Christine: Hello, and thank you for taking the time today to advance your knowledge base on the role of occupational therapy and aging in place.
Aging in Place
Aging in place is the ability to live in one's own home and community independently, safely, and comfortably, regardless of age, income, or ability level (CDC, 2013). Further, aging in place means that adults are actively seeking and engaging in daily activities both within their home and their larger community. Today, as we mentioned, our focus is on occupations and interventions. To start that conversation, we must define occupations.
Occupations
Occupations are everyday life activities that older adults want, need, and are expected to do.
What do I want to do?
What do I need to do?
What am I expected to do?
•Maintain good hygiene
Focusing on occupations is a great way to guide your intervention with them. There are many occupations that older adults may take part in. Asking 'what do you want to do" allows your client to express the occupations that are probably the most meaningful to them. Do they want to be able to take a shower by themselves? Bake cookies for their grandchildren? Or attend church service on Sunday? Each one of these occupations requires a different set of interventions to be independent. Asking them, "What do you want to do when you get home?" Or, "What do you want to do now that you are home?" This gives you a great conversation piece to start your occupational therapy treatments. This question also allows the older adult to be honest about what occupations they must complete to be successful at home. "I need to be able to use the toilet by myself." "I need to be able to prepare my own meals." "I need to get sufficient sleep at night so that I can do the things that I need to do the following day." The need part of this expresses in so many ways what responsibilities they have at home, and what you might want to prioritize in your therapy treatment. The next is what they are expected to do. This question gives you the opportunity to understand what occupations the older adult is responsible for may also lead to interventions to maintain a safe home environment. The older adult may be expected to take medications daily and on time, pay bills, and maintain good hygiene. What they are expected to do may be very different from what they want or need to be able to do.
Disability
In order to perform an intervention focusing on occupation, we must understand what disability means. Disability covers impairments, activity limitations, and participation restrictions. The International Classification of Functioning, Disability and Health, or ICF, is a classification of health and health related domains shown in Figure 1.
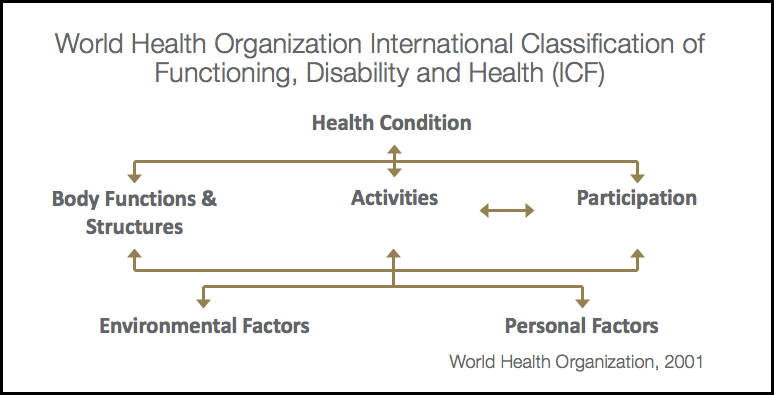
Figure 1. ICF.
The ICF measures health and disability. It acknowledges that every human may experience some level of disability in their life with a change in health or environment. It assesses the ability or inability to participate. It is important that we recognize the correlation between participation and activity. If you look at this chart, something that we want to look at is how does an activity affect participation, and vice-versa? How is participation affected if you have a disability? All of these are very important, but if we can focus in on the interactions of activity and participation while we are treating a patient, we might come up with better interventions that can assist the patient in being more independent and age at home.
Instrumental Activities of Daily Living (IADLs)
Let's first take a look at some of the instrumental activities of daily living.
Common Considerations
•Shopping
Can the patient drive? Do they use a cell phone, or do they only have a home phone? If they have a cell phone, what kind of cell phone do they use? Is it a flip phone, is it an iPhone or an Android? Do they use a computer or tablet to communicate with their families? Do they know how to do virtual things? Is the older adult responsible for paying the bills? Do they prepare their own pills on a daily, weekly, or monthly basis? Are they filling a pillbox? Do they separate their pills appropriately? You can see so many different ways that people do this. It is a very common thing that we look at, but are we looking at it in depth and following up? Who cleans the house or does the laundry? And depending on where a person lives, is their laundry in the basement, on the first, or the second floor? Do they live in an apartment? Do they have to go out of their apartment in order to do the laundry? And if they do have to do that, is it something that is on the same floor that they are already on, or do they have to use an elevator and get to another part of the building? It also depends on where their apartment is. They may have only have to walk right outside their apartment, or they may have a really long walk in order to access. Do they receive Meals on Wheels, or who prepares their meals? Do they have to cook, or do they have somebody assist them? Does a family member bring meals in? It is really important to know what meals they have to prepare and at what level. Can they dial 911? If they have an iPhone and they do not know how to use it very well, can they successfully be safe in their home and dial 911? Or can they push an alarm button? Do they wear that alarm button? Then of course, do they shop? What kind of shopping do they do? Do they do grocery shopping? Are they responsible for going out on a daily or weekly basis for their family? Or does somebody help them do that? These are some of the most common ones that we focus on.
Less Common Considerations
•Safety and emergency maintenance (Escape route for fire, replacing batteries in smoke alarm)
These are some IADLs that are a little bit less commonly considered but are just as important. Some of these are the reason why people can be successful in their own home and maintain the aging in place. Do they have a pet? Do they need to take care of that pet? Can they lean forward and feed the pet, and put the dog food out or the cat food out? Can they clean up after their pet? Can they walk that pet on a daily basis? All of these activities that are related to caring for a pet might not always be considered when you are treating a client, especially if treatment is not occuring in their home. The next one is community mobility. Many of our clients lose their ability to drive, and they feel stuck or confined to their home. Is there a bus that is close to them? If there is, can they read a bus route? Do they know how much it costs to get on the bus? Can they get a card that pays for them to be on the bus? And then most importantly, can they walk to the bus stop? Can they wait as long as it takes for the bus to get there? Can they get on and off the bus? Can they do those steps, or do they know how to ask for the bus to be lowered or an elevator portion to come up? The other piece is access. Can they call access and schedule an appointment? Can they get outside their home in order to wait for access? Many times, they have to be prepared 15 minutes prior to their appointed time. Can they stand outside or wait at a door for 15 minutes in order not to miss their appointment with the access van or bus? The other piece of that is do they qualify for it, and how to sign up for it? Can they use Uber or Lyft? This is a new and upcoming thing, and it requires technology. Can they get the app on their phone? Are they willing to put an app on their phone? Can they see what they need to see? Are they able to pay for that ride independently? The other thing is keeping scheduled appointments. Can they easily call the doctor, put it on their calendar, and then plan for the transportation that it takes to get there? Are they able to write it on the calendar at home? Do they use their phone? How are they reminded that they have an upcoming appointment? We also have to take into account that they need to refill their prescriptions, usually monthly. What pharmacy do they use? Do they get reminders? Do they know when their prescription is out of refills and that they have to call the doctor? This might require them to go into the doctor's office. Can they process all of that? For their diet, can the person follow a diabetic or heart healthy diet? Can they read the labels on a product? Do they know what they are looking for? Do they know how to break down whether there is too much sodium, carbohydrates, or sugar in something that they are preparing? Especially if they are grocery shopping, we need to help them know what to look for when they go into a grocery store. It is also educating them if they are not going to the grocery store on what they need to tell somebody else to buy them. Lots of people want to help, but they may not be making them meals that are healthy for them and following a diet that they have been instructed to use. Another big piece of living at home is home management. Do they know where the fuse box is? Can they get to the fuse box? Can they change a light bulb? Who would they call if they needed a light bulb to be changed? This is something that definitely increases their risk of falling when there is not proper light in the home. As in the introduction, I am from Pittsburgh, and it is currently snowing. Snow removal is a big issue in our area. How are they safely going to get out of their home with ice and snow on the steps or on their sidewalk? Do they need to hire somebody to do that even for a short term, or is there a way that they are successfully able to do this? Can they fix a toilet that is leaking, or shut off the water valve? All of those things take a patient bending over, standing up, and having good balance. We need to be addressing these things in the home, and if you are not in the home, you may have to look at that when they are home. We also want to look at safety and emergency maintenance. It is so important that our patients have an escape route and that they know how to get to the nearest exit either in their home or in their apartment. If they cannot get up quickly from a chair or they cannot walk very fast, we need to work on those things. We also want them to be able to change the batteries in a smoke alarm. If they cannot do it, who will help them do those things? Once again, I think that these are some of the IADLs that are overlooked. It is important that we focus on the big picture, and that we are asking the right questions to help the older adult attempt to age in place.
Activities of Daily Living
We are all pretty familiar with activities of daily living. I think that sometimes we miss asking the right questions like whether a client has a disability or has exhibited trouble with these things prior to us seeing them for therapy.
•Personal hygiene
One thing that we probably do not look as much is functional mobility. Most people have difficulty with their mobility in their house or their apartment. This seems to be a recurring theme which leads to deficits in other areas. Now, if a patient that has problems walking in their home may not always want to then take a shower or a bath. It may be difficult for them to stand up for an increased amount of time to sponge bathe, or they may have a fear of getting into the shower because, by the time they get into the bathroom, they are short of breath, tired, or weak. I think focusing on the ability that they have and seeing how long they can do those things like standing or walking can help you gain a little bit more knowledge into what they are able and not able to do when it comes to bathing or showering, or even toileting. Balance also comes into play. Many components occur during toileting, completing toilet hygiene, or pulling up pants. I think that we need to look at the big picture to see what they are able and not able to do, and try to help them to become more safe and independent in that area. If a patient has a lot of endurance issues, it also might be hard for them to eat. It is hard to chew, swallow, and catch one's breath all at the same time.
Community and Social Participation
As we talked about earlier, it is important to know what an older adult wants to be able to do. Volunteering is one of these activities that a lot of people take pride in. It can be a social activity. We want to make sure that we are asking them what types of things they do outside of their home. What other types of things do they do for socialization? Are they part of a community? Do they go to a senior center on a consistent basis? This can help with their socialization. They can get meals there and participate in exercise and/or community events. When you are them about what they do outside of their home, find out what they do at those places to make the occupations that you are focusing on in your intervention more meaningful. Do they make the Thanksgiving dinner for their family? Is it near a holiday? Or do they invite their family over every week to have a big meal? What do they do with their peers?
