Introduction
It's wonderful to be with you all here on this Tuesday afternoon and today we're going to talk about multiple sclerosis and occupational therapy treatment for this disorder.
Multiple Sclerosis Pathophysiology
- Inflammatory disorder of the central nervous system and optic nerves (Preissner, Arbesman, & Lieberman, 2016).
- Associated with damage to myelin sheaths and the axons of nerve cells
- Myelin is a protein and lipid-based insulating sheath that covers nerve fibers
- Myelin increases the speed of action potentials as they travel through and across neurons.
Multiple sclerosis is a disorder of the brain, spinal cord, and optic nerve that can cause occupational impairments for ADL, IADL work, leisure, and social activities. The disorder is caused by the degrading of myelin protective sheath which acts as a protective and insulating barrier around the axons of neurons. Myelin is made of a fatty lipid-based substance that has multiple functions. One, it protects the axons of neurons, and two, it increases the speed of action potentials or nerve conduction as impulses move across the axon. The myelin sheath has openings called nodes of Ranvier. These openings or gaps leave the axon uncovered and allow for action potentials by way of the sodium-potassium pumps to drive and move nerve conduction quickly across cells. These openings are strategically placed in the myelin to make the nerves conduct impulses even faster. Thus, it allows the sharing of information between neurons to happen even faster. Myelin sheaths are created and maintained by cells called the oligodendrocyte glial cells. These cells are very similar to Schwann cells in the peripheral nervous system; however, the oligodendrocytes are only found in the brain and spinal cord in the central nervous system.
Multiple Sclerosis Incidence
- 135 in 10,000 U.S. residents have MS
- 200 diagnosed per week
- Effects approximately 2.8 million worldwide
- More common in countries further from the equator
- Most are diagnosed between 20 and 40 years old
(Yu & Mathiowez, 2014a; Multiple Sclerosis International Federation, 2020)
This slide provides some information on the incidence and occurrence of multiple sclerosis in the United States worldwide. It is a fairly rare disease with only 135 per 10,000 U.S. residents having it. It is diagnosed at a rate of about 200 patients per week, and worldwide it affects approximately 2.8 million people. It is more common in countries that are further from the equator. The further north or south you get from the equator, the greater incidence of the disease. Most people are diagnosed between the ages of 20 and 40 years old.
Multiple Sclerosis Causes
- Auto-immune disorder in which the immune system attacks myelin sheaths
- Genetic Factors
- 2% chance of a child developing MS when a parent has MS
- 20-30% chance of developing MS if an identical twin has the disease
- Linked to specific genes that influence components of the immune system.
- Environmental Factors
- Smoking
- Epstein Barr Virus
(Multiple Sclerosis International Federation, 2020)
You will remember at the beginning of the lecture I referred to multiple sclerosis as being an inflammatory disorder. It is an inflammatory disorder caused by an autoimmune response in which the body's own immune system attacks the myelin sheaths. This results in nerve damage which disrupts communication between the brain and the body along with slowing down nerve impulses across all neurons. There are genetic and environmental factors that have been linked to multiple sclerosis, but the cause of the disease is unknown. You can see that there is a small percent chance of a child developing MS when the parent has the disease. It is also more prevalent among identical twins. There have been specific genes that are linked to developing MS, and these specific genes do influence components of the immune system. Other non-genetic environmental factors are smoking and virus exposure specifically the Epstein-Barr virus. Epstein-Barr is a very common virus that is also called human herpesvirus 4 which is also linked to Hodgkin's lymphoma among other disorders. Another factor associated with MS is excessive stress and anxiety.
Symptoms
- Extreme Fatigue
- Weakness
- Paresthesia
- Spasticity
- Bowel and Bladder Changes
- Visual Disturbances
***Significant Impact on participation and performance in meaningful activities (Preissner, Arbesman, Lieberman, 2016)
The symptoms of MS include extreme fatigue, weakness, paresthesia, spasticity, bowel and bladder changes, and visual disturbances. One symptom not listed on this slide that we will talk about in an upcoming slide is cognitive impairments. As occupational therapists, you can see how this would have a significant impact on participation and performance in meaningful activities.
Anatomy
Central Nervous System
This is a normal working central nervous system and motor tracks in Figure 1.
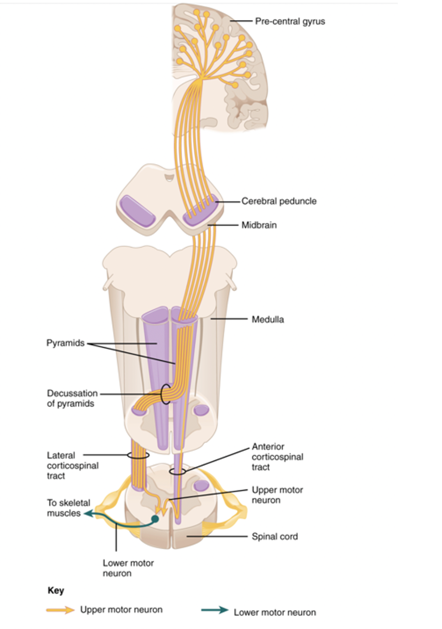
Figure 1. Central nervous system. (OpenStax College / CC BY (https://creativecommons.org/licenses/by/3.0))
The yellowish colored tracks that you see are all part of the central nervous system. Here we see the prefrontal gyrus posterior and the primary motor cortex of the brain. Motor nerve fibers travel down through the cerebral peduncles in the midbrain through the medulla and brainstem. The pyramid tracks continue to carry nerve impulses down the brainstem and into the spinal cord. Before entering the spinal cord, the motor tracks cross over to the opposite side of the body at the decussation of pyramids. The lateral cortical spinal tract is the largest primary motor tract for the somatic motor system and controls most voluntary movement to the limbs. The anterior cortical spinal tract controls the movement of the trunk. Ultimately, both of these motor tracts terminate into the lower motor neurons which are the nerves that innervate the muscles all over the body.
Myelin Sheath
Figure 2 is an illustration of the myelin sheath, nodes of Ranvier, and the oligodendrocyte.
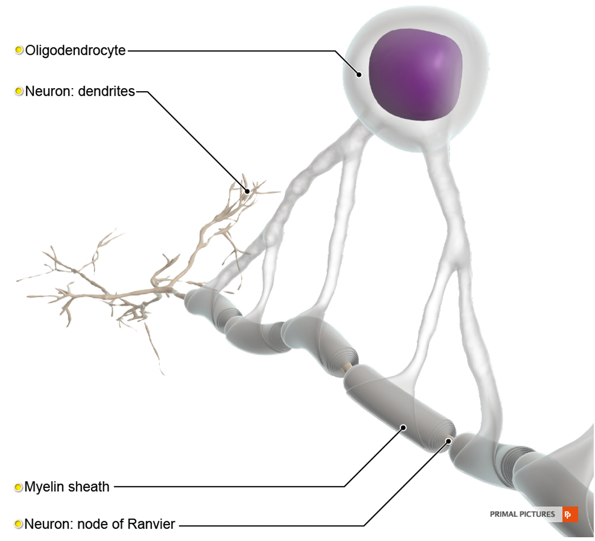
Figure 2. Normal myelin sheath.
The oligodendrocyte creates and maintains the myelin sheath. You can see the gaps in the myelin sheath where the nerve impulses are driven and transferred across the axon by the sodium-potassium pumps. The sodium-potassium pumps are not listed, but this is what I mean by the nodes of Ranvier. These are the little separations specifically placed in the myelin sheath. The myelin which is like insulation around an electrical wire and underneath the fatty tissue is the axon of the cell. The oligodendrocyte creates and maintains the myelin sheathing around neurons. Figure 3 illustrates what happens when the myelin sheath and the oligodendrocyte are damaged.
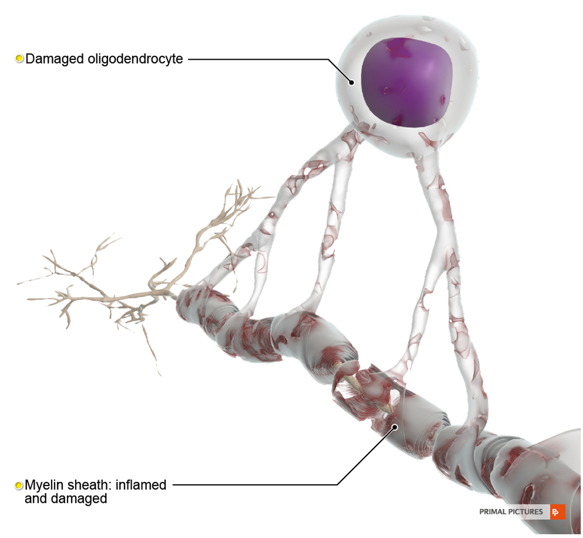
Figure 3. Damaged myelin sheath.
The axon of the nerve is exposed disrupting and slowing the nerve signal. The nerve signals can no longer jump from node to node. Figure 4 illustrates further destruction of the myelin sheath further exposing the axon.
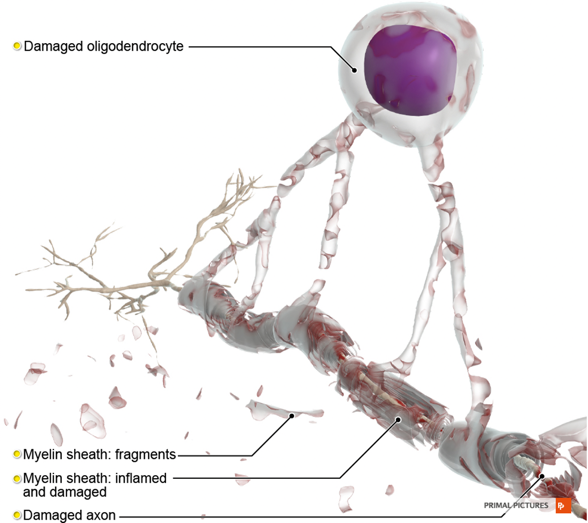
Figure 4. Further damage to the myelin sheath.
The axon loses its protective barrier and is exposed resulting in nerve death. The oligodendrocyte is damaged, and it cannot keep up with the task of reapplying the myelin sheath. In fact, as the oligodendrocyte continues to try to reapply myelin, it often does so in the form of scar tissue that is not optimal for nerve functioning.
Dorsal Column System and Spinothalamic Tract
This slide illustrates the dorsal column system and the spinothalamic tract (Figure 5).
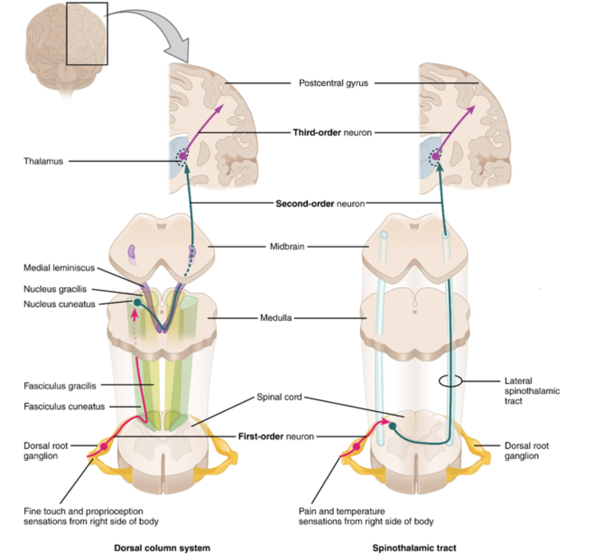
Figure 5. Dorsal column system and spinothalamic tract (OpenStax College / CC BY https://creativecommons.org/licenses/by/3.0).
The dorsal column system is a sensory pathway by which fine touch, vibration, pressure, two-point discrimination, and proprioception from the skin and the joints travel up the spinal cord to the thalamus. The thalamus is a sensory processing network in the midbrain that relays motor and sensory signals to the cerebral cortex. The collection of neurons in the thalamus act like a gate that sends information to the correct portion of the brain to process, interpret, and inform decision making. Remember though, the brain functions as one organ that initiates responses and behaviors based on the information it receives from the body in the form of billions of nerve signals. Decision making includes how to plan motor, behavior, and verbal responses to the information received. The spinothalamic tract is an ascending neural pathway that transmits important sensory information including pain, temperature, and crude touch to the somatosensory region of the thalamus. When we think about the previous slides and the myelin deterioration, what do we think about the motor and sensory information ascending and descending the spinal cord to inform the brain? How does this information inform sensory-motor function behavior and emotion? I am sure you can imagine the effects that the demyelination would have on occupational performance.
Signs of MS- Upper Motor Neuron (UMN)
- Spasticity
- Occurs due to lesions in the UMN of the primary motor cortex (PMC)
- PMC is responsible for voluntary and purposeful excitation and inhibition of LMN –resulting in coordinated muscle contractions and functional movement
- Degeneration of neurons in the PMC causes loss of control of LMN
- Causes difficulty with ambulation, ADL, and IADL (Ashworth, Satkunam, & Deforge, 2006).
I want to specifically look at spasticity as a sign of MS. Spasticity is velocity-dependent resistance during the passive stretch of muscles. Spasticity occurs in MS due to the demyelination of neurons in the primary motor cortex. The primary motor cortex is responsible for voluntary and purposeful excitation and inhibition of lower motor neurons resulting in coordinated muscle contractions needed for the production of functional movement. With the loss of the primary motor cortex, the ability to inhibit and control the lower motor neurons causes increased activity and a constant state of contraction in skeletal muscles. Spasticity can cause difficulty with ambulation, and completion of ADL and IADL. Spasticity can be managed through prolonged passive stretching to lengthen muscle fibers. Additionally, splinting and casting can be used along with bracing to maintain motion and flexibility of the joint. Baclofen is a common injectable or oral medication used to reduce spasticity. If you have treated or are treating a patient with MS, these are some of the basic things to start with to maintain joint flexibility and to decrease spasticity.
Modified Ashworth Scale
- 0 – No Increase in muscle tone
- 1 – Slight increase in muscle tone, manifested by a catch or by minimal resistance at the end of the range of motion (ROM), when the affected part(s) is moved in flexion or extension.
- 1+ – Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (less than half) of the ROM.
- 2 – More marked increase in muscle tone through most of the ROM, but affected part(s) are easily moved
- 3 – Considerable increase in muscle tone and passive movement is difficult
- 4 – Affected part(s) are rigid in flexion or extension
- 9 – Unable to test
The Modified Ashworth Scale is a way to assess and measure the degree of spasticity in patients with upper motor neuron disease. If you look at the Modified Ashworth Scale, zero would be no increase in muscle tone (completely normal). A one would just be a slight increase in muscle tone. You would support the client's elbow and do a quick stretch on it. You may feel normal resistance to the stretch, but then at the end range, like 160 degrees of extension, you might feel a catch followed by a release of the muscle at that point. One plus would be a slight increase in muscle tone manifested by the catch and release then followed by minimal resistance throughout the remainder of the ROM, less than half. Thus, you might feel the catch and release at 110 degrees of extension and a little bit more moderate resistance throughout the rest of the range of motion. Nonetheless, you would be able to achieve 180 degrees of extension at the elbow joint in our example. A score of two would be a more marked increase in muscle tone throughout most of the range of motion but affected body parts move easily. Going back to the elbow again, you would feel more resistance throughout the range of motion (more than half even at the beginning stages) for a score of two. A three would be more muscle tone and passive movement would be very difficult. You might have to apply your passive stretch for a much longer period of time to achieve a full range of motion. Then, if you had a score of four, the affected body parts would be rigid, and you would not be able to achieve full range of motion. The client may even have beginning contractures. You would score the patient at nine if for some reason you were unable to test that joint due to pain or some other reason like an inability to position them correctly.
Types of MS
- Relapsing-Remitting MS
- Unpredictable
- Attacks followed by periods of remission
- Primary-Progressive MS
- The steady and ongoing deterioration of function
- Secondary Progressive MS
- Initial relapsing-remitting followed by primary progressive.
- Progressive-Relapsing MS
- Periods of acute attacks followed by a steady decline in function
(NationalMSSociety.org)
Multiple sclerosis has different types. Relapsing-remitting MS is one type of disease where patients experience attacks for varying periods of time, but then it is followed by periods of remission. Basically, the patient experiences an acute demyelination phase followed by remyelination and repair of this protective sheathing. During the remyelination phase or remission phase, the oligodendrocyte reapplies myelin. The issue is that each time there is an attack, during the remission phase, the oligodendrocytes' ability to correctly apply the myelin diminishes. As the nerve becomes more and more damaged, the nerve becomes more and more damaged. Each remission results in a diminishing return a function so they go through a constant state of decline in function. While they do gain back some function as they go into remission, they are not quite as well off as they were during the previous remission. Each time the gains are less and less. Primary progressive MS is a type of MS without remission. It is a steady and ongoing deterioration of function. Secondary progressive MS is initially relapsing-remitting followed by primary progressive. Initially, the patient experiences attacks followed by periods of remission but then moves into more of the steady and ongoing deterioration of function and MS symptoms. Finally, progressive relapsing MS is described as periods of acute attacks followed by a slower and steady decline in function. These patients initially decline quickly but then start to decline at a slower rate.
Diagnosis
- McDonald Criteria
- Combination of Magnetic Resonance Imaging (MRI) scans in conjunction with clinical evaluation.
- Evidence of damage to the CNS and optic nerves
- Damage occurs at different times
- Damage on two or more parts of the CNS and or optic nerves
- Evidence of damage to the CNS and optic nerves
- Combination of Magnetic Resonance Imaging (MRI) scans in conjunction with clinical evaluation.
The McDonald criteria use a combination of magnetic resonance imaging scans in conjunction with a clinical evaluation to diagnose. In order to diagnose MS, there needs to be evidence of damage to the central nervous system and/or optic nerve, and the damage must occur at different times in two or more areas. Also, the damage cannot be explained by any other neuropathology process. If you want more information on this, I encourage you to do a literature search on McDonald's criteria and what that entails.
Research
Now, we are going to talk about the efficacy of OT interventions for patients who have MS. There are two really great systematic reviews in the American Journal of Occupational Therapy that I am going to talk about first. They investigate the efficacy of occupational therapy-based interventions but not specific to the discipline of OT. This means that in most of these studies, as you would imagine, OTs did not exclusively provide the interventions. However, most of the interventions were done in a rehab type of setting, and it was inclusive of occupational therapy in addition to other disciplines like physical therapy, speech therapy, social work, and nursing. These studies used a multi-disciplinary approach. Both reviews were completed by the same authors, and they did two back-to-back reviews.
Efficacy of Activity and Participation Based Interventions (Yu & Mathiowetz, 2014a)
- Systematic Review
- Activity and participation-based interventions not specific to the discipline of occupational therapy
- Many articles focused on multi-disciplinary care in various rehab settings
The first of the reviews explored activities and participation-based interventions. Many of the articles, as I mentioned, focused on multidisciplinary care in rehab settings.
- Moderate to strong evidence for rehabilitation programs improving:
- Motor function
- Self-perceived quality of life
- MS-related disability
- Mobility
- Transfers
- Arm and hand dexterity
- Balance
- Walking speed
- Fatigue management
The authors found moderate to strong evidence for rehabilitation programs including interventions focused on improving activity and participation. Outcomes that did involve occupational therapy were shown to have positive effects on motor function, self-perceived quality of life, MS-related disability, mobility, transfers, and arm-in-hand dexterity along with balance, walking speed, and fatigue management.
- More research is needed to determine the dosage, intensity, and length of the benefit of the various interventions
- The studies were inconclusive of the contribution of OT services on the outcomes.
- Most studies were multi-disciplinary
- However, the researchers found strong evidence for fatigue management courses as an intervention, which is well within the OT scope of practice.
The study concluded that more research is necessary to determine the dosage, intensity, and length of the benefit of the various interventions. And, the studies were inconclusive of the contribution of OT services on the outcomes being that most studies use a multidisciplinary approach. I think we all agree that multidisciplinary care is required not only for patients with MS but for all of our patients. However, we as occupational therapists need to focus more research and energy to identify specific evidence-based OT interventions for this population. I will point out that the fatigue management programs that were used in this study did show strong evidence for efficacy. This type of intervention is well within the OT scope of practice and used in most OT programs.
Efficacy of OT Interventions Focused on Client Factors (Yu & Mathiowetz, 2014b)
- Systematic Review
- Interventions aimed at the impairment level (i.e., client factors and performance skills)
- Interventions were broken down into studies focused on:
- Mental Functions (including cognition)
- Emotional Regulation
- Motor and Praxis Skills (including exercise)
- Motor Training
This is the second part of the systematic review published in a second AJOT article. This review looked at the efficacy of OT related interventions aimed at the impairment level. For example, it may be client-related factors such as strength, cognitive abilities, activity tolerance, and vision. This review categorized all of the studies into mental functions, emotional regulation, motor and praxis, and then motor training. It looked at the effectiveness of client-centered interventions in these specific categories.
- Moderate evidence from high-quality studies supports the effectiveness of computerized cognitive training programs
- Moderate evidence from medium quality studies supports the effectiveness of memory training
- Self-generated recall strategies
- Strong evidence from high-quality studies for interventions targeting emotional regulation
- Cognitive Behavioral Therapy
The review found moderate evidence that supports the efficacy of computerized cognitive training programs. In particular, these computerized cognitive training programs involved intensive activities where patients use sustained, alternating, and divided attention information processing and executive functioning skills. The studies were mostly focused on relapsing-remitting MS in patients with lower levels of disability. For example, one double-blind control study by Flavia and colleagues (2010) used patients with an Expanded Disability Status Scale (EDSS) of less than four. The EDSS is a rating for MS progression where zero is no impairment and four is an ability to walk 500 meters without an aid. A ten on this scale would be the highest level of disability and death from MS. The intensity of the computerized cognitive program lasted three months. They compared this with a control group that received no intervention. After the rehabilitation program was completed, only the control group had significant improvement in tests of attention information processing and executive function. The study group also had a significantly lower depression score. The outcome measures that were used in this study were the Paced Auditory Serial Addition Test (PASAT) and the Wisconsin Card Sorting Test (WCST).
The study did not state if these improvements translated into improved participation or performance with day-to-day activities like home management, leisure, socialization, or work. The interventions were based on neuropsychology and were not focused on cognitive functioning in real-life situations. As occupational therapists, we would want to see more studies focused on the efficacy of interventions focused on functional cognition that are supplemented by computerized activities that replicate real-life functional situations. It would be interesting to do this with a virtual reality system which supplemented the type of cognitive function and decision making that patients have to utilize in real-life situations. This could then be used in conjunction with doing real-life tasks like shopping, community mobility, planning the use of public transportation, and housework.
Other studies included in this AJOT systematic review focused on person factors found moderate evidence from medium quality studies supporting the effectiveness of memory training. They used recall strategies such as imagery, mental rehearsing, mental stories, and mnemonic strategies all designed to increase memory for the purpose of functional tasks. They also found strong evidence from high-quality studies for interventions targeting emotional regulation using cognitive behavioral therapy. We will discuss how OTs can use this type of intervention in a few slides using the Cognitive Orientation to Daily Occupational Approach or the CO-OP approach. Cognitive-behavioral therapy strategies work through guided discovery where the patient or client becomes more aware of unhelpful cognitive processes and thought patterns that they are using and change to more useful behaviors and cognitive strategies. This improves mental health coping and emotional regulation.
- Strong Evidence from high-quality studies supports physical activity and yoga
- High-intensity training three times a week was recommended
- Aerobic exercise can include leg cycling, treadmill walking, and aquatic exercise
- Yoga was found to be beneficial for improving balance and selective attention ability
They also found strong evidence from high-quality studies that supports physical activity and yoga. Some examples of physical and aerobic exercises can include leg cycling, treadmill walking, yoga, and aquatic exercises. In fact, yoga was not only shown to be beneficial for balance, but they also found an improvement in selective attention ability amongst the patients who participated in that type of activity. I think this is because it requires so much attention to be able to hold the yoga poses while concentrating on balance. Additionally, if there are distractions in the environment, you have to be aware of your body's own positioning and make adaptive changes to be able to hold that position. One thing to be mindful of is that yoga can be fairly strenuous. Occupational therapists may be able to find adaptive techniques or poses for those with MS.
- Conclusions
- Few studies had OTs as part of the research team
- OTs should make use of metacognitive strategies to improve performance.
- Tele-medicine programs should be used as an extension of cognitive training
- Group CBT based interventions can improve depression and self-efficacy
- Exercise interventions can improve endurance
In conclusion, few studies in the second study had OTs as part of the research team. There is starting to be more OT led research on MS. OTs should make use of metacognitive strategies to improve performance and help patients become more aware of their own behavior and thought patterns. The theory is that as you become more aware of your own behavior and thought patterns, the more you can start to integrate different strategies that will improve your performance with day-to-day activities.
Tele-medicine programs can also use this cognitive approach. This could be very useful as an extension of cognitive training. I can tell you that in the midst of the COVID-19 pandemic, in my home health agency, we have been supplementing in-home visits with telehealth. We are finding that patients are making quicker progress. Sometimes our interventions are not a quick fix, and they require a lot of work. We have to develop a very strong therapeutic relationship to help the client to make progress toward day-to-day activities. Another conclusion was that cognitive-based group training interventions can improve depression and self-efficacy. Lastly, they found that exercise interventions can improve endurance.
Efficacy of Exercise (Bjarnadottir, Konradsdottir, Reynisdottir, & Olafsson, 2007)
- Randomized Control Study
- Effect of aerobic and strength exercise on physical fitness and quality of life in patients with mild MS (EDSS<4; ability to walk 500 m without an aide)
- Expanded Disability Status Scale (0 no impairment 10 is death due to MS)
- Exercise Group:
- 60 minutes of exercise, three times a week, for 5 weeks, totaling 15 hours.
- Monark Cycle Ergometer – 3 minutes at 33% peak oxygen uptake (VO2peak)
- 15-20 minutes at 55% of VO2 peak)
- Resistance exercise involving major muscle groups
With MS, often there is a loss of strength and endurance. This randomized control study provided one group with an exercise intervention while the control group received no treatment at all. They looked at the effect of aerobic and strength-type exercises on the physical fitness and quality of life in patients with mild MS. Earlier, I spoke about the EDSS. They looked at patients who had less than four on that test meaning they had the ability to walk 500 meters without an aid. These patients were at least below four. The exercise group received 60 minutes of exercise three times a week for five weeks. The total was 15 hours. They were looking for activity engagement with a specific peak oxygen uptake. A peak oxygen uptake is also known as the maximum aerobic capacity or the maximum rate of oxygen consumption. The participants used Monark lower extremity ergometers for three minutes at 33% of their peak oxygen uptake. Then they engaged in the same activity for about 20 minutes at 55% of their peak oxygen uptake. The rest of the time was spent on resistive exercises involving major muscle groups.
- Control Group: No exercise
- Results:
- Exercise group:
- 14.7% increase in VO2 peak
- 18.2% increase in peak workload
- 27.3% increase in anaerobic threshold
- The decrease in BORG rating for exercise from 17.2 to 17.0
- A tendency towards improved quality of life (not significant), on the SF-36
- Control Group:
- No significant change
- Exercise group:
They found with the exercise group that there was a 14.7% increase in their ability to engage in peak oxygen uptake and more intensive activity by the end of the rehabilitation program. There was an 18.2% increase in peak workload and then a 27.3% increase in anaerobic threshold. There was also a decrease in the BORG rating by the participant for the exercises. The BORG rating is the rate of perceived exertion. There also was a tendency towards improved quality of life.
- The study showed no negative effects of exercise in the participants, although, there is concern that intensive exercise in patients with more severe MS (>6 on the EDSS).
- What if exercise was replaced with strategies to improve participation and performance with meaningful activities, including socialization and community-based activities?
- Increased aerobic capacity?
- Increased quality of life?
While there is some concern that intensive exercise could negatively impact patients with severe forms of MS, this study found no negative effects of exercise on the participants with milder MS. As an occupational therapist, I view this study in a more activity-based and functional manner. I would like to know if exercise could be used as a supplement to meaningful activities to improve participation. With these improvements in aerobic capacity, were the participants able to walk further into the community? Were there improved effects on cognitive function and problem-solving during higher-level activities including yard work, managing the use of public transportation, or getting to and from grocery stores? Could a combination of engaging in exercise and functional activity further increase a client's quality of life?
Cognitive Impairments in Patients with MS
- Patients with MS require significantly more time to learn tasks through verbal instructions(DeLuca, Barbieri-Berger, & Johnson,1994)
- Patients living with MS have difficulty with decision making in situations that involve risk and ambiguous information, demonstrating risk aversive behavior and longer deliberation times (Neuhaus, Calabrese, & Annoni, 2018).
- Learning and incorporating new and novel tasks into a daily routine can be difficult for patients with MS
Patients with MS have been shown to have difficulty processing verbal instructions and making decisions during novel or risky and ambiguous situations. Education should be delivered in small and short segments with increased time to process. We should back up verbal information with written and visual material including videos and demonstrations. Patients should also be encouraged to trial new strategies immediately followed by a discussion of how well each strategy or technique worked. This goes for self-care techniques, transfer techniques, use of adaptive equipment, assistive equipment, energy conservation strategies, mental imagery, and rehearsing strategies. Learning and incorporating new and novel tasks into a daily routine can be difficult for patients with MS. The information on this slide brings relevance as to why patients with MS are prone to depression and have difficulty regulating their emotions. If you think back to the pathophysiology of the disease, remember that demyelination results in a deterioration of nerve signals and impulses ascending the spinal cord through the thalamus and to the areas of the brain responsible for processing and interpreting that information. When you think about that, this alone would lead to deregulated emotions and a depressive state of the central nervous system which would affect thought, behavior, and ability to adapt to occupational challenges. The slowing down of the nerve impulses because of this demyelination is going to affect the brain's ability to function as one unit.
- Goal discrepancy and loss of function can lead to negative thoughts and depressive rumination (Watkins & Noelen-Hoeksema, 2014).
- Emotional state can alter decision making and ability to process information and learn from it
- Anxiety
- Sadness or Anger
- Pessimism
In addition, goal discrepancy and loss of function will contribute to negative thoughts leading to depressive rumination. Remember, there is a loss associated with this disease and a discrepancy in what the patient wishes they were able to do or wants to be able to do and what they are capable of. When you start to lose your ability to participate and perform day-to-day activities, you also lose your identity. This is how we all define who we are in social situations or what we talk about with people. What do you do for a living? What is it that you like to do? This loss of identity affects a person's emotional state leading to depressive symptoms. This then alters their decision-making, their ability to process information, and their ability to learn from past experiences to adapt. All of this can lead to anxiety, sadness, anger, and pessimism. When you meet your client with MS for the first time, do not think, "They are not motivated," or "They do not want to listen to anything I have to tell them." This is part of the disease process. We have to utilize a more therapeutic approach to engage clients to help them to identify strategies that are going to work for them. Let's take a look at this right now.
Cognitive Orientation to Daily Occupational Performance (CO-OP) (McEwen, Mandich, & Palatajko, 2018)
- Cognitive Strategies focused on performance
- Does not focus on addressing specific cognitive impairment
- Client-Centered
- Performance-Based
- Strategies are developed by the patient
- OTs role is that of a coach
- Non-prescriptive with assigning strategies
- Guide the patient as they discover solutions to solve performance deficits
We are now going to discuss how occupational therapy theory can guide us in our interventions for patients with MS. The Cognitive Orientation to Daily Occupational Performance, or CO-OP, is a client-centered, performance-based, problem-solving approach that uses guided discovery to enable the acquisition of skills to overcome occupational challenges and impairments. The CO-OP approach encourages individuals to identify solutions to motor problems to improve occupational performance. CO-OP improves motor acquisition, cognitive awareness, or metacognition, and skill generation so that they can be transferred to multiple situations. The therapist acts like a coach in this process whereby he or she guides the patient through the global strategy of the process, "goal-plan-do-check." You are saying to the patient, "What do you want to do? How do you want to do it? Let's try it and then let's review how it went."
- Goal-Plan-Do-Check is used to optimize self-identified strategies
- Assessments used in CO-OP
- Activity Card Sort
- Canadian Occupational Performance Measure (COPM) (Dedding, Cardol, Eyssen, Isaline C.J.M., & Beelen, 2004)
- Performance Quality Rating Scale
In other words, you are developing goals, planning strategies to achieve the goals, implementing the strategies, and evaluating and re-evaluating the effectiveness. This sounds rather simple when you boil it down like that, but there is a method to all of this. It provides a platform for you to engage the client in the repetition of the activity so that you could find where the breakdowns are happening. As they do it more, they become more aware as to where the breakdowns are happening, and then together you can strategize activity modifications, adaptive equipment, or energy conservation techniques to improve performance. It may be a new way of doing the activity or a new thought process that helps the patient realize they have to remember a certain step as an example.
With any program, you are going to start off with an assessment. The Canadian Occupational Performance Measure (COPM) is a good assessment that you can use in the CO-OP strategy. The COPM is a semi-structured interview that helps patients identify meaningful daily activities across multiple performance domains that the patient wants to do, needs to do, or is expected to do. The performance domains include self-care, productivity which would include paid work and housework, and also leisure activities. The patient then chooses the five most important activities across those performance domains and rates their performance and satisfaction each on a 10 point scale. Ten is the highest performance and satisfaction and zero is the least. The COPM provides a platform in which to develop patient-centered meaningful goals with the patient's input.
We recently had a patient with MS that had many of the cognitive impairments that come with the disease as well as depression. She was unable to make decisions that impacted her performance. She was really focused on spasticity and exercise. However, when it came to allowing us to help her with more advanced day-to-day activities like community reintegration, the use of a power wheelchair, or driving, she was less engaged. She had many resources available including money. In fact, she probably could even have afforded to buy an adaptive van. I think at one point we talked to her about going back to work, but she just did not want to. We felt this was part of a larger pathology of the disease. She was depressed and her decision-making and ability to cope and learn new strategies was impaired.
We decided to do a reassessment and use the COPM in order to identify new goals and strategies. She did not like to COPM as she did not want to disclose "all this personal information." Remember, the COPM is a valid, reliable, and structured platform for you to engage with the patient around the identification of goals. In the end, we found out that her two biggest worries were toilet transfers and toilet hygiene. Her biggest goal was to be able to get out to socialize more. Toilet transfers and toileting were holding her back. In particular, she was worried that if she was at a friend's house that she would not be able to use the bathroom independently.
This assessment provided an avenue to start working with her on some strategies that might improve her performance in these activities. We came up with a bathroom schedule, energy conservation strategies, and transfer techniques so that she could feel confident enough to use the bathroom with minimal assistance. We also worked on some strategies so that she would feel comfortable enough to be able to ask friends for help. We even worked with some of her friends and brought them in as caregivers to help utilize these strategies. Thus, we were utilizing these strategies in a more broad platform. This information was being transferred to the outside environment and making use of other resources available to her so that her long-term goal of getting out and socializing more would be achieved. As a result, she started having some planned visits to her neighbor's house for coffee as she used to when she was more independent.
Using the CO-OP approach, the therapist can make recommendations, and we did this with this patient as we identified the activities that she was interested in. For example, we made recommendations on how to modify the activity, change body positions, or how to use special tools. While using the CO-OP approach, it is important to remember that therapists should only address one task at a time. The therapist should guide and coach the patient but not be overly prescriptive. It is important to also provide immediate feedback when strategies work. Examples are that the activity took less time, there were fewer mistakes there, or less assistance or cueing was needed. The point is to make the activities as fun as possible to further engage the patient in the process. The therapist should also involve others in the activity just like I talked about with the other caregivers and friends to improve generalization and automaticity of strategy use.
Case Study (Preissner, Arbesman, Lieberman, 2016)
We will now work through in the remaining time through a case study example where a client with MS made use of multiple strategies to improve performance with various daily activities.
- 49 y/o female
- Diagnosed with MS 9 years ago
- Inpatient rehab stay after 3 days of acute care due to an MS exacerbation
- Clinical Information from chart review
- Increased difficulty flexing hip and dorsiflexion
- Significant difficulty walking that worsened over 3 days
- Increasing fatigue
This case study was written up in AJOT. This is a 49-year-old female diagnosed with MS when she was 40 years old. This patient had an exasperation of MS and had an inpatient rehab stay after a significant decline in function. Per the therapist's from the chart review, this patient had increased difficulty flexing at the hips and dorsiflexing. During ambulation, her feet were sort of dragging on the floor, and this was a change from how she was previously. The patient had significant difficulty walking that worsened over three days, and she had increased fatigue.
OT Assessment
- Informal Interview
- Canadian Occupational Performance Measure
- Lives in a single-story home with 19 y/o daughter and husband
- Alone for most of the day
- Unemployed and on disability
- Previously worked as a paralegal
- Prior to MS exacerbation, the patient was independent with self-care and shared household management activities with husband and daughter.
Increasing fatigue, limiting ADL/IADL performance
The OT assessment started with an informal interview. They used the COPM. They found that the patient lived in a single-story home with her 19-year-old daughter and husband. She was alone for most of the day and was unemployed and on disability. She had previously worked as a paralegal, and prior to her MS exasperation, the patient was independent with self-care and shared household management activities with her husband and with her daughter. She was mostly independent with ADL and IADL and now had increasing fatigue which limited her performance with self-care and home management tasks.
COPM Results
Figure 6 shows the result of the Canadian occupational performance measure.
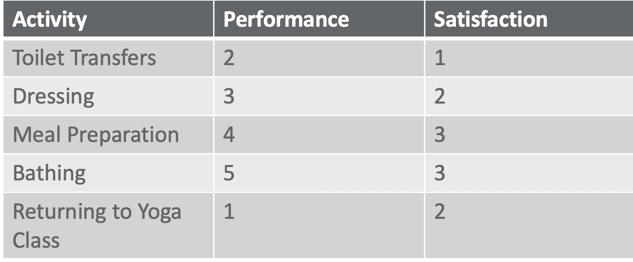
Figure 6. COPM results.
The five most important activities that the patient identified in the COPM were toilet transfers, dressing, meal preparation, bathing, and returning to yoga class. You can see her performance scores on a 10 point scale were rather low although she did feel that she was able to do meal prep and bathing better than some of the other activities. Nonetheless, her satisfaction was low with all of these activities as well. She wanted to be able to perform them better.
Functional Independent Measure (FIM)
A functional independent measure assessment was also done by the therapist in Figure 7. This was observational, and the therapist found that the patient required minimal assistance with eating, grooming, upper body dressing, and then more moderate to maximum assistance with bathing, toilet transfers, and tub transfers.
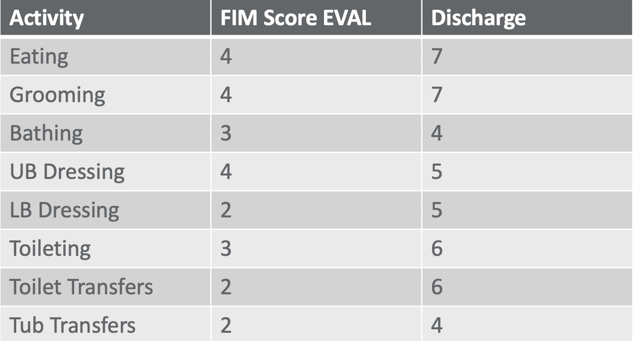
Figure 7. FIM results.
Assessment of Motor and Process Skills (AMPS)
- Assessment of Motor and Process Skills (AMPS)
- Two Activities Chosen
- Making a grilled cheese sandwich
- Washing Dishes
- Findings
- Safety
- Physical Assistance
- Difficulty stabilizing her body
- Difficulty reaching, grasping, and lifting tools and supplies
- Difficulty transporting task objects
- Decreased Endurance
The Assessment of Motor and Process Skills (AMPS) was also used. The two activities chosen for this were making a grilled cheese sandwich and washing dishes. The occupational therapist found that there were some safety concerns. The patient required physical assistance with both of these activities, and she had difficulty stabilizing her body with reaching, grasping, and transferring tools and supplies. She demonstrated fatigue and decreased endurance with the tasks.
OT Interventions
- Basic ADL (toilet transfer, dressing, bathing)
- OPTIMIZE POSITIONING OF THE BODY: sit versus stand
- SIMPLIFY ACTIVITIES: Choosing clothing the night before, having tools and supplies organized, use of a bedside commode or urinal to save energy
- USE OF APPROPRIATE ASSISTIVE DEVICES: sock aides, reacher, tub seats, commode.
- REST BEFORE BECOMING FATIGUED
- Bank energy – build in rest breaks prior to participation
- MS patients have difficulty recovering from over-fatigue
Interventions came down to optimizing the positioning of her body, simplifying activities, making use of appropriate assistive devices, and resting before becoming fatigued. The therapist suggested basic things like sitting versus standing or choosing clothing the night before to make that process easier. It was also suggested to have tools and supplies well organized so she knew where they were and did not have to reach for them. In this way, she was not wasting energy looking for items in a drawer or in another room. All of those types of things like walking to another room or reaching down further than you need to are going to expend energy and limit performance in the current task or with something in the future that you wish to do. You want to try to help patients be as efficient and organized as possible. Even the use of a bedside commode or urinal can save energy. This also helps the patient adhere to a toileting program because remember bowel and bladder function is also something to consider with this diagnosis. This is especially true when you want to engage in social or higher-level activities like getting out into the community and being around friends and family. I know that during these times of this pandemic this is not something we can regularly engage in. This is leading to our own levels of depression or feeling like we are not able to engage in any activity the way we want to. However, imagine how it would be for this patient with MS or any patient with MS.
When you prescribe adaptive equipment, you want to make sure that you are not making this more difficult than it needs to be. Sock aides for example are something that could be very helpful, but if the patient does not have upper body strength and fine motor dexterity, you do not want to prescribe a sock aide because it might make the activity or task of putting on a sock even more difficult. You want to make sure you are prescribing the right equipment.
Resting and banking energy before they engage in a task is another idea. MS patients have been known to have a hard time recovering if they become overly fatigued. In order to prevent this, they can plan out their day. For example, they might have an appointment with their neurologist. They may need to conserve energy by avoiding or accepting help with certain activities prior to engaging in a more intensive activity.
- Yoga Class
- The patient described various yoga poses to the therapist
- Analyze and modify poses, given the patient’s current level of function.
- The practice of modified poses
- Development of a home program of progressively modified poses
- Use of fatigue management strategies
- Progress back to attending a yoga class
This patient wanted to participate in a yoga class. The occupational therapist had the patient describe various yoga poses, and she analyzed and modified the poses given the patient's current functional level. She developed a program where the patient sat versus standing, held the pose for a shorter period of time, or held the pose with more support with either a walker or table. The patient was able to use this program at home and expanded upon that to eventually participate in yoga at a much more satisfactory level. Making use of fatigue management strategies and progressing back to be able to attend in-person yoga classes was very meaningful for this patient.
- Emotional Regulation
- Positive imagery
- Meditation
- Positive Self Talk
- Plan and prioritize activities
- Utilize social support
They also worked on emotional regulation using positive imagery, meditation, and positive self-talk. They helped her recognize negative self-impulses and negative talk that we all have sometimes. They taught her to replace this with something more positive. By taking stress and anxiety out of the situation and planning and prioritizing activities, this can go a very long way with patients with MS to reduce the exacerbation of symptoms. Another area for emotional regulation is utilizing social support. Identifying social affordances and involving them in the care and strategies will help to improve performance. It's very important to do that.
OT Outcomes
Here are the outcomes that came from this case study in Figure 8.
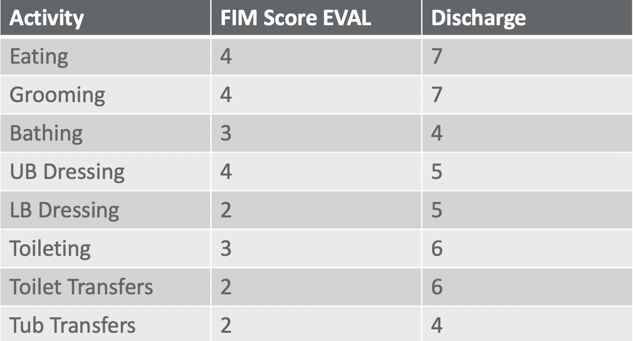
Figure 8. Summary of OT outcomes per the FIM.
You can see the FIM scores from the eval and after treatment. There was an improvement in eating, grooming, bathing, dressing, toileting transfers, and tub transfers. The patient made improvements in every single level on the FIM. As the FIM is observational, the therapist was able to see that there was a direct improvement in the patient's ability to perform those tasks. The COPM scores are in Figure 9.
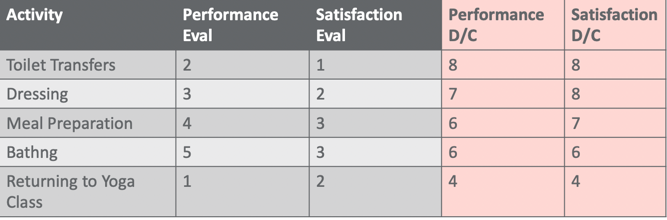
Figure 9. Summary of OT outcomes per the COPM.
You can see that the patient's self-perceived performance scores in all of those five activities that she identified at the beginning (toilet transfers, dressing, meal prep, bathing, and yoga) all improved both from a performance perspective and self-perceived satisfaction level as well.
Summary
Thank you everybody for attending. I hope you enjoyed this lecture. MS is a very diverse disease where you can have a lot of different impairments. When I was creating this lecture it was a little difficult for me to identify which performance components I wanted to focus on and which specific symptoms of the disease that I would call out. I tried to make it a little bit more broad and useful for a variety of different therapists depending on your practice area. I tried to bring in OT theory as well to help guide you. I hope I achieved that.
References
Available in the handout.
Citation
Rushanan, S. (2020). Occupational therapy treatment for patients with multiple sclerosis. OccupationalTherapy.com, Article 5367. Retrieved from http://OccupationalTherapy.com
