Editor's note: This text-based course is a transcript of the webinar, Complex Regional Pain Syndrome: Functional, Biomechanical, And Psychosocial Interventions, presented by Janice Rocker, OTD, OTR/L, CHT, CEAS.
Learning Outcomes
- After this course, participants will be able to:
- recognize two self-reported functional outcome measures, Rand SF and Upper Limb Functional Index, which address physical and psychological concerns.
- compare and contrast biomechanical, psycho-social, and realistic functional OT goals and treatment strategies with this population.
- identify recent research on CRPS.
Hello everyone! Let's get started.
CRPS Definition
- “Chronic
- “Pain out of proportion to the severity of the initial injury
- “…cause isn't clearly understood
- “Treatment is most effective when started early. In such cases, improvement and even remission are possible.”
Mayo Clinic (n.d.)
The definition of complex regional pain syndrome, or CRPS, by the Mayo Clinic and multiple sources, is chronic pain out of proportion to the severity of the initial injury. We do not clearly understand why treatment is most effective when started early, but it is great that Mayo Clinic has recognized that. We can improve our clients and whatever the goals they are working on, and remission is possible. It is important to tell our clients because they sometimes think this diagnosis is a death sentence. I have been in CRPS chat rooms, and everybody is miserable. We want to turn that around and tell them it is possible to get better.
CRPS Classification
- “CRPS type I: A specific nerve lesion has not been identified (90%)
- “CRPS type II: There is an identifiable nerve lesion”
- CRPS NOS (not otherwise specified)
(Smart et al., 2016; Zangrandi et al., 2021)
For CRPS classification, type one is 90% of the population where a specific nerve lesion has not been identified. Type two is an identifiable nerve lesion; type three is not otherwise specified.
Occurrence
- “3-4x more frequent in women
- “CRPS evolves into a chronic condition in 15-20% of cases”
(Zangrandi et al., 2021)
There is some confusion about the occurrence of CRPS. It is more frequent in women, but I have seen it in men. It evolves into a chronic condition in 15 to 20% of the cases. Again, they can get better.
Cause
- “…Caused by an injury to or difference in the peripheral and central nervous systems”
- “Autonomic and sensorimotor disturbances due to underlying plastic changes in the central nervous system”
- Why? Don’t know
(Mayo Clinic, n.d.; Zangrandi et al., 2021)
We do not know the cause. Is it by an injury to or a difference in the peripheral and central nervous systems or both? Is it automatic? Is it sensory-motor disturbances due to underlying plastic changes in the central nervous system? We will talk about those plastic changes but do not know the cause.
Self-Reported Functional Outcome Measures
- Rand SF 36
- Short form survey with 36 items (5 typed pages)
- Computerized scoring
- Separate scores for: Physical functioning, role limitations caused by physical health problems, role limitations caused by emotional problems, energy/fatigue, emotional well-being, social functioning, body pain, general health perceptions
- “Most widely used measure of health-related quality of life today.”
(Hays, & Morales, 2001)
- Upper Limb Functional Index
- 25 items (2 typed pages)
- Easy math to score
- Overall one score
- Easier for client to complete
- Easier for clinician to score
- “The ULFI is suggested as the preferred upper limb regional tool due to its superior practical characteristics and clinical utility, and comparable psychometric properties without a tendency toward item redundancy.“
(Gabel et al., 2006)
I suspect most people know or use The Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire. The DASH provides some good information.
I first saw the Upper Limb Functional Index published in the Journal of Hand Therapy. I liked it because it was only two pages as opposed to five pages, which is the DASH. The other bonus is that the math is easy to score (one overall score), and you do not need a computer.
We also started using also the Rand SF 36 because we were involved in some research. There are five typed pages with 36 questions, and it uses computerized scoring. It does take some time to input the scores. The great thing about the Rand is that you get separate scores from zero to 100. A 100% means you are fine, and zero means you have a lot of problems. This scoring is the opposite of DASH. The scores break down into physical functioning, role limitations caused by physical health problems, role limitations caused by emotional problems, energy or fatigue, emotional wellbeing, social functioning, body pain, and general health perceptions. It is nice to have these separate categories for goal creation. We can also use the scores from 0-100 for insurance purposes.
These functional outcome measurements are usually required by insurance, and it is a nice way to show people they have made progress. The thing about these types of self-reported functional outcome measures is our clients can think about how they are doing versus us rating how we think they are doing. They are based on disability, and so we want to give clients things they can do in the clinic that shows that there is hope. This is why graded activities become so important in the clinic.
Budapest Criteria for CRPS
- Pain and at least one symptom in 3 of these categories:
- Sensory: hyperalgesia and/or allodynia
- Vasomotor: temperature asymmetry and/or skin color changes and/or skin color asymmetry
- Sudomotor/Edema: edema and/or sweating changes and/or sweating asymmetry
- Motor/Trophic: decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
- Must display at least one sign at time of evaluation in two or more of the following categories:
- Sensory: hyperalgesia (to pinprick) and/or allodynia (to light touch and/or deep somatic pressure and/or joint movement)
- Vasomotor: temperature asymmetry and/or skin color changes and/or asymmetry
- Sudomotor/Edema: edema and/or sweating changes and/or sweating asymmetry
- Motor/Trophic: decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
- There is no other diagnosis that better explains the signs and symptoms
https://www.blbchronicpain.co.uk/news/what-are-the-crps-budapest-criteria/
The Budapest criteria are the best way to classify someone as having CRPS and the gold standard. There are things that we can observe in the clinic and other changes that are detected with blood tests and things like that. We will get into that a little bit later.
If you are seeing symptoms and are unsure where to classify them, this is a nice reference to use.
Case Studies
- Nurse with R dominant humeral fx
- Linguist with R dominant DR fx
- Highlights:
- Treat pain based on neuroscience strategies
- Aim to normalize cortical representation to decrease pain and improve function
Throughout this presentation, I am going to present two case studies and talk about treatments based on neuroscience principles and some top-down approaches. Overall, we want to normalize cortical representation to decrease pain and improve function.
Case Study 1: Nurse with R Dominant Proximal Humeral Fracture
- Age: 47
- FOOSH at night, ambulating from bed to toilet
- Wore a sling x4 wks, then referred to OT
- Concerned about RTW, aging, and being a burden to her 2 grown children
Treatment Includes:
- Specific-client reported functional goals
- Psycho-social
- Paraffin
- Mirror tx
- Manual tx, ther ex
My first one is a nurse with a right dominant proximal humeral fracture. I saw her four weeks after her injury; she had worn a sling for that whole time. Her shoulder was not moving well, but she was mostly concerned about the pain in her wrist and her fingers, which were very swollen. It was obvious to me that she had CRPS. She did not have any broken bones or ligament injuries distally.
Her main concern was she had to pass her CPR exam and was worried about doing the chest compressions. She was divorced with two adult children but did not want to be a burden. There were psychosocial types of things that we needed to address in her treatment.
We gave her a couple of balance exercises that she could do, and she did well with them. For people who are severe, I refer them out for balanced training. Shoulder motion came easily to her, but wrist and finger were difficult.
Research-Evidence is Mixed: Cochrane Database
- Evidence is mixed “about the effects of physiotherapy interventions on pain and disability in CRPS.
- “Large-scale, high-quality RCTs with longer-term follow-up are required to test the effectiveness of physiotherapy-based interventions for treating pain/disability in adults w CRPS I and II.”
(Smart et al., 2022)
What is the research showing? The Cochrane database has mixed evidence about whether therapy can help, and we need more large-scale, high-quality RCTs with longer follow-ups. Most follow-up is short, so we want to know if people can get better over time.
Research-Evidence is Mixed: Systematic Review, Meta-analysis, RCT
- "…results suggest that graded motor imagery and mirror therapy alone may be effective, although this conclusion is based on limited evidence
- “Further rigorous studies are needed to investigate the effects of GMI and its components on a wider chronic pain population.”
- Top-down vs. bottom-up tx approach
- GMI helps
(Bowering et al., 2013; Dilek et al., 2018)
There are systematic reviews and meta-analyses that suggest graded motor imagery and mirror therapy alone may be effective. This conclusion is based on limited evidence, so we need more rigorous studies.
The top-down versus bottom-up treatment approach seems to help, but we are not exactly sure, and GMI, graded motor imagery, can also help.
Everything is mixed, and it is hard to do research on this population.
Mechanism Specific Management
- Tx may be peripheral or central or both
- What does this unique client need?
- If an intervention does not work, change the intervention
- (Packham et al., 2018)
- “The most dangerous brain is one that does not understand what is going on”
(Gift, 2018)
Mechanism specific management is what we need to focus on. One person with CRPS may need a peripheral approach, a central approach, or both. We have to look at everybody as a unique client, and we do that naturally. We see if something works; if it does not, we try something else.
"The most dangerous brain is one that does not understand what is going on." Hannah Gift published in ASHT Times about CRPS, saying that often, we do not know where they are getting their information. They may be going on some crazy internet sites. We can say, "The Mayo Clinic says we can turn this around, and you can get better with this."
With the nurse, I used some paraffin. This is not her hand but an example.

Figure 1. Examples of uses of paraffin.
She cannot make a fist, as her wrist hurts. I showed her how to put her hand in the paraffin. I also had her make a ball of paraffin and rub that around her forearm. She was in charge, and if she had a painful area, she stayed away from it. We do not want to cause more pain. We always say, "Don't be a pain terrorist." They go at a pace that is comfortable for them.
I also have them make a gentle C when going into the paraffin. I then ask them to try to make a small ball. As their fingers warm up, you can ask them to go further. You do not want to crank on the person; it is all very gentle.
CNS Vs. PNS
A whole trauma cascade is involved with CRPS, as shown in Figure 2.
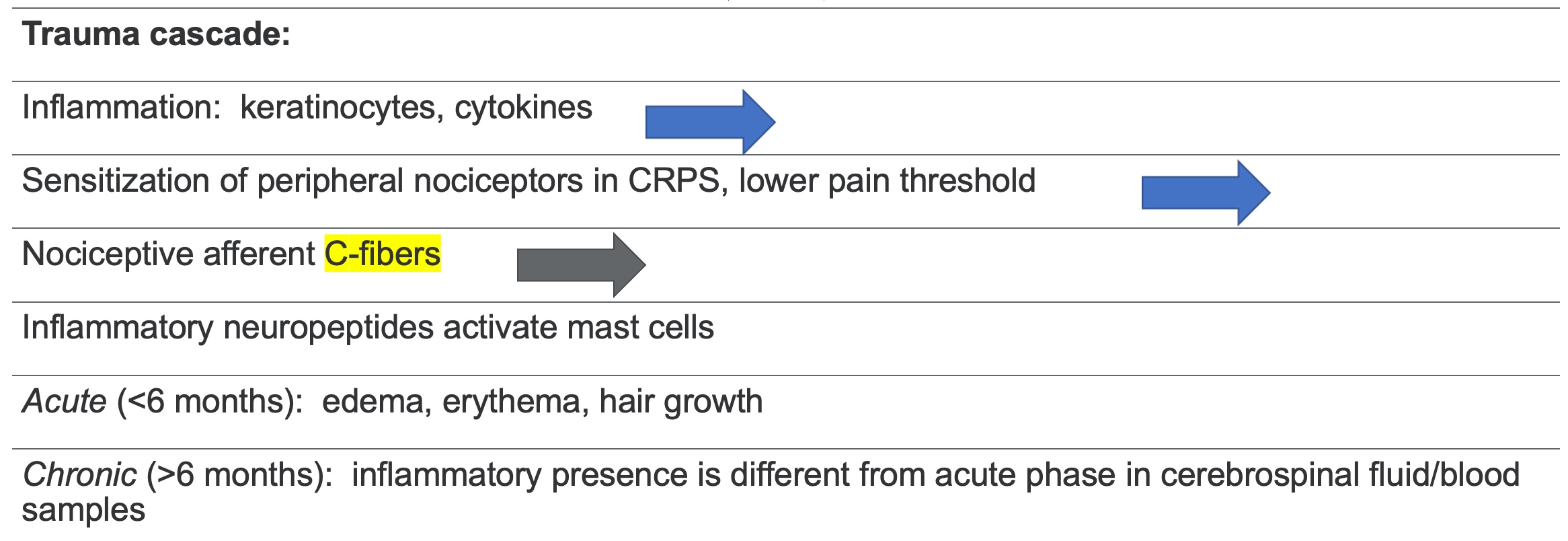
Figure 2. Example of the trauma cascade.
C-fibers transmit the awful pain that people with CRPS talk about, and some others. We can control C-fibers with TENS, so we will get into that a little bit later in the talk. The inflammatory presence is different from the acute phase in the cerebrospinal fluid and in a blood sample. We need to get our doctors to test for this.
Treatment
- Graded exposure to help overcome central reorganization
- Gain positive association with activity, self-efficacy
- Consider psychotherapeutic tx
- Beliefs, cognition, emotions, pain-related behaviors
- Pain is subjective and can be modulated (PNS v CNS)
- (Birklein et al., 2015; Hamasaki et al., 2018)
- Education: Brain’s role in pain
- Brain changes, plasticity
- (Gift, 2018)
I had her visualize doing CPR first. She said, "I like seeing that I can do it." Sometimes people are anxious, and it can cause pain just visualizing a task. It was good to see that she could successfully do this. Next, we practiced CPR with no resistance. She stated that moving her wrist or spreading her fingers was hard. I then had her try to spread her fingers and put them in a prayer position. The strong arm tells the brain how the weaker arm should work. Gradually, we worked on doing compressions on a pillow at the height she would need to do it and then moved to a rubber ball with some air out of it. She felt good about that. Normally your dominant arm is on top for CPR, but she switched that.
For infant CPR, she was concerned about how she was going to hold the baby and do little compressions with the two fingers. I made a "baby" with a ball and a weight in a pillowcase. She did not feel comfortable doing it with her dominant hand, so we switched arms. The compressions have to be fast for CPR, but we started slowly. When she fatigued, she would lie on the mat, and we would do some myofascial release exercises.
I said to her, "Your arm will be sore, so you may want to take an anti-inflammatory before." Ice was not something she liked, but she liked the heat. We worked on this, and Figure 3 shows the results.

Figure 3. Nurse holding her CPR certification.
The person on the right is our OTD resident at the time.
Graded exposure helped her overcome central reorganization and gain a positive association with activity and self-efficacy.
We also want to consider psychotherapeutic treatment, like a person's beliefs, cognition, emotions, and pain-related behaviors. Pain is subjective and can be modulated, and the brain can change, as it is plastic. Sometimes people with medical backgrounds are harder to treat, but she understood that and had an intrinsic motivation to get better. She had to support herself because she did not want to rely on her children.
Somatosensory Rehab and Graded Motor Imagery Combined (1/4)
- Case study of 39 yo CRPS and severe touch-evoked pain (static mechanical allodynia)
- Tailored rehab program combining somatosensory rehab, GMI, and more conventional approaches improves functional status
(Quintal et al., 2018)
This article about a single case study can help us understand this technique. They had a person who went through conventional therapy at another clinic and still had severe touch-evoked pain. The therapists tailored treatment for this client, and they talked about the approach that they used.
Somatosensory Rehab and Graded Motor Imagery Combined (2/4)
- SRM:
- Uses comfortable peripheral somatosensory stim that can potentially act on peripheral sensitization mechanisms
- Does not require active mvmt
- Avoids/reduces any cutaneous stim where touch evokes pain (allodynic area)
- Stimulates somatosensory system at a distant site in a comfortable area proximal to an allodynic area
(Quintal et al., 2018)
Somatosensory rehab is comfortable peripheral stimulation that can potentially act on peripheral sensitization mechanisms. For my nurse, we used paraffin before we used visualization. It did not require active movement and avoided cutaneous stimulation, which caused pain. I did myofascial release on the opposite arm. It was a gentle touch that relaxed her. We are stimulating the somatosensory system at a distant site in a comfortable area proximal to where the pain is.
Somatosensory Rehab and Graded Motor Imagery Combined (3/4)
- GMI:
- Regulates cortical reorganization mechanisms in CRPS
- Steadily integrates the progression of active mvmts in its advanced stages (graded activities)
- Graded activities create new neural connections, which helps normalize the representation of the affected body part in the primary somatosensory cortex
- 3 stages: L/R discrimination, motor imagery, mirror therapy
- SRM and GMI are two different mechanism-based intervention approaches
- (Stay tuned for 4th comment from the study)
(Quintal et al., 2018; Gift, 2018)
Graded motor imagery regulates cortical reorganization mechanisms in CRPS. We can integrate the progression of active movements in its advanced stages, like the graded activities that I talked to you about with the nurse with the CPR. These activities created new neural connections to help normalize the representation of the affected body part in the primary somatosensory cortex. We can map where in the brain the representation of pain is.
There are three stages: left and right discrimination, motor imagery, and mirror therapy. I have never had someone who could not tell their left from right, but you can start with photos to identify right from left.
I had a doctoral resident create a graded motor imagery handbook. Students are great at creating projects that are helpful in the clinic. They also know how to access research. Many people think, "I do not want to take a student because they're so much work." However, you can have them work a little for you in the clinic.
Somatosensory rehab and graded motor imagery are two different mechanism-based intervention approaches. There is one more comment from the study, which we will get into in the second case.
Top-down Modulation
- Gate control theory -> Neuromatrix Theory
- The brain interprets pain differently
- The brain neural network has genetic and sensory influences modulated by
- Stress, cognitive brain functions, and PNS
- Psychological factors are an integral part of pain processing
(Melzack, R., 1999)
Melzack and Wall came up with the Gate Control Theory. This is what revolutionized us using TENS in the clinic. They first published their evidence in 1965, and then in 1999, Melzack updated that and called it the Neuromatrix Theory. I love the Neuromatrix Theory because this talks about how the brain interprets pain differently. The brain neural network has genetic and sensory influences modulated by stress, cognitive brain functions, PNS, and psychological factors.
I like the way The Neuromatrix Theory fits into our psychosocial biopsychosocial theories. We know when we get stressed, we do not act as we should, and with everything going on in the world, there is a lot of stress. We can say to the person, "Your brain can change because the brain is plastic."
Pain Biopsychosocial Educational Approach
- Pain is our alarm system to protect us
- Sometimes alarm system is too sensitive even with no threat
- Together we will retrain the brain alarm system “to only alert you when protection is needed”
- (Gift, 2018)
- AOTA position statement: “The Role of OT in Pain Management”
- Supports OTs practicing from the biopsychosocial model (AOTA, 2021, p 4)
- Pain Neuromatrix Theory fits into this model
- (AOTA, 2021)
In a pain biopsychosocial educational approach, we can say pain is an alarm system to protect us, but sometimes it is too sensitive, even with no threat. An analogy would be walking by a car, sneezing, and the car alarm going off. If your "alarm" is too sensitive, it needs to be reset. You want to collaborate with the client on how to work together to retrain their brain.
AOTA has a position statement on the Role of OT in Pain Management, and this position statement supports OTs practicing from a biopsychosocial model, and the Pain Neuromatrix Theory fits into this model well.
Brain Pain
- Able to map pain intensity/pain processing to specific areas of the brain (e.g., hyperalgesia, allodynia)
- Are these changes due to CRPS or other chronic pain concerns?
- Does treatment focus on the cause or the consequence?
- “Most importantly, some abnormal brain changes … reversed, even normalized, concomitantly to the improvement of symptoms and CRPS resolution”
- “Improvement depends on the normalization of these brain changes.”
(Zangrandi et al., 2021)
With brain pain, we can map the pain intensity and processing to specific areas of the brain and can see it on an MRI. There can be changes due to CRPS or another chronic pain concern, so it can get tricky. When treating someone, we want to know about past trauma or experiences. We will get into this with my next case.
Does treatment focus on the cause or the consequence? Most importantly, abnormal brain changes can be reversed and even normalized. We want to let our clients know this, and improvement depends on normalizing these brain changes.
Neuroplasticity
- If we make our clients move their affected limb, does that make it worse?
- “People w CRPS can feel pain only by the thoughts of moving the painful part, thus creating additional discomfort that could even worsen brain changes”
- We must “improve sensorimotor control without creating pain, to normalize the brain neuroplasticity” and improve CRPS outcomes
- Need individual approach, since everyone responds differently
(Zangrandi et al., 2021)
If we make our clients move their affected limb, does that make it worse? People with CRPS can feel pain only by thoughts of moving the painful part, thus creating additional discomfort that could even worsen brain changes.
In my nurse's case, when I had her visualize, she was fine, Thus, I knew I could move on. However, if I have someone with whom visualization evokes fear, then I have to use a different approach.
We have to improve sensory-motor control without creating pain. Do not be a pain therapist. We have to improve the control without creating pain to normalize the brain neuroplasticity and improve the outcomes.
No two clients are alike, so we have to use different approaches. I think this is why a lot of our research is mixed because the research makes you only do a certain protocol.
Case Study 2: Linguist with R dominant DR fx
- Age: 59 yo
- Dx: R DR IA fx (FOOSH)
- DOI: 4-29
- DOS: 4-30. Closed reduction with k-wires in Baghdad, Iraq
- First seen in OT 6-8 with CRPS & PTSD
- Subsequent dx: cervical and lumbar herniation, R shoulder impingement. First seen in PT 7-14.
Here is my second case in Figure 4. Can you tell which hand has the issue?

Figure 4. The hands of the second case study.
Her hand is able to get flatter in this picture, but it took a long time. Even in the non-injured hand, there are arthritic changes going on.
She had a right distal radius interarticular fracture from a FOOSH injury, or fall on an outstretched hand. She was a linguist working for the US Army in Baghdad, Iraq. She had a closed reduction with k-wires in Baghdad, and I saw her two months later. It was obvious when I met her that she had CRPS and a lot of PTSD. She also had cervical and lumbar spinal issues, and her shoulder was not moving well.
I had to advocate for her to the doctors and insurance on my own time. It was a Federal Workers' Compensation issue. It took a lot to get her into the therapy that she needed.
- Pain 9/10. Stabbing, constant, pt. tearful
- What do you do to make it feel better?
- “I cannot make it better. I have pain in my entire R arm, low back, and hip.”
When I first see someone, I ask about their pain level, with zero as no pain and 10 being so bad that we need to call 911. She replied, "It is a nine out of 10, and it is stabbing and constant." She started to cry. When asked, "What do you do to make it feel better?" she replied, "I cannot make it better. I have pain in my entire right arm, lower back, and hip."
She had the typical protective posture but made it to the clinic. I said, "It's good you got dressed and made it here with all this going on." Remember, we want to show them some successes.
Figure 5 shows how much she can make a fist without hurting herself, even though she is in pain.

Figure 5. The client demonstrates limited finger flexion.
Figure 6 shows how much she can straighten over a rolled-up towel.

Figure 6. The client demonstrates limited finger flexion.
These images were three weeks after I started seeing her. I was seeing her three times a week and asked if she minded me taking pictures for teaching. She did not mind as she liked helping other people to learn.
PTSD/Pain
- Treatment mat supine:
- Culture
- War
- Past trauma
- Family/support systems
Her story may be triggering for some people, so please move on to the next section of the text, "Multiple Brain Changes," if so.
She was slumped with her shoulder internally rotated and her head leaning. I could tell she was hurting in this position. I put her supine on the mat with a wedge under her thighs to help her back and told her that I was going to do some gentle myofascial release on the opposite arm. The second I touched her, she started crying. We were in a private area, and I said, "It's okay. You're safe here." Then, she started telling me about her background.
OT Cultural and Psycho-Social Sensitivity
- Kurd
- Saddam Hussein
- Uncle
- Linguist in Iraq
- Shower
- Plane
- Husband
- Children
- Everything contributes to everything else
- Stress, fatigue, sleep, diet
- Psychological trauma
- Perceived threat value leads to pain response
- CNS, PNS
Learned non-use of the affected limb
(Woolf, 2010; Packham & Holly, 2018)
She is a Kurd from Iraq. Back in the eighties, Saddam Hussein gassed all the Kurds because he found oil on their nomadic lands. Her uncle was a leader, and he was kidnapped and ransomed. The tribe tried to get all the money together for the ransom, but they got a box with her uncle's head in it before they could do so. When we talk about past trauma, I have had people who have incurred broken bones or have been molested as a child. Often, therapy can bring back memories, and how our brain is affected by all these other things that have happened in our lives.
She had two children in college, but they did not want to be bothered by her and her discomfort. Her husband went to one of her appointments with her and said to the doctor, "When can we have sex?" She told me, "I am sick of him, and told him to get a mistress. I do not want anything to do with him and want him to move out of the house." I had to support these feelings on top of all the other things that we were working on, but this is all important.
Additionally, while she was in Baghdad working with the US Army, she told me there was one nice man who would stand guard while the very few women would shower so that nobody would rape or molest them. And, when you go home from the Army, you have to wait for the next plane out. The planes are full of dead servicemen that are also going back home.
This information was important to her, and I needed to address it. I tried to get psychological counseling for her, but it took a lot of time due to it being Federal Workers' Comp. My documentation had to have psychosocial types of notes and interventions in there.
Everything contributes to everything else. We want to ask how they are eating and sleeping and validate their experiences. Can we look at a sleep routine or a pillow to prop their arm when they sleep? We can also say, "You've had a lot of trauma." I do not think anybody ever recognized this with my client. A perceived threat value leads to a pain response.
What is going on centrally or peripherally? Do they have "learned non-use" of the affected limb? If they are not using their arm, we need to get to use it again.
Multiple Brain Changes
- “Neuronal maladaptive plasticity:
- The capacity of neurons to modulate…synaptic connections
- Long-term depression due to a decrease in synaptic strength
- Change may be influenced by neuromodulators (eg, dopamine, serotonin)”
Neuronal maladaptive plasticity is the capacity of the neurons to modulate our synaptic connections. Long-term depression is due to a decrease in synaptic strength, so for some people, neuromodulators, like dopamine or serotonin, can be helpful for some people. Some people on this webinar may be taking these, but we want an individualized approach.
Central Sensitization
- “The more often pain pathways are activated, the lower will be the threshold to trigger pain messages."
- “In chronic pain, the NMDA receptors (learning/memory) activate sensory and nociceptive pathways at a lower threshold of peripheral stimuli.”
(Zangrandi et al., 2021)
The more often pain pathways are activated, the lower the threshold is to trigger pain messages; it is this endless loop.
In chronic pain, the learning memory receptors activate our sensory and nociceptive pathways at a lower threshold. This is a good example to tell your client so they are educated on how this works.
Recall Case Report Journal Article: SRM & GMI combined (4/4)
- Pt also used TENS, cryotherapy, and superficial heat during the entire rehab
- TENS (x20 min) and cryotherapy (x1-2 min) on the ulnar nerve palmar branch because this nerve branch is in the vicinity of the allodynic area, but not directly on the painful territory. (Stim on neighboring nerve branch)
- Conclusion- For each patient: must choose the right intervention for that specific patient
(Quintal et al., 2018)
In the case report, they also used TENS, cryotherapy, and superficial heat. In this case, they put the TENS on the palmar branch of the ulnar nerve because this nerve branch is near the allodynic area, but not directly on the painful territory. Instead, it stimulates a neighboring nerve branch. You can stimulate the opposite spot on the arm on a totally different arm.
Again, choose the right intervention for that specific patient.
TENS for CRPS
- “…Approach must be individualized owing to the integrity of the brain and corticospinal function
- Non-invasive neurostimulation of the brain or of nerve/muscles/spinal roots, alone or in combination w conventional therapy, represents a fertile ground to develop more efficient approaches for pain management in CRPS.”
- (Zangrandi et al., 2021)
- C fibers: small diameter, little/no myelin, slow conductors of painful stim up SC to brain
- TENS inhibits C fibers by stimulating large-diameter, highly myelinated A-beta fibers
- A-beta fast conductors flood the path to the brain
- The gate closes before C fibers get to the brain, which reduces pain transmission
- (Bracciano, 2008)
For CRPS, the approach has to be individualized for the integrity of the brain and corticospinal function. In this article, they talk about non-invasive neurostimulation of the brain. We are not stimulating the brain with TENS but using it on nerves, muscles, and spinal roots.
Stimulation alone or in combination with conventional therapy represents a fertile ground to develop more efficient approaches for pain management.
Electrical Stimulation for Pain Control
- “It is almost always worthwhile to consider TENS as part of a multidisciplinary approach.”
- Low-intensity conventional TENS (<10 Hz): maximal analgesic effects
- High-intensity TENS (>50 Hz): spatially diffused analgesic effects
- Only high-intensity TENS produced long-lasting changes in the brain (S1 and M1 areas) and in their connectivity to a brain area that helps inhibit pain (vmPFC)
- Activation of pain inhibition systems promotes the release of endogenous opioids for a diffuse analgesic effect
If you try TENS on anybody with CRPS and succeed, write up your case study. I think case studies are valuable and have good outcomes, even if they are not RCTs or other complicated types of research.
I teach master's students about TENS, and Figure 7 shows different areas of the brain. The C-fibers are the small diameter fibers with little or no myelin and are slow conductors of the painful stimuli from the spinal cord to the brain.
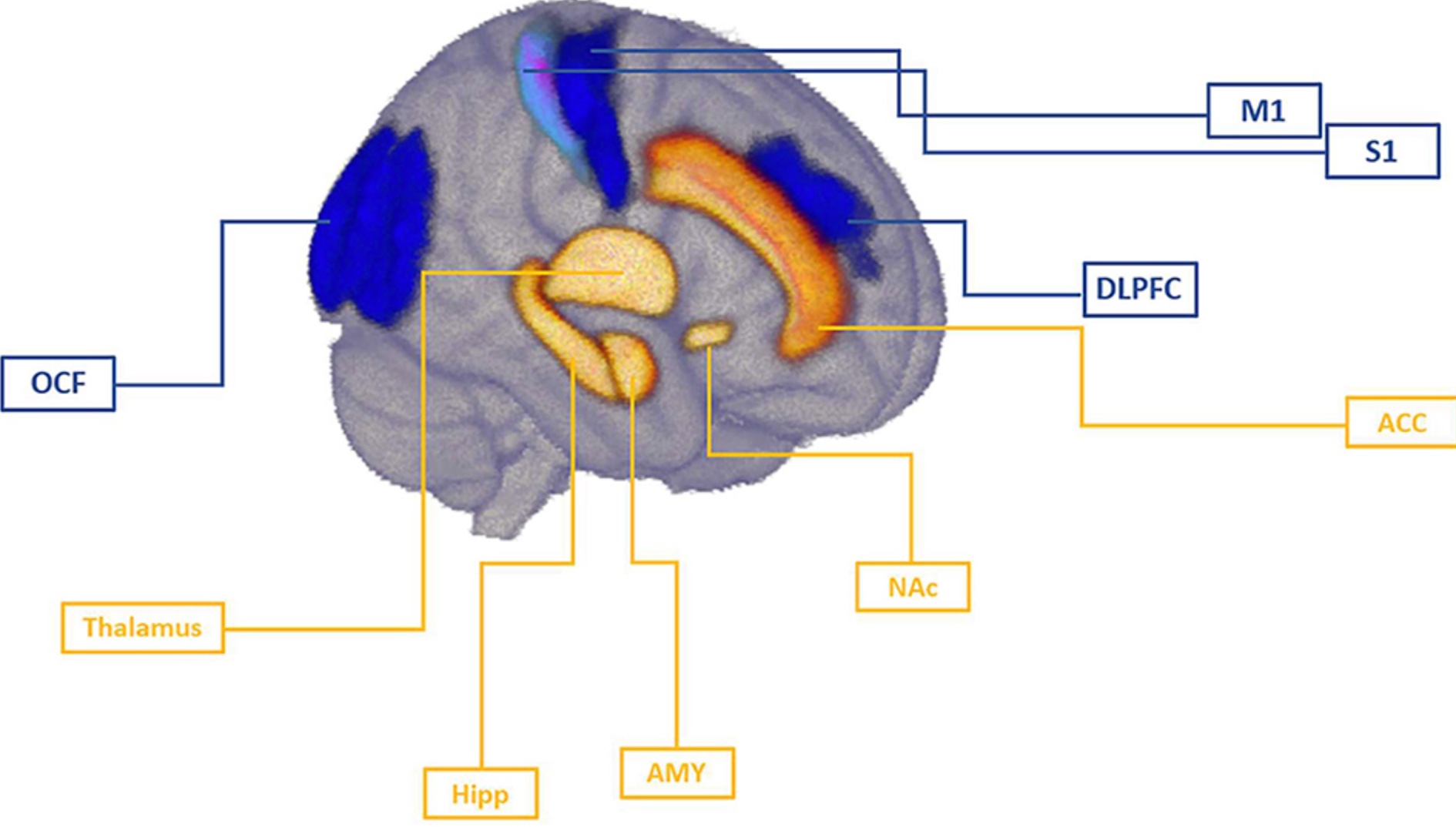
Figure 7. Areas of the brain.
The TENS inhibits the C-fibers by stimulating large-diameter, highly myelinated A-beta fibers. They get there first and are not the super painful ones that everybody talks about when they have uncontrollable pain. The A-beta floods the path to the brain, and the gate must close before the C-fibers reach the brain. This reduces pain transmission. An example is when you bump your arm. The first thing you do is rub your arm, providing deep pressure. This helps to stop the discomfort of that initial banging of your arm into the wall.
The Pain Frontiers article says it is almost always worthwhile to consider TENS as part of your approach.
There are different kinds of TENS. High-intensity TENS produces long-lasting changes in the brain in specific areas that we can map in the brain. Those are the top two areas of that brain picture that you see(S1 and M1)). Their connectivity to the brain area helps inhibit pain, which can also be mapped in your brain on MRI studies.
Activation of pain inhibition systems promotes the release of endogenous opioids; thus, TENS can release endogenous opioids. An example of that is a runner's high without drugs. It is pure TENS. Some people say that TENS did not work for them, but I always say, "Can you try it with me?" Perhaps, they did not manipulate the TENS unit in a way that can help them specifically. If you earn their trust, they may be willing to try with you.
TENS Clinical Reasoning
- 9/10 constant pain entire R UE
- Cannot hold a coffee mug
- Pt guards entire R UE: Just think to yourself--
- Where will you place electrodes?
- What are you targeting? (muscle, nerve, bone?)
- Why?
- What ther-ex while TENS is in place?
My client had a nine out of 10 constant pain in her entire right arm. Her main goal was to hold a coffee mug. "I need my coffee, and no one is helping me at home." She guards her entire right upper extremity, so pause and think about where are you going to put the electrodes. Figure 8 shows where I placed the electrodes.
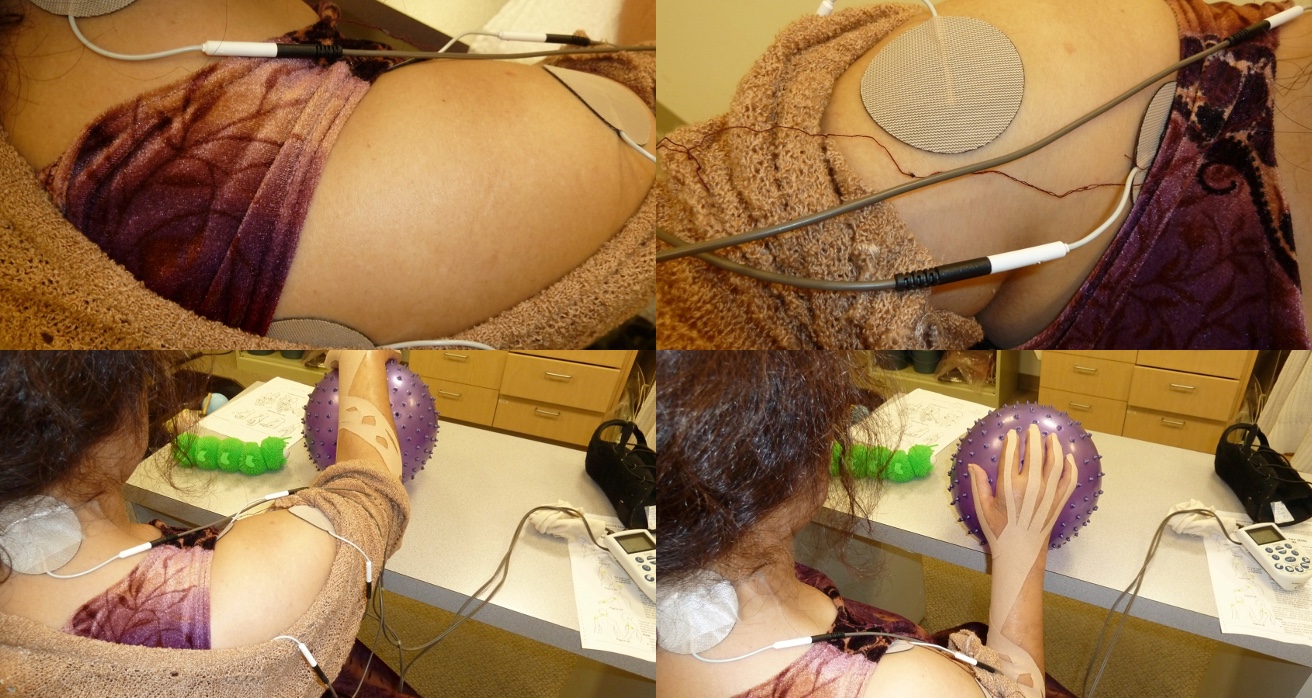
Figure 8. Treatment with client #2.
What are you going to target (muscle, nerve, or bone, and why are you targeting that? What exercise are you going to have her do while the TENS is in place? I do not typically have them sit there with the TENS. I want them to do some exercise or diaphragmatic breathing to help with the stress and to calm down the heart rate, which we can measure.
I used two leads with four electrodes around the brachial plexus with this client. I said, "I'll put it on your other arm so you can see what it feels like," and she said, "No, I trust you." With the TENS in place, I had her roll a rubber ball that was a little bit deflated. With the ball, she was getting shoulder, elbow, wrist, and finger motion. She gets a little wrist extension when rolling toward her by keeping her palm on the ball. The table supports her entire arm so she can control how fast or slow she moves it. I want to ensure the table is the right height so there is no shoulder hiking.
I can also gently place my hand on her shoulder to give her proprioceptive input. She can do shoulder flexion, horizontal abduction, and adduction.
She did not like the kinesiotape or the thermal glove we were trying to use for edema and pain control, so we discontinued them. Figure 9 shows a close-up of her holding a mug and a caterpillar toy.

Figure 9. The client holding a mug and a caterpillar toy.
She loved the caterpillar. It is cool to the touch, and she liked that feeling. If you shake it enough, it would blink. If people cannot do their normal things, they are going to get depressed. Give them something totally out of the norm, especially if they like fun. To shake the caterpillar, she had to abduct her thumb a little bit while her arm was supported on the table. The bottom picture is a plastic clapper. If you move it gently, it makes a noise. I also have a chicken that I bring out that squawks when you squeeze it. She could not make it squawk with one hand but could do it with two. Then, she would burst out laughing. She said, I only laugh here." These silly activities can be fun and create new neural connections.
For holding a coffee mug, I started with something much smaller so that she had success with the thumb abduction. We had to grade the activity to get more water in there. Next, we moved to filling a container in Figure 10.

Figure 10. The client is filling a container.
We had cool water in the tub because that felt good to her. I had her put water into the container and then dump it into the tub. This worked on shoulder flexion, abduction, and pronation.
Selection of TENS Waveforms is Confusing
- Uncontrolled variables
- Pathologies
- Tissue conductivity continuously changes
- Intersubject variations
- Body parts
- Equipment differences
Waveforms are confusing, as there are too many uncontrolled variables, and I think that is why our research often does not work.
TENS for Pain Control
- “It is almost always worthwhile to consider TENS as part of a multidisciplinary approach”
- Idiot button
- Waveforms ??? pps?
- Bracket nerve, muscle, painful area, or neighboring site?
(Zangrandi et al., 2021)
"For pain control, it is always worthwhile to consider TENS as part of a multidisciplinary approach." This is from the article in Pain Frontiers. In my class, I teach students to try different settings to see what they like. I then poll them to show how everybody is all over the map with what they prefer. For example, if I prefer 35, but you have me on 100, is that going to work? No, it is very easy to go into the TENS unit and change it.
I started bracketing the brachial plexus, but you could also put it on a neighboring painful area or the opposite arm. She once came in and asked, "Can we try it here?" We moved the electrodes to where she wanted, and she liked it. The next time, she said, "Instead of bracketing, can we put it directly on this area?" We moved it again. Listen to your client, as they know their body better than anybody else.
It took a while for her insurance to allow it, but my client got a TENS unit for her home. This was very effective as she could walk around with it.
Nutrition/Diet
- Vitamin C after wrist fx:
- People who take high doses of vitamin C after wrist fx have a lower risk of CRPS compared to those who do not take vitamin C
- Vitamin C > 0.5 g/day, 45-50 days post wrist fracture sx
- Vitamin C is an antioxidant, preventative for early on changing the cascade
- Antioxidants control the body’s immune response to sx
(Carr, 2017; Gift, 2020)
People who take high doses of vitamin C after a wrist fracture have a lower risk of CRPS than those who do not take vitamin C. Vitamin C is an antioxidant that can help the body's immune response to surgery. So maybe people need to be taking vitamin C.
Others may ask about the influence of sugar on the diet. I typically say, "I am not a nutritionist or dietician, however, that might help."
Research Needed
- “Studies ought to clearly identify
- If there are responders and non-responders to one or another technique
- If brain changes detected are due to CRPS or other consequences of limb non-use related to chronic pain”
- Crucial to customize an individual approach
- Recommend more research on neurostimulation of the brain or of nerve/muscles/spinal roots, alone or in combination with other treatments
(Zangrandi et al., 2021)
We need more research to clearly identify if there are responders and non-responders to different techniques. We also need to know if the brain changes are detected due to CRPS or other consequences of limb non-use related to chronic pain.
Have I knocked you over the head enough with an individual approach? I hope so, as it is crucial to treatment.
More research is needed on neurostimulation, either the brain, nerves, muscles, or spinal roots, in combination with other treatments. TENS works well on nerves, especially if you want to treat a broad area.
Neuromatrix
- Inputs into the system and outputs into the behavior response
- Bottom-up
- Address symptoms
- e.g., Swollen hand -> wear a glove
- Top-down
- Help them understand pain neuroscience and what their triggers are for self-management
- Retrain brain responses to peripheral stimulation
- Graded activities for new perceptions
Back to our neuromatrix, the behavior response has inputs and outputs. Bottom-up is what I concentrated on, although we did touch on biopsychosocial and mechanical types of things with these clients.
For top-down, we want to help them understand pain neuroscience and their specific triggers for self-management. We want to retrain the brain responses to that peripheral stimulation and grade activities for new perceptions.
CRPS Conclusions
- Each person with CRPS presents with unique symptoms
- Recovery varies
- Tailor treatment approach to the individual:
- CNS, PNS, both
- Validate, educate, support
- Create success
Each person with CRPS presents with unique symptoms. Recovery varies, and we have to tailor the treatment approach to the individual, either the central nervous system types of things, peripheral nervous system types of things, or both. Always validate, educate, and support them to create success.
These two clients appreciated that we could laugh in the clinic when they felt so hopeless. It was also important to grade the activities so they could have success.
Summary
This is the best way to reach me, rxrubino@outlook.com. Please put in this subject title line, "CRPS webinar." I would like to thank you for attending.
References
AOTA (2021). Position statement-role of OT in pain management. AJOT, 75(Suppl.3), 7513410020. doi.org/10.5014/ajot.2021.75S3001
Birklein, F., O'Neill, D., & Schlereth, T. (2015). Complex regional pain syndrome: An optimistic perspective. Neurology, 84(1), 89–96. https://doi.org/10.1212/WNL.0000000000001095
Bowering, K. J., O'Connell, N. E., Tabor, A., Catley, M. J., Leake, H. B., Moseley, G. L., & Stanton, T. R. (2013). The effects of graded motor imagery and its components on chronic pain: A systematic review and meta-analysis. The Journal of Pain, 14(1), 3–13. https://doi.org/10.1016/j.jpain.2012.09.007
Bracciano, A. G. (2008). Physical agent modalities: Theory and application for the OT. 2nd Ed. SLACK, Incorporated.
Carr, A. C., & McCall, C. (2017). The role of vitamin C in the treatment of pain: New insights. Journal of translational medicine, 15(1), 77. https://doi.org/10.1186/s12967-017-1179-7
Dilek, B., Ayhan, C., Yagci, G., & Yakut, Y. (2018). Effectiveness of the graded motor imagery to improve hand function in patients with distal radius fracture: A randomized controlled trial. Journal of hand therapy: Official journal of the American Society of Hand Therapists, 31(1), 2–9.e1. https://doi.org/10.1016/j.jht.2017.09.004
Gabel, C. P., Michener, L. A., Burkett, B., & Neller, A. (2006). The Upper Limb Functional Index: development and determination of reliability, validity, and responsiveness. Journal of hand therapy: Official journal of the American Society of Hand Therapists, 19(3), 328–349. https://doi.org/10.1197/j.jht.2006.04.001
Gift, H. (2020). Dietary influences on neuropathy symptoms. ASHT Times, 27(2), 10-12.
Hamasaki, T., Pelletier, R., Bourbonnais, D., Harris, P., & Choinière, M. (2018). Pain-related psychological issues in hand therapy. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 31(2), 215–226. https://doi.org/10.1016/j.jht.2017.12.009
Hays, R. D., & Morales, L. S. (2001). The RAND-36 measure of health-related quality of life. Annals of medicine, 33(5), 350–357. https://doi.org/10.3109/07853890109002089
Llewellyn, A., McCabe, C. S., Hibberd, Y., White, P., Davies, L., Marinus, J., Perez, R., Thomassen, I., Brunner, F., Sontheim, C., Birklein, F., Schlereth, T., Goebel, A., Haigh, R., Connett, R., Maihöfner, C., Knudsen, L., Harden, R. N., Zyluk, A., Shulman, D., … Moskovitz, P. (2018). Are you better? A multi-centre study of patient-defined recovery from Complex Regional Pain Syndrome. European journal of pain (London, England), 22(3), 551–564. https://doi.org/10.1002/ejp.1138
Mayo Clinic (n.d.). Complex regional pain syndrome. Retrieved from: https://www.mayoclinic.org/diseases-conditions/crps-complex-regional-pain-syndrome/symptoms-causes/syc-20371151?p=1
Melzack R. (1999). From the gate to the neuromatrix. Pain, Suppl 6, S121–S126. https://doi.org/10.1016/S0304-3959(99)00145-1
Miller, C., Williams, M., Heine, P., Williamson, E., & O'Connell, N. (2019). Current practice in the rehabilitation of complex regional pain syndrome: a survey of practitioners. Disability and rehabilitation, 41(7), 847–853. https://doi.org/10.1080/09638288.2017.1407968
Nelson, K. W., Hayes, D. & Currier, P. (1999) Clinical electrotherapy, 3rd ed. Roger M., Appleton & Lange, Stamford, Connecticut
Quintal, I., Poiré-Hamel, L., Bourbonnais, D., & Dyer, J. O. (2018). Management of long-term complex regional pain syndrome with allodynia: A case report. Journal of Hand Therapy, 31(2), 255-264.
Smart, K. M., Wand, B. M., & O'Connell, N. E. (2016). Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. The Cochrane database of systematic reviews, 2(2), CD010853. https://doi.org/10.1002/14651858.CD010853.pub2
Packham, T., & Holly, J. (2018). Mechanism-specific rehabilitation management of complex regional pain syndrome: Proposed recommendations from evidence synthesis. Journal of hand therapy : official journal of the American Society of Hand Therapists, 31(2), 238–249. https://doi.org/10.1016/j.jht.2018.01.007
Packham, T. L., Spicher, C. J., MacDermid, J. C., Michlovitz, S., & Buckley, D. N. (2018). Somatosensory rehabilitation for allodynia in complex regional pain syndrome of the upper limb: A retrospective cohort study. Journal of hand therapy: Official journal of the American Society of Hand Therapists, 31(1), 10–19. https://doi.org/10.1016/j.jht.2017.02.007
Woolf C. J. (2010). What is this thing called pain? The Journal of clinical investigation, 120(11), 3742–3744. https://doi.org/10.1172/JCI45178
Zangrandi, A., Allen Demers, F., & Schneider, C. (2021). Complex regional pain syndrome. A comprehensive review on neuroplastic changes supporting the use of non-invasive neurostimulation in clinical settings. Frontiers in pain research (Lausanne, Switzerland), 2, 732343. https://doi.org/10.3389/fpain.2021.732343
Questions and Answers
Do strategies remain the same for children? I have a 12-year-old suffering from chronic right upper limb pain.
I would ask the child, "Do you want to improve this?" You want to get buy-in and then try to discuss other topics. What TV shows do you watch? What music do you like? Depending on the child's interests, I may play music, or we may dance. Dancing allows for more spontaneous movement of your arms. I would definitely try this, as it is such a great area. If some of your techniques work, you could present the information somewhere.
I do not know if you're a member of ASHT, but they have a newsletter. You do not have to be a researcher to publish your work. You can even poll people, "What are other people doing for children?" I think that is a ripe area.
I am an OTA that has worked in a skilled nursing facility for 15 years. I think I see CRPS in stroke patients, mostly in the upper arm and shoulder.
Yes, CRPS can definitely happen with people who have had strokes. Their arms are independent positions, and depending on their stroke, people tug at that arm when they try to get out of bed or off a commode. They are in slings and dependent positions, which can cause edema and pain.
You can still help. TENS may be helpful if they have good cognition. You can put it on their other arm and then go from there.
Do you find that psychologists and psychiatrists are educated in CRPS?
I worked at a university hospital. I am not trying to throw shade, but I think the people in the pain management area only used ketamine and stellate ganglion blocks. I have not seen people get relief with those. I would talk to referring hand surgeons and say, "That's all they're doing, and I do not think it is helping." They would say, "Yeah, I do not think it is helping, but I do not know what else to do." I would then ask for a psychology evaluation. It is so hard to see somebody nowadays with all the other mental health things going on.
At USC, we have a program, Lifestyle Redesign, that helps with pain management strategies and cognitive behavioral therapy. I think OTs may be better than some psychologists, unless they need some medications.
One idea that might be considered as an adjunct treatment is a simple Chinese Qigong treatment for total body movement and nervous system integration.
I think that is great.
I have a certification in structural yoga therapy, another technique you can use. Is there anybody in your organization who does these kinds of alternative treatments?
I use a lot of gentle, myofascial release on these people. It is fun if you want to learn more about it. Many other approaches out there can help with whole-body-mind connections.
Citation:
Rocker, J. (2023). Complex regional pain syndrome: Functional, biomechanical, and psychosocial Interventions. OccupationalTherapy.com, Article 5587. Available at www.OccupationalTherapy.com
