Editor's note: This text-based course is a transcript of the webinar, Caregiving For The Spinal Cord Injury Patient, presented by Alaena McCool, MS, OTR/L, CPAM.
Learning Outcomes
- After this course, participants will be able to identify caregiver expectations associated with spinal cord injury levels.
- After this course, participants will be able to identify challenges unique to patients with spinal cord injuries.
- After this course, participants will be able to list principles of good practice involved in conversations about safety/risk assessment.
Introduction
Today, I'm excited to lead a session on caregiving for spinal cord injury patients. Let's start by reviewing the learning outcomes and delving into some key facts about spinal cord injury and caregiving.
We'll then explore the different spinal cord injury levels, their impact on function, and the expectations placed on caregivers. Throughout the session, we'll discuss the challenges patients and caregivers face and brainstorm possible solutions to address them.
We'll examine case studies highlighting real-life caregiving scenarios for spinal cord injury patients to bring these concepts to life. Join me as we embark on this journey of understanding and supporting individuals with spinal cord injuries and their caregivers.
Content
- Learning Outcomes (see above)
- Fast Facts
- SCI Function and Caregiver Expectations
- Caregiver Challenges
- Possible Solutions
- Case Studies
Before our discussion, let's review our learning outcomes for today's session. Our first goal is to understand the expectations placed on caregivers for individuals with different levels of spinal cord injury. Next, we aim to recognize the unique challenges faced by patients with spinal cord injuries. Finally, we'll explore various resources and solutions to address these challenges for caregivers and patients.
Now, let's take a moment to consider who can fulfill the role of a caregiver.
Who Can Be a Caregiver?
- Formal (Paid) or Informal (Unpaid)
- Formal: Through an agency typically, it can also be through other platforms.
- Informal: Typically, a family or friend
- Provide assistance with ADLs, IADLs, transfers, mobility, transportation, and/or other community needs.
- Responsibilities may change depending on the patient’s needs.
Let's clarify the term "caregiver." We can categorize caregivers into two main groups: formal and informal.
A formal caregiver is someone who is compensated for their caregiving services, typically through an agency or private pay arrangement. On the other hand, an informal caregiver is unpaid and is often a family member or friend. Both types of caregivers play crucial roles in providing assistance with activities of daily living (ADLs), instrumental activities of daily living (IADLs), transfers, bed mobility, transportation to appointments, and fulfilling other community needs.
It's important to note that the responsibilities of caregivers may evolve over time as the needs of the patient change.
Spinal Cord Injury (SCI) Fast Facts
- 250,000-500,000 people are diagnosed with SCIs worldwide annually. (Keihanian et al., 2022)
- Traumatic injuries are the main cause of SCI; however, non-traumatic injuries are increasing yearly.
- SCI patients are predisposed to secondary health complications and neurological comorbid conditions.
- Direct and indirect costs attributable to SCI were 2 to 20 times more than other neurological disorders. (Keihanian et al., 2022)
Spinal cord injuries affect hundreds of thousands of people globally each year, with traumatic incidents being the primary cause. However, nontraumatic injuries are also becoming increasingly common. These injuries predispose patients to various secondary health complications and neurological comorbid conditions, adding to the complexity of their care.
The financial implications of spinal cord injuries are significant, far surpassing those of many other neurological disorders. A recent study revealed that the lifetime costs of healthcare and associated needs for a patient diagnosed with a spinal cord injury at the age of 25 could reach a staggering $4.7 million. This highlights the substantial burden placed on both individuals and healthcare systems.
Caregiver Fast Facts
- Caregivers play a pivotal role in optimizing healthcare outcomes and the recovery process.
- Per the United States Census Bureau, more than 65 million people in the United States provide informal care to an individual with a chronic illness or disability. (Juengst et al., 2019)
- Caregivers of people with SCI, compared to other chronic diseases, are at greater risk of developing physical, mental, and social problems. (Keihanian et al., 2022)
- Caregiver burden is associated with poor health-related quality of life and well-being of the caregiver. (Uhm et al., 2023)
Caregivers are essential contributors to the well-being and recovery of individuals with spinal cord injuries. In the United States alone, over 65 million people provide informal care to those with chronic illnesses or disabilities, emphasizing the widespread impact of caregiving responsibilities.
However, caregivers of individuals with spinal cord injuries face unique challenges compared to those caring for individuals with other chronic conditions. They are at a heightened risk of experiencing physical, mental, and social difficulties, which can significantly impact their quality of life and overall well-being. The burden of caregiving is closely linked to poorer health-related quality of life for the caregivers.
Next, we will discuss spinal cord injury levels, their function, and the caregiver's expectations.
SCI Levels
- Cervical
- High cervical C1-4
- Low cervical C5-8
- Thoracic
- T1-12
- Lumbar
- L1-5
- Sacral
- S1-5
The spinal cord levels include cervical, which I have broken up into a high cervical and a low cervical level, thoracic, lumbar, and sacral.
High Cervical (C1-4) Function
- Neck movement and diaphragm intervention
- 24/7 care
- Dependent for all ADLs
- Concerns
- Respiratory
- Safety
- Accessibility
- Adaptive equipment needs
The high cervical level, spanning from C1 to C4, presents significant challenges for patients with spinal cord injuries. While some neck movement and innervation may be present at C1 to C3, it's at C4 where diaphragmatic innervation begins, crucial for respiratory function.
Individuals with injuries at this level are typically completely dependent on caregivers for all activities of daily living, necessitating 24/7 care. Safety concerns, particularly respiratory function, are paramount at home and in the community. Additionally, adaptive equipment needs are significant.
In terms of mobility, there is potential for the patient to use a power wheelchair equipped with either a head array or chin control, depending on their remaining strength and mobility. These adaptations can significantly enhance their independence and quality of life.
Caregiver Expectations
- 24/7 Care
- Dependent for All ADLs and Transfers
- Assist With Transition to Home
- Training
- Follow-up appointments
- Accessibility and modifying the housing
- Equipment needs
The caregiver of a patient with a high cervical spinal cord injury faces immense responsibilities and expectations. Providing 24/7 care is a fundamental requirement, whether it's managed by one individual or split among several caregivers. This constant supervision is crucial due to the patient's inability to be left alone, particularly if they rely on a ventilator for respiratory support. In such cases, the caregiver must ensure the patient can always access assistance, even if they're not in the same room.
Additionally, the caregiver assumes the role of extensively trained support, equipped to handle emergency situations and perform daily activities of living for the patient. This includes assistance with transfers, modifying the home environment for accessibility, and addressing equipment needs tailored to the patient's requirements. Shower chairs with specialized supports, various types of Hoyer lifts, and other adaptive equipment may be necessary, demanding a thorough understanding and adeptness in their usage from the caregiver.
Moreover, the caregiver is responsible for coordinating follow-up appointments and ensuring the patient's safety and well-being at all times. The depth of training and expertise required for these tasks underscores the caregiver's critical role in facilitating the patient's care and recovery journey.
Cervical (C5-C8) Function
- C5
- Muscles Innervated
- Elbow flexion, shoulder flexion
- Upper body ADLs
- Use of hand orthosis
- Modifying daily ADL items (i.e., adding a hook to a cup)
- Mobility
- Power wheelchair
- Muscles Innervated
- C6
- Muscles Innervated
- Wrist extension, supination
- Upper body ADLs
- Tenodesis
- Use of hand orthosis for grasping
- Mobility
- Power vs. manual chair
- Muscles Innervated
Moving on to the lower cervical region, from C5 to C8, we witness increased upper extremity function. At the C5 level, patients exhibit elbow flexion and greater shoulder involvement, enabling independence in upper body activities of daily living (ADLs). Patients may use hand orthoses or compensatory movements, such as hooks, to facilitate this independence for grasping objects. The introduction of powered wheelchairs becomes essential at this stage, offering tilt-in-space functionality for pressure relief and maneuverability.
Progressing to the C6 level, we observe further improvements in wrist extension and supination, enhancing the patient's ability to perform upper body ADLs independently. With the potential utilization of tenodesis, patients can achieve a functional grasp, although hand orthoses may still be necessary for support. While some patients may entertain the idea of transitioning to a manual wheelchair, considerations for fatigue, shoulder integrity, and postural support must be carefully addressed before making such decisions.
- C7-8
- Muscles Innervated
- Elbow extension, pronation, digit flexion, thumb movement
- ADLs
- More independence with fine motor function
- Mobility
- Power vs manual
- Muscles Innervated
Continuing to the C7 to C8 region, we observe further improvements in upper extremity function. Elbow extension at C8 and some digit flexion provide patients with increased independence in upper body ADLs. While they may require less assistance for lower body tasks, fine motor interventions still necessitate caregiver assistance. Despite the potential for increased independence, concerns regarding skin integrity and shoulder pain persist, mirroring those seen in the C5 to C6 levels.
Before delving into caregiver expectations, I've included photos showcasing various adaptive equipment that may benefit patients at these spinal cord injury levels.
Adaptive Equipment
Currently, I'm focusing solely on self-feeding, as an extensive array of equipment is available. Figure 1 shows some examples. The abundance of options can quickly become overwhelming for patients and caregivers alike.

Figure 1. Examples of feeding equipment.
Here we have a cup holder with two ends to hold the cup with both hands. This is a fantastic addition for patients who prefer using a straw or wish to participate in self-feeding tasks. Moving on, we have a zipper pull, which requires the patient to use a U cuff and exert enough strength, utilizing muscles such as the lats, adductors, and pecs. Lastly, we have a rubber gripper at the top, a simple yet effective tool for opening jars and handling small, fine motor tasks like toothpaste. These grippers come in various sizes to suit different needs. In Figure 2, you'll see a variety of adaptive feeding utensils.
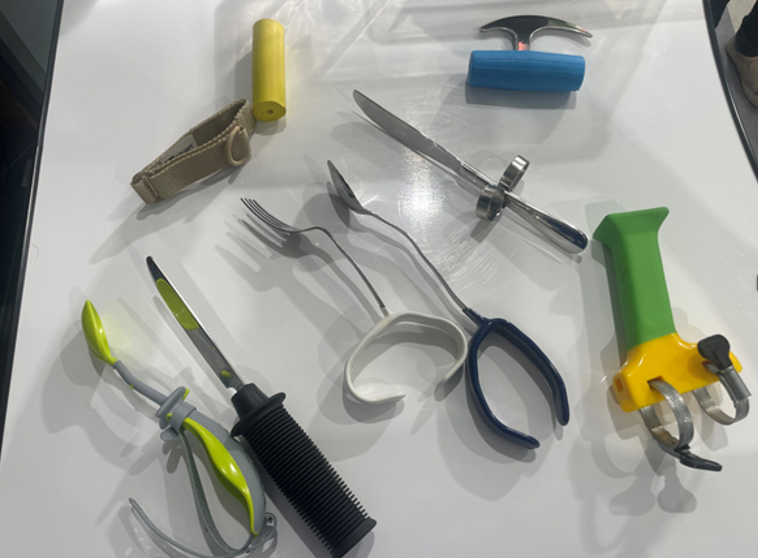
Figure 2. Adaptive feeding utensils.
In Figure 3, several adaptive utensils are aimed at addressing different needs. These include utensils with U-cuffs for added stability, built-up handles for easier gripping, a rocker knife for simpler cutting, and utensils designed for digit isolation. These adaptations aid individuals with limited hand function manage utensils more effectively during mealtime. You can also see built-up bowls with rims and a plate guard, which help prevent spills and facilitate easier food scooping for individuals with motor challenges.

Figure 3. Other feeding equipment.
One bowl has a suction cup, while another is weighted. Simple things like this make a big difference for the patient.
Orthotics
Lastly, I just wanted to show some different orthotic options, including the bar splint in Figure 4.

Figure 4. Two orthotic options.
It can be adjusted on that dorsal region of the wrist to give a little more wrist extension. Another one is a McKie splint for thumb stabilization (Figure 5).

Figure 5. McKie splint.
Figure 6 shows an elbow air splint. You blow it up to stabilize different parts of the arm, like the elbow.

Figure 6. Air splint.
This is a great option if you're trying to increase the patient's independence.
Caregiver Expectations
- ADLs
- Requires set up for grooming, dressing, self-feeding
- Assistance for lower body ADLs
- Assistance for morning and bedtime routines, bowel/bladder management
- Equipment Needs
- Home modifications
- Appointments
It's important to recognize the significant level of care required for individuals with spinal cord injuries, which varies depending on the injury level. According to the Paralyzed Veterans of America (PVA), patients with spinal cord injuries at different levels require varying amounts of daily care from caregivers. For example, those with injuries at the C5 level may need up to 16 hours of daily care, while those at the C6 level may require 10 hours, and those at the C7 to C8 level may need 8 hours.
This care involves assisting with activities of daily living, instrumental activities of daily living, bowel and bladder management, transfers, and home modifications. Caregivers also play a crucial role in setting up assistive technology to help patients access their environment and manage follow-up appointments and other administrative tasks. Additionally, caregivers may need to provide assistance with setting up and troubleshooting technology, ensuring that patients can effectively utilize these tools for independent living.
Thoracic (T1-12) Function
When considering the thoracic level of spinal cord injury, it's important to understand the functional differences between the upper and lower halves. The upper half, typically ranging from T1 to T5 or T1 to T9, depending on the source, poses challenges for activities of daily living due to the potential involvement of respiratory muscles. Above T6, respiratory concerns become more prominent, while at T10, the engagement of abdominal muscles plays a role in function. This variability in classification underscores the complexity of spinal cord injury levels and their impact on function and caregiving needs.
- T1-5
- Muscles Innervated
- Back extension and increased musculature for breathing
- ADLs
- Independent for upper body
- Assistance more for lower body
- Adaptive equipment
- Postural supports
- Muscles Innervated
- T6-12
- Muscles Innervated
- Core muscles closer to T10
- ADLs/IADLs
- More independence from sitting
- Ambulation
- Potential to perform with braces and devices
- Muscles Innervated
In the upper thoracic region, which includes the muscles innervated from T1 to T5 or T1 to T9, there is involvement of back extension and intercostal muscles, contributing to more efficient breathing. Patients at this level should exhibit independence in upper body ADLs, although assistance may be needed for lower body tasks depending on their position. Adaptive equipment may still be necessary, particularly for postural support to maintain balance, given the limited engagement of abdominal muscles.
Similarly, patients in the lower thoracic region should demonstrate independence in upper body ADLs but may require assistance with lower body tasks, especially concerning bowel and bladder management. Additionally, there is potential for ambulation with braces and devices, although reliance on a wheelchair is still likely as part of the process.
Caregiver Expectations
- ADLs/IADLs
- Less reliance on ADLs
- Assistance for accessibility within the house
- Transportation
- Preparation
- More assistance may be required later due to Secondary Complications
Per the PVA guidelines, caregivers for patients at the thoracic level are estimated to require two to three hours of caregiving daily, significantly less than those at the cervical level. While their responsibilities may be reduced, caregivers may still need to assist with tasks such as bowel and bladder management, lower body ADLs, transportation, and IADLs. It's important to note that due to the increased use of arms throughout the day, there is a heightened risk of strain, pain, and injuries for the patient, which may necessitate additional assistance from the caregiver. Therefore, patients and their families should initiate conversations early on about potential needs and develop a plan accordingly.
Lumbar and Sacral Function
- L1-5
- Muscles Innervated
- Hip flexion, knee extension, ankle flexion, toe extension
- ADLs
- Independent
- Special equipment for bowel/bladder
- Mobility
- Wheelchair vs ambulating with braces and/or assistive devices
- Muscles Innervated
- S1-5
- Muscles Innervated
- Ankle extension
- ADLs
- Bowel and bladder focused
- Mobility
- Fewer or no devices needed
- Muscles Innervated
In the lumbar and sacral region, muscles innervated include those of the hip, knee, and ankle. Patients in this category should generally be independent in all ADLs, although they may require some assistance with fine motor skills related to lower body dressing. If the patient has tone or contracture issues, they may also need bowel and bladder management assistance. While patients may still use a wheelchair for longer distances, they may begin to utilize braces and other devices.
Caregiver Expectations
- ADL/IADLs
- Potential bowel bladder program assistance
- Homemaking activities
- Assistance varies per patient
- Emergencies
The PVA suggests that a patient with a lumbar or sacral injury may require just 1 hour of assistance per day, primarily for homemaking activities. However, it's crucial to recognize that the level of assistance needed can vary based on individual circumstances. For instance, caregivers may be involved in establishing and maintaining a bowel and bladder program, especially as patients encounter challenges like UTIs or medication-induced issues such as constipation. In such cases, caregivers may need to provide additional support beyond the usual expectations, including assistance with ADLs and household tasks. This highlights the significant impact that bowel and bladder issues can have on a patient's overall well-being and the extent to which caregivers may need to adapt and provide additional care as needed.
SCI Considerations
- Complete vs. Incomplete
- Age of Onset
- Prior Health
- Acute vs Chronic
- Secondary Complications
- Pain
Spinal cord injury is a complex issue that defies simple categorization. Despite our efforts to understand and treat it, patients and caregivers face numerous challenges and uncertainties. While we've provided an overview of spinal cord injury levels and caregiver expectations, it's essential to recognize that each case is unique and may deviate from these generalizations.
Various factors can influence the needs and experiences of patients and caregivers. For instance, the completeness of the injury—whether it's classified as complete or incomplete—plays a significant role in determining the level of function and support required. Additionally, the age at which the injury occurred, the patient's prior health status, their understanding of their condition, and whether they're in the acute or chronic phase of injury all contribute to shaping their needs and goals.
Moreover, secondary complications such as pressure sores, orthopedic issues, mental health challenges, and the presence of chronic pain further complicate the caregiving process and can significantly impact a patient's independence and quality of life. These factors underscore the importance of addressing not only the primary injury but also its associated complications and the patient's holistic needs.
Given the complexity of spinal cord injury care, caregivers—whether formal or informal—face significant burdens and uncertainties. It's crucial to acknowledge and support caregivers' invaluable role in patients' lives. By understanding their challenges and providing appropriate resources and support, we can help alleviate some of the burdens they face and enhance the overall well-being of patients and caregivers.
Challenges
- Limited Training
- Adjustment to New Role
- Home, Equipment, and Accessibility
- Continuity of Care
- Finances
- Insurance
- Support
- Resources/Services
- Waiver Availability
Navigating the challenges of spinal cord injury care challenges requires a comprehensive understanding of the multifaceted needs of patients and caregivers. In the initial stages of rehabilitation, healthcare systems are designed to facilitate patients' safe and swift transition back home. However, this often translates to shorter rehab stays and limited training opportunities for caregivers, who are suddenly tasked with assuming significant responsibilities.
Whether a caregiver is a paid professional or a family member, they play a crucial role in the patient's ongoing care journey. Yet, the burden placed on them is immense. From learning to assist with daily activities to managing medical appointments and household responsibilities, caregivers are thrust into new roles while juggling their existing commitments. This transition period can be overwhelming and demanding, particularly as caregivers strive to maintain their own lives and responsibilities.
Moreover, the complexity of navigating insurance coverage, financial considerations, and accessing support services adds another challenge for caregivers and patients alike. Even after the initial adjustment period, ongoing challenges may arise, such as changes in caregiver availability, insurance modifications, and evolving healthcare needs.
Throughout this journey, caregivers and patients are actively coping with the profound changes brought about by the spinal cord injury diagnosis. It's crucial for healthcare professionals to recognize the ongoing nature of these challenges and provide continuous support and resources to help patients and caregivers navigate the complexities they face at every stage of the journey.
Negative Outcomes
- Role Strain
- Relationship Issues
- Financial
- Social
- Mental health
- Illness
The challenges faced by caregivers of spinal cord injury patients can have profound and far-reaching impacts on their well-being. From the strain of assuming multiple roles to financial instability, social isolation, and mental and physical health issues, caregivers are confronted with a myriad of stressors that can take a toll on their quality of life.
The demands of caregiving can lead to strain on relationships, particularly when intimate connections are disrupted due to the caregiver's additional responsibilities. Financial burdens can exacerbate stress, forcing caregivers to make difficult decisions about employment and financial stability. Social isolation, compounded by factors such as the COVID-19 pandemic, further compounds the challenges faced by caregivers, limiting their support networks and increasing feelings of loneliness.
Mental health concerns, including depression, anxiety, and burnout, are prevalent among caregivers, who may struggle to cope with the emotional and psychological demands of their role. Additionally, caregivers may experience physical strain and limitations, further impacting their ability to provide care effectively.
As healthcare professionals, it is essential to recognize and address the multifaceted needs of caregivers. Providing education, resources, and support can empower caregivers to navigate their roles more effectively and mitigate the negative impacts of caregiving stress. Encouraging self-care practices, fostering social connections, and offering respite care can help alleviate the burden on caregivers and promote their overall well-being.
Furthermore, advocating for policies and initiatives that support caregivers, such as caregiver training programs, financial assistance, and access to mental health services, can help alleviate the challenges they face. By taking a holistic approach to caregiver support, healthcare professionals can better serve both patients and caregivers, enhancing the quality of care and promoting positive outcomes for all involved.
Possible Solutions
- Caregiver Preparedness
- Monitoring
- Creating a New Normal
- Specialists
- Therapist Provided Education
- Resources Available
- Advocacy
How can we help this with the caregiver burning or caregiver burden? Some possible solutions include caregiver preparedness, monitoring the patient throughout their care, creating a new normal, specialist referrals, therapist-provided education, available resources, and advocacy. Know that there are a lot of other solutions. These are just the main ones I want to discuss today.
Caregiver Preparedness
- Problem-Solving Training
- Self-management intervention
- ABCDEF
- Assess
- Brainstorm
- Consider
- Develop
- Evaluate
- Flex
- Provide information
- Symptom relief
- Daily care
- Treatment options
- Nutritional support
- Emotional and stress support for caregivers
Caregiver preparedness is crucial for effectively managing the challenges associated with caring for individuals with spinal cord injuries. Problem-solving training, a self-management intervention facilitated by therapists or trained professionals, has shown promising outcomes in empowering caregivers to address and overcome obstacles. Through this intervention, caregivers learn to identify problems, explore various solutions, set realistic goals, and reassess their progress with the support of a therapist. Providing caregivers with relevant information and resources is essential for their preparedness. This information can cover many topics, including symptom management, daily care techniques, treatment options, nutritional support, emotional well-being, and caregiver support services. Tailoring information delivery to match the caregiver's preferred learning style, whether through email, verbal communication, web-based resources, or printed materials, ensures effective communication and knowledge transfer. By equipping caregivers with problem-solving skills and essential information, healthcare professionals can enhance their preparedness and ability to navigate the complexities of caregiving for individuals with spinal cord injuries.
Monitoring
- Follow-up Through Transitions
- Open dialogue with patient and caregiver
- Assess caregiver
- Caregiver Burden Inventory (CBI)
- Caregiver Burden Scale (CBS)
- Caregiver (CG)
- Caregiver Strain Index (CSI)
- Build trust and rapport
- Connect to Support
Continuous monitoring of patients with spinal cord injuries throughout their lifetime is essential for ensuring optimal care. Maintaining an open dialogue with both the caregiver and the patient facilitates this process, as caregiving is dynamic and subject to change over time. Through regular assessments and communication, healthcare professionals can evaluate the caregiver's well-being and provide appropriate support. Building trust and rapport with the patient and caregiver fosters a collaborative relationship and enhances the effectiveness of care delivery. Even if the caregiver or patient is not immediately receptive to advice or recommendations, persistence in offering support and education can lead to positive outcomes in subsequent interactions. By remaining engaged and supportive, healthcare professionals can adapt to the evolving needs of patients and caregivers throughout their caregiving journey.
Creating a New Normal
- New Daily Routine
- Adapt in Current Phase of Life
- Work
- Vacations
- Sports
- Hobbies
- New Hobbies/Activities
As healthcare professionals, we can assist caregivers and patients by facilitating the transition to a new normal. This involves identifying stressors for the caregiver and addressing them through practical solutions. For example, we may explore adjustments to the daily routine, such as implementing a modified morning or bedtime schedule to alleviate caregiver burden. In therapy sessions, we can focus on promoting patient independence by teaching tasks that can be performed at the edge of the bed, allowing the caregiver to attend to other responsibilities.
Additionally, we should consider the caregiver's personal interests and aspirations. Is there a hobby or activity they wish to pursue? Are there opportunities for respite or support programs that cater to the patient's needs while providing the caregiver with a break? By understanding the preferences and goals of both the patient and caregiver, we can tailor our recommendations and support services to enhance their overall well-being and quality of life.
Specialist
- Assistive Technology
- Accessing environment
- Communication
- Increase independence
- Mental Health Provider
- Individual and family support
- Routine Care Follow-up
- Referrals for Other Medical Needs
Referrals are an essential aspect of comprehensive care for patients with spinal cord injuries and their caregivers. As healthcare professionals, we must recognize when additional support or specialized services are necessary. This may include referrals for assistive technology to improve the patient's ability to access their environment or enhance their independence. Depending on clinic protocols, referrals may be made directly by the therapist or through collaboration with other healthcare providers.
Moreover, it's crucial to address any mental health concerns that may arise for both the patient and caregiver. Initiating discussions about counseling or therapy options and connecting them with appropriate resources can significantly impact their well-being. Additionally, educating patients and caregivers about routine care, follow-up appointments, and self-advocacy ensures they remain engaged in their healthcare journey.
Furthermore, if there are changes or complications in areas such as bowel and bladder management, prompt communication with the primary care provider or specialist is essential. This may involve coordinating referrals to urologists or other specialists to address emerging issues and optimize the patient's overall care plan. By proactively addressing needs and facilitating appropriate referrals, we can better support the holistic health and well-being of patients and caregivers alike.
Therapist Provided Education
- Keep Simple And Short
- Provide Up-To-Date Information
- Provide Resources
- Support groups
- Peer to peer
- Adjustment to new roles
- Creative Solutions
- Immediate and future implementation
- Recommendations
- New or modified equipment
- Referrals
Providing education and information is fundamental to our role as healthcare professionals. It's essential to tailor our approach to the individual's needs, keeping explanations concise and easy to understand. Offering up-to-date information and resources ensures that patients and caregivers can access the most relevant support available, whether peer support groups or educational materials.
When setting goals with patients and caregivers, it's beneficial to establish both short-term and long-term objectives. By collaboratively identifying creative solutions that can be implemented immediately and adapted for future use, we empower them to take proactive steps toward achieving their goals. This may involve exploring compensatory techniques, introducing adaptive equipment, or modifying their existing equipment to enhance functionality and independence.
Furthermore, regularly monitoring their progress and evaluating the effectiveness of interventions allows us to make necessary adjustments and continue supporting them on their journey toward improved quality of life. Additionally, having equipment available for trial in the clinic and offering guidance on home modifications can further facilitate their adaptation and integration of assistive devices into their daily routines. By providing comprehensive education and practical solutions, we empower patients and caregivers to navigate their challenges with confidence and resilience.
Resources
- National
- National Council on Independent Living
- National Caregivers Association
- VA services for respite for veterans
- National Spinal Cord Injury Association
- Caregiver Action Network
- Local
- Maryland Access Point
- Maryland Department of Aging
- Local hospitals
- Medicaid Waiver programs
- State funding options
- Local support groups
Navigating resources can be overwhelming for patients and caregivers, especially considering the vast array of options available at national and local levels. It's essential for healthcare professionals to be aware of these resources and to guide patients and caregivers toward accessing the support that best meets their needs.
Local organizations such as Maryland Access Point and the Maryland Department of Aging can provide invaluable assistance with services like transportation and home accessibility modifications. By familiarizing ourselves with these local resources and maintaining connections with experts in the field, such as case managers or community outreach coordinators, we can ensure that patients and caregivers receive the support and assistance they require.
Furthermore, it's crucial for healthcare professionals to advocate for change by actively identifying and sharing the challenges patients and caregivers face. By raising awareness of these issues within our healthcare systems and communities, we can work towards implementing meaningful solutions and improving the overall quality of care and support available to individuals affected by spinal cord injury.
Advocacy
- Advocacy Groups
- ADAPT
- Access Living
- United Spinal Association
- Disabled Word: Spinal Cord Injury
- Family Voices
- Paralyzed Veterans of America
- Events
- Roll on Capitol Hill
- Walks
- Runs
- Fundraisers
- Networking
- Connecting with other peers
- Writing to local politicians
Active participation in advocacy efforts is crucial for making a positive impact on the lives of our patients. There are numerous advocacy groups and events available where we can engage and contribute to advancing the interests of individuals with spinal cord injuries. Additionally, networking with colleagues allows for exchanging valuable information and opportunities to join collective advocacy initiatives.
For instance, staying informed about policy changes and advocating for necessary adjustments, such as recent alterations in orthotic billing, can significantly benefit patients. By signing petitions and reaching out to local politicians, we can amplify our voices and draw attention to the importance of maintaining essential services and support for individuals with spinal cord injuries.
Ultimately, we can effectively drive positive change and improve the quality of care and resources available to our patients through our collective advocacy efforts, whether through letters, emails, or direct engagement with policymakers.
Patient Perspective
- “If you want good help, you need to pay for it.”
- “I’ve had 5 caregivers in the last 2 months.”
- “I used Craigslist to find help, and she stole from me.”
- “It is difficult to find someone, especially someone who wants to stay consistent.”
It's evident from the feedback I received during the preparation of this lecture that caregiving is a challenging and frustrating experience for many individuals. Some of the sentiments shared by patients include the difficulty in finding reliable and consistent help, as well as the financial strain associated with securing quality caregiving support. For instance, one patient emphasized the importance of adequately compensating caregivers to attract reliable assistance, while another highlighted the challenges of finding trustworthy help, even resorting to unconventional methods like Craigslist, which unfortunately resulted in negative experiences. These quotes underscore the significant obstacles and frustrations faced by caregivers and the importance of addressing these issues to improve the caregiving experience for patients and their families.
Update-CPT Codes
- New CPT codes
- 97750 Caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community (e.g., activities of daily living [ADLs], instrumental ADLs [iADLs], transfers, mobility, communication, swallowing, feeding, problem-solving, safety practices (without the patient present), face-to-face; (30 minutes)
- 97751 Caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community (e.g., activities of daily living [ADLs], instrumental ADLs [iADLs], transfers, mobility, communication, swallowing, feeding, problem-solving, safety practices (without the patient present), face-to-face; (additional 15 minutes)
- 97752 Group caregiver training in strategies and techniques to facilitate the patient’s functional performance in the home or community (e.g., activities of daily living [ADLs], instrumental ADLs [iADLs], transfers, mobility, communication, swallowing, feeding, problem-solving, safety practices) (without the patient present), face to face with multiple sets of caregivers.
Before we delve into these case studies, I'd like to share an important update: CPT codes for caregiver training have been approved. This marks a significant milestone in recognizing the vital role of caregivers in the rehabilitation process. Now, let's explore these case studies together, examining real-life scenarios and focusing on each one's caregiving aspect.
Case Studies
Case Study #1: E.G.
- The patient is a 64-year-old female diagnosed with Neuromyelitis Optica (NMO) in 2005. She presents today with worsening left UE weakness in the last year due to “flare up.” Prior to this she was working full time, driving self in adapted van, and fully independent in all ADLs.
- C3 AIS A (sensory)
- Left weaker than right (3-4/5 throughout UE); dependent to max A for all ADLs and unable to drive
- Attends OT and PT 1x a week; however has missed 3 times since bout of care started 2 months ago.
This is a 64-year-old female diagnosed with NMO in 2005. She's experiencing worsening left upper extremity weakness over the past year due to a flare-up. Prior to this, she maintained full-time employment, drove herself in an adapted van, and was fully independent in activities of daily living (ADLs), with normal use of her left hand. However, now she presents with significant weakness in the left hand, rated around three to four out of five strength throughout. Fatigue sets in quickly, and she requires maximum assistance for all ADLs. Additionally, she's unable to drive. Despite attending occupational and physical therapy once a week, she's missed three sessions in the past two months. This is her first time seeking OT services, so we need to approach her care with patience and thorough assessment to understand her specific needs and limitations.
- Questions/Concerns
- What is the issue? Why is she missing these sessions?
- How can we ensure patient is getting benefits from rehabilitation services?
- How can we increase attendance?
- Can we support the family members taking over the rest of the care during the one afternoon?
- Any resources available to help with the financial burden?
Throughout the sessions, I delved into understanding the reasons behind her missed appointments. It turned out that she was paying out of pocket for a caregiver who was supposed to provide nine hours of care four days a week, with an additional four hours set aside for appointments. Even if the caregiver couldn't fulfill the full nine hours on a given day, the patient still paid for the entire time to ensure caregiver retention. This arrangement made it challenging for her to attend therapy sessions regularly.
To address this, we explored scheduling medical appointments more efficiently and increasing home exercises to ensure continuity of care. I also provided resources for financial support and caregiver services and reached out to our case manager to discuss additional assistance options. Considering her impending loss of disability benefits, we discussed planning for the financial impact and offered social work support, which she declined for now but may reconsider in the future. It's crucial to keep evaluating her needs and adapting our approach accordingly.
Case Study #2: T.G.
- The patient is a 13-year-old boy s/p non-traumatic SCI due to Acute Flaccid Myelitis with onset in 2018. The patient presents with worsening contractures in LE and weakness throughout UE and LEs. Since the last bout of care, the patient has been minimally participating in home program recommendations. The patient was last seen in this clinic 6 months ago, attending 2 out of 6 appointments, and was discharged early due to a high level of anxiety. The patient’s father and mother are the main caregivers.
- C4 AIS D
- Attends OT and PT 2x/week
The next case study is a 13-year-old boy who had a nontraumatic spinal cord injury due to acute flaccid myelitis or AFM onset in 2018. The patient presents with worsening contractors and lower extremity weakness throughout the upper and lower extremities. And since last battle of care, patient has been minimally participating in the home program. Recommendations. Patient was last seen in this clinic six months ago. He attended two out of six appointments and was discharged early to a high level due to a high level of anxiety, and patients father and mother remained caregivers. Currently, the patient is back for one to two hour belts of OTMPT two times a week.
- Questions/Concerns
- How would you approach this evaluation?
- What happened between the last bout of care vs now?
- What resources have been given to the family? Were they utilized?
- What have they utilized?
- How can we play a role to make sure the family and patient are getting the support they need?
Approaching the evaluation for this 13-year-old boy requires careful consideration of his age, psychosocial dynamics, and previous experiences with therapy. Before starting, I collaborated with the PT counterpart to optimize our approach. We decided to meet with the patient and family together initially, ensuring a supportive environment and addressing any concerns about anxiety openly.
Thankfully, the patient was receptive to discussing mental health, as he was already under treatment and medication. The family prioritized his mental well-being over physical therapy during the previous bout of care, leading to therapy cessation until he was ready. We discussed scheduling therapy sessions in advance to alleviate anxiety and ensure preparedness.
Inquiring about the resources provided and utilized by the family was crucial. They had engaged with a behavioral psychologist, which positively impacted the patient's readiness for therapy. Encouraging the family to take breaks during sessions and empowering the patient to advocate for himself were essential strategies.
To enhance home program compliance, I tailored activities to the patient's interests, such as modifying a video game controller to promote upper extremity movement. Additionally, I offered ongoing support and connected the family with relevant support services as needed.
By addressing the patient's mental health needs, ensuring clear communication and collaboration with the family, and customizing therapy interventions, we aim to optimize outcomes and support the patient's rehabilitation journey.
Case Study #3: C.B.
- The patient is a 43-year-old male s/p SCI due to MVC 2005. The patient attends therapy every 6-7 months and is able to turn neck and shrug shoulders, with minimal activation of scapular musculature, and uses a power chair via chin control. He typically has similar goals and evaluation results in each bout of care. Before the pandemic in 2019, patients had 8 hours of paid caregiving provided during the day. Since the pandemic, the patient has been unable to find assistance, and the mother has become the sole caregiver. His mother is requesting not to participate actively in this bout of care and using this time as her break.
- C4 AIS A
- Attends therapy 1x a week for 2 hours of OT
Approaching the case of this 43-year-old male with a spinal cord injury requires sensitivity to his functional limitations and the challenges he faces in accessing care, especially during the pandemic. Despite attending therapy infrequently, he demonstrates consistent abilities, primarily relying on a power chair controlled by chin movements.
The significant change since the pandemic is the absence of paid caregiving assistance, resulting in his mother assuming sole caregiver responsibilities. His mother's reluctance to actively participate in therapy is understandable, given her existing caregiving role and full-time employment. Respect for her boundaries is crucial while ensuring the patient receives optimal care.
Given the patient's c4 Asia A classification, therapy goals typically focus on maintaining and improving functional abilities within his limited range of motion. The reduced frequency of therapy sessions necessitates a targeted approach to maximize outcomes within the available time frame.
Exploring strategies to enhance independence and alleviate caregiving burden is paramount. This may involve modifying activities of daily living to accommodate his abilities and providing education and resources to support both the patient and his mother.
In conclusion, while the patient's therapy attendance is sporadic and the caregiving situation has evolved, our goal remains to optimize his functional abilities and support his overall well-being, respecting the boundaries and challenges his primary caregiver faces.
- Questions/Concerns
- How can we increase carryover at home?
- Are there other caregiver services available to the patient outside of mom?
- How do we respect mom’s role and educate importance of therapy to prevent secondary complications?
What questions can we use to increase carryover at home? Are there other caregiver services available for the patient outside of mom? How do we respect mom's rule and educate importance of therapy to prevent secondary complications? Some solutions I came up with were offering telehealth appointments to see if we could look how the home was set up and help increase exercise carryover. This proved to be challenging though, because the mother was expected to set up either an iPad or help with setting up zoom on the phone. We are still working on that.
We can assist them in finding free resources, programs, or partnerships with local grad programs. We've connected this with different institutes around us, providing more local resources and having our case manager on this. It's the same issues we're having over and over. There are limited services and resources available where he lives. We know it's a problem, but we're not sure how to solve it right now.
With the patient's permission, I am continuing to chat with the patient's mom to see if we can think of things outside the box.
Summary
Spinal cord injury presents unique challenges, and there's no one-size-fits-all solution for caregiver issues. It's essential to remain open-minded and collaborative in finding creative solutions that work best for each individual and their circumstances. Sharing ideas and experiences with colleagues and professionals in the field can lead to innovative approaches and support networks. I'm always eager to learn from others and discover new strategies to enhance patient care and support caregivers. So, if you have any insights or creative solutions, I'm all ears!
Exam Poll
Let's go over the exam. Please answer the poll questions.
1. What will those with a cervical spinal cord injury most likely need to complete upper body ADLs?
2. Which of the following is NOT a TRUE statement about a person with a T1-T5 spinal cord injury?
3. A person with an L1-L5 injury may need what assistance?
4. What are some SCI considerations?
5. What is NOT a caregiver challenge for this population?
Thanks for participating in the exam poll. The majority of you chose the correct answers.
Questions and Answers
Regarding case study number two, I love the "one week ahead of time" treatment plan. Did you have this created before seeing the patient in advance, or did you create next week's plan with the patient during the current session?
It depends on my thoughts about the patient or how that session went. Sometimes we would make it together, and sometimes I would say, "Hey, I really want to try this with you. What do you think?" I always give a choice of the type of stim or a new type of treatment. "What do you want to play?", "How do you want to have your arms set up?" or "Do you want to stay in your chair or on the mat?" I would always give him that choice that week in advance. Be aware that when patients or caregivers have anxiety, you can add to their anxiety by having them think about those plans a week in advance. So sometimes it might work better in the moment. In this particular case, we did it a week in advance.
References
Adhikari, S. P., Gurung, G., Khadka, B., & Rana, C. (2020). Factors influencing depression in individuals with traumatic spinal cord injury and caregivers' perceived burden in a low-income country: A cross-sectional study. Spinal cord, 58(10), 1112–1118. https://doi.org/10.1038/s41393-020-0451-5
Baker, A., Barker, S., Sampson, A., & Martin, C. (2017). Caregiver outcomes and interventions: A systematic scoping review of the traumatic brain injury and spinal cord injury literature. Clinical Rehabilitation, 31(1), 45–60. https://doi.org/10.1177/0269215516639357
Elliott, T. R., & Berry, J. W. (2009). Brief problem-solving training for family caregivers of persons with recent-onset spinal cord injuries: A randomized controlled trial. Journal of Clinical Psychology, 65(4), 406–422. https://doi.org/10.1002/jclp.20527
Hlabangana, V., & Hearn, J. H. (2020). Depression in partner caregivers of people with neurological conditions; associations with self-compassion and quality of life. Journal of mental health (Abingdon, England), 29(2), 176–181. https://doi.org/10.1080/09638237.2019.1630724
Jeyathevan, G., Cameron, J. I., Craven, B. C., Munce, S. E. P., & Jaglal, S. B. (2019). Re-building relationships after a spinal cord injury: Experiences of family caregivers and care recipients. BMC neurology, 19(1), 117. https://doi.org/10.1186/s12883-019-1347-x
Jeyathevan, G., Catharine Craven, B., Cameron, J. I., & Jaglal, S. B. (2020). Facilitators and barriers to supporting individuals with spinal cord injury in the community: Experiences of family caregivers and care recipients. Disability and Rehabilitation, 42(13), 1844–1854. https://doi.org/10.1080/09638288.2018.1541102
Juengst, S. B., Osborne, C. L., Holavanahalli, R., Silva, V., Kew, C. L., Nabasny, A., & Bell, K. R. (2019). Feasibility study of problem-solving training for care partners of adults with traumatic brain injury, spinal cord injury, burn injury, or stroke during the inpatient hospital stay. Archives of rehabilitation research and clinical translation, 1(3-4), 100009. https://doi.org/10.1016/j.arrct.2019.100009
Keihanian, F., Kouchakinejad-Eramsadati, L., Yousefzadeh-Chabok, S., & Homaie Rad, E. (2022). Burden in caregivers of spinal cord injury patients: A systematic review and meta-analysis. Acta neurologica Belgica, 122(3), 587–596. https://doi.org/10.1007/s13760-022-01888-2
Kent, E. E., Ornstein, K. A., & Dionne-Odom, J. N. (2020). The family caregiving crisis meets an actual pandemic. Journal of pain and symptom management, 60(1), e66–e69. https://doi.org/10.1016/j.jpainsymman.2020.04.006
Li, C. Y., Velozo, C. A., Hong, I., Li, C., Newman, J. C., & Krause, J. S. (2018). Generating Rasch-based activity of daily living measures from the Spinal Cord Injury Longitudinal Aging Study. Spinal cord, 56(1), 14–21. https://doi.org/10.1038/sc.2017.99
Lynch, J., & Cahalan, R. (2017). The impact of spinal cord injury on the quality of life of primary family caregivers: A literature review. Spinal cord, 55(11), 964–978. https://doi.org/10.1038/sc.2017.56
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with C1-3 Spinal Cord Injury (Pamphlet), Washington, DC.
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with C4 Spinal Cord Injury (Pamphlet), Washington, DC.
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with C5 Spinal Cord Injury (Pamphlet), Washington, DC.
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with C6 Spinal Cord Injury (Pamphlet), Washington, DC.
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with C7-8 Spinal Cord Injury (Pamphlet), Washington, DC.
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with T1-9 Spinal Cord Injury (Pamphlet), Washington, DC.
Paralyzed Veterans of America. (2002). Expected outcomes: What you should know: A guide for people with L2-S5 Spinal Cord Injury (Pamphlet), Washington, DC.
Pilusa, S., Myezwa, H., & Potterton, J. (2019). Prevention care for secondary health conditions among people living with spinal cord injuries: research protocol. BMC research notes, 12(1), 179. https://doi.org/10.1186/s13104-019-4202-7
Ryerson Espino, S. L., O'Rourke, K., Kelly, E. H., January, A. M., & Vogel, L. C. (2022). Coping, social support, and caregiver well-being with families living with SCI: A mixed methods study. Topics in spinal cord injury rehabilitation, 28(1), 78–98. https://doi.org/10.46292/sci21-00013
Shepherd Center (n. d.). Understanding spinal cord injury. Retrieved from https://www.spinalinjury101.org/
Smith, E. M., Boucher, N., & Miller, W. C. (2016). Caregiving services in spinal cord injury: a systematic review of the literature. Spinal cord, 54(8), 562–569. https://doi.org/10.1038/sc.2016.8
Tien, N. L. B., Thanh, V. V., Hanh, K. T. H., Anh, P. G., Huyen, L. T. M., Tu, N. T., Mai, D. T. N., & Toi, P. L. (2021). Quality of life and activities of daily living among patients with complete cervical spinal cord injury and surgical treatment in Vietnam. International journal of environmental research and public health, 18(18), 9703. https://doi.org/10.3390/ijerph18189703
Tough, H., Brinkhof, M. W. G., Siegrist, J., Fekete, C., & SwiSCI Study Group (2019). Social inequalities in the burden of care: a dyadic analysis in the caregiving partners of persons with a physical disability. International journal for equity in health, 19(1), 3. https://doi.org/10.1186/s12939-019-1112-1
Uhm, K. E., Jung, H., Woo, M. W., Kwon, H. E., Oh-Park, M., Lee, B. R., Kim, E. J., Kim, J. H., Lee, S. A., & Lee, J. (2023). Influence of preparedness on caregiver burden, depression, and quality of life in caregivers of people with disabilities. Frontiers in public health, 11, 1153588. https://doi.org/10.3389/fpubh.2023.1153588
Citation
McCool, A. (2024). Caregiving for the spinal cord injury patient. OccupationalTherapy.com, Article 5697. Available at www.occupationaltherapy.com
