Introduction
Thank you, I am excited to be here to talk about this topic. This is part of a three-part series on women's health.
Why OTs Should Treat Urinary Incontinence (UI)
- Incontinence and pelvic floor disorders have a profound impact on occupation, the daily activities that give life meaning.
Many people ask why OTs should treat incontinence. We, as OTs, know the answer to this. While there are several professions that treat this, incontinence and pelvic floor disorders have a profound impact on occupation. This is why it is so important for occupational therapy to also be a part of this team.
Incontinence and Occupation
- UI is recognized as one of the leading causes of institutionalization of the elderly (AHCPR,1996).
- Impairments in bowel, bladder and urogenital function result in loss of self-esteem, difficulty maintaining a healthy and independent lifestyle, and fulfilling relationships (Hajjar, 2004; Nygaard, 2003; Bharucha, 2005).
- Activities outside the home, social interactions with friends and family, and sexual activity may be restricted or avoided entirely (Fultz, 2004; Handa, 2004; Salonia, 2004).
Urinary incontinence (UI) is recognized as one of the leading causes of institutionalization of the elderly. Impairments in bowel bladder and urogenital function results in loss of self-esteem. I notice this a lot with my patients as it limits their activities outside of the home. They do not really want to go out and be with their friends, go to church, or do preferred activities. Their sexual activity may also be restricted or avoided entirely.
Psychosocial Impact of UI
- Effect on individual
- Psychologic strain
- Shame
- Anger
- Depression
- Embarrassment
- Loss of confidence
- Loss of self-esteem
- Social interactions
- Isolation
- Disengagement
- Abandonment
- Diminished sexual interest and activity
- Fear of institutionalization
- Decreased mobility and travel
- Decreased involvement in hobbies and activities
- Diminished interpersonal contact and relationships
- Increased dependence
- Psychologic strain
- Effect on caregiver
- Caregiver burden and burnout
- Resentment
- Increased financial burden
- Potential for neglect and abandonment
- Avoidance and diminished interpersonal relationships
- Increased likelihood of placement in long term institution
- Effect on Community
- Increased financial burden
- Avoidance behavior
- Feeling guilt towards involved patients
- A feeling of resentment or disdain
- Extrapolating health image to assume the individual is
- Demented
- Debilitated
- Nonfunctional
- Incapable of realizing a good QOL
- Fully dependent
(Hajjar, 2004)
This is a very big slide and I know you cannot really go over all of it this quickly, but I do want you to know about the psychosocial impact of urinary incontinence. It can affect the individual, the caregiver, and the community. For psychological strain, people can have shame, depression, embarrassment, and a loss of confidence and self-esteem. Occupational therapists have a wonderful opportunity to talk with clients and show empathy. We cannot forget the caregiver in all of this. I like to educate the caregiver, especially with the elderly population.
Basic OT Interventions
- All occupational therapists and occupational therapy assistants have the education and training to provide the following skills defined as BASIC OT interventions:
- Assessment and training self-care skills
- Clothing management
- Toilet transfers
- Hygiene
- Recognition of toileting needs
- Environmental modifications
- Prompted or scheduled toileting
In the role of OT and the treatment of incontinence, we definitely have the education and training to provide basic OT interventions. This includes an assessment and training of self-care skills, toileting needs, environmental modifications, and prompted or scheduled toileting.
- Identification of the need for adaptive equipment or adapted techniques
- raised toilet seat or bedside commode
- adapted handles or methods for suppository insertion, digital stimulation, and toileting
- use of adapted clothing fasteners
- training in adapted techniques for intermittent self-catheterization, and use of urine collection devices
There may also be a need for adaptive equipment like a raised toilet seat, bedside commode, or clothing fasteners. Some OTs teach patients how to use catheters.
Role of OT in Treatment of Incontinence
- “Some OTs may specialize in evaluating and intervening with a specific function, such as incontinence and pelvic floor disorders, as it relates to supporting engagement in occupations and activities targeted for intervention.” AOTA Practice Framework: Domain and Process 2009
There are some OTs that specialize in evaluating and intervening with a specific function such as incontinence and pelvic floor disorders. This was put out by AOTA's OT Practice Framework, and there are links to that as well that you guys can check out if you are looking at getting into this line of work.
Advanced OT Interventions
- Specialized or advanced occupational therapy intervention requires the therapist to understand body functions such as urinary, digestive, and reproductive functions and involves administering specific tests and treatment for pelvic floor muscle dysfunction.
There are advanced OT interventions available, and we do have the ability to go on for further training. This would be important if you want to get more into the urinary, digestive, or reproductive types of patients. This is an introduction to bladder dysfunction.
Competency
- OTs should acquire specialized training to perform advanced intervention for the treatment of incontinence and pelvic floor disorders.
- OTs should demonstrate competency prior to the delivery of services. Methods to obtain competency:
- comprehensive continuing education
- comprehensive clinical training with a qualified mentor
- certification through an accredited training program such as the Biofeedback Certification International Alliance.
Competency is very important, and OTs should acquire specialized training to perform these advanced interventions. Much of this is done through different organizations for continuing education. I also recommend getting a mentor in this area. You would be surprised at the amount of OTs there are in this line of work now. There is a huge group on Facebook, and there are many OT groups that are working together to try to get more of the OTs educated. I have a certification through the Biofeedback Certification International Alliance, and I will give you some more information on that toward the end of my talk.
Overview of Presentation
- Pelvic Anatomy
- Incontinence Symptoms/Definitions
- Treatment Options and the Role of Occupational Therapy
- Resources and Practical Tips
The first thing I like to do is to review the pelvic anatomy as that is very important. We will talk about incontinence symptoms and definitions, treatment options, and the role of the OT. Finally, I will touch on some resources and practical tips.
Understanding the Body Functions-Relevant Anatomy and Physiology
- Bladder
- Urethra
- Uterus
- Vagina
- Prostate
- Rectum
- Pelvic Floor Muscles
For body functions and the relevant anatomy, we have the bladder, urethra, uterus, vagina, and for the males the prostate, rectum, and the pelvic floor muscles.
Anatomy
First, we are going to look at a very simple diagram (Figure 1) that I show my patients the very first time I see a patient. I spend about 15 minutes educating them on anatomy as it is very important for them to understand how their body works.
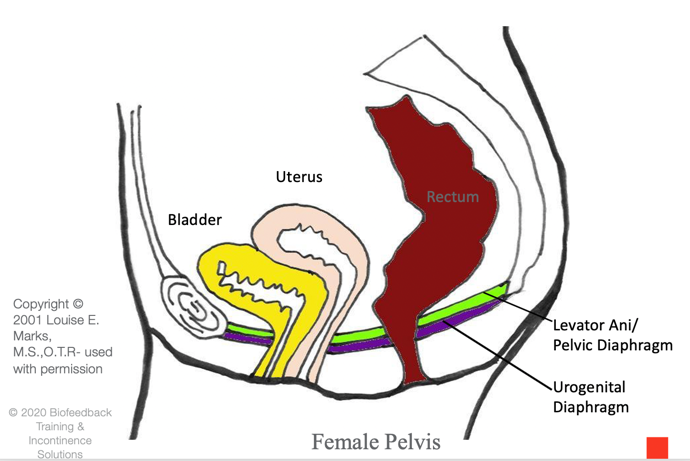
Figure 1. Female pelvis.
If you look at this diagram, at the front of the body is the pubic bone and the back of the tailbone, and all the muscles under the organs are the pelvic floor muscles. There is a superficial and deeper layer. The bladder sits in the front and the uterus sits on top of the bladder like a hat, and then you have the rectum in the back. Basically, there are three outlets, the urethra, the vagina, and the anus. These are all muscular tubes.
In Figure 2, you see the male pelvis.
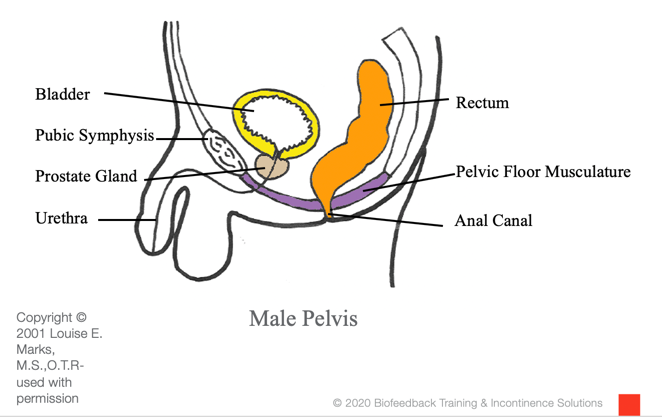
Figure 2. Male pelvis.
There is also the pubic bone and the tailbone, and there is the musculature like a pelvic floor bowl underneath the bladder, the prostate, and the rectum as well.
Figure 3 shows a more in-depth picture of the initial female pelvic diaphragm.
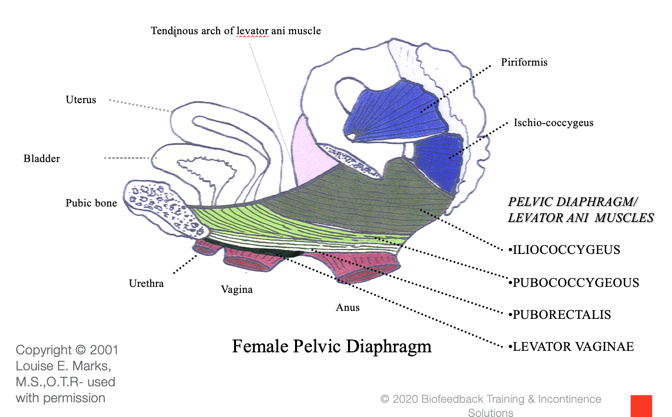
Figure 3. Female pelvic diaphragm.
I like this picture as you can see the urethra, vagina, and anus are all muscular tubes, and they are coming through the pelvic floor musculature. You have a big bowl of muscles front to back, like a hammock, that supports those three outlets.
This is another picture showing a bottom and top view of that musculature (Figure 4).
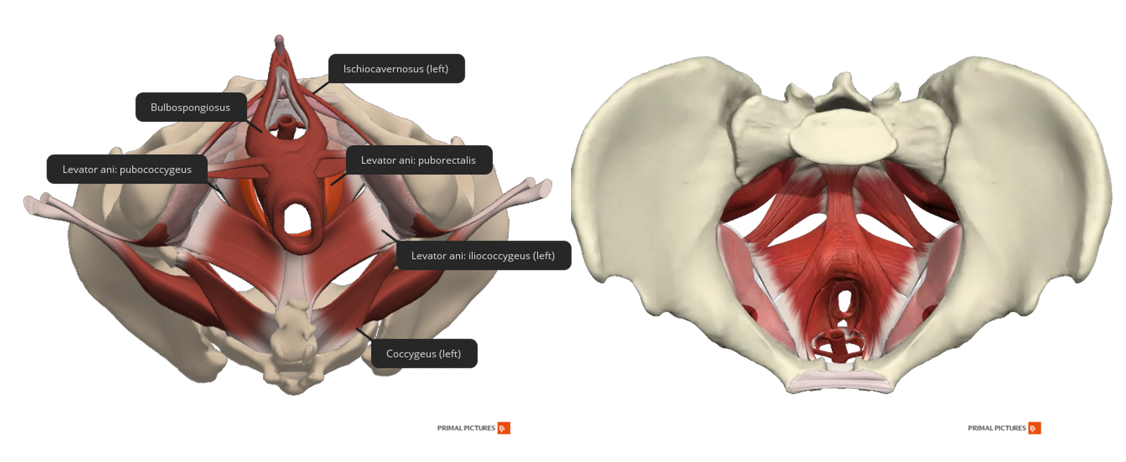
Figure 4. Female anatomy- top and bottom view of the pelvic floor musculature.
I know the muscles have small wording, but I really just wanted to show you all of the muscles that are located in the pelvic floor from the bottom view and the top view. My patients are very surprised to see how much muscle they have in the pelvic floor bowl. It is very similar to the male anatomy in Figure 5.
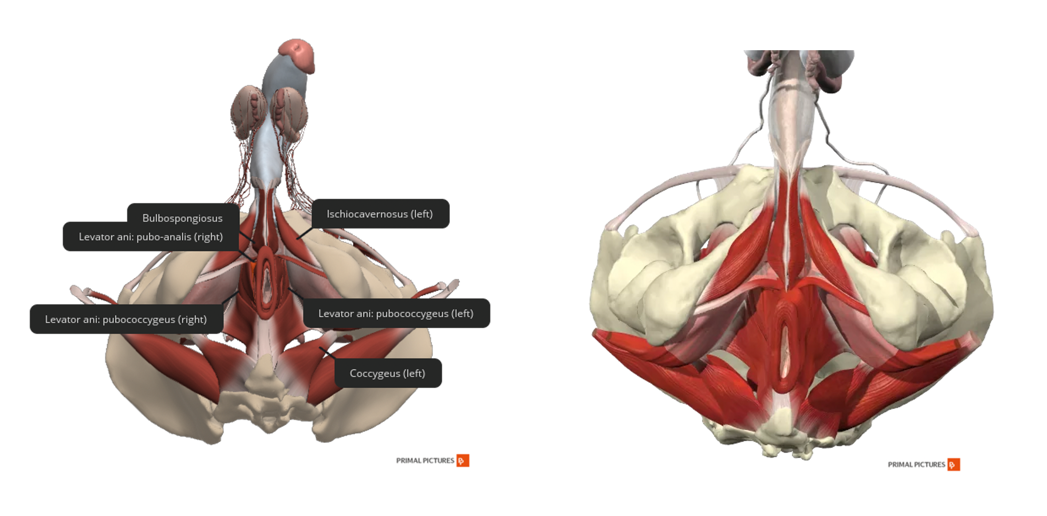
Figure 5. Male anatomy-top and bottom view of the pelvic floor musculature.
The only difference between the female and the male anatomy is how large the pelvis is. The female anatomy has a larger pelvic floor bowl for carrying and giving birth to children. I also like to show my clients these videos.
Videos 1 and 2
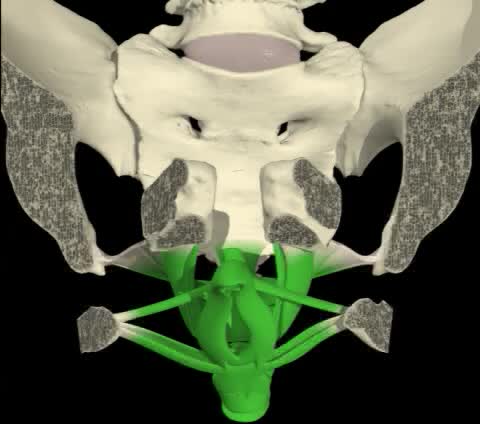
Video 1. Pelvic floor from the front.
The first video shows a woman lying on her back. There are the vaginal opening and the back of the anus with all the muscles and ligaments attached. When a person does a pelvic floor contraction, it works like a unit. I tell my patients even though you cannot feel the urethra, if you feel your anus tightening, it is also making changes elsewhere.
Video 2. Woman's pelvic floor from the side.
This is a side view, and my favorite one that I like to show my patients. There is a very important muscle that attaches to the pubic bone and wraps around the rectum. it is called the puborectalis muscle. The reason why it is easier to do a pelvic floor contraction by actually squeezing at the anus is because of the way the muscles are surrounding each other. Thus, the puborectalis muscle acts like a scarf or a sling, and it pulls everything shut and forward.
With these graphics and videos, the patients can get a really good understanding of how the pelvic floor muscles work together. Now, I am going to talk about the bladder.
Bladder
- Detrusor muscle: Circular and longitudinal fibers forming an interlacing meshwork
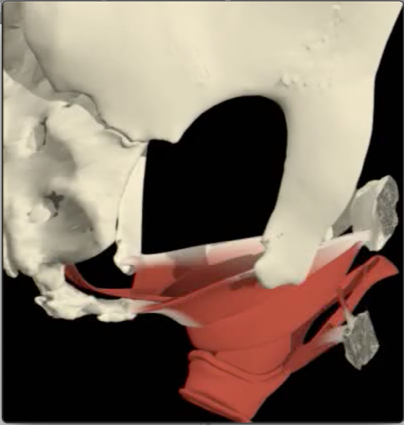
The bladder is a smooth muscle, meaning we do not have the ability to actually contract it. It is going to contract on its own (Figure 6).
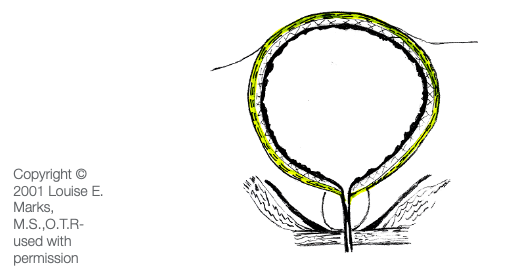
Figure 6. Bladder and detrusor muscles.
Another word for the bladder is the detrusor muscle. It is made up of circular and longitudinal fibers that form an interlacing meshwork. This is a male bladder with the prostate, and then the pelvic floor muscles are underneath that.
Pelvic Floor Function
- Support organs
- Maintains storage-anal and urethral closure
- Inhibits or permits contraction of the rectum and bladder (the gatekeeper)
- Full relaxation is needed to empty the rectum and bladder
The pelvic floor has several functions. It supports the organs and maintains storage, which is the anal and urethral closure that keeps everything in. The pelvic floor also inhibits or permits the contraction of the rectum and the bladder. It is kind of the gatekeeper. You have to be able to fully relax your pelvic floor muscles to empty the rectum and the bladder. Many patients have pelvic floor pain conditions where they are not able to fully relax. In the third series, we will talk about that in more detail.
Physiology of Micturition
This is a great video. I encourage you to take time and watch the physiology of micturition or the voiding of urine as it is a very complex system.
What Is Incontinence?
- Loss of bladder or bowel control
- The complaint of any involuntary leakage of urine or stool
What is incontinence? Incontinence is a loss of bladder and bowel control and the complaint of any involuntary leakage of urine or stool. I have patients that will say they do not have incontinence, but they do have a little bit of leakage with a cough, sneeze, or laugh.
Types of Incontinence
- Bladder Incontinence
- Stress
- Urge
- Mixed
There are three types of urinary incontinence: stress incontinence, urge incontinence, and mixed incontinence (stress and urgency issues). We will now go over each of these definitions.
Type 1: Stress Urinary Incontinence (SUI)
International Continence Society (ICS) 2019 Definition
- A complaint of involuntary loss of urine on effort (increase in intra-abdominal pressure) or physical exertion including sporting activities, or on sneezing or coughing.
Stress urinary incontinence is a definition by the International Continence Society from 2019. It is the complaint of an involuntary loss of urine on effort as there is an increase in intra-abdominal pressure on the bladder. It can include physical exertion during sporting activities or a sneeze or cough. It can also happen during standing and moving. It is usually a smaller leak than you have with urge incontinence. If you see someone cross their legs when they sneeze, you know that they probably will need your services.
Reasons for SUI
- Storage problem
- A deficient urethral closure mechanism
- Associated with intra-abdominal pressure (coughing, sneezing, running, laughing, etc.)
- Pressure gradient mechanism does not work
- Usually small amounts
- Women>Men (prostate surgery)
- High levels of physical activity (gymnastics)
- Neurologic innervation
Stress incontinence is a storage problem. There is a deficient urethral closure mechanism, and it is associated with intra-abdominal pressure. Coughing, sneezing, running, laughing, and jumping on a trampoline are all activities that might cause this. There is a pressure gradient mechanism that is not working. And again, it is usually small amounts. Women more than men will have stress incontinence; however, I have seen many men after prostate surgery with this issue. This is because their internal sphincter is affected. Additionally, high levels of physical activity can cause this. There was a recent study about female athletes, particularly within gymnastics and volleyball, that had later pelvic floor weakness. There can also be a neurologic innervation issue.
SUI with Pregnancy and Childbirth
- 46% urinary incontinence during pregnancy
- antenatally, usually transient
- postnatally, likely more severe and permanent/weakened urethral sphincter closure mechanism
- Relaxin hormone softens all ligaments and muscles of the pelvic outlet
- Partial denervation of the pudendal nerve during pregnancy reduces the postural tone of the sphincter mechanism
- Complications during labor
- poor bladder management, over-distention of bladder
- damage to the urethral sphincter closure mechanism
- long first and second stage labor, baby’s weight
- forceps, tearing, or episiotomy damaged pudendal nerve
Many females deal with stress incontinence during pregnancy and after childbirth. In fact, it is reported that 46% of patients can have urinary incontinence during pregnancy, and sometimes it stays with them. In other cases, once they stop breastfeeding and the relaxing hormone is no longer in their body, then things go back to normal with no leakage. It can also depend upon the type of delivery as there can be partial denervation of the pudendal nerve, a very important nerve in the pelvic floor. There can also be other complications during labor like poor bladder management, and sometimes there can be damage. For example, in some of my older patients, who have had forceps deliveries, they have some pelvic floor issues. Additionally, episiotomies, where they cut between the vagina and the anus at the perineum, can cause some future weakness.
Other Causes of SUI
- Weakened pelvic floor muscles and bladder outlet muscles and tissues
- urethral hypermobility (childbirth stretching)
- Intrinsic urethral sphincter dysfunction (ISD)
- Prolapse
- Prostate surgery
- Childbirth
Other causes of stress incontinence could be from childbirth stretching and/or prolapse, and we will definitely get into that in a future discussion. Prostate surgery and childbirth are other causes of stress urinary incontinence. Figure 7 shows a demonstration of this.
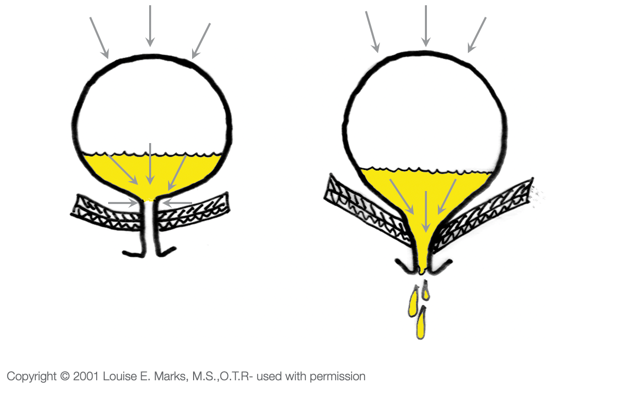
Figure 7. Bladder demonstration.
If you think of the bladder like a balloon, when there is any pressure coming down from above, like a cough, sneeze, or laugh, a lot of times that pressure is too much for that weak pelvic floor, and there will be some leaked urine. The picture on the right shows someone who has a weakened pelvic floor while the one on the left has a stronger one.
Hormones and SUI
- Age-related hormonal deficiencies and atrophy of tissues
- lower estrogen levels
- changes in urethral mucosa
- changes in cell structure/connective tissue
Hormones can also cause problems for patients as they age. They can have atrophy of the tissues especially with the lower estrogen levels, and there are going to be changes in the urethral mucosa and the connective tissue. Many of my elderly patients are on some form of estrogen therapy. The treatment for this used to cream but that was very messy. Now, we are seeing the use of a vaginal estrogen pill. The patient places a pill in the vagina and this will give their vagina more estrogen.
Treatment for Stress Incontinence
- No approved pharmacologic agents
- First-line therapy – PF rehab (BF, E-stim, vaginal cones)
- Urethral bulking with injectable agents
- Surgery (urethral support by a sling)
There really are no approved pharmacologic agents for an overactive bladder. This is where we come in. We can do things like Biofeedback, electrical stimulation, vaginal cones, pelvic floor weights, and many other treatments. There are also urethral bulking agents. The physician will put a little bit of bulking agent around the urethra which will thicken it up so that the client has a little bit more control. The problem is if they thicken it up too much, then the person cannot pee. The urogynecologist I work with uses very conservative injectables and will go back a month later to do a little bit more. There are also surgeries to place a sling for urethral support.
2017 AUA Guidelines - SUI
- In patients with stress urinary incontinence or stress-predominant mixed urinary incontinence, physicians may offer the following non-surgical treatment options: (Expert Opinion)
- Continence pessary
- Vaginal inserts
- Pelvic floor muscle exercises
The American Neurological Association came out with guidelines in 2017 that stated that physicians may offer the following non-surgical treatment options for patients with stress incontinence or mixed incontinence. The first is a continence pessary which is a little ring that you can put in the vagina, vaginal inserts, or pelvic floor muscle exercises.
- In index patients considering surgery for stress urinary incontinence, physicians may offer the following options: (Strong Recommendation; Evidence Level: Grade A)
- Midurethral sling (synthetic)
- Autologous fascia pubovaginal sling
- Burch colposuspension
- Bulking agents
If the above options do not work, the more conservative methods are the different types of slings and other surgeries.
Type 2: Urge Incontinence
Now, we are going to move to urge incontinence. This really has a bigger impact on my patients because they have an urgent need to pass the urine.
NAFC and ICS Definition
- “the urgent need to pass urine and the inability to get to a toilet in time” (NAFC)
- “the complaint of involuntary leakage accompanied by urgency” (ICS)
- Uninhibited bladder muscle contractions
The National Association For Continence came out with these definitions. With this type of incontinence, they are trying to rush to get to the toilet, and sometimes, they can have much larger accidents. An example might be your elderly patient with a rolling walker that is not able to get to the toilet quickly. They also may not have the endurance in those muscles to make it and have an uninhibited bladder muscle contraction.
Overactive Bladder Syndrome (OAB)
- International Continence Society (ICS) 2019 definition:
- Urinary urgency, usually accompanied by increased daytime frequency and/or nocturia, with urinary incontinence (OAB-wet) or without (OAB-dry), in the absence of urinary tract infection or other detectable diseases.
You will also hear the term overactive bladder syndrome. The ICS in 2019 defined it as urinary urgency usually accompanied by an increased daytime frequency and/or nocturia. Nocturia is getting up at night to go to the bathroom more than one time with urinary incontinence in the absence of urinary tract infection or another detectable disease.
- 12% of both men/women, incident increases 70-80% by age 80 years
- Urgency is a key symptom-sudden compelling desire to void
- Urgency UI-involuntary leakage accompanied by or immediately preceded by urgency
- Detrusor overactivity: A urodynamic observation characterized by involuntary detrusor contractions during the filling phase, which may be spontaneous or provoked.
Twelve percent of both men and women can have OAB symptoms, and 70 to 80% by the age of 80 years. I do see a lot of patients with OAB symptoms. Urgency is the key symptom. They have this sudden compelling desire to void, and urgency urinary incontinence is an involuntary leakage accompanied by the urge. The detrusor, which again is another word for bladder, is a smooth muscle. To assess for detrusor overactivity, they do something called urodynamics. It is a test used to see if someone has involuntary bladder contractions during the filling phase.
OAB Treatments (AUA 2014)
- First-Line Treatments:
- Clinicians should offer behavioral therapies (e.g., bladder training, bladder control strategies, pelvic floor muscle training, fluid management) as first-line therapy to all patients with OAB.
- Behavioral therapies may be combined with pharmacologic management.
According to the American Neurological Association (2014), first-line treatments should be behavioral therapies like bladder training, bladder control strategies, pelvic floor muscle training, and fluid management. These are all things I use with patients. These can be combined with pharmacologic management. Bladder medications include Detrol, Ditropan, and Myrbetriq. I never recommend someone gets off a medicine as they can gradually get off of those as they learn how to control their symptoms. However, that is a discussion for their doctor.
OAB Causes
- Uncertain predisposing factors
- Voiding against urethral obstruction
- Some thought that detrusor muscle thickening or bladder trabeculation causes decrease compliance, low volume voiding-ICS says not verified by studies on humans
- A habit of low volume voiding
- lower sensory threshold
- sensory urgency
- Diet-bladder irritants
- Fluid restriction
Some of the causes can be voiding against an obstruction. While in other patients, they are doing low volume voiding and going more than they should be going. This is going every 15 minutes because they do not want to leak. The problem with that is they are training their bladder to go too often and so they are going to have more of those urge feelings. Additionally, there can be bladder irritants, and we will review those in just a minute. Lastly, there are those that restrict their fluids as they are scared to drink. In these cases, the urine actually becomes a bladder irritant as it becomes very concentrated. We want our patients to drink an appropriate amount of fluid, water if possible because that does not irritate the bladder.
Treatment for Overactive Bladder
- Lifestyle modifications
- Behavioral therapy
- Pharmacotherapy (antimuscarinics)-
- Oxybutynin, Tolterodine, Fesoterodine, Trospium, Solifenacin, Darifenacin, Propiverine, and Mirabegron (beta-3 agonist)
- If above unsuccessful – consider botox, posterior tibial nerve stim, sacral neuromodulation (spinal implant)
There are many treatments for an overactive bladder. Lifestyle modification and behavioral therapy top the list. As OTs, we would use these interventions. Doctors can give them antimuscarinics, which are the medicines that relax the bladder so they do not feel those strong urges. If that is not successful, they can consider Botox. Yes, this is the same Botox you would use for wrinkles in the forehead, but they inject the bladder. Posterior tibial nerve stimulation is another treatment that they can get in a doctor's office, and then finally, there is a spinal implant that can be used as well.
Type 3: Mixed Incontinence
- “the complaint of involuntary leakage associated with urgency and with exertion, effort, sneezing, or coughing.” (ICS)
- Symptoms of both urge and stress incontinence
If we talk about mixed incontinence that's basically both stress and urge combined so patients can leak with coughs, sneeze, laugh, jump, move, as well as on the way to the bathroom or with strong urges so a lot of my patients have both.
Mixed Urinary Incontinence
- Combination of stress and OAB
- Pelvic floor muscles serve to inhibit bladder contractions
- When the pelvic floor is weakened, an unstable bladder can result-stress incontinence can lead to OAB
- Frequent voiding habits to avoid urinary accidents can lead to sensory urgency
This is a combination of stress and overactive bladder. A lot of times, the pelvic floor muscles can inhibit bladder contractions. One great thing that you can teach your patient is to do an appropriate Kegel squeeze, and that will inhibit the bladder. When we do pelvic floor contractions, that sends a message physiologically to the bladder to calm down. These are called urge suppression techniques, and we will talk a little bit more about those. When the pelvic floor is weakened, an unstable bladder can result, and then you can have stress incontinence.
The reason why I say stress incontinence can lead to an overactive bladder is that a lot of my patients when they start having those small leaks with a cough, sneeze or laugh, they start going frequently to avoid leaking. This then tells the bladder, "Hey, let's go to the bathroom all the time." They start developing the overactive bladder, which is a very busy bladder. You can turn the stress type into more urgency and larger leaks with frequent voiding habits which then leads back to more sensory urgency. You begin a cycle as seen in Figure 8.
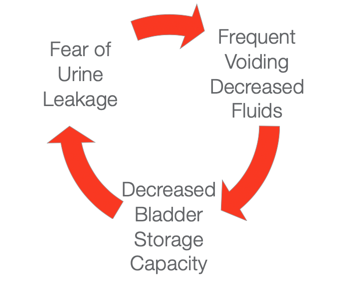
Figure 8. Urine mixed urinary incontinence cycle.
Risk Factors
- Constipation/Straining
- Age & Race (Caucasian-SUI / AA-UUI)
- Sex (women higher risk than men)
- Smoking
- Obesity
- Occupation (heavy lifting)
- Physical Activity (sports)
- Childbearing
- Family History
(Muller, 2005)
Now, we are going to talk about risk factors. One of the biggest problems I see is patients with constipation and straining. Straining is going to put a lot of pressure on the pelvic floor muscles. Age and race also play a role. More Caucasians can have it and women obviously are going to have more incontinence risk than men because of having babies. Smoking is a risk factor because there is something in the nicotine that will irritate the lining of the bladder as well as the coughing that can occur. Coughing puts tremendous pressure on the pelvic floor. Obesity is also a high risk due to the increased pressure on the pelvic floor. Many studies show that if you lose even 10% of body fat that will take the pressure off of the pelvic floor and reduce leakage. Patients who have an occupation involving heavy lifting that can also put a strain on the pelvis. Additionally, someone who is really active in sports or does a lot of jumping can also cause incontinence. Another risk factor is childbearing and family history. I have seen moms and daughters or sisters that seek treatment. It could be hereditary or there could be looser ligaments, which could also lead to patients who have a higher risk factor for prolapse.
Impact of Incontinence
- Economic Burden
- Depression
- Limited social and work activities
- Limited sexual/physical activities
- Falls/Skin lesions
- Fear of embarrassment and odor
- Toilet mapping
The impact of incontinence is huge. There can be an economic burden. There are billions of dollars spent on adult pads more so than actual pads for babies. It is a huge business. The other impact is depression. Clients tend to not go out and limit their social life and work activities. I have had patients actually lose their jobs because they go to the bathroom too frequently. We have a huge Amazon supply company right down the road from us. The bathroom is one-half mile away from where they are working. Imagine if you have an overactive bladder, and you have to walk half a mile to get to the bathroom and you only get one break. This can definitely impact someone's work. They also tend to limit their sexual and physical activities. Some of the patients can have falls and skin lesions as they are falling in the middle of the night trying to get to the bathroom. There is also a fear of embarrassment and odor. They tend to toilet map and know where every single toilet is in their community.
Emotional Cost
- Loss of Independence
- Impaired social interaction
- Low self-esteem
- Loss of intimacy
- Fear of going places
- Anxiety
- The bladder begins to control life
Let's talk a little bit about emotional cost. There is a loss of independence, impaired social interaction, low self-esteem, and a fear of intimacy. They are embarrassed and scared to go anywhere because they are tied to a bathroom. There can also be a lot of anxiety, and they begin to let their bladder control them. How can I take a vacation? Can I take a flight? It can restrict a lot of their activities.
Quotes From Our Patients
- “I don’t like to go anywhere because I’m constantly looking for a bathroom, so I just stay home”.
- “This isn’t something you usually talk to anyone about. It was psychologically affecting me. It made me feel like a hermit. I felt trapped.”
I hear the above statements all the time from my patients. It is very difficult for them to get out. The reason why I love this work is that your patients really connect with you, and they feel like they have someone that they can talk to. They tell me things that they do not tell their husbands or friends. I am an ally and someone who can help them take back that control.
Treatments for Incontinence
- Surgical
- Pharmacological
- *Behavioral Therapy
The treatments for incontinence are surgical, pharmacological, and behavioral therapy.
Behavioral Therapy
- Recommended as first-line treatment for UI
- “Behavioral techniques are low-risk interventions that decrease the frequency of UI in most individuals when provided by knowledgeable healthcare providers.”
(Agency for Healthcare Policy and Research 1996 and the 3rd International Consultation on Incontinence)
The first line of treatment is behavioral therapy We hope that physicians choose this before going right into surgery. Back in 1996, the Agency for Healthcare Policy and Research came up with a recommended UI treatment. These are low-risk interventions, and they decrease the frequency of urinary incontinence in most individuals when provided by a knowledgeable healthcare provider, like us. We can give our patients this treatment and be successful. There are many aspects as seen in Figure 9.

Figure 9. Behavioral therapy components.
If you look at behavioral therapy there are many aspects to this. Habit teaching is where you teach the patient how to control their bladder. There are dietary and fluid modifications to make sure they are getting the right fluids. Pelvic floor muscle re-education talks about strengthening, biofeedback, and Estim options. There are many things that you can do for the re-education. There is also bowel and bladder retraining. If you plan on only doing bladder therapy, I promise you are not going to be successful. You have to learn more about the bowel retraining as well, and that is our next topic in this series. It is very important to cover as someone that has constipation puts a lot of pressure on their bladder. And, there can be a prompted or scheduled toileting program that is necessary for some of your patients if they have dementia. You might have to train the families to help to remind or help them to the toilet every two hours. This will help with leaks and decrease the risk of any lesions on their skin. Here is a summary of the treatments.
- Diet, Fluid, & Lifestyle Modification
- Pelvic Floor Muscle Exercise/Kegels
- Biofeedback Treatment
- Bowel and Bladder Retraining
- Urge Suppression
- Home Programs/Patient Education
- Nocturia management
- Facilitate voiding and bladder emptying
- Treat constipation
Fluid and Diet Modification
- Eliminate or reduce bowel or bladder irritants
- Modify timing and amount of fluid intake
- Modify bowel habits if needed
For lifestyle interventions, fluid and diet modification is very important. If your patient discusses that they want to lose weight, you can let them know that it will help with the decrease of leakage with that decreased weight on the bladder and the pelvic floor. If they are smoking, you can tell them about the risk factors of how that will impact the bladder. You might have them do some relaxation training as they may have a lot of anxiety and stress. Nocturia again is getting up more than once a night so nocturia management is important to talk about with those patients. Again, constipation is important to treat as many patients strain and push with constipation.
Common Bladder Irritants
- Caffeine
- Alcohol
- Coffee/Tea
- Chocolate
- Citrus Products
- Artificial Sweeteners
- Spicy Foods
- Tomato Products
- Vitamins B & C
- Sodas
We want to make sure that they are eliminating or reducing bowel or bladder irritants or modify the timing and amount of fluid intake if needed. Pretty much everything that the bladder hates is what everybody loves. Examples are caffeine like coffee and tea. Keep in mind that one cup of coffee is as much caffeine as three cokes so if I have a patient that is drinking two cups of coffee, I will tell them it is the same amount of caffeine as a six-pack of coke. Sometimes that is surprising enough to them that they might move to decaf or reduce their intake. Chocolate also has caffeine especially the dark variety. For my clients that love their chocolate, I tell them to have it after lunch instead of after dinner.
Alcohol also has an impact. If someone has wine before they go to bed at night, they will definitely have to get up in the middle of the night because the bladder does not like alcohol. Anything that is citrusy will also cause irritation to the bladder. Anything sweetened whether it is natural or not will irritate the bladder. Additionally, spicy foods or tomato-based products can be irritating to the bladder. Lastly, vitamins are very important. I do have my patients continue their vitamins, but I have them do it in the morning rather than the evening.
Other Bladder Irritants
- Carbonated Beverages
- Milk or Dairy Products
- Sugar
- Melons
- Artificial Colors
- Concentrated Urine
Sodas have carbonation, coloring, and often caffeine. Milk or dairy products can also cause nighttime issues. For kids and bedwetting, I try to get them to not drink milk in the evenings. Melons have sugar in them so that will irritate the bladder as well. Anything artificially colored is another irritant. And then finally, if someone is limiting their fluid intake, they are going to have concentrated urine which also irritates the bladder. I like to give a list of these bladder irritants to my patients, and we discuss this as part of their treatment.
Pelvic Muscle Exercises-Arnold Kegel - 1948
- Used to teach patients to strengthen the pelvic floor muscles
- Originally taught using a pressure feedback device
Let's talk about Kegel exercises. In 1948, Dr. Kegel used this method to teach patients how to strengthen the pelvic floor muscles. However, it was also taught with a pressure feedback device. It was not just learning how to squeeze the muscles, but they actually also used a Biofeedback device that was inserted vaginally, and then when they squeezed on it. It provided that feedback so that they could know that they were doing the Kegel correctly.
Kegel Exercise
- Gently contract the muscle as though you are holding back gas or the flow of urine
- Keep your abdomen, hips, buttocks relaxed
- Don’t hold your breath
When you do a Kegel exercise, it is very important that you gently contract the muscle as though you are holding back gas or the flow of urine, but I make sure my patients are not doing Kegels on the toilet. A lot of patients are taught to squeeze when they are actually peeing, which will stop and start the flow of urine. However, this is not a good idea because it can back up urine and cause UTIs. And, I do have patients that come in with voiding dysfunctions because they are constantly stopping and starting the flow of urine. I have heard both doctors and therapists tell patients to stop and start the flow of urine because they want them to recognize where the muscle is. But, if I asked you right now to squeeze your urethra, you probably would not be able to find it because it is so small and difficult to feel. If my patients can feel their vaginal contractions then great, but many do not feel that sensation especially when they are elderly.
Most of the time if they have bowel control or they are able to hold in gas, this is the easiest way to encourage this exercise. I tell them that they will feel pressure at the anus as they are contracting, kind of like cinching of a purse. This contraction will roll from the back to the front. You do not want them to squeeze their buttocks or legs because you want them to only work on the sphincters that control urine and stool. We also do not want them to hold their breath. When you hold your breath, this puts pressure on the pelvic floor as the diaphragm and pelvic floor work together in concert. When you are exhaling, the pelvic floor is rising, and when you are inhaling the pelvic floor is relaxing down. So, you want your patients to breathe normally, do not hold their breath, do not squeeze their buttocks or legs, and just pretend that they are stopping gas.
I always start them on a very short squeeze so maybe a three-second hold, six-second rest, and I want them to do 20 squeezes three times a day. Research also shows 60 to 80 Kegel squeezes per day can build muscle, but if your patient is doing random exercises and they are not doing consistent contractions, they will not get better. If they say, "I have done Kegels my whole life and they're not working," they are probably not doing 60 to 80 squeezes per day. That is what it takes to build muscle. I keep them on that plan slowly building up their endurance every week. For example, I add one second on so if they start with a three-second hold, the next week it is a four-second hold, the next week a five-second hold, and so on. We build up to a 10-second hold, 10-second rest for 20 reps, three times a day. It is going to take them about six to seven weeks to get to that point. We are not trying to rush it. and we do lying down or sitting, not standing right away because it is too hard for the pelvic floor and they will end up holding their breath.
Kegel Exercises Alone Are Often Inadequate
- In current practice, patients are often given a simple handout with limited explanation by their physician.
- Research indicates simple written and verbal instructions are inadequate (Burgio,1985).
- 30% perform incorrectly even with intensive instruction (Bump,1991)
Kegel exercises alone are often inadequate. In current practice, patients are given a simple handout from their physician and a lot of times that is not enough. They need more instruction and 30% of patients perform the exercise incorrectly even with intensive instruction. This is where Biofeedback comes in.
Biofeedback
- Small electrical signal monitored with electromyography (EMG)
- Information about an unconscious process is presented visually on a computer screen
- Immediate knowledge of muscles becomes available to teach the patient how to alter the physiologic process
I have been doing Biofeedback for 15 years. I absolutely love it, and there is a great certification for OTs. There are not a lot of women's health certifications out there, but one of them is this Biofeedback certification, which I recommend. There is also one through Herman and Wallace, but you have to have two or 3000 hours of patient care treating pelvic floor dysfunction. The Biofeedback one you can start immediately, and you can learn all the foundations of the bladder, bowel, and pelvic pain and then learn how to use the Biofeedback machine.
Biofeedback uses a small electrical signal that is measured via EMG. I tell my patients that it is a lot like an EKG that measures heart activity, but the EMG measures muscle activity. It is information about an unconscious process that can be seen visually on a computer screen. If your patient cannot figure out how to do the Kegel exercise or you are not seeing improvement, I recommend that they have Biofeedback. This way they have immediate knowledge of the muscles they are activating. Here is an example in Figure 10.
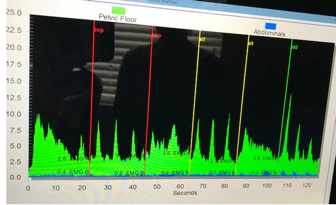
Figure 10. An example of biofeedback.
The green is the pelvic floor and the blue (at the bottom) represents the abdominals. I place electrodes on both the abdominal muscles as well as the pelvic floor by a small sensor inserted either vaginally or rectally. You can do this or the client can do this. You do need to go to a course if you are not familiar with how to do a pelvic floor exam, which we do not learn in school. I highly recommend going to Herman and Wallace Institute for pelvic floor series where you learn that. It is definitely within our practice act to do that. In this particular case, this person inserted the sensor privately in the restroom.
At first, I had them lying down. The first part of this picture shows a10-second contraction. You can see how that line gradually goes down and that means the muscle is not able to hold for a full 10 seconds. As I stated earlier, I am not going to give this patient a program of holding a contraction for 10 seconds right away. The second set of green spikes are quicker squeezes. Those are called quick flicks, and I am measuring the coordination of the muscle. Then, I put the patient in a sitting posture, and they try again for a 10-second hold, three quick Flicks, and finally, they move to a standing position and do the same things. You can see that it gets a little more challenging at the very end (way to the right). They are having a much more difficult time in the standing position which is pretty typical. This is what an assessment could look like for Biofeedback. If they were using their abdominals, you would see a lot of blue. This would give me an indication that they are using their abdominal muscles which would put extra pressure on the pelvic floor.
Pelvic Floor Muscle Exercises
- 20-25 repetitions 3x a day
- Focus on slow sustained contractions building up to 10 seconds
- 1x a day- quick isolated contractions
- Progress from supine to standing as skill improves
- Use Olson Kegel App (search Kegel trainer pelvic floor exercises – green box with a checkmark)
As you have probably realized from my talk today, pelvic floor muscle exercises or Kegels are important. I try to get them to do 20 to 25 repetitions three times a day while slowly building up their endurance. I want them to go from a three-second hold to a 10-second hold 7 weeks later. The quick flicks are more for working on coordination as mentioned as 30% of your pelvic floor is made up of fast-twitch muscle fibers. These are the ones that if you cough, sneeze, laugh, have to be coordinated enough to grab those muscles. I call them the holders and the grabbers. The fast-twitch muscle fibers are grabbing and these slow-twitch muscle fibers (70% of the pelvic floor muscles) are the endurance ones. These help you get to the bathroom in time. I do progress a patient from supine to standing as their skill improves.
I like the app, Kegel Trainer, that is available both for Android or iOS operating systems. I also recommend the paid version. It is $5.99 as a one time fee. I have had this app for 6 years, and I use it on a daily basis. Clients can bring it in and you can see how they are doing with their exercise program and it keeps them accountable. There are some great ones out there but be careful because there are some apps that you might pay a lot of money for someone to write on a piece of paper on how to do a Kegel squeeze. I have purchased all of them, and this is the one I find that is the most user friendly.
Bladder Training
- Review bladder diary
- Determine the longest comfortable interval for the patient
- Gradually increase voiding interval
- Goals - increase storage capacity, decrease frequency and urgency
I like to review a bladder diary with my clients. In this, they indicate how often they are going to the bathroom, if and when they have a leak, was it on the way to the bathroom or during a cough, sneeze, or laugh, and their fluid intake.
I want to determine their bathroom intervals. If they are going to the bathroom every 30 minutes, this is too often. I will have them gradually work on increasing the time between voids. I will try to move them from 30 minutes to 45. I tell them, "You have to be in charge of your bladder and not let it be in charge of you. Once they are comfortable with 45 minutes, you can move it up to one hour. Every week you can go up by 15 minutes. This basically takes an out of control bladder and puts it on a good time schedule. Bladder training helps them to increase their storage capacity and decrease the frequency and urgency.
Urge Suppression
- Stay still or sit down
- Take some deep breaths and relax the abdominal muscles
- Perform gentle PFM contractions to calm the urge
- Wait for urge to pass
- Walk to the bathroom at a normal pace
Many times, they have to suppress those urges. It can be difficult so they are going to have to use an urge suppression technique. The easiest way to do this is to stay still. If they run, they will jiggle the bladder. I tell them when they feel an urge they need to sit down and take the pressure off of the bladder. They then need to take some deep breaths and relax the abdominal muscles and do some Kegels. They can either do quick squeezes or long holds to calm that urge. They want to wait for that urge to pass. If you go right when you feel the urge, I call that an "urgency emergency." You are letting the bladder win and you want to make sure you let that urge pass. Once it passes, you want to walk normally to the bathroom and do not run. I even have patients who will set a chair between their kitchen on the way to the bathroom so that they can stop and do an urge suppression technique before they continue to the bathroom.
Stress Strategies-KNACK
- Squeeze before you sneeze, cough, laugh, lift, blow your nose, etc.
- Make it a lifetime habit
- Requires practice and coordination
- Decreases risk for further weakness and prevents leakage
The other thing I teach my patients is this called the KNACK maneuver. KNACK does not stand for anything and is not an acronym. It is just getting the "knack" of it. When you cough or sneeze, usually there is tremendous pressure coming down onto the pelvic floor, and a lot of patients will have leakage when that happens. Prior to a sneeze, I have them do a Kegel squeeze, so they squeeze like they are stopping gas, which in turn will close the vagina and the urethra. By doing this, they are keeping that pelvic floor contracted during the sneeze. And, if they have three sneezes in a row, they maintain that contraction. Once they stop sneezing they can let go. This is something I try to get them to make a lifetime habit. I even have little buttons and magnets that say squeeze before you sneeze. Those are great little marketing tools that you can use. I give my patients these to stick on a refrigerator to remind them that it is important to squeeze when you have that pressure coming down onto the pelvic floor to support it. It does require practice and coordination but it does to decrease that risk for further weakness. And, it also helps those patients who have had minor leaks.
Home Programs
- Bowel or bladder diary as needed
- Lifestyle modifications
- PFM exercises 3x a day
- Urge suppression techniques
- Relaxation exercises if needed
I love using diaries. I have one on my website, pelvicfloorbiofeedback.com, that you are welcome to use. It is important to give them the lifestyle modifications and make sure they are completing their pelvic floor exercises. If they cannot do 20 squeezes, you can have them do 10 pelvic floor contractions every two to three hours throughout the day trying to get in those 60 reps. However, if you do less than 10 squeezes, you are not going to build muscle. The minimum would be 10 contractions in a row with a rest in between. If they're squeezing for several seconds, they need to be resting for several seconds so the muscle doesn't get too fatigued. You want to have them do urge suppression techniques and relaxation exercises if needed.
Behavioral Therapy Modalities and Tools
- Scheduled toileting (every 2-4 hours) for frail elderly or Alzheimer’s patient with the goal to keep the patient dry
- Timed voiding & double voiding
- Retention
- Absorbent pads & skincare products
- Habit training
- Enema or laxative to clean bowels
- Attempt BM at a regular time after the meal
- If no BM after 48 hours, repeat enema or laxative
Some different behavioral therapy modalities and tools are also available. I would recommend scheduling toileting if a patient has Alzheimer's or dementia. You want to get them on a scheduled voiding and toileting program. You can time voiding and double voiding. Double voiding means if someone does not feel they are completely empty, and they sit back down again. It is important to have your patients lean forward, with their elbows on knees after they are done to make sure they are done. It can take an entire minute to completely empty a bladder. Many patients get up too quickly. It is very important that your patients do not push out their pee. Though their pee will come out faster, they will actually be weakening their muscles. Thus, teach your patients to lean forward, elbows on knees completely, relax the pelvic floor, and stay for one minute after the urine flow stops. They are going to hear dribbling and draining, but they need to let those muscles completely relax.
There are also different types of products available. Make sure that they are taking care of their skin.
Lastly, habit training can be helpful. For instance, if they are having constipation, they may want to ask their MD about laxatives or enemas. However, if they are not having regular bowel movements and this is affecting their bladder, I do recommend they see their MD. I do encourage them to attempt a bowel movement at a regular time after meals, and we will talk more about that in the bowel section in two weeks. And, if they are not having a bowel movement, they can also increase their fiber and water intake.
- Pessaries
- Dilators
- Dyspareunia
- Vaginismus
- Weighted cones
- Graduated weights
- Stress urinary incontinence
A pessary is one thing that my patients will use especially if they have a prolapse, meaning the bladder or the uterus or the rectum will fall as the ligaments loosen a little bit. Probably 80% of my practice deals with prolapse. I have a lot of patients that the physician will place a pessary which will then lift that organ back up in a proper position.
A dilator will be discussed more with the pelvic pain talk. It is used with dyspareunia or pain with intercourse. The word vaginismus means a patient's muscles in th
