Introduction
Carrie: We are so happy to be back and presenting again on developing in the NICU. Today is Stress Cues and Strategies for Infant Feeding, and it is the third part of a series. I am Carrie and this is my sister, Jenny.
Evidence on Feeding
- 70% of infants born prematurely have trouble transitioning to breast or bottle feeding (Dodrill, 2011).
- Feeding difficulties in infancy often lead to long-term eating problems (Pickler et al., 2009).
- Feeding difficulties lead to poor parent bonding, adding stress to an already stressful time in a family's dynamics (Medoff-Cooper et al., 2009).
- The cue-based clinical pathway for oral feeding initiation and advancement of premature infants resulted in the earlier achievement of full oral feeds (Kirk et al., 2007)
- A relationship exists between consistency & continuity of feeding practice and improved feeding performance (Sable Baus et al., 2013).
"Houston, we have a problem." Seventy percent of infants born prematurely have trouble transitioning to breast or bottle feeding (Dodrill, 2011). And, feeding difficulties in infancy often lead to long-term eating problems and poor parent bonding adding stress to an already stressful time in family dynamics (Pickler et al., 2009; Cooper et al., 2009). A cue-based clinical pathway for oral feeding initiation and advancement of premature infants resulted in the earlier achievement of full oral feeds (Kirk et al., 2007). Lastly, a relationship exists between the consistency and continuity of feeding practice and improved feeding performance (Sable Baue et al., 2013). Some of these references are older, but they had already identified feeding is an issue in the NICU.
Feeding Problems Upon Discharge
Then, as babies get discharged, there is an even bigger issue. New parents realize that they have a poor feeder on their hands. It does not take much to scratch the surface of the Internet and find that preemie moms are reaching out for help as they are discharged with a poor feeder and do not know how to support that. There are people all over the Internet reaching out for the help that their preemies will not eat after coming home.
Suck-Swallow-Breathe (SSB)
SSB occurs across multiple neuromotor and sensory pathways converging together & even cross-activating the same areas of the brain during feeding as language.
The pattern of suck-swallow-breathe occurs across multiple neuromotor and sensory pathways converging together and even cross-activating the same areas of the brain during feeding as language. There are a lot of areas that light up with feeding.
Volume Feeding
Short-term Problems of Volume Feeding
- Delayed discharge
- Rising costs
- Family stress
- Staff struggling to feed
What are some of the short-term problems of volume feeding? The first problem is a delayed discharge. The second problem is the rising costs. Increased family stress and staff struggling to feed appropriately are the third and fourth issues.
Long-term Outcomes of Volume Feeding
- Oral aversions
- Failure to thrive
- Language delay
- Feeding therapy
There are long-term outcomes of volume feeding as well. We see oral aversions, failure to thrive, the need for feeding therapy. Most of these babies end up needing feeding therapy after they get discharged. And, if you look back in the previous slide, there is cross-activation in the brain where language is formed. Thus, they may also have language delays.
Where Do These Problems Come From?
- Not normal- When the womb is lost, a storm of sensory input changes their sensory system.
- Too much, too soon- Sight, sound, multiple types of touch, pain, temperature changes & gravity assault the system.
- VIP- As caregivers, you become part of the new environment. Everything you do matters.
- Outdated- Volume-feeding does not align with current neuroscience.
Where do these problems come from? When the womb is lost, a storm of sensory input changes the preemie's whole sensory system. It is too much, too soon with sight, sound, multiple types of touch, pain, temperature changes, and gravity all assaulting the nervous system. As caregivers, you become a part of this new environment, and so, everything that you do matters. Feeding can contribute to the amount of stress the preemie is experiencing when trying to learn this new skill. And, we are using an outdated way of feeding preemies. Volume feeding does not align with current neuroscience and what we know how the brain wires around sensory experiences. What we end up doing is creating the poor feeders just by doing what we have been doing all along.
Sensory Memory
- When something is repetitive, it makes a memory in the hippocampus of the brain.
- Hippocampus- Long-term memories are stored throughout the brain as groups of neurons that are primed to fire together in the same pattern that created the original experience.
When something is repetitive, it makes a memory in the hippocampus of the brain. Long-term memories are stored throughout the brain as groups of neurons that are primed to fire together in the same pattern that created the original experience, creating a sensory memory. "Neurons that fire together, wire together."
It's Not Just Eating
- Many preemies in outpatient therapy have issues with sensory input to their hands, feet, face, and head; all areas that experience so much variety of touch during hospitalization.
Many preemies in outpatient therapy have issues with sensory input to their hands, feet, face, and head. All these areas experience a variety of touch during hospitalization. If you have ever dealt with a kid that has a sensory processing disorder or has sensory issues, you understand how the normal type experiences like putting on a sock can feel to them. These preemies' neurons were fired and wired together around new (sometimes noxious) experiences setting them up to be overstimulated to just normal activities.
Volume is king. In the traditional culture, signs of stress during feeding often went unnoticed and unsupported allowing the pattern of negative oral feeding experiences to be unknowingly reinforced. Because we are just trying to get the baby to eat, we ignored a lot of signs that a baby was trying to communicate.
History of Volume Feeding
- In the traditional culture, signs of stress during feeding often went unnoticed and unsupported, allowing the pattern of negative oral feeding experiences to be unknowingly reinforced.
- The first decades of neonatology focused primarily (and necessarily) on helping infants survive.
- Intermittent gavage was the only means to provide the infant with full volume if they fatigued.
- Insertion and removal of the tube caused gagging and emesis every 3 hours. "Getting" the infant to eat the remainder seemed benign in comparison.
Let's now look at the history of volume-feeding. The first decades of neonatology focused primarily on helping infants survive. How did this culture develop? Intermittent gavage was the only means to provide the infant with full volume if they fatigued. Insertion and removal of the tube caused gagging and emesis every three hours. So, getting the infant to eat the remainder seemed benign in comparison.
When we only look at quantity, we are missing a critical component of feeding which is the quality of the feed. How did the infant take the milliliters? This is important because OTs look at the quality of activities that people do in their lives and this pertains exactly to infants trying to learn this new skill.
We are now at a crossroads for infant feeding. The difference is between "feeding them" and "helping them learn to eat." As OTs, we obviously know that you have to practice any new skill and this is no exception. These preemies need to learn the skill of eating rather than just feeding them.
Infant-driving Feeding
- Infant-driving feeding has emerged as the clinical gold standard for preterm and sick term infants transitioning to oral feeding (Nfant, 2016).
Infant-driven feeding has emerged as the clinical gold standard for preterm and sick term infants transitioning to oral feeding. It was created by Sue Ludwig and Kara Waltzman, and it is a specific protocol that is recommended if your hospital or NICU can adopt this method in teaching preemies how to feed.
- True or False? A successful feed is defined only by the volume that the infant consumes. FALSE
- True or false? Feeding "competition" in the NICU teaches parents and caregivers that THEY are completely responsible for the volume that the infant consumes? TRUE
- True or false? It is acceptable to use any technique to get the infant to take more volume regardless of the stress signs displayed. FALSE
In summary, volume alone is no longer the definition of successful feeding. Both volume and quality matter. Secondly, we recommend IDF, infant-driven feeding, be adopted in hospitals and NICUs because it recognizes your critical thinking skills, not your feeding skills. And, your ability to feed says nothing about the ability of the infant. If we can constantly do and do a task for the infant, they do not learn. Then, when they are discharged, problems arise as the baby did not truly learn to feed and eat.
What signs should we look for if a baby is ready to eat or should continue to eat? Just because you start the feed, doesn't mean you should always finish it. And Jenny's going to go over the stress signs, right now.
How Does A Baby Communicate?
Respiratory/Cardiac/Digestive Systems
Respiration
- Oxygen saturation < 90%
- Changes in color: such as red, pale blue, ashy gray
- Oddly timed coughing, sneezing, hiccuping, or sighing
- Cardiac
- <100 or >160 beats/min
- Digestion/Elimination
- Gagging, gasping
- Excessive reflux
- Undigested residuals
Jenny: What are some signs of stress? When the oxygen saturation drops below 90 is one sign, but it is easier to intently watch the baby to look for color changes. This is much more indicative of the baby's experience over a number on a monitor. They may quickly change colors between red, pale blue, and ashy gray. When I was first started my journey in feeding compromised infants, I remember hearing that infants changed colors and thinking, "Oh boy, how do you ever figure that out?" However, it really is quite an obvious sign. This is also great for parents as they can recognize this very quickly and not have to worry about what the numbers are saying. They can see in realtime what is happening to their baby's respiratory system. Oddly timed coughing, sneezing, hiccuping and sighing are other signs. Unfortunately, a lot of people think that these are common, but it is not. These signs are the nervous system's way of telling us that the respiratory system is not keeping up with what the demand is. The demand at the time of feeding is swallowing and holding your breath for one swallow which is adding up over time, especially with our babies who do not have sufficient suck-swallow-breathe. Every time they swallow, they are essentially stopping breathing for a second. And then the more a baby is swallowing, the sooner they can get behind in those respirations. Then, you may see gasping or drops their O2. So, if you look for these little coughing, sneezing, hiccuping signs and teach parents about those, this is realtime information about the respiratory system to help them decrease stress during feeding.
Beats that drop below 100 or go over 160 is indicative of a heart overworking or underworking. We definitely need to pay attention to this. And in this case, you probably have missed respiration cues of stress and now the heart is responding. The primary stress response is in the breathing, and then when that gets ignored, either intentionally or inadvertently, the heart will begin to also stress.
There also might be gagging, gasping, excessive reflux, and undigested residuals before the next feed as signs of stress in the digestion/elimination system. In the baby feeding world of the hospital, these kinds of digestion and elimination stresses get overlooked. "This is just the NICU baby experience." This is the thought process we have to get away from and something that OTs have to constantly educate on. None of this should be considered normal. We need to get to the source of the problem, not bandaid the symptoms that we see because they do have long-term consequences in how a baby wires their feeding experiences. As an example, we do not want a baby to have excessive reflux. Acid filling the esophagus is uncomfortable and very quickly gets associated with the response to reject feeding. Gagging and gasping feels like you are dying. Even as adults, we can understand how stressful that is and undigested residuals tell a lot about the microbiome of the preemie which is super important for their immunity and their continued neurodevelopment.
Since feeding is supercritical for life, we have to take all of this at the same time and make daily decisions about how our baby is practicing eating.
Other Signs of Stress
- Finger splaying (STOP)
- Taut mouth
- Nasal flaring
- Furrowed brow
- Stiffening or flopping of musculature
What are some signs of stress? A lot of people know that finger splaying, or full extension of the hand is a stress sign. It is commonly called the stop sign in the NICU. You can see a taut mouth, nasal flaring, a furrowed brow, and then the stiffening or flopping of musculature. You can see this with neurological shutdown. When a baby is being asked to continue to eat when they have already given their stress cues over and over, they will eventually lose all their tone and do this flopping posture. Many parents will perceive that as, "They are just tired. Let's wake them up." The final result is a baby that either gets floppy or the opposite which is stiffening. Stiffening can be quite alarming especially for any babies who have had any type of adverse brain event. Basically, almost every baby in the NICU has had this either from early or traumatic birth. Stiffening is a full-body kind of rejection of what is happening at the moment. You are going to see that first, and then it will be followed by the flopping out or neurological shutdown. Those are the final stress cues that are going to shut a baby down. An eating experience at this point will not be beneficial to them.
I love this watercolor and I print this for every one of my patient's parents and I tape them all over the isolette (Figure 1).
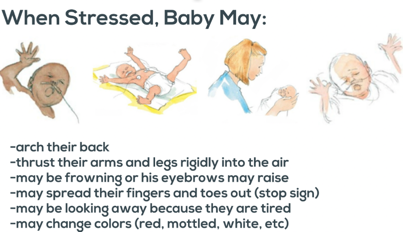
Figure 1. Stress signs resource.
When a baby is stressed, you may see them arch their back and thrust their arms and legs rigidly into the air. They may frown or their eyebrows may raise. They also may spread their fingers and toes out in the stop sign or look away when tired. Lastly, they may change colors to red, mottled, or white. This simple visualization can subtly encourage parents, caregivers, and staff to recognize these signs and slow down in response to them. They can take a scan of the environment to assess what might have caused the baby's reaction. It is beneficial to watch these in realtime.
Video 1
This is a mom and dad with their baby completing the first feed. These are solo feeding experiences that parents have recorded. This is a preemie, and we are going to look for color changes, stop signs, frowning, leaking at the mouth, and any kind of respiratory stress that we just talked about. Listen to the conversation between the parents because it is very telling that they have no education from any of the staff about what to be looking for or even how to feed this baby. So, you can see very clearly how this cycle of feeding in the NICU gets perpetuated and becomes a rampant problem.

As you can see, the poor mom gets defensive because she was feeding the baby. However, it does not take a trained eye to recognize that the baby is changing colors. What it takes is understanding what that color change means. There were a good five seconds before that choking experience happened. It could have been prevented with the first double stop sign. And while that was a very quick experience, we know these babies are making millions of neuronal connections all seconds of the day and night. Each time they have an experience like this, they learn that feeding is uncomfortable. They may feel like they are drowning. They cannot breathe and are trying to clear their lungs. This is something that is happening every single day with many staff and parents feeding babies. The simple recognition that the baby turned white tells you ahead of time it was not a great time to feed the baby as he was clearly having some respiration issues.
Video 2

You can see the fluorescent light that is right over that baby's eyes, as well as the beeping alarms which are almost unavoidable in the NICU setting. These are environmental factors in how a baby experiences their sensory environment. The baby is beginning to exhibit double stop signs even before the feeding continues. The parent does not recognize it and continues. You can also see gaze aversion. It is not the best video quality, but you can see how the baby is trying to turn away from the bottle. These signs are subtle but loud. Once you know them, you cannot miss them. They burn an image in your head about what is happening in that baby's brain. We need to use our common sense. Babies, unfortunately, are not thought of as intelligent creatures from the beginning. We believe we need to help them to survive and eventually, they will become more human-like in their behaviors. This is absolutely incorrect. The infant brain, even when arriving prematurely, shows tremendous potential to wire around its sensory experiences. And, it can be wired positively from the beginning if we have the knowledge and tools.
Video 3

We see some frowning. The baby's eyes are closed with some more stop signs on the side. Every one of these things is just compounding how this baby is experiencing stress in feeding. This is no different than if you were going to go take up skiing. You go to Colorado and hit the slopes. The first day you fall the whole way down and get some bruises. You are uncomfortable and sore the next day. You might not want to jump up out of bed and hit the slopes again. That is no different for how a baby learns to eat. If a baby is having negative experiences during a feed, then the next time we go to feed him, which is typically three hours later, the next feed is probably not going to go well. We are not going to address scheduling in this continuing ed, but scheduling infant feeding also plays a part in a baby's ability to learn to eat. We have to create positive practice experiences so they will want to try again. This is why we know that when we do not recognize this, the long-term outcomes end up being poor oral sensory feeders and late talkers.
Video 4

This baby does not really look hungry to me. At the end of the video, the baby begins to suck, and the dad says, "Good boy." However, there is a sucking reflex on the roof of the mouth on the hard palate. Any stroke of your finger, a nipple, or a pacifier will elicit this reflex to begin sucking. When we do not understand infant neurology, this can contribute to the problem overall. If we are using the sucking reflex to continue to feed the baby, then they obviously have no control over the experience. "I am telling you that I'm stressed and yet I have to keep sucking." We are just compounding that stress experience. The parents do not realize that if they keep sticking the nipple in the baby's mouth, they are going to hit that reflex at some point and the baby is going to start sucking. You need to base your assessment only on how the baby is responding to the eating and not by the fact that they are sucking.
The Five Systems Exhibiting Stress
- Autonomic: Mottled skin
- Motor: Decreased tone
- Slack jaw
- Excessive leak
- Unfisted hands
- State: Neurological shut-down
- Interactive: Absent
- Self-regulatory: Absent

Figure 2. Example of systems exhibiting stress.
This is a still picture, but it is very clearly a baby in a neurological shutdown. The baby has a leaky mouth and mottled skin color with blues and red. There are also two open palms. Fisted hands are a sign that tells us whether a baby is hungry and truly ready to practice eating. This is because they are alert and ready to go. They have the muscle tone that is ready to practice. A baby that is loose and limp is not.
We covered the different systems above in the second part of this series. This is Als' Synactive Theory of Development. We can identify five systems exhibiting stress here. The autonomic system keeps us alive for respiration, heart rate, and digestion. This baby has mottled skin so there is a respiration issue. By looking at the picture, we can also see a nasal cannula. Thus, this baby does not breathe well on its own and is already at risk for poor feeding experiences. We should question why are we feeding a baby that cannot maintain their breathing. Why are we feeding these babies? Feeding is an intricate response in the body that is learned by sucking, swallowing, and breathing. If they do not even have their breathing down, we are doing these babies a major disservice to try to teach them to eat. That is in full display with the mottled skin.
For the motor system, we see decreased tone and a slack jaw. There is an excess leak around the mouth and unfisted hands. The baby is floppy in their musculature. They may have gone from a normal tone to low tone. Or, they maybe did a stiffening right before this and then flopped out into shutdown.
What is their state? Are they in a quiet alert? Are they active alert? Are they drowsy? Sleeping, light sleeping, or deep sleeping? This baby is in neurological shutdown which is a survival mechanism of the premature and early newborn that when they have too many stimuli. They will reject their environment.
This baby's interactivity and self-regulatory abilities are absent. In the bottom tier of the triangle that Dr. Als created, the foundation is autonomic. So, this one is actually in reverse in terms of how we look at it. The highest achievement would be a baby's ability to interact during a feed. But, what happens is that each system will shut down until you get to the last one which would be the self-regulatory system that is also absent. There are obviously no coping skills happening there.
We are now going to go through this again with this baby, who looks completely different than the last baby but is still telling a tale about how they are enjoying their feeding experience (Figure 3).
- Autonomic: Slightly red
- Motor: Raised eyebrows, wide-eyed
- State: Active alert/panic
- Interactive: Likely to gaze avert
- Self-regulatory: Stops sucking
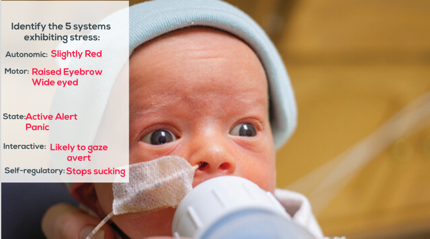
Figure 3. Another example of systems exhibiting stress.
In this picture, the baby is slightly red so we know that there is a respiration issue. The baby's raised eyebrows and wide eyes show that they are experiencing motor stress. The state that you see this baby in is called active alert or panic. This is pretty easy to recognize. We cannot see the quality of the interaction as this is a picture, but my best guess is that if this was a video, this baby would immediately start looking to the left or to the right in order to shut down the visual system. And then for self-regulation, the only coping skill a baby would have would be to stop sucking if their hard palate was not being touched. So, if they had the opportunity when their swallowing reflex was not being activated, they would stop sucking to diminish the stress that they are feeling.
Video 5
In this next video, think about this baby's color, alertness, and inappropriate sensory information around the mouth.
I did not want to talk over the video because I wanted you to start to use your own assessment of what you were seeing. A video like this probably would have been sent to dad. "Look how cute she is. We tried eating today." The alert state of this baby is almost nonexistent, and it does not take any training to recognize this is not the optimal time for somebody to practice learning to feed. We would not walk into an adult patient room, see them with their eyes cracked like this, and say, all right, "Time to get up and shower." Again, it does not matter whether babies are awake or asleep, or drowsy or crying. We are just focused on the agenda of getting this child fed versus watching the baby's cues.
Video 6
If you look quickly, you can see a shutdown. This baby is receiving too much sensory stimulation to the mouth and closes her eyes. Again, you can see that this baby does not breathe well on her own. I think it is very interesting that we chose to feed a baby that cannot independently breathe, but we expect them to manage suck-swallow-breathe independently.
Video 7
Right here you can see a gaze aversion probably three degrees to the right. It is not a lot of movement and not very obvious, but it is 100% telling of what that baby is experiencing. This is why it is so critical for parents and staff to understand everything a baby is communicating matters. I think at the end of this video she fully closes her eyes and goes into neurological shutdown. She is already white, does not breathe well, and then she gaze averts to try to manage the amount of stress that her little body is under during this experience. No mother would intentionally do this to their baby if they understood the consequences. We want to nurture our children even when we do not understand this entire NICU experience and what it means for our babies. We are doing parents and babies a disservice when we do not educate the parents, first and foremost, above anybody else. They are the ones who are going to have these babies for the rest of their life and deal with the long-term outcomes. Carrie and I treat preemies in the NICU, and then we treat them for followup from what they experienced in the NICU. We have literally seen it come full circle. What is happening in the NICUs is making a huge difference in the outcomes of these babies.
Video 8
You can see in this clip that all that matters is that she eats that bottle. Mom probably has no clue about the sucking reflex and is going to jam the bottle back in until the baby starts sucking. And, it only affirms in her mind that it is ok to feed her baby as eventually, the baby will start sucking.
Video 9
This is a mother feeding for the first time. His primary nurse is there observing and the dad is there. We are going to watch this through and then we will go back and look at a couple of little things.
The first thing we notice is that the baby is very red. This is not a great time to practice feeding, but we are going for it. The second thing we see is that there is a leaking nipple. The myth of the leaking nipple is pervasive in NICU feeding. Some say that it is okay for some milk to leak out around the mouth. I am here to tell you that it is NEVER okay for a baby to leak milk. We do not leak fluid out of our mouths as adults, and we should not do this as an infant. This matters in terms of oral development. The first issue that does not get identified is that this nipple is likely too fast of flow for the baby to manage. We are going to look at that more when we get into strategies. But, we have to be looking at these things ahead of time before they cause a problem. He very clearly is saying something is not right. After the color, the second thing we notice is the frown on his forehead which is a motor stress cue. Then, you see the widening eyes. We go from a frown to widening eyes and frown to widening eyes. He is experiencing motor stress, and he is panicking, but the caregiver and his parents are not recognizing that at the moment.
Video 10
A couple of things I want to point out. Babies need warm milk. You should never feed a baby, especially a baby learning to eat, a room-temperature bottle. Room temperature in the hospital is more or less 65 degrees, and that is cold. This is not a normal sensory experience for a baby. We have to warm the milk up ahead of time even if it adds to our caseload. The baby chokes, and we had all the cues to prevent it. This baby experiences feeding as a drowning experience.
Video 11
There you go. His nurse says, "That's just him being a preemie." This tells you the pervasiveness that this is allowed to continue onward because we do not recognize what is happening at the moment.
Video 12

This was not a successful feed.
Scheduling
Now, we are going to talk about scheduling and then strategies. We do not eat when we are asleep. And, a baby that is woken to eat has their safety at risk with every swallow and increases the chance of oral aversion and negative feeding experiences.

Figure 4. Levels of alertness and readiness to eat.
We have talked about this before in the first developmental care model, but when we are sleeping and then woken up out of that sleep to try something new or something we are not good at, that is not how normal human behavior gets organized well. We would never pull somebody out of deep sleep and then ask them to go skiing. It just does not work like that. We already know that as adults because we do not make that demand on ourselves. When we want to learn something, we are interested in it and we are set up to receive the learning experience because of our interest in it. This is no different for a baby. They very clearly show you when they are ready to eat and when they are not.
The hospital setting totally disregards infant sleep. It is getting better, but most developmental care practices in the hospital are at least 15 to 20 years behind our modern neuroscience and what it knows about the human brain. Infant sleep in the NICU for that early brain is so critical. Sleep is going to mediate a lot of the sensory experiences that are on overload for a preemie. Thus, waking to feed a baby is never correct, but this happens all the time.
Is this baby ready to practice eating? In Figure 5, we see a baby in an active alert state looking at their caregiver.

Figure 5. Baby in active alert and sucking on hands.
Video 13
The earlier picture (Figure 5) is a baby sucking on their hands, in active alert, and looking at their caregiver. This video shows two babies. The first baby shown is the next level down of being ready to eat. It is definitely worth trying to feed this baby because they are alert, rustling, smacking, and kind of playing and bringing their hands to their mouth.
The next baby (Video 14) is getting a diaper change. Unfortunately, clustered care, which has been studied and does have some benefits, has to be weighed with following an infant's behavioral cues. Clustered care can be a massive amount of overstimulation. For example, we decide to change their diaper, dress them, and then feed them all at once. We are trying to "cluster" everything in, but a baby might not tolerate that well. I think this needs to be looked back at again in terms of infant cues. Like I said, most of the research that hospitals go off of is from the late 80s to 90s in terms of the developmental care practices.
Video 14
You are going to see a baby that is in a neurological shutdown. They cannot handle the amount of stimulation that is happening with the fluorescent overhead, the beeping alarms, the people talking around them, the sensations of the wires, and the diaper change. They are very clearly in a hypotonic state, which is that flopping of the musculature. Unfortunately, these are the babies that will then get picked up, swaddled to kind of give them some motor support, and then fed. Then, they have poor feeding experiences because we just cannot recognize what they are already telling us.

You can see a slight stiffening of the baby's feet into the air. It is very subtle. It happens quickly, but all these things are stress signs that are just underrecognized and compounding the problem. I feel stressed when I go see that. It bothers me to my core mainly because I work with these babies and I know it is not hard to do it the correct way. We have so much more success when we do it the correct way. And, we are causing problems that parents deal with for lifetimes. I also experience it on a very emotional level because I am a mother. It is hard to watch these babies go through these types of stressful experiences when all it takes is just a little more information. Infant feeding is my soapbox. Caregiving techniques can help improve the feeding experience.
Caregiver Techniques
We are now going to review the caregiver techniques. Think about the times that you have fed an infant where you could have used a technique differently or when you provided a technique, and it significantly improved their performance. Those are not accidents. Those are us using our own observation skills and becoming collectively better at what we are doing when we help a baby learn to eat.
Technique: Side-lying
- Indications: Infants with difficulty controlling the flow
- Symptoms: Eyebrows raising, big eyes, pulling back, milk leaking laterally, apnea, desaturation, choking, gulping or nasal flaring
- Rationale: Positioning the infant to the side allows the bolus to fall to the side, versus in the back of the infant's pharynx (which happens with traditional supine position).
- Semi-upright sidelying helps facilitate coordination of SSB pattern with preterm infants.
- Implement: Be sure to support the infant's head and trunk in the midline without too much pressure on the back of the head
This position is indicated for every baby. I really do not know why we even feed a baby upright. If you have ever laid in the bed and tried to drink a water bottle, it is very uncomfortable. The reason we do a side-lying position is that it is the exact same position that a baby would naturally nurse in. They are 100% on their side. Bottle feeding should also be on their side. This is going to prevent choking from happening because the extra fluid that is coming out of the bottle can run out of the lower cheek if need be. We know that this is good for all babies that have difficulty controlling the flow which is basically all babies in the NICU. Remember we can tell when the baby is having issues with these types of signs: eyebrows raising, big eyes, pulling back, milk leaking, apneas, desats, choking, gulping, or nasal flaring. Positioning the baby on the side allows the bolus to fall to the side versus the back of the infant's pharynx. This should be common sense. And, if we are positioning the bottle over the baby's throat, this is going to happen. The semi-upright side-lying helps facilitate the coordination of suck-swallow-breathe patterns simply because you have better control and a view of what the baby is actually doing in front of you. Be sure to support the infant's head, trunk, and midline without too much pressure on the back of the head. Video 15 demonstrates this method.
Video 15
Technique: External Pacing
- Tip bottle downward/break the seal at the breast to remove or decrease the flow of liquid to facilitate SSB pattern
- Indications: Infants with poor coordination of SSB pattern or who have a respiratory compromise for any reason
- Symptoms: Eyebrows raising, big eyes, pulling back, milk leaking laterally, apnea, desaturation, choking, gulping or nasal flaring
- Rationale: Tipping the bottle down allows the infant to swallow the liquid so he can take a breath. This allows the infant to drive the feeding, helping him to get into a rhythm of sucking, swallowing, and breathing,
- Caution: Do no pull out the nipple each time you pace, as this is not Infant-driven, but caregiver driven
Another technique is external pacing and this is when we tip the bottle downward or break the seal at the breast to remove or decrease the flow of liquid. This can help them catch up from breathing or even prevent a breathing issue. Infants with poor coordination of suck-swallow-breathe or respiratory compromise of any kind can benefit from this technique. Any baby with a nasal cannula is not going to be able to suck-swallow-breathe properly. Anytime you see it, you do not even have to question it. External pacing is going to be your first line of defense for helping them. Again, stress signals are the same. The rationale behind external pacing is that when we tip the bottle down, it allows the infant to swallow the liquid so he can breathe, and this allows the infant to drive the feeding. This helps them get into a rhythm of suck-swallow-breathe. However, do not pull the nipple out each time you pace as this is not infant driven but caregiver driven. We are going to look at this in video 16.
Video 16

With external pacing, you are counting the respirations. Most immature babies, who are just learning to eat, do three to five breaths before they will try to breathe. Then, as they get to be more mature, they will get up to eight to 10 sucks before they take a breath. The problem then is the baby that does not realize to take a breath at the right time. You can actually count off three to five sucks and then bend the nipple to teach them that you can take a breath now. This is opposed to inadvertently keeping that swallow reflex firing where they are nonstop sucking and then get behind.
Technique: Specialty Nipple
- A nipple other than standard for a specific purpose (i.e. nipple shield, slow flow, Haberman)
- Indications: Infants who will be breastfed infants who are unable to handle the flow provided. Infants with a small chin. Infants with a poor lip seal.
- Symptoms: Poor latch. Eyebrows raising, big eyes, pulling back, milk leaking out front, apnea, desat, choking, or sucking and not getting anything
- Rationale: Nipple shield allows infants increased oral sensory input to facilitate sucking patterns when breastfeeding. Slow flow nipple reduces the rate to allow for safe and efficient feeding. Dr. Brown's nipple has an oral pattern similar to breastfeeding. Ask parents to bring in.
- Caution: Do not change nipples frequently as this inhibits the infant's ability to develop consistency with their SSB pattern and changes the sensory experience.
Nipples really should not be a "specialty" unless it is a Haberman. I named this category as such as these are nipples other than standard hospital nipples. These have a specific purpose, but they also lump in Nipple Shields, slow flows and Haberman as a specialty as well. This is I think part of where the big separation happens between therapy and nursing feeds. Nurses are not trained to understand what the nipple flow is. Thus, they are going to go with what they know best which is the hospital standard nipple. Then, they have to call in therapists after a baby has had poor feeding experiences and is already starting to wire stress with feeding. So, it really should not be a case of specialty nipple, but rather it should be a case of, "This is the nipple that you use in this X, Y and Z case." The indications for using a different nipple are infants who will be breastfed or who are unable to handle the flow provided of the nipple, infants with a small chin, and infants with a poor lip seal. The symptoms include a poor latch, eyebrows raising, and big eyes. The rationale for a Nipple Shield is that it allows the infant increased oral sensory input to facilitate a sucking pattern when breastfeeding, and it pulls the nipple outward into the shield. I have mixed feelings about the Nipple Shield, but it is successful for some babies to be able to attain breastfeeding, which is primarily far more beneficial for a baby especially a preemie. The slow flow nipple, which should not be a specialty nipple, should be the standard nipple for all babies to start out on. They can then work up to a higher flowing nipple. The slow flow reduces the rate which allows for more safe and efficient feeding. As stated before, Dr. Brown's nipple has an oral pattern similar to breastfeeding. Most hospital NICUs tend to use Dr. Brown. But, if they do not, you can ask parents to bring it in. It is widely available in retail stores. It is also something that a parent can pick up once they leave the hospital as well. Nipples do not really cause "nipple confusion." It is flow confusion. Once a baby does not immediately take to a bottle or a nipple, a parent, nurse, or another staff member will suggest switching. If we are switching equipment every single time, they are not learning. Using the skiing metaphor again, if I had one pair of skis the first day and a second pair of skis the next day and a third pair of skis the next day, I am going to be a basket case. This is the same thing with bottle feeding.
Several factors should be considered when choosing the correct nipple for a particular infant including size, shape and flow rate. And, if you have fed a baby in the last decade, you will likely recognize some of these in Figure 6.

Figure 6. Types of nipples.
The red ones are no longer manufactured. I had to ask our hospital for over a year to take them off the shelf, even though it was everyone's favorite because they are so dangerous for babies. The most critical factor for a nipple is the flow rate. When a baby is eating they have four options (Figure 7).
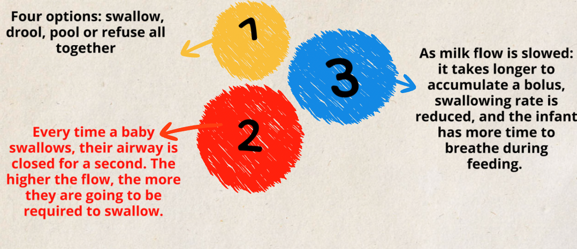
Figure 7. Overview of the importance of flow.
They can swallow, drool, pool or refuse altogether. Every time a baby swallows their airways close for a second. The higher the flow the more they are going to be required to swallow. And as milk flow is slowed, it takes longer to accumulate a bolus, swallowing rate is reduced, and the infant has more time to breathe during a feed.
Technique: Cheek Support
- Indications: Infants with a poor lip seal
- Symptoms: Milk leaking laterally (out of corners of the mouth)
- Rationale: Support is needed to help form lip seal around the nipple to create intraoral suction. Otherwise, it's like drinking out of a straw with a hole in the side--you get some milk, but it's not efficient. The side that is down during sidelying feeding. Cheek support should not be provided if the infant does not have a poor lip seal.
- Caution: Do not provide support on both sides, as this increases volume and the infant could choke and/or develop an oral aversion. If signs of stress are noted with unilateral cheek support discontinue the use of the technique.
You actually see this done very frequently incorrect in the hospital. Most people will squeeze both cheeks together, but you are actually only supposed to turn the baby in side-lying. If they need check support, you would support the cheek that is face down on the pillow or on your leg because that would be the one that gravity is pulling downward, not the one on top. When you squeeze both of the cheeks together you can create a more efficient seal on a bottle; however, we do not want a baby to have a more efficient seal if they are not managing the milk. If the milk starts leaking, we need to check several things: the nipple, flow rate. and then also, how the baby is able to form suction on the bottle. So, do not squeeze both cheeks together because you can send more fluid down their throat and into their lungs.
Technique: Chin Support
- Indications: Infants with poor tongue stripping of the nipple, small chin, or wide jaw excursion
- Symptoms: Smacking noise, increased air intake, inefficient eating (sucking a lot and not getting much)
- Rationale: Infants with small chins with posterior tongues benefit from this slight forward pressure to pull chin forward. Likewise, infants with a wide jaw excursion may require chin support for the initial latch and then let go.
- Caution: Do not push up or use chin support if it is not needed, as this could make the infant orally aversive.
This technique is commonly used in a NICU setting along with the cheeks. You squeeze the cheeks and pull the chin. It is like a double whammy for incorrect feeding. I am going to force the suction of the nipple, and then I am going to pull the chin out so that literally the baby is doing nothing on their own. This is used when a baby is poor tongue stripping and has a small chin or wide jaw. They kind of chomp on the nipple. The symptoms are a smacking noise, increased air intake, inefficient eating, and sucking a lot or not getting much. Infants with small chins and posterior tongues benefit from this slight forward pressure to pull chin forward. Likewise, infants with wide jaw excursions do as well. Babies with genetic issues and low tone may require chin support for the initial latch and then you can let go. Caution, do not push up or use chin support if it is not needed as this could make the infant orally aversive.
Video 17
We are going to look at some of these techniques and also what should not be done.

There is no kind of seal or management of the milk flow. Again, this is such a subtle experience. This baby is probably uncomfortable having this milk all over its face, and that is not a positive experience for their learning to eat. When milk is running out of the mouth, what does that mean? This means a poor lip seal, the flow is too fast, or both. If we sipped our water bottle and it ran out all over our face, we would adjust something. But a baby is relying on us to adjust it for them. They cannot adjust it for themselves.

