Introduction
Thank you and I am so glad to be here. I hope everybody can join us for Part Two of this talk as well as there will be a lot of case studies. I am excited to talk about this subject as it is near and dear to my heart.
Overview
- Elimination Disorders
- Anatomy/Physiology of Bladder
- Incontinence symptoms/definitions
- Prevalence, Impact and Risk Factors
- Diagnostic Tests
We are going to be talking about elimination disorders today. I know a lot of you are working in the pediatric population only. Bowel and bladder control for children is a little different, especially how we discuss things with them. We will be talking about these disorders and go over the anatomy and physiology of the bladder. We will also talk about the different symptoms and definitions, the prevalence, impact, and risk factors. Lastly, we will review some of the diagnostic tests that the kids in your care may have received.
What Is An Elimination Disorder?
- Incontinence: involuntary loss of urine or feces
- Functional incontinence: no apparent disease, injury or congenital malformation
- Dysfunctional voiding or defecation: incontinence as a result of voiding or defecatory phase dysfunction
- Urinary retention associated with incomplete bladder emptying
- Constipation due to withholding of feces
What is an elimination disorder? The definition of incontinence is an involuntary loss of urine or feces. The definition of functional incontinence is when there is no apparent disease, injury, or congenital malformation. There is dysfunctional voiding or defecation, and that is incontinence as a result of a problem in the voiding or defecatory phase. There is also urinary retention associated with incomplete bladder emptying. Many of these kids will have constipation and withhold their stool. This is called encopresis. Some kids will hold their stool because it hurts when they go. The longer they hold, the more it hurts, and so on. They are then fearful of going to the bathroom.
Dysfunctional Elimination
- Many presentations
- Often not recognized by health professionals
- Basically means holding urine or stool or inappropriate elimination
- Both of these functions need to be frequent and regular
There are many presentations. Often, it is not recognized by health professionals. Dysfunctional elimination is holding urine or stool or inappropriate elimination. Both of these functions need to be frequent and regular for them to have the diagnosis of dysfunctional elimination.
How Do We Control Continence and Prevent an Elimination Disorder?
- Use pelvic floor muscles to provide closure of the urethra and anal canal to maintain continence
- Use pelvic floor muscles to signal the bladder, rectum, and colon when to void or defecate
- Use pelvic floor muscles to provide the opening of the urethra and anal canal by TOTAL relaxation to allow for complete and EFFORTLESS elimination
We use our pelvic floor muscles, which we will be going over in a minute, to provide closure of the urethra and anal canal to maintain continence. There is a partial contraction at all times of these muscles, but we are also able to hold the stool and urine if we cannot get to the toilet in time. Some people have a difficult time with that if they have weakness in the pelvis.
We use pelvic floor muscles to signal the bladder, rectum, and colon when to void or defecate. We also use the pelvic floor muscles to provide the opening of the urethra where the urine comes out, and the anal canal, where the stool comes out by total relaxation. This allows for complete and effortless elimination. When we go to the restroom, we should be able to go without worrying about it. However, if there is any dysfunction, it can be difficult for kids to do that. If you think about someone with hemorrhoids, they may have pain and not want to go because it is painful. As such, they are not getting that full and effortless elimination. Teaching kids how to hold when they need to hold and to release when they need to release without pain is so important.
Skeletal Muscle Vs. Smooth Muscle
- The pelvic floor muscles are normally under voluntary control (skeletal muscles) and can be contracted at will
- The bladder, colon, and rectum function automatically and are smooth muscles
The pelvic floor muscles are normally under voluntary control. These are the muscles that we call skeletal that we can contract and relax. The bladder, colon, and rectum are smooth muscles. They function automatically.
Interaction Between Smooth and Skeletal Muscles in the Pelvic Floor
- Interaction between voluntary and involuntary muscles is complex as we all know!
- Smooth muscle here is inhibited by the contraction of the skeletal muscles of the pelvic floor
- Essentially, the coordinated interaction between smooth and skeletal muscle is essential for normal B and B control
The interaction of the pelvic floor is voluntary and involuntary, and it is a very complex process. Smooth muscles are inhibited by the contraction of the skeletal muscles of the pelvic floor. I will give you an example. I work with women who have a lot of urgency issues. When their bladder is contracting, it is telling the pelvic floor that it is time to relax and open. One of the urge suppression techniques I teach them is if you do Kegel exercises, or you contract the pelvic floor muscles (skeletal muscle), this will send a message physiologically to the bladder (smooth muscle) to calm down. There is definitely coordination between the two and is essential for normal bladder and bowel control.
Anatomy and Function of the Pelvic Floor
Let's look at the anatomy and function of the pelvic floor. This is a picture of a side view of a woman in Figure 1.
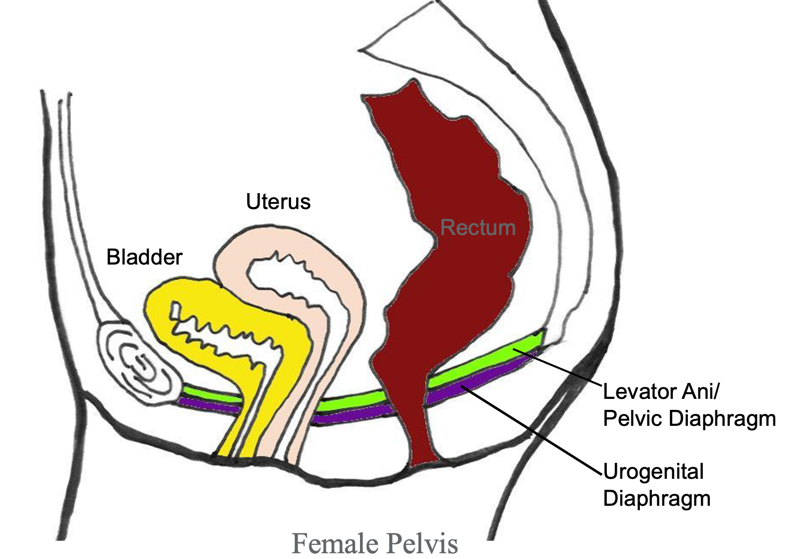
Figure 1. Side view of a woman's anatomy. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
In the front of the body, you can see the pubic bone, and then in the back is the tailbone. There is a sling of muscles like a hammock on the bottom. The bladder sits in the front and the uterus is on top. The rectum in the back. There are three outlets. The urethra carries the urine out underneath the bladder. You have the uterus and the vaginal canal, and finally the rectum and the anus. These three outlets pierce through the pelvic floor hammock.
Figure 2 shows another view.
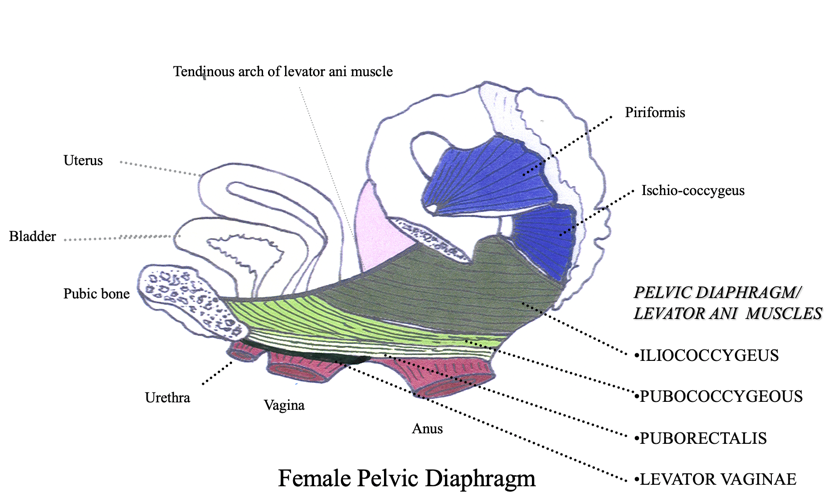
Figure 2. An alternative view of the side of a female pelvis. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
This is a little bit more complex to look at, but I do like that it shows that the urethra, vagina, and anus are all muscular tubes. Thus, we can contract them to hold in urine, gas, or stool. We can also relax them in order to go to the bathroom. There are many muscles that form that hammock from the front to the back.
This is a view of someone lying on their back with their legs open (see Figure 3).
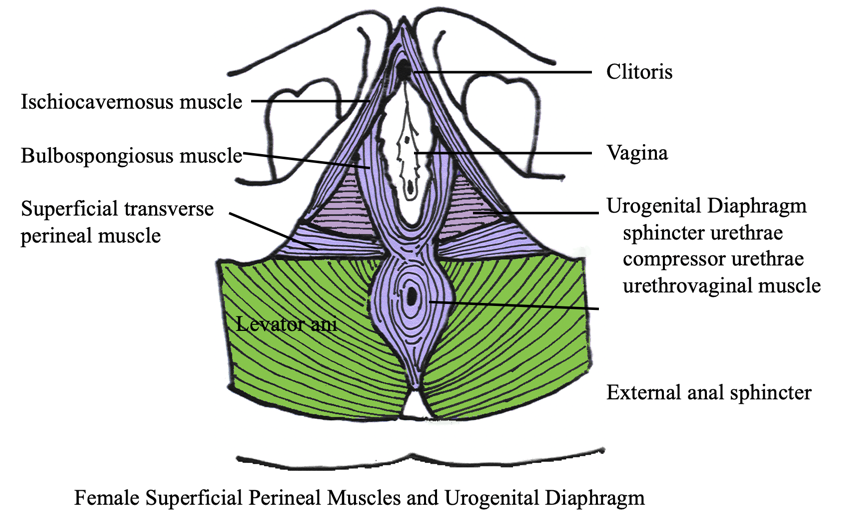
Figure 3. Image of a female with legs open. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
The urethra is at the top, the vaginal opening is in the middle, and then the anus at the bottom. You can see all the muscles that are in this area. The perineum sits between the vagina and the anus. This is where women may have an episiotomy or muscle tearing during childbirth. What I really want you to see from this image is the amount of musculature and coordination required for normal physiological function.
Figure 4 shows an example of the male pelvis.
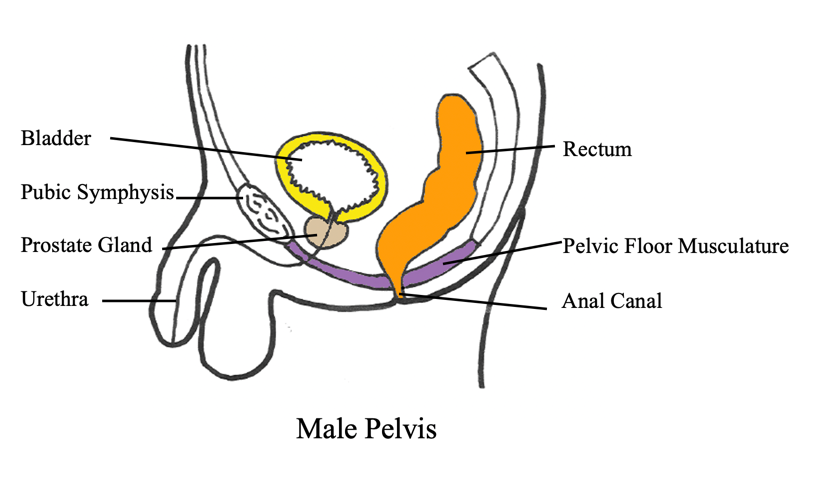
Figure 4. Side view of a male pelvis. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
You can see the pubic bone and the tailbone. Right underneath the bladder is the prostate. Think of the prostate like an apple and the urethra goes through the middle of it. When you are treating boys, they have a much longer urethra and they might hold a little bit differently than a girl that you might be treating. While some of the musculature is the same, men have two outlets.
This is another picture just to show that it is very similar to what it looked like for the female pelvis (see Figure 5).
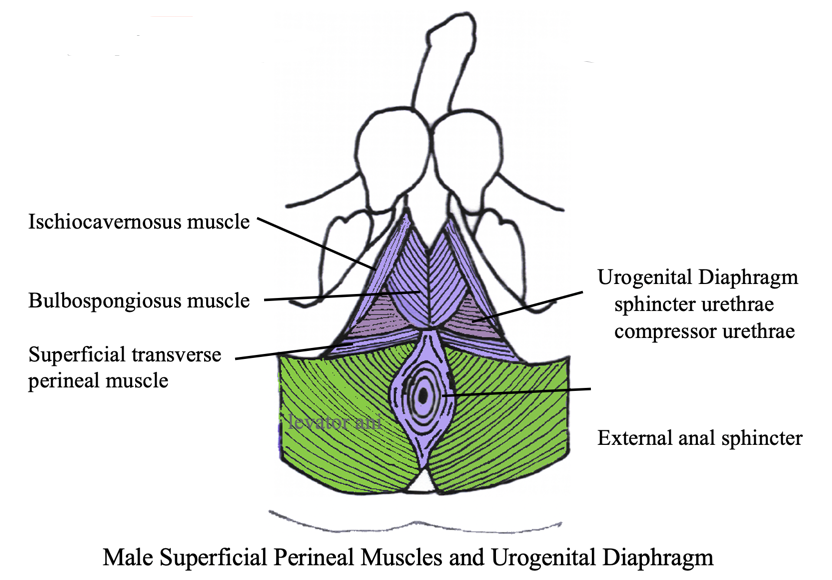
Figure 5. Image of a male with legs open. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
Pelvic Floor Function
- Support organs
- Maintains storage-anal and urethral closure
- Inhibits or permits contraction of the rectum and bladder (the gatekeeper)
- Full relaxation is needed to empty the rectum and bladder
There are many muscles, but this is not something I would go over with a child or their parent. Basically, I collectively call them the potty muscles as it is a little bit easier for them to understand. We will talk more about that in a bit. The pelvic floor supports the organs and maintains anal and urethral closure. They also inhibit or permit the contraction of the rectum and bladder. They are the gatekeepers and full relaxation is needed to empty the rectum and the bladder.
Bladder Anatomy and Physiology
Bladder Like a Balloon
- Think of the bladder like a balloon and the sphincter as the knot
The bladder is an elastic muscle that stretches to hold urine being sent from the kidneys via ureters. The sphincter muscle remains tightly shut, preventing urine from leaking out.
When I am working with the children, I like to have a balloon in my office as the bladder is very much like a balloon and the sphincter that releases is like the knot at the base. The bladder is an elastic muscle, and it stretches to hold urine that is sent from the kidneys via the ureters, and the sphincter muscle remains tightly shut, preventing urine from leaking out. This is a great visual to have in the office if you are discussing bladder control with your patients and families.
Coordination Between the Bladder and Sphincter
- When full, the bladder signals the brain, and the brain in turn signals the sphincter to relax and open. The bladder then contracts and squeezes all the urine out. Then the sphincter closes tightly so the refilling can resume. (pic-Louise Marks)
The sphincter and the bladder are perfectly coordinated in a person with good urinary control. This is a picture of a male bladder because there is a prostate underneath it with the muscles at the base in Figure 6.
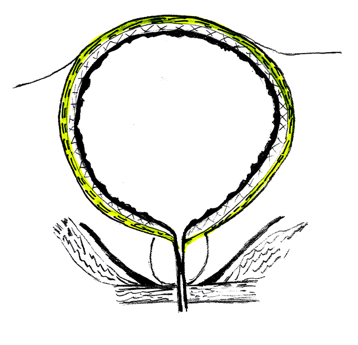
Figure 6. Male bladder. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
When full, the bladder tells the brain which in turn signals the sphincter to relax and open. The base of that balloon is going to relax and open as the balloon or bladder contracts and squeezes all the urine out. The sphincter will then close back tightly so the refilling of the bladder can resume.
Where Do Urinary Control Problems Begin?
- In the bladder: failure to store or failure to empty the urine
- In the sphincter: failure to open, to close, or stay closed
- In the spinal cord: absent or incorrect signals
- In the brain: no message or the wrong message
There may be a failure to store or a failure to empty the urine in the bladder. In the sphincter, there an be a failure to open, close, or stay closed. In the spinal cord, you can also have problems if there are absent or incorrect signals. For instance, someone with diabetes might not get the signal they need to go. In the brain, there may be no message or the wrong message can be sent.
Again, think of a bladder like a balloon (see Figure 7).
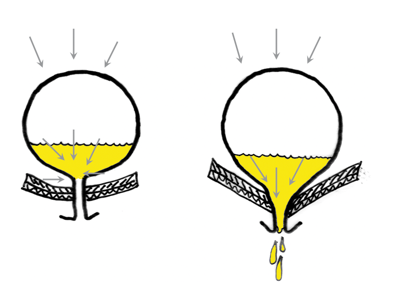
Figure 7. Bladder emptying. (Copyright © 2001 Louise E. Marks, M.S., O.T.R- used with permission)
This is an example I use with my adult patients. If someone has stress incontinence, which means their bladder is full and they cough or they sneeze, that pressure from above comes down. If the muscles are weak, there can be a little bit of leakage. With children, they are going to notice that this happens more if they are constipated because of the pressure of the stool from above.
Normal Bladder Capacity
- Age (in years) +2 = Ounces of urine in a normal bladder
- For a six-year-old:
- 2 + 6 = 8 ounces of urine (8 x 30 = 240 cc of urine)
- Residual: less than one ounce or 30 ml
For normal bladder capacity, you take their age in years and add two for the number of ounces of urine they can normally hold. For example, a six-year-old's bladder can hold eight ounces of urine or 240 cc. When they do void, they should have less than an ounce left. We do not fully empty our bladder each time and there is a bit of residual urine, but you do not want more than one ounce or 30 milliliters.
Normal Voiding
- Normal voiding should be approximately every two to three hours
- Normal fluids: 8-12 ounces at breakfast, lunch, and dinner, or 36 ounces
- One half of body weight in pounds = number of fluid ounces per day
- Example: 60 lbs.. child should drink 30 oz.
Normal voiding should be approximately every two to three hours for children. For normal fluid intake, they would take in about eight to 12 ounces at breakfast, lunch, and dinner, which should be 36 ounces. For adults, we always say about eight cups or 64 ounces. Typically, we take one half of body weight in pounds, and that is the number of fluid ounces per day. For instance, a child who is 60 pounds would drink 30 ounces of water.
Night Time
Nocturnal Enuresis
- Definition
- Commonly called bedwetting
- Frequently associated with a family history:
- Children whose parents were not bedwetters have a 15% incidence
- If one or both parents were bedwetters, rates jump to 44% and 77% respectively.
The term nocturnal enuresis is another way of saying bedwetting. Frequently it is associated with a family history. Kids are really embarrassed and upset about bedwetting. I like to tell them that it is not their fault. We also want to make sure that they are not being punished for bedwetting. Typically, their parents were bedwetters. In fact, the rates can jump to 44 to 77% if one or both parents were bedwetters. You want to make sure that they know that they are not the only person in the world that is having this issue as it is very prevalent.
- Can be related to:
- Sleep disorders
- Psychological issues/stress – controversial: is it cause or effect?
- Genetics
- Endocrine dysfunction
- Maturational delay of bladder development.
- Constipation
- OAB
- UTIs
- Diabetes
Bedwetting can be related to sleep disorders. Many parents report that their kids are deep sleepers and that they are hard to get up in the mornings. Some people think it is psychological or that there is stress in the home. Is that the cause or the effect of what is going on? Genetics can also play a part in this. There are some studies saying that endocrine dysfunction can lead to this or a maturational delay of bladder development. The number one reason for many kids with issues with bladder and bowel is constipation. There can also be other things like overactive bladders, urinary tract infections, or diabetes.
- Can see an increase in detrusor contractions with a decrease in pelvic floor activity during enuretic episodes (see this in adults with sleep apnea also)
- Sleep studies show enuretic children are deep sleepers and tough to arouse
- High urine production during sleep
You can definitely see an increase in detrusor (bladder) contractions and a decrease in pelvic floor activity. Remember, this is the base of the balloon that is less active when you are sleeping. If the bladder is contracting on its own, then it can definitely have issues with leakage during the night. If you are seeing adults with a lot of urine leakage during the night, they may have sleep apnea. There is a big correlation between sleep apnea and nocturia, which is getting up at night to go to the bathroom. Sleep studies show enuretic children are deep sleepers, and they are tough to arouse. A lot of these kids can have high urine production during sleep. This is why want to monitor what they are drinking after dinner.
- Most girls stay dry by age six
- Most boys stay dry by age 7
- By age 10, 95% of children are dry at night.
- Treatments can include bedwetting alarms (bedwetting store.com), medications (hormones or DDAVP known as desmopressin), surgery (urethral dilation), and behavioral treatments with biofeedback.
Many people start potty training at two years old. Sometimes, physiologically their bodies are not quite ready. Girls typically stay dry by 6 and boys by age seven. And by age 10, 95% of children are dry at night.
There are many treatments that can include bedwetting alarms. There is a resource called bedwettingstore.com, and they carry these. While there are many doctors that support this, many do not. There is a little clip that you can put on their underwear and there is an alarm that is on their shoulder. If they wet in the middle of the night, the sensor and the underwear will turn this alarm on. Although this alarm is loud, sometimes it does not wake the child, but it can also give a vibration to help wake them. Typically, the parent will hear the alarm so they can wake the child to finish going to the restroom.
Waking up a child all night long or every two hours is going to disrupt both the child's and parents' sleep, and it is not physiologically when the child is supposed to be going. The alarm teaches the child physiologically when they are supposed to be going to the bathroom. It does take a lot of work, sometimes three to six months; however, there is good research saying it is effective.
There are also medications that kids can take. Desmopressin is one. There is a surgery called urethral dilation, but I am not a fan. That was more in the past, and we are not doing that as much. Lastly, there are behavioral treatments, like biofeedback, which we will talk more about. We will also do some case studies in Part Two that includes this type of treatment.
General Enuresis
- 5-7 million children in the US with enuresis
- Most common urologic complaint
- 30% of parents punish
- Children with enuresis often have self-esteem and emotional distress
- Parental expectations may be unreasonable
- Females>males
- Daytime leaking: maybe anywhere from damp to soaked
- Loss of sensation to void
Enuresis is very common. In fact, five to seven million children in the US having enuresis. I think that number might be higher because I do not think everybody is admitting it, or they are surveying everybody. This is one thing I like to tell kids when I first meet them. I also like to say, "I'm going to be talking with your mom or your dad." I then give them a bunch of adorable books about bedwetting or urinary dysfunction to read.
Again, this is the most common urologic complaint. Reportedly, 30% of parents punish which is sad. They get really frustrated, and they do not understand why their kid is doing this. They feel like they are doing it on purpose. The quicker we can get to these kids and treat them the better because we do not want them to have low self-esteem or psychological issues from the bedwetting and resultant punishment.
Parental expectations may also be unreasonable. You are treating the parents as well as the kids when they come in. Daytime leaking can be anywhere from a damp pad to soaked underwear. Sometimes these kids have a loss of sensation to void, and that can also lead to enuresis.
Can You Outgrow Bedwetting?
- About 15% of affected children outgrow bedwetting on their own each year without medical intervention but inadequate knowledge and lack of support and guidance from family may lead to a child’s mental distress and low self-esteem
Can a child outgrow bedwetting? About 15% of affected children outgrow bedwetting on their own each year without medical intervention. Inadequate knowledge, lack of support, and guidance from family may lead to a child's mental distress and low self-esteem. Sometimes this happens when they start to get invited to sleepovers. They do not want to go and be the kid at the party that has an accident. Most of the older kids really want to get better. You want to help them get to the point where they can have a sleepover.
Preventing Bedwetting
- A hormone that reduces urine production at night needs to be produced: antidiuretic hormone. This hormone is not present at birth but develops between ages two and six, and sometimes not until the end of puberty.
- The patient needs to wake when the bladder is full.
There is an antidiuretic hormone that reduces urine production at night, and sometimes that is not produced yet for these clients. It is not present when we are born, but it develops between the age of two and six. Sometimes, it does not develop until the end of puberty. These are the kids that you occasionally see that are teenagers and are still having bedwetting issues.
A patient needs to be awake when the bladder is full. Many times the kids are not getting the signals, whether they are deep sleepers or there is just not the right signal from the brain to the bladder. As people age, it is normal for people to get up maybe once a night, but most of the time it is due to drinking too late into the evening. I usually have a cutoff time the I recommend. For example, if someone goes to bed at 10:00 p.m., I recommend cutting out liquids by 8:00 p.m. and make sure that there is nothing but water after dinner.
- No fluids after 6 pm (tea, coffee, soda)
- Water only with dinner
- No dairy/sugar snacks after dinner
- Void right before bed (double void)
- Use a waterproof mattress pad
- Disposable pads when traveling
- Teach the child how to clean sheets
- Sense of responsibility
- Can lessen embarrassment
Make sure that the child is not drinking too late. This would be no fluids after 6:00 p.m. especially tea, coffee, soda, or Gatorade. Anything that is colored or red, like Koolaid, should be avoided. I recommend water for dinner. Encourage the water with the kids as it is good for the bladder. However, it is not good when we slam water or drink it too quickly. You want to encourage the slow sipping of water.
They should also not have dairy or sugar snacks after dinner. So, if a child likes to have ice cream, a bowl of pineapple, or anything like that that would irritate the bladder, you want to discourage that. Chocolate is another irritant. Make sure they are eating this earlier in the day.
You also want to make sure that they go to the bathroom before we get into bed. However, kids can get distracted while they are doing other things. You need to encourage the child to go to the bathroom.
Always suggest the use of a waterproof mattress because the urine can sit and create a lot of bacteria. You can get those on Amazon, or even on the bedwettingstore.com pages. And when they are traveling, they can use disposable pads.
You can also teach a child how to clean sheets. We are not doing this as a punishment. When the child gets up, you immediately say, "Let's get the sheets washed." This is not as a punishment but as a responsibility. This can lessen the embarrassment if you teach them how to clean the sheets on their own. They do not have to worry about being embarrassed in the morning or hiding their underwear in the closet.
- Positive reinforcement (sticker chart)
- Kegels (muscle awareness)
- Bedwetting alarm to help the brain-bladder connection
- Drink water throughout the day and not in the evening
Positive reinforcement is great like sticker charts. I know it seems a little bit weird that you could get a child to stop bedwetting with a sticker chart, but this has worked for me. I had a patient once that was bedwetting every single night. We went to the store and picked out a dog calendar as he loved dogs. He got a sticker for every time he went without bedwetting. And then, if he went a few days without incident, he got a special treat like Uno or ice cream. Once they get to the two nights and they have a sticker chart, then you are going to move it to three nights. I had another little boy that was completely dry after 30 days just by using positive reinforcement. A sticker chart is wonderful, and it also encourages the parent to be involved.
Many people wonder why would I teach a child Kegels. It is not only that they have a weakness, but you want them to understand their muscles. I will show them a pelvic floor model so that they can actually see what the muscles are. We talk about the "potty muscles," and how they can squeeze those muscles to keep pee and poop in. You can also talk about gas. You will have to decide the best word. Some kids will say the word "fart," while others will say "toot" or "gas." You let them pick their word. I usually jot it down in my chart so I remember to use the terms that they use. You will discuss that if you want to hold in a toot, "What do you do?" "What does it feel like?" They need to understand that that is the muscle that has to be fully relaxed and release when they have a bowel movement. What you are doing is working on muscle awareness versus strengthening.
How does the alarm work?
- “When a non-bedwetting child sleeps and pressure builds up in the bladder, a signal is sent to the brain to keep the bladder sphincter muscle closed until they can wake up and walk to the bathroom. In bedwetting children, this signal is not recognized by their subconscious reflex system. Instead of waking to go to the bathroom, the child relaxes the sphincter muscle that keeps his bladder closed and wets during his sleep.”
Source www.bedwettingstore.com
A bedwetting alarm helps the brain to bladder connection. It is going off when you are having the signal for the bladder to release. Drinking water throughout the day is important. You do not want the child to be drinking a lot in the evenings, but sometimes that will happen because you cannot really monitor what they are drinking. You can help them to pick out a water bottle that they really love to encourage them to drink. There are some great devices now, even water bottles that glow if they are not drinking enough. It might even give you a text. There are many products out there that can help a child remember to drink their water.
Bedwetting alarms.
- “When a non-bedwetting child sleeps and pressure builds up in the bladder, a signal is sent to the brain to keep the bladder sphincter muscle closed until they can wake up and walk to the bathroom. In bedwetting children, this signal is not recognized by their subconscious reflex system. Instead of waking to go to the bathroom, the child relaxes the sphincter muscle that keeps his bladder closed and wets during his sleep.”
Source www.bedwettingstore.com
How does the bedwetting alarm work? This quote comes from the bedwettingstore.com. The alarm lets them know that it is time to go to the bathroom.
- To maximize success when using a bedwetting alarm, Dr. Hyun (pediatric urologist) recommends several things.
- “It takes time, around three months, and it requires parental involvement. It’s important to make the time commitment.
- The alarm tells you when the wetting happens. It isn’t there to prevent the accident from happening.
To maximize success when using a bedwetting alarm, Dr. Hyun, a pediatric urologist, recommends several things. It takes around three months, and it does require parental involvement. It is important to make that time commitment. The alarm tells you when the wetting is happening to prevent the accident. Chances are if they wake up immediately, they can hold that and get to the bathroom if it is close by.
- The child needs to be involved, getting up to the bathroom when reminded and resetting the alarm before going back to sleep.
- You have to be consistent. Your body doesn’t learn by just using the alarm a few nights a week.
- Older kids ( 9 or 10) tend to be more motivated to make changes.
- The bedwetting alarm needs to be loud enough for the parents to hear. It also needs to be one that the child can easily reset by himself during the night.” www.bedwettingstore.com
The child needs to be involved and get up when reminded. They then need to reset the alarm before going back to sleep. It takes a lot of consistency. Your body does not learn by just using the alarm a few nights a week. It is something that should be used on a daily basis. It can be difficult for some. As an example, I see a lot of kids that are from broken homes. They might go to a different parents' house on the weekends thus it can be a little more complicated when you are dealing with bladder and bowel issues. Again, older kids between nine or 10 may be more motivated to make changes.
There are also alarms that, rather than being connected to the body, are across the room. In this way, they have to actually get up, walk over to the alarm, and turn it off. The bedwetting alarm needs to be loud enough for the parents to hear. They may have to be close by or have the doors open to hear it. It also needs to be one that the child can easily reset by himself during the night.
Normal Nighttime Control
- Begins between age 2-3 during the day and 4-5 at night.
- Children with ADHD are 2.7 times more likely to have issues
- Caffeine increases urine production (soda, tea, coffee, vitamin drinks)
- Constipation: full bowels put pressure on the bladder and change nerve signals (the poop drives the pee).
Normal nighttime control begins about the age of two to three during the day and four to five at night. Children with ADHD are almost three times more likely to have issues. Caffeine does increase urine production and stimulates the bladder. If you drink a cup of coffee, you are going to have to pee much quicker than if you had a cup of water. It is important to limit soda, tea, and coffee, as well as vitamin drinks.
Constipation or full bowels put pressure on the bladder, and they can change the nerve signals. We always say in the pelvic floor world, "the poop drives the pee." If someone has normal bowel movement behaviors, even adults, their bladder dysfunction will clear up if you can get the stool to be more normalized as well.
Daytime
Let's now talk about the daytime and issues we may see.
- “No one ever died from wetting, but some may have wished to…”
This is a big problem for kids. Most kids are very scared to go to school. They do not want anyone to hear them and sometimes they hold it all day. It creates a lot of issues. They may be rushing to get home, or they may have an accident on the way home if they are on the bus.
Child's Perspective
- Children rated wetting themselves at school as the third most catastrophic event, behind losing a parent and going blind.
(Ollendick et al., Behavioral Research Therapy, 1998)
As you can see, this is pretty important to kids.
Urinary Incontinence
- According to the International Children’s Continence Society (ICCS):
- Incontinence is defined as the uncontrollable leaking of urine.
- Two broad categories:
- Continuous (constant leaking related to congenital abnormalities) and
- Intermittent (voiding dysfunction).
According to the International Children's Continence Society (ICCS), incontinence is defined as the uncontrollable leakage of urine. There are two broad categories. Continuous, which is constant leaking related to congenital abnormalities, or intermittent, which is more of voiding dysfunction.
Daytime Incontinence
- ICCS: Accidents at least every two weeks in children over 5 years of age. Can be related to:
- family history
- emotional stress
- male sibling history
Daytime incontinence every two weeks in children over the age of five can be related to family history, emotional stress, or a male sibling history.
Daytime Statistics
- Some degree of daytime urinary incontinence:
- 10% < 7 years old
- 2-9% 7-10 years old
- 2-6% 10-15 years old
- Urinary incontinence 2x/week or more:
- .5% 9 years old
As you can see, accidents diminish as they age. Additionally, 20 to 40% of children with daytime urinary incontinence have behavioral disorders.
(O. Dede, G. Sakellaris, Essentials in Pediatric Urology, 2012; 57-68)
Definitions
- Intermittent urinary incontinence is a voiding dysfunction
- Dysfunctional voiding is a subset of voiding dysfunction (confusing!!)
Intermittent urinary incontinence is a voiding dysfunction. Dysfunctional voiding is a subset of voiding dysfunction This sounds very confusing, but we can break it down more as we move through this talk.
Daytime-Types of Urinary Incontinence
- OAB
- Dysfunctional voiding (not voiding dysfunction)
- Non-neurogenic / neurogenic bladder
- Elimination syndrome
- Voiding postponement
- Lazy bladder: poor bladder emptying due to underactive bladder
- Giggle incontinence
- Vaginal entrapment/vesicovaginal entrapment
- Primary bladder neck dysfunction
There are different types of urinary incontinence. There is an overactive bladder. This is someone who continually has to go or they feel a lot of urges. A non-neurogenic or neurogenic bladder is more related to brain function. They do not get the signal that they need to go or their bladder is not working because of a neurological disorder. They can have an elimination syndrome or voiding postponement. Again, many kids will hold their urine because they are busy playing. They do not want to miss out on anything. Then, the bladder gets so full that it just kind of leaks out a little bit.
A lazy bladder is poor bladder emptying due to an underactive bladder. It does not contract the way that it needs to contract. Giggle incontinence, especially with teenage girls, is when there is leakage with giggling. This is similar to stress incontinence in older women.
There is something called vaginal entrapment or a vesica vaginal entrapment. When a child has obesity and their legs are closed a lot, their pee can get trapped. The urine is stored in the vagina, and they will have leakage after they go. You want to make sure that they are sitting correctly on the toilet. Sometimes, in the beginning, they even have to learn to sit backward on the toilet and rest their arms on the back of the toilet so that their legs are wide.
The other thing that can happen is a lot of kids will pull down their underpants to their knees. This causes internal rotating at their hips and closes their adductors. If you think about the pelvic floor muscles, they need to be open for full release. This may cause entrapment or bladder neck dysfunction.
Long Term Risks
- Childhood daytime incontinence associated with adult urge incontinence
- Women with childhood daytime frequency more likely to report adult urgency daytime incontinence secondary to OAB and dysfunctional voiding associated with:
- Decreased quality of life
- Constipation
- Increased risk of UTIs
(Fitzgerald MP et al, J Urol 2006; 175; 989-993)
Childhood daytime incontinence is associated with adult urge incontinence. I see many women that say they had either bedwetting problems or urgency when they were teenagers. It can be a lifetime issue for some of these patients. Women with childhood daytime frequency are more likely to report adult urgency daytime incontinence secondary to an overactive bladder. Dysfunctional voiding is also associated with a decreased quality of life, constipation, and risk of UTIs.
Urinary Incontinence
- Loss of urine at an inopportune time
- First recorded reference was in 1550 BC
- In 77 AD boiled mice were used as a treatment!!!
- 1472 AD the first book of pediatric diseases was published with an entire chapter on enuresis!
Urinary incontinence is a loss of urine at an inopportune time. Urge incontinence is when you leak on the way to the bathroom, and stress incontinence is when they cough, sneeze, laugh, jump, and move. Any kind of movement that puts pressure interabdominally down into the bladder can cause a leak. Usually, they're the smaller leaks. Mixed incontinence is both the stress and urge combined.
The first recorded reference to urinary incontinence was in 1550 B.C. In 77 A.D., they used boiled mice as a treatment. They would boil mice and you would drink it, which I do not know how that helped. And in 1472 A.D., the first book of pediatric diseases was published with an entire chapter on enuresis.
Socio-cultural Factors and Psychopathology
- Stress (i.e. as a result of marital separation) increases the incidence of diurnal or mixed UI
- Increased incidence of attention problems and delinquent behavior in voiding postponement syndrome
- Children with ADHD are three times more likely to have daytime UI Delayed Maturation or MR – increases the risk of daytime wetting (OR 1.9% and 4% respectively)
Stress is something that can lead to bladder and bowel issues as a result of marital separation. This increases the incidence of diurnal or mixed urinary incontinence. There are also attention problems and delinquent behavior in voiding postponement syndrome.
If you think about it, there are two things that we can control. As a child, they can control what goes in their mouth, their eating, and if they want to hold in poop or pee. This can become a control issue for a child.
Children with ADHD are three times more likely to have daytime urinary incontinence and this increases the risk of daytime wetting. Kids who have difficulty focusing or attending also do not recognize the signals when they need to go. They can be very distractable and do not sit on the toilet long enough.
Other Considerations
- Divorce: How does this impact the child?
- Psychological considerations
- Overwhelming sadness
- Two homes, two lifestyles, two sets of rules, two sets of routines
- Living with “Strangers”
- Communication between parents
How does a divorce impact the child? You have to look at psychological considerations. There can be overwhelming sadness. If there are two homes, there will be two lifestyles, two sets of rules, and two sets of routines. If one of their parents has a new relationship, they can feel like they are living with strangers. Sometimes, there is not good communication between parents. I have children who do really well during the week, and then when they go to the other parent's household, it all falls apart. They have sweets and junk, and there is no set routine. Then, they have to start all over again on Monday. It becomes pretty challenging for those kids.
Urge Syndrome (OAB)
- Frequent episodes of an urgent need to void caused by bladder over-activity
- Bladder contractions countered by contraction of the pelvic floor muscles (guarding reflex) and holding maneuvers
- The mucosal lining of the bladder may be damaged due to strong bladder contractions and strong pelvic floor contractions. This can increase the risk of UTIs
- May also present with constipation and fecal soiling
There is something called urge syndrome, which is also an overactive bladder. There are frequent episodes of an urgent need to void caused by bladder overactivity. These are bladder contractions countered by the contraction of pelvic floor muscles, which is the guarding reflex and holding maneuvers. If you have ever seen a child that crosses their legs and holds it, they are either trying to keep everything in or do not want to go to the bathroom. The mucosal lining of the bladder may be damaged due to both strong bladder and pelvic floor contractions. This can increase the risk of UTIs because they are not emptying, and the bladder is storing the urine for too long. Many of these kids can also present with constipation. We will talk a lot about that in Part Two, and they can have fecal soiling. Many parents think that their child has diarrhea because of this soiling when in fact they are completely impacted and constipated. The liquid is still sneaking around the impacted stool.
Vincent Curtsey
- Potty dance
- Perineal pressure applied by the heel of the foot during urge to urinate
- Contraction of external urinary sphincter inhibits bladder contractions
- (S.A. Vincent, Lancet, September 1966)
Vincent Curtsey coined the term "potty dance." You have probably seen a child dancing around or applying perineal pressure with their heels. This is done to decrease their urge to go to the bathroom. They figure this out on their own. This is what I was talking about at the beginning of the talk. You can teach these kids how to do pelvic floor contractions or Kegels to decrease that urge feeling as well. The contractions of external urinary sphincters inhibit bladder contractions. If you are doing those squeezes, you can make the bladder calm down.
Dysfunctional Voiding
- Inability to fully relax the urinary sphincter or pelvic floor muscles during voiding
- Present with incontinence, UTIs, and constipation
- May be due to OAB
- Staccato voiding – periodic bursts of pelvic floor activity during voiding, prolonged voiding time, and possibly residual urine. Flow is continuous.
- Interrupted voiding – incomplete and infrequent voiding with micturition in separate fractions. Doesn’t empty well.
Dysfunctional voiding is the inability to fully relax the urinary sphincter, or the pelvic floor muscles during voiding. If a person is presenting with incontinence, urinary tract infections, and constipation, it may be due to overactive bladders.
There is also something called staccato voiding, where you get bursts of pelvic floor activity during voiding. You can hear intermittent squirting as they are going to the bathroom. Interrupted, incomplete, and infrequent voiding are the different types of dysfunctional voiding.
- Initial signs reflect detrusor over-activity with poor emptying and may include:
- Small bladder capacity
- Increased bladder thickness
- Decreased bladder contractility
- Impaired relaxation of the external sphincter during voiding
- Weak or interrupted stream
- Increased PVR
- Fecal soiling and constipation
Thre are some initial signs that reflect the bladder overactivity with poor emptying. One is a small bladder capacity where it cannot hold very much. They can have increased bladder thickness. Imagine again that the bladder is like a balloon. A balloon with a thick wall is not going to be able to hold as much due to decreased bladder contractility. There could also be an impaired relaxation of the external sphincter during voiding so they are not getting that full release. They can have a weak or interrupted stream or an increased post-void residual (PVR), which means how much urine is left in the bladder after the void. Lastly, it can be a result of fecal soiling and constipation.
Underactive Detrusor and Poor Bladder Emptying
- Lazy bladder – former terminology
- Use Valsalva maneuver to void
- Most common in girls
- May be the later stage of chronic voiding postponement
- Large capacity and no contraction during voiding – overstretched detrusor
- At risk for UTIs and high residuals
- Need UDS to determine
An underactive bladder and poor bladder emptying used to be called a lazy bladder. You can use the Valsalva maneuver to void, which means that you put pressure on the abdomen to open the pelvic floor. This is most common in girls, and it can be in the later stage of chronic voiding postponement. There can be a large capacity within the bladder and no contraction during voiding. Basically, the bladder is overstretched. These kids are at risk for UTIs and high residual volumes. They often do a study called urodynamics to determine if they have an underactive bladder.
Giggle Incontinence
- Originally described in 1959 by MacKeith as Enuresis Risoria or Giggle Micturition
- Etiology unknown
- Theories:
- Laughter causes hypotonic state with urethral relaxation
- Laughter triggers micturition reflex overriding central inhibitory mechanisms
They are really not sure why it happens in kids, but the theory is the laughter causes a hypotonic state. I have seen this in women if I am doing biofeedback on their pelvic floor muscles. During laughter, I have seen the pelvic floor activity on the biofeedback go up and down. Laughter triggers the micturition reflex, and it overrides the central inhibitory mechanisms that are happening in the body.
Voiding Postponement
- Postponement of imminent micturition until overwhelmed by urgency, then rush to the toilet, it’s too late, UUI occurs.
- Significantly higher frequency of behavioral issues in these children compared to those with OAB
- Children will restrict fluids to increase voiding interval over time
- Proposed by Lettgen et al. (Lettgen B. Acta Pediatr 2002; 41, 978)
Voiding postponement is when a client is overwhelmed by urgency. They rush to the toilet, but it is too late. They might have an accident on the way to the toilet. There is a higher frequency of behavioral issues in these children as compared to those with an overactive bladder. They are postponing, which is different from having an overactive bladder. Children will restrict fluids to increase voiding intervals over time. I see this in adults as well. They restrict their fluids so they do not have accidents, and then they become dehydrated and constipated, which causes more problems.
Vesicovaginal Entrapment (Vaginal Reflux Voiding)
- May be related to anatomical abnormalities such as labial adhesions, or a funnel-shaped hymen.
- Improper position on the toilet
- Obesity may be a risk factor (large thighs)
- Symptoms include urinary leakage a short time after voiding and is not associated with urgency.
We also discussed vaginal reflex voiding. It can be due to something like a funnel-shaped hymen or sitting improperly on the toilet. It can also be from obesity. They can have urinary leakage a short time after voiding, but it is not associated with urgency. It is more the way that they are sitting or how their legs are closed. The urine gets trapped.
- Patients with reflux have a tendency to have dysfunctional elimination
- The goal for treatment:
- Protect kidneys
- Prevent UTIs (? Daily antibiotics)
- Treat dysfunctional elimination
Patients with reflux have a tendency to have dysfunctional elimination. The goal for treatment is to protect the kidneys, prevent UTIs, and treat dysfunctional elimination.
Elimination Syndrome
- Females have a greater incidence than males.
- Associated with VUR and UTIs
- Abnormal recruitment of the external anal sphincter during defecation
- There are a concomitant urethral sphincter and pelvic floor contraction during micturition.
- Can lead to bladder hypertrophy, detrusor overactivity.
For elimination syndrome, females have a greater incidence than males. There is abnormal recruitment of the external anal sphincter during defecation. The urethral sphincter and pelvic floor contract at the same time making it difficult to eliminate. When the pelvic floor closes, the bladder releases, and you have this nice little coordination going on. However, if they are always contracting the pelvic floor, it can lead to bladder hypertrophy making the lining thicker. If someone is constantly contracting and holding, that bladder has to get stronger and thicker.
- Symptoms include:
- Urinary incontinence
- Nocturnal enuresis
- Recurrent UTIs
- Urgency
- Frequency
- VUR
- Constipation
- No regular bowel routine and fecal soiling
They can have urinary incontinence and nocturnal enuresis, which is the bedwetting. They can get urinary tract infections, feel urgency, and frequency. We are going to talk about the VUR in just a second. Constipation is no regular bowel routine, and again, they can have fecal soiling.
Other Definitions
- Functional Incontinence – Difficulty getting to the restroom in time because of pain, CP, and other musculoskeletal problems.
- Urinary Retention – Lack of ability to urinate.
- Frequency – voiding more than is age-appropriate. Often considered a classroom behavioral issue by teachers.
Another definition to be aware of is functional incontinence, which is difficulty getting to the restroom in time because of pain. They may have cerebral palsy or other musculoskeletal problems. If they are using a walker, they cannot get there quick enough. It is called functional incontinence if there is no specific reason. Urinary retention is the inability to urinate or not emptying well. Frequency is voiding more than is age-appropriate. If somebody is going too often, that can be a problem as well. An example might be someone going hourly. Many times, the kids ask the teachers to go to the bathroom, but they are denied as it viewed as behavioral.
Determining Voiding Dysfunction
Physician Evaluation
- Detailed History: family history, social, age of toilet training, fluid intake, voiding habits, medications, surgeries, psychiatric history, history of UTIs
- Voiding Diary: the time of voids, frequency, amounts, nocturia, stream quality
- Physical exam: rule out any anatomical or neurological causes
A physician will evaluate and get a detailed history of the family, social status, age of toilet training, fluid intake, voiding habits, medication, surgeries, psychiatric history, and history of UTIs. If they do not have them do a voiding diary, then that is something that you should have the patient fill that out. How often do they go to the bathroom? How frequently are they getting up at night to go to the bathroom? Are they having bedwetting episodes? What is the stream quality? When they pee, does it sound like a normal stream? Is it delayed? Is it staccato? I will even take a glass of water and simulate that type of voiding to see if that is how it sounds for them. A physical exam will rule out any anatomical or neurologic causes.
Evaluation Process
- History of the problem
- Bladder and bowel diary helpful
- Review medical history, physical exam results, family medical history
- Social history – family structure/stressful situations
- Patient motivation
- Previous treatments
- KUB
- Bladder/renal ultrasound
- UDS
- Uroflow/EMG
They look at the history and a bladder and bowel diary, which is really fantastic if they can fill that out. What is their social history? Are there stressful situations? Is the patient motivated? Did they have any previous treatments? Bladder and renal ultrasounds may be done. Other tests are a urodynamics study, a uroflow, which is looking at how quickly they are peeing, or an EMG/biofeedback.
Diagnostic Testing
- Urine analysis and culture
- Ultrasound: assess post-void residual, bladder wall thickness, abnormalities
- Voiding cystourethrogram: -(VCUG) used in children with recurrent or febrile UTIs to show reflux, bladder emptying, and abnormalities in bladder size, shape, capacity. Looks at the urethra. Uses fluoroscopy for visualization. The contrast agent introduced through a catheter into the bladder.
The diagnostic testing can be a urine analysis and culture. They can also do an ultrasound to look at post-void residuals. After a child goes, how much is left in their bladder? They can look at that with an ultrasound machine. They can look to see how thick is the bladder wall, and if there are any abnormalities. Finally, there is the voiding cystourethrogram.
VCUG. The VCUG is used in children with recurrent or febrile UTIs to show reflex. Is their urine backing up? Are they emptying okay? Are there any abnormalities to the bladder size, shape, and capacity? They are looking at the urethra, which is the tube that carries out the urine. They use a contrast where they can see all of these things. Figure 8 shows a picture of a VCUG. That is the bladder in the middle.
 .
.
Figure 8. VCUG showing the bladder.
With this, they can see how large the bladder is. They can also see if there is good release by looking at the urethra as well.
- MRI: for children with neurological abnormalities on exam
- Uroflow: hold urine until a strong urge to void then void into a collection device that measures flow time, voided volume, and maximum and average flow rate. Generates a flow curve.
- KUB: X-ray of kidneys, ureters, and bladder. Used to determine constipation.
They can also do an MRI or a uroflow where they hold the urine until there is a strong urge to void. Then, they use a collection device that measures the flow time. These are just good words to know so that if you have a patient coming to you, you will have a better understanding of what is being looked at.
KUB (Kidneys, Ureters, Bladder). The KUB is an x-ray of the kidneys and the ureters, which are the tubes that go from the kidneys to the bladder. With this, they can also determine if a child is constipated or backed up?
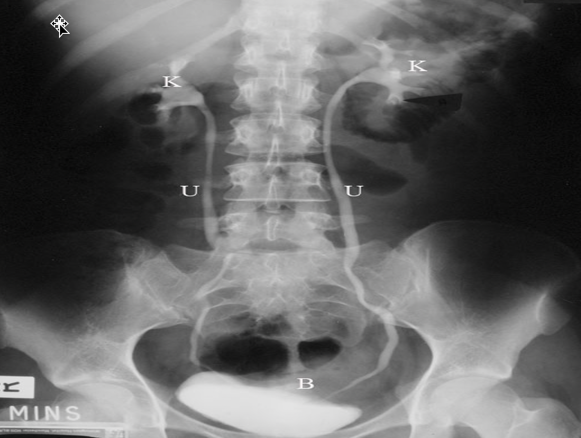
Figure 9. This is an image of a KUB.
The K is for the kidneys, the U is the ureters, and the B is the bladder. This is a very detailed x-ray or picture for the physician to look at. A lot of times, they will see that there is a lot of stool impaction or if there is a problem anatomically with either the kidneys, the ureters, or their bladder. It can give you some great information.
Urodynamics
- Gives more information than other tests, but more invasive (just like an adult test)
- Shows entire filling and emptying phase of urination
- Can give child medication to keep calm
- Determines: OAB, dysfunctional voiding, underactive bladder
The urodynamics study is something that is a little more invasive. Most adults get urodynamics tests, especially if they have pelvic floor prolapse. It shows the entire filling and emptying phase of urination. A child would most likely need to have medication to keep calm because it does involve a catheter. This will determine if they have an overactive bladder, dysfunctional voiding, or an underactive bladder.
Resources for Training and Certification
- Biofeedback Training & Incontinence Solutions
- Telephone 1-512-557-6310 or www.pelvicfloorbiofeedback.com
- hosts a 3-day course annually in April and September which fulfills didactic and practicum requirements for certification
- Biofeedback Certification International Alliance
- Telephone 1-866-908-8713 or www.bcia.org
- offers certification in pelvic floor muscle dysfunction biofeedback
For training, you can get board-certi
