Laura: I really enjoy presenting on this platform, and I think it is great that we have practitioners from all over joining us today. I am excited to have another opportunity to discuss this population. Working with this population motivated me to improve myself as a therapist. Survivorship rates are on the rise, and we all need to know how to work with these fragile patients. You should leave today's course being able to identify common pediatric cancer diagnoses as well as other non-malignant conditions that may warrant stem cell transplantation. I also want you to better understand what stem cell transplantation involves, the process as well as the potential side effects across the entire continuum of care. You should be able to select appropriate tools and interventions to implement during your occupational therapy practice.
Introduction
I would like to start by giving a quick overview of different types of pediatric cancer.
Types of Pediatric Cancer
I think most people commonly associate bone marrow transplantation or stem cell transplantation with the treatment of different types of blood cancers. I would like to give a quick overview of exactly how many individuals that we are seeing, and then go over conditions that people may not be as familiar with unless they work in a cancer specialty institution or clinic.
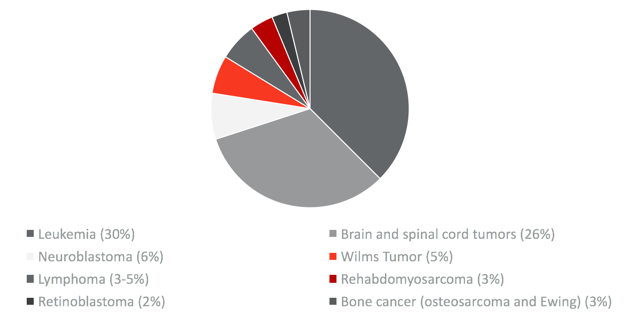
Figure 1. Types of pediatric cancers (ACS, 2016).
Leukemia is the most common type of pediatric cancer. I want to highlight three of the main types today. We are not going to get into detailed specifics on a cellular level, but it is important to understand these three common types. Leukemia makes up about 30% of pediatric cancer. Acute lymphoblastic leukemia, ALL, is the most common which makes up 80% of all pediatric leukemia diagnoses. Acute myelogenous leukemia, AML, is the second most common, and then CML, or chronic myelogenous leukemia, is the third most common among pediatric clients.
The second most common type of pediatric cancer are those of the central nervous system, so the brain and spinal cord tumors are the second most common. They make up about 26% of pediatric cancers. They may be initially present with headaches or vision changes, decreased coordination, and speech changes. Those are just some of the subtle signs of potential CNS-type tumors. Neuroblastoma is most common in younger children, most commonly diagnosed in children 1 to 2 years old. It is not very common to see this in older children. It is especially important to understand that, in over half of the children who are diagnosed with neuroblastoma, about half of them have some type of bony involvement. Thus, the primary disease can really be present anywhere in the body along the nervous system. It is most common throughout the abdominal and thoracic cavity, but it is frequently spread to the bone. This is important for our practice because that individual may have a change or restriction in their weight-bearing status. Mobility and weight-bearing can be a little tricky to navigate in younger children, especially for those who have not achieved their gross motor milestones and are learning to crawl, shift their weight, and transition from sit to stand from the ground. Wilms tumor makes up about 5%. This is cancer of the kidney in young children. Symptoms include abdominal swelling, fever, pain, and nausea. Unfortunately, these symptoms often go undiagnosed or misdiagnosed as something else or even a non-malignant condition.
There are multiple types of lymphoma. These are conditions related to blood and blood production. Rhabdomyosarcoma is a rare disease of muscle tissue. This is another type that can be present anywhere throughout the body, and it is more common in younger children. Retinoblastoma is cancer of the eye. It is usually identified because the eye looks a little bit different and the pupil has a white or pinkish color behind it. They may also have vision changes. Bone cancers include osteosarcoma and Ewing's sarcoma. Both of which are very rare and occur in the long bones. It is not uncommon for an adolescent-aged individual to experience some type of sports injury that just does not heal. After a scan, this is how this type of cancer may be diagnosed. For many of these conditions, a bone marrow transplant or stem cell transplant is appropriate.
Commonly Treated
- Leukemia
- Lymphoma
- Myelodysplastic Syndrome (MDS)
- Myelofibrosis
- Multiple myelomas (cancer of plasma cells)
(www.bethematch.org, 2019)
I mentioned leukemia and lymphoma above. I also want to discuss other types of conditions that are not in the category of malignancy. Myelodysplastic syndrome (MDS) is a blood-forming disease or condition that is also related to blood production like leukemia and lymphoma. Myelofibrosis is another type of cancer of the bone marrow, and then multiple myeloma is a malignancy of plasma cells. The bottom three of this list are more common in adults, but I think it is helpful to list them here for people trying to understand the reasons why stem cell transplants can be used for treatment.
Usually, bone marrow transplants are performed in the acute care setting in a pediatric specialty or cancer specialty institution. Different websites have registries available. You can search the type and age of client you are interested in learning about, the opportunities for them to be treated for a bone marrow transplant, and it can give you a pretty specific list about which services are provided in each state.
Non-malignant Conditions
These are other conditions that may require bone marrow or stem cell transplantation.
- Severe aplastic anemia
- Fanconi’s anemia
- Paroxysmal Nocturnal Hemoglobinuria (PNH)
- Sickle cell disease
- Thalassemia
- Wiskott-Aldrich Syndrome (WAS)
- Severe Combined Immunodeficiency Syndrome (SCIDS)
Severe aplastic anemia is a condition of the bone marrow where the body does not produce enough blood cells for physiological purposes. Fanconi's anemia is just a rare type of anemia that is in a similar category to PNH. Sickle cell disease and thalassemia are related to poorly functioning red blood cells. And then, Wiskott-Aldrich syndrome or WAS is an inherited condition that children are born with. WAS is related to a weak immune system from birth. Replacement of that immune system can be done by bone marrow transplant or stem cell transplant.
I want to take a minute and expand on severe combined immune deficiency syndrome (SCIDS). This is what a lot of people refer to as Bubble Boy disease. These infants are born without an immune system, and from birth, they are very prone to infection and complications. In some states, pediatricians are starting to automatically recommend this screening for this after birth as part of the standard newborn screening. The reason for that is because treatment with a bone marrow transplant or stem cell transplant has been proven to be more effective the younger the child is. Thus, it is critical that these children are screened early because the evidence supports that their survival rates are better the earlier the treatment.
Statistics
I also want to share just a few statistics.
- In 2015, approx. 429,000 childhood cancer survivors lived in the US (SEER Cancer Statistics Review 1975-2015; cancer.gov/childhood)
- In 2018, approx. 10,590 new cases were diagnosed among children birth – 14 years (NCI, 2018)
- According to the NCI, approx. 1,180 children were expected to die in 2018
- Survival rates have dramatically improved over the last 30 years
Some of these are about childhood cancer in general, and later on, I will share some statistics specific to stem cell transplantation. In 2015, there were approximately 429,000 childhood cancer survivors in the US. They estimated close to 11,000 new cases were expected to be diagnosed this past year in children under 14 years of age, and according to the National Cancer Institute, around 1,200 of those children were expected to die last year. It will be interesting to see when the new information is published to see if the actual number was close to that. I bring this up because survival rates are dramatically improving if you look at the trajectory over the last 30 years. Back in the '70s, the survival rate was about 58%. This number is referring to pediatric cancer as a whole. Of course, this number is going to look different depending on the type of cancer. Today, they estimate that the overall survival rate is over 83% and growing. This is one of the many reasons I want to talk to you today about the more sophisticated treatments available that are helping there individuals survive. The problem is that there are long-term side effects, so I want to highlight some of those today as well.
Pediatric Cancer Treatment and Stem Cell Transplantation (SCT)
Let's now talk about pediatric cancer treatment and stem cell transplantation specifically. I think most of us are probably familiar with what these approaches are so I am just going to highlight these briefly. And of course, we are going to focus on stem cell transplantation. However, it is important to understand the other treatments these individuals are receiving at the same time because those side effects are so dramatic when combined with stem cell transplantation.
Treatments
- Surgery
- Radiation
- Chemotherapy
- Immunotherapy
- Stem cell transplantation (SCT)
Surgery is often needed to remove solid tumors, and it is also used to place things like G-tubes or different central lines and ports in order to provide medications or nutrition, if necessary. We think about radiation in two main broad categories, and there are many different types among those, but those two are an internal and external beam. The nice thing about radiation is to treat a very small localized area of disease. The problem is that healthy tissue can be affected, and the margins can be pretty significant. Side effects like radiation fibrosis can be an issue, as well as, soft tissue changes and hardening of skin that can have later functional implications. Radiation is usually combined with some type of chemotherapy. If we are going to consider something like a gold standard for cancer treatment, chemotherapy is it. It could be administered in many different ways: intravenously, directly into the spinal column, or via a peripheral IV. It can also go straight into some type of metal port or central line. And, it can be taken orally as a pill. There are many different types of chemo. It is important to understand why a patient is getting chemotherapy, and that may be dependent on where they are in their care. Were they just diagnosed and is the goal to cure the disease or are they at end stages and is the goal really to improve their comfort? Chemo may be used to stop disease growth, cure cancer, prevent the further metastatic disease from growing, or simply to ease the symptoms. Immunotherapy is also common, especially in the individuals we will talk about today. Immunotherapy is designed to help an individual boost their own immune system to independently fight cancer and different conditions. Finally, there is stem cell transplantation, which is what our focus will be today.
Other Team Members
- Pediatric oncologist
- Pediatric surgeons
- Radiation oncologists
- Pediatric oncology nurses
- NPs and PAs
I want to highlight other individuals on the team that we interact with to determine an appropriate occupational therapy plan of care. We will most likely receive our referrals from these practitioners as well. The pediatric oncologist usually oversees each team. In the event someone receives a bone marrow transplant, in my experience, there has always been a specific bone marrow transplant team on the pediatric floor. It is a specialty within a specialty. We frequently reach out to pediatric surgeons directly, especially if a child has had distal bony metastatic disease resected. They may have changes in weight-bearing status or have a central line placed that may cause them to have activity restrictions specific to that. Radiation oncologists can help us to understand the disease process and exactly what area is being treated. Pediatric oncology nurses are just incredible. I miss working with them. They are critical in helping us to promote occupational performance and the engagement of our clients. We work closely with them to understand our client. The kids are on so much medication so the pediatric oncology nurses are really helpful for coordinating schedules and timing sessions to allow the children to get the most out of therapy. They can also help us to decrease the number of lines and tubes that we are working with during therapy. Nurse practitioners and physician assistants will also be important members of the team on which we work.
Stem Cell Transplantation (SCT)
Now that we have talked about other treatments, let's take a step back and talk about what bone marrow is. A more familiar term to many people is bone marrow transplantation. Bone marrow is the spongy material located typically in the long bones responsible for stem cell production. Stem cells eventually grow into productive blood for our system. I mentioned the conditions before as they are specific to blood production. Depending on what the needs of the individual may be for the purposes of a transplant, cells may be taken from peripheral blood or from the bone marrow, specifically. In general, stem cell transplantations do not fight cancer directly. They are used more as a protective mechanism if the individual's immune system is weak. They are usually performed to help strengthen the body's ability to produce healthy stem cells to fight after getting some of those intensive and toxic types of treatments, like radiation and chemotherapy. They may also be necessary after someone has received treatment for another primary tumor, like neuroblastoma. Cancer treatment can be intense as the immune system is completely destroyed so it may be required after someone has received certain types of cancer treatment. I was excited for the opportunity to dig a little bit deeper as I prepared for this presentation, and I want to get into the history of stem-cell transplant a bit because it is such a complex, sophisticated procedure.
SCT History
It has been in the works for many years. Even as far back as ancient times, the idea and thought of replacing an unhealthy part of the body or system of the body with healthy organs or healthy parts is an idea that has been around as long as medicine. So, this is not a new idea, but it was first documented by the American Medical Association back in 1896.
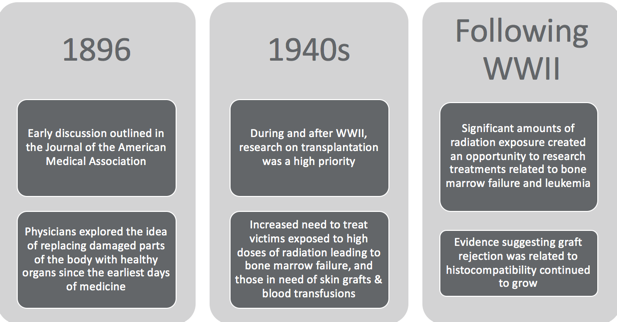
Figure 2. SCT timeline. (de la Morena & Gatti, 2011)
There were early discussions of bone marrow transplantation and transplantation of other organs as well. Around World War II, the opportunity to study it emerged quickly, and that is, unfortunately, the result of a significant amount of radiation exposure. It was a high priority to understand how to treat individuals who had experienced burns, needed skin grafts or required blood transfusions. These clients had been exposed to radiation which led to bone marrow failure. There was an acute need to better understand the process and opportunities of transplantation.
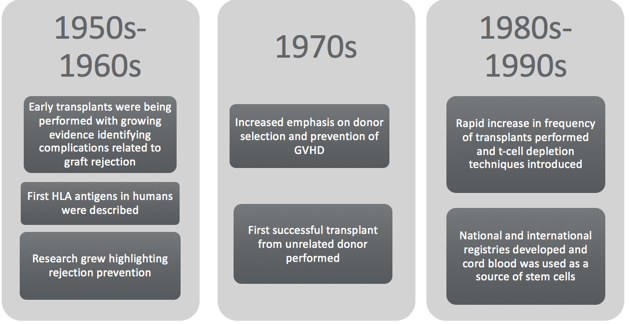
Figure 3. SCT timeline continued. (de la Morena & Gatti, 2011; MSKCC, 2019)
