Introduction
- We will be learning about various expressive arts techniques to supplement and enrich your OT treatment sessions.
- Many of these techniques have been developed, researched, and enhanced by professionals from other valuable disciplines. These individuals are remarkable members of the treatment team and are the experts in these fields.
- If your patient enjoys a type of expressive art in treatment and may benefit from more in-depth expertise utilizing the technique, please strongly consider referring your patient to one of these certified professionals: Art Therapist, Dance and Movement Therapist, or Music Therapist.
- Contact and relevant referral information for each discipline will be provided at the end of this presentation.
We are going to be talking about expressive arts in occupational therapy and getting back to our roots as a profession to use creative ways to help get our patients to their next functional goals. Before we begin, I just have a little bit of a disclaimer that I would like to say. We will be learning a lot about different expressive art modalities and interventions that were created and heavily researched by other disciplines of the healthcare team. If you have a patient who enjoys the type of expressive art that you are using and you feel they would benefit from further expertise using that specific modality, I would highly recommend you consider referring out to other disciplines such as art therapists, dance movement therapists, music therapists, and drama therapists, who are the experts in these techniques and would be great to continue to work with your patients. I will have contact information for each of these disciplines at the end of this presentation.
- Every child is an artist. The problem is how to remain an artist when we grow up.
Pablo Picasso
I wanted to start with this quote from Pablo Picasso. If you decide to use any of these expressive art interventions you will probably run into a lot of intimidation. Patients verbalize that, "they are not artists," "they cannot draw," "they draw stick figures," and "they cannot even draw a straight line." What is important to remember is it is not about the product, but rather it is about the process. It is the creative process, the growth, and the self-discovery that happens during that process. Like Pablo Picasso said, "Every child is an artist. The problem is how to remain an artist when we grow up." Reassure your patients that we all have it in us to be creative, and it is just a matter of reaching into that inner child and using that in today's rehab world.
What is Expressive Art?
- "Expressive Art is a process by which various art modalities are used as a catalyst for creative expression to enhance personal growth, awareness, and healing." (13)
- Examples include:
- Visual arts i.e. painting, drawing, sculpting
- Drama and storytelling
- Dance and movement
- Writing
- Music
What is expressive art? This is a direct quote from one of the research articles referenced in the works cited page at the end of this presentation. "Expressive art is a process by which various art modalities are used as a catalyst for creative expression to enhance personal growth, awareness, and healing." Examples of these modalities are the visual arts, and this is not an exhaustive list, but it is painting, drawing, sculpting, photographies, scrapbooking crafts, and things like that. There are also drama and storytelling, dance and movement, writing, and music.
We are going to talk about each one separately and the supporting evidence behind each one, and then we will go into the different intervention and treatment ideas that you could use.
Fine Art Vs. Expressive Art
- Fine art- The focus is on the piece of art that is created.
Expressive art- The focus is on experiencing growth and self-discovery through the creative process.
To kind of touch upon what I said before is that fine art is very different than expressive art (see Figure 1).
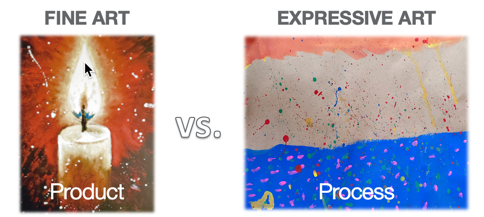
Figure 1. Examples of fine art vs. expressive art.
Many times when we bring up these creative processes in rehab, patients will scoff at it saying that they think it is all about fine art. What does the product look like in the end? How good is the art? In reality, it is all about the process. Please continue to talk about that with your patients so that they can feel comfortable using these modalities. The focus again is on experiencing growth and self-discovery.
Visual Arts
Let's start with the visual arts. This is not an exhaustive list, but these are the most common ones used. I will give a brief description of each one, and then I will go into the supporting evidence for each one.
- Painting
- Drawing
- Clay Sculpting
- Pottery
- Photography
- Printmaking
- Crafts
- Scrapbooking
For visual arts, there is painting, drawing, sculpting, pottery, photography, printmaking, crafts, and scrapbooking.
Supporting Evidence: Visual Arts
- Increase sensory input
- Activate areas of the brain that lead to motor development in children
- Improve patients’ sense of self, hope for recovery, self-esteem, and perception of control over their situation
Research supports visual arts as a means to increase sensory input. What we find is various receptors are engaged in the fingers and hands, and we know as OTs that this is where there nerve endings and receptors.

Figure 2. This is an example of visual arts providing sensory input.
The nerve impulses in these receptors transmit to the cerebral cortex, and this helps to enrich the sensory experience. It lights up a lot more areas of the brain to make those neuro connections much stronger. And in children, these areas can lead to motor development. It also helps to improve the patient's sense of self, hope for recovery, self-esteem, and perception of control over their situation. I think these are big factors, especially for your patients. I know in my practice I have seen a lot of patients get completely unmotivated and depressed with their current situation. They say that life is totally different, and they are not themselves anymore. They lose hope and feel out of control because of this big event that happened to them. This could be a stroke, a car accident, or something else outside of their control. It is pretty cool that visual arts can help them feel hopeful again.
- Improve perceptual skills
- Improve global cognitive function
- Help to prevent cognitive decline and dementia
Furthermore, it can help to improve perceptual skills. When you look at drawings and paintings, there is a lot of contrast in the colors and the shades, the foreground, and the background. This can help someone improve their perceptual skills that may have been either damaged in a stroke or were never developed as a child. There can also be improvements in global cognitive function, especially in individuals with dementia. Additionally, many interventions have used visual arts to prevent cognitive decline, which is a pretty big area for dementia as well. As we all know, dementia is a degenerative disease so anything that prevents the actual decline is pretty big. It also can help with working memory, attention, and executive function.

Figure 3. Examples of visual art projects.
I want to call your attention to the top picture that says hold on and let go. This is a pretty successful intervention to supplement OT practices with any child or adult that seems to be struggling psychologically. They trace their hands and on the left and draw or write out things about their life that they want to hold on to. On the right, they draw and write things that they want to let go of. It is a good visual representation of what they want to keep working towards in life and what is okay to let go. It can also be used to discuss their feelings if they are comfortable.
Drama and Storytelling
- Projective play
- Purposeful improvisation
- Performance
- Scripting
- Role-playing
- Multi-sensory storytelling
- Puppetry
- Rituals
Projective play is just a type of play therapy. It is most appropriate for the pediatric population. This is when the child is using a doll or a puppet and taking them through a situation and expressing how this doll or puppet feels. A lot of times kids will do that when they are actually talking about themselves, but it provides a comfortable atmosphere for them to express how they are feeling.
Purposeful improvisation is when you act out a potential situation, and you have the patient behave in a way that they would ultimately want to behave in. An example of that is if you are working with a child with autism and you have them act out the situation of approaching a lunch table full of middle school friends and asking to sit there. This lets them practice how they want to act in that situation.
Performance is used a lot in nursing homes. This is just strictly theater or drama. You have a script, a dialog, and you perform a short play or a musical. People have found a lot of success in terms of psychological well-being, with nursing home residents especially.
Scripting is used a lot by speech-language pathologists. This is the repeated practice of words, phrases, and sentences embedded in a monologue. A monologue of a popular play or musical that the patient likes. This could even be a song. This is used to help treat aphasia a lot of times. You can also combine this with a song, and we will talk about this later. That is a multimodal approach. This is a script that you develop with the patient, and ideally, you have the patient create it as much as possible. They can describe the words that they would like, but again if they have aphasia, this can be difficult. You can have them practice asking someone how their day is or practice talking about their illness, and then, you can build onto each phrase. For example, "I had a stroke." They practice that repeatedly and then they say, "I had a stroke six months ago." "I had a stroke six months ago and it impacted me ______." You keep building on the phrases that you have already developed with the patient.
Role-playing is a good one where the therapist acts as someone and the patient does as well. You present a situation to the patient, like kitchen safety, to determine if the patient is likely to return home. You present them with a situation in the kitchen and you see how the patient responds. You can then talk about what happened in that situation so that the patient can start to recognize patterns of behavior and maybe things that they missed or need to work on. According to research, whenever a person is able to identify their own limitations, it helps to create much stronger bonds and self-awareness to address situations in the future.
Multisensory storytelling involves multisensory techniques. This is done typically in the memory care unit, where you are trying to stimulate every sense that you possibly can to help them to interact with their environment. I will talk more about this a little later.
Puppetry is where you use puppets. We have also used things called social robots, specifically a company called Pure Robots, where you use either a robot or a puppet with children with autism or with the elderly population. Basically, it just provides a much less intimidating entity for that person to communicate with. It helps to aid in communication, and we have seen some generalization into actual human interaction, which is pretty cool.
Lastly, we have rituals. This is an enactment of a myth or an old story of oneself. That can help to ease the transition from rehab to home. For example, you can have them talk about an old belief system that maybe they do not feel safe. They do not think that they will be able to do it. You then talk through what that belief is and point out why they would in fact be able to go home and be safe doing it.
Supporting Evidence: Drama and Storytelling
- Improvements in self-worth, overcoming self-imposed limitations, and in self-advocacy
- Props are less antagonistic and threatening and can aid in communication
- Multi-sensory storytelling can be used to improve retention and recall for individuals with intellectual disabilities
Some supporting research evidence of drama and storytelling in the therapy world is that they have seen improvements in self-worth, overcoming limitations, and improvements in self-advocacy. Again, this is huge. We talked about those benefits before, but this is big for a patient to take ownership of themselves and be confident in their recovery. Like I mentioned before, props are seen as less antagonistic and threatening. It can help to aid in communication. We have seen this mostly with kids with autism who are largely nonverbal.
Multisensory storytelling is also supported in the literature, especially with individuals with developmental and intellectual disabilities. When they are trying to learn new information, this can be a very difficult task for someone with an intellectual disability. However, whenever you engage as many senses as possible, a person tends to retain and be able to recall it much later. For instance, if you are teaching somebody, a child, or an adult of any age, how to be safe taking a shower, if you do not have an actual bathroom or shower to do it, you could break it up into steps. You could have them test out cold and hot water reinforcing the appropriate temperature. You could have them hold the soap to their nose to smell it as you are describing the situation. You can have them plant their feet on the ground to feel that proprioceptive input of what the bottom of the tub might feel like. And as you are engaging their senses this way, you can talk through this safe scenario for showering. This technique was developed by a company called Fine Art Miracles in Pittsburgh that I have worked with specifically in memory care units. We are engaging their senses in every way possible. We have had family members come up to us and say this is miraculous. "They have not been awake like this or interacting like this in so long. This is great." In this picture (see Figure 4), this shows a woman engaging in one of these multisensory sessions.
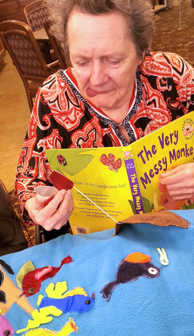
Figure 4. Example of a multisensory session.
She has a sensory mat with all kinds of different textures (felt and rough) that she can feel as she is reading through a story. Thus, she is being stimulated in a lot of different ways.
Drama Programs with the Elderly Population
- Provide a sense of mastery and connection with others
- Reinforce positive coping strategies
- Increase memory recall
- Improve sense of vitality and regulated, relaxed breathing
Here is some further evidence for drama programs with the elderly population specifically is it provides a sense of mastery and connection with others. These people learn new skills, and they are proud of themselves. This video demonstrates this.
Video 1.

This gentleman is singing a song from a musical that he learned, and he is quite proud of himself. He had a great time, and he was then able to talk to others about his performance. This gave him something else to talk about which was great for him, his caregivers, and his friendships. This has been shown to reinforce positive coping strategies. Residents in nursing homes, when they engage in these plays and musicals, tend to embody the character. The character might meet with some adversity in the plotline, and the character gets through it. This might generalize to their own situation. It also helps to improve memory recall because they are learning lines, however simple. They can see that they learned something, and as such, they have an improved sense of vitality and regulated, relaxed breathing, which was also an interesting side effect of this.
Dance and Movement
- Travel
- Mirror
- Mirroring
- Life’s journey
- Simon says
- Movement metaphors
Next, we have dance and movement. There is something called travel that is used quite frequently. That is where the therapist prompts the patient to move across the room in a certain way. For instance, you might say, "Move across the room as if you feel good about yourself.". "Okay, now move across the room as if you feel good about your physical health." "Now move across the room as if you are excited and feel safe going home." Or, you could say "Move across the room as if you are stressed out or scared about something." This provides another way for self-expression that a patient may have not been able to do. You can tell a lot by how someone moves, especially in relation to a prompt. The act of moving itself can be both therapeutic and physiologically strengthening, which is great.
The technique is using a mirror. You would place a patient in front of a mirror and use similar prompts as the technique of travel. "Move as if you are excited to be here." "Move as if you have a good support system at home." You could also change it into more of a neurophysical framework or rehabilitative framework by saying, "Sit in the midline and move your right arm." You could also show them something like a PNF pattern. It is good to give them that mirror feedback for many reasons.
Mirroring is used when the therapist does a movement and the patient is facing them and has to mimic the movement or vice-versa. The therapist does whatever movement the patient is doing. I will get into why this is beneficial a little bit later.
Next, we have life's journey. This is where the therapist prompts the patient to do a series of movements that represent their life from birth to where they want to see themselves in the future. You might prompt them to do a movement that represents what it was like when they were three-years-old or a teenager. Or, "What it would feel like if you had everything you wanted in the future?"
Simon Says is good to work on inhibition, command following, and attention. We have all probably played that as a kid. It is just as you would expect it to be. You are prompting the patient to only move and do what the prompt is. This is more appropriate for kids, but there are some adults that enjoy that too. You have to use your clinical judgment to see who is appropriate for that and who is not. It is good for one-step command following as well.
And lastly, we have what is called movement metaphors. This is where a patient uses a prop or a metaphor to help them demonstrate achievement or a challenge that they might be experiencing at that current time. They may grab a stuffed animal and say this represents how comfortable now with my situation.
Supporting Evidence: Dance and Movement
- Improves strength, balance, and proprioception with kinesthetic activity
- Reduces depressive symptoms
- Slows cognitive decline
- Activates motor neurological brain regions to improve muscle memory
- Reduces fall risk
- Stimulates communicative capacities through shared experiences in dance
Dance and movement improve strength, balance, and proprioception with all of that kinesthetic activity. There is a lot of benefit from moving around like that, especially with some rhythm. Video 2 demonstrates this.
Video 2.

It has also been shown to reduce depressive symptoms, slow cognitive decline, and activate motor neurological brain regions to improve muscle memory. This can be important especially with individuals after a brain injury or stroke. It can help reduce fall risk because that person is challenging their balance and working on their core and proprioception. It can also stimulate communicative capabilities through shared experiences in dance. If you are doing a group session, and a lot of these expressive art interventions are most beneficial in groups, it can help to stimulate some social interaction.
Expressive Writing
- Letters
- Phrases or mantras
- Journaling
- Poetry
- Timed writing
- Prompts
Expressive writing can include letters, phrases, or mantras. A phrase could be like carpe diem or seize the day. It could be their mantra throughout the day. Journaling, poetry, timed writing, and prompts are other examples. Obviously, expressive writing can have a lot of psychological and physical benefits. There are also some cognitive benefits that we will talk a little bit about that later.
Supporting Evidence: Expressive Writing
- Provides inspiration and “ego-support”
- Shown to improve immune function
- Reduces intrusive and negative thinking
- Improves working memory capacity
Some of the supporting evidence for expressive writing is that it provides inspiration and ego support. This is especially true in the group setting that I talked about. The group members may become inspired by one another. They may receive positive feedback on having engaged in the task and having opened up and been vulnerable with their peers. This next one is incredibly interesting in my opinion. Expressive writing was also shown to improve immune function. This seems to be directly correlated with the fact that it also reduces intrusive and negative thinking and depression and anxiety. Anxiety and depression can decrease immune function and this can cause people to get sick more. There were some key inflammatory biomarkers that researchers saw in the blood work of people who engaged in expressive writing. And another cool part of that was that the effects lasted for a couple of months afterward. It also helps to improve working memory capacity, which is always important especially working with clients with neurological issues. Remembering what the prompt was can help with sequencing. Creative writing also can be used for reminiscence.
Music and Singing
- Songwriting
- Playing instruments
- Drumming
- Melodic Intonation
- Music reminiscence
- Singalong
- Music stimulation
- Lyric discussion
There are different types of music and singing we can use. Songwriting is exactly what it sounds like. You just write some songs and lyrics with a person. This is especially beneficial for somebody who tends to be more of the artsy type. They might have expressive aphasia that this can help. It also can a way for both the therapist and the patient to bond with each other.
There is also a type of music and singing therapy that involves playing instruments. That is very good for a lot of different things, even physically. If you think about the dexterity it takes and the bimanual operation using both arms to play an instrument, this is a very complex task. They also have to follow the rhythm, and perhaps join in with other instruments.
There is also something called drumming. This is performed in a group setting, and each person has their own little drum. This is used for communication. When someone does not feel comfortable verbalizing something, or maybe they are not able to, drumming can be used. For instance, you start with one person, they tap out a beat, and whomever they are looking at has to respond with their own tapping and beating of the drum. This a musical dialog between the two of them to help them to feel connected and that they are being heard. This continues throughout the group.
Melodic intonation means singing. We are going to discuss this shortly.
The next type is music reminiscence. This is when you listen to familiar songs with the patient, and you reminisce about what the song meant to them, who comes up in their memory, what time of life was this around, and how it made them feel. Whenever we hear certain songs, we can be transported back into memories. It can be therapeutic. It can also be difficult if it drudges up some things that might not be enjoyable to think about. For instance, you could have a patient that was listening to a certain song when they crashed their car, which landed them in rehab. This can be therapeutic to reframe what that song actually means to them if you want to discuss which song was playing.
You can have a singalong. This is great for anyone with aphasia. There are times that people with non-fluent expressive aphasia can still sing familiar songs, but they cannot verbalize spontaneously. I have seen that a lot with my patients, which I always find intriguing. It can provide hope for these patients. It can also create connections between the patient and the therapist and the whole group.
Next, we have something called music stimulation. This is when you use songs, rhymes, and chants and have the patient fill in the blanks. You use a familiar song or a familiar lyric that is meaningful to the patient. This is for someone with aphasia or limited verbalizations. "Twinkle twinkle little, ____," is an example. You keep building up their store of words that they can produce.
The last one is a lyric discussion. You take a meaningful lyric and have them choose to the best of their capabilities to discuss it in a way that helps them express something about themselves. This helps you to get to know them better. If they are not able to verbalize these things to you, then perhaps this intervention is not appropriate. However, you might be able to combine it with another medium for a multimodal approach. For example, you could have that song playing and have them paint their response to it.
Supporting Evidence: Music and Singing
- Increase neuroplasticity
- Enhance alertness, leading to improved attention and memory
- Decrease depressive symptoms and improve motivation
- Activate multiple parts of the brain, fostering dendritic sprouting and synaptic plasticity
Music and singing have been shown to increase neuroplasticity. It enhances alertness leading to improved attention and memory. It also creates changes in the temporal region that process sound and this has been shown to decrease depression. On functional MRIs and different studies that have used music, it has been shown to improve motivation as well. And when motivation is improved, depression is usually decreased and vice-versa. It also activates multiple parts of the brain fostering dendritic sprouting and synaptic plasticity, which is just a fancy way of saying it strengthens the neuro connections in the brain.
There is also something called musical improv and that is when someone creates a musical performance or they just perform musically, impromptu, or immediately after hearing a musical prompt. You might play a meaningful song and then prompt them to continue with any type of singing or dancing that they want to with that. This has also been shown to activate multiple parts of the brain as well because there is a level of creativity as they are not overthinking it. Here is an example in Video 3.
Video 3.

This elderly woman is singing one of her favorite songs, and it is very meaningful. She gets a little bit emotional in the end. This is also one of the major strengths of music and singing because when there can be an emotional connection. She also normally does not stand up for that long. When we were working on standing tolerance and balance, she engaged in singing a meaningful song which helped distract her from the fact that she was standing for a lot longer than she normally does, which was another fun way to combine physical rehab with expressive arts.
Clinical Utilization: How to Use Expressive Art in Your OT Practice
Now, we are going to get into the clinical utilization of a lot of these techniques. I think it is very important that you guys feel comfortable being able to use some of this in your practice.
Visual Arts: Indications and Interventions
Clay Sculpting.
- Targeted Skills
- Attention
- Grip strength
- Dexterity
- Emotional regulation
- Activity idea:
- “Create your favorite animal.”
- Use with the pediatric population to work on attention to a task
- Discussion after task, especially beneficial in a group setting
Some targeted skills that you might want to think about when you are using clay are attention, grip strength, dexterity, and emotional regulation. Grip strength and dexterity are obviously the physical benefits to this, but there are also a lot of cognitive and psychological benefits to this as well. I have used this with children before who need to work on attention to a task. I might prompt them by saying, "Create your favorite animal." Often, they will attend for longer than they have ever attended to an activity. First, it takes some hard loading work to mold that clay and use it. They are using physical force. They are also excited to dive in and get their fingers on something that feels kind of cool and squishy. They want to attend to create that animal. Afterward, you discuss that either in a group or individually by asking the child, "Describe to me what you just built here. What does that represent?" Or, "What kind of animal is that? Have you ever seen one?"
Painting.
- Targeted Skills
- Visual-motor/Perception
- Grip strength
- Emotional regulation/Mood
- Proprioception
- Adapted brushes, finger paints (sensory)
- Activity ideas
- Paint a familiar photograph
- Paint mood
- Mural (group effort)
I use this tool the most frequently. I think painting tends to be the most therapeutic and the least intimidating. Painting provides calming input with a variety of colors. Some targeted skills include visual motor and perception. This goes back to what I was talking about using contrast and different colors to help with perception. Grip strength is needed to maintain a grip on that paintbrush. Emotional regulation and mood are tapped as this activity is calming. Many times people will paint their emotions which can help them to identify what they are feeling and the ability to express themselves. This activity can also help with proprioception, especially if they are using finger paints. You are increasing that sensory input and this can be used with both adults and children. I have had adults dive into finger paints, and they have loved it. You are going to have to use your clinical judgment on what might be appropriate for which patient.
There are also a bunch of adaptive brushes, but we can certainly adapt paintbrushes as well. You could use a cut-up toilet paper roll (in Figure 5) to make some cool designs and to give a bigger grip for a client that needs that.

Figure 6. Modified paintbrush.
You can also use paper towels or sponges to provide some texture and easier tools to grip as well.
For some activity ideas here, you could paint a familiar photograph. That might be most appropriate for someone who you think would be less critical of themselves. They can use it for reminiscence or hang it up in their room right next to the real photograph. You can also prompt patients to paint their mood. I like to combine this with music and songs. I will play an instrumental song, and I will prompt the patient to paint with whatever colors they want, for however long they want, and in whatever direction. This does not have to be a picture or anything. In the end, I will ask them questions. "What color doe this represent?" "There are some jagged lines here. Was this during a louder part of the song?" "What does that represent to you?" In this way, you can see how they responded to the different rhythms and pitches of the song. The last activity idea here is a pretty fun one. It is a mural or large pictures that are usually hung on the wall. You can use the big brown rollout paper that is at Home Depot, or you can use a big chalkboard. This is great for visual scanning and accommodation, neglect, and inattention. If you assign a section of the mural to a patient, they have to know to organize themselves to create that one piece of the mural. This is usually a group effort, and it turns out to be pretty cool. It lights up a rehab room, and the patients are always very proud of it.
Drawing.
- Targeted skills
- Dexterity/grip strength/B UE use
- Attention
- Emotional regulation/mood
- Sequencing
- Activity ideas
- Draw repetitive lines & circles
- Draw self-portrait while looking in mirror/draw human figure
- Draw mandala
Video 4 shows an elderly man drawing.
Video 4.
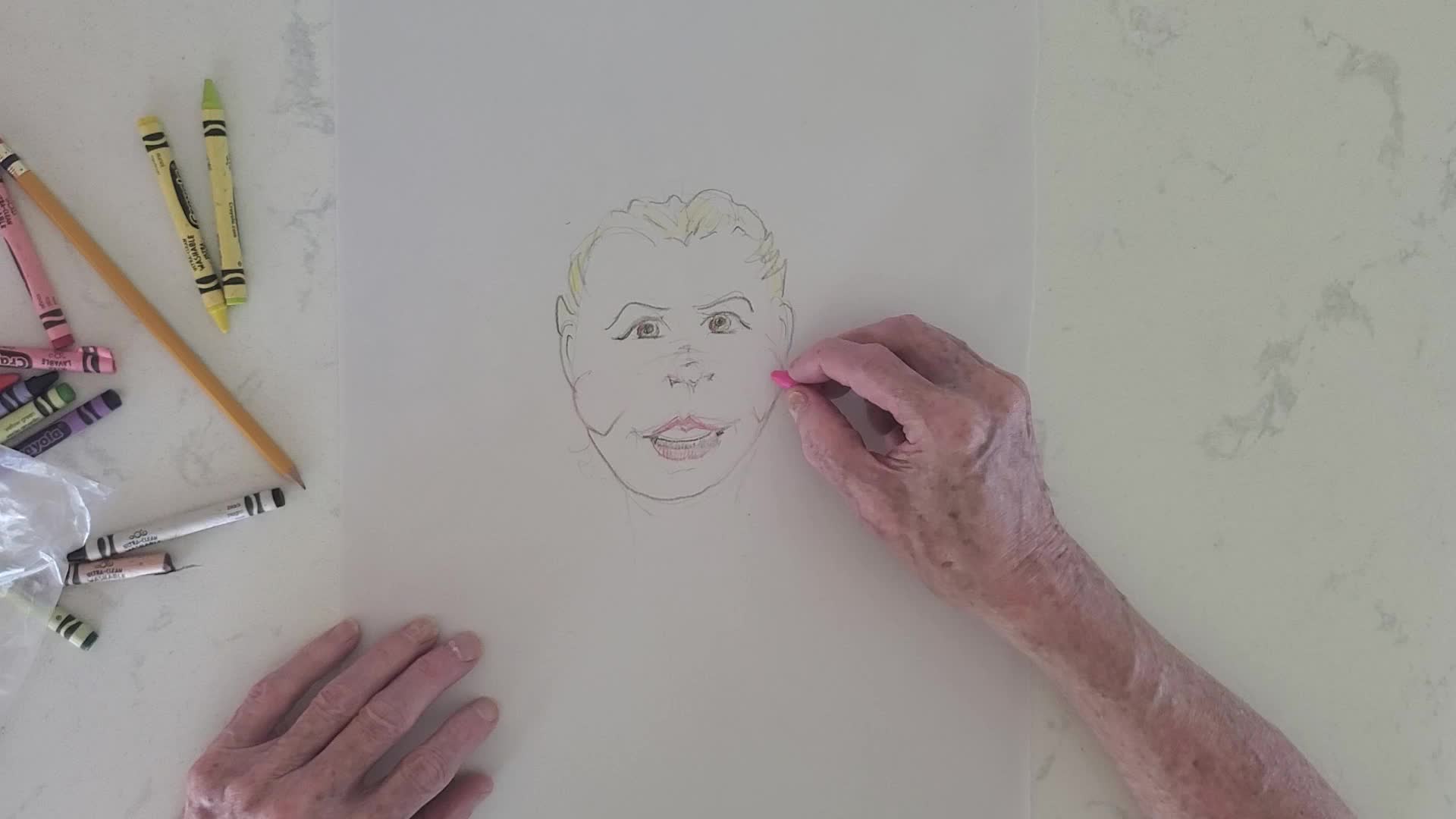
This man clearly has some artistic talent, but he is also engaging in something that he is proud of. He is maintaining a grip on a writing utensil and utilizing those intrinsic muscles that he would not normally be using. This also gave him something to talk about with his friends afterward. He was very proud of the fact that he even attempted that task, which is great. For targeted skills, this worked on dexterity, grip strength, and bilateral upper extremity use. This is a great way to get that person to utilize one hand as a stabilizer and the other hand to do the drawing. You can also work on standing tolerance and balance. You can put a mirror in front of them while they engage in it and ask them to maintain midline while they are drawing. And, you can also set the coloring utensils out of reach so that they need to cross midline or reach diagonally to get their writing utensils. You can also challenge their balance in that way. Some other targeted skills are attention, emotional regulation, mood, and sequencing.
For some activity ideas, the first one I use for calming is drawing repetitive lines and circles. They can be vertical, horizontal, or diagonal. They can draw their lines however they want. It can help with muscle memory and helps with calming the person and getting them out of their own head, which can be necessary at times. You can also prompt them to draw a self-portrait while looking in a mirror or drawing the human figure. If you have someone who had a stroke and now they have inattention or neglect, especially to one side of their body, drawing a human figure or their face is a great way to help them attend to both sides of their body. This can also help them to feel for the proprioceptive input. And then after they draw it, if there are any missing pieces of the human figure or their face, you can help compare it to a real-life example to address their neglect. The last activity is drawing a mandala This is a very common picture that you might see in adult coloring books and is used for stress reduction. They are usually big circular forms, and you create lines through the diameter. It looks like a pie that is cut into slices and then you make little repeated lines and shapes all throughout the circle. For a lot of people, this is very calming. You can then prompt the person to color the mandala after they are done. This can help with visual discrimination, visual scanning, and visual accommodation.
Photography.
- Targeted Skills
- Mood
- Memory recall
- Visual scanning
- Perception
- Activity ideas
- Collage from magazines
- Historical photos for reminiscing
- Locate objects in pictures
Next, we have photography. For the purposes of this treatment, we are talking about photography and looking at photos that already exist as it might be difficult to take pictures in the clinic due to HIPAA reasons. This can work on mood regulation, memory recall, visual scanning, and perception.
For activities, I like to make collages from magazines. They have to cut, visually scan, and paste. A collage can also be good for neglect and attention. I have had patients make their own vision boards this way. They will go through some magazines and cut out things that mean something to them or are motivating to them. They then hang up in their room and address this each for rehab. You can also take some historical photos for reminiscing. You can ask the person where they were when that event happened or if they knew anyone that was directly impacted. It helps the client to open up about their life, work on their memory, to help build rapport, which is also very important. This next one is locating objects in pictures. It helps with visual scanning, attention, and neglect. This can target a lot of different skills, especially in the neurological population.
Drama and Storytelling: Indications and Interventions
Multi-Sensory Sessions.
- Targeted skills
- Sensory modulation
- Attention/memory recall
- Mood/Emotion Regulation
- Sequencing
- Social skills /Communication
- Coping strategies
- Activity ideas
- Essential oil diffuser
- Reminisce looking at old photographs
- Listen to music
- Sensory mats
- Sandboxes
We talked briefly about multisensory sessions, and I mentioned that they were created by this company called Fine Art Miracles in Pittsburgh. They have developed this technique where you work with nursing home residents in memory care units, and you try to stimulate as many senses as possible to get them to interact with the world around them. This woman in Figure 7 is part of one of those sessions.

Figure 7. A woman engaged in a multi-sensory session.
She usually does not interact with her environment at all. She is very under-stimulated, and therefore, does not talk, attempt activities, or move much at all. However, when she is in these sessions smelling perfumes, touching furry teddy bears, and wearing colorful hats, she lights up and becomes a different person. As I said, we have had loved ones come in and just exclaim over how successful these sessions are with their loved ones. This goes back to storytelling, as I mentioned with the individuals with intellectual disabilities. We are trying to stimulate as many senses as possible to foster learning and retention. The targeted skills here are sensory modulation, attention, memory and recall, mood and emotion regulation, sequencing, social skills and communication, and coping strategies.
As I mentioned earlier, the activity ideas include bathroom safety like feeling the different temperatures of the water, smelling the soap, feeling the floor, etc. For these multisensory sessions, you could use things like essential oil diffusers for the fragrance, reminiscing by looking at old photographs, listening to music, and using sensory mats with different textures on them, different materials, so that patients can touch different things and kind of wake up those receptors in their fingers. And then also. You can also use sand bins. Patients will sift through the bins and try to find different objects and work on their stereognosis skills in that way. Obviously, in the COVID world, this can be difficult, and you would have to employ some hygienic techniques to be able to use that.
Role-Playing and Improvisation.
- Targeted skills
- Social skills/interpersonal relationships
- Confidence
- Mood
- Planning and sequencing
- Recall
- Empathy
- Activity ideas
- Act out a social situation, like approaching a middle-school lunch table and asking to sit there
- Memorize simple lines of a play and perform it in front of an audience
- Reconstruct a past situation and act out a different end
Role-playing and improvisation target social skills, interpersonal relationships, confidence building, mood, planning and sequencing, recall, and empathy. We talked about role-playing earlier where the therapist plays a role and the patient reacts in whatever way they feel fit. After, you can review how the patient reacted. We already talked about the social situation of approaching a middle school lunch table. You could also have the patient memorize simple lines of a play and perform it in front of an audience. That works on a ton of different skills. Many times patients regain a sense of pride and control over their situation when they learn a new skill and engage in this activity. You can also reconstruct a past situation and act out a different ending. This can be very therapeutic. For instance, if you have someone who had a stroke, a heart attack, or fell down the steps, you could have them talk about the events that sort of led up to that incident and how they could change that. What I find a lot of times is this is therapeutic because my patients will play the "what-if game." We all have done that, but it can be detrimental to recovery if you dwell in the past. They can talk about what would have happened otherwise, and then move past it and address what is going on currently.
Creative Visualization.
- Engage as many senses as possible to visualize a situation
- Targeted skills
- Sequencing
- Emotional regulation
- Mood
- Creativity
- Goal-setting
- Can be scripted or improvised
- Activity ideas
- Visualize a future self, write down desired traits and goals to achieve
- Identify a habit to get rid of and describe life without the habit
Creative visualization is where you engage as many senses as possible to visualize a situation. Some targeted skills here are sequencing, emotional regulation, mood, creativity, and goal-setting. It can be scripted or improvised, and it is based on your patient's cognitive and intellectual level. Some activity ideas here visualizing a future self and writing down desired traits and goals to help get you there. This can be great to develop an occupational profile at evaluation. It can help you to see what is important to somebody and what they want to work on. They can also identify a habit to get rid of and describe life without that habit. An example might be envisioning life if they started using their walker and were safer in their household. What would that look like for their loved ones? What would that look like for when they are moving around in the house?
We have a lovely resident here in Figure 8. She is engaged in a storytelling time with some multisensory components. Obviously, she lights up during those sessions.

Figure 8. Client participating in storytelling.
Dance and Movement: Indications and Interventions
Mirroring.
- Targeted skills
- Empathy
- Social interaction
- Emotional regulation
- Self-awareness
- Mobility (kinesthesia)
- Activity ideas
- Patient mirrors therapist and vice versa through a sequence of movements completing a task – e.g. building a “castle” to signify a safe space
- Patient mirrors movements of therapist doing Big and Loud or PNF movements
We talked about mirroring before, but it is best used to build empathy. We see this a lot with kids with autism or someone after a brain injury. They have a very difficult time identifying with how someone feels. This mirroring is where the therapist does some moves, and the patient faces them and does the same moves. As I said, this can build empathy, as well as social interaction, emotional regulation, self-awareness, and mobility. Some activity ideas are building a castle to signify a safe space or mirror your movements while you are doing big and loud movements for Parkinson's. Here we have a couple of videos of people mirroring. The first one is a young man mirroring me in Video 5.
Video 5.

The next one is two sisters, and they were trying to work on empathy with both of them and trying to relate to each other (Video 6).
Video 6.

The little sister is trying to mirror her sister. It does not go quite as well as planned, but they are expressing themselves and engaging in some parallel play. These were both done with virtual therapy because of COVID.
Expressive Writing: Indications and Interventions
Here are some ideas for expressive writing.
Prompts.
- Targeted skills
- Emotional regulation
- Grip strength/Handwriting
- Attention to task
- Examples:
- Write about a time you felt angry with someone. What did that emotion feel like to you?
- Write about the happiest memory you can think of, then describe your environment, the time of day, and the people around you.
There are prompts that you can give. For example, "Write about a time you felt angry with someone. What did that emotion feel like to you?" Or, "Write about the happiest memory you can think of, then describe your environment, the time of day, and the people around you." This can work on a lot of different things, but targeted skills are emotional regulation, grip strength for handwriting, and attention to a task.
Timed Free Journaling.
- Targeted skills
- Attention to task
- Emotional regulation
- Handwriting
- Mood
- Description: Have patient write in a journal for a preset amount of time with no direction – prompt patient to “not think about what [they’re] writing, just let it flow”
You can also do timed free journaling. The patient can write about whatever they want, but it is for a preset amount of time. I like to use this when I am having someone work on standing balance or tolerance as they are distracted with the writing. I can also get to know them a little bit better based on what they are writing or how they are feeling. This can be used to work on attention to task, emotional regulation, and handwriting in general. I have a lot of patients after stroke or brain injury that want to work on handwriting. This can obviously be used with children as well. This can also help with mood. Many research studies show that journaling helps anxiety and depression tremendously. It is sort of like a mood or emotion dump. It might help a client to psychologically move forward in their rehab.
Phrases and Mantras.
- Targeted skills
- Self-awareness
- Emotional processing/regulation
- Motivation
- Self-compassion
- Activity ideas
- Daily handwritten notes on goals/mantras
- Gratitude mantra – what are you thankful for?
- Multi-modal: write a favorite phrase or lyric, then draw an associated image.
Other parts of expressive writing phrases and mantras like that "carpe diem" I talked about. Targeted skills here are self-awareness or 'what is important to me?' This determines the mantra that they will follow. It can also work on emotional processing and regulation. It could be, "Take a deep breath." This can help the client to process some of their emotions and calm themself down. It also helps with motivation. These mantras can be motivating for a lot of people and provide self-compassion. Maybe you have a patient that tends to be overcritical. You might want to help them to develop a phrase or mantra that they can repeat to themselves as soon as they start hearing that negative voice speak up
Some daily activities are handwritten notes on their goals and mantras. This can be helpful as patients tend to forget everything that they are working on or they have achieved. They can write down how far they have come. A gratitude mantra is what you are thankful for doing each day.
A multimodal treatment might be to write a favorite phrase and then draw an associated image. Here is an example in Figure 9 with this funny poem.
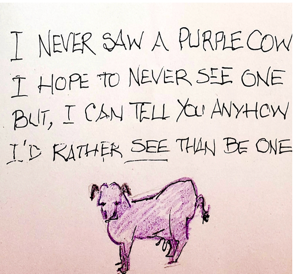
Figure 9. Example of a mantra and drawing together.
The elderly gentleman loved this poem, and he drew an image to represent the poem. He got a lot of joy from that, and it was a great way to engage multiple senses.
Poetry.
- Targeted skills
- Emotional processing/regulation/Empathy
- Attention to task
- Expressive language
- Activity ideas
- ”Fill in the blank” – poem with blanks
- Sentence stem – start the patient off with a stem, i.e. “If you knew me…” and have the patient finish the sentence.
Poetry has some targeted skills including emotional processing, regulation, and empathy. They can look through some of their favorite poems and read them while they are standing or on their way to the bathroom. This also helps with attention to task and expressive language. This is similar to be talking about them finishing a phrase or a song lyric. You could also use that with poetry.
Besides filling in the blank, you can use sentence stems. I like using this during evaluation as it helps me get to know the patient on a much deeper level. I might start them off with a sentence stem of, "If you knew me..." and then they finish that sentence. I have gotten to learn a lot of interesting things about patients that have come up in therapy. It helps to build that rapport and gets them more invested in their rehab.
Music and Singing: Indications and Interventions
“Singing for the Brain."
- Indicated for individuals with their caregivers (7)
- A group with a musician leading participants in singing familiar songs
- Promotes acceptance of the diagnosis, improved social relationships and memory, and decreased anxiety
There is a distinct technique called "Singing for the Brain." It is interesting how people use it, and it is indicated for individuals with their caregivers. We know that caregiver burnout is a real thing. This is used for both patients and caregivers, and it is a musician-led group or for anyone who feels comfortable singing or playing an instrument. They lead group participants with their caregivers in singing familiar songs. It promotes acceptance of the diagnosis, which I think is very important not only for the client but also the caregiver. It can improve the social relationship between the caregiver and the patient, and it gives them common ground to talk about. It also helps memory and decreases anxiety, which is pretty cool.
Melodic Intonation Therapy.
- Indicated primarily for individuals with nonfluent aphasia post neurologic injury (9)
- Uses words and simple phrases with melodic accompaniment and rhythmic tapping
- Appears to be most appropriate for individuals with an intact right hemisphere (e.g. left CVA)
Melodic intonation therapy is indicated primarily for individuals with non-fluent aphasia. It uses words and simple phrases with rhythmic tapping and melodic accompaniment. You might have a phrase like, "I love you." You have them tap out the syllables, and this can help to transfer that to regular expression. It appears to be most appropriate for individuals with an intact right hemisphere. In Video 7, we have a child who had amniotic band syndrome, and some of his fingers weren't fully developed because of it. He is super excited to get involved with his musical instrument and singing. He is gaining confidence and using his hands at the same time. Music provided that motivation for him.
Video 7.

Vocal Music Therapy.
- Can be used with patients suffering from chronic pain (13)
- Uses music-guided breathing, toning and humming, discussion of somatic experiences and biological benefits of music, and instrument improvisation
- Decreases depression, improves self-efficacy and motivation, increases social connections
Vocal music therapy is used with patients with chronic pain. Research has seen a lot of success with this. A lot of times patients in chronic pain try to get out of their bodies so that they do not feel it anymore, which makes them move less and makes them feel detached from their own bodies. This is music-guided breathing and humming. They discuss their somatic experiences and the benefits of music. They can also use instruments. This helps to improve self-efficacy, motivation, and socialization. It has been a big benefit for that population.
Deep Breathing Exercises Set to Music.
- Patients of all ages and diagnoses
- Stress reduction, pain management
- Combine Big and Loud movements to music for treatment of Parkinson’s Disease
Patients of all ages benefit from deep breathing. It is a big stress reducer and is great for pain management. You can combine it with big and loud movements for the treatment of Parkinson's disease. This is a great way to get creative and motivate a patient who enjoys music.
Multi-Modal Approaches
- Shown to improve the overall quality of treatment and goal attainment
- Approach to treatment: goal-oriented and problem-solving approach with guided discovery component (10)
- Example: CO-OP approach, see reference source #13
- Can be used with any patient
- Clay + Music: Play a classical song, prompt with “Mold your clay into something representing an emotion that comes up during this song.”
- Optional: ”close your eyes”
- Indicated to treat depression, pain, sensory deficits, and FM impairments
- Combining stretching/yoga program with multi-sensory crafts (8)
- Indicated to treat chronic pain in patients of
- Approach to treatment: goal-oriented and problem-solving approach with guided discovery component (10)
