Dr. Gardner: Thank everyone for joining me today. I appreciate you taking time out of your busy schedules to listen to this webinar. I have been a physical therapist for many years, and I have focused solely in wound care for the last 15 years. It is my passion, but it is something that most therapists have no desire to be a part of, but I really find it rewarding. I hope that this presentation is of value to you as occupational therapists and occupational therapy assistants.
Introduction
Chronic wounds affect a large amount of people, but it does not get the recognition that other types of comorbidities get. You do not hear "The American Wound Society." You may hear a lot about research that goes toward cancer, diabetes, etc., but you probably do not hear a lot about chronic wounds. There are millions of people living with chronic wounds that are not recognized, and they just try to treat themselves. Approximately 2% of the general population are affected by chronic wounds, and the care to treat these chronic wounds costs more than 50 billion dollars a year.
In a study that Dr. Carolyn Fife and her colleagues did in 2012, they said that this 50 billion dollars is 10 times more than the annual budget of the World Health Organization. That statistic is very striking. Of these chronic wounds, venous and arterial ulcers make up a significant percentage, and that is why we are going to focus on that today. Again in Dr. Fife's study, after analyzing wound center data across the country, she found that approximately 8% of the patients seen in a wound center have venous ulcers. I know in my wound center it is definitely more than 8% with venous ulcers.
Arterial ulcers and non-healing amputations make up about 1.5% of the patients seen in a wound center (Fife et al., 2012). This data is about five years old, and I think if they were to go back and do another analysis they would find even more people with venous ulcers, or wounds complicated by venous insufficiency. First, we are going to look at arterial ulcers, and then we are going to contrast them with venous ulcers a little bit later in the presentation.
Arterial Insufficiency Ulcers
Introduction
Arterial ulcers only make up about 5-10% of all lower extremity ulcers, but the problem is that arterial insufficiency often goes unnoticed or unrecognized because it is asymptomatic. And as such, it causes about 5% of all amputations. Over 80% of people with arterial insufficiency have a history of smoking. So, there is a high correlation with smoking. By getting people to stop smoking, we could hopefully decrease the percentage of arterial insufficiency that we see in the population. It is important to note that other disease processes besides arterial insufficiency can cause ischemia, such as as thromboangiitis, vasculitis, Raynaud's disease, pyoderma gangrenosum, and sickle cell disease.
Arterial System Overview
Let's now go over a quick overview of the arterial system. The arteries carry blood from the heart and take it to the rest of the body. Arteries are made up of three separate layers. There is the external, middle, and inside layers. The external layer is called the externa, or tunica externa, and that is the protective outer layer. The middle layer, the tunica media, is made up of smooth muscle, collagen and elastin fibers. It gives the artery its strength and flexibility. The intimal layer (inside) is a single layer of endothelial cells that are in direct contact with the blood. And as we know, arteries vary in size depending on what they are supplying blood to. The bigger the tissue or the bigger the area, the bigger the artery will be. Smaller arteries are called arterioles. And then, capillaries are the simplest vessel. It is made of only one layer of endothelial cells and a thin basement membrane. They are so tiny that they only allow one red blood cell through it at a time. There are the internal layer, the tunica intima, the tunica media, the middle layer, and then the tunica externa. Again, the protective layer, the middle layer, gives stretch and flexibility to the artery, and then the internal layer is what is in contact with the blood.
The blood comes out of the aorta into the arteries, then into the arterioles, crosses in through the capillaries where it becomes deoxygenated, and then goes into the venules, back into the veins, and then up through the vena cava.
Etiology of Arterial Insufficiency and Related Tissue Damage
Let's consider why arterial insufficiency damages tissue. Arterial insufficiency is the term for a decrease in blood getting to the extremities. Arterial insufficiency is not usually associated with the trunk. However, any artery can become blocked or damaged and cause arterial insufficiency. However, we are typically talking about the extremities when we discuss arterial insufficiency. It is often associated with trauma, an acute embolism, rheumatoid arthritis, and diabetes. This is why a large percentage of our patients that we see in the wound center are diabetic and have some degree of arterial insufficiency. Ischemia can also be seen in other diagnoses.
The most common cause for arterial insufficiency is arteriosclerosis. As we know, atherosclerosis is thickening and hardening of the arteries. This is where the lumen of the artery, for whatever reason, gets encroached upon or gets narrowed. It can be from cholesterol sticking to the vessel walls causing plaques, and as that cholesterol thickens and thickens inside the vessel, it leads to narrowing of the artery. And as you can imagine, if the artery is narrowed, it is harder to get blood to the extremities, and it takes more blood pressure from the heart to pump that blood through with resultant decreased overall blood flow. The cholesterol plaques narrow the diameter of the artery. It is going to be harder for the blood to get pushed through with a lack of blood flow to the extremities. This means a lack of oxygen and nutrition to the extremities.
Peripheral Arterial Disease Sequelae
When looking at arterial insufficiency or peripheral arterial disease, there are phases of the disease. The first step that patients might recognize is intermittent claudication (pain and cramping). and then it progresses to nocturnal pain. The next is pain at rest, and finally ulceration and gangrene. Now, we will talk about each of these steps.
Intermittent claudication. Intermittent claudication is activity dependent. This is when the patient comes to the doctor and says, "I can only walk about two blocks and then I start getting this cramping sensation in my calf or in my thigh. I have to sit down and then I can walk another couple blocks, but then the pain comes back again." These are classic signs and symptoms of intermittent claudication. And as I mentioned, usually the pain is in the calf. However, depending wherever the occlusion or the blockage is occurring, that is where the patient will complain of pain. If the blockage is higher up in the artery, they may complain of pain in the buttock or the thigh. The degree of ischemia really depends on what leg muscles are affected by the narrowing of the artery (Figure 1).
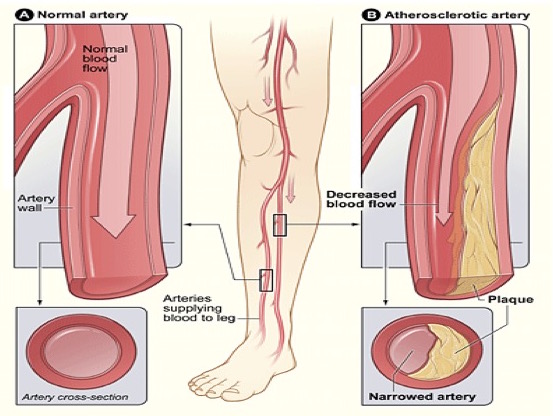
Figure 1. Example of intermittent claudication.
As you can see in Figure 1, it is much harder to get blood flow down to the extremity in the narrowed artery. There is also an example of a patient grabbing his calf after he has walked a couple of blocks.
This is a video that I recommend you take a look at on your own time. It is called Intermittent Claudication An Important Leg Symptom Not to be Ignored (https://www.youtube.com/watch?v=1FgJpvMoOKU). It gives a good overview on intermittent claudication and some of the signs and symptoms that we need to know. A client might casually mention some of these during their treatment session, but you need to be able to realize that this is a sign of a bigger problem. After the patient starts to experience intermittent claudication they might just blow it off. They do not talk to the doctor about it, or they do not think it is really that big of a deal. They can control it, per say, by taking a rest. It progresses from the intermittent claudication to ischemic rest pain.
Ischmic Rest Pain-Nocturnal and Rest. This is where patients begin to have pain in their calf or thigh even if they are not walking. They may think this pain might be attributed to a back injury or sciatica. They might go through the whole gamut of CAT scans, MRIs, et cetera of their back and find that there is really nothing wrong with their back. This is when it is time to consider that they have some arterial insufficiency going on. Many times clients will say that the pain gets better when they dangle their leg over the side of the bed. They also say it hurts more when their leg is elevated.
There are two types of ischemic rest pain. One is nocturnal and one is rest pain. Nocturnal pain is when they only feel the pain at night. It is a form of ischemic neuritis, and they feel it at night because when we go to sleep the blood flow to the extremities slows down. The body continues to pump a lot of blood to the core organs to keep them going, but the blood flow slows to the extremities. In someone with arterial insufficiency that already have issues with getting blood flow to the extremities, this slowing down of blood flow at night causes pain. They will usually say the pain is in the toes or at the base of the metatarsals, in the arch. They can relieve it with standing, dangling their feet over the edge, and occasionally with a little bit of walking to help get that blood flow to the extremities. As the disease progresses, they go from simple nocturnal pain, or pain that only comes at night, to rest pain. It will be worse at night and usually will require narcotics to treat the pain. It is a sign that their arterial insufficiency is worsening. Again, the pain is decreased by lowering the extremity, and increased by heat, elevation, and exercise. When they get to this phase where they have rest pain, there are usually at least two significant arterial occlusions happening. If a patient is complaining of rest pain, they get an Ankle Brachial Index Test (ABI) done, and typically, they will have less than 0.5 millimeters of mercury.
Ulceration. When arterial disease progresses the furthest down the line, that is when ulcerations occur. This is when the demand for blood exceeds the amount that the body is able to supply. You will generally see these wounds on the distal portions of the foot, the toe, and maybe the heel. They can be very painful. Many patients will have ill-fitting shoes, a pressure issue from lying on a body part and cutting off the circulation, or shearing, where the internal tissue and the external tissue are moving in opposite directions. Typically, arterial ulcers do not bleed as there is not a whole lot of blood flow to the area, and they will have necrosis or dead tissue in the wound. If we are doing everything to treat a musculoskeletal issue and the pain is still not getting better, that is when I would recommend that they get a vascular workup.
As part of ulceration, the patient may experience gangrene, either dry or wet (see Figure 2).

Figure 2. Dry vs. wet gangrene.
Dry gangrene is what is normally seen with arterial insufficiency. This is not as urgent as wet gangrene would be because it has a slower progression. The extremity is going to be cold, and the tissue will start to contract or shrivel up as compared to another toe or the opposite foot. With wet gangrene, there is some type of infection going on. This is an urgent medical diagnosis, and they need to get to the hospital and have surgery right away. Wet gangrene is frequently seen in diabetics, and it advances very quickly.
With dry gangrene, you might see an autoamputation, where the toe or the toes might just fall off if they do not have surgery to amputate. However, with wet gangrene, they really need to get diagnostics done right away, like a CAT scan or an MRI, to see if there is gas in there and how far the damage goes. Or they need to go right to the operating room and have the surgeon get in there and get rid of all the necrotic gangrenous tissue.
Risk Factors
What are some risk factors that contribute to arterial insufficiency? What are some things that we can modify or we can educate our patients on to help prevent arterial insufficiency from ever occurring or decreasing the harm that the arterial insufficiency will cause. A couple of the risk factors can be modified. One of them is hyperlipidemia or hypercholesterolemia. If we can get the patient to eat better and on the right medications, then hopefully we can lower their cholesterol levels and decrease the amount of plaque being deposited in the blood vessels. A lot of times however, it is not a diet-related diagnosis. Hyperlipidemia has a high familial tendency. Even though a patient might exercise, eat cleanly, and do everything right, if they have a family history of high cholesterol, then they are more prone to high cholesterol. They need to keep an eye on it and take the correct medications.
The number one modifiable risk factor we have already mentioned is smoking. Smoking is a huge contributor to arterial insufficiency. It causes vasoconstriction, which obviously decreases the amount of blood flow that gets to the area, and decreases tissue perfusion. It decreases the amount of oxygen available. Smoking will also increase the rate of clot formation because it thickens the blood. And then, if the patient also has hyperlipidemia, then smoking is going to increase the effect of that hyperlipidemia. So, if we can get patients to stop smoking, this should help with their arterial insufficiency.
Hypertension is another modifiable risk factor. If we again can get them to eat correctly, exercise, and get them on the right medications, then we can decrease the pressure of the blood flow, and therefore not damage the delicate endothelial cells inside the artery. Trauma is another common cause of arterial ulcers in younger individuals. If there is a car accident or a fall, and the artery is damaged, this can lead to an arterial ulcer. A risk factor that we cannot modify, unfortunately, is advanced age. They are less able to adapt to the changes in oxygen demand and may have an arterial ulcer even if their arterial insufficiency is not as great as in other individuals.
