Amanda: Hello, everyone. Thank you for logging in today to hear the presentation about Returning to Activity Following Concussion. The topic of concussion is a hot topic right now. It is in all the news, and it is an area in which occupational therapy can have a huge impact on clients' recovery.
Concussion
Definition
According to the CDC (2016), a concussion is a type of traumatic brain injury, or TBI, caused by a bump, blow, or jolt to the head, or a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull, stretching and damaging the brain cells and creating chemical changes in the brain.
Incidence
When we talk about the incidence of concussion, we do not know how many individuals are sustaining a concussion each year.
- 1.6 million to 3.8 million annually (Langlois et al., 2006)
- Number likely to be higher due to the incidence of unrecognized concussions
- National Concussion Surveillance System
- Current data systems may only capture 1 out 9
- Promote prevention, treatment, and recovery
- Causes:
- Sports-Related Concussion (SRC)-most common
- Falls
- Car Accidents
- Work Injuries
There are some estimates out there that it is somewhere between 1.6 million to 3.8 million annually. But there is also a lot of reporting, that says this number is much higher, most likely, because of unrecognized concussions and underreporting.
Signs and Symptoms
An unrecognized concussion is when someone may be experiencing signs and symptoms, but they do not realize that it is because they have injured their brain.
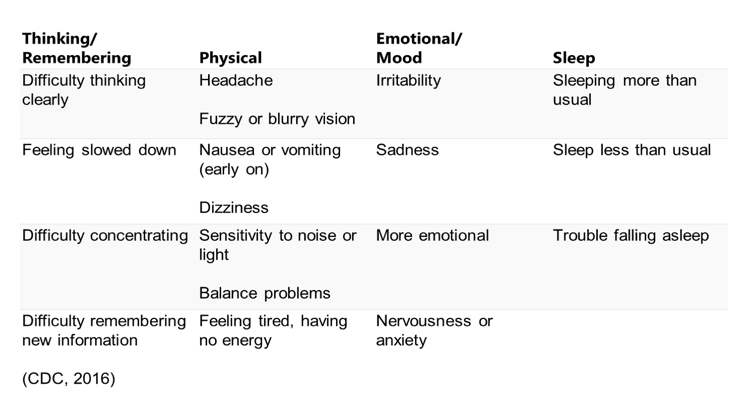
Figure 1. Signs and symptoms of a concussion.
Another reason for the underreporting is that a lot of times people do not want to report that they have had an injury. It may prevent them from playing a sport, going back to work safely, or doing the things that they need to do every day. The CDC is working on developing and building a national concussion surveillance system because the current data systems may only capture one out of nine people that have sustained a concussion. The goal of this is that if they can determine how many people are experiencing a concussion, they can look at prevention, treatment and if there are any patterns emerging.
The most common way concussions occur are through sports-related injuries. This is what is most often seen in the media and probably receives the most attention. However, there are also a lot of injuries that happen from falls, car accidents, and work injuries. Those are just a few of the examples where I have seen the most concussions in our clinic.
What we know about diagnosing a concussion is that it is not as simple as having them get a CT scan or an MRI and seeing where the damage is. A lot of times the diagnosis revolves around these signs and symptoms, what they are experiencing, and how these affect their ability to do everyday activities. They typically fall into four categories and depending upon which signs and symptoms, charts, or checklist that you look at, some of them may be broken up into more categories. However, these are the typical symptoms that you are going to see on most of the different checklists. It is really important that we get a good idea of how the clients are experiencing these signs and symptoms based on the severity so that we can better establish how they are improving. W will talk more about this as we go along.
Recovery from Concussion
- Recovery time refers to the amount of time required to recover from symptoms resulting from a concussion
- Average recovery time is about 7-10 days
- 90% of concussions sustained during sports fully recover within 30 days (McCrea et al., 2003; Meehan et al., 2014; Zuckerman et al., 2012)
- Factors affecting recovery:
- Severity and duration of symptoms
- Type of symptoms present
- Age and gender
- History of previous concussion
(Castille et al., 2012; Conder & Conder, 2015; Giza & Kutcher, 2014; Guskiewicz et al., 2003; Majerske et al., 2008; McClincy et al., 2006; Meehan et al, 2014; Shim et al, 2015; Wasserman et al., 2015)
Recovery time for a concussion is one of the big areas that has changed over the past few years. The thought used to be that patients needed a lot of rest right after it happened. The average recovery time is seven to 10 days or seven to 14 days. A new study that came out in 2017 talked about that college students may take longer to recover than maybe pediatric patients, and that females often took longer to recover than male clients. And, if you have a history of previous concussion, this could also increase recovery time. Around 90% of people who sustain a concussion usually recover within 30 days. Now, this is where occupational therapy can be an asset. We can help individuals return to their everyday activities. During the initial few weeks, I do not typically see a lot of my clients. I may get a consult or something saying, "Need to progress back into school or back into work." Sometimes, the doctors manage the symptoms. Where I see most of my patients is when they do not recover quickly, and they cannot return to their previous level of functioning. This is where we can make a huge impact because it is just like treating anyone else or anybody else that has a brain injury. We are not necessarily treating the diagnosis. We are treating the things that are limiting them from being able to do those activities that they want to do and need to do.
Guiding Principles of Recovery
There are some guiding principles of recovery for concussion regardless of the type of activities that they are trying to get back to, and this is what we are primarily going to talk about today.
- Cognitive rest is usually recommended for the first 24-48 hours after injury when symptoms are most severe
- Extended cognitive and physical rest may not improve recovery time
- Avoid activities in all environments (e.g., home, work, leisure) that are known to exacerbate signs and symptoms which may prolong recovery
- Adapt the environment and activity requirements:
- Implement strategies and accommodations
- Facilitate a gradual, progressive plan to engage in functional activities while managing symptoms
(Acord-Vira, et al., 2018; Baker, 2014, Buckley et al., 2016, Giza et al., 2013; Hall et al., 2015; Harmon et al., 2013; McCrory et al., 2013b)
How do we help individuals get back to doing those everyday activities? Usually, cognitive rest is only recommended for the first day or two, and those are usually when the symptoms are most severe. There have been some studies that say cognitive and physical rest may not improve their recovery time, and in some situations, it actually can make it worse. Because if you avoid everything and you rest, trying to return to those activities can be very overwhelming and actually can cause your symptoms to be worse. As you are returning to some activities, the important thing is that you try to avoid the activities that are known to make your signs and symptoms worse. If every time you turn on the TV you get a headache, you quit turning on the TV. If working on the computer is causing you trouble, then stop working on the computer. If being in a classroom all day is the problem, then is there a different way that you could get the material? We need to adapt to the environment and activity requirements. We can implement different strategies and accommodations, and we will talk about some of these in the case studies at the end.
We also want to facilitate a gradual progressive plan to engage in these functional activities while we also manage the symptoms. That is the key piece. We have to help them grade and progress while we are making sure that we are not making their symptoms worse. We want to take to them to their max ability to do it, without them experiencing extensive symptoms. Once they start experiencing those symptoms, it may prolong their recovery.
Occupational Therapy's Role
Where does that put OT?
- Use the occupational profile to guide intervention plan
- Goal setting
- Holistic client-centered approaches to treatment
- Grade and accommodate activities to maximize performance for returning to occupation
- Return to Learn
- Return to Work
- Return to Play
- Modify routines and habits to facilitate recovery
- Education on managing symptoms
- Remediate client factors and performance skills
(Brayton et al., 2016, Parkinson, n.d.; AOTA Tip Sheet, 2014)
When I think about clients and concussion, what they need most is help getting back to doing those everyday activities. They need to develop strategies and abilities to advocate for what they need to be able to reemerge and do their everyday activities. I have had several patients that have been referred to a different discipline, where they have worked on some of those skills and things to improve their dizziness, improve their balance, or improve their vision, but clients still indicate, "I can't go back to school. I can't go back to work. I'm still having trouble." And, a lot of times when these injuries go on for a period of time, that is when employers or school personnel start questioning it. "Why is this taking so long? Why is it you're having trouble with those things?" Many times, the patients cannot put that into words. They just know they are not performing to the way they were before their accident.
We have a huge role that we could play in concussion recovery. It is an emerging area. I truly believe that we should develop concussion clinics that occupational therapy run and participate in. We are also a part of a multi-disciplinary team that is addressing the needs of clients that get a concussion. Some of the things that we do are complete an occupational profile, work on goal setting, and make sure that our patients are engaging in activities they want to do. When the client is engaged, motivated, and able to understand why they are doing what they are doing, it improves their performance. We are the professionals that work to grade and accommodate activities.
There are some guidelines that are out there that can help us with that. Most of us have heard of "return to play" guidelines. Those are where you start with no activity and you start to build up with light aerobic activity until you can get all the way to being able to participate back in your sport. The other two are not as well known. Return to learn actually has not been emphasized until recently. There is not an exact step progression like there is with a return to play. However, there are different ones that can guide you. Finally, return to work has probably received the least amount of information about how we should go about it, but there is some articles and things out there that can help. One of the other things that we do is we help individuals modify their routines and habits. We can educate on how to manage symptoms. We can also help clients remediate client factors and performance skills, or the things that may be impairing their ability to do everyday activities.
Evaluation
Our evaluation needs to look at everything that we typically assess because concussions can affect an individual's ability to participate in everything.
- A concussion can affect an individual’s ability to participate in:
- Activities of daily living
- Instrumental activities of daily living
- School
- Work
- Driving
- Leisure
- Top-Down Approach
- Occupational Profile
- Analysis of Occupational Performance (Baseline)
- Observation: direction following, attention, frustration, fatigue
I had a client's concussion impact her sleep routine which affected her ability to get up in the morning and do her self-care. I have another client who was so fatigued that she could not manage a lot of her daily activities at home. She had to rely on a lot of people to help her with cooking, cleaning, grocery shopping, and paying bills. We have clients that have difficulty managing a full course load, completing assignments, taking tests, or receiving the grades that they had before. Students can get really far behind really fast, and so we do worry about them being able to catch up. If they are higher up in school, like in their high school years or in college, it can be even more detrimental to like their livelihood and aspirations for what they want to be.
Work performance can also be affected. If all of a sudden physically you look fine, but due to cognitive changes you cannot work independently or up to your fullest potential, then this is a significant problem. And, if you are not getting the help and care that you need, this may affect job performance.
Some patients report driving as a problem. They may have problems with their vision or light sensitivity. Leisure is another big area. Patients often report that they are not able to engage with their friends and their social networks as much. They may have trouble keeping up with conversations because of poor attention skills. Sometimes they get a little irritable because there is a lot going on and it can be noisy.
We need to utilize a top-down approach with these clients. It is very important to figure out what it is they can not do. Sometimes when we have physical impairments, it is easier to describe and understand. If someone was lacking the range of motion in their shoulder, we really do not know that it is a problem until we assess them completing functional activities. Likewise, when we are assessing patients that have cognitive deficits, we want to see if it is affecting their performance. Sometimes if you just do a cognitive assessment, you may not see all the impairments and the problems. But if you do some of these occupational type things, this is where things start to fall apart because these tasks require higher executive functioning skills. Fatigue is another one that can impact our client's ability to do everyday activities.
Occupational Profile
Where do we start?
- AOTA Occupational Profile Template
- Canadian Occupational Performance Measure
- Occupational Self-Assessment
- Occupational Performance History Interview (OPHI-II)
- Activity Card Sort
AOTA has really done a nice job of developing an occupational profile template. Specifically with concussion, taking this approach has really helped me see what the clients are truly having trouble doing. As we were developing the concussion clinic here at our clinic, we spent a lot of time trying to look for measures that would address specific things that people with a concussion may be experiencing. Sometimes it scares therapists to treat someone that is very high functioning. What type of things do you do? This occupational profile really helps us see what the problems are because it does require some creativity, some grading and being able to truly analyze all the different aspects of ADLs and activities that we engage in.
The other one that I have been using a fair amount is the COPM. I really like the COPM specifically with this population because it detects the client's self-perception of their performance and their satisfaction over time. It does cost a little bit, but it is not too bad. Clients may struggle to tell you everything that is happening or they miss things. By using one of these measures, you can go down through a checklist and see where the concussion is impacting them. In some of the case studies, you will see how this comes into play. This is probably the most important tool that I have used during an evaluation to guide intervention planning.
