Introduction
Maternal health is one of these emerging practice areas for occupational therapy practitioners, and there are lots of ways to get involved. One of the areas that I am looking into is using ergonomics to help prevent musculoskeletal disorders. I am a mom of three young boys, but that is not really where my interest started. It came out of my clinical experience. About 10 years ago, when I was in outpatient hand therapy, I started getting an increase in referrals. There were new moms who were being referred in for de Quervain's tenosynovitis. They would get an injection from the doctor, and then he would send them to me for a splint. I made the splint and was then done with them. I did not feel that I was doing the best I could to help them. I felt I was putting a bandaid on the problem. Using my background and work in ergonomics, I started thinking about how we can do more activity modifications and be more client-centered. It was important to start looking at the underlying behaviors and help to fix them rather than just putting on a splint and receiving an injection. So, that is my background and interest.
New Mothers- A Special Population
If you look at the practice framework, caring for children is an IADL.

Figure 1. Childcare is an IADL.
We need to treat new moms as a special population because lots of people care for young children. It could be Mom, Dad, grandparents, other caregivers, daycare workers, or babysitters. There are people who care for these children, but really, mom is a specialized population. Childcare is physically and emotionally demanding. Mom usually has what could be considered a 24-hour workday because not only is she caring for her child during the day, but many times, she is also getting up during the night. There is constant vigilance in caregiving. Also, when Mom does get any downtime from child-rearing tasks, she is often doing other physically demanding tasks in the home or at work. There are also postnatal body changes which I will discuss in a few slides. The evidence points to an increased incidence of developing musculoskeletal disorders. There is a lack of knowledge or evidence out there of how exactly we can help that.
OT and Ergonomics
Ergonomics and occupational therapy fit really well together. We are used to thinking of ergonomics as being a skill for work in the industry but really it fits with occupational therapy. If you break it down, it uses our PEO concepts. Looking at the person, the environment, and the occupation, we make sure that there is a good fit between them. You are not just dumping a person into a job or a role and saying, "Do this job." There is an interaction between the person, the environment and the occupations with which they are engaging.
When we look at it this way, occupational therapy practitioners are really well suited to address ergonomic concerns both within and outside of work and industry. If we take the concepts that the AOTA uses to describe ergonomics and rework them for moms, it is going to look more like this.
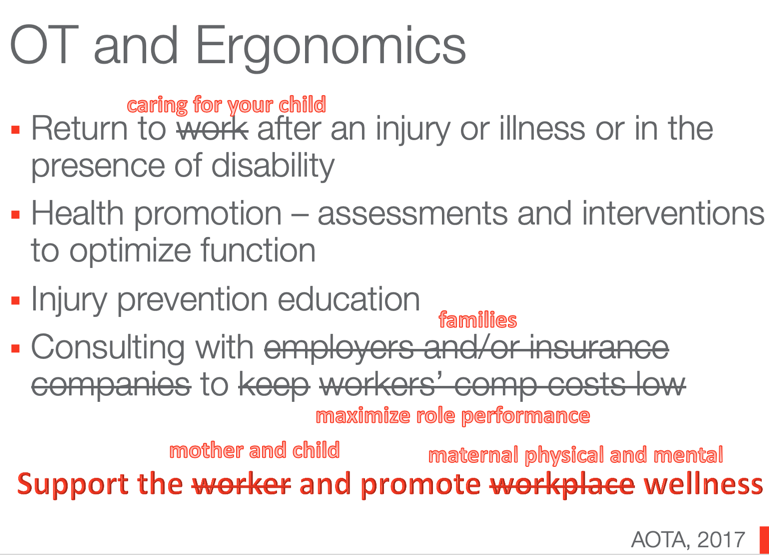
Figure 2. Adjusting the AOTA definition to include childcare.
First, we can help a mom to care for her child if she has an injury, like a musculoskeletal disorder, an illness, or a disability. Another area would be using the health promotion model to help mom do her job better, safer, or healthier. How can we help a mom prevent a musculoskeletal disorder, pain, or discomfort from occurring? We can also consult with families to help them maximize their role performance. Here is where these concepts are going to start to deviate a little bit because a mom is not going to get Workman's Compensation or days off if she starts feeling discomfort while doing her job. What we really need to do is help her and the whole family maximize their role performance. The overall goal here is really the same. We are going to decrease injuries, decrease fatigue, and look at decreasing aches and pains that are occurring while doing the job. We are also increasing productivity and workplace (or family) morale. We need to help them to enjoy activities outside of work to promote maternal, physical, and mental wellness. Traditional roles tell us that we can work with new moms to promote maternal health. But, additional skills are definitely available and useful to enhance your knowledge and ability to address moms' concerns. Sometimes, there is a general lack of awareness that occupational therapy can help fill this need as part of an interdisciplinary team within maternal health. There are plenty of studies to support our role in mental health if you look for them and not all of them are in the United States.
OT and Maternal Health
- Women are asking for more support and information in the perinatal time period
- A holistic perspective is needed
- Health promotion model and/or prevention model
- Serving the ‘well’ mom & baby population
- Occupational therapy can fill this need
- Various methods for delivering the information
- Face-to-face, virtually, print education
(Slootjes, McKinstry, & Kenny, 2016)
Here is a Dutch study where women were requesting more education about the postnatal time frame. They wanted the education to be focused on the physical, emotional, and psychosocial changes that occur postnatally. They needed to feel more prepared to take on the role and responsibility of motherhood. This study talked about how important it is to address this from a holistic standpoint and being client-centered. Again, it is a perfect fit within occupational therapy.
There was another study that looked at 92 first-time mothers. They talked to them eight weeks postpartum and the moms wanted to know more about stress management, mental health, and other supports to help them to parent. They did not feel like the best way to do this was just to give a handout and send them on their way. They really wanted to talk to somebody face-to-face, watch videos, or engage in a phone call. If a mom has a preexisting condition or the child has a disability, occupational therapy services are most likely going to be offered. But, what we need to do is shift the focus to offering these services for what is considered the "well population" as well.
Postpartum Care
- Association of Maternal & Child Health Programs
- “reimagine the postpartum visit and improve postpartum care and wellness” p.S39.
- Need for “mother-centered solutions” because we know that improving women’s health can improve maternal and infant health
- Will mom seek help?
(Cornell et al., 2016)
Here is something out of the Maternal and Child Health Journal. They also talked about strategies to increase postpartum health and wellness. However, this is coming from the Association of Maternal & Child Health Programs. Typically, a woman is going to have a six-week postpartum visit. This visit focuses on the health of her reproductive organs are healthy and discusses contraception going forward. But otherwise, mom is going to be spending most of the time visiting the pediatrician on a regular schedule, and there the focus is on the baby. We lose a little bit of the focus of helping mom. This article discusses the Association of Maternal & Child Health Programs and their idea of how to reimagine the postpartum visit to improve postpartum care and wellness. They feel that we need to provide a mother-centered solution. We know that improving mom's health is going to improve the overall maternal and infant health. The question becomes then, "Will moms seek out that help?" I like this graphic in Figure 3 that shows all the reasons that a mom might not be doing this due to all of the barriers in the system. It also highlights what we can do to support moms in making sure that those barriers either do not exist or helping her to overcome them.

Figure 3. Infographic used with permission from AMCHP (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5290048/).
This comes from the Association of Maternal & Child Health Programs. I know the College of Obstetricians and Gynecologists is also making new recommendations to push up the six-week visit, shorten the time period, and also make it a more comprehensive visit. This is a great opportunity for occupational therapy practitioners to jump on board and help here. During pregnancy, almost all women are going to experience some musculoskeletal discomfort, and as many as 25% of them are going to have disabling symptoms. The biggest culprit is going to be low back pain. Because of this discomfort, women are starting to stop engaging in at least one daily activity due to this pain.
Physiological Risk Factors
- Soft tissue edema
- Ligament laxity – relaxin & estrogen production
- Weight gain (+ ligament laxity = joint discomfort)
- Weakened core muscles: Abdominals, pelvic floor
- Sleep deprivation
- A shift in the center of gravity
- The emotional stress of new role (plus other roles)
(Borg-Stein & Dugan, 2007; Robson, Iqbal & Howarth, 2009)
One of the issues that are at play here is soft-tissue edema or fluid retention. This is going to begin during pregnancy and is still resolving in the postpartum days. Another one is ligament laxity. This happens throughout pregnancy as well because of the increased production of relaxin and estrogen. That ligament laxity, along with the weight gain that occurs, is a recipe for joint discomfort. In addition, the core muscles are weakened as the body prepares for the expanding size of the baby. The abdominal muscles start to separate, and this occurs in the second and third trimester, or it can occur as a result of pushing during delivery and lead to something called diastasis recti. This is also going to contribute to a risk of back injury due to poor posture. There is a long list of risk factors of why this occurs including mom's exercise status before pregnancy, size of the baby, over the age of 35, size of the pelvis, and single vs. multiple children. It is estimated that 30 to 60% of women are going to experience this. And, up to 45% of them will still have diastasis recti six months postpartum. Those are large numbers. Pelvic floor muscles are also going to be affected. They work hand in hand with the transverse abdominis and the deep abdominal muscles to help support posture. Moms are also obviously undergoing sleep deprivation as they are waking often to attend to the baby's needs and feeding schedule. There is going to be a shift in the center of gravity because pregnancy distorts the natural curvature of the spine, and it is not going to just immediate correct itself after childbirth. I will talk about that a little bit later as well. Finally, there is the emotional stress of being a new mom while maintaining all of your other roles.
Health Risks of Motherhood: Slippery Slope
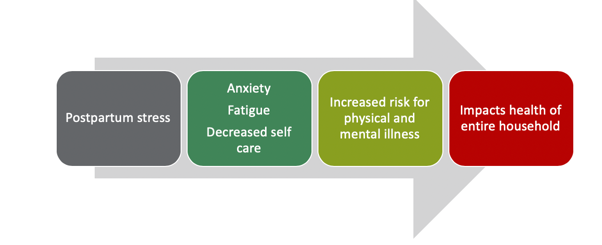
Figure 4. Slippery slope. (Fahey & Shenassa, 2013)
This is what I call the slippery slope of motherhood or the health risks that lead to the slippery slope. We already said that there is a lot of postpartum stress, and if you do not address that postpartum stress, it can lead to anxiety, fatigue, decreased self-care. This is going to put mom at risk for either physical or mental illness or other disorders like postpartum depression. This is going to impact the health of the entire household. Other things can occur like early discontinuation of breastfeeding, a negative maternal perception of the infant, and a compromised attachment. It can also lead to delayed language acquisition or behavioral problems in the child.
Link to Postpartum Depression
- The connection between body posture, pain & PPD
- Back pain may be a risk factor and comorbidity of PPD
- Mental and physical symptoms & changes are interdependent (Angelo et al., 2014)
- Connection between exercise/wellness interventions & PPD prevention
- Exercise has psychosocial impact postpartum
- Weight loss
- Less costly & time-intensive than other interventions
- Teaches healthy behaviors to engage in the long term (Lewis et al., 2018)
- Exercise has psychosocial impact postpartum
There are links to postpartum depression as well. A study by Angelo and Colleagues in 2014 talked about the influence of body posture on postpartum depression and pain. It was a Brazilan study that looked at 80 women with postpartum depression. They also had back pain that intensified and exacerbated with changes in postural alignment that happened at six weeks postpartum. They felt the pain had a connection with postpartum depression, and that back pain specifically, could both be a risk factor and comorbidity of postpartum depression. What I also liked about the study was they talked about how physical and mental disorders are interdependent. Thus, you cannot look at one without looking at the other as they are going to influence each other. If one is occurring, those physical symptoms could lead to mental issues that mom could be experiencing.
Another study by Lewis and Colleagues in 2018 talked about collecting data for the Healthy Mom II Trial. They looked at exercise and wellness interventions to prevent postpartum depression. Exercise is a known intervention for depression already, but they tried to create evidence to say that exercise could be an intervention for postpartum depression specifically. They collected baseline data and have about 450 participants now. The idea is that exercise is advantageous psychosocially due to its impact on mom's weight loss after having the baby. Other psychosocial interventions, like counseling, are going to be costly and time-intensive, and exercise will help to teach motivation for healthy behaviors that are longterm and can impact health in a more longterm way. The connection here is that exercise is also advantageous for reducing musculoskeletal disorders by preparing the body for birth, helping the body to recover from birth, and being able to perform the demands of the child-care tasks.
Prevention & Health Promotion
- “Using an evidence-based approach, occupational therapy practitioners can contribute to preventing pain, increasing function, and promoting meaningful occupations during pregnancy and the postpartum period” (p.1).
- OT practitioners are seeing women during the perinatal period in clinics with musculoskeletal diagnoses
- Women expect pain/discomfort during the perinatal period – may not talk about it
- OT can address issues preventatively via health promotion
(Fernandes, 2018)
Using a health promotion model is important. Here is an article from the American Journal of Occupational Therapy that was recently published. It says if mom is not going to seek out help, can we approach this from a wellness and health promotion model? She may not seek out help once symptoms are occurring. OT practitioners are seeing women during this perinatal period in clinics with musculoskeletal complaints and conditions that are already kind of brewing and developing. We need to educate those women and families to change their habits and to modify their childcare techniques in order to halt the injury progression and positively affect the way they approach future pregnancies and children. I have seen this firsthand with some mothers that I have worked within the clinic. Many moms report that injuries are impacting their ability to care for their children and making them think twice about expanding their family in the future.
