Introduction
This is the second part of a women's health series. It is okay if you missed the first part because it is now available in the library. That focused on bladder disorders and part three will be on pelvic pain. I appreciate the opportunity to be here, and I am excited to talk about this topic. I know most people might think it is strange to talk about bowel disorders but it is a great area to treat. You will have many patients that also have bladder disorders along with this. The more you learn about each, the better you will be able to treat them comprehensively.
- Bowel anatomy and physiology
- Medical Assessments and Diagnostic Tests
- Fecal Incontinence, Constipation, and Dyssynergia
- Behavioral interventions for bowel disorders
We are going to review some of the bowel anatomy and physiology and also talk about some medical assessments and diagnostic tests. This is important to know because they may ask you questions about certain tests. Having a general idea of what is out there is good practice. We will talk about the most common issues that you might see in your clinic which is fecal incontinence, constipation, and dyssynergia. There are many others, but these are the most common. We will also review behavioral interventions for bowel disorders.
Anatomy
- Anal Canal
- anal skin margin to the pelvic diaphragm
- 3-4 cm long
- two sphincter muscles
- Internal Anal Sphincter
- near the rectum
- partial contraction-smooth muscle
- External Anal Sphincter
- distal to and overlaps the internal
- striated muscle both voluntary and involuntary control
- subcutaneous, superficial, deep
- deep layer fuses with puborectalis
The anal canal is three to four centimeters long, and there are two sphincter muscles, the internal and external anal sphincters. The internal is more smooth muscle, and it is going to react when stool is present. The internal anal sphincter sends a message to the external anal sphincter, which is going to the outside, that there is a stool that is ready to come down. The external anal sphincter is at the exit, and it is a more strident muscle that we can voluntarily and involuntarily control.
- External Anal Sphincter
- usually in a state of involuntary partial contraction
- gas, diarrhea, solid stool discrimination
- pudendal nerve
- Puborectalis Muscle
- pubic bone and loops around the anorectal junction
- part of levator ani muscle-medial
- involuntary partial contraction
- maintains anorectal angle
- voluntary action
- usually contracts along with the external anal sphincter
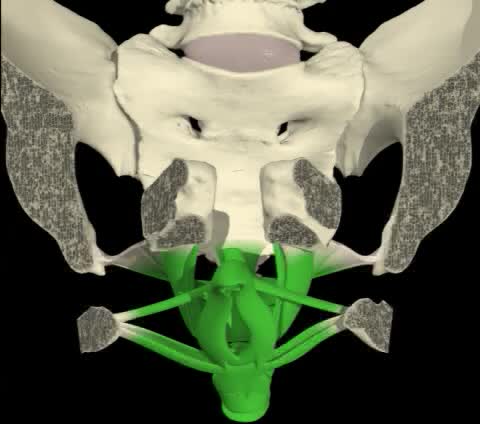
The external anal sphincter is usually in a state of involuntary partial contraction which is important because you want to make sure that you keep your stool and gas inside. The pudendal nerve is also a very important nerve that we will be talking about as well. The puborectalis muscle starts at the pubic bone, wraps around the rectum, and comes back around in a loop. It is a very important muscle and part of the levator ani muscles. This also has an involuntary partial contraction along with the external anal sphincter. And, there is an angle that is formed so that when we are sitting upright, it keeps the stool in place. We do have voluntary control over this muscle as well and it partners with the external anal sphincter.
- Other pelvic diaphragm (levator ani) muscles
- pubococcygeus
- iliococcygeus
- ishiococcygeus
- all support pelvic viscera
- Anal Canal Nerves
- upper half-sympathetic and parasympathetic
- lower half-pudendal nerve (inferior rectal nerves)
Other pelvic diaphragm (levator ani) muscles include the pubococcygeus, illicoccygeus, ishiococcygeus, and other supportive pelvic viscera. There is a lot to go over with anatomy I do recommend looking more into it when you do have a chance because you do want to understand anatomy when you are talking with your patients. There are also sympathetic and parasympathetic nerves involved.
- Rectum
- 15 cm
- longitudinal muscle fibers
- SNS and PNS
- sensory fiber ANS, low to pain, high to distention, stretch
Finally, the rectum is 15 centimeters in length. It is comprised of longitudinal muscle fibers and the two different branches of the nervous systems. There are sensory fibers, low to pain, high distension, and because it has to distend to have stool, there are stretch fibers as well. Figure 1 shows the puborectalis muscle.
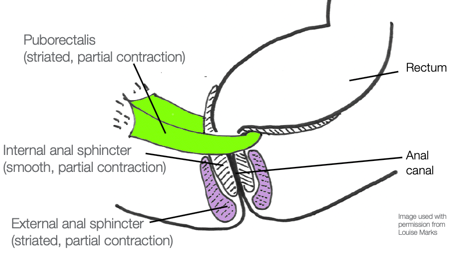
Figure 1. Puborectalis and sphincters as rest. (Image used with permission from Louise Marks.)
I like to show this picture to my clients. Louise Marks, who is an OT, gave me permission to use her drawings. Figure 1 shows the puborectalis muscle looping around and creating that angle to keep the stool in. The top of the rectum is where the stool is going to be stored. The puborectalis muscle, in green, wraps around that. The external anal sphincter, in purple, is the one we can control. You can squeeze this if you need to hold in stool or gas until appropriate. Remember these muscles always have a partial contraction to keep the stool and the gas in.
The defecation reflex is next. (Figure 2). This is when the rectum is contracting because it is trying to push out a stool.
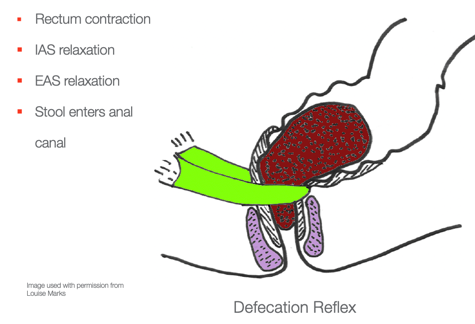
Figure 2. Defecation reflex. (Image used with permission from Louise Marks.)
The puborectalis muscle and the external anal sphincter have to relax to allow this to happen. The rectum squeezes and pushes out while the muscles that we can control are relaxing at the same time. Figure 3 shows the accommodation of the rectum.
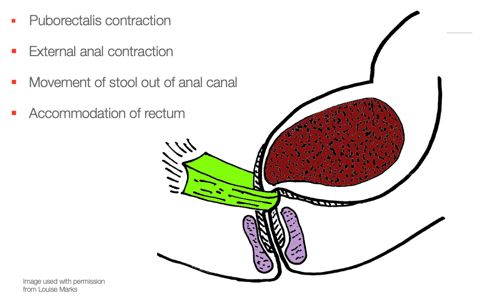
Figure 3. Accommodation of the rectum. (Image used with permission from Louise Marks.)
What you would do is you would contract the puborectalis muscle and the external anal sphincter. With this accommodation, the stool pushes back into the rectal area so you will not get that feeling as much. The problem is if you do this too often the stool is going to sit there or scoot back up into the colon. It might then remain for a couple of days and not come back. For your patients with constipation, you really want to encourage them to go when they need to go. If they continue to inhibit the defecation reflex, this might result in a harder stool and make constipation worse.
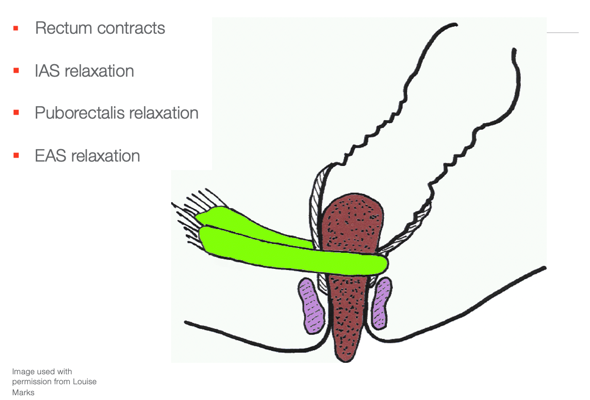
Figure 4. Defecation. (Image used with permission from Louise Marks.)
With defecation, the rectum contracts and the stool is going to pass through. To allow this the muscles have to relax. And, then the external anal sphincter helps to push all of that through.
Mechanism of Defecation
- Coordination of both voluntary and involuntary responses
- Peristaltic activity large intestines
- Rectal walls stretch (rectal distention)
- Nerves in rectal wall detect rectal distention and initiate the defecation reflex
- Defecation Reflex-3 simultaneous actions
- rectal wall contracts
- internal anal sphincter relaxes
- external anal sphincter relaxes
There is a coordination of both voluntary and involuntary muscles as we control some of this. There is peristalsis which happens in the large intestines to move things through. The rectal wall has to stretch, and there are nerves in the rectal wall that will detect that. All of this initiates the reflex that you feel when you need to have a bowel movement. There are also three simultaneous actions: the rectal wall contracts, the internal sphincter relaxes, and then the external one will as well.
Anorectal Anatomy and Physiology
- Inhibition of Defecation Reflex
- Rectal distention is perceived
- Message to the external anal sphincter and puborectalis muscles to contract
- EAS and puborectalis override the reflex
- Rectal accommodation
- Voluntary Defecation
- Valsalva maneuver (bear down)
- Voluntary relaxation of EAS and puborectalis
First, there is inhibition when you are contracting so that you can override that reflex, and then the stool shoots back up and the rectum will accommodate for that stool. Then, there is the voluntary defecation when you actually want to have a bowel movement. You do something called the Valsalva maneuver which is bearing down. If you think about it, when you are having a bowel movement, you bear down but not with too much straining. This causes pressure internally. Finally, there is the voluntary relaxation of the external anal sphincter and the puborectalis muscle. Figure 5 is from the Rome Foundation showing this process.
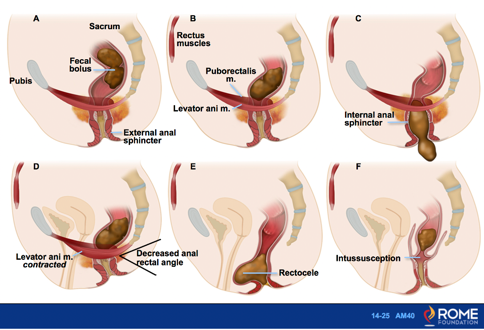
Figure 5. Overview of voluntary and involuntary control of the muscles during defecation. (Image used with permission.)
This is a great foundation and you will see many slides from them. This slide gives you an idea here what is happening with the different types of muscles with both voluntary control or involuntary control. It also highlights different types of problems that there can be as well.
In the top right picture, there is the pubic bone and the puborectalis muscle that is coming around the back. You can also see the external anal sphincter. The levator ani muscles are also shown. When you have a contraction of this muscle that is keeping the stool up, you have a decreased rectal angle (Image D). We will talk a little bit more about a rectocele (Image E). A rectocele can happen if people strain continuously or have asthma and are coughing all the time. This creates a significant amount of pressure coming into the rectum which causes the stool to get stuck in a pocket. I also see a lot of patients with bladder, uterine, and rectal prolapses. This is when and can be corrected by something called a pessary that can be inserted vaginally or surgery to correct that. You can imagine that this can cause some problems if the stool is stuck here (Image F). Intussusception is a part of the intestine folds into itself and can cause a blockage.
Factors Maintaining Continence
- Normal transit time with normal consistency (time for food to travel through GI tract)
- Normal capacity to store
- Normal voluntary control
- Normal reflexive action of the anal sphincter complex
- Contraction of EAS and puborectalis muscle
- Sensory awareness of stool in the rectum
Incontinence is when you are unable to control the leakage. In order to maintain continence, you want to have a normal transit time with a normal consistency of the stool. You also need the capacity to store the stool. Additionally, you need to have normal voluntary control of your muscles to keep everything in. There is normal reflexive action of the anal sphincter complex and you have to have a contraction of the external anal sphincter and puborectalis muscle that I showed you a little while ago. Lastly, if you do not have sensory awareness in the rectum, then it is difficult to have that control as well.
Video 1
This is a view of a female patient that is lying on her back. When the patient contracts her muscles, everything comes in including the urethra, the vagina, and the anus. They are all contracting together. I like to show my patients this video so they can see that it is one unit working together when I am teaching them how to do Kegel exercises.
Video 2
This is a side view which I like even more because you can see the puborectalis muscle. This looping muscle attaches to the pubic bone and runs back around the rectum. It is an extremely important muscle and the biggest muscle in this whole bowl of muscles. You can see how everything works together. When I am teaching Kegels, I want them to squeeze at the anus as if they are trying to hold in gas. This is going to give them back gas and stool control as well as urinary control.
Transit Time
- Slow transit time > more water gets reabsorbed by the body, and the stool becomes harder
- To increase transit time = increase fiber which triggers peristalsis
When someone has slow transit time, it means more water is getting reabsorbed by the body and the stool is getting harder. The slower the stool goes through the colon, the harder it gets. To increase the transit time, we definitely want to add fiber which will trigger peristalsis, which is the movement of that colon.
Disorders Involving the Anus and Rectum
- Fecal incontinence
- Anal or rectal pain
- Dyschezia (difficulty expelling fecal material from the rectum)
- Pelvic floor dyssynergia (an inappropriate contraction of the anal sphincter muscle when straining to have a bowel movement)
There are many disorders that can involve the anus and rectum. Fecal incontinence is the leakage of stool. There can also be anal or rectal pain. Dyschezia is difficulty expelling fecal material from the rectum. Lastly, there is a pelvic floor dyssynergia. Dyssynergia is the inappropriate contraction of the anal sphincter muscle when straining to have a bowel movement. During a bowel movement, you should be relaxing the external anal sphincter but some people might contract instead. For example, if someone has hemorrhoids or pain, they may tense if they are worried that it might hurt. In these cases, it might be hard to get the stool out so they can have that incoordination as well.
Patient Intake For Behavioral Interventions
- Physical exam
- Comprehensive history
- Diagnostic tests
- Biofeedback assisted behavioral interventions
Physical and Comprehensive History
We want to look at the patients their physical exam and comprehensive history. It is also important to look at any diagnostic tests that they have had. Personally, I am passionate about biofeedback, it helps a lot with patients that have bowel disorders.
- Onset and duration of bowel symptoms
- Frequency of episodes (3x a day to 3x a week is normal)- Men usually 2-3x a day vs women once every 2-3 days due to physiologic function
- Change in bowel habits
- Stool consistency
- Straining
- Neurological symptoms
- Blood or mucus in stool
It is important to know the onset and duration of the bowel symptoms and the frequencies of the episodes. Typically, what is normal are bowel movements three times a day to three times a week. I know a lot of people will think, "Wow! Three times a week means that someone is constipated." However, what you really need to look at is the consistency of the stool. If it is soft like a banana, then it is normal. If it is hard like pebbles, then that is a sign of constipation. Usually, men go two to three times a day versus women who are once every two to three days. This is just due to physiologic function. If there is a change in bowel habits, then we want to know what the stool consistency is. Are they straining? Do they have neurological symptoms that could be impacting this or blood or mucus in the stool?
- Diarrhea
- Difficult vaginal delivery
- History of pelvic or anal surgeries
- Abdominal cramping
- Pelvic or anal pain
- Present medications
- Type and number of protective pads
- Effects of various foods
- Are there urgent calls to stool
Other things to note, do they have diarrhea. did they have a difficult vaginal delivery that maybe they had some muscle tearing causing problems, any history of pelvic or anal surgeries if they have abdominal cramping, pelvic or anal pain, what presents medications are they on? There are many medications that can cause constipation. Are they wearing any types of protective pads, what are the effects of various foods, a lot of your patients will know okay, if I have something fried and greasy it really affects my stools or if they eat eggs or certain things will definitely be a trigger for them and they usually know those triggers. And do they have urgent calls to stool, are they rushing? Do they have fecal urgency?
Medical Assessment and Diagnostic Investigations for Anorectal Disorders
I want to go over a few medical assessments and diagnostic investigations so that you guys are familiar with these.
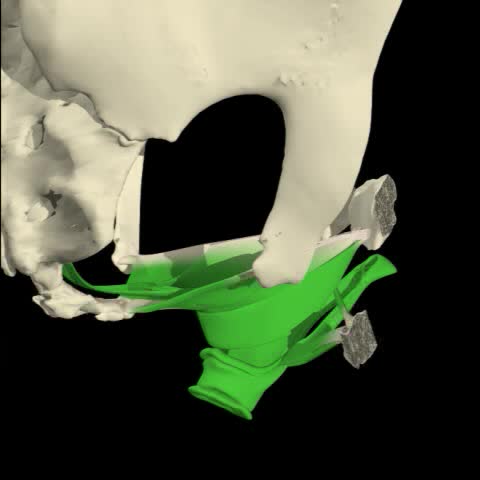
Anorectal manometry. Anorectal Manometry is a diagnostic procedure designed to examine the muscle function of the anorectal area. The procedure consists of placing a (pencil thick) flexible tube into the rectum that holds multiple sensors to detect and record pressure activity in the rectum and anal canal.
As OT's, we can get trained in doing this. Many doctor's offices are doing this especially the GIs and urogynecologists. Anal rectal manometry is a diagnostic procedure designed to examine muscle function.
- Strength and control of the anal sphincter muscles
- The sensation of stooling in the rectum
- Reflexes that govern bowel
- Movements of the rectal and anal muscles
- Coordination with defecatory straining.
During this procedure, you place a pencil-thick, flexible tube into the rectum. It has multiple sensors to detect and record pressures in the rectum and the anal canal. It also looks at the strength and control of anal sphincter muscles. It differs from biofeedback as biofeedback does not measure strength only the electrical activity of the muscle. This also tests for sensation which is extremely important to have for bowel function. This test also looks at the reflexes, movements of the rectal and anal muscles, and coordination with the defecatory straining. It gives the practitioner a lot of valuable information.
Figure 6 is an example of what it would look like.
Figure 6. Example of anorectal manometry. (Image used with permissionfrom the Rome Foundation).
Again, this assesses the internal and external anal sphincters and also sensation. The tube is placed inside, and they can either add air or sometimes liquid to test the sensitivity, strength, and function of the muscles.
- Anorectal manometry is useful in the diagnosis of the following conditions:
- Constipation, particularly difficulty with stool evacuation (dyssynergic defecation)
- Stool leakage or fecal incontinence
- Anorectal function before or after bowel surgery
It also is useful or diagnosing things like constipation, especially if they have dyssynergia, stool leakage or fecal incontinence, and anorectal function before after bowel surgery. So if a patient comes to me from a urogynecologist's office, typically, they have an anorectal manometry to view. This is an example of what manometry would look like (Figure 7).
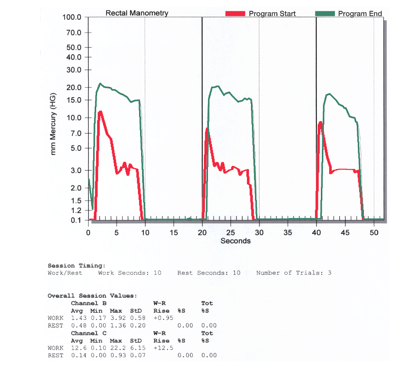
Figure 7. An example of anorectal manometry (Author's image).
The green line is what happened by the end of treatment; whereas, the red is when we started. Again, this tests muscle strength and endurance. You can see that the red is where the patient is squeezing. They have a hard time holding even for 10 seconds. They are holding that contraction for a couple of seconds, and then the muscle strength drops. After many sessions of doing Kegels and many other things to increase that strength, you can see that they are able to hold the contractions longer. The green lines show that they are able to hold for a 10-second contraction.
Rectal Sensation Test.
- Balloon Expulsion Test
- Measurements:
- First sensation
- First urge to defecate
- Maximum tolerable volume
- Rectoanal inhibitory reflex (RAIR)
This is the Rectal Sensation Test in Figure 8. This typically is used in a GI office as well. There are some courses to learn how to do this because we need to be able to test sensation if that is not being done with their physician. This is called the Rectal Sensation Test where they put a balloon in the rectum.
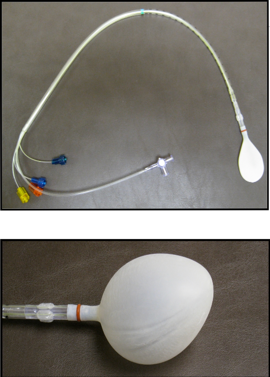
Figure 8. Rectal Sensation Test (Author's image).
They are testing the first sensation as they fill the balloon with air. When does the patient feel that pressure? When do they feel the urge to defecate? They are also able to test something called the RAIR, which is the rectoanal inhibitory reflex.
Digital Rectal Exam.
- This is for the estimation of the tonicity of the anal sphincter which may be useful in the case of fecal incontinence or neurologic diseases.
- To test EAS strength and EAS/IAS resting tone
There is also a digital rectal exam that can be done. The Herman and Wallace and the Pelvic Institute both teach how to do pelvic and rectal exams, especially if you will be working with males. For example, to test the tenacity of the anal sphincter, you can use the digital rectal exam. This will also test the external anal sphincter strength and resting tone. Figure 9 shows an example of what that would look like. You are placing a finger into the rectum to palpate the puborectalis muscle which is attached to the pubic bone and wraps around that rectum. You can also test to see if there is any tenderness.
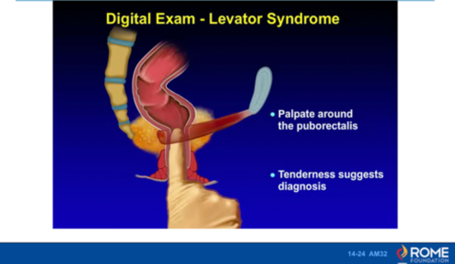
Figure 9. Digital exam.
Transit time studies.
- Colonic marker study to measure colonic transit
- 24 markers ingested
- X-rayed 3-5 days later
- > 20% of rings present after 5 days -delayed colonic transit
Transit time studies are another thing that you might hear your patients talk about. What happens is a patient will ingest a capsule that has 24 markers. Then they are going to be x-rayed to look at how that is moving through their system. (Figure 10).
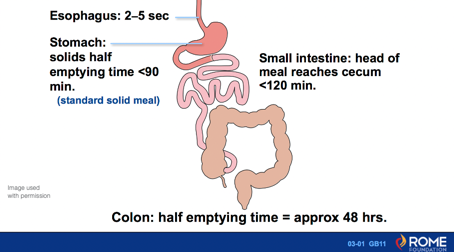
Figure 10. Regional differences in transit along the GI tract.
For example, they know that in the esophagus it takes two to five seconds to get food down. It is then in the stomach for less than 90 minutes, and then it is in the small intestine for less than 120 minutes. The colon should be at the half emptying time in approximately 48 hours. Many patients think that if they eat something, it immediately has an impact on them, but it does take about 48 hours to get through.
During a transit test, we are looking at sitz markers. They may take a look at the movement of these markers on a Monday, Wednesday, and Friday. They are looking for what is called inertia. This means it does not move through as well as it should. This is an example in Figure 11. You can see the markers throughout.
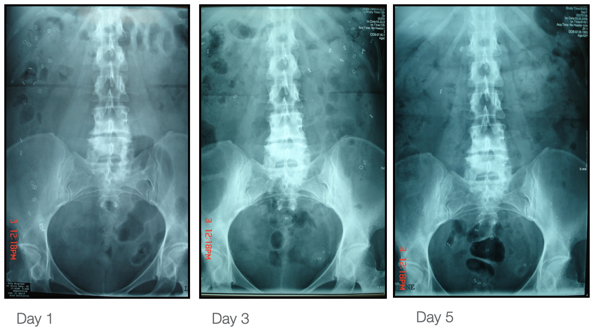
Figure 11. Sitz markers in the system seen via x-ray. (Image used with permission.)
Figure 12 depicts this a little bit better. It is normal that after five days, 80% of the markers should be evacuated. You can see the rings scattered all through the colon.
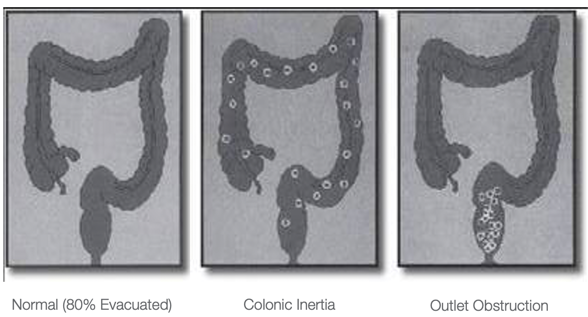
Figure 12. Example of inertia and obstruction. (Image used with permission.)
There is something called outlet obstruction that means all the rings are kind of stuck at the outlet. This could be someone with incoordination issues who do not relax when they are supposed to. They tighten their muscles when they should be relaxing.
Bristol Stool Scale.
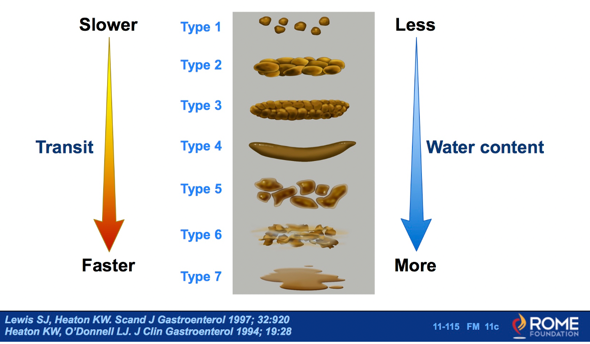
Figure 13. Stool form depends upon water content and correlates with transit time. (Image used with permission).
Many physicians show the Bristol Stool Scale to their patients, and I have it in my office as well. You might also hear Type one, Type two, Type three, and so on. We are shooting for Type four. We want our patients to have a soft and formed stool that is easy to push out. Many patients will think that they are not constipated because they have Type one or small pellets. Even though they might be easy for them to get out, this is the most constipated you can be. Type 2 is cracked showing that they are not getting good water intake.
Fecal Incontinence (FI) or Accidental Bowel Leakage
Common Causes
- Surgical repair procedures
- Fistulas: track of inflammation that bores a hole through tissue
- Fissures: tear or open crack-like sore in the anus
- Hemorrhoids-often from straining
- Neurological causes
- upper or lower motor neurons
- diabetic mixed motor and sensory
- Sphincter trauma
- fecal impaction
- common geriatric problem
- youth, mega rectum or congenital anorectal malformation
- fecal impaction
- Idiopathic constipation
Fecal incontinence is also termed an accidental bowel leakage. One common cause of fecal incontinence is a surgical repair. There can also be fistulas, which is a hole that can go through the rectum. This can be very uncomfortable for patients. You can also get fissures or cracks in the anal area. Hemorrhoids are also common with straining.
- Obstetric trauma
- most common
- sphincter damage- difficult delivery
- delayed pudendal nerve latencies
- Sultan et al 128 woman 1/3-had EAS damage
- Pudendal nerve neuropathy
- Rectal Prolapse
- Hirschsprung’s disease
- children
- anorectal malformation
Another common cause of fecal incontinence is sphincter trauma that can happen during deliveries. A difficult delivery can also cause pudendal nerve damage. There can be a pudendal nerve neuropathy or rectal prolapse as I showed you earlier which is that pocketing of stool. Hirschsprung's disease with an anorectal malformation in children is another one.
Medical and Post-surgical Conditions
- Impaired rectal sensation
- Inadequate EAS contraction
- Poor resting tone of IAS
- Diminished rectal capacity
- Incomplete relaxation or paradoxical contraction with defecation
- Severe constipation (overflow)
If there is fecal incontinence, there can be impaired rectal sensation. There can also be an inadequate external anal sphincter contraction, poor resting tone of the internal anal sphincter, diminished erectile capacity, incomplete relaxation, or that paradoxical contraction. Many patients with severe constipation can have overflow or staining of stool. This can also happen if you are working in pediatrics. Whenever patients or children have stool staining, it is thought that they need their stool bulked up. However, it is the opposite. They are usually compacted with so much stool in there. Ninety-five percent of the time that pediatric clients are leaking stool is because they are extremely constipated.
Impaired Rectal Sensation
- Damage to afferent nerve fibers
- Damage to sensory areas of the brain
- Chronic rectal dilation-constipation
- Lack of appropriate response to normal “sampling”
- IAS relaxation-anoderm in the anal canal
- Options: pass gas, toilet, EAS contraction
- No closure of the distal anal canal with an increase in proximal anal canal pressure
Impaired rectal sensation is another one. If there is damage to the nerve fibers, which of course can start in the brain, they may not get the proper signals. If someone is constipated and they always having rectal dilation, this can impair the rectal nerve, and they will not feel the ability to go.
There may be a lack of appropriate response to normal sampling. This means that if you are going to pass gas or have a bowel movement, then you have that sampling ability. However, some people do not know when they have that feeling. There can also be no closure of the distal anal canal with an increase in proximal anal canal pressure.
Paradoxical PFM Contraction
- Abnormal contraction with defecation attempt
- Outlet obstruction type constipation
- Straining with stool
- Need to assess with fecal incontinence (Rectocele or prolapse repair, hemorrhoidectomy)
- Incomplete emptying, post-defecation seepage
The paradoxical pelvic floor muscle contraction is an abnormal contraction when they are trying to have a bowel movement. Their muscles are contracting when they should be relaxing. You might also hear "outlet obstruction type" of constipation. One time I had a client with this, and I had to remind myself that the person was not releasing. It all goes back to the muscle. If you think about any of these bladder and bowel disorders it has to do with the muscles and are they doing what they are supposed to be doing? Are they holding when they are supposed to or are they relaxing when they are supposed to? Also, if someone is straining, they can be contracting their pelvic floor at the same time that can create that paradoxical contraction. This needs to be assessed with fecal incontinence as there can be incomplete emptying and post-defecation seepage. Many patients say, "Well, after going to the bathroom, I find later that I have a little bit of stool that is stuck in my underwear." We have to be careful with that because if they do not change often, they can get urinary tract infections that have E Coli in it. I make sure that they are very good at cleaning.
Sensory Impairment/Sphincter and Muscle Issues
- Sensory impairment
- Sensory training with manometry biofeedback
- Strengthening assisted by EMG biofeedback to increase stretch reflex of PFM
- Increase stool bulk with fiber-want daily stool
- Deficient EAS
- Sphincter and puborectalis strengthening assisted by biofeedback
- Low IAS tone
- Increase PFM tone and strength to compensate for IAS
- Increase anal canal tone
- Address related constipation
- Avoid bowel irritants
With sensory impairment, you can do sensory training with that manometry that I showed you earlier. You can also do strengthening assisted by EMG biofeedback. I do a lot of biofeedback with these patients. If they have fecal incontinence, I instruct them to increase their water intake as well as fiber. Then, they will not leak as much because it is solid versus liquid. If they have a deficient external anal sphincter, then you want to do strengthening. If someone just has a lot of weakness in the pelvic floor, then you do want them to do that Kegel exercises as long as they do not have pelvic pain. If they have a low internal anal sphincter tone, you want to increase that tone and strength. You want to address related constipation. Constipation is a biggie and if you go into just looking at bladder disorders, you have to remember that at least 20 to 30% of your patients are going to have the bowel disorders along with that. You want to make sure that your clients understand bowel irritants and what they are, so I always review that with my patients. This is just another example of information from the Rome Foundation.
Fecal Incontinence-Moderate Treatment Options (Rome Foundation)
- Fecal incontinence (Moderate)-Treatment Options
- Conservative management should be tried first
- Education about the physiology of continence
- Normalize stool consistency with fiber, or antidiarrheal drug
- Improve the strength of pelvic floor muscles by daily squeeze exercises
- Biofeedback
- Squeeze pressure using instrument-based biofeedback
- Duration of sustained squeeze
- Ability to recognize weaker rectal distentions through sensory training
- Teach deep breathing as a coping skill to counteract anticipatory anxiety and increase tolerance for rectal distention
- Sacral nerve electrical stimulation (neuromodulation)
- Inject inert bulking agent (dextranomer) into the submucosal space to increase resting and pressure
- Surgery, e.g. sphincteroplasty, mesh slings, or colectomy
- Conservative management should be tried first
You always want to talk to your patients about the physiology of continence. I always go over what the muscles are doing as an example. You also want them to normalize that stool consistency with fiber. Of course, I do not give them any drugs or tell them what to take over the counter. I talk more about fiber rick foods and water, and whatever their GI doctor has told them that they can take following that plan. I do not want to change the plan of the GI doctor.
They can work on improving the strength of the pelvic floor muscles via a Kegel program, and biofeedback is fantastic. Some people can also consider using manometry. Anything that is giving the patient information is going to be biofeedback. While I do the EMG biofeedback, manometry is done by a physician. It is also important to do sensory training and deep breathing as a coping skill if they are having anxiety.
Sacral nerve electrical stimulation is performed using an internal sensor either vaginally or rectally (Figure 14).
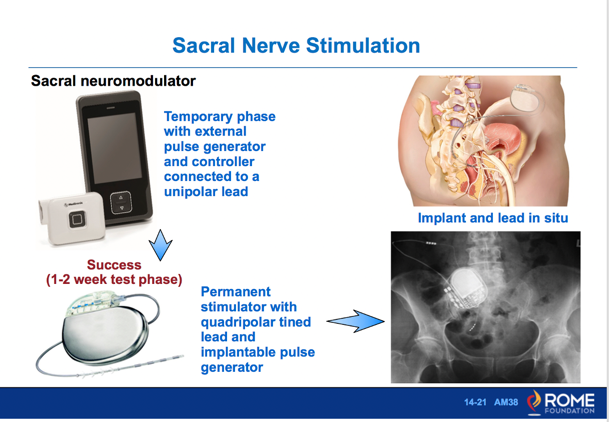
Figure 14. Overview of sacral nerve stimulation.
Some people will only need a bulking agent, while others have to go through surgery. Many times if clients are undergoing surgery, they will get an implant at the same time. The FDA has approved these implants for someone with fecal incontinence. They are implanted under the skin in a low back to give them pulses. They start with a temporary one on the outside, sometimes up to two weeks to see if it is working for them. Then if it is working, they get a permanent stimulator put in to help with the nerves and the functioning of the pelvic floor.
Dietary Factors
Dietary factors are very important.
- Bulky stool stimulates GI peristaltic activity-decreased transit time
- Individual responses to foods
- Offer dietary information as suggestions to try
- Elimination diet approach
Bulky stool stimulates the GI peristaltic activity and decreases the transit time. There are individual responses to foods, and your patients will have different sensitivities. We can offer dietary information and sometimes use an elimination diet approach to see what their trigger food is.
Foods That Can Thicken Stool-Fiber
- Bananas
- Toast
- Potatoes
- Yogurt
- Cheese
- Creamy Peanut Butter
- Apples
- Bread
- Tapioca
- Pasta
- Applesauce
- Rice
These are some of the foods that can thicken stool and have more fiber in them. Bananas, toast, potatoes, yogurt, cheese are some things that can help to thicken stools. However, some can sometimes constipate as well so you have to use it in moderation.
Foods That Can Loosen Stool or Stimulate Bowel Movements
- Warm foods
- Warm drinks
- Fried foods
- Prune juice
- String beans
- Chocolate
- Raw fruits
- Grape juice
- Raw vegetables
Many things will loosen the stool. Many clients will have a cup of coffee in the morning, but if that irritates the bladder, they can drink a cup of warm water or hot water and that will have the same effect on the colon. Fried foods prune juice, string beans, and chocolate will also loosen stool. Chocolate has caffeine in it so sometimes that is a stimulant in itself. Other stimulants include fruits, grape juice, and raw vegetables.
Foods That Can Produce Gas
- Apple juice
- Broccoli
- Beans
- Soda
- Wine
- Cabbage
- Vinegar
- Seltzer
- Onions
- Beer
Many foods also produce gas. If you have someone with flatal incontinence, or an inability to control their gas, they may be ingesting too much of these foods. Some of these include apple juice, broccoli, beans, soda, wine, cabbage, vinegar, seltzer, onions, and beer. Often, these are items that you consume in a group setting so they might want to avoid them is they are having these issues.
Foods That Can Produce Odor
- Alcohol
- Asparagus
- Garlic
- Cabbage
- Fish
- Vitamins / Medications
- Beans
- Onions
These are a list of foods that can cause odor. Asparagus is one that is commonly discussed in this category.
Food That Can Cause Bowel Irritability
- Milk and milk products
- Tomatoes and tomato-based food
- Fried foods
- Greasy foods
- Artificial sweeteners
- Caffeinated fluids (tea, coffee, soda)
- Chocolate
- Eggs
- Salads
- Citrus fruit/juice
- Alcohol
Other foods can cause bowel irritability. I had a lady once who was having a lot of salads and eggs every morning. She had no idea that that could cause some bowel irritability. We eliminated that for two weeks, and she saw a big improvement. I like to show my clients this list to help them understand the problem foods. Not every single one of your patients will be irritated by eggs or salads, but it is good to know which ones might cause some bowel irritability.
High Fiber Foods
- Blackberries
- Beans
- Prunes
- Corn
- Oatmeal
- Nuts
- Pears
- Celery
- Cabbage
- Apples
- Carrots
- Raspberries
- Baked potatoes
- Whole grains
- Dried apricot
- Bran cereals
- Bananas
- Raisins
- Popcorn
- Spinach
- Dried Figs
- Lentils
These are some of the higher fiber foods including berries, beans, prunes, and corn. Pears have a very high fiber count, and they are sweeter than an apple. One of my favorite things to suggest to clients is a Quest bar. These are very high fiber, high protein, and low sugar. You can get them in most grocery stores and on Amazon. They have 15 grams of fiber and only one gram of sugar which is stevia. These are great for diabetic patients. It has been a lifesaver for a lot of my patients. They will have one Quest bar a day, make sure they drink eight glasses of water and use a squatty potty, which I will talk about soon.
Fiber
- How much?
- General recommendation 25-30 grams per day
- American diet 13 grams per day, African 60 grams
- Possibly more with constipation
- How to increase fiber?
- Bran containing cereals (4-5 grams per serving)
- Increase fruit and vegetable
- Cooked beans of all types (4-5 grams per 1/2 serving
How much fiber is enough? The general recommendation is 25 to 30 grams per day. In an American diet, we usually get only 13. It is important to have your patients track this intake. I like to give them a diary to track how much fiber they are getting because that does make a big difference. They can increase fiber with brand cereals, fruits, and vegetables like the Quest bar. If they are not a very good eater, a fiber pill may be a possibility. Beans, of course, also have a lot of fiber in them.
Bowel Recipe
- 1 cup of unsweetened applesauce
- 1 cup coarse unprocessed wheat bran (Miller’s brand) or oat bran
- ¾ cup prune or cranberry juice
*Begin with 2 TBLs every day with a glass of water. Increase to 2 TBLs 2x a day if needed.
There is something called a bowel recipe. Some people call it power pudding, but they have done a lot of research on this actual recipe. I have my clients take two tablespoons every day with a glass of water. It is kind of an oatmeal type consistency. If this does not work, they can go up to two tablespoons, two times a day.
Diet Modification
- Bowel Habit Regulation
- Goal: Regular and predictable
- Adequate Fiber (25-30 grams a day)
- Avoid straining
- Fluids and Exercise
- Regular time
- Heed the Urge
- Avoid constipation
- Bowel Recipe
You want to get them into a routine. The goal is a regular and predictable bowel movement. We also want to make sure they are getting adequate fiber and are avoid straining at all costs as it will weaken the pelvic floor. This can cause a rectocele or rectal prolapse.
Home Exercise Program for FI
- Tailor the prescription to the patient to maximize compliance and eventual success
- 5 sets of 20 contractions, 100 per day (shape up to at least 10 second holds)
- Do sets in a variety of positions (start with reclined, add on sitting and standing)
- Train to contract external sphincter and puborectalis with any sensation of fullness
- Maintain relaxed abdominal muscles (obliques and rectus)
Exercise also helps with peristalsis. A lot of times you can train your bowel to go at the same time every day. It is a very trainable organ and you probably know people who go at 10 o'clock every single morning. Your client must heed the urge meaning if they need to go, then they should go. The more you put off that bowel reflex because you are too busy, then the worse it is. The longer it sits in there, the harder it gets.
- Kegel exercises increase sensitivity to rectal fullness as well as strengthening
- Individualized exercise program
- Home trainer
- Bowel diary for symptom tracking, exercise compliance, dietary factors
For fecal incontinence, I might increase their Kegel exercise program. If they truly have a lot of weakness, instead of the 60 to 80 reps with the urinary or bladder disorders, I might try five sets of 20 contractions. I like the Kegel trainer by Olson apps. We want to increase to at least a 10-second hold. Most of my patients with fecal incontinence can maybe hold for two or three seconds. It is very difficult to hold up to 10 seconds, and it may take them six weeks to two months to get to that point. It can be a very slow progression.
I usually start them in a reclined or lying down position to do their Kegel exercises because they are not dealing with gravity. As they get stronger, you can add in sitting and standing. You want to train them to contract the external anal sphincter and the puborectalis which are the two muscles that we have control over. Some therapists have their clients squeeze their muscles to feel that fullness right before they go to feel that sensation. They want to maintain relaxed abdominal muscles and only use their pelvic floor to do this. However, when they are having a bowel movement, they want to engage their abdominal muscles to increase internal pressure to push that stool out.
There are home trainers and biofeedback home units as well.
Biofeedback
- Used to improve or compensate for:
- PFM/EAS weakness, incoordination, poor endurance, poor rectal support
- Paradoxical contraction (failure to relax)
- Ability to use abdominals correctly to increase abdominal pressure for strain-free evacuation
- Sensory deficits
Source: Jeannette Tries, OT
My very favorite tool, of course, is the biofeedback with this population. We can look at what their pelvic floor is doing. Are they having an overactive pelvic floor? Do they have tension in the pelvic floor when they are supposed to be relaxing? Are they having a paradoxical contraction? The biofeedback teaches them to coordinate their muscles. I put sensors on their abdominal muscles, and I can teach them how to contract the abdominals and relax the pelvic floor. Sometimes patients can learn to do this while they are sitting on the toilet. This is the most functional position, especially with the pediatric population. You can also put external sensors around the anus that measures the activity of the muscle.
Figure 15 is an example of a basic biofeedback screen. The green line represents the pelvic floor.
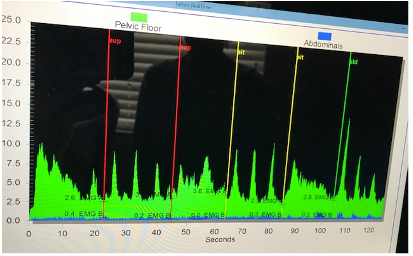
Figure 15. Example of biofeedback.
They are not using a lot of abdominal muscles which is that blue line which is good. They are doing a pelvic floor 10-second contraction and some quick squeezes to check that coordination. Then, we move to a sitting position and that is shown in the third section. Then, standing is at the end in the last box. You can see they do have more control or ability to hold a muscle contraction when they are lying down versus standing. If I am doing the training for the bowel movements, I use the bars because it tracks better for patients where they can see a bar going up and down. I do want to see more blue when they are doing a bear down to engage the abdominals, and I want the green to go down which is pelvic floor relaxing. This works really well with those with coordination issues or that dyssynergia that we talked about.
Biofeedback Goals for Treatment
- Improve selective PFM contraction
- Decrease long-latency to relax after contraction
- Decrease baseline activity
- Decrease paradoxical EAS activity with evacuation maneuvers
- Instruct in bowel management (diet, fluids, gastrocolic reflex)
- Establish a HEP
Source: Jeannette Tries, OT
Biofeedback goals are to improve pelvic floor contractions. I do not want both the pelvic floor and the abdominals to contract at the same time. I try to teach them how to use each muscle, and the baseline activity should be relaxation. You also want them to decrease that paradoxical, external anal sphincter activity when they are trying to release the stool. I also instruct on bowel management, diet fluids, and the gastrocolic reflex. This is important and what that means is that the best time to have a bowel movement is the first thing in the morning. As soon as you stand up, I encourage my patients to walk straight to the bathroom. They usually have to pee so they can do that, and then I want them to eat something immediately to stimulate that gastrocolic reflex. For all of us, the best time to go is first thing in the morning, but you do want to introduce either a warm fluid or food (this works better) so that is part of their homework. They have to eat immediately something, and then they can continue doing what they need to do.
Patient Characteristics and Biofeedback
- > 5 years old
- Motivated
- Sufficient intelligence and memory to understand training
- Defecation reflex response with rectal distention (manometry)
- Some sensation of rectal distention (manometry evaluation)
- BFB overall effectiveness 70-80%
I usually work with patients over the age of five because they have to have the ability to sit for a little bit and focus. It is kind of like playing a video game with their pelvic floor. They are looking at the computer, and we are doing different things with the ultimate goal of training two different muscles. While five is pretty young, it depends upon the maturity of that patient, their level of intelligence, and their memory to understand the training. Some of them will have that manometry done as well. The biofeedback overall effectiveness with this population is 70 to 80%.
Childhood Fecal Incontinence
Overview
- Over the age 4 with leakage
- Encopresis
- Overflow incontinence
- shyness at school, sluggish colon, decongestants, painful fissures
- Pain-vicious cycle
- Paradoxical diarrhea-relaxed IAS and EAS, impaired sensation
- Megacolon and megarectum
- The Poo in You – YouTube video
- It’s No Accident (book by Steve Hodges)
For children, and I talked a little bit about this earlier with fecal incontinence, you almost always want to assume that they are extremely constipated. Sometimes I will see children over the age of four that are having leakage. Their parents often say that they hide their underwear due to staining. Encopresis is the withholding of stool. Many kids hold in their stool because it either hurts or they are scared. However, the more they hold, the more they can have that overflow incontinence.
Many kids are scared to go to the bathroom at school. They are embarrassed and do not want anyone to hear them. So, they start having a lot of problems there, and if it is painful, they are not going to go. Thus, it becomes more and more difficult for them. These kids may also have that paradoxical diarrhea. Additionally, with this, they have impaired sensation. They can also get something called megacolon or a megarectum which means that the rectum gets so overstretched that it is like a floppy balloon. It sometimes takes up to a year to get that back to the normal size.
Many physicians prescribe Neorelax to keep everything moving because these kids get so impacted and constipated that it causes a lot of problems. If you get a chance, I highly recommend watching the Poo in You video on YouTube. It was a nurse that did this video to show kids. I also recommend that you get 'It's No Accident.' It is a book by Steve Hodges who is a pediatric urologist that noticed that many kids were having urinary problems because of constipation problems.
Causes and Rx
- Imperforate anus
- Rare anorectal anomaly
- No opening to outside
- Lack of proper neuronal connections
- Damage during surgical repairs
- Toilet fears
- Severe toilet training
- Treatment
- Behavioral habit training or re-training
- Biofeedback
Other causes for fecal incontinence can be an imperforate anus and so what that means is they do not have an opening. They have an area where the anus would be but there is no actual opening. I can work with these types of patients because they still have muscles underneath that. They can learn how to use their muscles as well. I know that sounds weird but it does work. Sometimes patients have toilet fears or they have had severe toilet training. They do not want to go or they are withholding. One of the treatments is behavioral habit training or retraining using biofeedback.
Biofeedback Treatment
- Biofeedback has been used to train the musculature of the pelvic floor through specific exercises, which, in cases of pelvic dysfunction (synonyms: anismus, paradoxical contraction of the puborectalis muscle, or spastic pelvic floor syndrome), aids the relaxation of this musculature during evacuatory efforts. This approach is recommended for children over 6 years of age and adults. Biofeedback therapy with the aim of training patients to relax the pelvic floor during defecation is appropriately recommended for the treatment of patients with symptoms of pelvic dysfunction.
- Diagnosis and treatment of constipation: a clinical update based on the Rome IV criteria
(Sobrado, Neto, Pinto, & Sobrado, 2018)
There has been a lot of research for biofeedback, and it is used to train the musculature of the pelvic floor through specific exercises. Again, paradoxical contraction is the one that we keep talking about, but we are trying to get these patients to relax their muscles. This approach is recommended for children over six years of age and adults. Biofeedback therapy has the aim of training patients to relax the pelvic floor during defecation is appropriately recommended for the treatment of patients with symptoms of pelvic dysfunction.
Rome IV Diagnostic Criteria For Functional Constipation
- Must include two or more of the following occurring at least once per week for a minimum of 1 month with insufficient criteria for a diagnosis of IBS:
- Two or fewer defecations in the toilet per week in a child of a developmental age of at least 4 years
- At least one episode of fecal incontinence per week
- History of retentive posturing or excessive volitional stool retention
- History of painful or hard bowel movements
- Presence of a large fecal mass in the rectum
- History of large diameter stools that can obstruct the toilet
After appropriate evaluation, the symptoms cannot be fully explained by another medical condition
DiLorenzo et al. (2016)
If you are going to be diagnosed with functional constipation, it must include two or more of the above list.
Constipation
Overview
- The most common digestive problem in the U.S.
- Constipation can lead to:
- fecal impaction
- fecal incontinence
- dilation and even perforation of the rectum
- The normal frequency of bowel movements
- three per week to three per day
- Some constipated individuals have dyschezia (pain)
- Causes can include:
- drugs and medications
- disorders and diseases (stress and depression)
Moving on, constipation is the most common digestive problem in the US, and it can lead to fecal impaction, fecal incontinence, dilation, or even perforation of the rectum. Normal frequency is three times per week to three times per day. Some constipated patients will have pain. Drugs and medications and other diseases can cause issues as well.
Bowel Management Principles
- Daily regular time utilizing the gastrocolic reflex
- Utilize method to reliably empty rectum (reflex, glycerin suppository, enemas, etc.)
- Start training after rectum empty
- Try abdominal massage 10-20 min. after insertion of a suppository
- Pay attention to posture on the toilet
Bowel management principles include a daily regular time utilizing the gastrocolic reflex. I talked about this a little earlier as soon as you get up in the morning. You want to utilize the method to reliably empty the rectum. Some patients will have to use glycerin suppositories or enemas and will need to discuss this with their physician or nurse practitioner. You want to start training when the rectum is empty. Abdominal massage works great with a lot of these patients 10-20 minutes after the suppository is inserted. Lastly, posture on the toilet is extremely important. Sometimes that can take away someone's problem just by sitting correctly.
Causes and Dynamics
- Elevated mean sensory threshold
- Nerve damage
- Megarectum, megacolon
- Rectocele
- Increased pelvic floor descent
- Muscle weakness, lax ligaments, poor funneling of stool
- Anismus-paradoxical contraction of EAS and puborectalis with defecation
- Pain - current or past
- Sexual abuse history
Someone can have an elevated mean sensory threshold. This can be caused by nerve damage, an overstretched rectum, or a rectocele which is that pocketing. They can also have increased pelvic floor descent via either muscle weakness or lax ligaments. Their funneling of stool may not be appropriate. Finally, they can have anismus or a paradoxical contraction of the external anal sphincter and the puborectalis. Some of these patients can have pain either current or past or a history of sexual abuse. This is one area that can transfer to bladder and bowel dysfunction.
- Colonic motility
- Slow transit time
- Diet-low bulk
- low amplitude contractions (most often)
- morning, after awakening, pre-defecation high amplitude contractions occur
- Poor habits
- Delaying call to stool
- Lack of exercise
They can also have colonic motility or slower transit time. This allows more time for the stool to get stuck and hard. Their diet and poor habits can have a big impact on that. They can&
