Kiley: I am excited to be here. I just want to start by introducing myself and share a little bit more about my own experience. I am passionate about this topic because my son was stillborn in 2005. It is from my own experience, which was inadequate both in the hospital and afterward, that I am passionate about making the experience better for other parents. I do not want them to have to be alone, feel isolated, and suffer. Through this, and through the film my husband and I created, I had the idea to create retreats for moms who have experienced a pregnancy or infant loss. Many people with this type of loss talk about the isolation they feel so I wanted to create that community. Through this process, I realized what a huge part mental health plays in a loss, and that is why I am talking about this. I want to try to help reduce the trauma and the symptoms that arise. How do we increase healing and resiliency in this population? I started my own center for healing, which is a virtual center, and I also became involved in 2020 Mom, which is a non-profit that focuses on closing gaps in maternal mental health. I wanted to make sure that the baby loss community was represented in the larger conversation about maternal mental health.
I am an OT. And as such, I want to make sure that this topic is also being included in curriculums. I know that infant mental health is, but often maternal mental health is not included in our education. We need to recognize that the infant's mental health is interdependent with the mother's mental health and that we cannot really separate the two. We have to look at them together. This is why I am here today. I want to share some basic knowledge about perinatal mental health, and then in Part Two of this series, we will talk more about how OTs can incorporate this into their own practice depending on where they work.
Mothering & Mother-Infant Co-Occupations
The "Motherhood Mindset"
In a book by Olson called, The Motherhood Mindset, it looks at the mom/woman and her lifestyle as being transformed. She is in this transition of her life from not being a mother to being a mother.
- Pregnancy = Active Participation
- Caring for the developing fetus
- Caring for the self
This starts during pregnancy with an active participation in caring for her developing baby. She also has to take care of herself. If she is not taking care of herself, she is not taking care of the baby. There are choices that she has to make in this process (Esdaile, S. A., Farrell, E. A., & Olson, J. A., 2004; Ruddick, 1994; Stern & Bruschweiler-Stern, 1998).
I think pregnancy is an occupation in itself. It is a right of passage. During this time, this is where an attachment is happening. A bond between a pregnant woman and her baby starts in the womb. We do not say, "A 'fetus' is growing in me," but rather, "My baby's growing." We know at each stage what the baby looks like and how they are developing. Thus, we attach "personhood" to the baby that is growing inside.
Expanding this just a little bit, I want to consider adoptive parents, They did not get that attachment period during pregnancy to bond with the baby. There are also moms who give their babies up for adoption. There can be a lot of trauma that is found in those moms. I have read that up to 30% of those moms become sterile because of the guilt and shame that is associated with that.
With people who are experiencing infertility, how does that impact their view of themselves and their mental health? There is a lot of guilt, shame, and blame about not being able to get pregnant and/or carrying a baby to a certain point. There are other scenarios that are important to consider, but I am going to stay pretty basic for this part of the talk.
Motherhood and Co-Occupations (Olson, 2004)
Looking at motherhood and co-occupation, the mother's primary occupation in this role of mother is parenting. It is to take care of her baby, but the role of the mother is not independent and not in isolation. It includes the baby. In our society, the expectation of a mom is that her primary occupation is to care for the child. The partner may share in this, but our society puts ultimate responsibility on the mom. If the mom is working full time, her role changes. She still often has to assume this new role, but also continue her other roles and responsibilities, which can be quite overwhelming. This is the way things work for most families in America.
In every occupation of caregiving, there are two actors (Zemke & Clark, 1996). We are looking at co-occupation with a mom and a baby, like feeding and eating. The mom would be feeding and the baby would be eating. For example, how can we support moms in breastfeeding? For some moms, breastfeeding can trigger more anxiety and lead to psychosis. They are feeling anxious already and then they can get the societal and hospital pressure to breastfeed. If they choose not to, we need to support those moms in their choice as well. Another example is sleep. How does the mom assist the baby in soothing and falling to sleep and maintaining that sleep? The baby is the one sleeping, but it is still a co-occupation. Crying and consoling is another. If the baby is crying, the mom is part of this interaction by consoling the baby.
A baby may have low weight gain, and this can negatively impact a mother's image. She might feel bad about herself and shameful. Getting a baby to sleep and staying asleep impacts the entire family and can create strain and tension in the family. There can be negative perceptions of that infant and decreased confidence in parenting. Those interactions really impact the mom and the entire family. Another example is communication, and in particular, crying. If the baby cries, its crying usually leads to some type of action by the mom to comfort the baby. If it is hunger, the mom will try feeding the baby. They may need a diaper change or a change the clothing if the baby is too hot or cold. If the baby is tired, the mom is going to soothe and console the baby to sleep. Mothers and infants are so intertwined on a daily basis in their co-occupations (Dunlea, 1996).
Occupational Performance
Occupational performance looks at the occupation, the individual, and the environment. I want to stress that looking at "the affective environments surrounding these co-occupations is as important to the development of the infant as the actual performance of the co-occupation (Olson, 2004, pg. 48)." The affective environment impacts the physical, mental, and emotional development of that baby. For OTs, supporting the occupation of mothering is significant. If we are to maintain a mother's ability to respond to the needs of the infant, we need to support the mom's mental health and her needs so she is effectively able to parent her child. An infant cannot regulate their emotions yet, but they can learn how to manage their emotions through their interactions with their caregivers. They look to their caregivers for cues. This is why it is important to be aware of the mom's and the dad's affect and their mental health.
Mental Health Disorders
I want to now give you a short review and definitions of maternal mental health disorders (Figure 1).
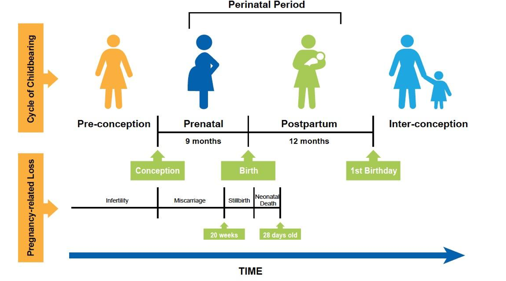
Figure 1. Overview of perinatal period. Used with permission from CA Task Force.
Perinatal is the time from conception to the child's first birthday. It includes pregnancy and postpartum. Looking at pregnancy-related loss, and we will talk a little bit more about this, infertility is the range of pre-conception, and then miscarriage is anywhere from conception to 20 weeks gestation. These are definitions in the United States. The definitions differ elsewhere. Stillbirth is the period between 20 weeks and birth. Finally, neonatal death is birth to 28 days of life. I will review the loss definitions later, but here, maternal mental health disorders include a range of disorders. They include depression, anxiety, OCD, and psychosis. These can occur during the pregnancy or within the postpartum period, so it is not only postpartum. We need to be aware of what is going on during pregnancy. When left untreated, these disorders can cause devastating consequences to the mom herself, her baby, and her family. This is why this is important to look at mental health during this period as it affects everybody in the family. This image, (Figure 1) is from the California Taskforce White Paper. They met for a year and wrote up a white paper with recommendations for maternal mental health in the state of California. It is in the reference section, and it is a really great document. I encourage everyone to read it. Some of this information is pulled from there, but it goes into much deeper details there.
Baby Blues
Here are the symptoms of the "baby blues."
- Increased emotional sensitivity
- Weepiness
- Feeling overwhelmed
Baby blues are an increased emotional sensitivity, weepiness, and a feeling of being overwhelmed. These symptoms can occur up to two weeks postpartum. It affects 80% of new moms. That is a lot of people, however, it typically resolves untreated within the first two weeks. The baby blues are not considered a mental health disorder because it is common, (80%), has a shortened duration (two weeks), and is generally less severe (California Task Force on the Status of Maternal Mental Health/2020 Mom, 2017). What we are going to talk about today are the more severe and long-lasting mental health issues that come up in this perinatal period.
Most Common Pregnancy Complication
Maternal mental health issues are the most common pregnancy complication. If you look at gestational diabetes, this occurs in about 2 to 10% of all pregnancies. Preeclampsia is at about 10%. Both of these are screened for during prenatal care. However, depression and anxiety in pregnant and postpartum women are at 20% (Figure 2).
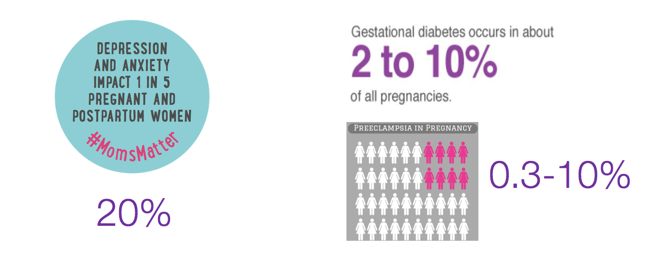
Figure 2. Statistics of common pregnancy complications (Copyright by permission 2020 Mom).
Depression and anxiety are double that of gestational diabetes and preeclampsia combined (Ananth, Keyes, & Wapner, 2013; Committee on Obstetric Practice, 2015; DeSisto, Kim, & Sharma, 2014; Gavin et. al. 2005; Fairbrother, Janssen, Antony, Tucker, & Young, 2016; Ryan & Kostaras, 2005; Sontag-Padilla, Schultz, Reynolds, Lovejoy, & Firth, 2013; Stewart, Robertson, Dennics, & Grace, 2003). And, this is not being screened for routinely at the moment. We are trying to increase screening and treatment because it is preventable and treatable.
Perinatal Mental Health Statistics
Here are some other quick statistics that I think that you will find interesting (Byatt, Levin, Zidonis, Moore Simas, & Allison, 2015; Ananth, Keyes, & Wapner, 2013; Committee on Obstetric Practice, 2015; DeSisto, Kim, & Sharma, 2014; Gavin et. al. 2005; Fairbrother, Janssen, Antony, Tucker, & Young, 2016; Ryan & Kostaras, 2005; Sontag-Padilla, Schultz, Reynolds, Lovejoy, & Firth, 2013; Stewart, Robertson, Dennics, & Grace, 2003).
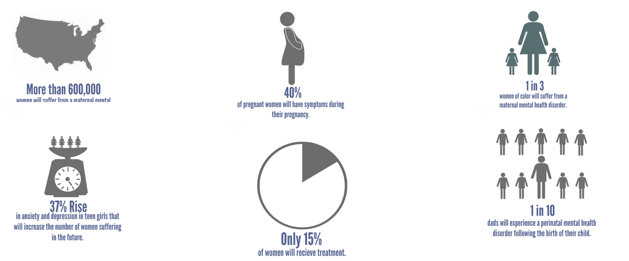
Figure 3. Perinatal mental health statistics (Copyright by permission 2020 Mom/Blue Dot Project).
More than 600,000 women will suffer from a maternal mental health disorder in the United States every year, and 40% of pregnant women will have symptoms during pregnancy. Are they being screened or not? One in three women of color will suffer from a maternal mental health disorder, and we will look at risk factors later. Poverty is a huge risk factor for developing a maternal mental health disorder. There is rising anxiety and depression in teen girls, which will then be a risk factor for when they are pregnant and increase their risk of developing prenatal and postpartum depression or anxiety. Only 15% of women will receive treatment, so of that 600,000, not that many are being treated. Dads also get perinatal paternal depression. One in 10 dads will experience this.
Types of MMH Disorders
These are types of maternal mental health disorders that you may have heard about or seen in the past. Again, we are stressing it is not just postpartum but in pregnancy as well. This is why it is really important to screen during the pregnancy period (Gavin et. al. 2005; Fairbrother, Janssen, Antony, Tucker, & Young, 2016; Ryan & Kostaras, 2005).
- Pregnancy/Postpartum Depression (PPD)
- Pregnancy/Postpartum Anxiety or Panic Disorder
- Acute Stress/Post-Traumatic Stress Disorder
- Perinatal OCD
- Bipolar Disorders
- Postpartum Psychosis
The Language of Postpartum Depression
I wanted to share with you some of the language of postpartum depression that we often hear in Figure 4.
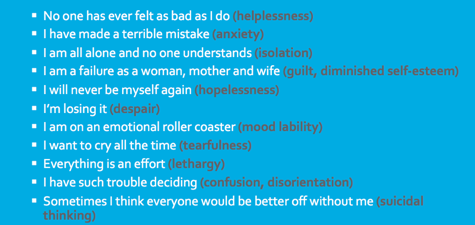
Figure 4. The language of postpartum depression (Copyright Diana Lynn Barnes, 2018; reprinted by permission only).
