Editor's note: This text-based course is a transcript of the webinar, Occupational Therapy’s Role In Bowel And Bladder Management For Individuals With Spinal Cord Injury, presented by Yvonne Monti, OTD, OTR/L.
Learning Outcomes
- After this course, participants will be able to:
- Identify SCI-specific deficits that may interfere with the client's management of bowel and bladder function.
- Recognize the role of OT in improving independence in bowel and bladder management.
- List three possible OT intervention strategies for individuals with SCI to self-manage bowel and bladder.
Introduction
It's nice to be back. Thank you for joining me today.
SCI Incidence
- 282,000 SCI patients in the US.
- 54 new cases per million annually
- Bowel and bladder dysfunction occur in more than 80% of individuals with SCI
- Presentation based on level of injury and completeness
(Perez et al., 2022)
In the United States, there are approximately 282,000 individuals currently living with spinal cord injuries, and each year sees 54 new cases per million people. Among this population, it's estimated that a significant majority, around 80%, experience some degree of bowel dysfunction. Additionally, between 70% and 80% of individuals with spinal cord injuries also face challenges related to bladder dysfunction.
It is crucial to recognize that the nature and severity of bowel and bladder dysfunction can vary greatly from one person to another within the spinal cord injury community. This variation is influenced by several factors, including the level of spinal cord injury, the extent of neurological damage, and individual physiological differences. These diverse factors play a substantial role in how these dysfunctions manifest and are managed in each individual case.
Multidisciplinary SCI Team
- OTP is an important part of the multidisciplinary team
- Patients, caregivers, physicians, nurses, physical therapists, dieticians, psychologists, social workers, and other healthcare professionals
- Treatment throughout the continuum of care
- Days to years following the injury
Occupational therapy practitioners hold a crucial position within the multidisciplinary spinal cord injury team. This team comprises not only the patients themselves but also their caregivers, alongside a diverse range of healthcare professionals such as nurses, physical therapists, dieticians, psychologists, social workers, and others. Together, they collaborate to address the complex needs of individuals dealing with spinal cord injuries.
Occupational therapy practitioners fulfill a vital role by providing interventions that span the entire spectrum of care, from the initial days following the injury through to the long-term management over the course of years.
OTP Role in SCI Education
- OT SCI education with clear ADL domains may improve rehab outcomes (Mostafa, Plastow, & Savin-Baden, 2020)
- Early and often
- Initial education and reinforcement from the team
- Meet the patient where they are; coping with a new injury is difficult
- Education of patients and caregivers
- The more educated you are as a practitioner, the better you can educate
It's essential to grasp that our primary role in supporting patients dealing with bowel and bladder dysfunction after spinal cord injuries revolves around education. We offer initial guidance to aid in managing these issues and reinforce the education provided by the broader healthcare team. It's crucial to initiate and maintain a continuous process of education for both patients and their caregivers. So, when I refer to education throughout this presentation, remember that it extends to both patients and their support network.
We're all aware of the immense emotional and practical challenges that come with coping after a spinal cord injury. Many patients may initially be resistant and not ready to assume full responsibility for their bowel and bladder management, especially during their acute hospital stay. This is precisely why we emphasize the importance of ongoing education throughout their entire care journey. In the upcoming presentation, I'll delve into the occupational therapist's role in more detail. But before we do that, let's begin with a review of the anatomical structures, processes, neurological interventions, and innervations related to bowel and bladder function. This foundational knowledge will not only enhance our understanding but also equip us to better educate our clients effectively.
OT Goals for SCI Care
- Improve occupational performance and participation
- Adapt/modify
- Improve health, wellness, and quality of life
- Prevention of further complications related to the condition
Occupational therapy in the context of spinal cord injury care is inherently client-centered, as we all understand as occupational therapists. Our profession is rooted in the principles of helping individuals achieve their highest level of participation and performance in meaningful daily activities, which we refer to as "occupations."
In this specific context, our goals are squarely centered around the occupations of toileting, bowel management, and bladder management. We recognize that these activities are not just essential for daily life but are also deeply personal and impactful on an individual's well-being. Therefore, our approach involves tailoring interventions to meet the unique needs of each patient.
Occupational therapy practitioners are dedicated to assisting our patients with spinal cord injuries in several key ways. Firstly, we aim to improve their overall health, well-being, and quality of life. This encompasses not only the physical aspects of care but also the emotional and psychological dimensions of adjustment and coping.
Furthermore, our interventions are designed with a preventive mindset. We understand that spinal cord injuries can carry long-term risks and complications, and our efforts extend to minimizing these potential issues. By addressing toileting and bowel and bladder management comprehensively, we strive to enhance our patients' long-term health outcomes and minimize the risk of future complications related to their spinal cord injury.
Case Example
- Name: John Smith
- Age: 32
- Diagnosis: Spinal cord injury (level T7, complete). Occupation: Office administrator
- Living Situation: Lives in a two-story house with his spouse and two children
- Background: John Smith sustained a T7 SCI from MVA 6 months ago, resulting in complete paraplegia. Since the accident, John has been using a manual wheelchair for mobility and requires assistance with various ADLs. He has regained some upper body strength and has limited sensation and movement below the level of injury.
John Smith is a 32-year-old individual with a T7 complete spinal cord injury, the location as seen in Figure 1. This case example will serve as a valuable reference point for applying the intervention strategies discussed later in the presentation.
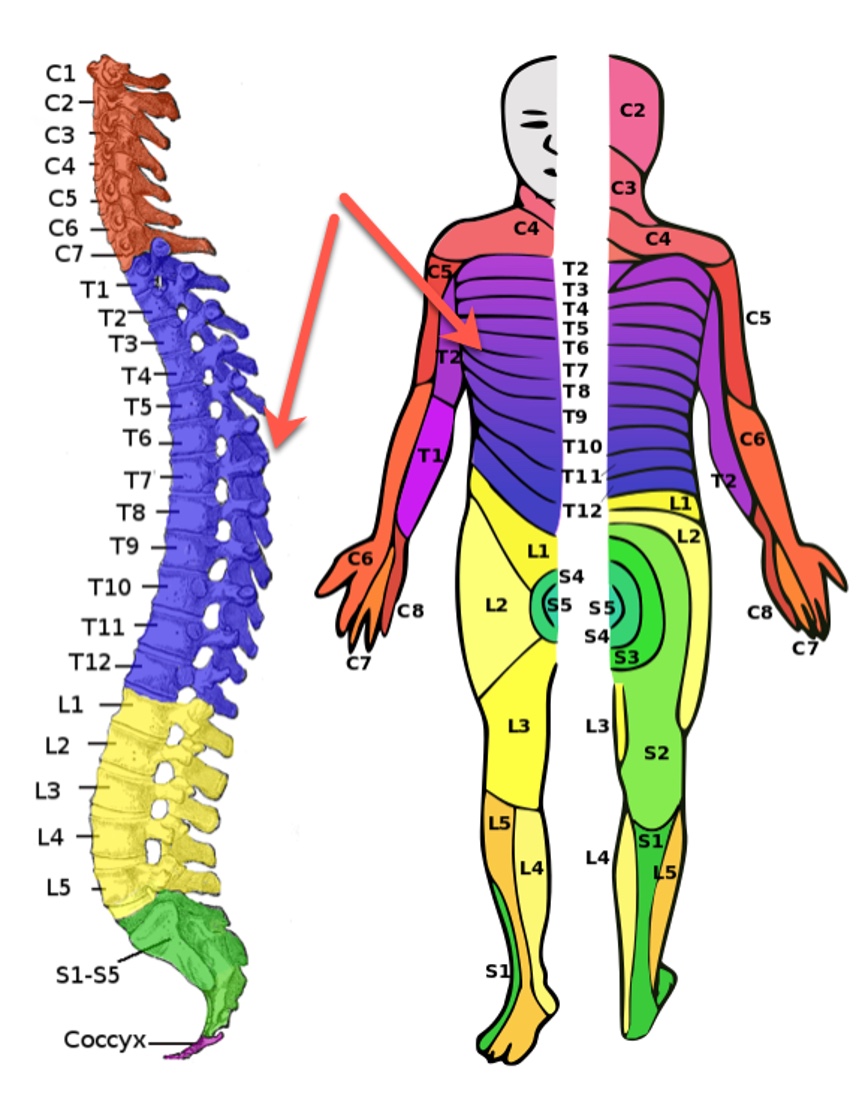
Figure 1. Location of the spinal cord injury for the case study (Image: Ralf Stephan, Public domain, via Wikimedia Commons).
John is an office administrator who resides in a two-story house with his spouse and two children. Six months ago, he had a car accident resulting in a complete T7 spinal cord injury. As a consequence, he now faces complete paraplegia. John utilizes a manual wheelchair for mobility and requires assistance with various activities of daily living. While he has made some progress in regaining upper body strength, he still experiences limited sensation and movement below the level of his spinal cord injury.
- John is experiencing difficulties with bowel and bladder management.
- He has unpredictable bowel movements and struggles with controlling his bladder.
- These issues are affecting his overall independence and quality of life, and he is eager to find strategies to manage his bowel and bladder function effectively.
- His wife has been assisting with catheterization and bowel care; however, he would like to complete toileting independently.
John is encountering challenges related to bowel and bladder management, which are affecting his daily life and his goal of returning to work. He experiences unpredictable bowel movements and accidents, as well as difficulties managing his bladder with occasional incontinence. These issues are impeding his independence and significantly impacting his overall quality of life.
At present, John's wife is primarily responsible for his bowel and bladder care. However, John has a strong desire to regain some autonomy in these aspects of his life. He aims to be able to manage his catheterization independently in public settings and perform his bowel care on his own. This desire for increased self-sufficiency is a crucial aspect of his rehabilitation and should guide our intervention strategies.
- Goals:
- John wants to establish a predictable bowel routine to manage his bowels effectively, reduce accidents, and promote independence.
- John aims to regain control over his bladder to minimize accidents and improve his ability to self-catheterize independently.
- John wants to gain the skills necessary to manage his bowel and bladder independently to enhance his overall independence in daily activities and quality of life.
John's goals are crystal clear. He's determined to establish a predictable bowel routine, regain control over his bladder, and develop the necessary skills to manage both his bowel and bladder independently. All of these goals are geared towards enhancing his overall independence in daily activities and improving his quality of life.
We'll keep John's aspirations in mind as we progress through the presentation and revisit them at the end to formulate tailored interventions that can help him achieve these objectives effectively.
Normal Urinary System Review
Let's begin by reviewing the normal urinary system. This foundational understanding will serve as a valuable reference point as we delve into the complexities of managing urinary dysfunction in the context of spinal cord injury.
Urinary System Overview
- Divided into upper and lower tract
- Upper tract: two kidneys and the ureters: T12-L3 level intervention
- Lower tract: portion of distal ureters, bladder, and urethra
- Filling of the bladder: sympathetic innervation T10-12
- Ureters T12–L2 level intervention
- Parasympathetic innervation S2–S4
(Perez et al., 2022)
The urinary system can be categorized into two tracts: the upper tract, consisting of the kidneys and ureters, which receives innervation from T12 to L3, and the lower tract, encompassing the distal ureters, bladder, and urethra, which reaches full innervation at S4. Sympathetic innervation for bladder filling comes from T10 to T12, while innervation for the ureters is at T12 to L2, and parasympathetic involvement occurs from S2 to S4.
- Kidneys: filter water, electrolytes, and waste from the blood, creating urine
- Urine is drained by ureters to the bladder, where stored
- Involuntary flow of urine from bladder to urethra controlled by internal urethral sphincter
- The detrusor muscle of the bladder contracts to release urine and relaxes to store urine
- The voluntary flow of urine is controlled by the external urethral sphincter controls
(Perez et al., 2022)
The kidneys perform the vital function of filtering water, electrolytes, and waste from the blood to create urine. This urine is subsequently transported through the ureters and stored in the bladder. The urinary system employs two sphincters to control the flow of urine: the internal urethral sphincter, which manages involuntary urine release from the bladder, and the external urethral sphincter, responsible for voluntary control over this process. Additionally, the detrusor muscle, a smooth muscle within the bladder, contracts to release urine and relaxes to facilitate urine storage.
Neurological Urinary Structures
- Pontine Micturition Center (PMC)
- Located in pons
- Contraction of detrusor muscle
- Relaxation of internal urethral sphincter
- The frontal cortex inhibits PMC to allow the bladder to fill until the appropriate time to void
- Sacral micturition center- controls bladder and sphincters- voiding reflex
(Perez et al., 2022)
Understanding the neural control of the urinary system involves examining the intricate interaction between the brain and the spinal cord.
The Pontine Micturition Center (PMC) is located in the pons and plays a central role in urination. It coordinates the contraction of the detrusor muscle (bladder muscle) and the relaxation of the urethral sphincter to enable voiding.
The frontal cortex of the brain has the crucial function of inhibiting the PMC, allowing the bladder to fill until the individual is ready to void. You can think of this as the brain's control over bathroom breaks during those long car rides.
In the sacral spinal cord, we find the sacral micturition center, which is responsible for the voiding reflex and the parasympathetic innervation of the lower urinary tract, as we discussed earlier.
Normal Urinary Function
- Requires communication between the PMC, sacral spinal cord, and lower urinary tract
- As the bladder fills, stretch and pain receptors send signals to S2–S4 level
- Signals sent to cortical structures to convey bladder filling or the need to urinate
- PMC triggers the lower urinary tract to allow for complete emptying of the bladder
(Perez et al., 2022)
Normal urinary function requires that all of the structures communicate. Figure 2 shows the normal urinary structures.
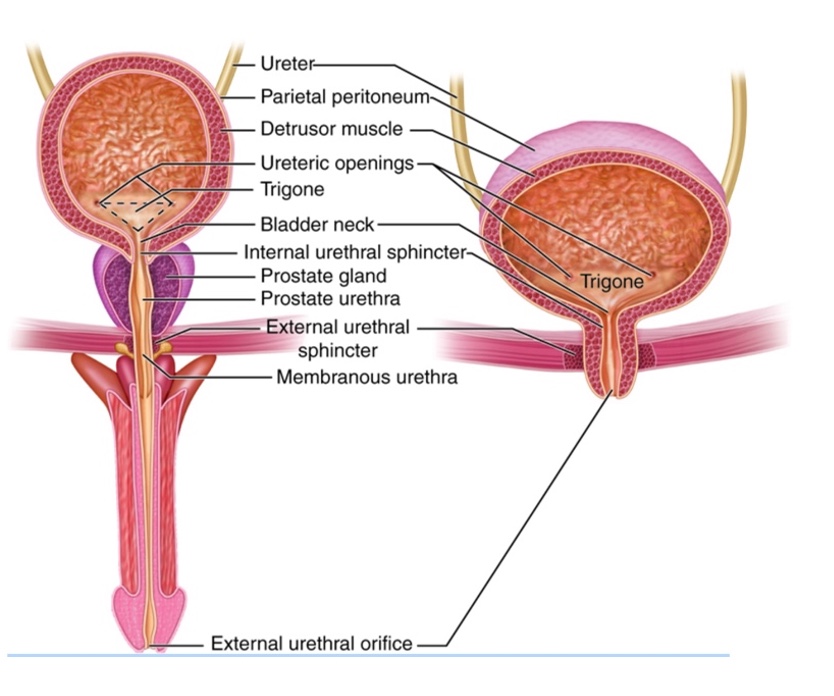
Figure 2. Structures of the urinary system (Image source: This work by Cenveo is licensed under a Creative Commons Attribution 3.0 United States (https://creativecommons.org/licenses/by/3.0/us/).
Now, let's delve into how bladder function can be affected following a spinal cord injury, leading to what's known as a neurogenic bladder. This condition is often categorized based on the level of the spinal cord injury and can be classified into three main categories: supra-sacral (above the sacrum), mixed, and sacral and infra-sacral. These distinctions help us understand and manage the diverse presentations of neurogenic bladder that individuals with spinal cord injuries may experience.
Neurogenic Bladder Based on Spinal Cord Injury
- Supra-sacral, Mixed, or Sacral/Infra-sacral
Spinal cord injuries can impact bladder function, leading to the development of a neurogenic bladder. This condition is typically categorized based on the level of the spinal cord injury and can be classified into three primary categories: supra-sacral (above the sacrum), mixed, and sacral and infra-sacral. These distinctions help us understand the diverse manifestations of the neurogenic bladder that individuals with spinal cord injuries may encounter.
Suprasacral Spinal Cord Injury: UMN Lesion
- Urine storage dysfunction
- Sacral reflex arc and PMC stay intact- SCI prohibits communication
- Disinhibition of sacral micturition reflex arc
- Detrusor muscle and urethral sphincter hyperreflexia (spasticity)
- Detrusor sphincter dyssynergia (DSD) and increased bladder pressures
- Upper urinary tracts at risk
- Incontinence
In cases of supra-sacral spinal cord injury, which involves damage or lesions above the sacral level of the spinal cord, the upper motor neuron pathway is affected. While the sacral reflex arc and the Pontine Micturition Center (PMC) remain intact, communication between the two is disrupted due to the spinal cord injury. This disruption results in the disinhibition of the sacral micturition reflex arc.
Characteristics commonly associated with this type of spinal cord injury and neurogenic bladder include increased muscle tone in the bladder, leading to spasticity and involuntary contractions of the bladder. These involuntary contractions can result in decreased bladder capacity, meaning the bladder cannot hold as much urine.
Another significant feature in supra-sacral spinal cord injuries is detrusor-sphincter dyssynergy. In normal bladder function, the detrusor muscle is responsible for bladder contraction, while the external urethral sphincter controls the release of urine from the bladder. However, in supra-sacral spinal cord injuries, there's a loss of coordination between these two structures, leading to dyssynergia and contractions. This can result in the bladder contracting while the sphincter remains closed, making it difficult to fully empty the bladder.
Additionally, supra-sacral spinal cord injuries may lead to an overactive bladder reflex, causing involuntary emptying of the bladder when it reaches a certain level of filling. This results in urinary incontinence, where the bladder fills to a specific point and then involuntarily releases urine.
Mixed SCI: UMN and/or LMN Lesion
- Urine storage dysfunction
- Conus medullaris or cauda equina
- Supraspinal disinhibition of the sacral micturition reflex can occur or be eliminated as a result of sacral root injury
- High bladder pressure may lead to upper urinary tract damage
- Urinary incontinence can occur
A mixed spinal cord injury, characterized by both upper motor neuron and lower motor neuron lesions, can manifest in various ways and impact bladder function differently based on the level and extent of the spinal cord injury. It's crucial to emphasize that the nature of bladder dysfunction in mixed spinal cord injuries can vary significantly depending on the specific location and severity of the injury. This variation may result in high bladder pressures or incontinence, and high bladder pressures can pose risks to the upper urinary tracts.
Mixed lesions can sometimes be associated with conus medullaris syndrome, which affects both the spinal cord and the cauda equina. This syndrome can introduce additional complexities to bladder dysfunction.
Lastly, the third type of neurogenic bladder we should mention is related to sacral or infra-sacral spinal cord injuries with lower motor neuron lesions. Bladder function can also be significantly affected in these cases.
Sacral/Infra-Sacral SCI: LMN Lesion
- Voiding dysfunction
- Voiding reflex arc disrupted, PMC remains intact
- Detrusor muscle flaccid
- External urethral sphincter flaccid
- Bladder increased volume
- Overflow incontinence
- The location of SCI lesions can help predict symptoms and diagnose urinary problems
(Perez et al., 2022)
In cases of sacral or infra-sacral spinal cord injury with lower motor neuron lesions, there is a disruption in communication between the bladder and the spinal cord. The resulting effects on bladder function can differ depending on the level and severity of the injury, but some common issues include a loss of muscle tone in the bladder. This leads to what is known as a flaccid, atonic, or underactive bladder. In this condition, the bladder may not contract effectively, resulting in incomplete emptying and urine retention. This increased retention of urine can elevate the risk of urinary tract infections and the formation of bladder stones.
The urinary system is illustrated in Figure 3 to provide a visual reference.
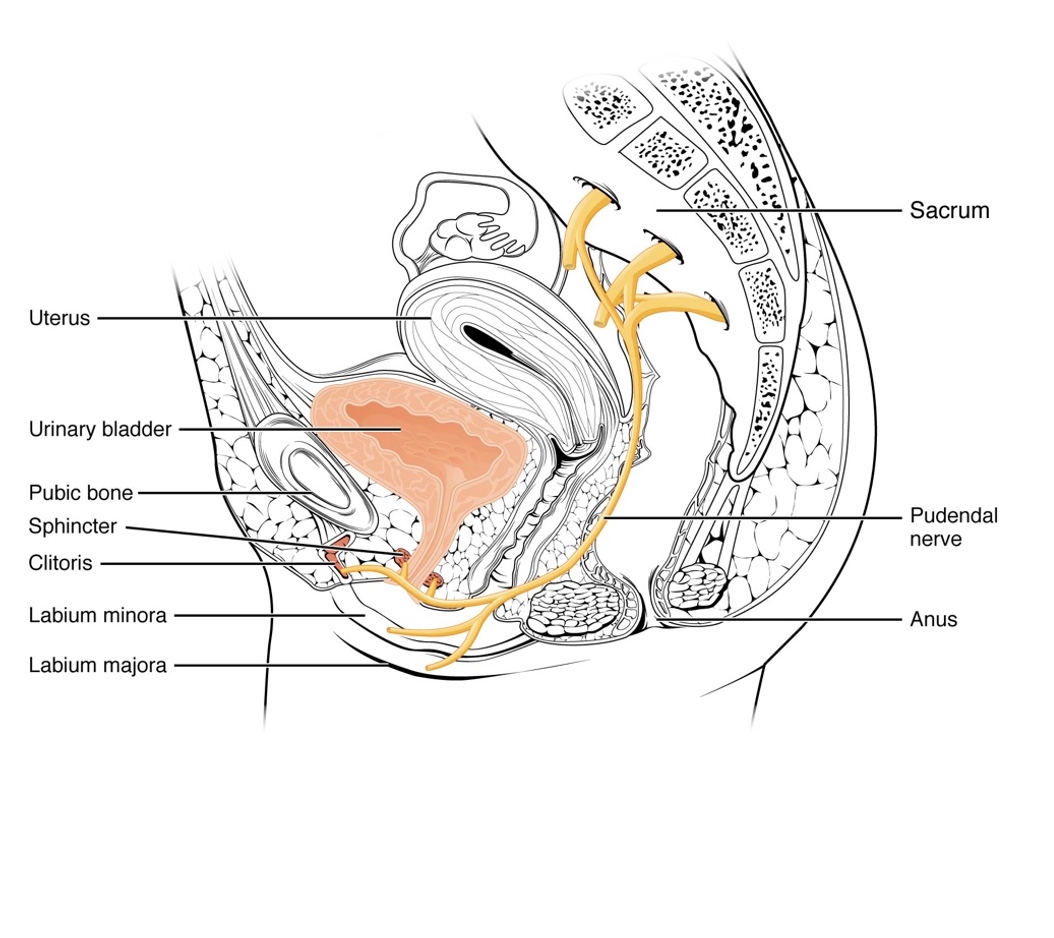
Figure 3. Illustration of the urinary system (Image source: OpenStax College, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons).
In certain cases, the bladder may become overfilled and unable to contract properly, causing urine to overflow and resulting in involuntary leakage or dribbling of urine. Additionally, the nerves responsible for transmitting sensory information from the bladder to the brain may also be affected, leading to a loss of sensation. This loss of sensation can make it challenging for individuals to perceive when their bladder is full or empty.
These are the three primary types of neurogenic bladder dysfunction. Now, let's explore how we manage neurogenic bladder to address these various challenges and improve the quality of life for individuals affected by spinal cord injuries.
Management of Neurogenic Bladder: Urinary Catheterization
- Clean Intermittent Catheterization (CIC): Best practice for preventing UTIs
- Indwelling urethral catheter (IUC) and suprapubic catheters (SPC) remain in the body for several weeks at a time
- SPC Advantages:
- No urethral trauma
- No catheter-induced urethritis
- Sexual function is not interrupted
- Bowel incontinence less likely to contaminate
(Perez et al., 2022)
Clean, intermittent catheterization (CIC) stands as the gold standard in bladder care and is considered the best practice for preventing urinary tract infections (UTIs) in individuals with spinal cord injuries. It distinguishes itself by not involving the long-term use of indwelling catheters, offering more natural bladder filling and voiding cycles.
Clean intermittent catheterization, or CIC, enables individuals to maintain a more normal lifestyle, facilitates greater mobility, eases transfers, and allows for more regular participation in sexual activities. In contrast, indwelling urethral catheters (those inserted through the urethra) and supra-pubic catheters (which remain in place for several weeks) increase exposure to bacteria and the risk of UTIs.
It's worth noting that recent studies suggest that the risk of UTIs may be comparable between supra-pubic catheters and clean intermittent catheterization. When helping patients make decisions, this information can be essential. Both indwelling and supra-pubic catheters can lead to bladder atrophy because they bypass the natural bladder function.
Supra-pubic catheters are inserted through a small hole in the abdomen above the pubic bone and are connected to a drainage bag. They offer advantages over indwelling urethral catheters, including no urethral trauma, no urethritis, uninterrupted sexual function, and lower susceptibility to contamination from bowel incontinence due to their location.
The choice between catheterization methods should be based on individual needs and recommendations from medical specialists. What works best for one person may not work for another, emphasizing the importance of providing education and guidance when patients are deciding on their preferred method of bladder management.
It's important to acknowledge the unique challenges individuals with spinal cord injuries face when it comes to self-catheterization or receiving assistance from a caregiver. Factors such as gender, access to the urethra, body size, visualization of the urethra, clothing management, and the nature of the injury can all impact the choice of catheterization method. These challenges can lead patients to make decisions and switch from clean intermittent catheterization to other methods based on their specific needs and circumstances.
- 70% of SCI patients change methods from CIC secondary to inconvenience and incontinence
- CIC and SPC have a comparable risk of UTI
(Perez et al., 2022)
The fact that 70% of patients transition from clean intermittent catheterization to another method to enhance their lifestyle, convenience, and reduce incontinence underscores the importance of adapting bladder management approaches to individual needs and preferences.
What is the role of occupational therapy practitioners in the context of clean intermittent catheterization (CIC)? While the actual catheterization procedure is typically carried out by nurses, occupational therapists play a crucial role in providing support and education to individuals with spinal cord injuries to promote their independence in managing their bladder function.
Occupational therapy practitioners can offer valuable contributions, such as education on catheter options, technique training for clean intermittent catheterization, guidance on adaptive strategies, and psychosocial support to address the emotional and lifestyle aspects of catheterization. This comprehensive approach empowers patients to make informed decisions, maintain independence, and enhance their overall quality of life.
OTP Role in CIC
- Education and Training:
- Reinforce catheterization techniques for safe, effective performance
- Proper hygiene practices and clean techniques
- Different types of catheters and their use/advantages
- Proper fluid intake
- Help patients advocate for insurance coverage
- Equipment Selection and Modification:
- Provide and instruct AE based on limitations for cathing and clothing management
- Modify equipment to improve optimal function and independence
OTPs can help individuals choose appropriate catheterization equipment based on their physical abilities and limitations. They may also recommend or assist in modifying equipment to ensure optimal function and independence during catheterization.
- Adaptive Techniques:
- Teach adaptive techniques and strategies for C5-C8 or those with limited reach
- Create assistive devices or develop alternative methods to manipulate the catheter and clothing
- Upper Extremity Rehabilitation:
- Interventions to improve UE function and strength to enhance their ability to perform catheterization
For individuals with limited hand function, such as those with C5 to C8 spinal cord injuries or individuals with paraplegia and limited reach, occupational therapy practitioners (OTPs) can provide valuable instruction on adaptive techniques and strategies to enable independent catheterization. These strategies may involve the use of assistive devices or the development of alternative methods to grasp and manipulate the catheter.
An illustrative example of such an adaptive technique can be seen in Figure 4.

Figure 4. An adaptive device to hold a catheter (Amazon).
OTPs can provide rehabilitation interventions to improve upper limb function and strengthening, which can enhance a person's ability to perform self-catheterization.
- Functional Independence:
- Promote independence in ADLs
- Develop strategies to incorporate into daily routines
- Address environmental barriers, such as bathroom accessibility and clothing management
- Promote time management skills for regular, timely catheterization
- Psychosocial Support:
- Address emotional or psychosocial concerns
- Collaborate with healthcare professionals to provide additional support
Occupational therapy practitioners (OTPs) have a primary focus on promoting independence in daily activities, and this extends to helping individuals incorporate catheterization into their daily routines effectively. It's not just about teaching the technical aspects; it's about assisting them in integrating this essential aspect of self-care into their lives. This is precisely what OTs excel at.
This assistance may encompass addressing environmental barriers, such as ensuring bathroom accessibility or managing clothing-related issues. For example, if someone wants to go shopping at a store like Target but is unsure how to catheterize in that environment, OTPs can help them figure out the logistics, including what to wear and how to manage their clothing. This problem-solving approach is a core aspect of occupational therapy practice.
Additionally, OTPs can help patients develop time management skills to ensure regular and timely catheterization, which is crucial when managing bladder function. Furthermore, occupational therapists can provide essential psychosocial support, addressing any emotional or psychosocial concerns related to self-catheterization, particularly if individuals rely on a loved one or caregiver to perform the activity for them. OTs are skilled at recognizing when referrals to other healthcare professionals are necessary and can collaborate effectively with the broader multidisciplinary team to provide comprehensive care and support to patients.
AE for Self-Catheterization
- Adaptive catheterization equipment
- Cuffed catheter inserter vs. U-cuff
- Mirror with or w/o leg spreader
- Wishbone labia spreader
- Penis support
- Adapted container to empty urine into
- Adapted scissors to open packaging
- Self-lubricated catheters
- Pumped lubricant
- Adaptive equipment for clothing management
- Pants holder for wheelchair
- Modified clothing
Occupational therapists (OTs) have a strong affinity for adaptive equipment, and they excel in assessing, recommending, and even crafting solutions to meet individual needs. When it comes to optimizing performance in bladder care, OTs can collaborate with patients to identify the adaptive equipment that will best suit their requirements. Figure 5 provides examples of such adaptive equipment solutions.

Figure 5. Adaptive equipment solutions for catheterization.
Occupational therapists are known for their resourcefulness in finding or creating adaptive equipment to enhance the independence of their patients, particularly in tasks like catheterization. Examples of such equipment include:
A wishbone labia spreader is a device often made from splinting material, that helps individuals with limited hand function spread the labia, making it easier to access the urethra for catheterization.
A penis support or penis prop is designed for one-handed catheterization. This device holds the penis in place, allowing individuals to perform the procedure independently.
A cuffed catheter inserter assists with catheter insertion, providing better control and precision during the process.
A mirror with a leg spreader can be helpful for individuals with limited mobility by facilitating access to the urethra.
Some patients may use capped containers, such as empty water bottles, for urine collection. OTs can adapt containers to meet the patient's needs.
Modified scissors make it easier for individuals with limited hand function to open catheter packaging, ensuring a sterile and safe procedure.
Self-lubricating catheters are especially beneficial for individuals with tetraplegia and limited hand function. Self-lubricating catheters simplify the process and reduce friction during insertion.
Unlike traditional squeeze lubricants, pumped lubricants can be easier to manage for individuals with limited hand dexterity.
There is a wide range of adaptive clothing available designed to simplify catheterization and other self-care tasks.
Please note that this list is not exhaustive, and OTs continuously explore and develop innovative solutions to meet the unique needs of their patients. If you have additional adaptive equipment suggestions or questions, please feel free to reach out.
Management of Neurogenic Bladder: Surgical Procedures
Surgical procedures like bladder augmentation and urinary diversion are important to understand because they may be relevant for patients with specific bladder issues. These procedures are typically considered for candidates who have high bladder pressures and poor detrusor compliance, inadequate responses to medical management, or frequent urinary tract infections (UTIs). These surgical interventions aim to address these issues and provide alternative solutions for bladder management.
Bladder Augmentation and Urinary Diversion
- Who is a candidate?
- Patient with high bladder pressures and poor detrusor compliance
- Poor medical management
- What is it?
- A larger urine reservoir created from part of the bowel or appendix
- Stoma created to catheterize through with diversion from:
- Appendiceal vesicostomy: Mitrofanoff procedure
- Ileal vesicostomy: Yang-Monti procedure
Bladder augmentation is a surgical procedure performed when the bladder lacks sufficient capacity to hold an adequate amount of urine, leading to issues like frequent urination, urinary incontinence, or urinary retention. During this procedure, a segment of the bowel, typically the small intestine, is reshaped into a pouch and connected to the existing bladder. This reshaping enlarges the bladder's capacity to hold urine, reducing urinary frequency and decreasing incontinence. In some cases, a portion of the original bladder may be removed as part of the procedure.
There are two different types of urinary diversion procedures used in the field of urology to create an alternative route for bladder drainage. The first one is the Mitrofanoff procedure, as shown in Figure 6.
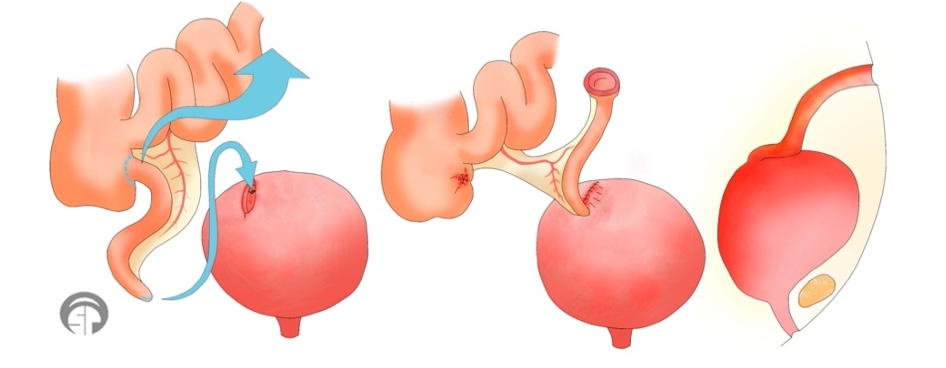
Figure 6. Illustration of the Mitrofanoff procedure
In the Mitrofanoff procedure, the appendix is used to create a channel between the bladder and the abdomen. The appendix is detached from its original location and reattached to the bladder. The other end of the appendix is brought out through a small opening in the abdomen, often in the belly button, forming a stoma. A catheter can then be inserted through the stoma to drain urine from the bladder. This method provides a more accessible and independent way to manage catheterization, which is especially beneficial for individuals who have difficulty accessing their urethra, such as women or those with tetraplegia.
The Yang-Monti procedure involves using a segment of the small intestine, typically the ileum, to create a conduit for urinary drainage. A section of the ileum is isolated and formed into a tube. One end of the tube is connected to the bladder, while the other end is brought out through the abdominal wall, creating a stoma. This procedure is an alternative when the appendix is not available or sustainable.
These surgical procedures aim to provide individuals with improved bladder management options and greater independence in catheterization.
- Why do it?
- Less urinary symptoms
- Less bladder management problems
- Increased satisfaction with their urinary function
- Possible complications: leakage of anastomosis, infection, UTI, bowel obstruction, ileus
- Improves occupational participation
(Perez et al., 2022)
Patients may opt for bladder augmentation or diversion as an alternative to clean intermittent catheterization. It's essential to note that approximately 70% of patients who initially use clean intermittent catheterization eventually explore other options, which can include supra-pubic catheters or different catheterization methods like bladder augmentation or diversion.
The benefits of bladder augmentation or diversion include a reduction in urinary symptoms, particularly with bladder augmentation, which can lead to less frequent urination and improved bladder management. Patients often report increased satisfaction with their urinary function after these procedures.
However, there are potential complications to consider, such as stoma leakage, infections, urinary tract infections (UTIs), and the risk of bowel obstruction or ileus, especially when the bowel is used in the procedure.
One significant advantage of bladder augmentation or diversion is the enhancement of occupational participation. These procedures can reduce the need for complex clothing management, making it easier for individuals to independently access and manage their urinary function.
OT Role in Bladder Diversion
- Education, Counseling, and Training:
- Provide education about the procedure
- Care and management of the stoma, drainage systems, skin hygiene
- Address concerns with coping with body image issues, self-esteem, and sexuality
- Guidance on selecting and using specialized clothing, ostomy pouches, and accessories to ensure comfort and ease of use
Our role in urinary diversion involves several key responsibilities.
Occupational therapy practitioners are instrumental in educating patients about the urinary diversion procedure. This education encompasses a thorough discussion of the potential risks and benefits associated with the surgery. It is crucial for patients to have a comprehensive understanding of what they can expect.
OTPs play a vital role in instructing patients on how to effectively manage and care for their stoma. This includes providing guidance on proper stoma hygiene and maintenance to prevent complications.
Occupational therapists provide essential psychosocial support to patients undergoing urinary diversion. They address emotional and psychological concerns that patients may experience in relation to the procedure. This can encompass body image issues, which may actually improve as a result of the surgery, potentially leading to increased self-esteem and enhanced sexuality.
OTPs assist patients in acquiring adaptive clothing and devices that may be necessary to effectively manage their new catheterization strategies. This includes recommending and facilitating the procurement of adaptive equipment to enhance patients' independence and comfort.
By fulfilling these roles, occupational therapy practitioners significantly contribute to the overall well-being and successful adaptation of patients undergoing urinary diversion procedures.
Neurogenetic Bladder Complications: Autonomic Dysreflexia
- Life-threatening hypertensive crisis
- Triggered by noxious stimuli below the level of SCI
- T6 and higher
- Symptoms include:
- Increase in systolic BP of >20mmHG
- Blurred vision
- Sweating and flushing above lesion
- Goosebumps
- Pounding headache
- Bradycardia
(Perez et al., 2022)
Complications related to the bladder can include autonomic dysreflexia, which is a critical medical emergency. It can occur in individuals with spinal cord injuries above the T6 level. This condition is characterized by a sudden, excessive response of the autonomic nervous system to a noxious stimulus below the level of the spinal cord injury. Symptoms of autonomic dysreflexia include hypertension (high blood pressure), a pounding headache, profuse sweating, flushing of the skin, blotching of the skin, goosebumps, nasal congestion, bradycardia (slow heart rate), and feelings of anxiety, impending doom, or restlessness.
Healthcare professionals, especially those working with spinal cord injury patients, are well-versed in recognizing and managing autonomic dysreflexia due to its potential life-threatening nature.
- Most Common Cause:
- Bladder distension
- Bladder or kidney stones
- Obstructed indwelling bladder catheter
- Catheterization itself
- Detrusor sphincter dyssynergia
- UTI
- Second Leading Cause:
- Bowel-related stimulus
- Bowel distension
- Bowel impaction/obstruction
- Bowel care reflexes
(Perez et al., 2022)
It's crucial for occupational therapists and healthcare professionals to recognize the symptoms of autonomic dysreflexia (AD) and take immediate action to address the underlying cause, as AD is often associated with the bladder. The most common causes of AD related to the bladder include bladder distension, kidney stones, bladder stones, an obstructed catheter, catheterization itself, dyssynergia, and urinary tract infections (UTIs).
The second leading cause of AD is related to bowel issues, which we'll discuss later. Bowel-related stimuli such as bowel distension, impaction, or obstruction, as well as bowel care procedures, can also trigger autonomic dysreflexia. Therefore, both bladder and bowel care can potentially lead to AD in individuals with spinal cord injuries above the T6 level. Recognizing and addressing these triggers is essential to prevent serious complications.
OT Role in AD Prevention
- Education and Training:
- Educate patients and caregivers about signs and symptoms of AD and prevention
- Provide training on positioning techniques, skincare, and techniques to manage bowel and bladder function
- Functional Independence:
- Enhance independence in ADLs and toileting
Our role in preventing autonomic dysreflexia (AD) as occupational therapists involves providing education and training to individuals with spinal cord injuries. We aim to enhance their independence in managing both bowel and bladder care. This includes educating them about the signs and symptoms of AD, scheduling regular care routines, and teaching proper techniques to minimize the risk of triggering AD.
Neurogenetic Bladder Complications: Urinary Tract Infections
- Commonly occurring in individuals with SCI
- Presentation of symptoms may differ in a patient with SCI
- Patients with SCI may identify unusual symptoms that predict a UTI reliably
- Early intervention can prevent life-threatening infections
- SCI patients with frequent UTIs had an increased risk of renal complications and mortality
(Perez et al., 2022)
Urinary tract infections (UTIs) are a common concern among individuals with spinal cord injuries, particularly those with neurogenic bladder dysfunction. What makes this population unique is that the presentation of UTI symptoms can differ from the general population. These distinctive symptoms may include unusual signs such as confusion or cognitive changes. Interestingly, these unusual symptoms consistently occur when a patient with a spinal cord injury has a UTI, making them reliable indicators of the infection.
As healthcare professionals, it's paramount to attentively listen to our patients and trust their reports of symptoms. Recognizing these atypical symptoms and promptly communicating them to physicians is crucial to ensure timely and appropriate treatment. This proactive approach is vital in preventing life-threatening infections and complications. Furthermore, it's essential to be aware that the more frequently a patient experiences UTIs, the higher the risk of renal complications and mortality becomes, underscoring the importance of effective prevention and management strategies.
OT Role in UTI Prevention
- Ensures patients are knowledgeable about and able to perform proper hygiene practices in all settings
- Establish regular voiding schedules
- Ensure proper catheter care
- Teaching to monitor fluid intake
- Recognize signs of UTIs
- Ensure the environment for cathing is organized, accessible, and clean
Our role in promoting bowel health is crucial, and it involves several key aspects. First and foremost, we play a pivotal role in educating patients on clean and effective bowel care techniques. Establishing reliable voiding schedules, monitoring fluid intake, and recognizing the early signs of UTIs are all part of our responsibilities. By empowering individuals with spinal cord injuries to proactively manage their bladder, we can significantly reduce the occurrence of UTIs and their associated complications.
Now, let's transition to discussing bowel function. As occupational therapists, we often find ourselves at the forefront of assisting individuals with spinal cord injuries in achieving bowel health and independence in managing bowel movements.
Normal Innervation and Physiology of the Bowel
Neurological Innervation of the Bowel
- Gut to the splenic flexure of the colon: Vagus nerve
- Colon & rectum: sympathetic T9-L3
- Upper GI tract: T9–T12
- Descending colon and rectal: T12–L3
- Vascular innervation small/large bowel: T7–T8
- External anal sphincter muscle: S3-S5
- Distal colon & rectum: parasympathetic S2-S4
- Internal anal sphincter- S2–S4
- Pelvic floor musculature- S2–S4
(Johns et al., 2021; Rodriguez & Gater, 2022)
Understanding the neurological innervation of the gastrointestinal (GI) system is crucial when working with individuals who have spinal cord injuries. The vagus nerve provides neurological intervention from the gut to the splenic flexure. The colon and rectum receive sympathetic innervation from T9 to L3, with the upper GI tract corresponding to T9 to T12 and the descending colon and rectum to T12 to L3. Vascular innervation for the small and large bowel comes from T7 to T8, while the external anal sphincter muscle is innervated at the S3 to S5 level. The distal colon and rectum, including the internal anal sphincter and pelvic floor muscles, receive parasympathetic innervation from S2 to S4. The rectoanal inhibitory reflex also involves parasympathetic innervation from S2 to S4. It's important to note that both the bowel and bladder are not fully innervated until the S4 level, which is higher than the typical level of spinal cord injuries. This knowledge is essential when working with spinal cord injury patients to address bowel function effectively.
Normal Defecation
- Movement of stool from colon to rectum via peristalsis
- Defecation reflex: the stretch of the rectal wall- triggering contraction of the rectal wall via reflex arch between the rectum and sacral spinal cord
- Rectoanal inhibitory reflex (RAIR): relaxation of internal anal sphincter muscle during rectal expansion: S2-S4 parasympathetic nerve fibers
- Voluntary contraction of the external anal sphincter muscle can stop defecation
(Johns et al., 2021)
Normal defecation begins when the stool is moved from the colon to the rectum, and this stretches the rectal wall and initiates the defecation reflex. The anatomical structures can be seen in Figure 7.
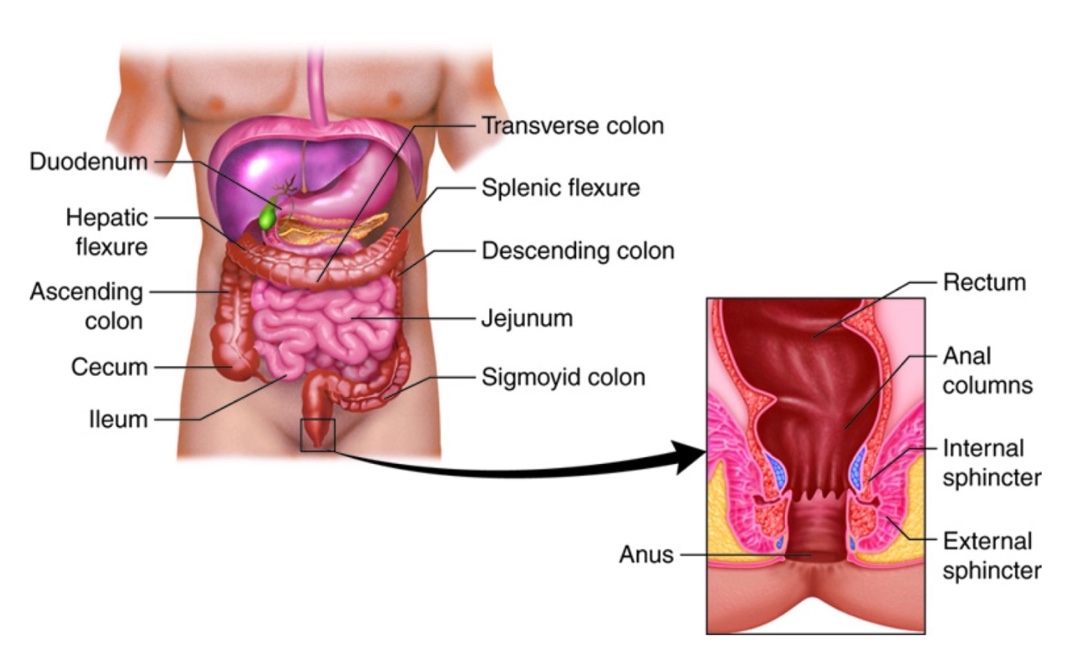
Figure 7. The anatomical structures for bowel function (Anatomical structures of the large intestine. This work by Cenveo is licensed under a Creative Commons Attribution 3.0 United States (https://creativecommons.org/licenses/by/3.0/us/).
The contraction of the rectal wall is stimulated through a reflex arc between the rectum and the sacral spinal cord. This reflex, known as the rectoanal inhibitory reflex, causes relaxation of the internal anal sphincter muscle during rectal distension, facilitating the process of defecation. This reflex is enhanced by the parasympathetic nerve fibers from S2 to S4. Importantly, we have voluntary control over the external anal sphincter muscle, allowing us to interrupt the process of defecation when necessary. This voluntary control is especially useful during inconvenient moments, like long trips, when you need to delay the urge to defecate.
Normal Continence
- Depends on complex interactions between:
- Consistency of stool
- Colon to rectal transition time
- Rectal tone
- Anorectal sensation
- Muscle tone of puborectalis and anal sphincter
- External anal sphincter muscle voluntary contraction
(Johns et al., 2021)
Normal continence relies on a delicate interplay of various factors, including stool consistency, colorectal transition time, rectal tone, anorectal sensation, muscle tone, and voluntary contraction of the external anal sphincter muscle. These elements must work harmoniously to maintain bowel control and prevent incontinence.
Neurogenic Bowel Dysfunction
- Symptoms include:
- Loss of voluntary control over bowel movements
- Decreased awareness of stool incontinence
- Difficulty with evacuation of stool
- Constipation
- Upper GI symptoms:
- Abdominal pain/discomfort
- Bloating
- Epigastric burning
(Rodriguez & Gater, 2022)
Neurogenic bowel dysfunction is a common consequence of spinal cord injury, characterized by a range of symptoms. These individuals often experience loss of control over bowel movements, leading to incontinence, and reduced awareness of this incontinence. Additionally, they may struggle with evacuating stool, resulting in constipation. These issues can give rise to upper gastrointestinal symptoms like abdominal pain, discomfort, bloating, and epigastric burning. Over time, these problems tend to worsen, leading to a decline in overall health and an increased risk of hospitalizations, especially as more time passes since the injury. Individuals with neurogenic bowel dysfunction often contend with heightened anxiety, depression, and fear of accidents, which can limit their participation in various activities, particularly those outside the home, due to the fear of incontinence.
Neurogenic Bowel Dysfunction and SCI
- GI issues may worsen with time
- May contribute to a decline in overall health and wellness
- May increase hospital admissions
- May contribute to an increase in anxiety, depression, and fear of incontinence
- Negative influence on occupational performance and participation
(Rodriguez & Gater, 2022)
Individuals with spinal cord injuries often experience reduced motility in the colon, as well as weakness in the pelvic floor and rectal sphincters. This combination of factors leads to impaired defecation and reduced awareness of incontinence, primarily due to decreased or absent sensation in the anal and perianal areas. Depending on the level and completeness of the spinal cord injury, individuals typically have either a spastic (reflexic) bowel or a flaccid (areflexic) bowel.
The reflexic bowel is associated with injuries above the sacral level (S2). In this case, the external anal sphincter muscle and the contractibility of the rectum are spastic.
- Decreased motility of GI (esp. colon), weakness in pelvic floor, rectal sphincters
- Impaired sensation in anal and perineal area
- Spastic bowel (reflexic) vs. flaccid bowel (areflexic)
(Rodriguez & Gater, 2022)
This individual will also have slow motility within the GI tract, a decreased urge to defecate, and a reflexive defecation. This leads to incontinence and unpredictable bowel movements.
Neurogenic Bowel Classification
- Supraconal lesions above S2: spastic external anal sphincter muscle and spasticity and contractility of the rectum (reflexic)
- Decreased motility of GI
- Decreased urge to defecate
- Causes reflex defecation
(Rodriguez & Gater, 2022)
Reflexic bowel occurs in the majority of those with neurogenic bowel, again, because the majority of individuals we work with have lesions above S2.
- Conal/intraconal lesions at or below S2: flaccidity of external anal sphincter muscle, decreased tone, and contractility of the rectum (areflexic)
- Decreased motility of GI
- Uncontrolled incontinence
(Rodriguez & Gater, 2022)
The areflexic bowel occurs when there's a conal or intraconal lesion, typically at or below the S2 level. In cases of areflexic bowel, both the rectum and the external sphincters are flaccid, meaning they have no muscle tone. This leads to decreased motility in the gastrointestinal tract and uncontrolled incontinence, as all the relevant muscles lack tone and control.
Management of Neurogenic Bowel
- Establish a bowel care program for assisted defecation
- Diet and fluid management
- Physical activity
- Oral and rectal bowel medications
- Techniques and devices for rectal emptying
- Education
- Supplies and equipment
- Scheduled bowel care
- Caregiver training
(Johns et al., 2021; Rodriguez & Gater, 2022)
The establishment of a bowel care program for individuals with spinal cord injury involves various healthcare professionals, including physicians, nurses, dieticians, and occupational therapy practitioners. These programs encompass multiple components.
For diet and fluid management, we can address the individual's dietary choices and fluid intake to regulate bowel movements effectively. Appropriate physical activities that can help stimulate bowel function and mobility should be encouraged. Oral or rectal medications can be used as needed to manage bowel function. Various techniques and devices that can assist in the emptying of the bowels. We can educate on bowel management strategies and techniques and provide the necessary supplies and equipment for effective bowel care. It is important for them to establish a regular and consistent schedule for bowel care procedures. Caregivers should be trained to assist individuals with spinal cord injuries in managing their bowel care. Lastly, collaboration among healthcare professionals, including occupational therapists, helps individuals with spinal cord injuries maintain proper bowel function and improve their overall quality of life.
Establishment of Bowel Program
- Initiate immediately in acute rehabilitation or before, if possible (even in spinal shock):
- Encouraged bowel habituation
- Prevent constipation and impaction
- The bowel program should be consistent, at the same time, and complete to:
- Help control bowel evacuation
- Allows predictability
- Helps reduce incontinence
(Rodriguez & Gater, 2022)
Establishing a bowel program promptly after a spinal cord injury, even during spinal shock, is crucial. Beginning the program on acute rehabilitation or as soon as possible helps the bowel adapt and reduces the risk of constipation and impaction. Involving the patient in determining the daily time for bowel care is essential to establish predictability and reduce incontinence.
Initially, as the bowel is being trained, there may be instances of incontinence, especially during strenuous activities like transfers. These activities can trigger reflexive bowel movements, a common experience known to those who have worked with spinal cord patients.
Goals for Bowel Management
- Regular BMs at a regular time daily
- Daily or every other day (at least 3x per week)
- Once daily independently (physically or instructionally)
- Completed in 30-60 minutes
- Sufficient stool amount per BM
- Daily:~1.5–2 cups
- Every other day:∼3–4 cups
- No episodes of incontinence
- Preventing hard stool and maintaining soft, formed stools
(Rodriguez & Gater, 2022)
Bowel management goals include establishing regular bowel movements (BMs) at the same time of day, ideally every day or at least every other day, with a minimum of three times a week. Achieving one daily independent BM is the ultimate goal. Bowel programs should be completed in a time frame of 30 to 60 minutes. There should be sufficient stool output, with approximately 1.5 to 2 cups for daily BMs or three to four cups for BMs occurring every other day. The aim is to prevent episodes of incontinence and maintain soft, formed stools for easier bowel movements.
OTP Role in Bowel Program
- OT collaborates with patients, physicians, and nurses, considering the factors that contribute to a successful BM program, including:
- Personal habits and routines
- Lifestyle factors influencing occupational participation
- Personal resources
- Educational levels and understanding
- Help to reinforce compliance, consistency, and regular routine schedule
- Monitor and adjust routine as needed
Occupational therapists play a crucial role in helping individuals establish a bowel program after a spinal cord injury. OTs work collaboratively with patients to discuss their personal habits and routines for bowel management, taking into account any habits they had prior to their injury. Lifestyle factors that influence bowel care, such as daily schedules, are considered in developing the program. OTs assess the patient's personal resources and education level to provide education that matches their understanding. OTs help reinforce compliance with the bowel care program, maintain consistency, and assist patients in developing a regular routine and schedule. Monitoring and adjusting the routine as needed is also part of the OT's role in bowel management.
- Ensuring compliance with the team's nutrition and hydration recommendations
- Total dietary fiber from food 25–30g
- Proper fluid intake 2.5–3.0 L water to prevent constipation
- Plan and prepare meals to promote health
- Meals with a diet to maintain soft, formed, bulky stools
- Establish and participate in diet routines to promote health
- Avoid caffeinated beverages: result in dehydration and hard stools
- Avoid gassy foods
(Rodriguez & Gater, 2022)
Occupational therapy practitioners play a vital role in ensuring that individuals with spinal cord injuries adhere to nutrition and hydration recommendations. OTs may be involved in feeding and eating activities with patients, allowing them to observe any signs of poor appetite, inadequate oral intake, significant weight changes, or fatigue. Monitoring and addressing these issues are essential.
In terms of nutrition, it's important to ensure that patients receive an appropriate amount of fiber (around 20 to 30 grams of total fiber) and drink an adequate amount of water (2.5 to 3 liters per day). Balancing fluid intake is crucial to promote optimal stool consistency and avoid constipation while also considering bladder management. OTs can work with patients to plan meals that support healthy bowel function, as food and fluid choices can influence stool consistency and transit times in the neurogenic bowel. Patients should be educated about avoiding or limiting foods that can lead to gas, bloating, or changes in bowel movements, as these can increase discomfort.
- Participation in physical activity
- Encouragement of regular physical activity to improve wellness and encourage bowel movements
- Develop habits and routines that encourage physical activity
- Standing programs may be beneficial for bowel function
(Rodriguez & Gater, 2022)
Occupational therapists (OTPs) can assist patients in developing habits and routines that incorporate physical activity, which can have a positive impact on overall wellness and mood, as well as promote regular bowel movements. Additionally, standing programs may be recommended to improve bowel health. These interventions can help individuals with spinal cord injuries maintain better bowel function and overall well-being.
Management of Reflexive Bowel
- BMs can be initiated by stimulating defecatory reflex activity with:
- Digital stimulation
- Rectal stimulant medication
- Enemas
(Rodriguez & Gater, 2022)
Individuals with reflexic bowels may require methods to initiate bowel movements, such as digital stimulation or the use of rectal stimulant medications, including Dulcolax, glycerin, and enemas. These interventions help trigger the defecatory reflex and facilitate bowel movements.
OTP Role in Reflexive Bowel
- ADLs: Toileting and Toilet Hygiene
- Retrieving and utilizing necessary supplies
- Managing clothing prior to and after
- Transferring to and maintaining position for toileting
- Cleaning self following
- Suppository management
- Maintenance of bowel movements
- Using equipment for bowel care or clothing management
(AOTA, 2020)
Occupational therapy practitioners (OTPs) play a crucial role in assisting patients with toileting and toilet hygiene. This includes helping patients with supply retrieval, clothing management, transferring to and maintaining positions for toileting, cleaning themselves properly, managing suppositories, maintaining bowel movements, and using equipment correctly for both bowel care and clothing management.
- Education and Training:
- Reinforce and train digital stimulation: a gloved and lubricated finger is inserted into the rectum with rotation to relax the internal anal sphincter to evacuate the bowel
- Educate on adequate bowel movement
- Instruct in equipment: patients with limited hand function, C6-C8 or patients with limited reach
- Monitor and modify routine as needed
OTPs play a significant role in educating and training individuals with reflexic bowels on how to perform digital rectal stimulation. This technique involves introducing a lubricated gloved finger into the rectum and performing gentle circular strokes at 20-second intervals, repeated every five to 10 minutes until the rectum is clear of stool. OTs may need to assist patients in problem-solving where and how this procedure can be performed, considering factors like the patient's positioning and hand function. Additionally, for patients with limited hand function or reach, OTs can train them to use adaptive equipment such as cuff digital stimulators or suppository inserters and provide ongoing monitoring and modifications to the routine as needed.
Management of Areflexic Bowel
- Pelvic floor and sphincter flaccidity and decreased or absent reflexes
- Managed by manual removal of stool or flushing enemas performed once or twice daily
- High risk of incontinence
- Caution should be used with oral bowel stimulants and/or osmotic medications since incontinence can be increased with watery stools
(Rodriguez & Gater, 2022)
In the case of an areflexic bowel, where the bowel muscles lack tone and responsiveness, stool removal must be carried out manually or with the use of flushing enemas once or twice daily. Because the muscles are flaccid, there is a high risk of incontinence in this population. It's important to exercise caution when considering oral bowel medications for these individuals, as they may lead to the production of watery stools.
OTP Role in Areflexic Bowel
- Education and Training:
- Reinforce the use of manual removal of stool or the use of enemas for patients and caregivers
- Instruct in equipment: patients with limited hand function, C6-C8 patients with limited reach
- Educate on adequate bowel movement
- Monitor and modify the program as needed
In situations where individuals have limited hand function, they may rely on verbal instructions and guidance to participate in and manage their bowel management program. Occupational therapy practitioners can play a crucial role in training and assisting caregivers in carrying out these programs effectively. This involves educating caregivers on proper techniques for stool removal and enema usage, emphasizing the importance of maintaining the appropriate size of bowel movements, and monitoring and adjusting the program as needed.
Adaptive Equipment for Bowel Care
- Adaptive bowel care equipment
- Cuffed suppository inserter vs. uncuffed
- Cuffed digital stimulator vs. uncuffed
- Mirror with or w/o leg spreader
- Adapted scissors to open packaging
- Finger condoms for digital stimulation
- Pumped lubricant
This is not an all-inclusive list of adaptive equipment for bowel care. These are the most popular ones, shown in Figure 8.

Figure 8. Adaptive equipment for bowel care.
Patients with limited hand function or reach can benefit from various adaptive equipment and devices to assist with bowel management. Occupational therapy practitioners can guide them in selecting and using these tools effectively. Some examples of adaptive equipment include cuffed or uncuffed suppository inserters, cuffed or uncuffed digital stimulators, mirrors with or without leg spreaders, adaptive scissors for opening packages, finger condoms (used carefully to prevent them from being pulled into the rectum), and pump lubricants to facilitate the process.
Mechanical Interventions
Here are a few surgical interventions.
Transanal Irrigation
- Used for both reflexic and areflexic bowel
- Pulsed irrigation is provided by a rectal balloon catheter and pumps to clean out the rectum up to the sigmoid.
- Effective in managing hard stools and impactions
- Helps to reduce constipation, decrease incontinence, improve bowel function, decrease total time for bowel care, improve GI symptoms, and quality of life
- OTPs can reinforce training.
(Rodriguez & Gater, 2022)
Transanal irrigation is a mechanical intervention used for bowel management. It involves a pulsed irrigation method using a rectal balloon catheter that is inserted into the rectum. Water is then pumped into the rectum, flushing out stool from the rectum to the sigmoid colon. This method is particularly helpful in managing hard stools, impaction, and constipation, ultimately reducing incontinence. It can improve overall bowel function, decrease the time required for bowel care, alleviate GI symptoms, and enhance the individual's quality of life.
Occupational therapy practitioners can receive training in the use of this device and provide education and training to patients and caregivers on its proper usage. This helps individuals with spinal cord injuries effectively manage their bowel function.
Pelvic Floor Therapy
- For those with incomplete SCI who have partially intact sensory and motor function
- To activate anorectal and pelvic floor muscles, visual, sensory, and mechanical techniques are used
- Combined with biofeedback and Kegals
- The goal is to retrain muscles to coordinate defecation
- OTP can complete specialized training to provide pelvic floor training for SCI
(Rodriguez & Gater, 2022)
Pelvic floor therapy is a therapeutic approach that can benefit individuals with incomplete spinal cord injuries, particularly those who have partially intact sensory and motor function. This therapy aims to activate the anorectal and pelvic floor muscles through a combination of visual, sensory, and mechanical techniques. Biofeedback and Kegel exercises may also be incorporated into the therapy program. The ultimate goal of pelvic floor therapy is to improve the coordination of these muscles to facilitate more controlled and effective defecation.
Occupational therapy practitioners can receive specialized training to provide pelvic floor therapy for patients with spinal cord injuries. By offering this form of therapy, they can play a valuable role in helping individuals regain better bowel control and improve their overall quality of life.
Surgical Interventions for Bowel Management
- Colostomy
- Malone Antegrade Continence Enema (ACE)
- Macedo–Malone or left-sided ACE (LACE)
- Recommended after conservative bowel programs failed, frequent bowel impactions/obstructions, or non-healing pressure injuries
(Rodriguez & Gater, 2022)
Colonoscopy
- Improves consistent and regular bowel emptying
- Reduces time spent on bowel program
- Decreases abdominal pain, bloating, and incontinence
- GI complications and hospital readmission reduced
- Independence and quality of life improved
- Improves participation in occupations outside the home and travel
(Rodriguez & Gater, 2022)
A colostomy is a surgical procedure familiar to many. It involves creating an abdominal wall opening (stoma) through which a portion of the colon is brought to the surface. This surgical intervention can be utilized to address various issues related to bowel management in individuals with spinal cord injuries.
The benefits of a colostomy can include improved consistency in bowel emptying, reduced time and effort spent on bowel care routines, decreased symptoms like abdominal pain, bloating, and incontinence, reduced gastrointestinal complications and risk of hospital readmissions, increased independence in managing bowel function, and improved participation in various activities outside of the home environment.
It's worth noting that some individuals who have undergone colostomies report that they wish they had done so earlier, emphasizing the potential benefits of considering this surgical option sooner for those who struggle with maintaining bowel health and programs.
- OTP Role in Colostomy Care
- Education, Counseling, and Training:
- Provide education about the procedure
- Care and management of the ostomy and skin hygiene
- Signs/symptoms of complications
- Address concerns with coping with body image issues, self-esteem, and sexuality
- Guidance on selecting and using specialized clothing, ostomy pouches, and accessories to ensure comfort and ease of use
- Education, Counseling, and Training:
Again, we can help with education and care of the colostomy.
Malone Antegrade Continence Enema (MACE)
- A catheterizable appendicocecostomy stoma: for access with a catheter to use for routine antegrade enema cleansing of the colon
- Flushes entire colon
- Performed 2–3 times a week
- Large amounts of water to flush
- 1–2 h to complete
(Rodriguez & Gater, 2022)
The MACE procedure is a surgical procedure that helps create a stoma in the belly button through which an enema can be administered to flush out the colon and promote regular bowel movements. This procedure with the MACE flushes the entire colon, and it can be performed two or three times a week. It uses large amounts of water, and it takes about one to two hours to complete.
Macedo–Malone or Left-sided ACE (LACE)
- A catheterizable tube is created from a segment of the descending colon that is joined to the left lower wall of the abdomen
- Flushes only distal descending colon
- Performed daily or every other day
- Use 200–600 mL of tap water
- BM in 10–20 min
(Rodriguez & Gater, 2022)
The LACE procedure only flushes out the descending colon. It's performed daily, uses smaller amounts of water, and can be completed in 10 to 20 minutes.
Bowel and Bladder Function and Other Occupations
Let's briefly touch on the intersection of bowel and bladder function with other daily occupations.
Health Care Management
- OTP support of medication management:
- Speaking to the physician regarding prescriptions
- Filling prescriptions
- Interpreting instructions for medication
- Taking medications routinely and as instructed
- Timely refilling prescriptions
- Understanding the importance of medications for bowel and bladder management
(AOTA, 2020)
Occupational therapists indeed have a multifaceted role in healthcare, encompassing various aspects of medication management and ensuring that clients receive the necessary support and education related to their prescriptions for bowel and bladder care. This comprehensive approach can significantly improve overall health outcomes and quality of life for individuals with specific medical needs.
Functional Mobility
- OTP training in functional mobility to safely perform elimination:
- Bed mobility
- Bathroom transfers
- Selection of proper bathroom equipment
- Selection of the safest transfer device
- Community transfers
- Head on toilet transfer
- Transportation of objects required
Occupational therapists' expertise in functional mobility and equipment selection is invaluable in helping patients with spinal cord injuries or other conditions achieve greater independence and safety in their daily activities, including bowel and bladder management. By providing education, training, and guidance on proper techniques and equipment, occupational therapists can enhance their clients' ability to perform these tasks effectively and with confidence.
Sexual Function
- OTP can develop education on sexual intimacy regarding bowel and bladder care for patients and sexual partners with specific sexual desires and goals
- Education should include:
- Pre-and post-intercourse perineal and bladder care
- Risk of infection
- Techniques to optimize the experience,
- Timing of sexual activity to reduce the chance of incontinence
- Effects on the intimate relationship if the partner performs care
- Resources on emotional support
(Fritz, Dillaway,& Lysack, 2015)
Occupational therapists play a crucial role in addressing the sexual health and intimacy needs of individuals with spinal cord injuries or other conditions that affect bowel and bladder function. By providing education, guidance, and support, occupational therapists can help clients and their partners navigate the challenges and concerns related to sexual function while managing their specific care requirements. This holistic approach can significantly enhance the quality of life and overall well-being of individuals with these conditions.
OTP Role in Performance and Participation in Occupation
- IADLs
- Rest and Sleep
- Education
- Work
- Play
- Leisure
- Social Participation
It's important to recognize how bowel and bladder management can impact all aspects of a person's life and daily activities. Occupational therapists are skilled at assessing and addressing these impacts to help individuals with spinal cord injuries achieve their goals and maintain their independence.
Now, let's discuss the case mentioned earlier.
Case OT Interventions
- Education and Training:
- Educate on the function of bowel and bladder, including the effects of spinal cord injury on these systems.
- Teach strategies to promote regular BMs, i.e. diet, hydration, and physical activity.
- Train on techniques for self-catheterization, including hygiene practices and potential complications
- Provide information on AE that can support bowel and bladder management, such as bowel stimulators and intermittent catheterization kits
Providing education on the anatomy and function of the bowel and bladder, as well as how spinal cord injury can impact these systems, can empower the patient with knowledge and help them better manage their condition.
- Bowel Management Routine:
- Collaborate to establish a consistent bowel management routine based on his preferences and daily schedule
- Develop a schedule for regular bowel movements and implement strategies such as digital stimulation or manual evacuation to facilitate bowel emptying
- Monitor and adjust the routine as needed to optimize bowel management and prevent constipation or accidents
We want to come up with a comprehensive plan to address his bowel and bladder management needs. Providing strategies for regular bowel movements, teaching proper hygiene practices, and discussing potential complications are all essential components of helping him maintain his bowel and bladder health.
- Facilitate peer support groups or connect John with individuals who have successfully managed similar challenges, providing a sense of community and encouragement.
- Discuss any issues regarding sexual intimacy and bowel and bladder care
We can address his psychosocial needs through peer support groups, connecting him with professionals for emotional support, and discussing sexual intimacy related to bowel and bladder care are crucial aspects of his holistic care. It's evident that you've considered all aspects of his well-being and have a comprehensive plan to support him in his journey to manage his spinal cord injury effectively.
Summary
Thanks for your time and attention. I will now take questions.
Questions And Answers
Are there any adaptive equipment options available for individuals with spinal cord injuries to assist with wiping after bowel movements?
There are some adaptive devices on the market designed to assist with wiping for individuals with limited mobility or spinal cord injuries. These devices can help extend the arm's reach and make the wiping process more manageable. Additionally, bidets are another option to consider, and there are various bidet models available, but the choice should be patient-specific. Some individuals prefer bidets, while others may find it more convenient to perform bowel care in the shower after a program that can take up to 60 minutes.
What is the highest level of spinal cord injury at which a patient can typically complete a bowel program independently?
The ability to complete a bowel program independently varies from one individual to another and depends on various factors. In general, patients with higher-level spinal cord injuries, such as C6, may be able to complete a bowel program independently if they possess specific attributes like strength, athleticism, and minimal fear or anxiety related to the process. However, it's important to note that independence in bowel care is patient-centered and highly dependent on individual capabilities. Additionally, individuals with hand function have a better chance of achieving independence. In some cases, adaptive equipment like digital stimulators can greatly enhance independence, even for those with high-level injuries, such as tetraplegia at C7.
References
Abu Mostafa, M., Plastow, N. A., & Savin-Baden, M. (2020). The effectiveness of spinal cord injury ADL inpatient education on rehabilitation outcomes: A systematic review and meta-analysis. British Journal of Occupational Therapy, 83(1), 15-28.
American Occupational Therapy Association. (2020). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy, 74(Supplement 2). 7412410010. https://doi.org/10.5014/ajot.2020.74S2001
Fritz, H. A., Dillaway, H., & Lysack, C. L. (2015). “Don’t think paralysis takes away your womanhood”: sexual intimacy after spinal cord injury. The American Journal of Occupational Therapy, 69(2), 6902260030p1-6902260030p10.
Johns, J., Krogh, K., Rodriguez, G. M., Eng, J., Haller, E., Heinen, M., ... & Korsten, M. (2021). Management of neurogenic bowel dysfunction in adults after spinal cord injury: Clinical practice guideline for health care providers. The Journal of Spinal Cord Medicine, 44(3), 442-510.
Perez, N. E., Godbole, N. P., Amin, K., Syan, R., & Gater Jr, D. R. (2022). Neurogenic bladder physiology, pathogenesis, and management after spinal cord injury. Journal of Personalized Medicine, 12(6), 968.
Rodriguez, G. M., & Gater, D. R. (2022). Neurogenic bowel and management after spinal cord injury: A narrative review. Journal of Personalized Medicine, 12(7), 1141.
Citation
Monti, Y.(2023). Occupational therapy’s role in bowel and bladder management for individuals with spinal cord injury. OccupationalTherapy.com, Article 5639. Available at www.occupationaltherapy.com
