Editor's note: This text-based course is a transcript of the webinar, An Overview Of Sleep Disturbances: A Practical Approach For Occupational Therapy Practitioners, presented by Cynthia Hoskins, DBH, MOT, OTR/L, CCTS-I.
Learning Outcomes
- After this course, participants will be able to identify at least 3 common types of sleep disturbances.
- After this course, participants will be able to compare and contrast the objective and subjective signs and symptoms of sleep disturbances and their impact on areas of occupation.
- After this course, participants will be able to apply the use of evidenced-based strategies to improve patient functional outcomes.
Introduction
Hello, and thank you for the warm introduction. I'm delighted to have each of you here today as we delve into the critical topic of sleep disturbances. I value your engagement, and towards the end, there will be an opportunity for questions and discussion. Additionally, my contact details will be shared, encouraging you to reach out for further queries or insights.
As practitioners, our overarching goal is to enhance patient functional outcomes and, in this case, sleep quality. While sleep is considered an area of occupation, we'll unravel its pervasive influence on every facet of our lives. Armed with these tools, we can navigate the complexities of sleep disturbances, ensuring a comprehensive and effective approach in our practice. I look forward to this collective exploration and knowledge sharing.
Defining the Terms
- Sleep disturbances/disorders- a set of conditions that present with interruptions in normal healthy sleep patterns (Karna et al., 2023). These disturbances involve poor or lack of quality and quantity of sleep.
- Circadian Rhythm-Cycles aligned with the internal/biological clock (Suni & Singh, 2023), “the physiological 24-hour time pattern of human life” (Czeisler & Buxton, 2017; Turek & Zee, 2017 as cited in Brown et al., 2019 p. 909).
- Zeitgeber – Nature's rhythmic occurrence that cues humans to engage in physiological processes such as eating, sleeping (e.g. light)
- Sleep – A biological process
- NREM- Non-rapid eye movement (The first 3 stages of sleep)
- REM-Rapid eye movement (Stage 4)
Let's start our exploration by defining the foundational concept of sleep disturbance. It encompasses a range of conditions that disrupt the natural sleep process, affecting both the quantity and quality of sleep. Such disturbances can arise from various factors, impacting an individual's established sleep patterns.
Circadian rhythm is often referred to as our biological clock. In the hustle and bustle of life, our 24-hour internal clock, which guides our sleep-wake cycle, can be thrown off balance. Disruptions to this rhythm can lead to challenges in maintaining healthy sleep patterns. An important term to note here is "Zeitgeber." Zeitgebers are natural cues in our environment that signal specific physiological processes, such as eating, sleeping, and socializing. Light, especially sunlight, stands out as a powerful Zeitgeber, influencing our wakefulness and sleepiness. Additionally, we can create our own cues, or Zeitgebers, through consistent activities like exercise or regular meal times, shaping our body's internal clock.
Now, let's shift our focus to the essence of sleep itself. Sleep is a vital biological process crucial for our daily functioning. Distinguishing between sleep and rest is essential, as the terms are often used interchangeably. Rest involves a pause in activity while staying awake and aware, whereas sleep represents a different level of consciousness and awareness, where the body operates on a distinct wavelength. Although our discussion today centers on sleep, it's paramount for clinicians to acknowledge and address the importance of rest in their assessments and interventions. Balancing adequate sleep with mindful rest becomes integral to promoting overall well-being.
To understand the stages of sleep, we encounter the terms NREM (non-rapid eye movement) and REM (rapid eye movement). NREM comprises the initial three stages of sleep, leading to the deeper, more restorative REM stage, commonly considered the fourth stage. While there might be variations in defining the stages, the general progression involves transitioning through these phases during a typical sleep cycle.
Overall Prevalence
- Approx. 70 million Americans in a given year struggle with some type of sleep disturbance
- 30 percent short-term insomnia
- 10-15 percent chronic insomnia
- 100,000 MVA can be attributed to sleep deprivation/leading preventable cause
- Approx ⅓ of drivers do not get the proper amount of sleep
- Approx. 34% of children, 33% adults, and 75% of high school students do not receive consistent quality/quantity of sleep (Ramar et al., 2021)
- The overall cost of health care is 10x higher for those with poor quality sleep (van Straten et al., 2018)
- So common that the CDC considers it a public health concern (Smallfield & Lucas, 2018)
- Women > Men
Let's now explore the prevalence of sleep disturbances, shedding light on the staggering numbers that highlight the urgency of addressing this issue. In a given year, over 70 million Americans grapple with some form of sleep disturbance, underscoring the magnitude of this challenge within the population. As clinicians, it becomes imperative for us to integrate discussions and interventions related to sleep into our therapy sessions.
Breaking down the figures, approximately 30% of individuals experience short-term insomnia, while 10 to 15% contend with chronic insomnia. Acute insomnia, lasting less than three days a week for less than three months, contrasts with chronic insomnia, persisting for more than three months and often occurring at least three days a week. These statistics emphasize the diverse and prevalent nature of sleep difficulties, urging us to tailor our therapeutic approaches accordingly.
Shifting our focus to an unexpected consequence, over 100,000 motor vehicle accidents annually result from sleep deprivation, challenging the conventional association with accidents and substance use. Alarmingly, a third of drivers fail to obtain adequate sleep, putting themselves and others at risk on the roads. Many can relate to instances of compromised awareness and response due to insufficient sleep, emphasizing the societal impact of this issue.
Concerningly, sleep deprivation extends its reach to children, adults, and high school students. A substantial 34% of children, 33% of adults, and a staggering 75% of high school students face inadequate sleep, affecting various aspects of their lives, including education and overall well-being. The repercussions of poor sleep quality contribute significantly to the burden on the healthcare system, with those experiencing poor sleep being ten times more likely to incur higher healthcare costs. Recognizing this, the Centers for Disease Control and Prevention (CDC) categorizes sleep deprivation as a public health challenge, highlighting the need for comprehensive solutions.
Gender disparities in sleep patterns emerge, with women tending to struggle more with sleep deprivation than men. Factors such as hormonal fluctuations and the demands of daily life contribute to these differences. As we navigate through the following slides, we'll delve deeper into these intricacies, acknowledging the multifaceted nature of sleep challenges and the necessity for targeted interventions.
Sleep Cycle/Stages Overview
- 4 Stages of Sleep/Average 4-6 Cycles
- Stage 1-3 Considered NREM/Stage 4 REM
- The average person cycles through all stages 4-6 times per night/Each cycle lasting approximately 90 minutes
- Stage 3(Deep Sleep)-Critical stage (body heals, tissue repair, builds immune system)
- Stage 4 (REM)- Crucial as well (Important for learning and cognitive skills; dreams occur; waves as if awake; emotional regulation)
The sleep cycle is a dynamic process with four distinct stages. On average, individuals cycle through these stages four to six times each night, with each cycle lasting approximately 90 minutes. This cumulative cycling typically results in a total sleep duration of six to nine hours per night, varying among individuals.
The initial stages (1 through 3) are classified as non-rapid eye movement (NREM), marking the transition from wakefulness to a more relaxed state. During this period, vital signs such as blood pressure, heart rate, and respiration gradually decrease. Stage 3, known as deep sleep, is particularly crucial for the body's healing processes, encompassing tissue repair and immune system bolstering.
Moving into stage 4, the landscape shifts to rapid eye movement (REM) sleep. Despite brainwaves resembling wakefulness, the body is in a state of profound rest. This paradoxical stage is where dreams unfold, and essential cognitive and emotional development occurs. Emotional regulation and learning are fostered during REM sleep, underscoring its significance for overall well-being.
Disturbances in these stages, whether due to interruptions or insufficient duration, can have notable consequences. Consider moments when you've been abruptly awakened from deep sleep, leaving you groggy and disoriented. This highlights the importance of completing each stage in the sleep cycle for comprehensive physical and cognitive benefits. As individuals traverse through these stages repeatedly throughout the night, the impact on overall health and functionality becomes evident, emphasizing the need for a thorough understanding of sleep dynamics in clinical practice.
Common Types of Sleep Disturbances
- Insomnia Disorders- most common; difficulty falling asleep, staying asleep, poor quality/quantity sleep
- Parasomnias- unwanted behaviors occurring during sleep (e.g., sleepwalking, teeth grinding, etc.)
- Sleep-Related Breathing Disorders- breathing is disrupted during sleep (e.g., sleep apnea)
- Hypersomnolence- presents with difficulty staying awake/excessive sleepiness during daytime hours (Hyperactivity, narcolepsy, etc.)
- Circadian Rhythm Sleep-Wake Disorders- “ My clock is off.” A sleep cycle is out of sync with the norm (e.g., shift work, etc.)
- Sleep-Related Sleep Disorders- involuntary body movement while sleeping (e.g., restless leg)
It's crucial to recognize the prevalence and impact of sleep disorders Over 70 million Americans grapple with various forms of sleep disturbances annually, marking a significant portion of the population facing challenges in achieving restful sleep. These disturbances encompass a spectrum, ranging from short-term insomnia affecting 30% of individuals to chronic insomnia, impacting 10 to 15% over a more prolonged period.
The repercussions extend beyond individual experiences, spilling into unexpected territories like motor vehicle accidents. Surprisingly, over 100,000 accidents occur yearly due to sleep deprivation, emphasizing the societal consequences of inadequate rest. This extends to children, adults, and high school students, where a substantial percentage face sleep deficits, influencing areas such as education and overall well-being.
Considering the cumulative effects, the Centers for Disease Control and Prevention (CDC) rightly categorizes sleep deprivation as a public health challenge. The burden on the healthcare system amplifies, with those experiencing poor sleep quality being ten times more likely to incur elevated healthcare costs.
Unpacking the intricacies of sleep, we touch upon the stages, emphasizing the importance of progressing through the four stages of non-rapid eye movement (NREM) and rapid eye movement (REM) sleep for holistic well-being. The dynamic nature of these cycles, occurring four to six times per night, illustrates the intricate dance of the body's restoration and cognitive processes.
Turning our attention to common sleep disturbances, insomnia takes the spotlight as the most prevalent disorder. Its manifestations include difficulties in falling asleep and staying asleep and variations in sleep quantity and quality. Parasomnias introduce unwanted behaviors during sleep, ranging from sleepwalking to teeth grinding, disrupting the natural sleep cycle.
Sleep-related breathing disorders, such as sleep apnea, present breathing disruptions during rest, potentially posing serious health risks if unaddressed. Hypersomnolence and hypersomnia differentiate between difficulty staying awake during waking hours and persistent excessive sleepiness throughout the day, respectively.
Circadian rhythm or sleep-wake disorders throw the internal sleep cycle out of sync, often influenced by factors like shift work or jet lag. Finally, movement-related sleep disorders, exemplified by restless leg syndrome, introduce involuntary movements during sleep, impacting both sleep quality and quantity.
As we navigate this multifaceted landscape of sleep disturbances, understanding their prevalence and diverse manifestations is pivotal for clinicians seeking to address these challenges effectively in their practice.
Causes for Disruptions in the Circadian Rhythm/Sleep-Wake Cycle
- Life Stages and transitions (e.g., aging)
- Shift work
- Chronic/Acute pain
- Chronic/Acute illness or injuries
- Dietary habits
- Low vision-(not as aware of cues)
- Jet lag
- New environment- hospital stays
- Medications
- Hormones
- Neurological disorders
- Mental health challenges (anxiety, depression, stress, etc.)
There are a myriad of causes that can disrupt the delicate balance of circadian rhythm and the sleep-wake cycle. Life stages and transitions, such as becoming a new parent, bring unique challenges, especially when infants exhibit irregular sleep patterns, testing parental sleep continuity. Aging is another factor, with research indicating that advancing age may introduce difficulties in maintaining a consistent sleep pattern.
Life roles, particularly that of a caregiver, introduce a distinctive layer of disruption to the sleep-wake cycle. Caregivers, responsible for individuals requiring around-the-clock attention, find their sleep quality and quantity compromised due to the vigilance demanded by their caregiving responsibilities.
Shift work, a reality for many, particularly those on night shifts, introduces a significant upheaval to the natural sleep-wake cycle. The conventional cues provided by natural light and darkness become distorted, impacting the body's internal clock.
Chronic and acute pain pose substantial challenges to a restful night's sleep. Whether from injuries, medical conditions, or illnesses like the flu or cold, the discomfort can disturb sleep patterns, making it challenging to find a comfortable position or simply attain rest.
Dietary habits play a vital role in sleep disruption. Consuming heavy meals before bedtime or experiencing sensitivity to caffeine can throw the circadian rhythm off balance. Caffeine's presence in the system for two to eight hours after consumption highlights its potential impact on sleep, varying from person to person.
Low or no vision affects the reception of environmental cues essential for maintaining a regular sleep-wake cycle. Without visual indicators, individuals may struggle to synchronize their internal clock with external cues, impacting their sleep patterns.
Jet lag, a common phenomenon for travelers crossing multiple time zones, disrupts the accustomed sleep cycle. The adjustment period may vary based on age and individual adaptability.
Medications, whether for blood pressure, steroids, or other conditions, can introduce sleep disturbances as a side effect. Hormonal changes, particularly during menopause or hormone supplementation, have a profound impact on sleep-wake cycles.
Neurological disorders, encompassing conditions like brain injuries, strokes, Alzheimer's, and Parkinson's, present challenges not only due to the disorders themselves but also due to associated symptoms like restless leg syndrome.
Lastly, mental health challenges, such as anxiety, depression, and chronic stress, create an environment where the constant production of cortisol hinders the ability to achieve both quality and quantity of sleep. Understanding these diverse causes is crucial as we approach assessments and interventions in our journey to address sleep disturbances effectively.
Areas of Occupation
I use an umbrella for this particular slide (Figure 1) because these are areas of occupation that we engage in on a daily basis.
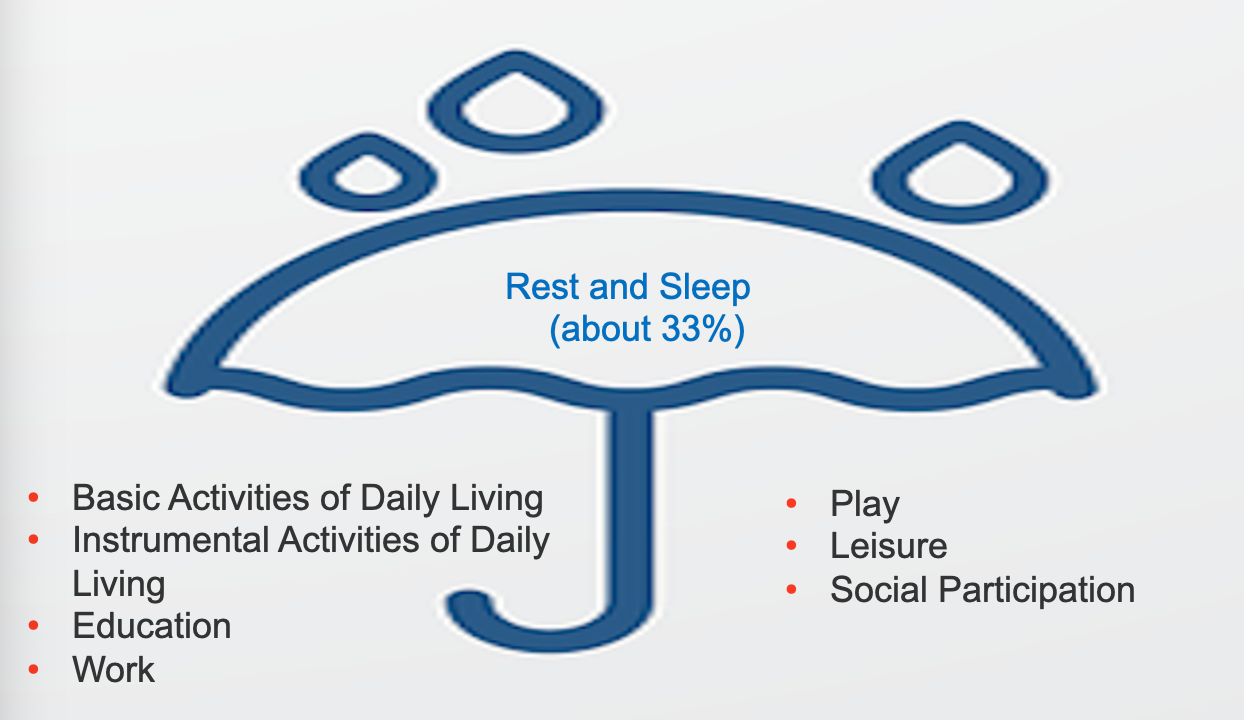
Figure 1. Areas of occupation.
Consider for a moment those aspects that define you, and that contribute to your identity—the work you engage in, your pursuit of education, the balance of leisure activities, and the richness of your social interactions. These elements, together with fundamental activities of daily living, such as dressing, bathing, grooming, and hygiene, form the fabric of your existence. Simultaneously, instrumental activities of daily living, like managing household chores and organizing, contribute to shaping your daily routine. All of these, in occupational therapy terms, fall under the umbrella of areas of occupation.
However, among these, rest and sleep emerge as a linchpin, influencing and intersecting with every other facet of your daily life. The reason for emphasizing rest and sleep in this context is rooted in the profound impact they wield across various areas of occupation. If you find yourself unable to obtain adequate sleep, even seemingly simple tasks like washing your face and brushing your teeth can become arduous. This is especially pertinent for high school students, where a staggering 75% face challenges in attaining quality sleep—a deficit that permeates their ability to think, concentrate, plan, and organize.
Consider the implications on work—a realm where optimal performance is essential. Quality sleep is not merely a luxury but a prerequisite for peak productivity. The risk of accidents, akin to the example of narcolepsy, underscores the potential dangers of compromised sleep, not only affecting work but also posing risks during daily commutes or social engagements. Sleep, occupying approximately 33% of our daily existence, is not merely a physiological necessity but a cornerstone influencing overall well-being.
Even in the realm of play, for both children and adults, the impact of sleep cannot be overlooked. It serves as a foundation for relaxation, unwinding the mind, and rejuvenating the body. As we navigate assessments and interventions in occupational therapy, acknowledging and addressing the critical role of sleep becomes paramount. Improving patient functional outcomes requires a comprehensive understanding of how sleep intricately weaves into the fabric of our daily lives across various areas of occupation.
Impact of Inadequate and Poor-Quality Sleep
- Prone to infections
- Mood instability
- Increased risk of substance use
- Weight gain/loss
- Increased risk for cardiovascular disease
- Increased risk of injuries
- Increased risk of suicide/homicide
- Depression/anxiety
- Impaired judgement
- Decreased attention, memory, attention to detail
- Delayed reaction time
- Low/No energy
- Decreased overall function/Quality of life
When adequate sleep eludes us, the repercussions extend far beyond mere fatigue. First and foremost, our immune system weakens, rendering us more susceptible to infections such as COVID-19, the flu, and the common cold. This vulnerability is particularly pronounced for individuals grappling with autoimmune disorders, compounding the risk of infections.
Beyond the physiological realm, inadequate sleep casts a shadow over our mood and emotional stability. Irritability, agitation, and altered responses to stimuli become more prevalent when the body is deprived of necessary rest. This can create a ripple effect, influencing our interactions and relationships.
Substance and alcohol use often become intertwined with sleep struggles. Some may turn to these substances to induce sleep, while others resort to them to combat drowsiness arising from inadequate rest. It's a delicate balance, illustrating how sleep deprivation can fuel a cycle of reliance on substances.
The impact on body weight is a common query, and the connection is twofold. Sleep deprivation can lead to unhealthy snacking habits, often involving less nutritious choices. This, in turn, contributes to weight gain. On the flip side, disrupted sleep patterns can also result in weight loss due to altered metabolic processes.
The toll on physical health extends to increased risks of cardiovascular disease, diabetes, and heart problems. Additionally, the likelihood of injuries escalates, spanning from falls to accidents involving machinery. The consequences become even graver when considering the augmented risk of suicide and homicide linked to impaired mood stability.
Mental health bears a heavy burden, with sleep deprivation acting as a catalyst for depression and anxiety. Impaired judgment, decreased attention, and compromised memory function further exacerbate the challenges, impacting everyday activities like driving, operating machinery, or even cooking.
In essence, sleep deprivation permeates every facet of our lives, leaving us with diminished energy levels and an overall decline in functioning. The intricate interplay of these factors necessitates a nuanced approach when employing screening tools to assess sleep disturbances, each tool offering unique insights into an individual's sleep patterns. While not delving into exhaustive detail on each tool, it is crucial to recognize their collective utility in guiding interventions that aim to alleviate the pervasive impact of inadequate sleep.
Screenings/Assessments for Sleep Disorders
(The first step for the OTP)
Informal (Subjective Approach)
- Interview- Should be a part of every assessment; Part of Occupational Profile
- Do you consider it to be an issue?
- Do you snore/Share a bed?
- Family/Work life
- Amount of sleep
- Diet/Substance/Alcohol use
- Prescription medications
- Sleep Diary- more specifics on routine and daily occurrences
Formal (Objective Approach)
- Screenings/Formal Assessment tools-more structured self-reports/outcome measures
- Insomnia Severity Index (ISI)
- Pittsburgh Sleep Quality Index (PSQI)
- Oviedo Sleep Questionnaire (OSQ)
- Patient Health Questionnaire (PHQ)
- Occupational Profile of Sleep –more formal assessment tool
- Technological devices
- BEARS screening tool for children
Understanding the importance of assessment is foundational in addressing sleep-related issues. The assessment phase serves as a compass, guiding the clinician to understand the patient's sleep patterns, identify potential challenges, and determine the impact on daily functioning. Recognizing the scope of practice is paramount; clinicians should acknowledge their capacity to address sleep-related mental health issues.
The initial step involves creating an occupational profile, an informal assessment that delves into the patient's routines, sleep patterns, and daily life. This can uncover whether the patient perceives sleep as an issue and provides essential contextual information. Collateral data from chart reviews or interviews with caregivers is valuable, especially when working with individuals who may struggle to articulate their sleep experiences, such as young children.
The sleep diary is beneficial, serving as an assessment and intervention tool. It captures details like daily schedules, dietary habits, and medication use. This tool complements the occupational profile, offering a comprehensive understanding of the patient's life.
The Occupational Therapy Sleep Profile enriches the assessment process by exploring various aspects of sleep, such as breathing difficulties and sleep-wake cycles. It aids in identifying disruptions that may impact sleep quality and quantity.
Several standardized tools, like the Insomnia Severity Index (ISI), Pittsburgh Sleep Quality Index, Oviedo Sleep Questionnaire, and Patient Health Questionnaire (PHQ-9), come into play during the formal evaluation. These tools provide baseline scores, aiding in categorizing the severity of sleep-related issues. The Oviedo Sleep Questionnaire stands out for its comprehensive approach, allowing patients to articulate their challenges in their own words.
Objective assessments, including sleep studies and technological devices like Fitbits, contribute valuable data. Fitbits, for instance, monitor sleep patterns and disruptions, offering insights into the duration and quality of sleep.
For children, the BEARS tool proves beneficial, offering a screening tool for parents to provide information on bedtime routines, excessive sleepiness, awakenings during the night, respiratory issues, and snoring.
The holistic assessment, combining subjective and objective measures, facilitates a nuanced understanding of the patient's sleep experience. This comprehensive approach aids in tailoring interventions that address the specific challenges identified during assessment. Pre and post-assessments with tools like ISI can gauge the effectiveness of interventions, providing a dynamic feedback loop for the therapeutic process.
In essence, assessment lays the foundation for an informed and targeted approach, allowing clinicians to devise interventions that promote improved sleep and, consequently, enhanced overall functioning in various areas of occupation.
Evidenced-Based Strategies/Interventions
Sleep Hygiene Training/Education
- Address the behaviors/habits that may lead to sleep challenges
- Avoiding exercise before bed
- Avoiding caffeine/sugar
- Set a bedtime routine
- Use the bed only for sleeping/intimacy
- Stretch, meditate, relax before bed
Another crucial aspect in addressing sleep disturbances is incorporating sleep hygiene training and education. Educating individuals about habits that may interfere with sleep is vital. For instance, avoiding exercise before bedtime is recommended, as it can elevate heart rate and hinder sleep. The timing of activities, such as taking a hot shower or bath, is also crucial, with the optimal time being 30 minutes to an hour before bedtime.
Limiting sugar and caffeine intake, particularly before bedtime, can significantly improve sleep. Establishing a consistent bedtime routine is another effective strategy, helping signal the body that it's time to wind down. This routine might involve activities like reading, stretching, or engaging in gentle meditation to promote relaxation.
Encouraging individuals to use their bed exclusively for sleep and intimacy reinforces the association between the bed and rest. Discouraging activities like working or watching TV in bed contribute to improved sleep hygiene. Similarly, avoiding screen time at least an hour before bedtime helps mitigate the disruptive effects of the blue light emitted by screens on melatonin production.
Incorporating stretching, meditation, and relaxation techniques into the evening routine can further promote a calm and conducive mindset for sleep. It's essential to emphasize that individual responses to these strategies may vary, and tailoring recommendations based on a person's unique lifestyle and preferences is key. Ongoing education and support enhance the effectiveness of these strategies in fostering better sleep habits.
Addressing the Client Environment
- Address the environmental factors that may lead to sleep challenges
- Mattress/pillow comfort
- Lighting
- Temperature
- Organization
Examining the client's environment is a crucial aspect of intervention. Simple elements like the mattress play a significant role; an aged mattress over eight years might contribute to sleep difficulties. Assessing the mattress's firmness and comfort, as well as the appropriateness of the pillow, is essential. Personal preferences vary, making it important to tailor recommendations based on individual comfort.
Lighting is another environmental factor that warrants attention. Natural cues for sleep involve the body's production of melatonin, and exposure to excessive light, especially blue light from devices, can disrupt this process. Evaluating the bedroom's lighting conditions, including considerations for window coverings, helps create an environment conducive to sleep.
Room temperature is a critical factor that can impact sleep quality. The room being too hot or too cold can disturb sleep patterns. Addressing temperature preferences and ensuring the room is comfortably regulated aids in creating an optimal sleep environment.
Additionally, the organization of the bedroom contributes to the overall sleep quality. A cluttered or disorganized room may create a sense of chaos and hinder relaxation. Encouraging clients to maintain an organized and serene bedroom atmosphere can positively influence their ability to unwind and sleep peacefully. Each of these environmental factors plays a role in shaping the conditions necessary for restful sleep, making them integral components of intervention strategies.
Sensory Approach
- Engage the sensory system to help improve sleep quality
- Weighted blanket
- Lighting
- Calming sounds
- Relaxation strategies like deep breathing, visualization, guided meditation
- Progressive muscle relaxation
- Calming smells (approach with care)
- Stress-relieving/relaxing tea
Addressing sleep deficits through a sensory approach involves engaging the sensory system. Exploring options like a weighted blanket, experimenting with calming lighting, and incorporating soothing sounds can be beneficial. Tailoring these sensory interventions to each individual is crucial, recognizing that what works for one person may not work for another. Additionally, when using calming smells, caution is advised due to the powerful impact scents can have, evoking either positive or distressing memories. Techniques such as progressive muscle relaxation, deep breathing, visualization, guided imagery, and meditation can relieve stress. Encouraging activities that promote relaxation, like using relaxing teas, can be effective components of the intervention process to address sleep deprivation.
Cognitive-Behavioral Approach (CBT-I)
- The focus is on identifying and addressing the negative and dysfunctional thoughts surrounding sleep
- Multi-component approach
- The premise is distorted thoughts leading to feelings leading to actions/behaviors
- Involves exploring the reality of thoughts and education on new behaviors that lead to quality sleep (sleep restriction, relaxation, etc.)
- Effective for the treatment of insomnia sleep disorder
Cognitive Behavioral Therapy for Insomnia (CBTI) stands out as a highly successful treatment approach, particularly for insomnia. This multi-component strategy incorporates sleep hygiene education and addresses distorted thoughts surrounding sleep. Challenging negative thoughts, such as unrealistic expectations about sleep duration, helps clients recognize and change counterproductive beliefs.
CBTI also includes sleep restriction, dispelling the myth that missed sleep can be made up. Establishing a consistent sleep routine is emphasized to promote healthy sleep patterns. This approach is particularly effective in addressing insomnia, although elements of it can be adapted for other sleep disorders, always considering potential underlying medical conditions that should be addressed by a primary care physician.
When working with clients, creating a grid to challenge negative thoughts and examining the realistic aspects of those thoughts can be helpful. It encourages individuals to identify unproductive thoughts and beliefs about sleep, fostering a shift in their perspective.
Additionally, it's crucial to know what is considered normal sleep duration for different age groups. This knowledge aids in assessing whether an individual's sleep patterns align with typical expectations for their age. Understanding the range of recommended sleep hours can guide the selection of screening tools and treatment interventions based on individual needs.
Key Take-Aways
- OT practitioners have an integral role in successful functional outcomes related to this area of occupation
- A key component in the assessment/screening process
- Research the underlying cause
- Incorporating sleep education critical in any setting
Occupational therapists are critical in enhancing functional outcomes across various life domains, including sleep. Quality sleep is foundational for overall well-being, affecting daily performance in essential activities. Exploring underlying causes of sleep difficulties is imperative, as clients may not readily disclose contributing factors such as psychiatric disorders or substance use. Integrating sleep education consistently into assessments and interventions is vital, fostering awareness about healthy sleep habits. Recognizing sleep challenges as a prevalent public health issue emphasizes the urgency for occupational therapists to address this concern actively. A comprehensive approach that considers sleep in the broader context of occupational therapy can significantly contribute to improved client outcomes.
Summary
In revisiting the learning objectives, we aimed to cover a comprehensive understanding of various sleep disturbances, enabling you to identify and differentiate between them. We delved into the signs and symptoms associated with sleep disturbances, exploring their impact on the body and various areas of occupation. The discussion spanned informal and formal assessment tools, ranging from subjective, rapport-building conversations to efficient screening tools like ISI and PHQ-9, with the occupational profile for sleep providing a more detailed evaluation.
Furthermore, we emphasized the importance of evidence-based strategies to enhance patient outcomes. This involved integrating sleep education into interventions, acquiring knowledge of Cognitive Behavioral Therapy for Insomnia (CBTI), recognizing the significance of the patient's environment, and understanding the role of the sensory system in promoting restful sleep. The broader consideration of incorporating rest into a client's routine was highlighted, acknowledging its distinct role in preparing the body for quality sleep. By addressing these objectives, occupational therapists can effectively improve their clients' sleep and overall well-being.
We will now look at some of the exam questions via polling.
1) What stage of sleep is considered "deep sleep," critical for body healing, repairing tissue, and building the immune system?
2) What is the most common sleep disorder?
Insomnia is correct. These are other sleep disorders, but insomnia is the most common, either acute or chronic insomnia.
3) What is the impact of inadequate and poor quality of sleep?
Mood instability
Decreased attention, memory, and attention to detail
Low or no energy
All of the above
Poor sleep quality includes all these areas, so D is the correct answer.
4) Which of the following is not part of the sleep hygiene training?
voiding exercise before bed
Avoiding caffeine and sugar
Watching TV in bed
Stretching/meditation
The correct answer is watching TV in bed. You will discuss this during your education, but it is not part of sleep hygiene training, as it is more environmental. You want to make sure blue lights are kept to a minimum. Blue light items include TVs, cell phones, and computers. Research has shown that it is very disruptive to sleep. You also do not want to watch the news or something that's high impact or intense before you go to bed as your mind will be racing.
5) Which therapeutic intervention involves a multi-component approach, which includes challenging negative thoughts surrounding sleep?
Sensory approach
Sleep hygiene training
CBT-I
Sleep restriction
CBT-I is a multi-component approach. This is where you're incorporating education, but you're also spending time finding out what are some of those distorted and negative thoughts surrounding sleep. This creates an opportunity to challenge and address those thoughts to improve sleep patterns.
You guys were paying attention.
All right, great job. Let's move into questions.
Questions and Answers
How does watching TV or having the TV on at night affect sleep?
Blue lights emitted by electronic devices, including TVs, disrupt sleep patterns. Additionally, exposure to light signals the body to decrease melatonin production, making it more challenging to fall asleep. The content being watched can also stimulate the brain, making it harder to wind down.
If sleep quantity is reduced to 5-6 hours but a person still feels refreshed, is that a problem?
It depends on the individual. While the average adult should get 7-9 hours of sleep, variations exist. It may not be an issue if the person feels refreshed and functions well. However, consistently getting fewer hours could pose challenges over time.
If total sleep is 7 hours with a 2-hour gap in between, is this a problem?
Yes, having interruptions in sleep, such as waking up in the middle of the night, can be problematic. It affects the quantity and quality of sleep, potentially leaving the person less refreshed upon waking.
Why does the recommended sleep duration decrease for those aged 65 and above?
As people age, their sleep needs may change due to medication, lifestyle changes, or underlying health conditions. While the general recommendation is 7-9 hours for adults, variations can occur based on individual circumstances.
Can sleep deprivation lead to mood disorders other than depression and anxiety?
Chronic sleep deprivation can contribute to various mood disorders, including major depressive disorder and bipolar disorder.
Does listening to autonomous sensory meridian response (ASMR) before bed contribute to relaxation for better sleep?
Listening to soothing sounds or ASMR can be helpful for relaxation, but choosing sounds that genuinely relax the individual is essential, as preferences vary.
How do toileting needs affect sleep cycles?
Frequent urination, often caused by factors like medication or age-related issues, can disrupt sleep cycles and impact the overall quality of sleep.
Can energy conservation education be linked with rest training?
Energy conservation education can complement rest training by focusing on managing and conserving energy throughout the day to support better sleep.
If someone takes sleep medication and gets only 5 hours, is that considered quality or quantity sleep?
Quality sleep is subjective, but taking sleep medication late may affect the intended sleep duration. Consultation with a primary care physician to adjust medication timing is advisable.
Feel free to reach out for any additional questions or clarifications!
References
https://www.mybib.com/b/V1LOQ9
Citation
Hoskins, C. (2024). An overview of sleep disturbances: A practical approach for occupational therapy practitioners. OccupationalTherapy.com, Article 5685. Available at www.occupationaltherapy.com
