Introduction
Thank you, everyone. I am glad you tuned in for this one. This is a little bit more of a challenging topic, and it is definitely an introduction. You are going to want to get further training if you treat the pelvic pain population. And, for those of you are back from the bladder and bowel disorders talks, I am glad you are back.
Overview
- Pelvic floor anatomy
- Common PP diagnoses seen in the clinic
- Treatment interventions for pain disorders
- Resources and certification information for women’s health
The overview of the presentation is going to be reviewing the pelvic floor anatomy and common pelvic pain diagnoses as well as treating some of those pain disorders. We will also discuss resources and certification information for women's health.
Pelvic Floor Functions
- Support of organs
- Urethral and anal closure-continence
- Signal to the bladder, rectum, and colon to contract
- Opening of the urethra and anal canal-total relaxation = full emptying
The pelvic floor has many functions. Of course, it supports our organs. It allows urethral and anal closure to keep us continent. It also signals to the bladder, rectum, and colon to contract, and the opening and emptying of the urethra and anal canal require full relaxation of the pelvic floor. Many patients with pain are unable to fully empty and have some difficulties because of that pain.
- Tonic action of PFM
- keeps urogenital hiatus closed
- Contraction of PFM
- squeezes the vagina, urethra, and rectum
- lifts the floor and organs-cephalic direction
- Uterus support-ship in its berth
- ship-uterus
- ropes-ligaments (stabilize the ship)
- water-pelvic floor (if the ship goes down, the ropes have to hold uterus up)
The tonic action of the pelvic floor muscle keeps the urogenital hiatus closed, allows us to contract the pelvic floor muscles, which squeezes the vagina, urethra, and rectum, and lifts the floor and organs towards the head. Think of the uterus support like a ship. The ship is the uterus and the ropes are the ligaments that hold everything in place. The water is the pelvic floor. So, if the ship goes down, the ropes have to hold that uterus up. There are a lot of ligaments in the system as well.
We are going to show a video of a pelvic floor contraction. For those of you who have been to the last two courses, you have seen this and know that this is my favorite video. This is someone lying on their back, legs open.
Video 1: Pelvic Floor Contraction
The urethra sits at the top, the vaginal opening is in the middle, and at the base, you have the anus. When there is a pelvic floor contraction, everything works together. The muscle ligaments are attached to bones, and it works as a system.
Video 2- Side View
In this video, we see a side view of the pelvic floor muscles. This gives us a good idea of how the muscles work as a team.
Thus, if you have tension in any of these muscles, this can cause pain. Think about any tension and muscles anywhere in your body and how that can cause pain. There are three layers of muscles. Keep this in mind as we move on in this talk because everything having to do with pain is typically going to be a muscle or nerve issue.
Purpose of Pain
- Protects you
- Alerts to danger
- Body’s alarm system alerts you to damage
- Makes you move and react differently
We could probably have a lecture for a week on pain, but there are some important things I want to mention. Pain is present to protect you. It alerts you to there is a danger, and it is the body's alarm system alerting you to damage possibly. It makes you move and react differently. For example, if you hurt your back, you will move differently.
Biomedical Model of Pain
- Problem: highly diverse responses to the same treatment for the same disorder
- The identified physical disorder does not predict well the level of pain or disability
- Depression, sleep disturbance, psychosocial disability, and pain are viewed as secondary to the disease or organic problem
- Psychological and psychosocial variables not recognized as contributing factors (Engel,1977)
- Pain is an experience, not just a sensation. I think that is very important to keep in mind.
The problem is that there are highly diverse responses to the same treatment for the same disorder. The identified physical disorder does not predict well the level of pain or disability. There are also people that can tolerate a lot of pain and those that cannot, thus each patient is going to present differently. Pain can cause depression, sleep disturbances, and psychosocial disability. Pain is often viewed as secondary to the disease or organic problem. Psychological and psychosocial variables are also not recognized as contributing factors.
Pain Education
- Resource: “Why Pelvic Pain Hurts” by Adriaan Louw
- https://www.amazon.com/Pelvic-Pain-Hurts-Adriaan-Louw/dp/0985718684
It is very important to have pain education. There is a book by Adrian Louw called "Why Pelvic Pain Hurts." It is a great book, and I have my patients read it. Your patients need to understand what pain is, because they may not even have the reason for that pain anymore due to the pain cycle they are experiencing. There is a lot of research showing that if you provide just 30 minutes of education to your patients about pain that this will significantly reduce that pain.
Pain Transmission
- Pain-subjective response to the perception of noxious stimuli
- Peripheral receptors
- Afferent fibers to the spinal cord
- Ascending tracts in the spinal cord to synapses in midbrain, pons, and diencephalon
- Reflex arcs along the way initiate aversive behaviors
- May or may not reach the limbic and somatosensory area of the cortex to sense PAIN
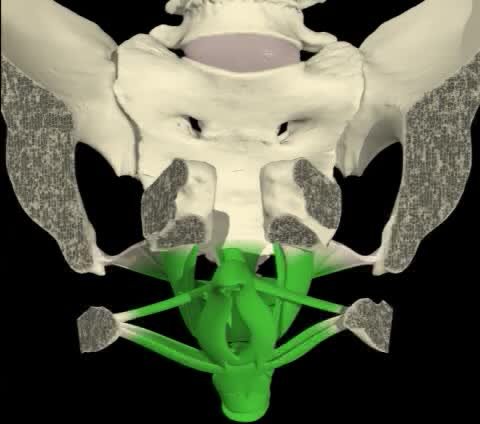
Pain is a subjective response to the perception of noxious stimuli. There are peripheral receptors send a signal to the afferent fibers in the spinal cord that ascend and synapse in the midbrain, pons, and diencephalon. Reflex arcs along the way initiate aversive behaviors. These may or may not reach the limbic and somatosensory area of the cortex to sense pain. We know pain is a very complicated topic so it definitely deserves more study. Figure 1 shows the transmission of pain.
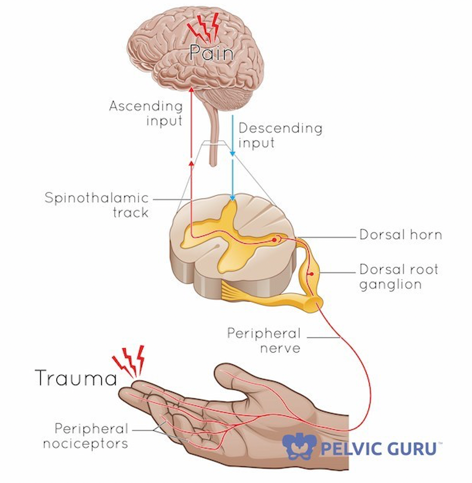
Figure 1. Overview of pain transmission. (Image used with the permission of Tracy Shur, the Pelvic Guru.)
Chronic Pelvic Pain (CPP)
Overview
- persistent pain of unexplained nature in lower abdominal and pelvic area
- lacks apparent physical cause to explain the pain
- six or more months in duration
- affects physical activity, work, family and social life in a negative way
- pain located in pelvis, genitals, abdominal, coccyx, sacral and/or lower back
- referred pain to legs is common
With chronic pelvic pain, it is persistent pain of unexplained nature in the lower abdominal and pelvic area. It lacks apparent physical cause to explain that pain. To have a chronic pelvic pain diagnosis it has to be six or more months in duration and affects physical activity, work, family, and social life in a negative way. When people ask why is OT involved with chronic pelvic pain, this is the reason. It affects our patients and their daily activities. Pain can be located in the pelvis, genitals, abdomen, or coccyx, which is your tailbone, sacral, and/or lower back. A lot of these patients can have referred pain to the legs as well.
- Definition:
- Nonmenstrual pain > 6 months
- Localized in pelvis
- Functional disability and medical or surgical treatment
- Complex etiology
- Various associated problems
- Bladder and bowel
- Sexual dysfunction
- Depression, anxiety, drug addiction
The definition is non-menstrual pain of more than six months localized in the pelvis that causes functional disability or requires medical or surgical treatment. It is also complex. These are the most difficult patients that I treat outside of anything with the pelvic floor. The various and associated problems can be with the bladder and bowel or sexual dysfunction. Clients can also have depression, anxiety, or drug addiction.
CPP Intake
- Pain characteristics
- Location (pain diagram)
- Precipitating factors (intercourse, posture, time of day)
- Alleviating factors (rest, heat, stretching, exercise)
- Quality (throbbing, pounding, shooting, pricking, boring, stabbing, burning, splitting, penetrating, etc.)
- Distribution (radiations)
- Intensity (pain scales)
- Onset and frequency
There are some great pain diagrams. I like to give one to my patients to mark where are they having the pain. We can also do a pain diagram. What causes the pain? Is it because they just had intercourse, and they have pain for either an hour after or maybe a day later? When do they have the pain? Is it in the morning? Is it in the evening? We can take a look at their posture. What alleviates that pain? Does rest, heat, stretching, and/or exercise help? We can also look at the quality of the pain. Is it throbbing, pounding, shooting, pricking, boring, stabbing, burning, splitting, or penetrating? I have a list of these symptoms for patients to pinpoint what they are feeling. There is also definitely going to be a distribution, and we will go over that in just a minute. We can look at the intensity using a pain scale. And, we want to know the onset and the frequency of the pain?
Associated Systems and Disorders
- Gynecologic and obstetric
- Urological
- Gastrointestinal
- Musculoskeletal
- Neurologic
- Psychological
Are there associated systems and disorders? Usually, there is a gynecological or obstetric problem. We need to look at all associated areas like urological, gastrointestinal, musculoskeletal, neurologic, and psychological.
Problems Associated with CPP
There are a lot of things that can be going on along with that chronic pelvic pain.
- low back pain
- constipation
- voiding dysfunction, urgency, frequency, low stream force, hesitancy
- poor sitting or standing tolerance
- dyspareunia (painful intercourse)
- lack of orgasm
Above are problems that are usually associated are low back pain. Many have pain with constipation. There is also a voiding dysfunction. Again, if you are having problems with the muscles of the pelvis, you can definitely have that voiding dysfunction. Urgency frequency with a low stream is one sign. They may even have hesitancy during a stream of urine. Poor sitting or standing tolerance are other signs. They tend to stand in your office or they have to lay down, but often, they do not want to sit as it is very uncomfortable. Some of these patients have dyspareunia, which is another word for painful intercourse. And, some have a lack of orgasm due to chronic pain.
Modalities for Pain Reduction
- Moist Heat - used for trigger points, spasm, soreness, to increase circulation
- Cold treatment – inflammatory conditions, decrease pain and spasm, swelling, hemorrhoids
- TENS – pain, spasm, pelvic or perineal pain, vulvodynia, coccygodynia
Here are some modalities for pain reduction. Some patients do well with moist heat, while others like a cold treatment. It just depends on each patient and what is going on for them. I have had many patients get a lot of relief from a TENS unit. There are many different ones that you can find, but the ones I see/use in the clinic are the ones that I will be discussing. First, I want to review the anatomy.
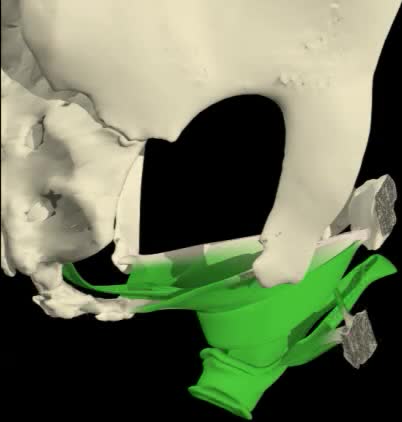
First, I want to show you the pelvic floor anatomy (Figure 2).
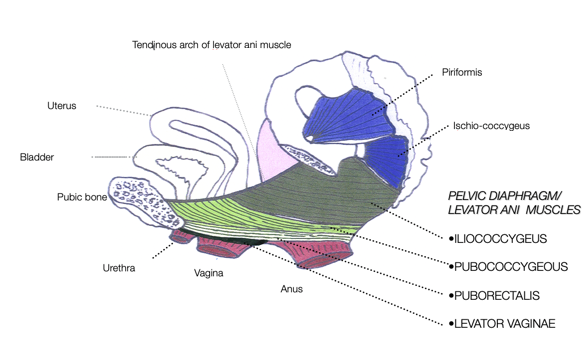
Figure 2. Female pelvic diaphragm. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission.)
The urethra, vagina, and anus are all three muscular tubes. All of the green depicts different pieces of the pelvic floor. There are three different layers. The hips are involved as well. We are also going to talk about the piriformis and the obturator internus as we get along into this. If you are looking from below, you can see that there are a lot of muscles involved, and one of them in particular can cause problems with the pelvic floor when someone has pain with intercourse as seen in Figure 3.
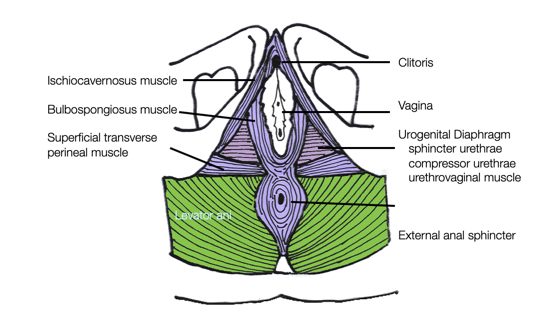
Figure 3. Female superficial perineal muscles and urogenital diaphragm. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission.)
- Bulbospongiosus
- It is one of the superficial muscles of the perineum. It has a slightly different origin, insertion, and function in males and females. In males, it covers the bulb of the penis. In females, it covers the vestibular bulb.
- In both sexes, it is innervated by the deep/muscular branch of the perineal nerve, which is a branch of the pudendal nerve.
The bulbospongiosus is oval-shaped and goes around the vaginal area. This muscle is very interesting as it has been called the "guarding muscle" in a lot of research studies. Its job is to protect. So if someone has a painful experience, whether it be trauma or the first time that they have intercourse, or maybe it is even a pelvic floor exam by their physician, that muscle remembers that hurt last time, and the next time it will fire and make sure that nothing gets in. When this happens, it is very difficult to have intercourse, insert a tampon, or have a medical exam. Keep this in mind as we talk about this muscle. Again, the bulbospongiosus is the one that surrounds the vagina and is a superficial muscle of the perineum. It has a slightly different origin, insertion, and function in males and females. In males, it covers the bulb of the penis and in females, it covers the vestibular bulb. In both sexes, it is innervated by the deep muscular branch of the perineal nerve, a branch of the pudendal nerve. If you start treating pelvic pain and become a specialist in this area, this is a nerve that you will need to understand.
Pudendal nerve
- The pudendal nerve is the main nerve of the perineum. It carries sensation from the external genitalia of both sexes and the skin around the anus and perineum, as well the motor supply to various pelvic muscles, including the external urethral sphincter and the external anal sphincter. If damaged, most commonly by childbirth, lesions may cause sensory loss or fecal incontinence.
The pudendal nerve is the main nerve of the perineum. It carries sensation from the external genitalia of both sexes, and the skin around the anus and perineum as well as the motor supply to various pelvic muscles, including that important external urethral sphincter and external anal sphincter. If it's damaged most commonly by childbirth lesions may cause sensory loss or fecal incontinence. We talked about that last time.
- Pudendal nerve pain distribution
- Trigger points may refer pain:
- Bulbocavernosus and Ischiocavernosus refer pain to the perineum and adjoining urogenital structures
- External anal sphincter refers to posterior pelvic floor
- Levator ani and coccygeus refer to the sacrococcygeal area
- Levator ani to the vagina
- Obturator internus to the vagina and anococcygeal area
- Trigger points may refer pain:
Trigger points can also refer pain. If you are working with other muscle groups in the body you know this already. The bulbospongiosus or cavernous can refer pain to the perineum. The external anal sphincter can refer pain to the posterior pelvic floor and the levator ani, which is a muscle support system in the pelvis. The coccygeus can refer to the sacrococcygeal area, the levator ani to the vagina, and the obturator internus is a deep hip muscle that can refer pain to the vagina and the anal coccygeal area. Figure 4 shows an example of pain distributions.
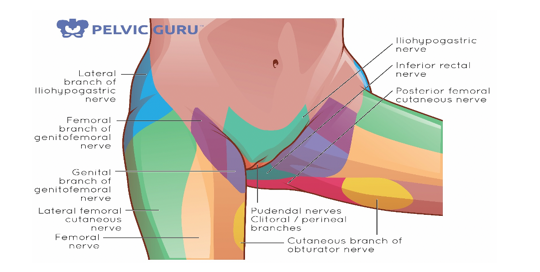
Figure 4. Pain distributions. (Image used with permission of Tracy Sher.)
This shows all the different types of branches and where someone can have referred pain. It is important to understand the chart. If someone is telling you that they have pain in a specific area, you can kind of look back and see what nerve or what branch of that main nerve could it be affecting.
Chronic Pelvic Pain Syndromes
Pelvic Muscle Myalgias
- High resting tone in levator ani, coccygeus, medial fibers of the gluteus, piriformis, and/or obturator internus.
- Pain around the rectum, low back, vagina, coccyx, posterior thigh
The piriformis and obturator internus are very important muscles. As OTs, we do not do a lot of lower extremity work, but when you get into the pelvic floor arena, you will need to learn more about the hip and the pelvis and how they interact with each other. These muscle masses can cause pain around the rectum, low back, vagina, coccyx or tailbone, and the posterior thigh.
Causes of pelvic muscle myalgias.
- Inflammation
- Trauma to sacrum or coccyx
- Pelvic fractures
- Referred pain from trigger points
- Infections
- Post-surgical consequences
- laminectomy or hysterectomy
- Rectal dysfunctions
- fissures, hemorrhoids
Some causes could be inflammation. If someone has trauma to the sacrum or coccyx or has a really hard fall on their tailbone, this can cause problems in the future. Pelvic fractures, referred pain from trigger points, and infections can also cause this. Post-surgical consequences and rectal dysfunctions are also things to assess. For example, a fissure or hemorrhoid can cause muscle pain.
Levator Ani Syndrome
- Puborectalis syndrome
- Pain and pressure in rectal and/or vaginal area
- Defecation can trigger pain
- An elevated resting tone in the pelvic diaphragm
- Defecation-voiding problems
Levator ani syndrome can also be called puborectalis syndrome. That is that muscle I showed you when you looked at the video. It wraps from the pubic bone around the rectum and back to the pubic bone. It is a looping muscle that can cause pain and pressure in the rectal or vaginal area. Some patients will say that bowel movements trigger this pain and then it goes away afterward. They can also show an elevated resting tone in the pelvic diaphragm. You can see that on surface EMG biofeedback. Many patients have problems with defecation and voiding because of this pain.
Causes of levator ani syndrome.
- Pelvic surgery
- Pelvic inflammation/infection
- Sexual assault
- Strenuous physical activity
- Lumbar disc surgery
- Childbirth trauma
Different causes include pelvic surgery, inflammation, sexual assault, strenuous physical activity, lumbar disc surgery, or childbirth trauma. To complete this type of pelvic floor work, you have to get further training. Figure 5 shows an example of a digital exam.
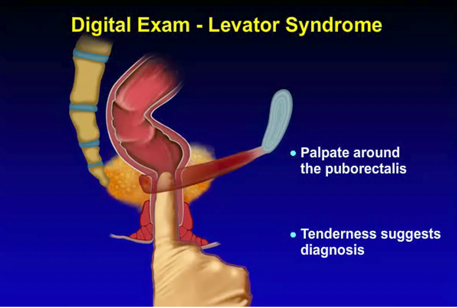
Figure 5. Example of a digital exam. (Image used with permission of the ROME Foundation.)
This is palpating the puborectalis muscle. If the patient says they have tenderness there, this is one sign of chronic pelvic pain.
Chronic Proctalgia Syndrome
A 45-year-old secretary complains of almost constant rectal pain and difficulty sitting. She is uncertain when it began but it is worse since her divorce one year ago. She appears anxious. Her bowel habits are normal. Colonoscopy was negative. GYN consult was negative. Physical exam reveals tenderness when pressing on the levator ani muscles and difficulty relaxing pelvic floor muscles when straining, otherwise normal. The balloon evacuation test was abnormal. The patient rates the impact of these symptoms on her life as moderate.
A. Categorical Diagnosis: Functional anorectal pain
B. Clinical Modifier: Levator ani syndrome
C. Impact on Daily Activities: Moderate
D. Psychosocial Modifier: Anxious
E. Physiological Features and Biomarkers: Levator tenderness, abnormal balloon evacuate test, paradoxical contraction of the external anal sphincter.
Used with permission of the Rome Foundation.
This is an example of someone with chronic proctalgia or anorectal pain via a case study put on by the Rome Foundation.
- Treatment Options
- Levator Ani Syndrome
- Anorectal biofeedback
- Alternative methods would include electrical stimulation to relax pelvic floor striated muscles
- Anxiety disorder
- Muscle relaxing drugs (e.g., baclofen, cyclobenzaprine) offer little benefit
- Referral to psychologist or psychiatrist
- Levator Ani Syndrome
*Functional Anorectal Pain (Chronic Proctalgia)- (Moderate)- Rome Foundation
One treatment option is biofeedback. You could do that either the manometry type or the surface EMG. Some patients benefit from E-stim to the pelvic floor. And of course, there are some drugs that they can be prescribed for anxiety. I actually saw a patient this morning that has a lot of anxiety and pain, and she started seeing a psychologist and started feeling much better. It is important that you have a good system that you can send patients to or clinicians that you trust.
Piriformis Syndrome
- pain in buttocks into the rectal area
- referral to the posterior aspect of the thigh
- may mimic disk problem
The piriformis syndrome is a pain in the buttocks into the rectal area and a referral to the posterior aspect of the thigh. It could mimic a disc problem. If you look at where the piriformis is in Figure 6, the sciatic nerve goes in between two muscle bodies.
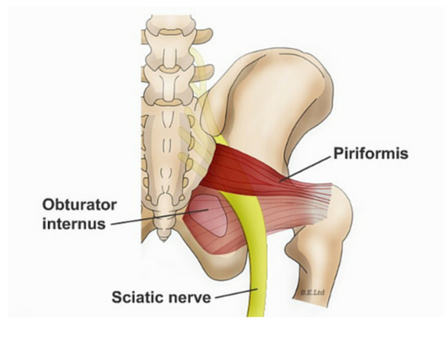
Figure 6. Sciatica due to piriformis syndrome. (Image used with permission of Tracy Sher.)
If you have tension in this muscle, you can imagine how much discomfort that can cause. This is something that typically PTs work on, but if you get into pelvic floor therapy as an OT you would be doing some of this work as well.
Coccydynia
- Pain around tailbone (coccyx)
- falls, arthritic changes, childbirth, spasms of coccygeus or piriformis muscles, neuralgia, malalignment
There is also something called coccydynia, and this is pain around the tailbone. This can happen with falls, arthritic changes, childbirth, spasms, neuralgia, and malalignment.
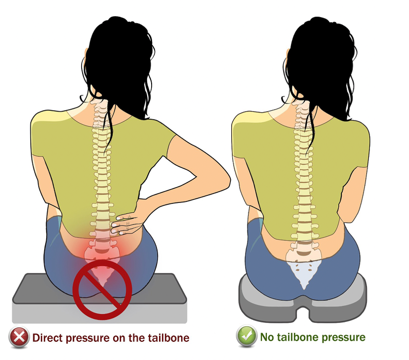
Figure 7. Coccydynia. (Image used with permission of Tracy Sher.)
Some people can have coccyx adjustments, and you can learn that as well. I like my patients to get a seat cushion that has a cutout for the tailbone as it really relieves their pain. I have three different kinds I keep in my office. So, if someone comes in with pelvic pain, I have them try each one while we are talking to see if it helps.
Vaginismus
- Pain, spasm around the vagina with penetration
- An elevated tone of the urogenital diaphragm and levator ani
- Sexual problems
- Involuntary spasms outer area of the vagina
- Atrophic vaginitis- thinning and decreased lubrication, fistula
- Psychological, past trauma
Dr. Oz had a whole series on vaginismus, and he called it the vaginal panic attack. I thought that was interesting because it is really the muscle that we talked about earlier. The muscles of the vagina actually will spasm or contract when there is a possibility of penetration. This is also going to increase the tone of the urogenital diaphragm. This can cause sexual problems as you can imagine due to the involuntary spasms on the outer area of the vagina. Some women have vaginismus because they have atrophic vaginitis as they get older due to the thinning of the tissue and do not have as much lubrication. They could also have something like a fistula. Past trauma could also be a cause. I have had many patients who, once they got married and were in a really healthy relationship, have had difficulty with intercourse due to this past trauma. Figure 8 shows the different muscles from below.
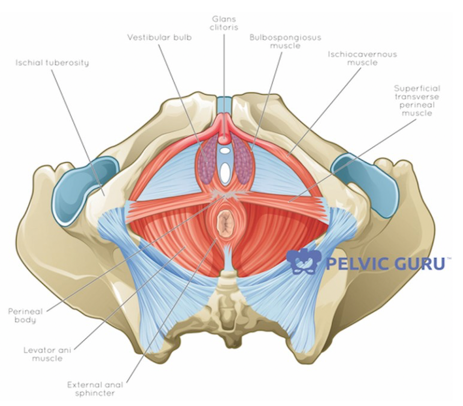
Figure 8. Pelvic floor muscles. (Image used with the permission of Tracy Sher.)
The bulbospongiosus muscle is the one that causes them the most grief.
Dyspareunia
- Vaginal and lower pelvic pain associated with vaginal penetration
- Intermittent or persistent
The word dyspareunia is just a fancy word for pain with intercourse. It can be vaginal or lower pelvic pain associated with vaginal penetration. Sometimes it is intermittent and sometimes it is persistent. Typically these patients do not have pain until intercourse.
- The location and frequency of pain with dyspareunia may vary. Symptoms often include:
- Pain at the entrance of the vagina with initial penetration; even from penetration from a finger or tampon
- Deeper vaginal pain with the thrusting of the penis
- Pain may be sharp and burning, or deep and aching
- You may also experience an involuntary tightening of the pelvic floor muscles (vaginismus) during penetration. The tightening can be severe enough that the vagina is unable to be penetrated.
The location and frequency of the pain may vary. Symptoms may often include pain at the entrance of the vagina or with initial penetration, even from a finger or a tampon. They can have deeper vaginal pain with thrusting. Some patients even have painful muscle knots that are being aggravated within the vagina. The pain can be sharp, burning deep, or aching, and they may also experience the involuntary tightening of the pelvic floor muscles, which is the vaginismus during penetration. The tightening can be severe enough that the vagina is unable to be penetrated. Some of my patients cannot even insert a Q-tip. You have to work very slowly with these clients.
- Dyspareunia/Vaginismus Tests and Measures
- Pain scales (visual analog or symptoms)
- Questionnaires (V-Q Vulvar Functional Status or FSFI Female Sexual Function Index)
- Pelvic floor and perineum exam
- Postural / musculoskeletal evaluation
- Pelvic alignment
- Lumbar mobility
- Abdominal wall length
- Strength and scar mobility
- External and internal exam if indicated
- Refer to pelvic floor therapist if not in the scope of practice
Again, there are pains scales and questionnaires that I will share shortly. You can perform a pelvic floor and perineum exam. Again, you would have to go to training for this, but there are some great courses. You need to check for other pain sources. It could be a skin condition that would need an MD referral. Also, you want to look at their posture. How is their alignment? Do they have good lumbar mobility? What does the abdomen look like? Do they have any strength there? Scar mobility is important if some of your patients have had episiotomies, especially with cutting and stitching in the perineum. You can refer to a pelvic floor therapist if this is not in your scope of practice.
- Dyspareunia/Vaginismus Manual Therapy
- Soft tissue mobilization-manipulation of soft tissue encapsulating a joint, called fascia, and muscles over joints that have restricted range of motion
- Connective tissue and trigger point release-TPs are hypersensitive areas which keep a portion of the muscle or surrounding soft tissues contracted
- Dry needling technique-multiple advances of a filament needle into the TP which deactivates the TP, reducing pain and restoring normal length and function
- The neural tension-the inability of a nerve to move freely within our body. The therapist can manually work along the path of the affected nerve to “free” it and improve circulation
- Visceral mobilization-addresses the body’s internal organs and tissues that anchor them to one another and to the skeletal system
- Manual lymph drainage-stimulate the flow of lymph from an affected area
- Joint mobilization-type of passive movement of a skeletal joint, usually aimed at the synovial joint (the most movable type of joint)
Manual therapy includes soft tissue mobilization, connective tissue, and trigger point release, some people are doing dry needling, neural tension, which is the inability of the nerve to move freely with the body. So the therapist is manually working along that that path of the affected nerve to free it up. Other things are visceral mobilization. They have got some great courses that will help keep things moving in the pelvis, manual lymph drainage, and joint mobilization. This is an example of internal work in Figure 9.
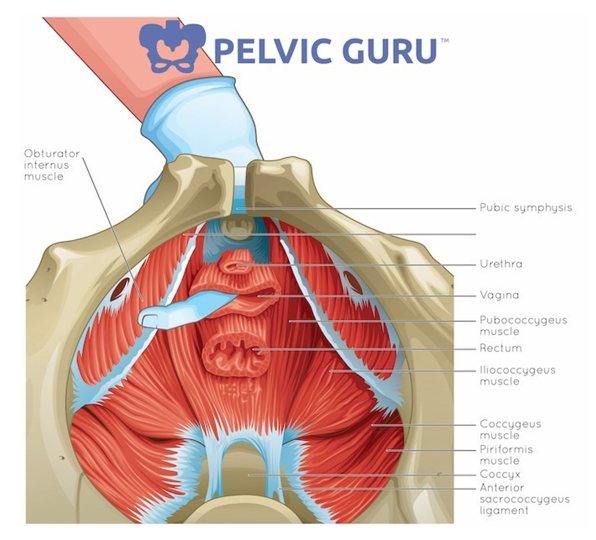
Figure 9. Example of manual therapy. (Image used with permission of Tracy Sher.)
There are many muscles in the pelvic floor. Sometimes the only way to give relief for pain for patients who have muscle trigger points, muscle knots, discomfort, or scar tissue is to internally work with the muscles. Many OTs and PTs are already doing this work out there, and it is extremely important for patients with pelvic pain.
- PRM Relaxation Training
- You would expect to see a poor and delayed return to baseline on sEMG.
- Physiological Quieting (Janet Hulme)
- Guided Imagery CD
- Visualization
- Breaking learned muscle tension (ex. Falling down the stairs, now always tense at top of stairs)
- Use small dilator so less painful (less bracing)
- Use words that work for your patient (relax, let go, melt, etc.)
Pelvic floor muscle relaxation training is definitely in our scope of practice. I do service EMG biofeedback when they have poor and delayed return to baseline. If I want them to try to quiet that muscle or they have a hard time letting the muscle go, I use this. There is also something called physiological quieting. With this, we are trying to get that parasympathetic nervous system to calm everything down. You can do guided imagery or visualization to help them learn how to break that muscle tension. For example, if you had a fall down some steps, every time you came to these steps, you might brace yourself. These patients with pelvic muscle pain have the same response. They do not want to insert anything as they feel that it is going to hurt. They may not really relax when you say that word relax either. It is important to find the words that allow your patients to let go or are trying to relax their pelvic floor.
- Diaphragmatic breathing (abdominal breathing)- inhale belly rises, and PF relaxes downward
- Body scanning- notice tension in PF throughout the day
- Motor imagery- mental practice visualizing pain-free intercourse
Diaphragmatic breathing is so important because the pelvic floor and the diaphragm are interconnected. Three-dimensional breathing gets everything moving so that they are not stuck. Body scanning is also fantastic. You can do body scanning from the head all the way to the feet to really notice tension in the pelvic floor throughout the day. I have my patients do a pelvic floor check. If they are sitting at the computer all day with their shoulders elevated, they may get neck pain. It is important that they recognize this and relax and perhaps massage their neck. I also have them do pelvic floor checks several times a day. You can also teach them motor imagery and mental practice where they visualize pain-free intercourse if that is their issue. Figure 10 shows a picture of the diaphragm and the pelvic floor and how everything is connected.
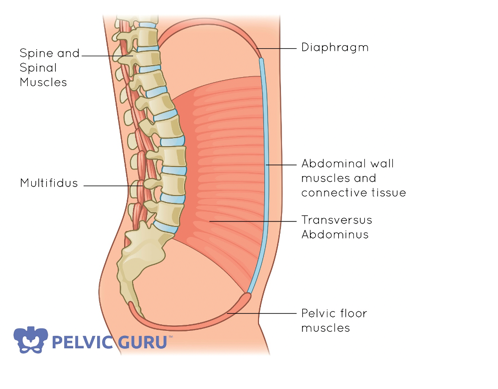
Figure 10. Diaphragm attached to the pelvic floor (Image used with permission of Tracy Sher.)
It is really important to understand the core when you get into the pelvic floor work because it all works together as a team.
- Perineal Bulging
- Doesn’t work if the patient has incoordination
- The patient places a hand on perineum/EAS while gently bearing down (gas)
- Tissues should bulge into the patient’s hand
- Hold 1-2 seconds and relax
- Repeat 5 times
- On EMG you will see a decrease in signal
There is also something called perineal bulging. The perineum is the soft skin between the vagina and the anus. This can work for men and women. For the man, it is going to be above the anus. If they have a lot of muscle tension you can have them do a little bit of bulging. This is not straining, but they're learning how to relax that pelvic floor. If they have in coordination and they cannot release the muscle, this is not one that you would do with them. They gently place their hand on the perineum or the external anal sphincter while they are gently bearing down as if they are passing gas. With this, you can feel the tissue bulge a little bit into the finger of the hand. Sometimes, if your patient is clothed and they give you permission you can place your hand there, you can feel that bulging and make sure they are doing it correctly. They hold it one to two seconds and relax, and repeat five times. And, if they are doing it correctly on an EMG, you will see the signal go down.
- Dyspareunia/Vaginismus Treatment
- Anatomy and role in sexual function
- Knowledge of sexual response-sex therapy consult if needed
- Lubricants
- Perineal massage and mobility
- Dilators with or without BFB (vaginismus.com)
- Ultrasound for scars and perineal ice packs
- Pelvic floor muscle awareness exercise
- BFB-resting, stability, up/downtrain, dilator with surface electrodes
- Manual techniques (perineal stretching/massage or positional releases)
There are other treatment ideas for painful intercourse or vaginismus as noted above. I spend a lot of time teaching anatomy and how important that is for sexual function. You also have to have knowledge of sexual response. They may need a sexual therapist, and it is important to refer them if that is the case. I do not want to send them to someone that that doctor does not normally send to so I make sure I talk with their physicians.
Lubricants are a whole other lecture. Make sure that you have really good natural paraben-free water-based lubricants because some of those KY jellies are not great for the tissue of the vaginal canal. Lubricants are important to discuss, and if anybody is interested I have some good information on that.
Perineal massage is something you can teach your patients. Dilators are something that can also help with stretching. You can do an ultrasound for scars, use ice packs, and teach pelvic floor muscle awareness exercises. Many of these patients have never even looked at their pelvic floor, thus they do not have a lot of awareness. They do not want to know anything about it. The more you teach them the more they can have control. When you do biofeedback, you are looking at the stability and their ability to relax and contract that muscle. You can use a dilator at the same time, and I will go over that. Finally, there are manual techniques that we have talked about already, along with some stretching massage and positional releases.
- Resource: Sex Without Pain: A Self-Treatment Guide To The Sex Life You Deserve by Heather Jeffcoat, DPT
- https://www.amazon.com/Sex-Without-Pain-Self-Treatment-Deserve-ebook/dp/B00K7IH67U
There are so many different dilators out there. You would be very surprised at how many sets are out there. Figure 11 is an example of one with a handle.
Figure 11 is an example of a dilator set.

Figure 11. Dilator set (Image used with the permission of Earl Carlow and www.cmtmedical.com)
You can see that they go from small to large, and you connect it to that blue handle. I always have patients start with the smallest. Even if someone holds it in their hand before treatment, this will automatically give them a muscle spasm. So, it is a very slow process, and most of my clients do this at home. I talk about it in the office so that they have a good plan if they are feeling uncomfortable.
I also like the book called "Sex Without Pain," that a pelvic floor physical therapist wrote it. Keep in mind the vagina is a muscular tube. If you need to stretch something that is like a cylinder then you have to put something in there to stretch. Some of my patients work to build their way up. Sometimes, they can keep a dilator in for 15 minutes once a day. To do so, it should not hurt and should be just a stretch feeling. If they have scar tissue from an episiotomy, they can also use this handled dilator for stretching.
If I am not able to see them in the office, I will prescribe the book and the dilator program if I have already talked with the physician and they know what I am giving the client. There are also plastic dilator sets and really soft ones in many different sizes and shapes.
The two lubricants that I do recommend are in Figure 12. The one on the left is called Slippery Stuff. You can get it on Amazon or through cmtmedical.com. They are a great company and all they do is pelvic floor supplies. If I am doing any pelvic floor work I use Slippery Stuff because if anyone has allergies it is very safe.

Figure 12. Lubricants (Image used with the permission of Earl Carlow and www.cmtmedical.com).
- Sexual Desensitization
- Have patient use dilator at home especially before intercourse
- Lidocaine or Valium suppository if needed
- Gradually increase dilator size
- Moving dilator while in control
- Have a partner hold dilator
- Play “dates” with no penetration
- Sexual positions that are less painful
- Gradual exposure to penetration
A dilator can also be used for sexual desensitization. They can use a dilator to stretch before intercourse. Some physicians also prescribe lidocaine or valium suppositories. They actually put the valium pill in the vagina, and that will calm everything down. They need to wait about 30 minutes before intercourse. You can also gradually increase the dilator size as it becomes more comfortable to the patient. The patient would move the dilator while they are in control and the muscle responds to the actual person. If I have pelvic floor pain, it makes sense that I am not going to hurt myself with a dilator. Your patients would do this once they are at home and have been trained. Again, it is very difficult if someone else does it because that will increase the muscle tension. After they have gone through all the dilators, they can then have their partner hold the dilator. It is important to keep intimacy up. For couples that are having difficulty, I recommend them to have play dates without penetration as we want the muscle to trust the partner again. There are also many sexual positions that are less painful. The client needs to determine these and also go slow with the gradual exposure to penetration.
- EMG Down-training with Dilator
- Use external electrodes
- The patient will start with placing dilator on outside of the vaginal canal
- Always pause if there is pain and wait until ready to continue
- Patient attempts to insert fully while watching EMG
- Once successful, the patient can try to move dilator in and out slowly
There is also EMG down training with a dilator. With these patients, I would use external electrodes. The electrodes would go around the outside of the anus, and the patient would just hold the dilator on the outside of the vaginal canal. They are not inserting at all. And then sometimes, you can see the EMG spike immediately just by having something placed near the entrance. If there is pain, you always want to pause for pain and wait until that person is ready to continue. The patient can watch the screen and insert the dilator while watching the EMG in order to keep everything calm. Of course, if this patient is uncomfortable, you can leave the room and have the EMG running in the background. It can be recording, and then you can come back when they are ready. You guys can talk about what they saw on the computer and how they calmed their muscles down.
Surface EMG Biofeedback
This is an example of surface EMG biofeedback in Figure 13.
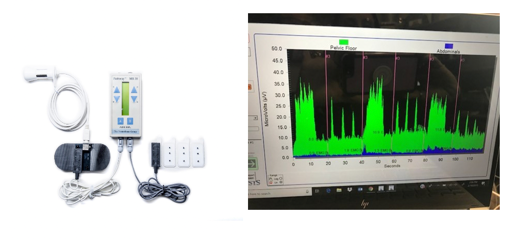
Figure 13. Surface EMG Biofeedback (Image used with the permission of Earl Carlow and www.cmtmedical.com)
The green lines are pelvic floor, and the blue ones are the abdominals. Typically, with someone who has an overactive pelvic floor, they are going to have solid green all the way across as they have difficulty releasing that muscle. You would not see the nice up and down movements. You would just see a solid green line all the way.
On the left is a Pathway MR20, a two-channel system. If you are going to be doing biofeedback, especially as an OT, you will want to get board certified. On this machine, there are two channels, and it uses the telesis software. There are other companies out there and other software. It does not matter to me what software someone has, I just want them to know how to use it. There are sensors for both the abdomen and vagina.
Pudendal Neuralgia
- It can affect both men and women. The pudendal nerve runs through your pelvic region, including your genitals, urethra, anus, and perineum. Your perineum is the area between your anus and genitals.
- The condition is also known as pudendal neuropathy, pudendal nerve entrapment, cyclist's syndrome, pudendal canal syndrome, or Alcock's syndrome.
We talked about the pudendal nerve and how important it is to the pelvic floor function. Pudendal neuralgia can affect both men and women. The nerve runs through your pelvic region, genitals, urethra, anus, and the perineum can be affected. This condition is also known as pudendal neuropathy, nerve entrapment, and cyclist syndrome as a lot of cyclists will get this. During cycling, this nerve gets compressed. This is when you will see pudendal canal syndrome or Alcock canal syndrome in men. Figure 14 is an example of the pudendal nerve and its distribution.
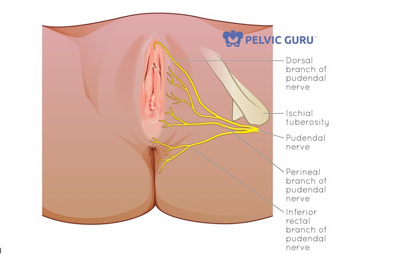
Figure 14. Pudendal nerve distribution. (Image used with permission of Tracy Sher).
You can see that if you have compression on that nerve it can affect anywhere from the top, at the clitoral branch, all the way down to the inferior rectal branch. It is an extremely important nerve.
- Irritation of the pudendal nerve providing sensation to the perineal, rectal area, penile, and clitoral branch
- Can radiate into the upper thigh
- Constant burning pain, the sensation of dryness
- Bikers, people who sit all day, deadlift
- Other causes: pregnancy, scarring due to surgery, accidents and surgical mishaps
It can cause irritation which provides sensation to the perineal, rectal, penile, and clitoral branches. This pain can radiate into the upper thigh which can cause constant burning and a dry feeling. A client that completes deadlifting can also get irritation to that nerve. Pregnancy can cause problems because the nerve does stretch during pregnancy. There can be scarring on that nerve via accidents or surgical mishaps.
- Pudendal Neuralgia Treatment Ideas
- Body mechanics (special work chair)
- Manual therapy
- Heat/Ultrasound/Ice
- Seat cushions (Tush Cush, or sky mall seat)
- Biofeedback
- Relaxation Exercises / Breathing
- TENS
- Sitting on Ball
If your client is working in an environment where they are sitting a lot, you want to make sure they get a special work chair and/or seat cushion. These patients do very well with manual therapy. Some like heat, ultrasound, ice, or biofeedback. Relaxation exercises and breathing are also extremely important. Some patients benefit from TENS that they can use that at home or at work. And, sitting on a ball sometimes can relieve that pressure or that pain feeling.
Vulvar Pain and Vulvodynia
- Vulvar Pain
- pain in the vulvar area
- itching, burning, stinging, stabbing
- many possible causes
- hormonal-estrogen deficiency
- herpes simplex
- vulvar warts
- precancerous and cancerous vulvar disease
- Vulvodynia-vulvar pain not associated with a specific disorder, 2003 classification by International Society for the Study of Vulvovaginal Disease ISSVD
There is also something called vulvodynia and vulvar pain, and there is a pain in the vulvar area. Patients describe itching, burning, stinging, and stabbing. This can be from an estrogen deficiency, herpes simplex, vulvar warts, or pre-cancerous or cancerous vulvar disease.
- “Data from a Harvard study, funded by the National Institutes of Health, indicates that 16 percent, or about 13 million American women of all ages and ethnicities, suffer from vulvodynia at some point in their lives.”
- “The Harvard study also found that 60 percent of vulvodynia sufferers consulted at least three doctors in seeking a diagnosis. Astoundingly, 40 percent of those who sought professional help remained undiagnosed after three medical consultations. ”
If you want to know more about vulvodynia, the National Vulvodynia Association (nva.org) has great information you can read more about it. A Harvard study found that 60% of vulvodynia sufferers consulted at least three doctors, and 40% of those who sought professional help remain undiagnosed. I see this a lot. I have patients that have been seen by up to seven or eight doctors. They are in so much pain, and sometimes because you cannot see actually the pain, the MDs cannot find anything. It is kind of like fibromyalgia of the vulvar area, and it is very painful for patients.
- Diagnosing Vulvodynia
- During the cotton-swab test, gentle pressure is applied to various vulvar sites and the patient rates the severity of the pain. If any areas of skin appear suspicious, the provider may examine them with a magnifying instrument or take a biopsy of the area.
Again, I do not diagnose someone. They usually come to me after this diagnosis. What the gynecologist does is take a Q-tip and apply pressure on different parts around the vaginal area to locate where the pain is.
A lot of patients have significant pain at four o'clock and eight o'clock. In pelvic floor therapy, we look at the whole vaginal area like a clock, where the top and clitoris is going to be 12 o'clock. The anus is at six o'clock. They move around the clock to find different pain points. If someone is found to have pain, then their physician can look at it under a magnifying instrument or take a biopsy of the area.
- Two types:
- Generalized Vulvodynia (Unprovoked)
- Pain occurs spontaneously and is constant, with occasional relief of symptoms
- Prolonged sitting, pressure to the vulva, wearing pants exacerbate symptoms
- Pain can be specific or in multiple areas
- Vulvar Vestibulitis Syndrome VVS (aka Provoked Vestibulodynia)
- Pain limited to the vestibule, the area surrounding the opening of the vagina
- Occurs during or after intercourse, tampon insertion, gynecologic exam, prolonged sitting, wearing fitted pants
- Primary VVS- since the first attempt at vaginal penetration
- Secondary VVS- experienced pain-free intercourse prior to the development of pain
There are generally two types of vulvodynia. The first is unprovoked where the pain occurs spontaneously. It can be from prolonged sitting or wearing pants that are too tight. Sometimes, your patients wear underwear that is too tight or g-strings. They are very uncomfortable so we try to get them to wear underwear that is cotton and more comfortable.
Or, you can have vulvar vestibulitis syndrome. This is provoked. The pain is limited just the vestibule area, which is the area surrounding the opening of the vagina. This occurs during or after intercourse, tampon insertion, a gynecological exam, or from a lot of sitting or wearing fitted pants. There is primary and secondary vulvar vestibulitis syndrome (VVS) as well.
- Not caused by STD or active infection
- Researchers speculate that one or more of the following may contribute to vulvodynia:
- Injury/irritation of nerves that transmit to the vulva
- An increase in nerve fiber density in the vestibule
- Elevated levels of inflammatory substances
- Altered hormone receptor expression in tissue
- Genetic susceptibility to pain and inflammation
- A localized hypersensitivity to Candida (yeast)
- Pelvic floor weakness or spasm
Researchers are trying to figure out vulvodynia and the causes. They know that it is not caused by an STD or an active infection. Researchers speculate that it could be one of the following. It could be an injury, irritation to the nerves, or an increase in nerve fiber density. Some doctors still take some of the skin off to decrease the nerve density. I have had a couple of patients that have had that done in the past. For some, it does absolutely nothing, while for others, it has helped. There can also be an elevation of inflammatory substances and altered hormone receptor expression in the tissue. There are many different things that they are speculating that this is caused by.
- Frequently associated with:
- Interstitial Cystitis/Painful Bladder Syndrome
- Urological conditions of urinary urgency, frequency, and bladder spasms
- Irritable Bowel Syndrome
- Fibromyalgia
- Chronic fatigue
- The suggestion of an autoimmune disorder
- Vulvar reflex sympathetic dystrophy theory
- Hyperalgesia (wind up) Activation of C fibers following inflammation
It is also associated a lot with the painful bladder syndrome that we talked about in that first section of this series focusing on the bladder. Urological conditions of urinary urgency or frequency can trigger this. Additionally, IBS is associated with this. A lot of my patients that have vulvodynia also have fibromyalgia or chronic fatigue. There has also been a suggestion of an autoimmune disorder. We know the hyperalgesia and activation of C-fibers can activate this with inflammation.
- Treatments for vulvodynia are directed towards alleviating symptoms. Current treatments include:
- surgical removal of sensitive tissue (for VVS/Provoked)
- antidepressants
- cold compresses, topical anesthetics/lubricants
- manual therapy
- steroids
- laser surgery (long and painful healing)
- nerve blocks
- neurostimulation and spinal fusion pump
- diet modifications
- biofeedback
There are different types of treatments directed toward alleviating the symptoms. Obviously, some of these we do not do. For example, we do not remove tissue but some physicians do. Some patients do well with antidepressants, cold compresses, manual therapy, steroids, laser surgery, nerve blocks, diet modifications, and biofeedback. Biofeedback is one of my favorites because it is conservative and will not harm the patient at all.
- Howard Glazer, PhD
- Discovered that the muscles of the pelvic floor in vulvodynia patients were abnormal. Correcting the muscle abnormalities through EMG assisted aerobic exercise of the pelvic floor musculature increases blood flow and restores vulvar tissue integrity leading to pain relief.
A big name in this area is Howard Glazer. He passed away a few years ago, but he was a doctor who did a ton of research on vulvodynia patients. He found that there was a muscle abnormality, and he did a lot of work with EMG as well.
- Glazer Testing Protocol
- One minute rest, pre-baseline
- 5 rapid contractions with 10-second rest in between (phasic)
- 5 – 10-second contractions with 10-second rest in between (tonic)
- Contraction of 60 seconds (endurance)
- One minute rest, post-baseline
He lived in New York, had patients come to his office, and he would give them this protocol. It is a one-minute rest, and this is with EMG. g.
- Glazer Home Program
- 60 reps: 10-second hold/10 second rest – 2 x a day for 20 minutes
- Accessory muscle activation and maximum contract/relax OK
The home program was time-consuming with the exercises taking 40 minutes a day. They could squeeze whatever they want. His theory was to squeeze to completely tire out and exhaust those muscles to knock out of this instability. Figure 16 is the equipment they would insert vaginally.
Figure 16. The equipment was given by Glazer for a home program (Author's image).
They would use this for 20 minutes, twice a day. When the patient would squeeze, that green little bar would go all the way up and come all the way down. They would track these. Some of the patients had a very high resting tone so the green bar would be all the way to the top. The goal was to get that green bar to relax more towards the end of the session.
- Glazer's Treatment Method
- Break high tension levels and create muscle stability
- Patients use accessory muscles
- internal obturator
- lower abdominals
- adductor longus
- Exercise pelvic muscles to point of fatigue
- Use of home trainers
He was trying to break the high tension levels and create some stability. You could use all the different muscles. I actually do not use this very often. I try to get someone to completely relax those muscles by using other methods. If nothing else will work, then we might try this, but I definitely would not have them do 40 minutes a day. This can be considered a full-time job nowadays.
- Howard Glazer, Ph.D. (“Treatment of Vulvar Vestibulitis Syndrome with Electromyographic Biofeedback of Pelvic Floor Musculature,” Glazer et al, 1995)
- Slightly more than 50% cure rate
- A self-report improvement rate of 83%
- 80% of sexually abstinent patients resumed regular intercourse
- Pelvic floor muscle rehabilitation/muscle-stabilizing program assisted by surface EMG
- Reduction of muscle variability overall and predominantly at rest
With his studies, he had more than a 50% cure rate, and there was a self-improvement rate of 83%. This is something I wanted you guys to be aware of because there is a lot of research that is backed by this method.
Urological Syndromes-General
- Pain and dysfunction of smooth bladder and urethra muscles
- Hypertonus of pelvic muscles
- Dyspareunia, low back pain, sacral pain
- Urgency, frequency
- Pressure sensations
- Voiding difficulties
- Constipation
You may see urological syndromes in general. Patients can have pain and dysfunction of the smooth bladder and urethral muscles. Hypertonus means an overactive pelvic floor, dyspareunia intercourse, and pain with intercourse. They can also have low back pain. Patients can have urgency and frequency, whether that be with a bladder or the bowel, pressure sensations, voiding difficulties, and constipation. All of these can be considered pain conditions that you might see, or there might have several of these.
Interstitial Cystitis (IC) or Painful Bladder Syndrome
- Urgency frequency syndrome
- increased afferent input
- spastic pelvic floor
- unidentified neurological injury
I also treat a lot is interstitial cystitis which is also called painful bladder syndrome. If they do a cystoscopy to look at the lining of the bladder, they can look like lesions. These patients cannot tolerate anything citrusy, anything with a high acid content, coffee, or things of that nature. It is like pouring acid on a wound and is very uncomfortable. They have to watch what they are drinking and eating so that it does not cause more of that pain.
- IC/PBS Symptoms
- S
