Editor's Note: This text-based course is a transcript of the webinar, Mental Health First Aid Awareness, presented by Tania Sofia Nogueira, MSc, HCPC – UK, COT – UK, ACSS – PT.
Learning Outcomes
- After this course, participants will be able to identify the meaning of Mental Health First Aid (MHFA).
- After this course, participants will be able to recognize what MHFA involves.
- After this course, participants will be able to list the action principles of MHFA.
Introduction
Hello. Thank you for joining me in this Mental Health First Aid Awareness session. My name is Tania, and I am an OT working in mental health as a care coordinator, clinical support manager, and safeguarding officer. Currently, I work as a clinician in an online mental health service for young people. We recently had World Mental Health Day on October 10th, where we are trying to make mental health and well-being for all a global priority. This is a way to recognize this field's progress and be vocal about what we need to do.
Before we start, I would like to make a couple of points. Mental health can be a sensitive subject. I do not know any of your backstories. Today in this session, we will not cover any specific case in depth, but that does not make us immune, so please, throughout the session, check in with yourself. If the session is negatively affecting you, step away from the session for a few minutes. And then, feel free to contact me at the end of the session. The second point I like to make before we start is that we will talk about mental illness. Again, let's acknowledge that none of us are immune to this. Let's try to be kind to ourselves and put self-care at the top of our to-do lists.
Polls
- How prepared do you feel to support someone feeling distressed?
- Not at all prepared
- Not sure
- Well prepared
- Someone you know sends you this text message 'Today is one of those days I want to get out of this sad world.' How confident do you feel about dealing with this?
- Not confident at all
- Somewhat confident
- Very confident
- Based on your personal and professional experience, what are some reasons someone might not seek help for their mental health issues?
- What comes to mind when you hear 'Mental Health First Aid?"
Throughout the session, we will have some polls where you can actively participate. In this process, I would like you to listen to or read any input provided in a non-judgmental way. I would also like to start exploring your experience and views as a step to start getting involved in this subject with samples. All answers are anonymous, and there are no right or wrong answers. Please be as honest as possible.
Poll 1
How prepared do you feel to support someone feeling distressed? The options are not prepared, not sure, and well prepared.
- The majority of you have described yourself as "not sure," while 28% are "well prepared," and 5% are "not all prepared."
I hope that by the end of the session, you will have more insight and awareness about this topic.
Poll 2
The second question is a practical example. If someone sent you a text message saying they were sad and wanted to get out of this world, how confident do you feel about dealing with this situation?
- Most of you responded that you are somewhat confident, 24% are not, and 4% are very confident.
Dealing with this type of text message can be quite overwhelming. Understandably, we may not feel confident dealing with this regardless if it is a professional or a personal context.
Poll 3
The third poll is an open-ended question. Based on your personal and professional experience, what are some reasons someone might not seek help for their mental health issues?
- Responses include embarrassment, stigma, pride, fear of judgment, fear of being found out by colleagues, financial issues, difficulty accessing healthcare, cost, compassion, lack of insight, insecurities, afraid of treatment options, lack of knowledge, cultural background, a sign of weakness, lack of insurance or coverage, and lack of belief.
Thanks for all of your responses.
Poll 4
What comes to mind when you think or hear the term Mental Health First Aid?
- Suicide hotline
- Intervention in Crisis
- Assistance for mental health emergencies
- Emergency conversations
- Counseling? We are going to cover this part. It is a bit different from counseling.
Let's hope that you will learn something today. People tend to associate Mental Health First Aid with Intervention in Crisis, which is included. But as we will see, Mental Health First Aid is a broader concept. We can also use Mental Health First Aid as an early intervention.
Why This Session?
- Based on WHO, about 1:8 people in the world live with a mental disorder. (1)
- According to NAMI, the average delay between the onset of mental illness symptoms and treatment is 11 years. (3)
- Based on a 2019 national poll from the American Psychiatric Association (APA), about half of workers were concerned about discussing mental health issues at their jobs. (2)
- According to Mental Health America, research shows that those with chronic pain are 4 times more likely to have depression or anxiety than those who are pain-free. (17)
- According to NAMI, 12+ million US adults had serious thoughts of suicide during the COVID-19 pandemic. (3)
Let's start by briefly exploring the scale of the problem. As I am sure you know, there is loads of research and data on mental health and the different domains covering it. I will present a few numbers and facts to give an overall picture. According to World Health Organization and before the pandemic, about one in eight people were shown to live with a mental health disorder. In all countries, mental health disorders are prevalent and largely undertreated.
In the US and according to National Alliance on Mental Illness, one in five adults experiences mental health issues each year. According to the same source, the average delay between the onset of mental illness symptoms and treatment is 11 years. We are talking about more than one decade between the onset of symptoms and seeking help.
A national poll by the American Psychiatric Association in 2019 showed that about half of the workers were concerned about discussing mental health issues at their jobs. And one of you mentioned that in the polls. They also found that more than one in three were concerned about retaliation or being fired if they sought mental healthcare. Again, this relates to the stigma that you have mentioned in the polls as well.
According to Mental Health America research, those with chronic pain are four times more likely to have depression or anxiety than those who are pain-free. They analyzed data from more than 150,000 people with arthritis and chronic pain who completed an online mental health screening between 2015 and 2019. They found that 79% of people with arthritis and other chronic pain screened positive for a moderate to severe mental health condition. Based on those numbers, I wonder how they cover and address mental well-being in their assessments because there is almost always a risk factor of having a mental health condition related to declining physical health.
Thinking about the COVID pandemic and its impact on our mental well-being, according to the National Alliance for Mental Illness, 12-plus million US adults had serious thoughts of suicide during the COVID-19 pandemic. That is a significant number.
- A recent systematic review across 65 studies involving 97,333 healthcare workers in 21 countries has identified a high prevalence of moderate depression (21.7%), anxiety (22.1%), and PTSD (21.5%) among healthcare workers during the C-19 pandemic. (4)
- In times of chaos, people are unable to perform normal activities; thus, they experience occupational disruption. (7)
- By 2030, mental health issues are predicted to be the leading cause of global mortality and morbidity. (6)
- Low health literacy is a significant problem in the US. (5)
- In 2018 in a survey to gain insight into current OTs' perceptions related to health literacy, over one-third of respondents reported having no knowledge or education on health literacy. (5)
A recent systemic review across 65 studies covering 21 countries identified a high prevalence of moderate depression, anxiety, and PTSD among healthcare workers during the COVID-19 pandemic. When healthcare workers decide to change their careers to leave healthcare, the reasons behind that are related to burnout and emotional fatigue. During pandemics, population displacement, climate emergencies, and other chaotic times, people cannot perform everyday activities. Occupational disruption has a tremendous impact on mental well-being. Current circumstances can contribute to a rise in mental health issues predicted by 2030 to be the leading cause of global mortality and mobility.
One of the key aspects of Mental Health First Aid relates to health literacy. A national assessment of adult literacy was completed in the US and published in 2006. This was the last one that was done. In that assessment, 88% of USA adults have limited health literacy. We know that patient education is a critical component of health literacy and a necessary OT intervention.
Based on research in general, patient education materials tend to be too complex for an average adult to understand. This is something to remember when we create our materials for patients so they can use and understand that information. In 2018, a survey was completed to gain insight into current OTs' perceptions related to health literacy. Over one-third of respondents reported having no knowledge or education on health literacy. In that survey, limited resources and a lack of training in health literacy were identified as barriers in practice. We know that engagement in continuing education has increased healthcare providers' health literacy awareness. That seems obvious; however, there is still a lack of opportunities. We need to bring this information back to our employers and teams.
- Mental health is everyone's business!
- OTs can assist in the creation of a more health-literate society through the development of approaches, materials, and solutions that are easy to access and understand. (5, 7)
- 'The AOTA's Societal Statement on Health Literacy explicitly calls for therapists to gain the communicative and educational skills necessary to promote clients' health self-management and participation skills, especially through the integration of health literacy-centered systems.' (8)
The high prevalence of mental health disorders increases the likelihood of any of us engaging with someone with a mental health problem, regardless of our professional background, which makes mental health everyone's business. The truth is that we do not need to be mental health professionals to be able to provide support. We can support others through our everyday interactions in terms of building their awareness and understanding of mental health by making every contact count.
This is similar to AOTA's Societal Statement on Health Literacy. It "explicitly calls for therapists to gain the communicative and educational skills necessary to promote client's health self-management and participation skills, especially through the integration of health literacy centered systems." You will see that Mental Health First Aid is aligned with this health literacy approach.
From Mental Health Literacy (MHL) to Mental Health First Aid (MHFA)
Generally, if someone breaks the leg, they go straight to the hospital, but that readiness to seek help tends not to be present when there is a mental health issue.
Health Literacy
- Several factors stop people from seeking help for mental health conditions, including (1)
- Poor quality of services,
- Low levels of health literacy in mental health, and
- Stigma and discrimination
- The WHO has identified Health Literacy as perhaps the most essential component of the social determinants of health. (9)
The truth is that several factors stop people from seeking help for mental health conditions, including poor quality of service, low levels of health literacy in mental health, and stigma and discrimination. Of course, there are many other reasons, as many of you mentioned in the poll.
The World Health Organization has identified low health literacy as, perhaps, the most essential component of the social determinants of health. The thought behind this is if the general public does not know about or is not interested in mental health issues, they are less likely to take responsibility for self-care, seek appropriate help when they are not well, or prioritize access to quality mental healthcare. Again, this is something to keep in mind for our OT practice.
In the US, there is a program called Healthy People 2030, a 10-year plan for addressing the most critical public health priorities and challenges. The Healthy People 2030 campaign defines personal health literacy as a degree to which individuals can find, understand, and use information and services to inform health-related decisions and actions for themselves or others.
- Personal Health Literacy is the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. (17)
- Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. (17)
This definition emphasizes people's ability to find, understand, and use information and services to make well-informed decisions. This incorporates the perspective of public health, where we are all called to action.
Healthy People 2030 acknowledges that this personal health literacy is contextual and that health-related services have a role in improving health literacy. They came up with this definition of organizational health literacy similar to people's health literacy but also put the responsibility on organizations.
Mental Health Literacy
- Includes 5 components: (11)
- recognition of problems and mental disorders in order to promote and facilitate help-seeking;
- knowledge of how to prevent mental disorders;
- knowledge of effective self-help strategies;
- knowledge of the professionals and available treatments;
- knowledge and skills to provide support and first aid to others.
How about mental health literacy? This concept of mental health literacy has progressed over time and currently includes five components: recognition of problems and mental health disorders in order to promote and facilitate help-seeking; knowledge of how to prevent mental health disorders; knowledge of effective self-help strategies; knowledge of the professionals and available treatments; and knowledge and skills to provide support and first aid to others. In the last poll, many things you mentioned fall into mental health literacy and Mental Health First Aid interventions. It acknowledges our crucial role in helping people with their health literacy. I want to take the liberty to suggest that you keep in mind these five elements and then reflect with your teams on what you are currently doing and what else can be done to promote each one of these components within your work with clients.
- Community mental health interventions can be categorized broadly into 3 groups: (10)
- Awareness and mental health literacy activities include mental health first aid training and the provision of information about local referral pathways.
- Prevention and promotion
- Management and rehabilitation
Community mental health interventions can be categorized into three groups. One of them is awareness and mental health literacy activities aiming to reduce the stigma and improve access to treatment. This is by improving mental health communities to identify the signs of mental ill health in themselves and others. Intervention can include activities like Mental Health First Aid awareness sessions or training and provision of information about local referral pathways. Any service can facilitate these actions. Two other mental health interventions we will not cover in this webinar are prevention and promotion and management and rehabilitation.
Mental Health
- Dual-Continua Model of Mental Health
We all have mental health with various degrees of mental well-being based on biological, psychological, and social factors. Mental health enables us to function, flourish, cope with stress, and adapt to change. It also allows us to build healthy relationships, connect with others, and support us to learn well and work productively.
There is a current view of mental health and well-being called the Dual-Continua Model of Mental Health developed by the Canadian Association of College and University Student Service and the Canadian Mental Health Association (Figure 1).
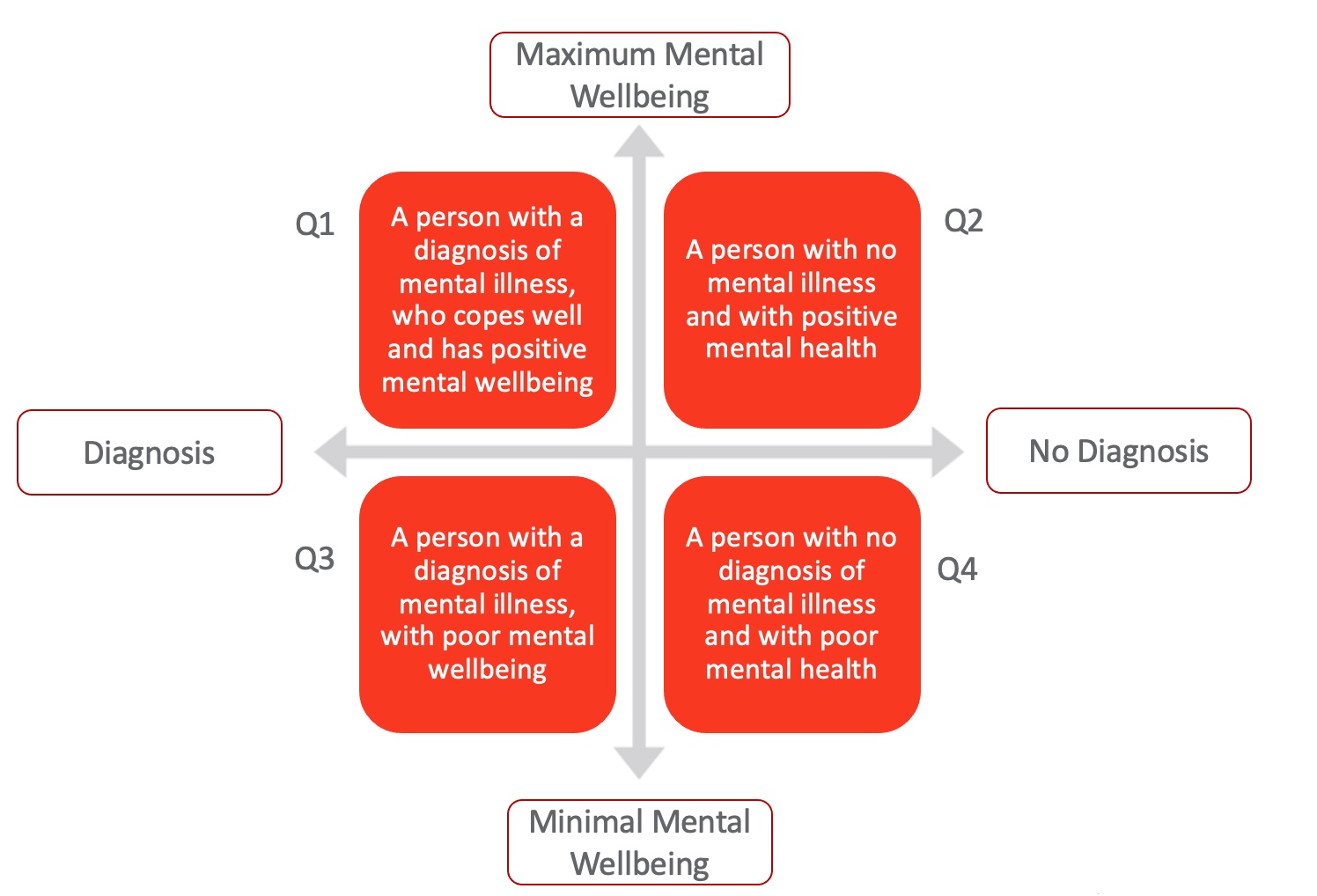
Figure 1. Dual-Continua Model of Mental Health (Dual-continuum model by CACUSS & Canadian Mental Health Association, 2013). Click here to enlarge this image.
This model integrates psychopathology and subjective well-being into a mental health continuum and is an adjustment to traditional health models. The Y axis is subjective well-being, with the top being "maximum mental well-being" and the bottom being "minimal mental well-being." When someone is at the top of this continuum, they are likely to feel full of energy and able to cope. The opposite is at the bottom of the graphic. People may struggle to cope with everyday challenges. The X-axis or the medical axis includes the words diagnosis and no diagnosis.
From there, we have four quadrants. Quadrant one is a person with a diagnosis of mental illness who copes well and has positive well-being. Quadrant two is a person with no mental illness and positive mental health. In quadrant three, there is a person with a diagnosis of mental illness with poor mental well-being. Lastly, in quadrant four, there is a person with no diagnosis of mental illness but with poor mental health.
In this model, the person within the continuum might be influenced by factors like stigma, perceptions about self, or level of insight. We may have someone resistant to seeking help but with poor mental health.
Let's move from theory to practice with a case study. I am going to read a case study. Joanna is a name that does not relate to any specific case. The case will progress across four quadrants. Throughout the presentation of the case, think about where Joanna might be in particular periods of her life.
From Theory to Practice
- Case Study- Joanna
Joanna is a 19-year-old student who is quiet and reserved but friendly enough. She has a part-time job to earn money to pay for her studies. She likes reading, listening to music, and going for long walks. Until recently, her mates thought of her as someone easygoing. Based on this description, what quadrant do you think Joanna is at this stage? (Many answered quadrant 2, which is correct.)
Her behavior changed in recent months when she suddenly lost her grandmother. She has been irritable with her colleagues, struggles to keep up to date with her assignments, and is sleeping poorly. Her flatmates are concerned when she starts isolating herself, missing classes, not answering calls, and calling in sick to work. When they spoke with her and offered help, she said she did not realize she was not doing well. At this stage, what quadrant do you guess? (Many answered quadrant four, which is correct.)
A colleague managed to visit Joanna. She notices that Joanna has scars on her arms, like little cuts. During the visit, Joanna breaks down in tears, says she does not know what to do and feels she is in a corner. They manage to get a medical appointment. Following assessment, Joanna is diagnosed with depression. At first, she struggles to accept her diagnosis and feels frustrated and angry. She often stops her medication. At this stage, what quadrants is she now? (Many answered quadrant 3, which is correct.)
As she started engaging in talking therapy services and gaining insight into her mental illness, she made good use of the available support. Joanna is now back at the university. She feels confident and motivated to finish her studies. She receives mental well-being support at school and engages with online support groups. At this stage, what quadrant do you think she is in? (Many answered quadrant 1, which is correct.),
When we talk about Mental Health First Aid, we are talking not only about intervention in crisis but also about helping people move around the continuum so they can get the help and support they need in each stage of their life. Thank you for your participation.
MHFA – What is This About?
- Central aim is to improve the Mental Health Literacy (13, 16)
- The specific aims of MHFA are to (13, 16):
- Provide help to prevent the mental health problem from becoming more serious;
- Provide comfort to a person with a mental health problem;
- Preserve life where a person may be at risk of harm;
- Promote recovery of good mental health
- Equips individuals and organizations with the skills to identify, assist, and act as a point of contact and reassurance for a person who may be developing or experiencing a mental health issue or emotional distress (13)
We can start approaching Mental Health First Aid (MHFA) intervention by paralleling with first aid or CPR, which I know many companies use in their mandatory training. In CPR training, people with no clinical background learn how to assist someone following a heart attack. Mental Health First Aid will be the equivalent to that, but with a focus on mental health. Mental Health First Aid can be applied at any point of the Dual-Continua Model.
The central aim of Mental Health First Aid is to improve mental health literacy. All of those concepts are related to increasing the knowledge around mental health and mental ill health. The aims of MHFA are to prevent the mental health problem from becoming more serious, provide comfort to a person with a mental health problem, preserve life where a person may be at risk of harm, and promote recovery of good mental health. From these specific aims, we can see that MHFA may have a different focus from prevention, intervention in crisis, and recovery support.
Basically, it is about individuals and services being equipped with the skills to identify, assist, and act as a point of contact and reassurance for a person who may be developing or experiencing a mental health issue or emotional distress. The evidence behind this intervention demonstrates that it builds mental health literacy, decreases stigmatizing attitudes, and helps individuals identify, understand, and respond to signs of mental illness.
- Relates with factors that seem to be most helpful to people's long-term. These include:
- feeling connected to others and hopeful;
- having access to support;
- feeling able to help themselves as individuals and communities (14, 15)
- MHFA: (13, 14)
- Can be integrated into our daily/work life
- Typically offered by someone in the person's social network or someone working in a public-facing role
- It is not a psychological 'intervention' or therapy.
- There is specific training available to be a qualified MHFAider. (https://www.mentalhealthfirstaid.org)
Mental Health First Aid relates to factors that seem most helpful to people's long-term recovery, including feeling connected to others and hopeful, having access to support, and feeling able to help themselves as individuals and communities. It is an approach that can be learned by both professionals and nonprofessionals who are in a position to support and help people.
MHFA can be integrated into our daily and work lives. Typically, it is offered by someone in the person's social network or someone working in a public-facing role, so we are in a position to support people in that regard.
It is not a psychological intervention or therapy. It is the first point of contact aiming to assist someone who may be struggling with mental well-being.
There is specific training available for people interested in being qualified Mental Health First Aiders. Mental Health First Aid training was created in Australia in 2001. The US is one of the many countries that have adapted the program from the original Australian program. Currently, Mental Health First Aid training in the US is managed and delivered by the Department of Mental Health.
MHFA – What Does It Involve and Include?
- MHFA can be useful in different stages: (12, 14)
- Prevention » Early Intervention » Treatment and support
- Taking practical steps to improve our mental health knowledge, understanding, and skills, including self-care, coping strategies, and knowing what to do when you notice someone who is struggling (e.g., complete MHFA training)
- Getting involved on building on safeguarding policies and procedures to promote positive workplace cultures and communities (e.g., Mental health champions)
- Making a list of all the organizations operating in your local area and how to access them (e.g. include it in the first aid kits).
Mental Health First Aid can be useful in the different stages, as we have seen. It can be an early intervention approach, or it can be helpful during treatment and support. Considering those different stages, what can we do to promote mental well-being and facilitate access to support?
Now, we will explore some examples of what can be an MHFA intervention. The first step is improving our knowledge within the context of mental health literacy, acknowledging that is the central aim of MHFA. It is about taking practical steps to improve our mental health knowledge, understanding, and skills, including self-care, coping strategies, and knowing what to do when you notice someone is struggling. You can complete an MHFA awareness session or training to become a "Mental Health First Aider."
Another way to develop MHFA interventions is by building safeguarding policies and procedures to promote positive workplace cultures and communities. For example, you can assign mental health champions in your workplace to put mental health on the agenda.
Another intervention is making a list of all the mental health organizations operating in your local area and how to access them. Many companies have first aid kits, but is there anything related to mental health crises? Perhaps you can make mental health first aid kits together for your company.
- Raise mental health literacy in the workplace/population by creating and having available easy-to-read information about mental health and mental ill health + support available » use reliable sources of info (e.g., WHO, NAMI, NIMH, etc.)
- Supporting others to feel comfortable with you and supporting others with active listening (e.g., Is there anything you'd like to share? What can I do to help you out?)
- Normalizing conversations about mental health, like including this topic in the agenda of team meetings (e.g., How are you really feeling today?)
- Checking mental well-being on a regular basis, like having this topic as no 1 of the agenda of line management meetings (e.g., Do you need some time to yourself? Did you know that you are doing an awesome job?)
Raise mental health literacy in the workplace and population by creating and having available easy-to-read information about mental health support. Again, we do not need to be specialists in mental health. Many reliable sources are available online, and some examples are listed above. You can print out their information.
You can also support others by using active listening. It is about having emotional availability to pay attention so they can trust you and reach out to discuss their issues.
Normalizing conversations about mental health, including at team meetings, is another proactive strategy. It is investing time to explore and check in on the well-being of others regularly. This is not because we have to but because there is a genuine interest in ensuring everyone's well-being.
- Helping someone who may be experiencing deterioration in mental well-being through an initial conversation to spot the early signs and symptoms of mental ill health (e.g., "I've noticed you have been missing class lately, and I am concerned about you.”)
- Offering information, encouraging and facilitating their access to appropriate professional support or self-help strategies (e.g., "If you would like, we can call together to make an appointment.”)
- Communicating any concerns about the mental health of someone to relevant services (e.g., report to line manager)
- Assessing risk to self, like self-harm behavior or suicide risk (engage in relevant training to learn how to have difficult conversations and assess risks)
- Supporting people in crisis and in risk by escalating to the appropriate emergency services, if necessary (e.g., "I am worried about your safety. I need to get support for you.”)
Here are some more examples. It is helping someone who may be experiencing a deterioration in mental well-being through an initial conversation to spot early signs and symptoms of mental ill health. The conversation can start with simple things like, "I've noticed you have been missing class lately, and I'm concerned about you." This statement can be enough to start a conversation and for someone to disclose what is going on.
We can also offer information and encourage and facilitate their access to create professional support or self-help strategies.
We can communicate any concerns about the mental health of someone to relevant services or people. For example, if you are concerned about a colleague that you do not know how to approach, maybe you can speak with your manager to decide the best steps to proceed.
Assessing risk to self, like self-harm behavior or suicidal ideation, is another strategy. As this can be a bit more complex, people might benefit from further training. We do not have time to cover this part of how to have difficult conversations and assess risks. That will be another session.
Lastly, we need to support people in crisis and at risk by escalating to appropriate emergency services if required. "I need to get help for you." It is about being assertive when there is a higher risk involved.
MHFA – Action Principles (13, 14, 15, 16)
The most recent version of the MHFA Action Plan is (13, 14, 16):
- Approach the person, assess and assist with any crisis
- Listen and communicate non-judgmentally
- Give support and information
- Encourage the person to get appropriate professional help
- Encourage other supports
The most recent version of the MHFA plan consists of these action principles, which form the acronym ALGEE. People that have completed the MHFA training will go into detail about this action plan. But today, we will cover these superficially to see what each step means and what it covers.
The first action principle is to approach the person. It is worth remembering when, where, and how to do this. It is worth exploring with a person whether it is a good time and place to start talking. The language we use should be based on what we have seen, heard, and noticed, not what we think is wrong with them. We can ask people how they are feeling and how long they have been feeling like that to introduce the conversation. At this time, assessing the risks and taking appropriate actions will be relevant. These conversations can be difficult, and I need another session to cover that part. It is about risks related to suicidal thoughts, signs of self-harm, severe signs of alcohol or drug misuse, and aggressive behavior toward other people.
The second action is listening and communicating non-judgementally. We talk about this a lot as healthcare workers. It is not easy to do active listening because our brains are programmed to assess and evaluate situations and make judgments to keep us safe. For active listening, a good reference is to have a 20/80 ratio where 80% of the time, the person should talk, and 20% of the time, we talk. Our talk will be based on asking questions, providing validation, paraphrasing, and ensuring that we understand what is being said.
Action three is to give support and information. It is not about providing professional advice about their mental health issues. Still, it is about recognizing, accepting, validating the person's feelings, and reassuring them that mental health conditions are real, common, and treatable. The earlier we can support, the better the outcomes. We can offer additional information from reliable sources if the client is amenable.
Encouraging the person to get appropriate professional help is action principle four. The support at this point relates to informing the person what options may be available. Exploring options may also help identify any barriers, resistance, or reluctance the person may experience about accessing support, such as stigma. Some people may refuse professional help, and it is their right. We have to respect that if there is no risk involved. It is good practice to keep the door open to show availability, revisit issues, and be approachable if they change their mind.
The last action point is to encourage other supports. People in recovery have found this to be a critical part of their recovery. It could be in the form of a support network that is in place already, including friends, colleagues, family, the community, and charities. Also, this action principle includes encouraging people to use self-help strategies to help them cope with mental health issues.
- Prepare – learn/know what is available, how to connect with those services, or who to ask
- Approach people who may need support
- Ask about people's needs and concerns
- Listen to understand, instead of listen to reply
- Offer and give information
- Help people connect people with formal and informal support network
- It is more likely that a person will seek help (professional, formal help) upon relying on someone's suggestion! (11)
Let's prepare, know what is available, and how to connect with those services. We never know when we will be approached by someone struggling with their mental health. Second, let's approach the person needing support and ask questions. Listen to understand instead of listening to reply. Offer and give information, and then help them to connect with the formal and informal support network. Research indicates that it is more likely that the person will seek help upon relying on someone's suggestion. We can play a key role in someone's recovery by approaching them and listening to them.
- Helping responsibly:
- Be sure that you are physically and emotionally able to help others
- Be aware of your own cultural background and beliefs so you can set aside your own biases
- Avoid putting people at further risk of harm as a result of your actions
- Offer help in ways that are most appropriate and comfortable to the people you are supporting
- Make sure people can access information and help as needed
Help in a responsible way. To be physically and emotionally able to help others, ensure your health and well-being are a priority. When looking after someone experiencing mental health issues, it can be easy to overlook our needs. Be aware of your cultural background and beliefs to set aside any biases. Avoid putting people at further risk of harm due to your actions. If in doubt and you do not feel like you are in a good state of mind, ask another person to address the issue. Offer help in the most appropriate and comfortable ways to the person you support. Please do not assume the help they may want or need. Ensure that people can access and understand information and then help as needed.
- Act on their best interests
- Know and follow your company policies and codes of conduct at all times if you work or volunteer for an agency that has these codes
- Maintaining appropriate boundaries, know your limits, and knowing when/where to refer
- Practice self-care and be aware of your own physical and emotional reactions
Always act in their best interests. Know and follow company policies and conduct codes, and maintain appropriate boundaries. Know your limits and when and where to refer. It is vital that we do not try to deal with difficult situations by ourselves, and crucial to share responsibility. So, be fully aware of what support is available within the area and that you understand the relevant policies.
As I said, sharing responsibilities and engaging with networks are crucial due to the practical demands when dealing with a challenging situation. Practice self-care and be aware of your own physical and emotional reactions. We know that supporting someone with a mental health issue can take time and emotional energy, so we must take care of ourselves. A vital part of looking after ourselves is having people talk about the situation and how it affects us. Please ensure that when you go through challenging situations, you debrief with someone you trust.
MHFA Within OT Context
- Occupational disruption & mental (ill) health
- OT role:
- Helping people regain control when facing challenging situations (7)
- WFOT – OT works with people to develop strategies to facilitate continued access to their occupations (7)
- Patients' education materials – readable and understandable
Occupational disruption temporarily disrupts a person's usual pattern of occupational performance and engagement. When people are not able to do what they want and what they need to do, this will negatively impact their help and well-being and vice versa. The World Federation of Occupational Therapy (WFOT) reminds us that our profession works with people to develop strategies to facilitate continued access to their occupations.
When you notice someone with a mental health issue, think about how you, as an OT, can help them to maintain or regain control and keep their level of engagement and participation. Please approach them, listen to them, offer information, and encourage them to seek help to prevent further mental health issues.
Health outcomes are negatively impacted by a mismatch between patient education ability and the grade level of education materials. Patient education materials that are readable and understandable are necessary to support informed health decision-making and, consequently, health outcomes. I will leave here two or three suggestions based on research to keep in mind when creating materials. Based on research, good tips are to simplify written materials with short sentences of 10 words or less; eliminate unnecessary words, active verbs, and words that can be illustrated; and pilot patient education materials with a small sample of patients from the target population.
MHFA- In Practice
I want to dedicate the last minutes of the session to some case studies.
Case Study 1
- You are providing occupational therapy session to a patient who tells you:
- "I have lost my job, my relationship has broken down, I have no money, I'm desperate need of help from the government, but they won't help me I have had enough I don't know what to do anymore"
- Regarding this client, you have noticed that recently he has not been socializing with you and other patients, as usual, being more quiet and vague, though you have always found him friendly previously. He has been arriving late to sessions, and there are unusual elements of an unkempt appearance.
- Polls
- What is the impact of this disclosure on you?
- What would you do?
You are providing occupational therapy to a patient who says, "I have lost my job. My relationship has broken down. I have no money. I'm in desperate need of help from the government, but they do not want to help me. And I have had enough. I do not know what to do anymore." You have noticed he has not been socializing with you and other patients as usual. He is also quieter and vaguer, though you always have found him friendly previously. He has been arriving late to sessions and is unkempt.
From this situation, what is the impact of this disclosure on you? What are the first thoughts that come to your mind? When talking about Mental Health First Aid, it is imperative that we acknowledge what is being impacted in ourselves before we start an intervention. What kind of emotions and thoughts cross our minds?
Answers to the poll: depression, concern, referral to psychology/social services, listening, encouraging support
People are already thinking of solutions, answering my second question, "What will you do in that situation?"
Answers to the poll: deterioration in their life, seems a bit lost, hopeless feelings, seeking additional help, non-judgemental listening, asking about the support available, do not make assumptions that they want help, do not jump straight away to solutions, taking time to listen, discuss concerns, give them available support options, informative handout, acknowledging feelings and provide listening ears
Now, we can go through the situation together. Talking with them gives them a sense of connection, which can be a protective factor. We must be genuinely willing to help them. We have to think about where and how to approach the conversation in an open gym. It is better to take the person to a more private setting.
Case Study 2
- You've started a new role as a team leader/manager
- Based on annual reports, sickness levels and employee turnover rates have been consistently increasing. When you try to explore the issue with your team, staff members are dismissive.
- Poll
- How could you foster a more open and talkative workplace and put mental health on the agenda?
Case study two is very different. You have started a new role as a team leader manager. Based on annual reports, sickness levels and employee turnover have been consistently increasing. When you try to discuss the issue with the team, staff members are dismissive. How could you foster a more open and talkative workplace and put mental health on the agenda?
Answers to the poll: work-life balance, discuss impacts of mental health on the workplace, share a personal story, lead by example, normalize mental issues, provide some education as a conversation start sessions about health and well-being, monthly communication, team building interest, weekly lunches, social elements in the workplace can also promote that mental well-being
These are excellent ideas.
Case Study 3
- You receive a message from someone you know:
- "You're free to do whatever you want, but there is no point in doing anything anymore, so it's probably best if you just give up on helping me like I've given up on life/living and move on/stop wasting time on a pathetic piece of shit like me…'
- Polls
- What are your first thoughts?
- What would you do?
The case studies that I am sharing today are all real. That was an actual text message that I received. Let's imagine that you received a message from someone you know with the following. "You are free to do whatever you want, but there is no point in doing anything anymore. It is probably best if you give up on helping me like I've given up on life/living. Stop wasting time on a pathetic piece of ... like me." What are your first thoughts? What would you do?
Answers to poll: the person is in crisis mode, needs immediate help, depressed and suicidal, struggling and sad, hopeless, need some help soon
This text message generates a lot of concern. If someone approaches you, they have something to say and trust you. We must not dismiss this. In this case, I tried to call him, and he did not answer. I then tried to engage with him via text message, and he did respond for a while but refused to give me his location. He mentioned that he was contemplating suicide by overdose. I knew he had a recent history of drug relapse and risk of becoming homeless. He was known to social care for family issues, and a history of engagement with support was available. Due to the risk and because he stopped engaging with me, I contacted emergency services to report my concerns and to request a welfare check.
Summary
Thank you so much for your participation today. When developing an MHFA intervention, it is hard to have difficult conversations. Some of us may not want to know about or deal with the issue. We might be unsure of what to say or worried that whatever we say, we will only make things worse. We might also experience different feelings, such as panic, fear, frustration, and even anger. All of these responses are understandable reactions to serious situations. Remember, we must look after our well-being to support someone in need. However, while having these feelings, it is essential not to let them and our reactions get in the way of talking openly with the person so that we can begin to understand the situation and provide support. Let's question ourselves to see if we are doing enough in terms of helping people to raise and to gain insight into mental health. I hope you found this talk helpful.
References
- World Health Organization. (2022, June 16). World Mental Health Report: Transforming mental health for all - executive summary. World Health Organization. Available at https://www.who.int/publications-detail-redirect/9789240050860
- Stigma, prejudice and discrimination against people with mental illness. Psychiatry.org - Stigma, Prejudice and Discrimination Against People with Mental Illness. (n.d.). Retrieved September 16, 2022, from https://www.psychiatry.org/patients-families/stigma-and-discrimination
- National Alliance on Mental Illness. (n.d.). Mental health by the numbers. Available at https://www.nami.org/mhstats
- Søvold, L. E., Naslund, J. A., Kousoulis, A. A., Saxena, S., Qoronfleh, M. W., Grobler, C., & Münter, L. (2021) Prioritizing the mental health and well-being of healthcare workers: An urgent global public health priority. Front Public Health, 9:679397.
- Attard, E., Vaas, K., Musallam, A., Chaney, T., Fortuna, J. K., & Williams, B. (2021). Health literacy in occupational therapy research: A scoping review. The Open Journal of Occupational Therapy, 9(4), 1-18.
- Wellcome Global Monitor & Gallup (2020). The role of science in mental health. Wellcome Global Monitor & Gallup [Internet]. Available at https://cms.wellcome.org/sites/default/files/2021-10/wellcome-global-monitor-mental-health.pdf
- Whitney, R. V., & Walsh, W. V. W. (2020). Occupational therapy's role in times of disaster: Addressing periods of occupational disruption. AOTA Publications Continuing Education Article.
- American Occupational Therapy Association. (2017). AOTA's societal statement on health literacy. American Journal of Occupational Therapy, 71(Suppl. 2)
- Kutcher S, Wei Y, Coniglio C. (2016). Mental health literacy: Past, present, and future. Can J Psychiatry, 61(3):154-8.
- World Health Organization (2018). mhGAP operations manual: mental health Gap Action Programme (mhGAP) [Internet]. Available at https://www.who.int/publications/i/item/mhgap-operations-manual
- Costa, T. F. O., Sampaio, F. M. C., Sequeira, C. A. D. C., Ribeiro, I. M. O. C., & Parola, V. S. O. (2020). Mental health first aid programs: A scoping review protocol. JBI Evid Synth. 18(9):2011-2017
- Iasiello, M., van Agteren, J., & Cochrane, E. M. (2020). Mental health and/or mental illness: A scoping review of the evidence and implications of the Dual-Continua Model of Mental Health. Evidence Base, 2020(1), 1–45. https://doi.org/10.21307/eb-2020-001
- Mental Health Commission of Canada (2020). Mental Health First Aid – Reference Guide (4th edition) [Internet]. Available at https://nabs.org/wp-content/uploads/2020/11/MHFA-Blended-PG-EN-secure-Sep-2020.pdf
- World Federation for Mental Health (2016). Dignity in mental health. Psychological and mental health first aid for all [Internet]. Available at https://www.mentalhealthconcern.org/wp-content/uploads/2016/10/WMHDReport.pdf
- World Health Organization (2011). Psychological first aid: Guide for field workers [Internet]. Available at https://www.who.int/publications/i/item/9789241548205
- Jorm, A. F., & Ross, A. M. (2018). Guidelines for the public on how to provide mental health first aid: Narrative review. BJPsych Open, 4(6):427-440
- Healthy People 2030. US Department of Health and Human Services & Office of Disease Prevention and Health Promotion. Health Literacy in Healthy People 2030. Available at https://health.gov/healthypeople
- Mental Health America. Chronic Pain and Mental Health. Available at https://www.mhanational.orgh
Citation
Nogueira, T. S. (2022). Mental health first aid awareness. OccupationalTherapy.com, Article 5549. Available at https://OccupationalTherapy.com
