Introduction and Overview
As per the American Joint Replacement Registry (AJRR) of 2016, more than one million people per year undergo either an artificial hip or a knee replacement. With an aging but still active population, the number of joint replacement surgeries is expected to grow dramatically to around four million people in less than 20 years; more than half of which will be younger than 65 years old.
Let's take a look at the numbers to provide an idea of how these procedures are growing. According to the American Joint Replacement Registry, between 2011 to 2015, the number of hospitals registered for joint replacement surgery increased significantly (from 20 to 612). Additionally, the 2015 average procedural volume for participating surgeons was as follows:
| Total Surgeons | Total Procedures | |
| Hip | ||
| Primary | 2572 | 57,673 |
| Revision | 1101 | 6688 |
| Knee | ||
| Primary | 2281 | 87,593 |
| Revision | 1538 | 9086 |
This is the distribution of how many hip and knee procedures were done in 2016, according to the AJRR (the quantity and percentage of the total procedures):
- Primary Knee: 235,718 (55.2%)
- Primary Hip: 150,320 (35.2%)
- Revision Knee: 22,403 (5.2%)
- Revision Hip: 17,180 (4.0%)
- Hip Resurfacing: 1,708 (0.4%)
Hip Replacement
The hip is one of the largest joints (Figure 1). It is a ball-and-socket joint. Bands of tissue called ligaments (the hip capsule) connect the ball to the socket and provide stability to the joint. The head of the femur is the ball; the pelvic bone, the acetabulum, is the socket piece. It has a nice joint capsule, which connects the ball to the socket and it maintains stability. The smooth weight-bearing surface is the head of the femur.
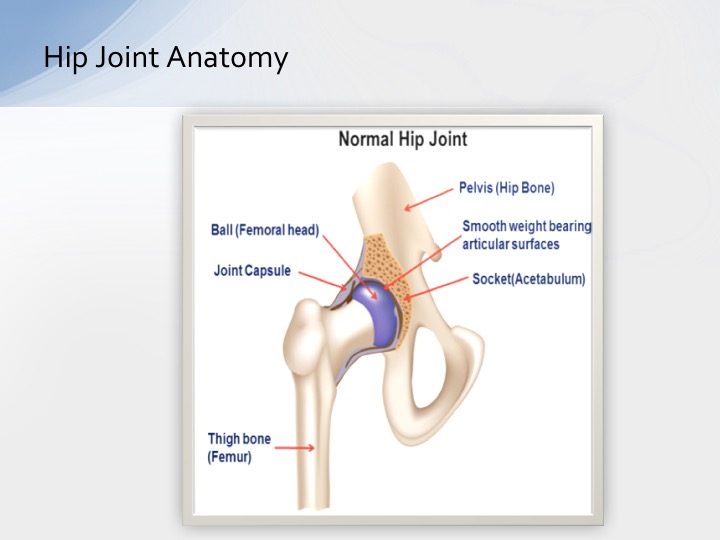
Figure 1. Normal hip joint.
Indications of Hip Replacements
Some conditions where hip replacement would be indicated include:
- Osteoarthritis
- Rheumatoid arthritis
- Post-traumatic arthritis (after a fracture)
- Avascular necrosis (common in young patients)
- Childhood hip disease
If a patient had a fractured head of the femur or subtrochanteric fracture, the surgeon would opt out for a hip replacement. It may not be a total hip replacement, depending on the fracture site and the degree of hip fracture.
When comparing a normal hip to one with arthritis, the normal hip has a smooth surface, and there is enough joint space between the two bones. On the other hand, with the osteoarthritic hip, the spacing is narrowed between the two joints. The cartilage is worn down and the surface is not smooth anymore.
Contraindications for Hip Replacement
Situations, where hip replacement would be contraindicated, include:
- Infection: An existing infection (e.g., osteomyelitis) is an absolute contraindication, and patients who are prone to infection may not be eligible for this surgery.
- Nicotine: Smokers and other tobacco users face a higher rate of medical complications and a higher risk of needing follow-up surgery or revision hip replacement surgery.
- Osteoporosis: Severe osteoporosis can be a contraindication for surgery, because bones may be too brittle to properly support and adhere to the new joint prosthesis.
- Other factors, such as dementia: Intellectually challenged individuals, or those with any type of memory loss, may not be able to reliably comply with the recommendations of their surgeons.
Types of Hip Replacements
There are two types of hip replacements. The most common is total hip arthroplasty. The second most common is partial hip arthroplasty (hemiarthroplasty). The partial is used when you just have a fracture of the head of the femur and all you need to do is replace the head. When you go to the total hip arthroplasty, that means not only replacing the head of the femur, but also the acetabulum piece.
Components of total hip arthroplasty.
- Acetabular component (socket): This piece is usually made of metal but is occasionally made of ceramic or a combination of plastic and metal.
- Acetabular line: This piece is usually made of high-quality plastic.
- The femoral head (ball): These are made of durable metal, plastic, ceramic, or a combination of materials.
- Femoral stem: Could be a cemented stem or uncemented stem. These days, it would most likely be the uncemented stem.
Different types of total arthroplasty.
The socket between the lining and the acetabular piece could consist of a few different material combinations: metal on polyethylene, metal on metal, or ceramic on ceramic.
Complications of Hip Replacement
An early complication after hip replacement surgery could include component malpositioning (i.e., the prosthesis is not positioned correctly). This may occur because of a pre-existing condition in the hip and pelvic bone, or the femur and pelvic bone. Also, component malpositioning could be the result of the abnormal structure or abnormal anatomy of a person, where the normal size hip would not fit them. Another very important complication is a fracture of the adjacent bone (likely the shaft or femur). There could also be nerve or vascular damage.
Immediate complications could include infection, fracture of the adjacent bone(s), and neurovascular damage. Finally, late complications that may occur are dislocation of the hip joint, loosening of the implant, joint stiffness, muscle weakness, persistent infection, and joint debris due to the wear and tear of the implant.
Surgical Options
In the early days of hip replacements, surgeons mostly used the posterior lateral incision. Recently, surgeons have started incorporating lateral incisions, although the most commonly used option today is the anterior approach.
Anterior Approach. The direct anterior (Smith-Peterson) and the anterior lateral (Watson Jones) approaches have the advantage of not violating the posterior, or gluteus maximus muscles. Additionally, there is often less damage to the posterior capsule.
The three positions of hip stability when a surgeon does an anterior approach are:
- Forward flexion
- Abduction to neutral
- Internal rotation
Conversely, according to Desai and Higuera-Rueda (2014), the positions of instability with an anterior approach (i.e., the positions that you want to avoid) are:
- Adduction
- External rotation
- Excessive hyperextension
Posterior Approach. Today, probably the most popular approach for a total hip replacement is the posterior approach. The disadvantage of the posterior approach is that the posterior capsule and muscles are cut during the approach, as the incision is made more posterior lateral (the surgeon goes through the gluteus maximus).
What are the posterior positions for hip stability?
- Flexion within the limitation of precautions (no more than 90 degrees of forward flexion)
- Abduction
- External rotation
The posterior positions of instability are exactly the opposite (Grandic, 2015):
- Flexion greater than the limitation of precautions (more than 90 degrees)
- Adduction
- Internal rotation
As occupational therapists, how would we educate the patient? What are the three movements that should be avoided? Keep in mind that we need to state it in "laymen's terms."
- Adduction = do not cross your legs
- Internal rotation = do not use a pigeon-toed position
- Flexion greater than 90 degrees = do not reach or lean forward and pick up items from the floor.
I always tell my patients that your hip should never be lower than your knee. In other words, do not push up from a very low stool or from the floor.
Comparison of the anterior vs. posterior approach. The risk for femoral fracture during surgery in a posterior approach is 1% to 2%, versus anterior approach is 2-4%. The femoral nerve injury is less than 1% for the posterior approach; with the anterior approach, it is 2-20%. Risk of dislocation in the first year is 3-4% for the posterior approach; the anterior approach is less than 1%. Functional outcomes with the posterior approach are lower in the first three months than anterior, but at 12 months, outcomes are almost the same compared to the anterior approach. With the anterior approach, the functional outcomes are much higher within the first three months after surgery. Hospital stays for a posterior approach average four days; with the anterior approach, the average is 2.9 days. After surgery, 84% of posterior approach patients went home, versus 97% of anterior approach patients (rather than going to a rehab facility). That's a significant difference between the anterior approach and the posterior approach.
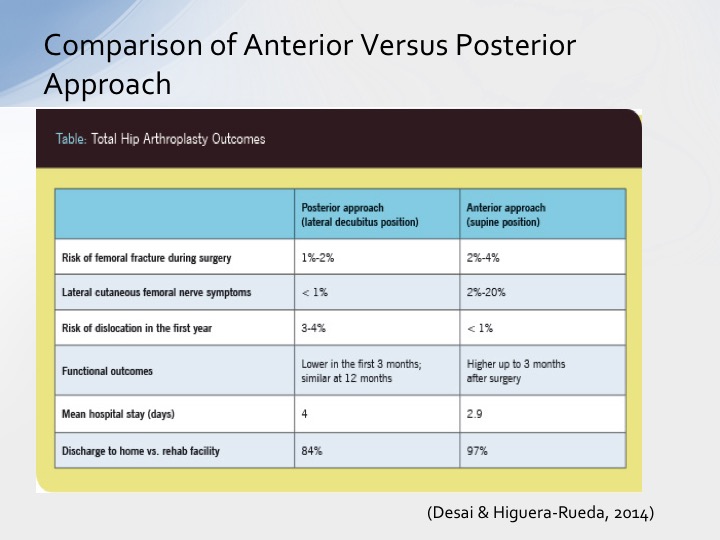
Figure 2. Comparison of anterior vs. posterior approach (adapted from Desai & Higuera-Rueda, 2014).
Knee Replacement
The knee joint is a hinge joint (Figure 3). The knee joint consists of three bones: femur, tibia, and patella. The menisci (C-shaped wedges between the femur and tibia) act as "shock absorbers.” The large ligaments (medial and lateral) provide stability to the joint.
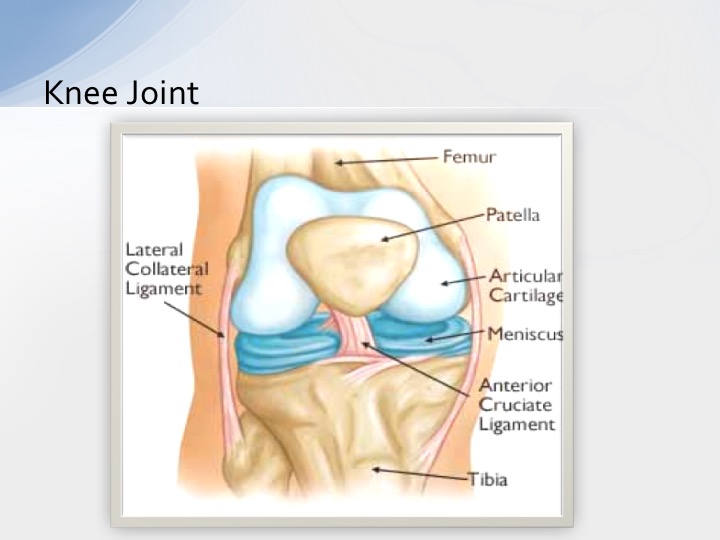
Figure 3. A normal knee joint.
Indications for Knee Replacement
Some common indications for knee replacement include:
- Osteoarthritis
- Rheumatoid arthritis
- Post-trauma
The normal knee joint has a nice space between the tibia and the femur. The cartilage is intact and smooth, and the menisci are smooth. In a knee with osteoarthritis, there are bone spurs, there is a loss of cartilage, and the space between the two joints is narrowed such that it is like bone-on-bone.
Contraindications for Knee Replacement
Knee replacement surgery is contraindicated in situations where:
- Infection is present (such as the presence of osteomyelitis)
- The patient smokes, uses any form of nicotine or drugs
Types of Knee Replacement
There are three types of knee replacements: total knee replacement, partial (unicompartmental) replacement, and kneecap replacement (i.e., patella-femoral arthroplasty).
In a total knee replacement, the femoral, tibial and patella components are replaced. In comparison, with partial knee replacement, only one piece is replaced, the tibial component. Hence, the term unicompartmental ("uni" means one).
What are the different components of knee replacement?
- Stem
- Patellar component
- Metal femoral component
- Plastic Spacer (to maintain the joint space)
- Tibial component
Complications After Knee Replacement
Some possible complications after knee replacement surgery include:
- Infection
- Blood Clot (PE, DVT)
- Implant loosening
- Stiff knee (Limited ROM)
- Scaring
- Continued Pain
- Neurovascular Injury
In an acute care hospital, to prevent infection, patients are given three bottles of antibiotics: one right before surgery, and two after surgery. For blood clot prevention, patients are given blood thinners, and we also can use athrombic pumps. When they go home, the patient can wear compression stockings to prevent blood clots. Mobilization and involvement in occupational and physical therapy are going to help prevent stiffness in the knee. For scarring, outpatient therapists and home care therapists can show patients how to massage the new scar or the new incision, in order to loosen the layers of the skin. Pain management can be an issue. Sometimes pain exists because of an infection or a stiff joint or any other reason. Sometimes there is so much scarring of the joint that the surgeon has to go back, remove the scarring and the additions, and take care of the pain. With a neurovascular injury, there could be a popliteal nerve injury. This can cause foot drop, at which point we must intervene accordingly.
Surgical Advancements
Hip Replacement
Super-Path hip approach. Originally, when hip replacements were performed, there used to be a big scar (about six to seven inches). Now, with the Super-Path approach, surgeons make a much smaller incision (about two to three inches). They do not dislocate the hip joint, nor do they twist or contort the leg, resulting in a quick recovery and a much lower chance of post-operative hip dislocation.
Direct Hip anterior approach. The direct anterior hip replacement approaches the hip joint through the shortest route, between muscle planes, and without cutting any muscles. A special operating table is typically used to position the leg during surgery.
MAKOplasty. The third and most important surgical advancement is navigation. MAKOplasty is an innovative total hip replacement procedure that is performed using a highly advanced, surgeon-controlled robotic arm system. This would be possible only with elective surgery, and not the traumatic hip replacement. The patient undergoes a CT scan and MRI. There is already a pre-existing MRI. It is fed into the computer. Once you put in the patient's data, the computer shows you exactly where the incision should be made. The robotic arm will guide the surgeon in making the incision and shows the proper placement of the acetabulum piece.
Knee Replacements
Patient-Specific custom implants. A CT scan of the patient's arthritic knee is used to digitally construct a computer-generated, three-dimensional model of the knee joint. Using a 3D printer, a custom knee can be created for the patient to the exact shape of their knee. The custom-made knee fits very precisely, as compared to "off-the-shelf" knees which only come in small, medium and large. A lot of surgeons have been using the custom-made knee replacements with a 3D printer. It takes a little longer to order and receive the implant versus immediate off-the-shelf ones, but the outcomes are phenomenal.
Gender-Specific knee replacements. In general, the female thigh bone (femur) is smaller than that of males. Traditional implants are very large, compared to the custom implants. Therefore, it makes sense to offer gender-specific implants that are custom-made for men and women, so that the correct size is achieved.
MAKOplasty. MAKOplasty uses a robotic arm to assist the surgeon in making the bony cuts around the knee. It is guided by MRI and the computer: the surgeon can look at the computer and know exactly where to make the incision and how to place the implant. It requires a pre-operative CT or MRI scan and intra-operative navigation. The benefit of MAKOplasty is that it improves implant positioning.
Importance of the Occupational Therapist
I work in a fast-track joint replacement surgery center where pre-op meetings and pre-op assessments are mandatory. Every patient who is going to undergo surgery comes to my pre-op assessment group. What are the benefits of pre-op OT assessment?
- It gives the patient a better understanding of the upcoming procedure.
- It reduces the anxiety and fear of surgery and assists with recovery after the surgery.
- It increases post-surgery compliance, especially for hip and knee replacement. The patient and the family and/or caregiver know the precautions; they know what is expected out of surgery. That makes them more compliant post-surgery and improves recovery.
- It reduces complications.
- It enhances knowledge about how to improve their occupational performance post-surgery.
- It gives the patient an understanding of what equipment they will need (e.g., hip kit, walker, commode, elevated toilet seat, etc.).
- Research has shown that occupational therapy assessment and education pre-op have a decreased length of stay and cost of surgery (Gentile, 2007).
Pre-Op OT Assessment
The preoperative occupational therapy assessment addresses the following issues:
- Occupational history and prior level of function: How active the patient has been? What is the person's occupation? What has been their prior level of function? Does this person lead a sedentary life? Prior to surgery, does this person need help with ADLs? Or are they completely independent and active in the community?
- Cognitive, emotional and social factors that may affect the surgical outcomes: Does this patient understand the precautions they need to take after surgery? Does this patient have a good memory, or are there cognitive deficits? Can they remember instructions?
- Need for durable medical equipment: Patients may ask where their grab bars should be, or how they are going to get in and out of the tub? Will they be able to prepare meals or navigate stairs?
- Fall risks
- Architectural barriers, hurdles or obstacles at the home
Pre-Op OT Education
After we complete the pre-op OT assessment, we provide education to the patient and family/caregivers so that they are better prepared before the surgery, and also to ensure faster recovery after surgery. Preoperative occupational therapy education includes the following:
- Exercises for upper and lower body strength, range of motion and endurance
- Diet and nutrition
- Alcohol and smoking use
- Certain medications
- Post-surgery precautions and limitations
- Mind and body relaxation techniques for pain management and anxiety
- ADL/IADL and mobility training (using a hip kit, leg lifter, walker or cane)
- Use of adaptive devices
- Home safety preparation
- Discharge planning and home care services (Does the patient need subacute care or acute care? Or will they go directly home and have outpatient therapy?)
Post-Op Role of OT in Various Practice Settings
After surgery, each patient will recover at a different rate, depending on a variety of factors (the type of surgery, age, health prior to surgery, etc.). They may find themselves in one or more of the following settings throughout the course of their recovery:
- Hospital/Acute
- Acute Rehab
- Subacute
- Homecare
- Outpatient services
Acute/acute rehab care after surgery. As OTs, we can use a holistic approach which integrates occupational-based activity. Everything we do must be client-centered (the evaluation, intervention, and task modifications) to facilitate progress towards performance-based goals. We need to analyze the prior level of function, and whether the patient is likely to resume those pre-hospitalization activities. That would be the goal to achieve after the rehab.
Immediately after surgery, we can provide OT training based on post-surgical orthopedic protocols. This includes informing the patient about appropriate weight-bearing and/or precautions during ADLs. In other words, we need to let them know their recommended weight-bearing status, whether it is full weight-bearing, partial weight-bearing, toe-touch bearing, or non-weight bearing. I've seen non-weight bearing advised mainly with a traumatic hip replacement if the surgeon thinks the joint is not very stable. Most of the time with total hip and total knee replacements, they are weight-bearing as tolerated. The more they walk and put weight on it, the quicker and faster they heal. If a patient has had intramedullary (IM) nails put in the mid-shaft femur, then most likely the recommendation is going to be weight-bearing as tolerated. If the patient had the plate and screws put in, those are more weight sharing, and the surgeon might not want the patient to bear weight fully (partial or toe-touch weight-bearing).
OTs can facilitate the use of adaptive equipment for ADLs and IADLs. This would be mainly for the hip joints or sometimes even knee joints may need the hip kit. The hip kit consists of a reacher, sock aid, long-handled sponge, and a long-handled shoehorn. Sometimes the patient will get a dressing stick and elastic shoelaces. Hips and knees may need a leg lifter to get in and out of bed, in and out of the car, or in and out of the tub.
Teaching specific techniques for functional mobility (e.g., safe car transfers, tub and shower transfers, and bed mobility) using appropriate adaptive equipment. Most of the time, they would use a commode. Sometimes I have recommended a shower seat or a shower stool. If the patient has had a bilateral knee replacement and if they have a tall tub, I have also recommended a tub bench. It all depends on how well patients do. We will definitely want to develop a home program to continue care.
As an acute occupational therapist, we play a role in assessing the patient's discharge destination. At the end of two or three days, we need to decide if the patient still requires continual care, if they are safe to go home with home care, or if they are safe to go home and start outpatient therapy.
SNF/sub-acute care. For patients who transition from the hospital to a SNF or sub-acute care, the primary focus would include training on self-care skills, use of adaptive equipment, compensatory techniques, and environmental modifications (from day three to around day 10 after surgery). OT intervention would include ADLs and IADLs related to the patient's discharge environment (e.g., preparing meals, managing finances, home activities such as laundry, etc.).
In the SNF/sub-acute environment, OTs would provide training on functional mobility, such as how to prepare a meal while using an ambulatory device, like a walker or a cane. Furthermore, we would help to prepare the client and family for community reintegration, as appropriate for the client's discharge site. This may include activities such as public dining, shopping or emergency response management. In addition, we would assess the need for recommending potential home modifications and safety equipment to reduce barriers and to promote safe functioning upon discharge. Once the patient is in sub-acute care, it is likely that the patient will go home without home health. OTs can assist with exploring adaptations and compensatory strategies for the patient to return to any volunteer work or paid employment. Finally, at the level of sub-acute care, we want to assess what the patient would like to do in their spare time, to determine whether their current leisure pursuits require modification to continue participation, or assist in the exploration of new leisure activities.
Homecare. Individuals who discharge home from the hospital after surgery may discover that their home environment impedes optimal performance. For example, their actual tub is not the same height as the tub that they practiced with. The space between the toilet and the tub may be too small; the space in the kitchen may not be wide enough for a walker. It is very important to do the home evaluation in the patient's own environment and in the patient's own home. This will ensure increased safety and efficiency of the patient's daily occupation and activities. Placement of grab bars, stair rails, or any other modifications would be much better evaluated, assessed, and implemented if the homecare therapist goes into the home.
Occupational therapists want to make sure the patient manages daily activities while reducing the risk of any injury or further decline of function. Also, they need to find the right balance between the patient's abilities, needed and desired activities, and their home environment, so patients and caregivers can manage safely and productively at home.
In summary, the goals for homecare therapists are:
- ADL/IADL independence
- Medicine management
- To address architectural barriers and make recommendations for safety at home
- Community reintegration
- Fall prevention
- Aging in place
Fall Prevention Recommendations. The occupational therapist is going to encourage exercises to improve strength, balance, and coordination. Proper shoes should be worn to give adequate support. We would recommend general decluttering to avoid tripping over things like throw rugs, extension or phone cords. In the kitchen, clean any spills immediately. For the staircase, ensure proper lighting and use of handrails. Put a non-skid mat inside the tub, and place a non-skid mat outside the tub to prevent slipping and falling. Make sure the bedroom has adequate lighting, and that there is plenty of open, decluttered space for the patient to move around easily with their walker. Finally, as a home care therapist, it is critical to highlight medications with side effects that could potentially lead to a fall.
Goals for Outpatient Therapy
During outpatient occupational therapy, the therapist assists the patient to develop and refine additional skills that will enhance their level of performance at home, as well as in the community. Goals for outpatient therapy include:
- Restoring the current level of independence.
- Preventing occupational dysfunction secondary to aging.
- Improving activity tolerance and work capacity.
- Aerobic exercises.
- Mind and body relaxation techniques to relieve stress and anxiety.
- Proper body mechanics to prevent any further injury or dislocation to the new joint.
Case Studies
I would like to review some case studies as examples of acute care, subacute care, home health, and outpatient settings.
Case Study #1: Acute Care
Mrs. S is a 78-year-old female patient who lives with her husband in a two-level home and has a step-in tub in the bathroom. Prior to surgery, the patient was independent with self-care, meal preparation, and homemaking. She's retired, but she enjoys gardening, walking, and playing cards with her friends. She also is a volunteer as a judge for flower shows in the community. Her increased pain in the right hip has limited her daily activities and she must take frequent rest periods during the day. She was diagnosed with degenerative arthritis in her right hip four months ago and was referred to occupational therapy after surgery for elective right total hip replacement.
Since it was elective surgery, Mrs. S attended the pre-op meeting, where she was informed how the recovery would be, what to do before surgery and after surgery, and what equipment she would require after surgery. She and her husband had already bought a hip kit from Amazon.com, a three-in-one commode, and a rolling walker. They installed grab bars in their bathroom, one close to the toilet and one in the tub. She had installed non-skid mats inside and outside her tub before the surgery. She had prepared meals and frozen them so that all she would have to do when she goes home is defrost and reheat them. Also, she had cleared her bedroom and her living room she would be able to move freely. She had expressed a desire to go home after discharge and would not prefer going to a sub-acute facility.
OT Evaluation: The OT assessment, which is conducted the day after surgery, includes evaluation of:
- Pain: How was her pain during rest and while moving? Was her pain premedicated by the nurses? Before an OT or PT goes into the room, you definitely want to make sure that the patient has been premedicated with pain medications so that they can manage better and they can participate better in therapy.
- The strength of upper extremities and trunk; posture: Her core muscles and her posture were assessed. We wanted to see whether she had an upright posture, whether she leans forward a lot, or if she has any kyphosis.
- Cognition and perception: We evaluated her memory, judgment, safety awareness, retention, and recall of information.
- ADL/IADL, functional mobility, and transfers: We assessed how much help she needed to perform basic ADLs, such as getting dressed, going to the bathroom, cleaning, bathing, getting in and out of the shower, pushing off from the regular height of the toilet. We evaluated her ability to manage pain while performing her ADLs. We observed her competence and compliance in using the adaptive equipment, as well as how cognizant she was of weight-bearing limitations.
- Home layout and accessibility: Was she living in a one-level or a three-level home? Is there a bathroom on the first level? Or does she need to go up or downstairs when she needs to use a bathroom? How easy is it to get in and out of her house, or to go from one level to another?
- Support at home: Does Mrs. S live alone, or with a spouse, family member or caregiver? Does her spouse work away from the home during the day? If so, does she have any family who will be helping her when her husband is working?
Problem List: Her problem list consisted of the following:
- Pain management
- Limited independence due to pain and restrictions
- Anxiety about recovery and dependence on others: She was worried about how her husband would manage, and whether he would burn down the house because he did not know how to cook.
- Inability to ambulate without an assistive device: Using a walker or a cane was degrading for her, and that was her main concern: how am I going to walk without an assistive device.
- ADL dependence
- Limited endurance
- Limited leisure activities: Remember, she loved gardening and walking and playing cards.
- Sleep deprivation: After surgery, sleep deprivation is common due to a variety of reasons (pain, unfamiliar environments, different beds, interruptions from nursing staff checking vitals).
OT Treatment Goals: Post-op day zero to three, the following goals would be set forth for Mrs. S:
Homecare Goals: Post-op day three to two weeks out, our goals would include:
- ADL/IADL training
- Upper and lower extremity strengthening and stretching activities, to improve posture, balance and trunk control.
- Home safety
- Functional activities for standing tolerance and balance
- Meal preparation
- Kitchen activities
- Grocery shopping activities
- Teaching compensatory techniques to modify leisure activities (e.g., how to modify a gardening activity without bending too far forward, using a stool to sit).
- Practicing safe walking with a walker in the neighborhood; maneuvering obstacles and uneven surfaces.
Case Study #2: Acute Rehab Care
Mr. P is a 52-year-old patient who lives with his wife and children in a three-story home. His office was in the basement. His kitchen, living room, and dining room were on the second level. His bedrooms were on the third level. He works as a computer programmer for a private company where he has to travel for work occasionally. He's a very active person who enjoys going to the gym five to seven times a week, playing tennis, and going hiking with his family. He had suffered a sports energy when he was in college and now had severe pain in both his knees. He was not able to hike this summer, as walking on an incline and on uneven surfaces would exaggerate his pain. He underwent bilateral knee replacement (both knees at the same time) at the fast track joint replacement center. After three days of being in acute care, Mr. P was admitted to the acute rehab setting in the hospital for the continuation of rehab.
The first three days, the acute care goals for Mr. P would be very similar to the goals we had for Mrs. S (see above).
Problem List:
- Pain: Pain was substantial and significant and not managed well with the pain medications.
- Postural Hypotension: Every time he would go from supine to sitting up at the edge of the bed, his blood pressure would drop. There were a number of days that we could barely manage to get him out of bed to sit in a chair, and he would have symptoms.
- Significant loss of blood -- poor activity tolerance
- Limited independence due to pain: He was unable to get himself dressed, go to the bathroom by himself, etc.
- Anxiety about recovery and dependence on others: Keep in mind that he was a 52-year-old very active person, who now could not even get out of bed on his own.
- Inability to ambulate without an assistive device
- ADL dependence
- Limited endurance
- Limited leisure activities: Previous to the surgery, he was a very active person who would go to the gym six or seven times a week. He loved playing tennis and going hiking.
- Sleep deprivation
Treatment Goals:
- Pain management while performing self-care: We made sure that this patient had the pain regimen and was always premedicated either before the occupational therapist or physical therapist would start working with the patient.
- Education about total knee replacement (TKR) restrictions and weight-bearing: What are the total knee restrictions? Extreme flexion (i.e., pushing up from the ground level) is restricted because that would need almost 130 degrees of forward flexion. Hyperextension is restricted. Weight-bearing on the surgical leg is absolutely not allowed in the initial stages after surgery.
- Management of orthostatic BP: To manage his orthostatic blood pressure, Mr. P used thigh-high compression stockings and an abdominal binder. Not only that, we started working with him on a tilt-table -- a flat table which gradually inclines, and you take the patient's blood pressure at intervals as the incline increases. We started with zero degrees (flat), then increase by five degrees, increase to 10 degrees -- eventually getting up to 90 degrees. At 90 degrees, the patient is sitting upright. If he can tolerate 90 degrees of tilt-table inclination without becoming orthostatic or hypotensive, or without getting symptomatic, that means he's ready to get out of bed and sit upright.
- Proper positioning while sitting, standing and lying in bed: Mr. P was much better lying on either his right or left side; he was very uncomfortable sleeping supine. We had to make sure that he had enough ankle support to position himself on the sides, having a pillow in between the knees. Whenever you have a knee replacement, you do not want to have a pillow under the knee, because that is going to position the knee in certain degrees of flexion, which would restrict the full extension and limit the full flexion. That's why you have two or three pillows that are supine under the ankle. That maintains the elevation and helps with pain and swelling in both the knees. That was educated and maintained. We also had a little wedge pillow for him just to maintain his position. Since he had both knees replaced, we had to make sure that he puts equal weight on both his surgical knees. Although he was weight bearing as tolerated, we had to teach him how to equally distribute his weight between the two knees, and not favor one knee over the other.
- Bed mobility and functional transfers using leg lifter: Since he had been in bed and he was not able to tolerate upright positioning, sitting, walking and standing, his knee had become very stiff. As such, he could not get in and out of the bed without using a leg lifter. For the first 10 days, he used a leg lifter to get in and out of bed, in and out of a chair, and on and off the mat in the gym.
- Self-care: Mr. P had to use the reacher, sock aid, shoehorn, and the dressing stick to put his clothes on. He did very well using the hip kit.
- Use of assistive device and training of compensatory techniques to safely perform transfers (toilet, tub, and car): He started using the walker for functional transfers (toilet transfer, using a commode, tub transfers, and car transfers). For the first few days, getting in and out of the tub was not practical without using a tub bench.
- Caregiver training: Caregiver education was very important because Mr. P lived with his wife and three children. There were four people to instruct on how to assist Mr. P getting in and out of bed, getting dressed, going from the living room to the bedroom, or going from one level to another (his office was in the basement). They needed to learn where to hold him and what adaptive devices to use for transitioning between levels.
- UE and LE strengthening and stretching exercises: He was used to going to the gym and working out, so we would take him down to the gym and have him do heavy weight lifting. He was fine because he was already conditioned, and he enjoyed that. As an occupational therapist, your goal is definitely upper body and lower body strengthening and core muscles and trunk muscles.
- Dynamic standing balance activities: At day 10, he was no longer orthostatic, and he was able to maintain his static standing. The next goal was to work on his dynamic balance and dynamic activities, such as standing, throwing a basketball, or playing golf.
- Light athletic activity training: Since he was an athlete, we worked on his light athletic activities.
- ADL/IADL training
- Work simplification and energy conservation training: He had lost so much blood, and his activity tolerance and his endurance had become low. We had to modify his work schedule and teach him how to conserve energy and simplify his work.
- Safety at home
- Transition to outpatient services
Outpatient Goals:
After two weeks of acute rehab, we transitioned Mr. P to outpatient services. Coming from the acute hospital setting to the outpatient setting, these are the goals we set for Mr. P:
- Continued high-level ADL/IADL training: OT worked on driving, meal preparation and work
- Workplace simplifications and modifications: He had a computer job that entailed sitting for a long period of time. The outpatient therapist made a recommendation of having a little step stool under his desk so he could rest his legs on the step stool. He was also encouraged to getting up and stretch often, strengthening his upper body and lower body while he is working.
- Driving adaptations: He drove a van, which was pretty high off the ground, so there wasn't much of an adaptation needed there. However, if he ever needed to get into a low car, we recommended putting a cushion or a pillow on the car seat so that his hip is higher than the knee.
- UE and LE strengthening and stretching exercises: He was encouraged to perform these exercises while working at his desk, and while away from his desk, to maintain his strength and range of motion in his both knees.
- Use of adaptive devices (rolling walker, cane) for functional mobility: When he was discharged from the acute rehab setting, he had already graduated from the rolling walker to the cane. The goal for the outpatient therapist was to make sure Mr. P could safely function and transfer and perform his ADLs and IADLs using the cane.
- Teaching compensatory techniques to modify leisure activities: He loved going to the gym and playing tennis. The OT had to teach him how to modify his leisure activities and compensate with his bilateral knees.
After four weeks, Mr. P went back to work and began driving again. He visited me after three months. He expressed that he was very happy because he was able to go hiking again with his family. He was very thankful for his total knee replacement surgery, and for the occupational therapy and rehab, he had received.
Case Study #3: Sub-Acute Setting
Mrs. J is a 64-year-old widow who lives alone in an apartment. There are 12 steps to enter her home. She has a walk-in shower. She also works part-time as a librarian in a local library. Three days a week, she takes care of her two grandchildren (five and seven years old) after they get out of school. Due to the pain of arthritis, she underwent left knee replacement. After her hospital stay, we decided that she would need the services of a skilled nursing facility because her pain was not managed. Also, she lived by herself and she did not have a support that would allow her to go home independently. She was admitted to a SNF on post-op day four for rehab.
SNF OT Goals:
- Education about total knee replacement restriction limitations and weight-bearing activities.
- Pain management protocols and skills while performing self-care.
- Proper positioning while sitting, standing, and lying.
- Bed mobility and functional transfers.
- Self-care (dressing, toileting, bathing)
- Recommendation of the appropriate use of adaptive devices (e.g., rolling walker, cane) for functional mobility. For the first week, she definitely had to use the rolling walker because of the pain and instability of the knee joint. Then she graduated to using a cane while she was in rehab.
- Use of assistive devices and training of compensatory techniques to safely perform transfers (toilet/shower/car). She had a very low car, so we recommended using a thick pillow to sit on so that she is in a higher position when she gets out of her low car.
- UE and LE strengthening and stretching.
- Dynamic standing balance activities
- IADLs: Since she lived alone, the goal was when she goes home, she should be able to manage all the IADLs independently (meal prep, laundry, house cleaning, grocery shopping, and driving).
- Workplace simplification and adaptation: She was a librarian. We had to recommend some modifications and simplifications for her place of work. Again, we recommended sitting on a high chair and not in a low chair, and also having a little step stool under her desk so that she can elevate her affected knee. We advised getting up between every 30 to 45 minutes to stretch her upper and lower body and correcting her posture.
- Safety at home and at work.
- Transition to outpatient services.
Future Directions for Occupational Therapy
I already mentioned some of the approaches and the surgical techniques that have been instrumental in advancing total hip and total knee replacement surgery. In addition to those innovations, we are entering the era of a fast track joint replacement surgery. Gone are the days of conservative surgery, where the patient would stay in the hospital for three, four or five days, and then transfer to sub-acute care. Many surgery centers throughout the country are transitioning to same-day elective surgery, for patients that are healthy with no comorbidities. They come in the morning, have surgery, stay in the post-anesthesia care unit (PACU) for three or four hours, and then go home. The home care agency will offer nursing, occupational therapy, physical therapy -- everything that is available in acute care -- to be administered and carried out in the patient's home. As such, occupational therapy has a critical role to play: for the pre-op education and assessment, as well during recovery immediately after the procedure, and safely transitioning the patient to their home environment.
Commercial and Medicare reimbursement is getting tighter and tighter every day. In other words, reimbursement for all care providers (including surgeons, hospitals, homecare) is going to be limited. We have to optimize our services to the best of the patient's benefit. This is where bundled payments come into play. Bundled payment arrangements are designed to pay multiple providers for coordinating the total amount of services required for a single, pre-defined episode of care. Hospitals are given a certain amount of money to manage a knee replacement patient, for example. The goal of the hospital is to get all the money for the treatment and interventions they do in the hospital. Let's say the hospital gets $5,000 for surgery. That money needs to be distributed across all of the providers who care for that patient, whether the treatment is given in a sub-acute environment, or if they go home and have home care therapy. Of course, home care is much cheaper than sub-acute care. Hospitals will try to keep the patient as long as they are safe to go home, versus recommending subacute care. If the hospital recommends sub-acute care, they have to share that bundled sum of money with sub-acute care providers, which is more expensive than home care. Having said that, the role of occupational therapy will become much more important and critical in-home care agencies, in-home care services, in the community, and primary care.
Fast Track Joint Replacement Surgery
Fast track joint replacement surgery is a very structured and organized program. First, the patient receives pre-op information and education. They are informed about surgical procedures, expected length of stay (generally less than three days), pain management, exercise before and after surgery, nutrition, and the role of occupational therapy and physical therapy.
During their surgery, they do not receive general anesthesia -- they will undergo spinal anesthesia and a nerve block. They can have multimodal opioid-sparing analgesia (IV Tylenol, NSAID). They will have several daily mobilization sessions. PT sees them on post-op day zero. If they had surgery in the morning, PT will get them up and work with them on the day of surgery. Then nursing mobilizes them. They take them for a walk on the day of surgery. Day one, they have one or two sessions of OT. Two sessions of PT. Day three, same thing. If they stay after two days, all the three days in the afternoon and in the evenings, they will be mobilized by nursing. They have no drains or catheter. They receive no benzodiazepines, which cause sleepiness and lethargy. The majority of patients (91% to 92%) who have fast track joint replacement surgery go directly home, versus going to a sub-acute facility.
Lastly, after the patient goes home, the pain medications and the analgesic regimens continue as necessary. They also have daily homecare rehabilitation services. Everyone will have physical therapy. If recommended, some of them will have occupational therapy as well. They will continue working with the homecare therapy team for two or three weeks, depending on the patient.
Outpatient Total Joint Arthroplasty
Most of my unicondylar knee patients would have surgery, go home the same day and begin homecare the very next day. Healthy patients are generally able to take this pathway. A lot of surgery centers are trying out this program.
The advantages of outpatient total joint arthroplasty include:
- Reduced hospital stay (there is no overnight stay)
- Reduced chance of hospital-acquired infection
- Possibility of increased patient satisfaction
- Potential for a reduced cost to the health care system
Some disadvantages include:
- Chance of having a complication at home
- Difficulty with pain management when the nerve block wears off
- Chance for readmission to the hospital
If a patient chooses outpatient same-day TJA surgery, the role of the occupational therapist will be vital, from conducting the pre-op assessment and intervention to acute care, and finally transitioning to home care. Healthcare reform implementation and bundled payment systems may lead to an increased contribution of OT services in the primary care setting, as well as in the community, allowing people to age in place.
Summary and Conclusion
In conclusion, best occupational therapy practices are evidence-based, occupation-focused, and highly dependent on client satisfaction outcomes. Whether you work in an acute care hospital or you are a practice owner, there's something out there that can help advance your practice. It may be a piece of technology, a marketing technique, or perhaps an educational opportunity similar to this webinar.
I have included a slide with all of my references and links to useful websites with a lot of informational videos. One of my favorite resources for the total hip and knee is the American Association of Orthopedic Surgery. The AJRR and AOTA also have different fact sheets and articles for activities after hip replacement, activities for acute care, activities, and role of OT for hip replacement and knee replacement in subacute care, home care, outpatient, and home health agencies. Another resource that I would encourage you to access is information on the MAKOplasty and the PRL. If you type "MAKOplasty" into a search engine, you will find a lot of information and demonstration videos, such as how the surgeon exposes the joint, what incisions they make, and how the patient recovers after surgery.
I would like to thank OccupationalTherapy.com for giving me the opportunity to share my knowledge and skills with you. Thanks to all of you for participating in this webinar. If you need more information or if you have any questions, please feel free to e-mail me at msheth32@gmail.com.
Questions and Answers
Is the bundled payment like a prospective payment system?
Yes, it is like the PPS system. In a subacute setting, you definitely have the dollar amount. In outpatient settings, you have not only the dollar amount but also the number of visits. The bundled payment is similar to the prospective payment system and the number of visits.
In reference to nutrition, what does the pre-op information entail?
We recommend having a high protein, high calcium, and low carb diet, particularly for the healing of the fracture, because they do surgical removal and fracturing the head of the femur. If the patient is diabetic, then you do not want them to consume a lot of sugar or carbs. Also, we recommend reduced consumption of caffeine, tea, coffee, and alcohol 10 days before surgery. As far as the medication is concerned, they cannot take any blood thinners 10-14 days before surgery.
Are you able to adequately conduct your pre-op assessment when people move quickly through the facilities, due to shortened stay and limited time with each client?
Yes, I have been able to manage. In the pre-op class, sometimes there are 10-12 patients in attendance, which is a small enough group to address. If they have more issues, they can always call me. I have also used Facetime, where they show me their home situation. I can see the bathroom and the height of the bed over Facetime. I can instruct someone where to put the step stool, or where to install the grab bars, etc. When they are admitted and have only two days, I would ideally like more time, but that doesn't happen all the time.
I would think that a person who has outpatient surgery needs a caregiver who is cognitively and physically able to assist at home.
Yes, an outpatient needs a very supportive and able caregiver at home to assist. If your patient is not physically able to be independent at home safely, then they do need a caregiver who can support and provide the level of assistance they need. That's why not many centers have been doing it. A very select group of surgeons in the Midwest started this program as a pilot program.
Citation:
Sheth, M. (2017). OT's role in joint replacements. OccupationalTherapy.com, Article 3963. Retrieved from http://OccupationalTherapy.com.
