Traci: Good afternoon, everybody. Thank you so much for taking the time today to advance your knowledge on the role of person, place, and aging in place. I want to start by sharing a few things about myself. I am an occupational therapist and currently practice in home health. I have worked in many settings, such as outpatient rehab and skilled nursing. I also work at the university as a study interventionist.
What is Aging in Place?
Aging in place is the ability to live in one's own home and community safely and independently, and comfortably, regardless of age, income, or functional ability level (CDC, 2013). Further, aging in place means that adults seek and engage in daily activities both in their home and the larger community.
How many of you have heard the term Silver Tsunami? There are 46.2 million people that are 65 plus. That is about one in every seven Americans, or 14.5%. The elderly patient population has increased 28% since 2004 in contrast to an increase in the under 65 population of only 6.2%. The baby boomers are getting older and now range in age from 52 to 74. This population is expected to double from 46 to 98 million by 2060. The 65 and older people will make up 24% of the people, versus 15%. The life expectancy in 1950 was approximately 68. In 2013, that number jumped to 70. In general, individuals are living longer due to the increases and advances in medicine. I currently have five individuals over 90 years old on my caseload, and the most senior patient I have seen is 104 years old. She is cognitively intact and full of arthritis, but she is quite spunky. Ten years ago, my most senior patient was about 79 or 80. We must be doing something right.
Aging
Normal Aging
Normal aging is not a disease, and this is a new concept. People are living longer despite their chronic medical conditions. It is important to understand normal versus disease-related changes, and its impact on the aging population, or the "Silver Tsunami." One of my typical signs of aging is that I can no longer document on my computer in the evening without wearing a pair of cheaters. If I do not wear the cheaters, I have a challenging time completing my tasks. I also use many stickies to remind myself of things that I need to do throughout the day.
Age-Related Sensory Changes
There can be some age-related sensory changes. This is another key topic that you are going to want to zoom in on. These changes occur in vision (as I mentioned), hearing, touch, olfactory, or in the way they smell or taste things. An example might be decreased driving at night. Many people start to have problems with this, especially when it is raining and dark due to the glare. Other visual changes may include a loss of focus and a general decline in vision sensitivity or contrast. An example might be a decreased ability to see brown carpeting against brown wooden steps as it is too close in color. A visual and olfactory example is not being able to see or smell spoiled food. Hearing is another age-related sensory change. Over time, they have a gradual loss. They may need increased time to process information. Women tend to have more difficulty hearing higher frequencies versus men and need more time to process things. You may also notice some of your patients saying things like, "I could not understand the phone message that was left on my answering machine." They might say that the person who left the message spoke too fast. They could not hear, so they could not understand. Often, my clients have a hard time remembering when I am going to arrive for their visit. I also see this a lot when folks try to make a doctor's appointment with their primary care physician. They get confused with all the recorded options like, "Press one for the nurse. Press two for authorizations. Press three if you want to make an appointment. Press four if you want billing." I think this is also true when they try to renew a prescription over the phone. For example, Rite Aid will allow you to call in to renew your medications, but several questions need to be answered correctly first. Again, age-related sensory changes include the sense of smell. Older folks may have trouble smelling gas. I had one client who could not detect the smell of gas and had a small explosion in her home. This could have been avoided had she had a better smell. Some detectors can be used as a modification. Another example is a client might wear a lot of perfume or cologne because they cannot smell it. Taste also declines, and clients may not be thirsty or have a lack of appetite as all food tastes "the same." Lastly is touch. Skin gets thinner and more fragile. They quickly get bumps and bruises with something as simple as bumping their leg on the end of the bed. Their sense of pain and temperature is also altered. These folks often have a higher threshold for a tactile response.
Age-Related Cognitive Changes
Let's talk about fluid intelligence versus crystallized intelligence. Fluid intelligence refers to the capacity to learn new information, reason, and the ability to problem-solve for familiar solutions that are not evident. It gradually declines throughout midlife until age 60, and then the decline becomes very rapid. A good example of fluid intelligence is determining an alternative route to work if the traditional way is closed. Crystallized intelligence refers to over-learned familiar skills and knowledge. It remains operative throughout your lifespan. There is an ability to show an increase in this in your 70s and 80s. A good example of crystallized intelligence is making chicken soup. Some people can make chicken soup the same way that they did when they were 20.
Let's now talk more about the cognitive change that you can have with your memory. Mental changes are variable. You may observe a decrease in short-term memory; an example is being able to pay attention. Another example is difficulty attending to new concepts. Speed of processing information declines in long-term memory as well. It becomes more of an effort to retrieve information. New learning for familiar tasks is also affected. A short-term example might be that your client takes the same medication every day, but all of a sudden, they start forgetting what time to do that. An example of a long-term decline might be forgetting the names of extended family, like cousins. This is my favorite, Age-Associated Memory Impairment, or AAMI. How many of us can identify with this? A client may think or recall information a little slower. Again, they may have trouble paying attention, and it takes more time for them to organize information.
These are all signs of cognitive decline that occur as part of the normal aging process. The good news is that someone can improve based on effort and environment. A good example might be running into someone you have not seen in a really long time. The whole time you may be thinking, "Wow, I can't think of this person's name, and "I should know this person's name." Half an hour later, you are walking through the mall and remember, "Oh yeah, that was Sam."
Lifestyle Habits
When you think about the person, you also need to think about their lifestyle habits. Habits and routines are important performance patterns that all humans develop, often without thought. They help us to increase ease and efficiency when performing daily tasks. Habits are automatic behaviors. Routines are established sequences of occupations or activities. Both habits and routines can be positive and negative. They are often hard to change when completing an occupation or activity in an environment. What are some daily habits or routines?
Participants' responses include cooking dinner, gardening, brushing teeth, walking the dog, driving the same route, and making coffee, kids' lunches, or the bed.
I have an 80-year-old mother-in-law who, all her life, has washed her kitchen window. There is no good way to access the window. She insists on pulling a chair over, putting one leg in the sink, and keeping one leg on the chair to clean the window. This is an example of how it is hard to change the activity or the occupation in an environment. She is resistant to changing this routine.
Other things to consider with lifestyle habits are shown in Figure 1.
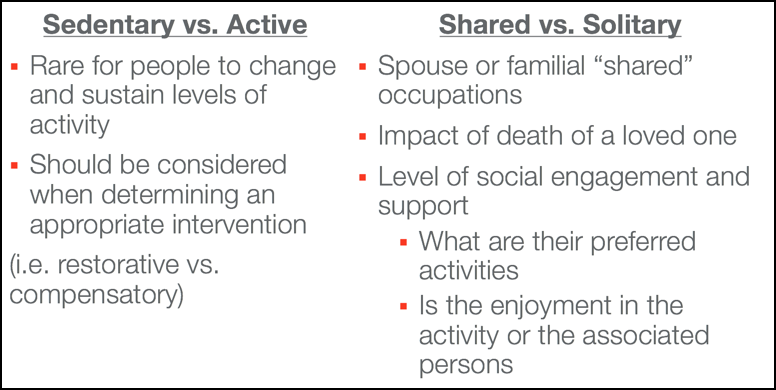
Figure 1. Lifestyle considerations.
It is rare for folks to make a change or sustain a level of activity. Think about this when you are looking at an intervention. For example, someone said making the beds is an example of a routine. Sometimes a person makes a bed a certain way. You can make a suggestion, but you are in their environment. They think their way works, and they have not had any trouble to this point, so they will continue to do it that way. Shared versus solitary is another consideration. Does the person share a particular occupation with a spouse or a family member? Imagine if a person's loved one dies. What would be the impact on that particular activity? Sometimes it is not necessarily the activity, but rather the enjoyment of doing that activity with a husband, wife, daughter, or son.
Case Example- Mrs. H.
Mrs. H. is 80 years old. She is a retired seamstress and a mother of four. Typically, she is not a physically active person. She enjoys church, gardening, and spending time with her grandchildren. She lost her husband 11 years ago, and she was used to them doing everything together. They had a huge garden, attended many church activities like bingo and prayer groups, and liked to travel to see the bishop. Since her husband's death, she does very little because her engagement was based on her husband's togetherness. Her lifestyle habit was active and shared.
Case Example- Mrs. R.
Mrs. R. is also 80 years old. She is a retired medical social worker and has never been married. She has traveled abroad to Germany, France, and Spain. She likes to take a five-mile walk every day. She enjoys hiking, playing tennis, golfing, and reading. In contrast to Mrs. H, she is an energetic, out-going person. Her lifestyle habit is active and solitary.
Disease-Related Conditions
Clients with disease-related conditions may have a more challenging time aging in place. Co-morbidities are two conditions that exist side-by-side by chance. Examples are arthritis and diabetes. What are some other examples?
Participants' responses include Diabetes and amputation, CHF and edema, stroke and low vision, stroke and UE spasticity post-stroke.
A secondary condition is a condition that results from the primary condition. Associated conditions are more likely to occur as a result of a primary condition. An example would be Lewy body dementia and Parkinson's disease. What do we do when we have folks that have multiple conditions and associated conditions? I have a patient right now that has about 10 co-morbidities and about six secondary conditions. He is 96 years old and went to the hospital to be treated for the flu. A nurse was seeing him at home, and when his oxygen level went down to about 60, they put him in the local hospital. With a case like this, it is hard to figure out what to address. I think his most difficult issue is CHF, so we started there. He had a lot of breathing issues before he went into the hospital.
Common Conditions in Older Adults
On average, four out of five adults have at least one chronic condition, and about 11 million live with five. Many of these fall into the categories of cognition, pain, and mobility. I would say, on average, most of my clients have three chronic conditions. For example, I have a client who sustained a left-sided stroke, a weakness, and a history of diabetes, functioning well within her home. With the changes in the weather, she now has hip pain. She is having difficulty with bathing and dressing, which she could do independently despite the post-stroke weakness. The cold and dampness have affected her joints, and now she is in a tremendous amount of pain. She went to the doctor and said, "I'm having pain, not walking as well, and I can't get in and out of my shower. I can't bathe other than at the sink." I have been seeing this lady for the past two weeks to address these issues.
I see many clients with Alzheimer's disease, vascular dementia, or an executive function impairment due to delirium. I have also seen many people lately with delirium associated with urinary tract infections that they did know they had. Unfortunately, I have seen depression so severe, like with the loss of a limb, that a client's cognition becomes impaired. It can be so affected that it impairs their performance in daily tasks like medication management. Depending on the type of cognitive impairment they have, they can decline, maintain a baseline level, or improve occupational therapy.
Another common condition in older adults is pain. Pain is usually a secondary or an associated condition. Pain is often due to not having cartilage in certain joints as with arthritis or a general stiffness from lack of mobility. Many have had the flu these past few months. Immobility on top of arthritis or chronic joint pain is going to make things worse. I have a patient with chronic back pain, and before getting the flu, she was doing great. Now, her pain is through the roof. We often manage these people through compensatory strategies. The most important thing we can do is try to engage them in occupation to have a positive impact. However, sometimes with pain, it is really hard to change someone's behavior. It can be due to the environment, cognitive issues, or inflexible routines and habits. Some ideas may be to set up a two-week trial and focus on a client-centered plan. I ask them what their goal is and how they think they can achieve it. Using the client with chronic back pain as an example, her goal was to get out of bed. When asked how she would do it, she replied, "I'm just getting up." I responded, 'How else could you do that?" Sometimes patients cannot figure that out, and they need help. In this case, I gave her some ideas of how to move to reduce strain to her back. Working with the client and asking their opinion can help to win them over. You can then see how they respond to that and adjust the plan and goals from there. Perhaps, my next step with her could be to offer adaptive equipment, like a bed cane, or lowering her bed. We also want to encourage these clients to walk and do some kind of exercise. Chair exercise is great. I encourage them to incorporate walking into their homemaking and activities of daily living.
Mobility is a secondary or an associated condition as a result of a lifestyle habit. It is the condition that all the patients and providers recognize the most when talking about problems. There is also strong evidence that links mobility to disability. I absolutely love when I go into someone's house and say, "What do you want to be able to do?" and the first thing they say is "Walk." I like to say then, "Are you going to walk clothed or unclothed?" Often, they will not know what I mean, so I go on to say, "Do you normally get up at your walker or your cane and walk without your clothes?" Once you start opening that dialogue, they often understand and can identify other goals. It is important to set manageable and doable goals and praise them. "Where do you want to walk? What do you want to do when you get there?" This can initiate a conversation about ADL and IADLs. We also want to be supportive and make sure they feel safe. Normally, if they are having trouble with mobility, we know that they are most likely having trouble with their daily living activities and taking care of their home.
Case Example- Mr. D.
Mr. D. is an 88-year-old man. He resides in his home with his wife. He's a retired auto mechanic and had his own garage. His diagnoses include elevated blood pressure, arthritis, left rotator cuff injury, and multiple fractures to the right and left uppers. He also has diabetes and poor posture. At the time of my intervention, he was doing okay with the driving a little over six months ago. Now, he has a new diagnosis of Parkinson's. The doctor has just requested that he have a driver's evaluation due to a recent accident. When he came up the driveway and stopped the car to get the mail, the car rolled down the driveway and hit the garage, scratching the entire driver's side of the car. I am not 100% sure if he put it in park. He also reports his walking and ability to complete his ADLs are declining. He has increased pain and is very frustrated.
When I met him for the second time, I felt compelled to really dig into what he was upset about. It all hinged on driving. I talked with the doctor, and he completed a driver evaluation. The bad news is he did not pass his driving test. He failed to stop at stop signs and did not park in the handicap spot correctly. He parked across horizontally instead of vertically. Some other cognitive things were going on besides the Parkinson's that might have been tied into his nutrition and diabetes.
Intervention with Mr. D. has focused on him doing exercises and increasing his walking. We are working on him to do some of the things that he used to do in the kitchen for his wife, which was cook breakfast and get dinner together at the end of the day. He was told that he could take the driving test one more time. I do not know if, in fact, he will pass as I was not in the car the first time, but he definitely has some judgment issues. I know that the increased pain and frustration stem from the fact that he cannot do something that he really wants to do. It is amazing the decline I saw from the first time that I worked with him to the second.
Defining the Person in Aging in Place
We all have habits and roles within our lifestyle. Roles are functions assumed by a person, and each person's roles in life differ. In addition to roles, each person's environment influences their roles either positively or negatively. These influences are also affected by age-related and disease-related conditions. What roles does Mr. D. have? He is a husband, chauffeur, community member, cook, food enthusiast, driver, social, father, etc. He only just closed his business down, so he is a provider as well.
He had normal aging-related factors: cognitive decline, arthritis, decreased mobility, and pain. I recommended that he go for an eye exam to rule that out for driving. Some of the disease-related conditions were loss of range of motion, decreased proprioception, PD, elevated blood pressure, and poor judgment. He also had intention tremors. He has both normal age-related mixed with some disease-related conditions. What could be the plan?
Participants' responses include public transportation, home modifications, increased exercise, support from friends, compensatory strategies, adaptive equipment, safety assessment, psychological support, medication management, diet education.
These are great ideas. A caregiver did some things for his wife, but he did not like that option for him. I provided him information about changes that he might experience and gave him specific exercises for maintenance. Medication management and diet education were other areas that I could address as I am not sure he was eating the healthiest diet. He had a favorite lunch spot, but I also think that breakfast was a donut or something like that. Ideas for cognitive and safety assessment might include asking him to give directions to get to a certain place or to talk about his knowledge of his auto mechanic experience. I could also assess judgment issues during ADLs and IADLs. Where he lives, they have a North Hills Community Outreach program, and they have Rides for Seniors. I suggested this as a way that he could still go to his favorite place or perhaps volunteer at another garage a few hours a week.
Best Practice Strategies
You need to listen to your client's goals/wishes and refrain from talking or imposing your own goals upon them. As a younger therapist, I was definitely guilty of thinking that all clients needed to dress independently. However, this might not be a goal of your client. Do they have any expectations from their family members or society? In this case, this gentleman had a daughter and a few sons. One son expected that his Dad would be able to drive. This is where we might run into a little bit of trouble. Have the person prioritize what is most important to least important. I try to get clients to list five things they really want to work on, and I ask them to prioritize them from one to five. One is the most important. Five being the least important. You then have to think about all the disease-related and age-related changes that might affect their ability to do these chosen tasks.
COPM
The Canadian Occupational Performance Measure, or COPM, is a structured interview that helps guide strategies. It is a semi-structured interview that allows an open dialogue between client and therapist. I started using the COPM to guide my home health evaluations. I like it because it is very client-centered, and I think that it helps focus the situation. The insurance industry has put many constraints on OTs with a decreased number of visits, the need to justify services, and the need to show good outcomes for reimbursement. The COPM has clients identify and prioritize everyday issues that restrict or impact their daily living. One of the strengths is that it has a broad focus. It covers all the areas of life, including self-care, leisure, productivity, and it goes through the lifespan. What I most love is that it is designed for OTs. It identifies issues a person might have and detect what their perception is over time. The COPM can help clients realize how much they have given up over time.
Summary
We need to help the Person to age in place by understanding the normal age-related and disease-related changes and identifying strategies to make accommodations for those.
Questions and Answers
How do you deal with unrealistic patient or caregiver expectations regarding aging in place? What information resources do you provide so that they are still motivated to participate and do not give up on occupational therapy?
I have some repeat offenders with this issue. Since I have started using the COPM, I would say this has decreased as it draws out those five things that they want to focus on and it engages them. We have then been able to problem-solve how to achieve these identified goals using a different approach. I am not going to say that it always works, but it does help with buy-in. I also keep it in a COPM booklet to track goals and see progress from beginning to the end. I also give people a lot of resources for where to find equipment. If they have VA benefits, I might recommend something like a stair glide to allow them to stay in their home. It is a less costly option than going into assisted living or a nursing home. Some people have said to me, "I really do not think you've helped me." However, they have come back later and have said, "I didn't want to listen before, but now I understand what you were trying to do."
Any tips for helping reluctant family members to buy into aging in place when your client wants to use that approach?
Some people do not realize and think that assisted living facilities are paid for by medical insurance. When they know this, they are more willing to look at options.
References
Citation
Dickson, Kelly (2018, February). Introduction: Defining the concept of aging in place. OccupationalTherapy.com, Article 4220. Retrieved from http://OccupationalTherapy.com.
