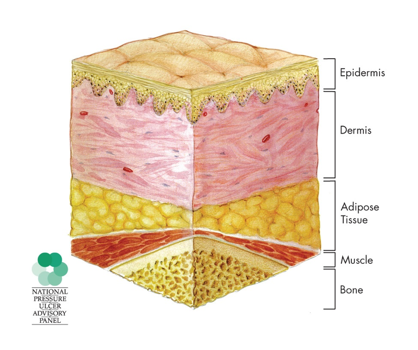
Figure 1. Normal skin.
We have the epidermis which is the top layer here, the dermis, adipose tissue, muscle, and then bone. In Stage 1, the upper layer is intact, but there will be an area of redness that does not blanch. When we push on it, instead of it turning white and then returning to red, it does not blanch at all. It stays red and that redness is often referred to as erythema. This is usually over a bony prominence, and that area of redness may be soft, warmer, or even cooler than the tissues around it.
Stage 1
Stage one is more difficult to determine in people who have darker skin tones. Often, it requires someone who is really skilled at this to determine a Stage 1 pressure injury.
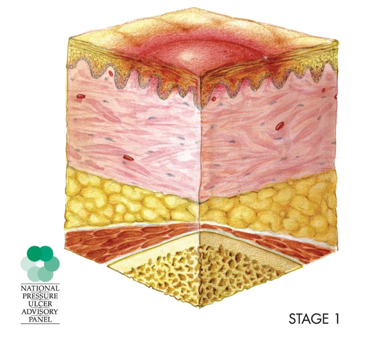
Figure 2. Stage 1 injury.
We want to catch these as early as possible because treatment is easier.
Stage 2
In Stage 2, we now have a partial loss of the dermis.
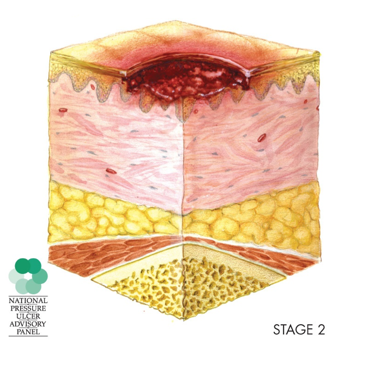
Figure 3. Stage 2 injury.
We have a shallow open ulcer wound with a red-pink wound bed, without something called slough. Slough is dead tissue that can be separated from living tissue. Sometimes this is filled with some of that material. There is often an intact or open blister that is filled with serous fluid, a clear yellowish fluid that is a result of blood plasma after a clot is formed. Also in Stage 2, we might find that the ulcer itself is dry or shiny. There might be bruising in some categories of wounds but there is none in this stage as bruising indicates a deep-tissue injury. Stage 2 does not apply to skin tears, tape burns, like medical tape, dermatitis from incontinence, or maceration of the skin. Each of those is defined below.
- Dermatitis: skin inflammation
- Maceration: softening of tissues by soaking
- Excoriation: skin abrasion
Stage 3
In Stage 3, we have full thickness skin loss, and now we have the epidermis and the dermal layers involved.
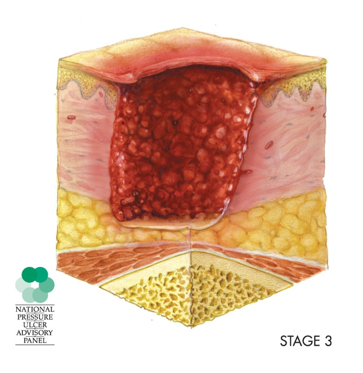
Figure 4. Stage 3 injury.
The subcutaneous fat may be visible, but we are not going to see muscle or bone in a Stage 3 injury. Slough might be present. Usually, it is not going to obscure the depth of tissue loss. There may also be undermining and tunneling and those are defined below.
- Undermining: base of the wound is larger than the opening
- Tunneling: a portion of the wound that moves away from the main opening, usually one direction
Depth is going to vary by where the wound is located. There are areas of our body where there is not as much tissue and so we might see a very shallow wound or a very deep wound. How we classify is going to depend whether this is over the ankle or at the buttock area, or ischial tuberosities, for example.
Stage 4
In Stage 4, we have full thickness tissue loss, and you may be able to see tendon, fascia, muscle, even bone.
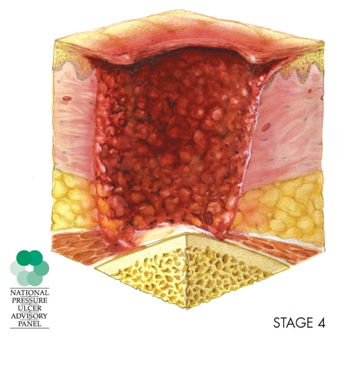
Figure 5. Stage 4 injury.
There may be some slough or eschar present. Eschar is dead tissue. As a tissue dies, it builds up within that wound bed, and there might be that undermining and tunneling. Again, this wound can be quite shallow or deep and can lead to bone infection or inflammation. Bone or muscle may be visible or directly palpable.
Unstageable/Unclassified
In addition to those four stages, we also have an un-stageable or unclassified pressure injury.
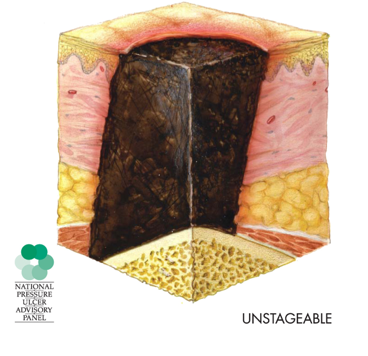
Figure 6. Unstageable injury.
This is used in the U.S. only at this time. It is where there is full thickness skin or tissue loss, but the depth is unknown because it is obscured. If the slough or eschar is removed and the depth is determined, then usually this is a stage three or four. Part of the reason this eschar is not always removed is it depends where it is. If the eschar is stable, it may not be removed because it provides a level of protection to the wound as it is treated.
Suspected Deep Tissue Injury
Another term you may hear when it comes to pressure injury staging is suspected deep tissue injury. This is also only used in the US. The depth of this injury is unknown. What is visualized on the outside is a purple or maroon localized area, discolored intact skin, or occasionally a blood-filled blister due to damage of the underlying soft tissue. This damage is from pressure and/or shear. This may progress, and then we have other issues. This is a newer pressure injury staging that is important to keep in mind as you might see in the documentation.
Despite the fact that we have some established definitions, stages, and guidelines, your workplace or team may use different terms than the ones that we see here. It is important to use the official definitions in staging.
Case Study #1
- 45-year-old woman
- Multiple Sclerosis
- Pressure relieving cushion, power tilt in power wheelchair
- Still ended up with a pressure injury
- The evaluation recommended for a new cushion
- Recommendation: adapted phone!
I treated this 45-year-old woman who had multiple sclerosis. She was seated on a pressure-relieving cushion and was in a power chair that had a power tilt available to her for weight shifts. However, she still ended up with a pressure injury. She showed up at our clinic for a new cushion. Instead of recommending a new cushion, we recommended an adapted phone. When we interviewed her to get a better sense of what had happened, she told us the following scenario. She had caregivers that would routinely come and help her transfer in and out of her chair and on and off of the toilet. The caregiver did not show up, and this woman spent 24 hours in her power chair in wet and soiled clothing. The cushion was a good cushion, and we felt it was adequate to meet her pressure needs. She was able to shift her weight using her power tilt in her power wheelchair. However, despite an appropriate cushion and the ability to shift her weight, she still needed to be transferred. No one should spend 24 hours a day in their chair, and she certainly needs to be clean and dry. If she had the ability to independently make a phone call, then she would have been able to alert someone to help her. It is very important whenever someone has a pressure injury to put on our detective hat to determine the true cause of the problem so that we can address that appropriately.
